Abstract
Long intergenic noncoding RNAs are transcripts originating from the regions without annotated coding genes. They are located mainly in the nucleus and regulate gene expression. Long intergenic noncoding RNAs can be also found in the cytoplasm acting as molecular sponges of certain microRNAs. This is crucial in various biological and signaling pathways. Expression levels of many long intergenic noncoding RNAs are disease related. In this article, we focus on the long intergenic noncoding RNAs and their relation to different types of cancer. Studies showed that abnormal expression of long intergenic noncoding RNA deregulates signaling pathways due to the disrupted free microRNA pool. Hampered signaling pathways leads to abnormal cell proliferation and restricts cell death, thus resulting in oncogenesis. This review highlights promising therapeutic targets and enables the identification of potential biomarkers specific for a certain type of cancer. Moreover, we provide an outline of long intergenic noncoding RNAs/microRNA axes, which might be applied in further detailed experiments broadening our knowledge about the cellular role of those RNA species.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Abnormal long intergenic noncoding RNA expression affects microRNA availability and function in cancer cells. |
The same long intergenic noncoding RNA may be involved in different cancers and may interact with different microRNAs depending on cancer type. |
Knowledge about biological pathways affected by long intergenic noncoding RNAs can provide new ideas for future research, diagnosis, and treatment of these diseases. |
1 Introduction
As much as 98% of the human genome does not encode proteins [1]. It was initially assumed that noncoding transcripts play no role, however, subsequent research has shown that noncoding RNAs provide an important source of knowledge that allows for a better understanding of cellular processes.
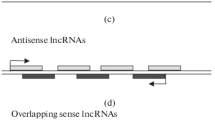
We can distinguish noncoding transcripts by length. Transcripts smaller than 200 nucleotides are called small noncoding RNAs; they include tRNAs, rRNAs, microRNAs (miRNAs), snoRNAs, and pi-RNAs. Long noncoding RNAs (lncRNAs) are noncoding RNAs longer than 200 nucleotides [2]. According to published studies, lncRNAs can be spliced and polyadenylated. These transcripts possess a 5′ terminal cap structure, which is a characteristic of mRNAs [3]. The lncRNAs generally do not have coding potential because of the lack of both open reading frames and translation termination regions [4]. Long noncoding RNAs include intergenic, intronic, sense, and antisense transcripts [5].
Long intergenic noncoding RNAs (lincRNAs) were first observed because of the usage of tiling arrays for the analysis of genomic sequences, as transcripts derived from the regions without known protein coding genes [6]. Although recent findings revealed that some of them might be the source of micropeptides, for example, LINC01420 [7]. Long intergenic noncoding RNAs have a variable conservation pattern. Only a minority of them can have both a highly conserved sequence and a secondary structure, this includes MALAT1 (metastasis associated lung adenocarcinoma transcript 1). At the sequence level, many lincRNA transcripts have variable conservation at their 3′ end, exemplified by the oncogene PVT1 (plasmacytoma variant translocation 1) [6]. One aspect of evolutionary conservation is shared between lincRNAs and protein-coding RNAs, and it concerns the promoter region. In both cases, promoter sequences are highly conserved, although the expression levels of lincRNAs are lower than those of coding RNAs [8].
Long intergenic noncoding RNAs are mainly located in the nucleus, where they are involved in gene expression control owing to the recruitment of specific enzymes that modify chromatin to activate or repress gene expression (Fig. 1A) [9]. Additionally, lincRNAs can regulate splicing events by sequestration of splicing factors, for example, MALAT1 within nuclear paraspeckles (Fig. 1B) [6]. At the translational level, lincRNAs can bind mRNAs by complementarity, thus influencing their translation (Fig. 1C) [10]. Moreover, lincRNAs can form complexes with proteins, which can inhibit function or even lead to degradation of the bounded peptide (Fig. 1D, E) [6]. In the nucleus, the lincRNAs can form scaffolds for proteins thus affecting chromatin availability, nucleus architecture, and gene expression (Fig. 1F) [11].
A Long noncoding RNA (lincRNA) recruit chromatin-modifying enzymes. Transcription is activated or inhibited. B Splicing activator and inhibitor are bound by lincRNA, which allows them to bind to the target gene. Splicing is activated or inhibited. C LincRNA binds to target mRNA. The translation is disabled. D Binding of the protein to the lincRNA prevents them from interacting with the target gene. E Binding of lincRNA to protein leads to protein ubiquitination. Protein is degraded. F LincRNA binds to protein and serves as scaffold. Protein can bind to the target gene. G In the lack of lincRNA, microRNAs bind to mRNA leading to its degradation, there is no expression. If present, lincRNA acts as a molecular sponge for microRNAs. The action of lincRNA ensures that mRNA is not degraded, which enables its expression
In addition, lincRNAs can sequester miRNAs and prevent them from forming RNA-induced silencing complexes and therefore from interacting with target mRNAs (Fig. 1G) [6]. MicroRNAs are 22-nucleotide-long RNA molecules. Each miRNA regulates expression of multiple genes, and each mRNA can be targeted by numerous miRNAs. Interplay between those molecules is possible owing to the highly conserved seed sequence located at the 5′ end of miRNA. Interaction occurs usually at the 3′-untranslated region of targeted mRNA as a result of perfect or near-perfect base-pair complementarities [12]. Sequestration of miRNAs by lincRNA is referred to as “microRNA sponging,” and it is an indirect means by which lincRNAs can regulate the levels of factors involved in biological and signaling pathways, and it is highly prevalent in cancer cells (Table 1). Through this function, lincRNAs can act as oncogenes or tumor suppressors. For example, LINC00152 and CDK9 (cyclin-dependent kinase 9) mRNA can both bind miR-193a through complementary binding sites in the 3′-untranslated regions; dysregulation of this LINC00152/miR-193a/CDK9 axis leads to the development of acute myeloid leukemia (Table 2).
Many lincRNAs in the human genome are involved in cancer-related biological processes. Errors in their sequence, dysregulation, and abnormal expression can lead to the development of neoplastic conditions (Fig. 2, Table 2). Studies of the human genome have indicated that many single nucleotide polymorphisms are found in intergenic or intron regions and can affect the function of lincRNAs [13]. Recently, bioinformatical tools enabled the prediction and identification of many cancer-related lincRNAs before in vitro research is conducted, for example, DRACA (detecting lncRNA cancer association) [14]. In addition, one can use modern databases annotating lncRNAs from RNA sequencing performed on cancer samples, such as lncExplore [15]. There is a high demand for experimental research to better understand the functions of many lincRNAs. This knowledge could lead to the identification of potential drug targets or cancer biomarkers [8].
This article provides data on different types of cancers and the respective lincRNAs involved in these cancers. We focus on leukemia, thyroid cancer (TC), glioblastoma, nasopharyngeal carcinoma (NPC), colorectal cancer (CRC), cutaneous squamous cell carcinoma (CSCC), esophageal squamous cell carcinoma (ESCC), and gastric cancer (GC) (summarized in Table 1, Fig. 2]). Because of publishing limitations, this review presents select examples of cancer-related lincRNAs, which act by inhibiting miRNA regulatory pathways. We describe lincRNA/miRNA axes to bring the readers closer to the biological and signaling pathways underlying particular cancer (summarized in Table 2).
2 LincRNAs in Different Cancer Types
2.1 Leukemia
Leukemia is cancer of the body’s blood-forming tissues, including the bone marrow and the lymphatic system. Many types of leukemia exist. They are grouped in two ways: by how rapidly the disease develops (acute and chronic leukemia) and by the type of blood cell involved (lymphoblastic and myeloid leukemia). In acute leukemia, bone marrow cells are immature and are unable to function normally. The number of abnormal cells increases rapidly. In chronic leukemia, cells are more mature and can carry out some of their normal functions. The number of abnormal cells increases more slowly. The most common types of leukemia are acute lymphocytic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia, and chronic myeloid leukemia [16]. Acute myeloid leukemia is marked by the abnormal abundance of clonal myeloid progenitor cells in the bone marrow and the repression of normal hematopoiesis [17, 18]. Many different genomic mutations, epigenetic aberrations, or abnormalities in gene expression could contribute to AML progression [17, 18]. Acute myeloid leukemia is characterized by a low survival rate, and the risk of AML increases with age [17, 18]. Acute lymphocytic leukemia is a cancer that begins in the bone marrow by generating large numbers of abnormal blood cells, including B and T lymphocytes as well as innate lymphoid cells [19]. Acute lymphocytic leukemia reaches peak incidence in the age group of 1–4 years. Factors promoting the development of ALL include chromosomal abnormalities and genetic changes related to the differentiation and proliferation of lymphoid precursor cells, as well as environmental conditions [20].
Analysis of nucleated bone marrow cell samples from 32 patients with AML and 32 healthy donors revealed that NEAT1 (nuclear paraspeckle assembly transcript 1) levels are significantly reduced in AML tissues. The change in NEAT1 expression is reflected in the intensity of cell proliferation, migration, invasion, and apoptosis [21,22,23]. One of the axes controlled by NEAT1 is NEAT1/miR-338-3p/CREBRF (regulatory factor CREB3). Acting as a molecular sponge, NEAT1 binds directly to miR-338-3p, which in turn leads to an increased level of its target, CREBRF mRNA. CREBRF is involved in the induction of cell apoptosis through the endoplasmic reticulum stress pathway. In AML, a low level of NEAT1 expression affects the miR-338-3p/CREBRF axis, leading to a reduction in CREBRF expression and the progression of the disease [21]. NEAT1 is also part of the NEAT1/miR-23a-3p/SMC1A (structural maintenance of chromosome 1 alpha) axis, as described in research of peripheral blood mononuclear cells derived from three patients with AML and three healthy donors. The SMC1A gene encodes the fundamental subunit of the cohesin complex, which plays a key role in the functioning of chromosomes as well as gene regulation; its implication in several cancers has already been described [24, 25]. In AML, a low level of NEAT1 accounts for a high level of miR-23a-3p and thus a lower level of SMC1A, which contributes to the development of AML [22]. Subsequent studies have revealed that the NEAT1 level can be regulated in AML through the miR-194-5p/DNMT3A (DNA methyltransferase 3 alpha) pathway. In healthy bone marrow cells, miR-194-5p targets and downregulates DNMT3A, one of the DNA methyltransferases, which is responsible for influencing the structure of chromatin, gene silencing, and disease development. DNMT3A can also methylate the NEAT1 gene. Researchers obtained monocytes separated from a bone marrow sample of 30 patients diagnosed with AML and 30 healthy volunteers and observed low expression of miR-194-5p in AML cells and consistently high expression of DNMT3A, increased methylation of the NEAT1 gene, inhibition of its transcription, and finally the development of AML [23].
Contrary to AML, research carried out on a group of 25 patients with T-cell acute lymphoblastic leukemia (T-ALL) and 25 healthy people, as well as T-ALL cell lines, revealed that NEAT1 expression is significantly higher in diseased cells, and this may explain the increased proliferation of T-ALL lymphocytes. NEAT1 has been associated with miR-146b-5p, which targets NOTCH1 mRNA [26]. A higher level of NOTCH1, which is the key protein in the NOTCH signaling pathway in T-ALL, stimulates regulators of cell proliferation to give cells a strong growth advantage [26, 27]. NOTCH signaling is an evolutionarily conserved pathway, involved in activation of the transcription of the target genes regulating cell growth and differentiation. NOTCH signaling deeply participates in the development and homeostasis of multiple tissues and organs, the aberration of which results in cancerous and noncancerous diseases [28]. In turn, negative regulation of miR-146b-5p contributes to the mobility of leukemia cells and their migration, invasion, and disease aggressiveness [26]. Moreover, scientists reported that NEAT1 can bind miR-335-3p, which in turn regulates the level of ABCA3 (member 3 of the ATP subfamily of the ATP binding cassette) and induces drug resistance in childhood ALL [29]. However, the mechanism by which ABCA3 affects drug resistance has not yet been elucidated.
Studies conducted with AML cell lines demonstrated upregulation of lincRNA UCA1 (urothelial cancer associated 1) and described how UCA1 influences cell proliferation, migration, and invasion, as well as cell apoptosis in AML. On the molecular level, UCA1 regulates tumor progression by affecting the miR-296-3p/MYC (MYC proto-oncogene, BHLH transcription factor) axis, which in turn leads to the enhancement of MYC mRNA. MYC is a proto-oncogene that acts as a regulator of cell proliferation and apoptosis [30]. Upregulated UCA1 also promotes proliferation of AML cells by inducing autophagy through the miR-96-5p/ATG7 (autophagy related 7) axis. In this axis, by sequestering miR-96-5p, UCA1 triggers overexpression of ATG7 [31]. ATG7 is an E1-like activating enzyme necessary for autophagy and cytoplasm-to-vacuole transport, which plays a significant role in cancer progression [31, 32].
Moreover, LINC00467 expression is significantly increased in tissues with AML but only in patients who achieved complete remission. For this study, samples were taken from 134 patients with AML and 40 healthy volunteers. LINC00467 is involved in promoting the development of many solid tumors, influencing apoptosis, invasive capacity, and metastasis in AML. LINC00467 has been shown to promote the progression of AML by sponging miR-339 and thus indirectly contributing to an increase in the expression level of its target, SKI (V-SKI avian sarcoma viral oncogene homolog). SKI is a proto-oncogene that acts as a repressor of transforming growth factor beta-1, a protein that regulates proliferation, differentiation, and cell growth. Knockdown of LINC00467 level in AML cell lines inhibited the development of this tumor [33].
The studies carried out on human bone marrow stromal cell lines and AML cell lines revealed upregulated levels of miR-4260, which was further found to be bound by LINC01128. The target of miR-4260 is the mRNA of the NR3C2 (nuclear receptor subfamily 3 group C member 2) gene. Both LINC01128 and NR3C2 transcript levels were reduced in AML samples [34]. NR3C2 is a mineralocorticoid receptor that can regulate electrolyte balance and has been shown to inhibit tumor progression by inhibiting proliferation, migration, and invasion, as well as epithelial-mesenchymal transition (EMT) [34]. Epithelial-mesenchymal transition is a process by which epithelial cells gain migratory and invasive properties, losing their cell polarity and cell–cell adhesion, and acquiring the phenotype of the mesenchymal stem cells [35]. Epithelial-mesenchymal transition is involved in many fundamental processes, including embryonic evolution, tissue formation, wound healing, and tissue fibrosis. Moreover, there are many reports about EMT as a part in the metastasis of tumor cells [36, 37].
Based on the bioinformatic analyses using The Cancer Genome Atlas and Gene Expression Profiling Interactive Analysis databases, LINC00899 expression level is also elevated in AML and this is significantly correlated with a poor prognosis for patients with AML. The discovery was further confirmed by checking the expression level of LINC00899 in peripheral blood mononuclear cells of 380 patients with AML. Next, experiments on AML cell lines showed that LINC00899 can promote cell proliferation and inhibit cell apoptosis in AML cells [38]. The mechanism of action of LINC00899 is based on sponging of miR-744-3p, which is accompanied by upregulation of the level of its direct target, the transcription factor YY1 mRNA. YY1 acts as an activator-specific repressor in many cancers and may also modulate AML cell proliferation and apoptosis, regulated by LINC00899 [38].
Another lincRNA upregulated in AML is MALAT1. Research on MALAT1 was carried out in a group of 20 patients with AML and a control group of 20 healthy donors with hematopoietic stem cells. The scientists showed that MALAT1 acts as a molecular sponge for miR-146a, decreasing its level in AML cells. The target gene for miR-146a is CXCR4 (C-X-C motif chemokine receptor 4); therefore, the CXCR4 protein is upregulated in patients with AML. CXCR4 mediates migration, adhesion, and drug resistance, promoting metastasis and progression of AML [39].
In turn, research describing the role of MALAT1 in ALL was conducted by Song et al. on peripheral blood mononuclear cells derived from 16 patients with ALL and 16 healthy patients as well as on ALL cell lines. In ALL cells analyzed, the level of MALAT1 was upregulated and correlated with the expression level of PTK7 (protein tyrosine kinase-7), which is a tyrosine kinase receptor involved in the regulation of the Wnt signaling pathway [40, 41]. Through activating the receptor of the kinase insert domain, PTK7 can promote tumor progression by increasing the capacity for proliferation, migration, invasion, and angiogenesis, as well as inhibiting apoptosis. In healthy tissues, the level of PTK7 is negatively regulated by miR-205, which in turn is antagonized by MALAT1. In ALL cells, overexpressed MALAT1 downregulates the miR-205 level, which affects the control of PTK7, resulting in induced proliferation and inhibited apoptosis [40]. Another MALAT1 parallel function has been described for T-ALL. Upregulation of MALAT1 was confirmed in a study conducted in a group of 64 samples from children with ALL and 30 healthy children. Scientists have reported that MALAT1, similar to NEAT1, can bind to miR-335-3p, which in turn regulates the level of ABCA3. As mentioned previously, an increase in ABCA3 levels might contribute to drug resistance in childhood ALL [29].
An elevated level of LINC00152 expression was detected in bone marrow samples taken from 33 patients with AML and was correlated with poor patient outcomes. Samples from 15 healthy donors served as a control. Furthermore, scientists showed that upregulated LINC00152 accelerates proliferation and inhibits apoptosis and cell-cycle arrest in AML by targeting the miR-193a/CDK9 axis. LINC00152 and CDK9 mRNA can bind miR-193a through complementary binding sites in the 3′-untranslated regions. CDK9 is known as an oncogenic gene in human cancers [42], and its expression is elevated in AML. The CDK9 protein belongs to the CDK (cyclin-dependent kinase) family, members of which are known to be important regulators of the cell cycle. CDK9 is also a component of the multiprotein TAK/P-TEFb complex, which is a transcription extension factor driven by RNA polymerase II [43]. In addition to LINC00152 and CDK9, miR-193a also hybridizes with many other target gene mRNAs, such as AML1/ETO (fusion gene RUNX1/RUNX1T1), DNMT3A, HDAC3 (histone deacetylase 3), KIT (KIT proto-oncogene, receptor tyrosine kinase), and CCND1 (cyclin D1), encoding proteins involved in the regulation of cell differentiation, cell proliferation, cell-cycle progression, and cell survival. miR-193a inhibits their expression in healthy cells therefore preventing tumorigenesis [42].
Another lincRNA overexpressed in ALL is H19 (H19 imprinted maternally expressed transcript). H19 levels were measured in 50 bone marrow samples taken from children under 12 years of age, including 33 cases with pediatric ALL and 17 controls. H19 has been identified as an oncogenic factor that leads to ALL due to the H19/miR-326/BCL-2 (BCL2 apoptosis regulator) axis, in which H19 sponges miR-326 and thus indirectly upregulates its target BCL-2 [44]. miR-326 has already been reported as a new diagnostic and prognostic factor for drug resistance in pediatric ALL [45]. BCL-2 is a potential oncogene in ALL, and its overexpression was shown to promote leukemogenesis in a mouse B-cell lymphoma/leukemia model. Furthermore, c-MYC was shown to directly induce H19 by binding to its promoter proximal E-box and inducing acetylation of histone H3 and H4 and recruitment of RNA polymerase II, potentially promoting oncogenesis [46]. Accordingly, Mofidi et al. hypothesized a possible network of interactions between all four factors, in which overexpression of BCL-2 is responsible for the induction of H19 by c-MYC. Subsequently, overexpressed H19 may upregulate BCL-2 through regulation of miR-326 levels. Further analysis based on available data revealed other oncogenes modulated by H19, such as ID2 (inhibitor of DNA binding 2), Bcr-Abl (breakpoint cluster region/Abelson), Let-7 (Lethal-7), and EZH2, as well as tumor suppressors inactivated by H19, such as TP53, RB (RB transcriptional corepressor 1), and RUNX1 (RUNX family transcription factor 1). Therefore, lincRNA H19 may act as an oncogenic factor that induces leukemia in ALL through a variety of mechanisms [44].
Analysis of bone marrow samples taken from 62 patients diagnosed with AML and 20 healthy people as a control group revealed increased expression of XIST (X inactive-specific transcript) in AML cells as well. High XIST expression in AML cells resulted in higher cellular activity and drug resistance and inhibited apoptosis. Along with XIST, MYC showed elevated levels in AML cells. Scientists showed the existence of a molecular axis in which XIST indirectly upregulates the expression of the MYC oncogene due to sponging of miR-29a. As mentioned above, MYC can modulate cell proliferation, survival, and metabolism by regulating gene expression. Silencing XIST inhibited neoplastic AML cells in vivo and led to a reduction in MYC expression via miR-29a, thereby reducing drug resistance and inhibiting the development of AML [47].
Studies by Yu et al. showed that the levels of ALG9 (ALG9 alpha-1,2-mannosyltransferase) and lincRNA MEG3 (maternally expressed 3) are decreased in patients with chemoresistant AML. Peripheral blood mononuclear cells were collected from 33 patients with diagnosed drug-resistant AML and 33 with nondrug-resistant AML. Low ALG9 and MEG3 expression was correlated with poor prognosis in patients with AML, and dysregulation of ALG9 levels corresponded with the drug resistance phenotype in AML [48]. The ALG9 gene encodes a-1,2-mannosyltransferase, which is responsible for the glycosylation process. Glycosylation is one of the most important translational or post-translational modifications, and changes in glycosylation are associated with tumor progression [48, 49]. The molecular pathway of the regulation of MEG3 and ALG9 involves miR-155, which is overexpressed in patients with AML. Under normal conditions, MEG3 sequesters miR-155 and thus indirectly regulates ALG3 gene expression. In chemotherapy-resistant AML cells, this axis is abrogated, leading to a low level of ALG9 and consequently to induced proliferation and drug resistance in AML cells [48].
2.2 Thyroid Cancer
Thyroid cancer is the most common endocrine tumor derived from thyroid parenchymal cells, and its occurrence is the seventh highest among female malignancies in developed countries. It is ranked first among malignant tumors affecting female individuals worldwide. Because of early diagnosis, the incidence of TC is increasing globally [50, 51]. Two main subtypes of TC include: PTC (papillary thyroid carcinoma) and FTC (follicular thyroid carcinoma). Papillary thyroid carcinoma is responsible for 80% of all TCs [52] and develops as a result of alterations in BRAF, RAS, or RET/PTC oncogenes, which lead to abnormal cell proliferation [53]. The recurrence of PTC tumors within 10 years after starting therapy is 15% [54]. Similar to PTC, FTC is a well-differentiated cancer; however, it has a more aggressive phenotype. On the genetic level, FTC occurrence originates because of RAS single nucleotide alterations and the PAX8/PPARγ rearrangement. Moreover, mutations and gene copy variations of the PI3K/AKT signaling pathway were detected in FTC [53].
Increased PVT1 expression was detected in PTC tissues and cells in comparison to healthy tissues and cells. Analysis showed that PVT1 expression was related to the cancer TNM (classification of malignant tumors) stage, and increased PVT1 levels were detected in the advanced stages of PTC. Overexpression of PVT1 resulted in increased cell proliferation and migration and a reduced rate of apoptosis, consequently leading to the development of papillary thyroid carcinoma. Moreover, PVT1 promotes EMT in PTC cells. Further experiments revealed an interaction between miR-30a and PVT1. miR-30a inhibits cell proliferation and stimulates PTC cell apoptosis, partially by targeting IGF1R (insulin-like growth factor 1 receptor) gene. In PTC cells, miR-30a expression was decreased, whereas the expression of IGF1R was increased, which in turn induced malignancy, metastasis, and angiogenesis in cancer [54, 55]. Furthermore, upregulation of PVT1 was detected in serum derived from patients with TC. Experiments revealed that PVT1 acts as a molecular sponge of miR-423-5p in TC. Therefore, in TC tissues, the miR-423-5p expression level is decreased, and the expression of its target, PAK3 [p21 (RAC1) activated kinase 3], is increased, resulting in the proliferation and invasion of TC cells [56].
H19 expression is also increased in PTC tissues compared with healthy tissues and in vivo experiments showed that it resulted in larger tumors compared with negative control tumors. H19 stimulates TC development through inhibition of apoptosis and stimulation of cell migration and invasion. Furthermore, it was shown that H19 mediates the miR-17-5p effect on the regulation of YES1 (Yamaguchi sarcoma viral oncogene homolog 1) expression. YES1 affects cell proliferation, differentiation, and survival and has been recognized as a potential therapeutic target in many cancers [57].
Studies by Liu et al. showed that XIST is upregulated in TC tissues and stimulates cell proliferation and tumor growth through the miR-34a/MET axis. High XIST expression occurs in the advanced stage of TC and is associated with a greater tumor size. Low XIST expression is related to a longer survival rate. XIST acts as a molecular sponge for miR-34a, and therefore, the miR-34a level is reduced in TC tissues. The target of miR-34a is a receptor involved in the PI3K/AKT signaling pathway, MET (MET proto-oncogene, receptor tyrosine kinase). Upregulated MET stimulates the PI3K/AKT pathway and modulates cell proliferation in TC tumors [58].
NEAT1 is highly expressed in PTC cells and tissues, and its level was correlated with a high cell invasion rate and reduced apoptosis. Using bioinformatics tools and a luciferase assay, researchers identified the interaction of NEAT1 with miR-129-5p. By acting as a molecular sponge, NEAT1 reduces the level of miR-129-5p in PTC cells and tissues, which in turn results in higher expression of the targeted gene KLK7 (Kallikrein-related peptidase 7). Experiments have suggested that KLK7 promotes cell proliferation and migration [59].
LINC00460 expression is also increased in PTC cells and tissues compared with healthy tissues, and its level correlates with the clinical stage of the tumor, with the highest expression detected in the advanced TNM stage. Additionally, LINC00460 expression was coupled with tumor size and lymph node metastasis. In turn, knockdown of LINC00460 resulted in reduced cell proliferation, migration, and invasion. Researchers discovered that LINC00460 targets miR-485-5p, and consequently miR-485-5p expression in PTC tissues was decreased in comparison to normal tissues. This in turn results in increased expression of the target, Raf1 (Raf-1 p-oncogene, serine/threonine kinase), which is involved in tumor progression pathways [60].
Studies have shown that LINC00284 is also upregulated in PTC cells and tissues. LINC00284 stimulates cell proliferation by sponging miR-3127-5p, whose expression is therefore decreased in PTC cells. miR-3127-5p acts as a tumor suppressor in many cancers and targets the E2F7 (E2F transcription factor 7) gene encoding a transcription factor involved in cell-cycle progression. Moreover, studies have shown that E2F7 is linked to drug resistance and DNA damage repair in many cancers. Thus, LINC00284 induces cancer development indirectly increasing the expression of E2F7 [61].
The expression of LINC00475 is increased in PTC cell lines as well, influencing cell viability, proliferation, migration, and invasion. LINC00475 acts as a molecular sponge by binding miR-376c-3p. ZCCHC12 (zinc finger CCHC-type containing 12) mRNA is a downstream target of miR-376c-3p and its level is increased in PTC cell lines. ZCCHC12 was previously identified as an oncogene in PTC, as it promotes cell proliferation, migration, and invasion [62].
Another study revealed overexpression of HCP5 (HLA complex P5) in tissues of 43 FTC patients compared with normal tissues collected from the same cohort. HCP5 promotes cell proliferation, migration, and invasiveness and improves angiogenesis. HCP5 acts as a molecular sponge for miR-22-3p, miR-186-5p, and miR-216a-5p, leading to the activation of ST6GAL2 (ST6 beta-galactoside alpha-2,6-sialyltransferase 1), a sialyltransferase that controls the binding of sialic acids and their level on the cell surface. The ST6GAL group is involved in many biological processes in cells and has been implicated in human diseases, including cancer [63].
In contrast, LINC-PINT (lincRNA-P53 induced transcript) is downregulated in TC. Its low expression is related to an advanced TNM stage and the induction of TC cell invasion and xenograft tumor growth. Experiments showed that LINC-PINT inhibits TC progression by sponging miR-767-5p. In TC, miR-767-5p upregulation stimulates cell proliferation, colony formation, and tumor growth by inhibition of the expression of TET2 (Tet methylcytosine dioxygenase 2). Further experiments showed that overexpression of TET2 reversed the miR-767-5p effect on cell proliferation and invasion [64].
2.3 Glioblastoma Multiforme
Glioblastoma multiforme (GBM) is the most common malignant tumor of the central nervous system and originates from mutated astrocyte cells, which leads to tumor growth. Many glioblastomas develop without distinguishable precursor lesions and hence are termed primary glioblastomas. This type of glioblastoma affects elderly patients, and its fast progression shortens the patient’s lifespan. The secondary type of glioblastoma derives from diffuse or anaplastic astrocytoma. It occurs in young patients and is found in the frontal lobe. This type of glioblastoma has a better prognosis. It is impossible to distinguish between these two types by histological analysis; however, they differ genetically and epigenetically. In primary glioblastoma, EGFR (epidermal growth factor receptor) gene amplification and mutation in the PTEN (phosphatase and tensin homolog) gene occur. In secondary glioblastoma, mutation in TP53 (tumor protein P53) is present. Additionally, in primary glioblastoma, loss of whole chromosome 10 occurs, whereas in secondary glioblastoma, chromosome 19q is lost [65, 66].
An increased level of LINC01446 was detected in glioblastoma compared with healthy cells according to the public dataset GSE51146 and the analysis of 31 pairs of glioblastoma multiforme samples and neighboring normal tissues derived from patients. Furthermore, high LINC01446 expression was correlated with a poor patient survival rate. Both in vitro and in vivo experiments indicated that LINC01446 stimulated glioblastoma progression. LINC01446 acts as a sponge for miR-489-3p, leading to the upregulation of TPT1 (tumor protein translationally controlled 1), a stimulator of cell proliferation and invasion [67].
LincRNA H19 is also overexpressed in glioblastoma cell lines, as well as vascular endothelial growth factor (VEGF) and hypoxia-inducible transcription factor 1α (HIF-1α). Vascular endothelial growth factor is essential for angiogenesis, and HIF-1α is responsible for adaptation to variable oxygenation levels. In glioblastoma, a low oxygen concentration leads to the upregulation of HIF-1α, which results in an increase in VEGF expression. Thus, the HIF-1α/VEGF axis regulates angiogenesis, which is crucial in the development of tumors. Furthermore, HIF-1α is targeted by miR-138, which in turn is sponged by lincRNA H19. Therefore, angiogenesis in glioblastoma cells is induced by H19 overexpression due to the downregulation of miR-138 and hence the promotion of HIF-1α and VEGF expression [68].
LINC01494 is another lincRNA upregulated in glioblastoma tissues, and its level correlates with a low survival rate. LINC01494 acts as a molecular sponge for miR-122-5p, which targets the cell-cycle regulator CCNG1 (Cyclin G1). In tumor cells, upregulated LINC01494 indirectly activates CCNG1 expression, which in turn promotes cancer cell proliferation, migration, and invasion [69].
MALAT1 is upregulated in glioblastoma as well, according to the analysis of the GSE23806 dataset and glioblastoma stem cells derived from 14 patient tissue samples. Experiments showed that MALAT1 stimulates glioblastoma stem cell growth. MALAT1 acts as a molecular sponge and interacts with miR-129, which targets the transcription factor SOX2 responsible for maintaining cancer stem cell properties. Stimulation of tumor growth by MALAT1 acting through the miR-129/SOX2 axis was further confirmed in a xenograft mouse model [70]. Interestingly, research has shown that MALAT1 induces resistance of U87, GBM34, U251, and A172 glioblastoma cells to TMZ (temozolomide) chemotherapy. Therefore, MALAT1 can be a potential target for chemosensitization [71].
2.4 Nasopharyngeal Carcinoma
Nasopharyngeal carcinoma is a tumor that originates from epithelial cells in the nasopharynx. There are three subtypes identified according to the World Health Organization: squamous cell carcinoma, nonkeratinizing carcinoma, and undifferentiated carcinoma. The NPC tumor can extend out of the nasopharynx to the base of the skull, nasal cavity, or oropharynx. The development of NPC is induced by genetic susceptibility, environmental factors, and infection with Epstein–Barr virus. Unfortunately, even radiotherapy combined with chemotherapy is not able to extend patients’ lifespan [72,73,74].
XIST is upregulated in NPC according to the analysis of 108 tumor samples and has been shown to promote NPC cell growth. Bioinformatics analysis and miRNA profiling identified seven differentially expressed miRNAs between XIST-expressing NPC and control NPC cell lines [75]. For additional study, researchers selected miR-34a-5p, whose expression was the lowest, assuming its sponging by XIST. Further study of potential miR-34a-5p targets resulted in the identification of 100 genes, including the oncogene E2F3. Cells treated with miR-34a-5p and cells with E2F3 knockdown showed reduced cell growth compared with untreated cells. On the contrary, treatment with antisense oligonucleotide against miR-34a-5p and with XIST molecule increased cell growth. These results suggest that XIST promotes cell growth and cancer development by acting as a sponge for miR-34a-5p, thus indirectly stimulating the expression of the E2F3 gene [75].
Upregulation of H19 was also detected in NPC cells and tissues, as well as in CNE2 and HONE1 cell lines, where it corresponded with increased expression of EZH2. Further analysis identified the H19/miR-630/EZH2 axis, by which lincRNA regulates both factors. EZH2 is responsible for the negative regulation of E-cadherin, which is a crucial molecule coupled with EMT. In NPC cells, the level of E-cadherin is decreased, which corresponds with increased cell invasion in nasopharyngeal carcinoma [76].
NEAT1 expression is also upregulated in NPC, and its high expression is associated with a shorter patient lifespan and EMT phenotype, according to the analysis of 131 NPC samples. Researchers have identified the NEAT1/miR204/ZEB1 axis, by which NEAT1 upregulates the EMT inducer ZEB1 and thus in turn induces EMT, which is a crucial process in cancer metastasis. As EMT contributes to the radioresistance of NPC as well, NEAT1 can be a potential target for novel treatments [77].
In addition, an elevated level of MALAT1 was found in NPC tissues derived from 131 patients. However, its high expression is not associated with age, sex, smoking, or T classification but with a short survival time and lymph node metastasis. MALAT1 stimulates cell proliferation, invasion, and migration and is also involved in NPC cell radioresistance by modulating cancer stem cell (CSC) activity. This role of MALAT is mediated via miR-1, which binds both to MALAT1 and to the transcription factor SLUG (Snail family transcriptional repressor 2), which is involved in CSC activity and radioresistance. MALAT1 acts as a molecular sponge of miR-1, which consequently leads to upregulation of SLUG and radioresistance in NPC tissues [78].
2.5 Colorectal Cancer
Colorectal cancer is one of the most abundant types of cancer worldwide [79]. It is responsible for 10% of annual deaths caused by cancers globally [80]. Studies have shown that sex and age are linked to the occurrence of the disease, with men and people of advanced age more predisposed to being affected by CRC [79]. Risk factors include environmental and hereditary factors (in 10–20% of patients); moreover, bacterial infections caused by Fusobacterium nucleatum and Bacteroides fragilis can also increase the probability of cancer development [81]. In terms of hereditary factors, genome-wide association studies have allowed to detect cancer susceptibility genes that are related to CRC. The development of cancer begins with the formation of polyps, eventually, over 10–15 years later, polyps can evolve into colorectal cancer. All the changes originate from stem-like cells, which are formed due to genetic alterations leading to the activation of oncogenes and the deactivation of tumor-suppressor genes [79].
LincRNA BCAR4 (breast cancer anti-estrogen resistance 4) higher expression was observed in CRC tissues and connected with the initiation, recurrence, and metastasis of cancer. In this study, CSCs were sorted into ALDH+ (aldehyde dehydrogenase 1 family member A1) cells and ALDH− cells, and enhanced BCAR4 expression was detected in ALDH+ cells. BCAR4 overexpression caused a stronger self-renewal ability of CRC cells and increased the expression of the NANOG (homeobox transcription factor Nanog), OCT4 (octamer-binding transcription factor 4), SOX2 (SRY-box transcription factor 2), CD44 (CD44 molecule [Indian Blood Group]), CD133 (prominin 1), and Lgr5 (leucine rich repeat containing G protein-coupled receptor 5) genes, which are markers of stem cell properties. Thus, BCAR4 positively regulates CSC stemness. Moreover, scientists have shown that BCAR4 negatively regulates miR-665, which targets STAT3 (signal transducer and activator of transcription 3), a transcription factor involved in stemness and responsible for CSC self-renewal [82].
In turn, MEG3 is downregulated in CRC tissues and cell lines. In healthy cells, it acts as a CRC tumor suppressor, inhibiting cell proliferation and migration. MEG3 binds miR-376; therefore, the miR-376 level increases in CRC tissues and cells. MiR-376 targets the PRKD1 (protein kinase D1) gene, which is involved in cell migration and differentiation; however, it is downregulated in CRC cells [83].
2.6 Cutaneous Squamous Cell Carcinoma
Cutaneous squamous cell carcinoma accounts for 20% of deaths annually in the group of skin cancers. Currently, CSCC is the second most common skin cancer. External factors influencing the occurrence of CSCC are ultraviolet radiation, chronic ulceration, and immunosuppression [84, 85]. The most common places for CSCC are the mouth, ears, face, and top of the hands, i.e., the most frequently exposed to sunlight parts of the body. Cutaneous squamous cell carcinoma usually takes the form of a hard lump with a scaly tip but may also appear in the form of ulcers [85].
Researchers detected increased expression of small Cajal body-specific RNA 2 (SCARNA2) lincRNA in CSCC cells compared with neighboring healthy cells. Experiments were performed on a pool of CSCC and nontumor specimens taken from 30 patients with CSCC, as well as on cell lines. Samples were taken before any treatment was initiated. Further research revealed that ectopic expression of SCARNA2 leads to uncontrolled cell growth and promotes cell-cycle progression. SCARNA2 was found to act as a molecular sponge of miR-342-3p. miR-342-3p suppresses the transcription factor E2F1, which is involved in the cell cycle and regulates the expression of tumor-suppressing proteins [86]. In disease states, overexpression of SCARNA2 leads to inhibition of miR-342-3p expression, which further results in excessive cell growth and promotion of the cell cycle [86].
PICSAR (P38 inhibited cutaneous squamous cell carcinoma associated lincRNA) is also overexpressed in CSCC cells compared with normal keratinocytes and stimulates cell proliferation and migration. PICSAR expression is correlated with tumor size and degree of differentiation [87]. PICSAR interacts with miR-125b, which acts as a tumor suppressor. YAP1 (Yes-associated protein) is a direct target of miR-125b and acts as a potent oncogene in various cancers [87]. Additionally, YAP1 is a key nuclear effector of the Hippo pathway and plays an important role in various cellular processes, such as growth, differentiation, apoptosis, and EMT. PICSAR sponges miR-125b, thus upregulating YAP1 expression and influencing the development of CSCC [87].
2.7 Esophageal Squamous Cell Carcinoma
Esophageal squamous cell carcinoma is a disease with the highest incidence after the age of 40 years and is the most common esophageal cancer in the world. Esophageal squamous cell carcinoma is generally associated with a poor prognosis, and its survival rate has been estimated at 15–20%. The most common occurrence of ESCC can be found in the middle or abdominal segment of the esophagus. The cause of ESCC may be repeated inflammation and damage to the esophageal mucosa [88, 89]. At first, the progression of ESCC starts with squamous cell dysplasia of the esophagus, then develops into cancer and eventually becomes invasive [89]. The development of ESCC leads to ulcerative and necrotic lesions. The spread of the neoplasm in the esophagus occurs through the lamina propria, and metastases to other tissues occur in approximately 30% of patients [88, 89].
LINC00152 has been found to have an oncogenic role in ESCC. By analyzing 23 tumor samples and their corresponding adjacent normal tissues from patients with ESCC, Zhou and Huang described the LINC00152/miR-107/Rab10 axis, which results in upregulation of Rab10 (Ras-related protein Rab-10) [90] in ESCC. Rab10 is a member of the RAS oncogene family that plays an important role in follicle migration and is associated with many types of cancer [91], affecting the proliferation, migration, and invasion of tumor cells [90]. Furthermore, Liu et al. analyzed a total of 66 ESCC tumor tissues and adjacent normal tissues obtained from patients undergoing esophagectomy. They demonstrated the stimulating effect of LINC00152 on the FYN (FYN proto-oncogene, SRC family tyrosine kinase) by sequestering miR-153-3p [92]. FYN encodes a protein that mediates the regulation of cell growth [93] and is a member of the SRC family of tyrosine kinases associated primarily with T-lymphocyte and neuronal signaling in cell development and normal physiology. Disruption of these pathways often results in the formation of various cancers [92, 93].
The expression of ESCC-related lncRNA 1 transcript (ESCCAL-1), also known as CASC9 (cancer susceptibility 9), is also increased in ESCC and correlates with poorer clinical and pathological features. ESCCAL-1 in ESCC mouse models showed an effect on cellular processes associated with malignancies, including proliferation, migration, invasion, and resistance to apoptosis. ESCCAL-1 acts as a molecular sponge for miR-590-3p, which in turn prevents miR-590-3p from inhibiting the expression of the APOBEC3G (apolipoprotein B mRNA editing enzyme catalytic subunit 3G). Thus, elevated APOBEC3G is also a biomarker of poorer clinicopathological traits in ESCC. APOBEC3G plays an important role in tumor development, and its high expression has been observed in various types of cancer. APOBEC3G inhibits apoptosis by inactivating PTEN and activating the PI3K/Akt pathway, which promotes metabolism, proliferation, cell survival, growth, and angiogenesis in response to extracellular signals by mediating serine and/or threonine phosphorylation [94].
Similarly, the level of LINC00634 in neoplastic tissues was higher than that in nonneoplastic tissues (41 tissue samples in total) and was associated with the TNM stage in patients with ESCC. Because of its elevated expression, LINC00634 affects the regulation of cell proliferation and apoptosis. The authors described the LINC00634/miR-342-3p/Bcl2L1 axis, by which lincRNA upregulates the level of Bcl2L1. Bcl2L1 belongs to the antiapoptotic protein family, Bcl-2, and its high expression is associated with paclitaxel resistance in solid tumors [95].
Another lincRNA upregulated in ESCC is FAM225A (family with sequence similarity 225 member A), as shown by the study of ESCC tissue pairs and para-cancerous tissues acquired from 30 patients. Zhang et al. demonstrated that a higher level of FAM225A in ESCC cells promoted their growth, migration, and invasion and inhibited apoptosis. Furthermore, scientists revealed that FAM225A sequesters miR-206, which leads to upregulation of NETO2 (neuropilin and tolloid like 2) and FOXP1 (forkhead box P1) proteins. NETO2, by activating the PI3K/Akt/NF-κB/Snail axis, drives metastasis in GC. FOXP1 may also act as an oncogene; moreover, by acting as a transcription factor, it enhances the expression of FAM255A. The FAM225A/miR-206/NETO2 and FOXP1 pathways influence the acceleration of ESCC progression and angiogenesis [96].
LINC00662 showed increased expression in tissues with ESCC as well and it was suggested to influence cell proliferation, migration, and invasion in ESCC. A total of 72 surgical tumor samples and adjacent tissues were obtained for the study. LINC00662 acts as a molecular sponge for miR-340-5p, which targets HOXB2 (Homeo box B2), a sequence-specific transcription factor that is engaged in the pathogenesis of human cancer, including cervical and pancreatic cancers [97].
Another lincRNA that exhibits higher expression in ESCC tissues and cell lines is MIAT (myocardial infarction-associated transcript), as shown by The Cancer Genome Atlas data. MIAT influences the cell cycle, proliferation, migration, and invasion. MIAT binds to miR-1301-3p, which targets INCENP (internal centromere protein), an important protein regulating the cell cycle [98].
By analyzing tumor tissues and adjacent paired nontumor tissues collected from a total of 100 patients diagnosed with ESCC, Liang et al. demonstrated that LINC01980 expression is upregulated in ESCC tissues and is associated with a poor prognosis of the disease. LINC01980 was shown to promote proliferation, migration, invasion, and EMT progression in ESCC cells. LINC01980 can sequester miR-190a-5p, which in turn results in increased levels of its targets, the oncogenes MYO5A (Myosin-Va) and transforming growth factor beta-1, which are responsible for promoting an epithelial plasticity response leading to EMT progression [99].
The expression level of testis-specific transcript TTTY15 (testis-specific transcript, Y-linked 15) is significantly increased in ESCC tissues, as shown by a study of ESCC samples and adjacent normal tissues obtained from 40 male patients with ESCC. TTTY15 knockdown led to a reduction in ESCC proliferation, migration, and invasion. TTTY15 binds miR-337-3p and reduces its level in ESCC cells [100]. miR-337-3p inhibits the progression of ESCC by targeting Janus kinase 2, which is involved in many signaling pathways regulating apoptosis and proliferation [100, 101].
2.8 Gastric Cancer
Gastric cancer is one of the most common cancers and fourth in terms of mortality, with a median survival of less than 12 months. The prevalence of GC can be influenced by both genetic and environmental factors, including diet, alcohol consumption, smoking, Helicobacter pylori, and Epstein–Barr virus. Age and sex are important in terms of the incidence of GC; the median age at diagnosis is 70 years, and men are two to three times more susceptible than women [102]. According to the Lauren classification, GC is divided into two subtypes, intestinal and diffuse, which differ on many levels, including clinical features, genetics, and morphology. The intestinal subtype includes tubular and glandular elements of many degrees of differentiation. The diffusion subtype shows a weakly coherent single cell without gland formation [103].
One of the GC-related lincRNAs is LINC01234, which increased expression in GC tissues resulted in a larger tumor size, lymph node metastasis, and shorter survival time. Higher expression of LINC01234 was shown according to The Cancer Genome Atlas and GEO databases, and then confirmed in 50 pairs of GC samples and surrounding healthy tissues. Researchers demonstrated that in GC, LINC01234 act as a molecular sponge of miR-204-5p, thereby derepressing its endogenous target CBFB (core binding factor beta). CBFB is a transcription factor that belongs to the PEBP2/CBF family, which regulates several genes specific for hematopoiesis and osteogenesis [104]
In turn, analysis of the GC microarray dataset showed a lower expression of LINC00619 in GC tissues than in normal tissues. Eighty-eight patients were included in the study, from whom neoplastic tissues and adjacent normal gastric mucosa tissues were collected. LINC00619 was associated with miR-224-5p, as well as with the OPCML (opioid-binding protein/cell adhesion molecule like) protein, which hinders tumor development by inhibiting intracellular RTK (receptor tyrosine kinase) activity. In GC tissues, both LINC00619 and OPCML have decreased expression, in contrast to miR-224-5p, resulting in the induction of cell proliferation, invasion, migration, and inhibition of apoptosis [105].
LINC00511 expression was increased in the tissues of 25 patients with GC compared with normal adjacent tissues. High expression of LINC00511 correlated with poor prognosis and advanced levels of GC development. LINC00511 overexpression was responsible for promoting proliferation, accelerating tumor growth, and arresting apoptosis as well as the migration and invasion of cancer cells. Experiments showed that LINC00511 acts as a sponge of miR-515-5p, suggesting the mechanism underlying its oncogenic functions. Furthermore, LINC00511 increases the activation of the MAPK signaling pathway, including genes that play a key role in tumor progression [106, 107].
LINC01857 is also overexpressed in GC tissues and correlated with higher rates of metastasis and promotion of GC cell invasion and migration [108]. Analyzing these mechanisms, researchers linked LINC01857 with miR-200b, which in endothelial cells promotes angiostatic effects by silencing the expression of the transcription factors ETS1 (E26 transformation-specific proto-oncogene 1) and GATA2 (GATA binding protein 2, as well as VEGF and VEGF receptor 2) [108, 109].
The MALAT1/miR-23b-3p/ATG12 axis has been suggested to lead to chemo-induced autophagy and chemoresistance in GC cells. Experiments revealed that MALAT1, which is overexpressed in GC cells, attenuates miR-23b-3p activity, resulting in upregulation of the autophagy regulator ATG12, whose overexpression has also been observed in other neoplasms [110].
3 Discussion and Conclusions
Differentially expressed genes have been recognized in many cancers. Likewise, many abnormally expressed lincRNAs have been observed in cancer cells and tissues. The majority of lincRNAs act as molecular sponges of miRNAs, which further regulate many genes involved directly or indirectly in oncogenesis (Table 2). It is worth noting that the same lincRNA may be abnormally expressed in different cancers, whereas it binds to the different miRNAs, for example, H19, LINC00152, MALAT1, MEG3, NEAT1, and XIST (Table 1). To identify the aforementioned interactions, it is crucial to verify the expression level of the inspected lincRNAs and miRNAs in the available databases or experimentally, followed by detection of miRNA binding sites in silico and in vitro. Additionally, the study of the miRNA targets enables us to verify whether a lincRNA-miRNA interplay is significant in cancerogenesis. However, there is still a need for more thorough research because of the controversy around competitive endogenous RNA (ceRNA). In cells, there are many transcripts that share the same miRNA binding sites, thus competing for the miRNAs. The abundance of ceRNA is crucial for the effective control of gene expression. When ceRNA contributes miRNA-binding sites similar to those already accessible in the cell, it leads to derepression of the miRNA-targeted genes. This is the nonhierarchical model proposed by Denzler et al. [111]. On the contrary, Bosson et al. suggested a model wherein miRNA binding is more effective to the low abundant ceRNA harboring high-affinity target sites. Therefore, there is a hierarchy of interaction, wherein highly abundant transcripts with low-affinity target sites are less prone to bind miRNA, when ceRNA is accessible [112].
The questions arise how or whether sponging of particular miRNA affects genes and further regulatory pathways, wherein the change of expression level of one of the miRNA targets contributes to a small part of the cellular expression profile. Moreover, one can obtain false-positive results when comparing only certain miRNA expression with its targeted gene in the presence or absence of putative ceRNA. This suggests it may be crucial to investigate more deeply the changes of the pool of many miRNAs instead of one particular miRNA, in the context of molecular sponging by lincRNA. Additionally, it may reveal the reason underlying cancer-specific miRNA sponging. It is worth noting, the results obtained in cell lines or cells and tissues derived from patients may differ because of the miRNA:RNA-induced silencing complex activity, which is less likely to repress genes in the adult tissues [113]. Moreover, in cellulo overexpression experiments may lead to false conclusions. The exogene is expressed at a higher level than in physiological conditions, therefore disturbing the abundance of the ceRNA network, which may cause the interaction to be impossible to occur at the normal cellular concentration.
Long noncoding RNAs are undoubtedly important regulators of cancer cell progression. This past decade has resulted in an extensive body of literature concerning lincRNAs and their roles in the pathogenesis of cancers. This article focuses on specific examples of cancer-related lincRNAs, with studies describing altered lincRNAs and showing, if possible, the consequences in disrupted cellular pathways and dysregulated proteins with important biological functions. With knowledge of the functions and the molecular pathways involved, we can further identify promising therapeutic targets and shed light on the treatment of these cancers. Additionally, because of differential expression in particular types of cancer, lincRNAs can serve as biomarkers for diagnosis and monitoring cancer progression.
References
Wilusz JE, Sunwoo H, Spector DL. Long noncoding RNAs: functional surprises from the RNA world. Genes Dev. 2009;23(13):1494–504.
Ma L, Bajic VB, Zhang Z. On the classification of long non-coding RNAs. RNA Biol. 2013;10(6):925–33.
Ruiz-Orera J, Messeguer X, Subirana JA, Alba MM. Long non-coding RNAs as a source of new peptides. eLife. 2014 Sep 16;3: 3523.
Dhanoa JK, Sethi RS, Verma R, Arora JS, Mukhopadhyay CS. Long non-coding RNA: its evolutionary relics and biological implications in mammals: a review. J Anim Sci Technol. 2018;25(60):25.
Ma L, Bajic VB, Zhang Z. On the classification of long non-coding RNAs. RNA Biol. 2013;10:925–33.
Ransohoff JD, Wei Y, Khavari PA. The functions and unique features of long intergenic non-coding RNA. Nat Rev Mol Cell Biol. 2018;19(3):143–57.
D’Lima NG, Ma J, Winkler L, Chu Q, Loh KH, Corpuz EO, et al. A human microprotein that interacts with the mRNA decapping complex. Nat Chem Biol. 2017;13(2):174–80.
Deniz E, Erman B. Long noncoding RNA (lincRNA), a new paradigm in gene expression control. Funct Integr Genomics. 2017;17(2–3):135–43.
Wang KC, Yang YW, Liu B, Sanyal A, Corces-Zimmerman R, Chen Y, et al. A long noncoding RNA maintains active chromatin to coordinate homeotic gene expression. Nature. 2011;472(7341):120–4.
Yoon JH, Abdelmohsen K, Srikantan S, Yang X, Martindale JL, De S, et al. LincRNA-p21 suppresses target mRNA translation. Mol Cell. 2012;47(4):648–55.
Zhao J, Sun BK, Erwin JA, Song JJ, Lee JT. Polycomb proteins targeted by a short repeat RNA to the mouse X chromosome. Science. 2008;322(5902):750–6.
Cai Y. A brief review on the mechanisms of miRNA regulation. Genom Proteom Bioinform. 2009;7(4):8.
Hindorff LA, Sethupathy P, Junkins HA, Ramos EM, Mehta JP, Collins FS, et al. Potential etiologic and functional implications of genome-wide association loci for human diseases and traits. Proc Natl Acad Sci. 2009;106(23):9362–7.
Yan H, Chai H, Zhao H. Detecting lncRNA: cancer associations by combining miRNAs, genes, and prognosis with matrix factorization. Front Genet. 2021;28(12): 639872.
Lee YW, Chen M, Chung IF, Chang TY. lncExplore: a database of pan-cancer analysis and systematic functional annotation for lncRNAs from RNA-sequencing Data base (Oxford), 2021 Aug 31;2021 https://doi.org/10.1093/database/baab053
Whiteley AE, Price TT, Cantelli G, Sipkins DA. Leukaemia: a model metastatic disease. Nat Rev Cancer. 2021;21(7):461–75.
Thomas D, Majeti R. Biology and relevance of human acute myeloid leukemia stem cells. Blood. 2017;129(12):1577–85.
Pelcovits A, Niroula R. Acute myeloid leukemia: a review. RI Med J. 2013;2020(103):38–40.
Brown G. Introduction and classification of leukemias. In: Leukemia stem cells. Springer; Mol Biol. 2021;2185:3-23.
Malard F, Mohty M. Acute lymphoblastic leukaemia. Lancet. 2020;395:17.
Feng S, Liu N, Chen X, Liu Y, An J. Long non-coding RNA NEAT1/miR-338-3p axis impedes the progression of acute myeloid leukemia via regulating CREBRF. Cancer Cell Int. 2020;20(1):1–11.
Zhao C, Wang S, Zhao Y, Du F, Wang W, Lv P, et al. Long noncoding RNA NEAT1 modulates cell proliferation and apoptosis by regulating miR-23a-3p/SMC1A in acute myeloid leukemia. J Cell Physiol. 2019;234(5):6161–72.
Duan MY, Li M, Tian H, Tang G, Yang YC, Peng NC. Down-regulation of lncRNA NEAT1 regulated by miR-194-5p/DNMT3A facilitates acute myeloid leukemia. Blood Cells Molecules Dis. 2020;82: 102417.
Pan XW, Gan SS, Ye JQ, Fan YH, Hong Υ, Chu CM, et al. SMC1A promotes growth and migration of prostate cancer in vitro and in vivo. Int J Oncol. 2016;49(5):1963–72.
Zhou P, Xiao N, Wang J, Wang Z, Zheng S, Shan S, et al. SMC1A recruits tumor-associated-fibroblasts (TAFs) and promotes colorectal cancer metastasis. Cancer Lett. 2017;385:39–45.
Luo YY, Wang ZH, Yu Q, Yuan LL, Peng HL, Xu YX. LncRNA-NEAT1 promotes proliferation of T-ALL cells via miR-146b-5p/NOTCH1 signaling pathway. Pathol Res Pract. 2020;216(11): 153212.
Liu H, Chiang MY, Pear WS. Critical roles of NOTCH1 in acute T-cell lymphoblastic leukemia. Int J Hematol. 2011;94(2):118–25.
Kumar R, Juillerat-Jeanneret L, Golshayan D. Notch antagonists: potential modulators of cancer and inflammatory diseases. J Med Chem. 2016;59(17):7719–37.
Pouyanrad S, Rahgozar S, Ghodousi ES. Dysregulation of miR-335-3p, targeted by NEAT1 and MALAT1 long non-coding RNAs, is associated with poor prognosis in childhood acute lymphoblastic leukemia. Gene. 2019;692:35–43.
Li J, Wang M, Chen X. Long non-coding RNA UCA1 modulates cell proliferation and apoptosis by regulating miR-296-3p/Myc axis in acute myeloid leukemia. Cell Cycle. 2020;19(12):1454–65.
Li JJ, Chen XF, Wang M, Zhang PP, Zhang F, Zhang JJ. Long non-coding RNA UCA1 promotes autophagy by targeting miR-96-5p in acute myeloid leukaemia. Clin Exp Pharmacol Physiol. 2020;47(5):877–85.
Gong C, Hu C, Gu F, Xia Q, Yao C, Zhang L, et al. Co-delivery of autophagy inhibitor ATG7 siRNA and docetaxel for breast cancer treatment. J Control Release. 2017;266:272–86.
Lu J, Wu X, Wang L, Li T, Sun L. Long noncoding RNA LINC00467 facilitates the progression of acute myeloid leukemia by targeting the miR-339/SKI pathway. Leuk Lymphoma. 2021;62(2):428–37.
Li H, Tian X, Wang P, Hu J, Qin R, Xu R, et al. LINC01128 resisted acute myeloid leukemia through regulating miR-4260/NR3C2. Cancer Biol Ther. 2020;21(7):615–22.
Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15(3):178–96.
Roche J. The epithelial-to-mesenchymal transition in cancer. Cancers. 2018;10(2):52.
Lambert AW, Pattabiraman DR, Weinberg RA. Emerging biological principles of metastasis. Cell. 2017;168(4):670–91.
Dong X, Xu X, Guan Y. LncRNA LINC00899 promotes progression of acute myeloid leukaemia by modulating miR-744-3p/YY1 signalling. Cell Biochem Function. 2020;38(7):955–64.
Sheng XF, Hong LL, Li H, Huang FY, Wen Q, Zhuang HF. Long non-coding RNA MALAT1 modulate cell migration, proliferation and apoptosis by sponging microRNA-146a to regulate CXCR4 expression in acute myeloid leukemia. Hematology. 2021;26(1):43–52.
Song Y, Guo N, Zheng J. LncRNA-MALAT1 regulates proliferation and apoptosis of acute lymphoblastic leukemia cells via miR-205-PTK7 pathway. Pathol Int. 2020;70(10):724–32.
Berger H, Wodarz A, Borchers A. PTK7 faces the Wnt in development and disease. Front Cell Dev Biol. 2017;5:31.
Zhang X, Tao W. Long noncoding RNA LINC00152 facilitates the leukemogenesis of acute myeloid leukemia by promoting CDK9 through miR-193a. DNA Cell Biol. 2019;38(3):236–42.
He S, Fang X, Xia X, Hou T, Zhang T. Targeting CDK9: a novel biomarker in the treatment of endometrial cancer. Oncol Rep. 2020;44(5):1929–38.
Mofidi M, Rahgozar S, Pouyanrad S. Increased level of long non coding RNA H19 is correlated with the downregulation of miR-326 and BCL-2 genes in pediatric acute lymphoblastic leukemia, a possible hallmark for leukemogenesis. Mol Biol Rep. 2021;48(2):1531–8.
Ghodousi ES, Rahgozar S. MicroRNA-326 and microRNA-200c: Two novel biomarkers for diagnosis and prognosis of pediatric acute lymphoblastic leukemia. J Cell Biochem. 2018;119(7):6024–32.
Barsyte-Lovejoy D, Lau SK, Boutros PC, Khosravi F, Jurisica I, Andrulis IL, et al. The c-Myc oncogene directly induces the H19 noncoding RNA by allele-specific binding to potentiate tumorigenesis. Cancer Res. 2006;66(10):5330–7.
Wang C, Li L, Li M, Wang W, Liu Y, Wang S. Silencing long non-coding RNA XIST suppresses drug resistance in acute myeloid leukemia through down-regulation of MYC by elevating microRNA-29a expression. Mol Med. 2020;26(1):1–11.
Yu Y, Kou D, Liu B, Huang Y, Li S, Qi Y, et al. LncRNA MEG3 contributes to drug resistance in acute myeloid leukemia by positively regulating ALG9 through sponging miR-155. Int J Lab Hematol. 2020;42(4):464–72.
Davis K, Webster D, Smith C, Jackson S, Sinasac D, Seargeant L, et al. ALG9-CDG: new clinical case and review of the literature. Mol Genet Metabol Rep. 2017;13:55–63.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86.
Peng X, Zhang K, Ma L, Xu J, Chang W. The role of long non-coding RNAs in thyroid cancer. Front Oncol. 2020;11(10):941.
Zhou Q, Chen J, Feng J, Wang J. Long noncoding RNA PVT1 modulates thyroid cancer cell proliferation by recruiting EZH2 and regulating thyroid-stimulating hormone receptor (TSHR). Tumor Biol. 2016;37(3):3105–13.
Laha D, Nilubol N, Boufraqech M. New therapies for advanced thyroid cancer. Front Endocrinol. 2020;11:82.
Feng K, Liu Y, Xu LJ, Zhao LF, Jia CW, Xu MY. Long noncoding RNA PVT1 enhances the viability and invasion of papillary thyroid carcinoma cells by functioning as ceRNA of microRNA-30a through mediating expression of insulin like growth factor 1 receptor. Biomed Pharmacother. 2018;104:686–98.
Yuan J, Yin Z, Tao K, Wang G, Gao J. Function of insulin-like growth factor 1 receptor in cancer resistance to chemotherapy. Oncol Lett. 2018;15(1):41–7.
Lin QY, Qi QL, Hou S, Chen Z, Zhang L, Zhao HG, et al. LncRNA PVT1 acts as a tumor promoter in thyroid cancer and promotes tumor progression by mediating miR-423-5p-PAK3. Cancer Manag Res. 2020;12:13403.
Liu L, Yang J, Zhu X, Li D, Lv Z, Zhang X. Long noncoding RNA H19 competitively binds miR-17-5p to regulate YES1 expression in thyroid cancer. FEBS J. 2016;283(12):2326–39.
Liu H, Deng H, Zhao Y, Li C, Liang Y. LncRNA XIST/miR-34a axis modulates the cell proliferation and tumor growth of thyroid cancer through MET-PI3K-AKT signaling. J Exp Clin Cancer Res. 2018;37(1):279.
Zhang H, Cai Y, Zheng L, Zhang Z, Lin X, Jiang N. Long noncoding RNA NEAT1 regulate papillary thyroid cancer progression by modulating miR-129-5p/ KLK7 expression. J Cell Physiol. 2018;233(10):6638–48.
Li G, Kong Q. LncRNA LINC00460 promotes the papillary thyroid cancer progression by regulating the LINC00460/miR-485-5p/Raf1 axis. Biol Res. 2019;52(1):61.
Zhou B, Ge Y, Shao Q, Yang L, Chen X, Jiang G. Long noncoding RNA LINC00284 facilitates cell proliferation in papillary thyroid cancer via impairing miR-3127-5p targeted E2F7 suppression. Cell Death Discov. 2021;7(1):156.
Yang Y, Hua W, Zeng M, Yu L, Zhang B, Wen L. A ceRNA network mediated by LINC00475 in papillary thyroid carcinoma. Open Med. 2021;17(1):22–33.
Liang L, Xu J, Wang M, Xu G, Zhang N, Wang G, et al. LncRNA HCP5 promotes follicular thyroid carcinoma progression via miRNAs sponge. Cell Death Dis. 2018;9(3):372.
Jia M, Li Z, Pan M, Tao M, Wang J, Lu X. LINC-PINT suppresses the aggressiveness of thyroid cancer by downregulating miR-767-5p to induce TET2 expression. Mol Ther Nucleic Acids. 2020;22:319–28.
Ohgaki H, Kleihues P. Genetic pathways to primary and secondary glioblastoma. Am J Pathol. 2007;170(5):1445–53.
Ohgaki H, Kleihues P. The definition of primary and secondary glioblastoma. Clin Cancer Res. 2013;19(4):764–72.
Zhang L, Wang Q, Wang F, Zhang X, Zhang L, Tang Y, et al. LncRNA LINC01446 promotes glioblastoma progression by modulating miR-489-3p/TPT1 axis. Biochem Biophys Res Commun. 2018;503(3):1484–90.
Liu ZZ, Tian YF, Wu H, Ouyang SY, Kuang WL. LncRNA H19 promotes glioma angiogenesis through miR-138/HIF-1α/VEGF axis. Neoplasma. 2020;67(01):111–8.
Li C, Hu G, Wei B, Wang L, Liu N. lncRNA LINC01494 promotes proliferation, migration and invasion in glioma through miR-122-5p/CCNG1 axis. OTT. 2019;12:7655–62. https://doi.org/10.2147/OTT.S213345
Xiong Z, Wang L, Wang Q, Yuan Y. LncRNA MALAT1/miR-129 axis promotes glioma tumorigenesis by targeting SOX2. J Cell Mol Med. 2018;22(8):3929–40.
Voce DJ, Bernal GM, Wu L, Crawley CD, Zhang W, Mansour NM, et al. Temozolomide treatment induces lncRNA MALAT1 in an NF-κB and p53 codependent manner in glioblastoma. Cancer Res. 2019;79(10):2536–48.
Brennan B. Nasopharyngeal carcinoma. Orphanet J Rare Dis. 2006;1(1):23.
Chan ATC (2010) Nasopharyngeal carcinoma. Ann Oncol 21: 308–12.
He R, Hu Z, Wang Q, Luo W, Li J, Duan L, et al. The role of long non-coding RNAs in nasopharyngeal carcinoma: a systemic review. Oncotarget. 2017;8(9):16075–83.
Song P, Ye LF, Zhang C, Peng T, Zhou XH. Long non-coding RNA XIST exerts oncogenic functions in human nasopharyngeal carcinoma by targeting miR-34a-5p. Gene. 2016;592(1):8–14.
Li X, Lin Y, Yang X, Wu X, He X. Long noncoding RNA H19 regulates EZH2 expression by interacting with miR-630 and promotes cell invasion in nasopharyngeal carcinoma. Biochem Biophys Res Commun. 2016;473(4):913–9.
Lu Y, Li T, Wei G, Liu L, Chen Q, Xu L, et al. The long non-coding RNA NEAT1 regulates epithelial to mesenchymal transition and radioresistance in through miR-204/ZEB1 axis in nasopharyngeal carcinoma. Tumor Biol. 2016;37(9):11733–41.
Jin C, Yan B, Lu Q, Lin Y, Ma L. The role of MALAT1/miR-1/slug axis on radioresistance in nasopharyngeal carcinoma. Tumor Biol. 2016;37(3):4025–33.
Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394(10207):1467–80.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Shang FM, Liu HL. Fusobacterium nucleatum and colorectal cancer: a review. WJGO. 2018;10(3):71–81.
Ouyang S, Zhou X, Chen Z, Wang M, Zheng X, Xie M. LncRNA BCAR4, targeting to miR-665/STAT3 signaling, maintains cancer stem cells stemness and promotes tumorigenicity in colorectal cancer. Cancer Cell Int. 2019;19(1):72.
Wu X, Li J, Ren Y, Zuo Z, Ni S, Cai J. MEG3 can affect the proliferation and migration of colorectal cancer cells through regulating miR-376/PRKD1 axis. Am J Transl Res. 2019;11(9):5740–51.
Waldman A, Schmults C. Cutaneous squamous cell carcinoma. Hematol Oncol Clin North Am. 2019;33(1):1–12.
Corchado-Cobos R, García-Sancha N, González-Sarmiento R, Pérez-Losada J, Cañueto J. Cutaneous squamous cell carcinoma: from biology to therapy. Int J Mol Sci. 2020;21(8):2956.
Zhang Z, Jia M, Wen C, He A, Ma Z. Long non-coding RNA SCARNA2 induces cutaneous squamous cell carcinoma progression via modulating miR-342-3p expression. J Gene Med. 2020;22(12): e3242.
Lu X, Gan Q, Gan C, Zheng Y, Cai B, Li X, et al. Long non-coding RNA PICSAR knockdown inhibits the progression of cutaneous squamous cell carcinoma by regulating miR-125b/YAP1 axis. Life Sci. 2021;274: 118303.
Lam AK. Histopathological assessment for esophageal squamous cell carcinoma. In: Esophageal squamous cell carcinoma. Springer; Mol Biol. 2020;2129:7-18.
Reichenbach ZW, Murray MG, Saxena R, Farkas D, Karassik EG, Klochkova A, et al. Clinical and translational advances in esophageal squamous cell carcinoma. Adv Cancer Res. 2019;144:95–135.
Zhou Z, Huang F. Long non-coding RNA LINC00152 regulates cell proliferation, migration and invasion in esophageal squamous cell carcinoma via miR-107/Rab10 axis. OncoTargets Ther. 2019;12:8553.
Chua CEL, Tang BL. Rab 10: a traffic controller in multiple cellular pathways and locations. J Cell Physiol. 2018;233(9):6483–94.
Liu D, Gao M, Wu K, Zhu D, Yang Y, Zhao S. LINC00152 facilitates tumorigenesis in esophageal squamous cell carcinoma via miR-153-3p/FYN axis. Biomed Pharmacother. 2019;112: 108654.
Saito YD, Jensen AR, Salgia R, Posadas EM. Fyn: a novel molecular target in cancer. Cancer. 2010;116(7):1629–37.
Liu J, Mayekar MK, Wu W, Yan M, Guan H, Wang J, et al. Long non-coding RNA ESCCAL-1 promotes esophageal squamous cell carcinoma by down regulating the negative regulator of APOBEC3G. Cancer Lett. 2020;493:217–27.
Zhang X, Feng Y, Gao Y, Hu J. Long noncoding RNA LINC00634 functions as an oncogene in esophageal squamous cell carcinoma through the miR-342-3p/Bcl2L1 axis. Technol Cancer Res Treat. 2020;19:1533033820928508.
Zhang C, Luo Y, Cao J, Wang X, Miao Z, Shao G. Exosomal lncRNA FAM225A accelerates esophageal squamous cell carcinoma progression and angiogenesis via sponging miR-206 to upregulate NETO2 and FOXP1 expression. Cancer Med. 2020;9(22):8600–11.
Zhang Z, Liang X, Ren L, Zhang S, Li S, Wan T, et al. LINC00662 promotes cell viability and metastasis in esophageal squamous cell carcinoma by sponging miR-340-5p and upregulating HOXB2. Thorac Cancer. 2020;11(8):2306–15.
Zhang C, Xie L, Fu Y, Yang J, Cui Y. lncRNA MIAT promotes esophageal squamous cell carcinoma progression by regulating miR-1301-3p/INCENP axis and interacting with SOX2. J Cell Physiol. 2020;235(11):7933–44.
Liang X, Wu Z, Shen S, Niu Y, Guo Y, Liang J, et al. LINC01980 facilitates esophageal squamous cell carcinoma progression via regulation of miR-190a-5p/MYO5A pathway. Arch Biochem Biophys. 2020;686: 108371.
Wang W, Yang J. Long noncoding RNA TTTY15 promotes growth and metastasis of esophageal squamous cell carcinoma by sponging microRNA-337-3p to upregulate the expression of JAK2. Anticancer Drugs. 2020;31(10):1038–45.
Xu Y, Lv SX. The effect of JAK2 knockout on inhibition of liver tumor growth by inducing apoptosis, autophagy and anti-proliferation via STATs and PI3K/AKT signaling pathways. Biomed Pharmacother. 2016;84:1202–12.
Machlowska J, Baj J, Sitarz M, Maciejewski R, Sitarz R. Gastric cancer: epidemiology, risk factors, classification, genomic characteristics and treatment strategies. Int J Mol Sci. 2020;21(11):4012.
Machlowska J, Maciejewski R, Sitarz R. The pattern of signatures in gastric cancer prognosis. Int J Mol Sci. 2018;19(6):1658.
Chen X, Chen Z, Yu S, Nie F, Yan S, Ma P, et al. Long noncoding RNA LINC01234 functions as a competing endogenous RNA to regulate CBFB expression by sponging miR-204-5p in gastric cancer. Clin Cancer Res. 2018;24(8):2002–14.
Fang X, Dong Y, Yang R, Wei L. LINC00619 restricts gastric cancer progression by preventing microRNA-224-5p-mediated inhibition of OPCML. Arch Biochem Biophys. 2020;689: 108390.
Wang D, Liu K, Chen E. LINC00511 promotes proliferation and invasion by sponging miR-515-5p in gastric cancer. Cell Mol Biol Lett. 2020;25(1):1–10.
Johnson GL, Lapadat R. Mitogen-activated protein kinase pathways mediated by ERK, JNK, and p38 protein kinases. Science. 2002;298(5600):1911–2.
Chen G, Sun W, Zheng K, Zhu W. LINC01857 promotes the development of gastric cancer by regulating microRNA-200b. Eur Rev Med Pharmacol Sci. 2020;24(7):3648–56.
Chan YC. MicroRNA regulation of angiogenesis. In: MicroRNA in regenerative medicine. Chandan K. Sen, Elsevier, Ohio, USA, Academic Press, 711-37.
YiRen H, YingCong Y, Sunwu Y, Keqin L, Xiaochun T, Senrui C, et al. Long noncoding RNA MALAT1 regulates autophagy associated chemoresistance via miR-23b-3p sequestration in gastric cancer. Mol Cancer. 2017;16(1):1–12.
Denzler R, McGeary SE, Title AC, Agarwal V, Bartel DP, Stoffel M. Impact of microRNA levels, target-site complementarity, and cooperativity on competing endogenous RNA-regulated gene expression. Mol Cell. 2016;64(3):565–79.
Bosson AD, Zamudio JR, Sharp PA. Endogenous miRNA and target concentrations determine susceptibility to potential ceRNA competition. Mol Cell. 2014;56(3):347–59.
La Rocca G, Olejniczak SH, González AJ, Briskin D, Vidigal JA, Spraggon L, et al. In vivo, Argonaute-bound microRNAs exist predominantly in a reservoir of low molecular weight complexes not associated with mRNA. Proc Natl Acad Sci USA. 2015;112(3):767–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Katarzyna Dorota Raczyńska received a grant (UMO-2018/30/E/NZ2/00295) from the Polish National Science Centre.
Conflict of interest/Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Code Availability
Not applicable.
Authors’ contributions
RP and GZ drafted the manuscript. GZ prepared the tables and RP prepared the figures. KDR edited and proofread the text.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pasieka, R., Zasoński, G. & Raczyńska, K.D. Role of Long Intergenic Noncoding RNAs in Cancers with an Overview of MicroRNA Binding. Mol Diagn Ther 27, 29–47 (2023). https://doi.org/10.1007/s40291-022-00619-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-022-00619-w