Abstract
Lutetium Lu 177 vipivotide tetraxetan (PLUVICTO™, formerly known as 177Lu-PSMA-617) is a radioligand therapeutic agent that is being developed by Advanced Accelerator Applications (a subsidiary of Novartis) for the treatment of prostate-specific membrane antigen (PSMA)-expressing metastatic prostate cancer. The active part of the radiopharmaceutical is lutetium-177, which is linked to a ligand that binds to prostate-specific membrane antigen (PSMA), a transmembrane enzyme overexpressed in primary and metastatic prostate cancers. Based on efficacy results from the phase 3 VISION trial, lutetium Lu 177 vipivotide tetraxetan was approved in the USA on 23 March 2022 for the treatment of adult patients with PSMA-positive metastatic castration-resistant prostate cancer (mCRPC) who have been treated with androgen receptor (AR) pathway inhibition and taxane-based chemotherapy. Regulatory review in the EU and other countries is underway. This article summarizes the milestones in the development of Lutetium Lu 177 vipivotide tetraxetan leading to this first approval as a therapeutic radioligand for mCRPC.
Similar content being viewed by others
Digital Features for this AdisInsight Report can be found at https://doi.org/10.6084/m9.figshare.19701922 |
A radioligand therapeutic agent (a radiopharmaceutical) being developed by Advanced Accelerator Applications (a subsidiary of Novartis) for the treatment of PSMA-positive metastatic prostate cancer |
Received its first approval on 23 March 2022 in the USA |
Approved for use in adult patients with PSMA-positive mCRPC who have been treated with AR pathway inhibition and taxane-based chemotherapy |
1 Introduction
Prostate cancer is one of the most frequently diagnosed cancers worldwide [1]. While 5-year relative survival is 100% in those with localized or regional prostate cancer, metastatic prostate cancer has a 5-year survival rate of ≈ 30% [2]. There are a number of treatment options available for patients with metastatic prostate cancer, including hormone therapy (gonadotropin-releasing hormone analogues and anti-androgens), immunotherapy and chemotherapy; however, treatment options for patients with metastatic castration-resistant prostate cancer (mCRPC) who progress on multiple lines of therapy are limited [3, 4]. Prostate-specific membrane antigen (PSMA) is a transmembrane enzyme highly expressed on prostate cancer cells [4, 5] as well as being overexpressed physiologically in various organs, including the salivary and lacrimal glands, the kidneys, and gastrointestinal tract [6]. Metastatic lesions in most patients with mCRPC are PSMA-positive [7], making PSMA a good therapeutic target for radioligand therapies [8].
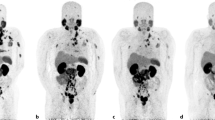
Lutetium Lu 177 vipivotide tetraxetan (formerly known as 177Lu-PSMA-617) is a radioligand therapeutic agent that has been developed for the treatment of PSMA-positive mCRPC [9], following early research conducted in Germany [10, 11]. The active part of the radiopharmaceutical is lutetium-177. Patients are selected for treatment with lutetium Lu 177 vipivotide tetraxetan based on PSMA expression in tumors using approved PSMA-11 imaging agents [9, 12]. On 23 March 2022, lutetium Lu 177 vipivotide tetraxetan received its first approval (in the USA [13]) for the treatment of adult patients with PSMA-positive mCRPC who have been treated with AR pathway inhibition and taxane-based chemotherapy. Lutetium Lu 177 vipivotide tetraxetan is also under regulatory review in the EU and other countries [14]. The recommended dosage of lutetium Lu 177 vipivotide tetraxetan is 7.4 GBq (200 mCi) intravenously every 6 weeks for up to 6 doses, or until disease progression, or unacceptable toxicity. Radiation exposure during and after treatment should be minimized in line with institutional good radiation safety practices and patient treatment procedures. Patients should increase oral fluid intake and void as often as possible to reduce bladder radiation. Dosage modifications may be required in the event of some adverse reactions, including myelosuppression and renal toxicity [9].
1.1 Company Agreements
In March 2020, ITM Isotopen announced it has expanded the long-term agreement for supply of no-carrier-added lutetium-177 to Endocyte (a Novartis subsidiary) and that it will continue to provide its 177Lu during the commercial phase, supporting the scalability and security of supply for patients world-wide [15]. In December 2018, Endocyte was acquired by Novartis [16]. In February 2018, Endocyte and ITM Isotopen Technologien München AG entered into a long-term global supply agreement under which ITM will supply Endocyte the highly purified, no-carrier-added lutetium radioisotope (177Lu), EndolucinBeta® to support commercial supply of lutetium Lu 177 vipivotide tetraxetan through to 2035 [17].
The prostate specific membrane antigen (PSMA-617) used in lutetium Lu 177 vipivotide tetraxetan was developed at DKFZ (German Cancer Research Center) and University Hospital Heidelberg and was exclusively licensed to Advanced Biochemical Compounds for early clinical development. In October 2017, Advanced Biochemical Compounds exclusively licensed worldwide rights PSMA-617 to Endocyte [18].
2 Scientific Summary
2.1 Pharmacodynamics
Lutetium Lu 177 vipivotide tetraxetan is a PSMA-binding ligand bound to a DOTA chelator (i.e., tetraxetan) radiolabeled with lutetium-177. Once lutetium Lu 177 vipivotide tetraxetan is bound to PSMA-expressing cells, the beta-minus emission from lutetium-177 delivers radiation to PSMA-expressing and surrounding cells, inducing DNA damage that leads to cell death [9]. The exposure-efficacy relationships of lutetium Lu 177 vipivotide tetraxetan and the time course of the pharmacodynamic response are not fully characterized [9]. Lutetium-177 decays to a stable hafnium-177 with a physical half-life of 6.647 days by emitting beta-minus radiation with a maximum energy of 0.498 MeV (79%) and photonic radiation (γ) of 0.208 MeV (11%) and 0.113 MeV (6.4%) [9]. Dosimetry of lutetium Lu 177 vipivotide tetraxetan was collected in a subgroup of 29 patients in the phase 3 VISION trial (NCT03511664) so that whole body and organ radiation dosimetry could be calculated. The highest radiation absorbed doses [mean calculated absorbed dose for 6 x 7.4 GBq (44.4 GBq cumulative activity)] were found in the following organs: lacrimal glands (92 Gy), salivary glands (28 Gy), large intestine [left colon (26 Gy), rectum (25 Gy), right colon (14 Gy)], kidneys (19 Gy) and urinary bladder wall (14 Gy). The 6-cycle cumulative estimated absorbed dose in the blood-based red marrow was 1.5 Gy [9, 19]. The maximum penetration of lutetium-177 in tissue is ≈ 2 mm (mean penetration is 0.67 mm) [9].

Key milestones in the development of lutetium Lu 177 vipivotide tetraxetan for the treatment of PSMA-positive mCRPC. EMA European Medicines Agency, MAA Marketing Authorization Application
Preliminary results from a retrospective tumour dosimetry analysis in a subgroup of patients (n = 6; 40 segmented metastatic lesions) with mCRPC treated with lutetium Lu 177 vipivotide tetraxetan in the phase 2 RESIST-PC trial (NCT03042312) found significant inter- and intra-patient tumour dose heterogeneity (possibly due to differences in PSMA expression in lesions). The mean absorbed dose in metastatic lesions was ≈ 3.48 ± 3.46 Gy/GBq [20].
Radiation dosimetry and the relationship to outcomes was examined in a subgroup of patients (n = 30) treated with lutetium Lu 177 vipivotide tetraxetan in the phase 2 LuPSMA trial (ACTRN12615000912583). The mean absorbed dose per unit of activity in various organs were consistent with those seen in the VISION trial. The median whole-body tumour-absorbed dose of 11.55 Gy correlated with PSA response at 12 weeks: the median dose was 14.1 Gy in patients achieving a ≥ 50% reduction in PSA, compared with 9.6 Gy in those who achieved a < 50% reduction (p < 0.01); only 1 of 11 patients receiving a dose of < 10 Gy achieved a > 50% reduction in PSA [21].
In patients with low-volume metastatic hormone-sensitive prostate cancer (mHSPC) treated with two cycles of lutetium Lu 177 vipivotide tetraxetan (n = 10) in a phase 1/2 trial (NCT03828838), lesion absorbed dose was considerably higher the organ absorbed dose in salivary glands, kidneys, liver and bone marrow [3.25 vs 0.39, 0.49, 0.09 and 0.017 Gy/GBq, respectively). Absorbed index lesion dose correlated significantly (p = 0.047) with treatment response [22].
Baseline haemoglobin level was an independent predictor of PSA reductions ≥ 50% at 4 weeks after completing treatment in a retrospective analysis of data from patients (n = 61) with mCRPC who had previously been treated with abiraterone or enzalutamide and docetaxel or cabazitaxel (i.e., AR pathway inhibition and taxane-based chemotherapy) and then received three cycles of lutetium Lu 177 vipivotide tetraxetan. In addition, baseline PSA ≤ 650 μg/L and baseline normal haemoglobin levels were associated with significantly (p < 0.05) longer median survival duration [23].
Significantly (p = 0.0002) more patients with mCRPC and plasma AR gene amplification (12/15) experienced early progressive disease (treatment interruption within 4 months of starting treatment with lutetium Lu 177 vipivotide tetraxetan) compared with patients with normal plasma AR (5/25) in a phase 2 study (NCT03454750). Median overall survival was significantly lower in the group with AR gene gain (7.4 vs 19.1 months; p = 0.02) [24].

Chemical structure of lutetium Lu 177 vipivotide tetraxetan
2.2 Pharmacokinetics
After intravenous administration of the recommended dosage, the mean maximum blood concentration of lutetium Lu 177 vipivotide tetraxetan is 6.58 ng/mL and the mean blood lutetium Lu 177 vipivotide tetraxetan area under the curve (AUC) is 52.3 ng · h/mL. Lutetium Lu 177 vipivotide tetraxetan has a mean volume of distribution of 123 L, and distributes to the gastrointestinal tract, liver, lungs, kidneys, heart wall, bone marrow, and salivary glands within 2.5 h of administration. Vipivotide tetraxetan and non-radioactive lutetium vipivotide tetraxetan are 60–70% bound to human plasma proteins [9].
Lutetium Lu 177 vipivotide tetraxetan is primarily excreted via the kidneys and exposure (AUC) increases with decreasing creatinine clearance (CLcr). No dose adjustment is recommended for patients with mild (baseline CLcr 60–89 mL/min) to moderate (CLcr 30-59 mL/min) kidney impairment; however, patients with mild or moderate kidney impairment may be at greater risk of kidney toxicity. The effects of more severe kidney impairment (baseline CLcr < 54 mL/min) or end-stage kidney disease on the pharmacokinetics of lutetium Lu 177 vipivotide tetraxetan has not been investigated [9]. A decline in kidney function that correlated with cumulative doses of lutetium Lu 177 vipivotide tetraxetan was seen in an analysis of data from 105 patients with mCRPC who were followed for 13 ± 9 months [25]. However, in a subgroup of patients with mCRPC and kidney impairment (glomerular filtration rate ≤ 60 mL/min) who were enrolled in a prospective patient registry (REALITY; NCT04833517), lutetium Lu 177 vipivotide tetraxetan treatment did not result in radioligand therapy-induced deterioration in kidney function [26]. The mean terminal elimination half-life of lutetium Lu 177 vipivotide tetraxetan is 41.6 h and mean clearance is 2.04 L/h [9].
Vipivotide tetraxetan is not a substrate of cytochrome P450 (CYP450) enzymes or of the transporters BCRP, P-gp, MATE1, MATE2-K, OAT1, OAT3 or OCT2. In in vitro studies, vipivotide tetraxetan did not induce CYP1A2, CYP2B6 or CYP3A4 and did not inhibit CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6 or CYP3A and BCRP, P-gp, MATE1, MATE2-K, OAT1, OAT3, OATP1B1, OATP1B3, OCT1 or OCT2 [9].
Features and properties of lutetium Lu 177 vipivotide tetraxetan
Alternative names | 177Lu-PSMA-617; 177-Lutetium-PSMA-617 - Endocyte; 177Lu-EB-PSMA-617; 177Lu-PSMA-617; 177LU-PSMA-617 - Endocyte; AAA617; Lu177 RLT; lutetium Lu 177 vipivotide tetraxetan - Advanced Accelerator Applications; Lutetium-177 PSMA 617; Pluvicto |
Class | Amides; Amines; Antineoplastics; Aza compounds; Carboxylic acids; Cyclic hydrocarbons; Cyclohexanes; Drug conjugates; Naphthalenes; Radiopharmaceuticals |
Mechanism of action | Ionizing radiation emitters |
Route of administration | Intravenous |
Pharmacodynamics | Once bound to PSMA-expressing cells, the beta-minus emission from lutetium-177 delivers radiation to PSMA-expressing cells and surrounding cells. Lutetium-177 decays to stable hafnium-177 with a physical half-life of 6.647 days |
Pharmacokinetics (mean values) | Blood Cmax 6.58 ng/mL, AUC 52.3 ng · h/mL, Vd 123 L, 60-70% bound to plasma proteins, t1/2 41.6 h, CL 2.04 L/h. |
Adverse events | |
Most frequent | Fatigue, dry mouth, nausea, anemia, decreased appetite, constipation ↓ lymphocytes, ↓ haemoglobin, ↓ leukocytes, ↓ platelets, ↓ calcium, ↓ sodium |
Clinically significant | Severe and life-threatening myelosuppression (including anaemia, thrombocytopenia, leukopenia, and neutropenia); severe renal toxicity |
ATC codes | |
WHO ATC code | V10 (Therapeutic Radiopharmaceuticals) |
EphMRA ATC code | V3C (Radiopharmaceuticals) |
Chemical name | O=C(O)CCC(C(O)=O)NC(NC(C(O)=O)CCCCNC(C(CC1=CC2=C(C=C1)C=CC=C2)NC(=O)C1CCC(CC1)CNC(=O)CN1CCN(CCN(CCN(CC1)CC([O-])=O)C[O-])CC([O-])=O)=O)=O.[Lu+3] |
2.3 Therapeutic Trials
2.3.1 Phase 3 VISION Trial
In the VISION trial (NCT03511664), treatment with lutetium Lu 177 vipivotide tetraxetan plus best standard of care (BSoC) significantly prolonged overall survival (OS) and radiographic progression-free survival (rPFS) [alternate primary endpoints] compared with BSoC alone in patients with progressive PSMA-positive mCRPC who had previously been treated with androgen receptor (AR) pathway inhibition and taxane-based chemotherapy [8]. Median OS was significantly longer with lutetium Lu 177 vipivotide tetraxetan plus BSoC (n = 551) than with BSoC alone (n = 280) [15.3 vs 11.3 months [HR 0.62 (95% CI 0.52–0.74); p < 0.001]. Median rPFS was 8.7 months in the lutetium Lu 177 vipivotide tetraxetan plus BSoC arm (n = 385) compared with 3.4 months in the BSoC alone arm (n = 196) [HR for progression or death 0.40 (99.2% CI 0.29–0.57); p < 0.001) [8]. The overall response rate was also significantly higher in lutetium Lu 177 vipivotide tetraxetan arm (n = 319 patients with evaluable disease at baseline) than in the BSoC alone arm (n = 120) [30% vs 2%; p < 0.001] [9]. Patients received up to 6 doses of lutetium Lu 177 vipivotide tetraxetan 7.4 GBq every 6 weeks plus BSoC or BSoC alone in this open-label, randomized trial. Treatment continued for up to 4–6 doses or until disease progression or unacceptable toxicity; those in the lutetium Lu 177 vipivotide tetraxetan arm with stable disease or partial response after 4 doses received up to 2 further doses at the investigator’s discretion. Median follow-up was 20.9 months [8].
2.3.2 Phase 2 Trials
Lutetium Lu 177 vipivotide tetraxetan was more effective than cabazitaxel in achieving a PSA response (PSA reduction of ≥ 50% from baseline; primary endpoint) in patients with mCRPC who had progressed after treatment with docetaxel in the TheraP trial (NCT03392428) [27]. 65 of 99 patients treated with lutetium Lu 177 vipivotide tetraxetan 6.0–8.5 GBq every 6 weeks for up to 6 cycles (n = 99) compared with 37 of 101 patients receiving cabazitaxel 20 mg/m2 every 3 weeks for up to 10 cycles achieved a PSA reduction of ≥ 50% from baseline [66% vs 37%; treatment difference 29% (95% CI 16–42); p < 0.0001 (ITT analysis)]. Lutetium Lu 177 vipivotide tetraxetan also delayed disease progression [HR 0.63 (95% CI 0.46–0.86;) p = 0.0028], radiographic progression [0.64 (95% CI 0.46–0.88); p = 0.0070] and PSA PFS [0.60 (95% CI 0.44–0.83); p = 0.0017] compared with cabazitaxel. Eligibility criteria in this open-label, randomized trial included PSMA-positive disease with no sites of metastatic disease with discordant FDG-positive and PSMA-negative findings; previous treatment with AR pathway inhibition was permitted. Cabazitaxel was considered the next appropriate treatment for these patients [27].
A PSA response (PSA reduction of ≥ 50% from baseline) was seen in 32 of 50 patients (64%) with progressive, PSMA-positive, symptomatic mCRPC who received up to 4 cycles of lutetium Lu 177 vipivotide tetraxetan every 6 weeks in the LuPSMA study (ACTRN12615000912583) [28, 29]. 22 of 50 patients (44%) had a ≥ 80% decrease in PSA. At a median follow-up of 31.4 months, median OS was 13.3 months in the overall population and 18.4 months in those achieving a PSA response. The mean injected activity delivered per cycle was 7.5 GBq (range 4–8.9 GBq) and the mean cumulative activity was 24.7 GBq. This trial consisted of an initial cohort of 30 patients [28] and a 20-patient extension cohort [28] Patients were excluded from this study if they had low PSMA expression or discordant sites of FDG–positive PSMA-negative disease [28, 29].
A significant treatment response (PSA reduction of ≥ 30% from baseline) was seen with lutetium Lu 177 vipivotide tetraxetan in 9 of 14 patients with progressive, symptomatic mCRPC in an Australian pilot study. A ≥ 50% reduction in PSA occurred in five patients and four of these experienced a > 70% reduction. Patients received up to 4 cycles of lutetium Lu 177 vipivotide tetraxetan 6.0–8 GBq every 6 weeks [30].
Treatment with lutetium Lu 177 vipivotide tetraxetan was associated with a median OS of 14 months in the RESIST-PC trial (NCT03042312) [31]. Eligible patients had progressive mCRPC after treatment with AR pathway inhibition, were either chemotherapy naïve or were post chemotherapy and had sufficient PSMA expression by PSMA PET and were randomized to receive up to 4 cycles of lutetium Lu 177 vipivotide tetraxetan 6.0 or 7.4 GBq. The trial was terminated early because of sponsorship transfer; data are from 43 patients the US arm of the trial [31].
Lutetium Lu 177 vipivotide tetraxetan was noninferior to docetaxel in chemotherapy-naïve patients with mCRPC in a trial conducted in India (CTRI/2019/12/022282) [32]. 60% of patients (9/15) in the lutetium Lu 177 vipivotide tetraxetan arm and 40% (8/20) in the docetaxel arm achieved a ≥ 50% decline in PSA from baseline [between-group difference 20%; 95% CI -12 to 47 (noninferiority margin of -15 in per protocol analysis achieved)]. Patients were administered lutetium Lu 177 vipivotide tetraxetan (6.0–7.4 GBq/cycle, every 8 weeks, up to 4 cycles) or docetaxel (75 mg/m2/cycle, every 3 weeks, up to 10 cycles) [32].
2.3.3 Other Trials
A > 50% reduction in PSA after administration of up to 6 cycles of lutetium Lu 177 vipivotide tetraxetan plus idronoxil (a synthetic flavonoid derivative with radiosensitising properties) was seen in 34 of 56 (61%) patients with progressive mCRPC previously treated with AR pathway inhibition and taxanes in the phase 1/2 LuPin trial (ACTRN12618001073291). The median PSA PFS was 7.5 months and median OS was 19.7 months. Patients received lutetium Lu 177 vipivotide tetraxetan 7.5 GBq on day 1 of each 6-week cycle, with escalating doses of NOX66 on days 1–10 of a 6-week cycle [33, 34].
A phase 1/2 study (NCT03042468) found that a single cycle of fractionated-dose of lutetium Lu 177 vipivotide tetraxetan [7.4–22 GBq on days 1 and 15 in the phase 1 dose-escalation cohort (n = 29); 22GBq on days 1 and 15 in the phase 2 cohort (n = 21); 27 patients treated at 22 GBq] was effective in patients with progressive mCRPC. A >50% PSA reduction was seen in 27 of 50 patients (54%); median PSA PFS was 5.6 months and median OS was 15.2 months [35].
The efficacy of lutetium Lu 177 vipivotide tetraxetan seen in preliminary results from patients with progressive mCRPC enrolled in the REALITY German registry (NCT04833517) was consistent with outcomes from clinical trials of lutetium Lu 177 vipivotide tetraxetan. A ≥ 50% reduction in PSA was seen in 52.0% of patients (132/254); at a median follow-up of 14.5 months, median PSA PFS was 5.5 months and median OS was 14.5 months. The median dose of lutetium Lu 177 vipivotide tetraxetan was 6.5 GBq/cycle (median cumulative dose 21.2 GBq), the median number cycles was 3, delivered at a median interval of 5.7 weeks [36].
A pilot study (NCT03828838) showed that treatment with lutetium Lu 177 vipivotide tetraxetan was effective in patients with PSMA-expressing, low volume (≥ 1 but ≤ 10 positive lesions on PSMA-PET) metastatic hormone-sensitive prostate cancer (mHSPC). After 2 cycles of lutetium Lu 177 vipivotide tetraxetan (a first cycle of 3 GBq, followed by a second cycle with 3–6 GBq after 7–9 weeks), 5 of 10 patients showed a > 50% PSA reduction and in one patient, PSA was undetectable [37].
Key clinical trials of lutetium Lu 177 vipivotide tetraxetan
Agent(s) | Indication | Phase | Status | Location(s) | Sponsor/collaborators | Identifier |
|---|---|---|---|---|---|---|
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 3 | Ongoing | Global | Endocyte | NCT03511664, VISION, EudraCT2018-000459-41 |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 3 | Recruiting | Global | Novartis, Alliance Foundation Trials, LLC, RTOG Foundation, Inc. | NCT04720157, PSMAddition EudraCT2020-003968-56, |
Lutetium Lu 177 vipivotide tetraxetan | mHSPC | 3 | Recruiting | Global | Novartis | NCT04689828, PSMAfore, EudraCT2020-003969-19 |
Lutetium Lu 177 vipivotide tetraxetan, Gallium (68Ga) gozetotide | mCRPC | 2 | Recruiting | Japan | Novartis, Eckert & Ziegler Radiopharma GmbH | NCT05114746 |
Lutetium Lu 177 vipivotide tetraxetan, enzalutamide | mCRPC | 2 | Recruiting | Australia | Australian and New Zealand Urogenital and Prostate Cancer Trials Group, National Health and Medical Research Council, Clinical Trials Centre, Prostate Cancer Research Alliance, Endocyte, Astellas | NCT04419402, ENZA-p |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 2 | Recruiting | Canada | Canadian Cancer Trials Group, Prostate Cancer Canada, Endocyte | NCT04663997 |
Lutetium Lu 177 vipivotide tetraxetan | mHSPC | 2 | Recruiting | Netherlands | Radboud University Medical Center, Prostaatkankerstichting, Advanced Accelerator Applications | NCT04443062, Bullseye |
Lutetium Lu 177 vipivotide tetraxetan | mHNPC | 2 | Recruiting | Australia | Peter MacCallum Cancer Centre, Movember Foundation, Prostate Cancer Research Alliance, US Department of Defense, Advanced Accelerator Applications, Australian and New Zealand Urogenital and Prostate Cancer Trials Group, ANSTO, ARTnet, BaCT | NCT04343885, UpFrontPSMA |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 2 | Recruiting | Italy | Istituto Scientifico Romagnolo per lo Studio e la cura dei Tumori | NCT03454750, EudraCT 2016-002732-32 |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 2 | Recruiting | Netherlands | Radboud University Medical Center | EudraCT2018-003088-79 |
Lutetium Lu 177 vipivotide tetraxetan, docetaxel | mCRPC | 2 | Ongoing | India | Postgraduate Institute of Medical Education and Research, Chandigarh | CTRI/2019/12/022282 |
Lutetium Lu 177 vipivotide tetraxetan, cabaxitaxel | mCRPC | 2 | Completed | Australia | Australian and New Zealand Urogenital and Prostate Cancer Trials Group, Endocyte, ANSTO, PCFAm ARTnet, Movember Foundation | NCT03392428, TheraP |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 2 | Completed | Australia | Peter MacCallum Cancer Centre, ANSTO, Endocyte | ACTRN12615000912583, LuPSMA |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 2 | Completed | Germany | Universitätsklinikum Freiburg | DRKS00013500, PCA-PSA-EPBR |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 2 | Discontinued | USA | Endocyte | NCT03042312, RESIST-PC |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 1/2 | Ongoing | USA | Weill Medical College of Cornell University | NCT03042468 |
Lutetium Lu 177 vipivotide tetraxetan, pembrolizumab | mCRPC | 1/2 | Ongoing | Australia | Peter MacCallum Cancer Centre | NCT03658447, PRINCE |
Lutetium Lu 177 vipivotide tetraxetan, idronoxil | mCRPC | 1/2 | Ongoing | Australia | Noxopharm | ACTRN12618001073291, LuPIN-1 |
Lutetium Lu 177 vipivotide tetraxetan | mCRPC | 1/2 | Recruiting | Australia | Peter MacCallum Cancer Centre, Endocyte, Movember Foundation, Medical Research Future Fund, E.J. Whitten Foundation Prostate Cancer Research Centre | NCT04430192, LuTectomy |
Lutetium Lu 177 vipivotide tetraxetan | mHSPC | 1/2 | Completed | Netherlands | Radboud University Medical Center | NCT03828838 |
Lutetium Lu 177 vipivotide tetraxetan, Gallium (68Ga) gozetotide | Renal cell carcinoma | 2 | Recruiting | China | Peking Union Medical College Hospital | NCT05170555 |
2.4 Adverse Events
The tolerability and safety of lutetium Lu 177 vipivotide tetraxetan was evaluated in the phase 3 VISION trial (NCT03511664) [n = 529 patients in the lutetium Lu 177 vipivotide tetraxetan plus BSoC and 205 in the BSoC alone arm] [8, 9]. The median duration of exposure to lutetium Lu 177 vipivotide tetraxetan was 7.8 months; patients received a median 5 doses (median cumulative dose of 37.5 GBq) [9]. The most common adverse reactions (all grades; occurring in ≥ 20% of patients receiving lutetium Lu 177 vipivotide tetraxetan plus BSoC and at a higher incidence than in the BSoC alone treatment arm) were fatigue (43% vs 23%), dry mouth (39% vs 0.5%), nausea (35% vs 17%), anaemia (32% vs 13%), decreased appetite (21% vs 15%) and constipation (20% vs 11%) [8, 9]. The most common laboratory abnormalities that worsened from baseline (all grades; occurring in ≥ 30% of patients receiving lutetium Lu 177 vipivotide tetraxetan plus BSoC and at a higher incidence than in the BSoC alone treatment arm) were decreased lymphocytes (85% vs 51%), decreased haemoglobin (63% vs 34%), decreased leukocytes (56% vs 22%), decreased platelets (45% vs 20%), decreased calcium (39% vs 28%) and decreased sodium (33% vs 23%) [9].
The most frequent grade 3–4 adverse events with lutetium Lu 177 vipivotide tetraxetan plus BSoC (incidence > 5%) in the VISION trial were anaemia (13% vs 4.9%), thrombocytopenia (8% vs 1%), fatigue (6% vs 1.5%), and the most frequent grade 3–4 laboratory abnormalities (incidence > 5%) were decreased lymphocytes (47% vs 18%), decreased haemoglobin (15% vs 7%), decreased platelets (9% vs 2.5%), decreased leukocytes (7% vs 2%) and decreased neutrophils (4.5% vs 0.5%). Other grade ≥ 3 adverse reactions of interest in patients treated with lutetium Lu 177 vipivotide tetraxetan plus BSoC included pancytopenia (1.1%), acute kidney injury (3%) and increased creatinine (0.9%). Other clinically relevant adverse reactions in lutetium Lu 177 vipivotide tetraxetan plus BSoC recipients included dry eye and vertigo (incidence < 5% for both) [9].
Treatment exposure was > 3 times longer in the lutetium Lu 177 vipivotide tetraxetan plus BSoC arm than in the BSoC alone arm in the VISION trial (7.6 vs 2.1 months) [8, 38]. An exposure-adjusted safety analysis found that the exposure-adjusted incidence of gastrointestinal events and fatigue with lutetium Lu 177 vipivotide tetraxetan plus BSoC was similar that that with BSoC alone; however, the exposure-adjusted incidence of musculoskeletal and renal events was higher in the BSoC alone arm, suggesting an association with treatment exposure rather than with lutetium Lu 177 vipivotide tetraxetan treatment. In contrast, the exposure-adjusted incidence of dry mouth, dry eye and acute myelosuppression remained higher in the lutetium Lu 177 vipivotide tetraxetan plus BSoC arm, confirming an association with lutetium Lu 177 vipivotide tetraxetan treatment [38].
Serious adverse reactions occurred in 36% of patients who received lutetium Lu 177 vipivotide tetraxetan plus BSoC in the VISION trial; these included hemorrhage (4%), musculoskeletal pain (3.8%), sepsis (3.2%), anemia (2.8%), urinary tract infection (2.6%), acute kidney injury (1.7%), pneumonia (1.7%), pancytopenia (1.3%), pyrexia (1.3%), spinal cord compression (1.1%). and pulmonary embolism (1.1%) [9].
Fatal adverse reactions occurred in 2.8% of patients who received lutetium Lu 177 vipivotide tetraxetan plus BSoC; these included sepsis (0.9%), pancytopenia (0.6%), hepatic failure (0.4%), intracranial hemorrhage (0.2%), subdural hematoma (0.2%), ischemic stroke (0.2%), COVID-19 infection (0.2%) and aspiration pneumonia (0.2%) [9]. Five fatal adverse events in the lutetium Lu 177 vipivotide tetraxetan plus BSoC arm were considered by the investigators to be drug-related [pancytopenia (2 patients), bone marrow failure, subdural hematoma and intracranial hemorrhage (in 1 patient each) [8].
Adverse reactions leading to a dose interruption of lutetium Lu 177 vipivotide tetraxetan occurred in 16% of patients, the most frequent (≥ 3%) of which were anemia (5%) and thrombocytopenia (3.6%). Adverse reactions leading to a dose reduction of lutetium Lu 177 vipivotide tetraxetan occurred in 6% of patients, the most frequent of which were thrombocytopenia (1.9%) and anemia (1.3%). Lutetium Lu 177 vipivotide tetraxetan was permanently discontinued due to adverse reactions in 12% of patients; anemia (2.8%), thrombocytopenia (2.8%), and leukopenia (including neutropenia) (1.7%) were the most frequent cause [8, 9].
2.5 Ongoing Clinical Trials
Numerous trials of lutetium Lu 177 vipivotide tetraxetan in patients with metastatic prostate cancer are currently active. The phase 3 VISION trial (NCT03511664) is ongoing and two other global phase 3 trials [PSMAfore (NCT04689828) and PSMAddition (NCT04720157)] are recruiting. PSMAfore compares lutetium Lu 177 vipivotide tetraxetan treatment with a change in AR pathway inhibitor in taxane-naïve patients with mCRPC [39], while PSMAddition compares lutetium Lu 177 vipivotide tetraxetan plus standard of care with standard of care alone in patients with mHSPC [40]. Several phase 2 and phase 1/2 studies [the Australian PRINCE (NCT03658447) and LuPIN-1 (ACTRN12618001073291) trials; a US trial (NCT03042468) and an Indian trial (CTRI/2019/12/022282)] are ongoing. Currently recruiting phase 2 and phase 1/2 trials include a Japanese trial (NCT05114746), a Canadian trial (NCT04663997), an Italian trial (NCT03454750), the Australian ENZA-p (NCT04419402), UpFrontPSMA (NCT04343885) and LuTectomy (NCT04430192) trials and two trials from the Netherlands [Bullseye (NCT04443062) and EudraCT2018-003088-79]. The German Registry Study (REALITY; NCT04833517) is also recruiting. A phase 2 trial of lutetium Lu 177 vipivotide tetraxetan in renal cell carcinoma (NCT05170555) is recruiting in China.
3 Current Status
Lutetium Lu 177 vipivotide tetraxetan received its first approval on 23 March 2022 for the treatment of adult patients with PSMA-positive mCRPC who have been treated with AR pathway inhibition and taxane-based chemotherapy in the USA [13].
References
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
SEER. Cancer stat facts: prostate cancer April 2021. 2021. https://seer.cancer.gov/statfacts/html/prost.html. Accessed 30 Mar 2022.
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): prostate cancer. Version 3.2022—January 10 2022. 2022. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed 30 Mar 2022.
Heidegger I, Kesch C, Kretschmer A, et al. Biomarkers to personalize treatment with 177Lu-PSMA-617 in men with metastatic castration-resistant prostate cancer - a state of the art review. Ther Adv Med Oncol. 2022. https://doi.org/10.1177/17588359221081922.
Bostwick DG, Pacelli A, Blute M, et al. Prostate specific membrane antigen expression in prostatic intraepithelial neoplasia and adenocarcinoma: a study of 184 cases. Cancer. 1998;82(11):2256–61.
Demirci E, Sahin OE, Ocak M, et al. Normal distribution pattern and physiological variants of 68Ga-PSMA-11 PET/CT imaging. Nucl Med Commun. 2016;37(11):1169–79.
Paschalis A, Sheehan B, Riisnaes R, et al. Prostate-specific membrane antigen heterogeneity and DNA repair defects in prostate cancer. Eur Urol. 2019;76(4):469–78.
Sartor O, de Bono J, Chi KN, et al. Lutetium-177-PSMA-617 for metastatic castration-resistant prostate cancer. N Engl J Med. 2021;385(12):1091–103.
Novartis AG. PLUVICTOTM (lutetium Lu 177 vipivotide tetraxetan) injection: US prescribing information. 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/215833s000lbl.pdf. Accessed 30 Mar 2022.
Rahbar K, Ahmadzadehfar H, Kratochwil C, et al. German multicenter study investigating 177Lu-PSMA-617 radioligand therapy in advanced prostate cancer patients. J Nucl Med. 2017;58(1):85–90.
Czernin J, Calais J. 177Lu-PSMA617 and the VISION trial: one of the greatest success stories in the history of nuclear medicine. J Nucl Med. 2021;62(8):1025–6.
Iravani A, Violet J, Azad A, et al. Lutetium-177 prostate-specific membrane antigen (PSMA) theranostics: practical nuances and intricacies. Prostate Cancer Prostatic Dis. 2020;23(1):38–52.
US Food & Drug Administration. FDA approves Pluvicto for metastatic castration-resistant prostate cancer [media release]. 23 Mar 2022. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-pluvicto-metastatic-castration-resistant-prostate-cancer.
Novartis. Novartis PluvictoTM approved by FDA as first targeted radioligand therapy for treatment of progressive, PSMA positive metastatic castration-resistant prostate cancer [media release]. 23 Mar 2022. http://www.novartis.com.
ITM Isotopen Technologien München AG. ITM expands PSMA-617 supply agreement for no-carrier-added lutetium-177 [media release]. 2 Mar 2020. http://www.isotope-technologies-munich.com.
Novartis. Novartis successfully completes acquisition of Endocyte [media release]. 21 Dec 2018. http://www.novartis.com.
Endocyte, ITM Isotopen Technologien München AG. Endocyte and ITM announce supply agreement for no-carrier-added lutetium for the phase 3 VISION trial [media release]. 26 Feb 2018. http://www.endocyte.com.
Endocyte. Endocyte announces exclusive worldwide license of phase 3 ready PSMA-targeted radioligand therapy for development in prostate cancer [media release]. 2 Oct 2017. http://www.endocyte.com.
Herrmann K, Rahbar K, Eiber M, et al. Dosimetry of 177Lu-PSMA-617 for the treatment of metastatic castration-resistant prostate cancer: results from the VISION trial sub-study [abstract no.97]. J Clin Oncol. 2022;40(6 Suppl).
Meyer C, Mirand D, Adams T, et al. Patient-specific tumor dosimetry in mCRPC patients treated with Lu-PSMA-617 [abstract no. 1572]. J Nucl Med. 2021;62(Suppl. 1).
Violet J, Jackson P, Ferdinandus J, et al. Dosimetry of (177)Lu-PSMA-617 in metastatic castration-resistant prostate cancer: correlations between pretherapeutic imaging and whole-body tumor dosimetry with treatment outcomes. J Nucl Med. 2019;60(4):517–23.
Peters SMB, Privé BM, de Bakker M, et al. Intra-therapeutic dosimetry of [(177)Lu]Lu-PSMA-617 in low-volume hormone-sensitive metastatic prostate cancer patients and correlation with treatment outcome. Eur J Nucl Med Mol Imaging. 2022;49(2):460–9.
Rasul S, Hartenbach M, Wollenweber T, et al. Prediction of response and survival after standardized treatment with 7400 MBq (177)Lu-PSMA-617 every 4 weeks in patients with metastatic castration-resistant prostate cancer. Eur J Nucl Med Mol Imaging. 2021;48(5):1650–7.
De Giorgi U, Sansovini M, Severi S, et al. Circulating androgen receptor gene amplification and resistance to 177Lu-PSMA-617 in metastatic castration-resistant prostate cancer: results of a phase 2 trial. Br J Cancer. 2021;125(9):1226–32.
Nguyen Ngoc C, Mader N, Davis K, et al. Risk and concomitant factors of renal insufficiency throughout radioligand treatment with 177Lu-PSMA-617 [abstract no. OP-985]. Eur J Nucl Med Mol Imaging. 2020;47:S490.
Rosar F, Kochems N, Bartholoma M, et al. Renal safety of [177lu]lu-psma-617 radioligand therapy in patients with compromised baseline kidney function. Cancers. 2021;13(3095):1–10.
Hofman MS, Emmett L, Sandhu S, et al. [177Lu]Lu-PSMA-617 versus cabazitaxel in patients with metastatic castration-resistant prostate cancer (TheraP): a randomised, open-label, phase 2 trial. Lancet. 2021;397(10276):797–804.
Violet J, Sandhu S, Iravani A, et al. Long-Term follow-up and outcomes of retreatment in an expanded 50-patient single-center phase II prospective trial of (177)Lu-PSMA-617 theranostics in metastatic castration-resistant prostate cancer. J Nucl Med. 2020;61(6):857–65.
Hofman MS, Violet J, Hicks RJ, et al. [177Lu]-PSMA-617 radionuclide treatment in patients with metastatic castration-resistant prostate cancer (LuPSMA trial): a single-centre, single-arm, phase 2 study. Lancet Oncol. 2018;19(6):825–33.
Emmett L, Crumbaker M, Ho B, et al. Results of a prospective phase 2 pilot trial of 177Lu-PSMA-617 therapy for metastatic castration-resistant prostate cancer including imaging predictors of treatment response and patterns of progression. Clin Genitourin Cancer. 2019;17(1):15–22.
Calais J, Gafita A, Eiber M, et al. Prospective phase 2 trial of PSMA-targeted molecular RadiothErapy with 177Lu-PSMA-617 for metastatic castration-reSISTant Prostate Cancer (RESIST-PC): efficacy results of the UCLA cohort. J Nucl Med. 2021;62(10):1440–6.
Satapathy S, Mittal BR, Sood A, et al. 177Lu-PSMA-617 versus docetaxel in chemotherapy-naive metastatic castration-resistant prostate cancer: a randomized, controlled, phase 2 non-inferiority trial. Eur J Nucl Med Mol Imaging. 2022;49(5):1754–64.
Crumbaker M, Pathmanandavel S, Yam AO, et al. Phase I/II Trial of the combination of 177Lutetium prostate specific membrane antigen 617 and idronoxil (NOX66) in men with Eed-stage metastatic castration-resistant prostate cancer (LuPIN). European Urology Oncology. 2021;4(6):963–70.
Pathmanandavel S, Crumbaker M, Yam AO, et al. (177)Lutetium PSMA-617 and idronoxil (NOX66) in men with end-stage metastatic castrate-resistant prostate cancer (LuPIN): patient outcomes and predictors of treatment response of a Phase I/II trial. J Nucl Med. 2021.
Tagawa ST, Sun M, Sartor O, et al. Final results of phase I/II trial of fractionated dose 177Lu-PSMA-617 for metastatic castration-resistant prostate cancer (mCRPC) [abstract no. 600P]. Ann Oncol. 2021;32:S645.
Khreish F, Ghazal Z, Marlowe RJ, et al. 177 Lu-PSMA-617 radioligand therapy of metastatic castration-resistant prostate cancer: Initial 254-patient results from a prospective registry (REALITY Study). Eur J Nucl Med Mol Imaging. 2022;49(3):1075–85.
Privé BM, Peters SMB, Muselaers CHJ, et al. Lutetium-177-PSMA-617 in low-volume hormone-sensitive metastatic prostate cancer: a prospective pilot study. Clin Cancer Res. 2021;27(13):3595–601.
Chi KN, Adra N, Garje R, et al. Exposure-adjusted safety analyses of the VISION phase 3 trial of 177Lu-PSMA-617 in patients with metastatic castration-resistant prostate cancer [abstract no. 85]. J Clin Oncol. 2022;40(6 Suppl.).
Sartor AO, Morris MJ, Chi KN, et al. PSMAfore: A phase 3 study to compare 177Lu-PSMA-617 treatment with a change in androgen receptor pathway inhibitor in taxane-naïve patients with metastatic castration-resistant prostate cancer [abstract no. TPS211]. J Clin Oncol. 2022;40(6 Suppl.).
Sartor AO, Tagawa ST, Saad F, et al. PSMAddition: a phase 3 trial to compare treatment with 177Lu-PSMA-617 plus standard of care (SOC) versus SOC alone in patients with metastatic hormone-sensitive prostate cancer [abstract no. TPS210]. J Clin Oncol. 2022;40(6 Suppl).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and Conflict of interest
During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the authors on the basis of scientific completeness and accuracy. Susan J. Keam is a contracted employee of Adis International Ltd/Springer Nature and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent to publish, Availability of data and material, Code availability
Not applicable.
Additional information
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Keam, S.J. Lutetium Lu 177 Vipivotide Tetraxetan: First Approval. Mol Diagn Ther 26, 467–475 (2022). https://doi.org/10.1007/s40291-022-00594-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-022-00594-2