Abstract
Background
Not all anterior cruciate ligament (ACL) injuries are preventable. While some ACL injuries are unavoidable such as those resulting from a tackle, others that occur in non-contact situations like twisting and turning in the absence of external contact might be more preventable. Because ACL injuries commonly occur in team ball-sports that involve jumping, landing and cutting manoeuvres, accurate information about the epidemiology of non-contact ACL injuries in these sports is needed to quantify their extent and burden to guide resource allocation for risk-reduction efforts.
Objective
To synthesize the evidence on the incidence and proportion of non-contact to total ACL injuries by sex, age, sport, participation level and exposure type in team ball-sports.
Methods
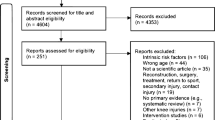
Six databases (MEDLINE, EMBASE, Web of Science, CINAHL, Scopus and SPORTDiscus) were searched from inception to July 2021. Cohort studies of team ball-sports reporting number of knee injuries as a function of exposure and injury mechanism were included.
Results
Forty-five studies covering 13 team ball-sports were included. The overall proportion of non-contact to total ACL injuries was 55% (95% CI 48–62, I2 = 82%; females: 63%, 95% CI 53–71, I2 = 84%; males: 50%, 95% CI 42–58, I2 = 86%). The overall incidence of non-contact ACL injuries was 0.07 per 1000 player-hours (95% CI 0.05–0.10, I2 = 77%), and 0.05 per 1000 player-exposures (95% CI 0.03–0.07, I2 = 97%). Injury incidence was higher in female athletes (0.14 per 1000 player-hours, 95% CI 0.10–0.19, I2 = 40%) than male athletes (0.05 per 1000 player-hours, 95% CI 0.03–0.07, I2 = 48%), and this difference was significant. Injury incidence during competition was higher (0.48 per 1000 player-hours, 95% CI 0.32–0.72, I2 = 77%; 0.32 per 1000 player-exposures, 95% CI 0.15–0.70, I2 = 96%) than during training (0.04 per 1000 player-hours, 95% CI 0.02–0.07, I2 = 63%; 0.02 per 1000 player-exposures, 95% CI 0.01–0.05, I2 = 86%) and these differences were significant. Heterogeneity across studies was generally high.
Conclusion
This study quantifies several key epidemiological findings for ACL injuries in team ball-sports. Non-contact ACL injuries represented over half of all ACL injuries sustained. The proportion of non-contact to total ACL injuries and injury incidence were higher in female than in male athletes. Injuries mostly occurred in competition settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The overall proportion of non-contact to total ACL injuries in team ball-sports was 55%. |
Injury incidence of non-contact ACL injuries in team ball-sports was higher in female athletes than in male athletes. |
Injury incidence of non-contact ACL injuries in team ball-sports during competition was higher than during training. |
1 Introduction
Anterior cruciate ligament (ACL) injuries commonly occur in team ball-sports [1,2,3] but we do not know how many of these injuries are preventable. ACL injuries that result from contact situations like a tackle are sometimes unavoidable [4] compared to those that occur in non-contact situations like twisting and turning in the absence of external contact [5]. Exercise-based injury risk reduction programs (IRRPs) are a prominent feature in ACL injury risk-reduction efforts [6] and these programs seem to have a stronger effect on reducing the risk of non-contact ACL injuries (odds ratio (OR) 0.39) compared with contact ones (OR 0.61) [5]. Syntheses of information about the epidemiology of non-contact ACL injuries are currently unavailable and this information is important for guiding ACL risk-reduction efforts [7, 8]. Prior epidemiological reviews on ACL injury incidence did not consider injury mechanism [1, 9], combined different exposure types (player-hours converted to player-exposures) [10, 11], did not utilize meta-regression analyses to investigate sources of heterogeneity and the association of categorical variables like sex and sport, and did not investigate the proportion of non-contact to total ACL injuries.
We need to better understand the extent of non-contact ACL injuries because they impose a wide-ranging personal, societal and economic burden [12,13,14]. ACL injuries are associated with, for example, a sevenfold increase in odds of end-stage osteoarthritis resulting in total knee arthroplasties [12], more than US$90,000 per injury to gain a quality-adjusted life-year [15], and psychological barriers that may affect recovery, return to sport and an increased risk of sustaining a subsequent injury [16]. Therefore, we undertook a comprehensive systematic review, meta-analysis and meta-regression to estimate the proportion of non-contact ACL to total ACL injuries, and describe the incidence of non-contact ACL injuries by unit of exposure, sex, age group, sport, participation level, and exposure type in team ball-sports.
2 Methods
This review is on ACL injuries only and it forms part of a larger systematic review on the epidemiology of non-contact knee injuries sustained in team ball-sports. Future publications will focus on other non-contact knee injuries like gradual-onset knee injuries. The review was prepared and conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement [17], and was prospectively registered with the PROSPERO International Prospective Register of Systematic Reviews (CRD42020179475). We were informed in an automated PROSPERO message that due to their focus on COVID-19-related systematic review registrations at the time of registration, this submission was automatically published and not checked for eligibility. Patients and public partners were not involved in the design, conduct or interpretation of this systematic review.
2.1 Search Strategy and Selection Criteria
Six electronic databases (MEDLINE, EMBASE, Web of Science, CINAHL, Scopus and SPORTDiscus) were systematically searched from inception to July 2021. Search terms consisted of controlled vocabulary and free text, and were mapped to medical subject where possible to capture records of knee injury (e.g., “anterior cruciate ligament rupture”, “patellofemoral pain”, “meniscus tears”) epidemiology (e.g., “prevalence”, “incidence”, “exposure”) in team ball-sports (e.g., “soccer”, “football”, “rugby”, “basketball”). The MEDLINE search strategy is provided in Appendix A1. All records were downloaded to EndNote X8 (Thomson Reuters, USA) where duplicates were removed, then uploaded to Covidence (Covidence systematic review software, Veritas Health Innovation, Melbourne, VIC, Australia; http://www.covidence.org). Bibliographic hand-searches were also performed to supplement the electronic database search.
Studies were included if: (i) the number of ACL injuries as a function of injury mechanism were reported; (ii) they were prospective cohort studies or retrospective cohort studies examining routinely collected data (e.g., league-wide injury surveillance databases and insurance databases); (iii) they featured athletes from field and court-based team ball-sports (Association Football or soccer, futsal, football or American Football, rugby union, rugby league, Gaelic football, Australian football, basketball, netball, handball, volleyball, field hockey, floorball, lacrosse, hurling, baseball, softball, and cricket) because ACL injury mechanisms on these surfaces were more comparable [4, 18, 19]; (iv) they reported exposure data in terms of athlete-hours, athlete-exposures, or per-event data. Examples of per-event exposure data are the number of tackles in rugby union or number of jumps in volleyball. If a study reported on knee injuries and injury mechanisms separately, but not knee injury as a function of mechanism, study authors were contacted via email to request more information. We excluded studies if more detailed data were not available or authors did not provide the information following two email contact attempts. Studies were also excluded if: (i) the data had been published in earlier papers, such as cases of secondary analysis of routinely collected data; in such situations, the paper that reported the most exposure data was included; (ii) they investigated non-organised or non-competitive sport, such as school-based recreation or physical education classes; (iii) the data recorded were not sport-specific (e.g., hospital emergency department admission records); (iv) they investigated post-surgical populations or re-injury outcomes; (v) they featured athletes competing on ice, sand, in water, or on horseback. Studies were not excluded based on their definition of non-contact injury mechanisms, or lack thereof. Two authors (LC and DS) independently applied selection criteria to screen studies by titles and abstracts, followed by full texts to identify eligible studies. Disagreements were settled through discussion and consensus, and a third author (EP) acted as a tie-breaker if needed.
2.2 Quality Assessment
Two authors (LC and MW) independently assessed study quality using a modified six-item Newcastle–Ottawa scale for cohort studies where one star was awarded for each item for a maximum of six stars [20]. A similar scale was previously used in a systematic review of acute hamstring injuries [21]. The six items were: (a) population description, (b) population recruitment, (c) surveillance methods, (d) duration of observation, (e) case definition, and (f) others (all other methods) (Appendix A2). Disagreement between assessors was settled through discussion and consensus, with a third author (EP) acting as a tie-breaker if needed. In accordance with previously published systematic reviews and meta-analyses of injury incidence [22, 23], the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system to assess certainty of evidence was not used because this review is not a clinical practice guideline and does not make clinical recommendations [24].
2.3 Data Extraction and Management
Publication information (authors, year), population characteristics (cohort size, age, participation level, sport, sex), exposure type (training, competition, composite), number of injuries, exposure, unit of exposure, surveillance information (definition of injury, how injuries were recorded, duration of surveillance), and severity of injuries were extracted and recorded on a customised spreadsheet by one author (LC), and double-checked by another author (DS). Disagreements were resolved by a third author (MW). Sample populations were classified into three age groups: children (≤ 12 years), adolescents (13–18 years), and adults (≥ 19 years). Participation level was classified into three categories: amateur (including recreational, high school and intramural athletes), intermediate (including collegiate and semi-professional athletes), and elite (including professional and national-level athletes) [9]. If not explicitly reported, incidences (per 1000 exposure units) were calculated from the available raw data using the following formula:
2.4 Statistical Analysis
All meta-analyses were performed in R (V. 3.6.1 and later, the R Foundation for Statistical Computing) using the meta (metarate, metaprop, metareg, and forest.meta functions) and tidyverse packages. Meta-analyses of incidence were carried out using a random effects Poisson regression model (unconditional model – random study effects) to produce forest plots with 95% confidence intervals (CIs) [25, 26]. The Poisson regression model was selected because of the binary and frequentist nature of the incidence data, corresponding to similar, previously employed methods [22, 27]. Statistical heterogeneity was assessed using the I2 statistic where I2 < 50% was considered as not important, 50–75% as moderate, and > 75% as high heterogeneity [28]. Between-study variance was estimated using the maximum-likelihood method. Meta-analyses were only performed when there were three or more included studies. Meta-analyses of proportions were performed using the Freeman-Tukey Double arcsine transformation [29, 30]. Confidence intervals for individual studies were calculated using the Clopper-Pearson interval, and estimations of between-study variance were performed using the DerSimonian-Laird method. The α level for all meta-analyses was set at 0.05. Funnel plots were used to assess publication bias in studies included in meta-analyses of overall proportion of non-contact to total ACL injuries and overall incidence of non-contact ACL injuries. Like previous systematic reviews [31, 32], we conducted subgroup and meta-regression analyses to investigate sources of heterogeneity and the association of the following categorical variables with proportion and incidence of non-contact ACL injuries: exposure type unit, sex, sport, age group, participation level, and exposure type (competition vs. training). For all analyses except meta-analyses of incidence by exposure type, we only synthesised studies when both training and competition data together were available. Additional sub-group analyses were attempted where possible.
3 Results
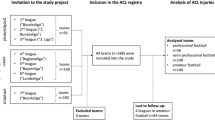
The online database and bibliographic hand search yielded 8,015 non-duplicate studies that were screened by title and abstract: 708 potentially eligible studies were identified. Following full-text review of the 708 studies, 45 met the inclusion criteria and were included in this review (Fig. 1) [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77]. Two studies shared the same dataset [43, 44], and therefore only 44 studies are reflected in Tables 1 and 2.
3.1 Description of Included Studies
A total of 2,748 non-contact ACL injuries were recorded across 45 million player-hours and player-exposures combined (5 million player-hours and 40 million player-exposures) from 13 sports (soccer, American Football, rugby union, Australian football, Gaelic football, basketball, netball, volleyball, field hockey, floorball, lacrosse, baseball, softball) (Table 1). Most studies defined injuries based on the “time-loss” definition (89%) [11], and injury data were primarily collected and recorded by medical staff (91%). In studies that defined non-contact injury mechanisms (68%), some seemed to consider non-contact and indirect contact mechanisms together [58, 62, 75], while the rest defined the non-contact mechanism as no apparent player-player, surface-player, and ball-player contact.
3.2 Study Quality Assessment
Initial agreement between reviewers was 80% (212 of 264 items), but all disagreements were subsequently resolved by consensus. Seventeen studies were awarded the maximum six stars and one study scored two stars (Table 2) [69]. Stars were most often not awarded because the population was not fully described (item (a): 41% awarded no stars), and because non-contact injury mechanisms were not defined (item (e): 32%).
3.3 Publication Bias
Visual inspection of the funnel plots indicated that almost all studies in the meta-analyses had low standard errors, possibly due to large cohort sizes (Appendix A3). Studies were missing from the lower right quadrant in the funnel plot to assess publication bias in studies included in meta-analyses of overall proportion of non-contact to total ACL injuries, and this quadrant represents smaller studies with a high proportion of non-contact to total ACL injuries. Studies were evenly distributed in the funnel plot to assess publication bias in studies included in meta-analyses of overall incidence of non-contact ACL injuries.
3.4 Proportion of Non-contact Anterior Cruciate Ligament (ACL) Injuries to Total ACL Injuries
The overall proportion of non-contact ACL injuries to total ACL injuries was 55% (95% CI 48–62, I2 = 82%) (Fig. 2).
Forest plot of meta-analysis of proportion of ACL injuries sustained by non-contact mechanisms by sex. AD, adults; ADO, adolescents; Am Football, American Football; Au Football, Australian Football; Union, Rugby union; blue square, point estimate; red diamond, combined point estimate and 95% confidence intervals
3.4.1 By Sex
Non-contact ACL injury proportion was higher among female athlete (63%, 95% CI 53–71, I2 = 84%) compared to male athletes (50%, 95% CI 42–58, I2 = 86%) (Fig. 2).
3.4.2 By Sport
The overall proportion of non-contact ACL injuries to total ACL injuries was 66% in floorball (95% CI 15–100, I2 = 73%), 58% in basketball (95% CI 49–67, I2 = 84%), 54% in rugby union (95% CI 18–88, I2 = 42%), 53% in soccer (95% CI 46–61, I2 = 78%), and 38% in American football (95% CI 28–48, I2 = 89%) (Appendix A4-1). We were unable to perform meta-analyses for the other sports because there were less than three included studies (Appendix A4-1). Only the difference between field hockey and American football was significant, as confirmed by meta-regression (β = 0.29, 95% CI 0.03–0.55, p = 0.03) (Appendix B1). There were sufficient studies to sub-group by sport and sex for soccer only. In female soccer athletes, the proportion of non-contact to total ACL injuries was 55% (95% CI 45–65, I2 = 76%) (Appendix A4-2).
3.4.3 By Age Group
The overall proportion of non-contact ACL injuries to total ACL injuries was 55% in adults (95% CI 48–63, I2 = 90%) and 68% in adolescents (95% CI 43–90, I2 = 88%) (Appendix A5-1). After sub-grouping by age group and sex, this proportion was 60% in adult female athletes (95% CI 49–70, I2 = 85%) and 52% in adult male athletes (95% CI 43–60, I2 = 86%) (Appendix A5-2). There were insufficient studies to investigate injury proportions by sex in adolescents (Appendix A5-3) [53, 59, 66]. None of the included studies investigated children.
3.4.4 By Participation Level
The overall proportion of non-contact to total ACL injuries by participation level was 61% in elite-level (95% CI 50–70, I2 = 16%), 55% in intermediate-level (95% CI 44–65, I2 = 93%), and 56% in amateur-level athletes (95% CI 45–767, I2 = 89%) (Appendix A6-1). After sub-grouping by participation level and sex, this proportion was 65% in elite-level female athletes (95% CI 47–70, I2 = 0%), and 59% in elite-level male athletes (95% CI 45–72, I2 = 31%) (Appendix A6-2). In intermediate-level athletes, the proportion of non-contact to total ACL injuries in females was 58% (95% CI 43–73, I2 = 89%), and in males was 50% (95% CI 36–64, I2 = 88%) (Appendix A6-3). In amateur-level athletes, this proportion was 67% in females (95% CI 52–81, I2 = 85%), and 48% in males (95% CI 35–60, I2 = 82%) (Appendix A6-4).
3.4.5 By Exposure Type
The overall proportion of non-contact to total ACL injuries by exposure type was 42% (95% CI 30–54, I2 = 92%) in competition and 47% in training settings (95% CI 29–64, I2 = 72%) (Appendix A7-1). After sub-grouping by exposure type and sex, the proportion of non-contact to total ACL injuries during competition in female athletes was 58% (95% CI 42–74, I2 = 79%), and 35% in male athletes (95% CI 23–48, I2 = 87%) (Appendix A7-2). This difference between females and male athletes was significant as confirmed by meta-regression (β = − 0.22, 95% CI − 0.42 to − 0.02, p = 0.02) (Appendix B2). In training settings, this proportion was 68% in female athletes (95% CI 0.34–0.95, I2 = 60%) and 36% in male athletes (95% CI 21–53, I2 = 54%) (Appendix A7-3).
3.5 Incidence of Non-contact ACL Injuries
The overall incidence of non-contact ACL injuries was 0.07 per 1000 player-hours (95% CI 0.05–0.10, I2 = 77%) (Fig. 3), and 0.05 per 1000 player-exposures (95% CI 0.03–0.07, I2 = 97%) (Fig. 4). Figure 5 displays a summary of injury incidence meta-analyses by player-hours.
Forest plot of meta-analysis of incidence of non-contact ACL injuries per 1000 player-hours by sex. AD, adults; ADO, adolescents; Am Football, American Football; Au Football, Australian Football; Union, Rugby union; blue square, point estimate; red diamond, combined point estimate and 95% confidence intervals
Forest plot of meta-analysis of incidence of non-contact ACL injuries per 1000 player-exposures by sex. AD, adults; ADO, adolescents; Am Football, American Football; Au Football, Australian Football; Union, Rugby union; blue square, point estimate; red diamond, combined point estimate and 95% confidence intervals
3.5.1 By Sex
In females, non-contact ACL injury incidence was 0.14 per 1000 player-hours (95% CI 0.10–0.19, I2 = 40%) and 0.06 per 1000 player-exposures (95% CI 0.04–0.11, I2 = 97%) (Figs. 3, 4). In males, injury incidence was 0.05 per 1000 player-hours (95% CI 0.03–0.07, I2 = 48%) and 0.04 per 1000 player-exposures (95% CI 0.03–0.07, I2 = 93%). Only the difference between female and male athletes per 1000 player-hours was significant as confirmed by meta-regression (β = − 1.15, 95% CI − 1.58 to − 0.73, p < 0.01) (Appendix B2).
3.5.2 By Sport
Overall, non-contact injury incidence was 0.06 per 1000 player-hours (95% CI 0.02–0.18, I2 = 68%) in rugby union, 0.08 per 1000 player-hours (95% CI 0.05–0.12, I2 = 84%) and 0.05 per 1000 player-exposures (95% CI 0.03–0.9, I2 = 97%) in soccer, 0.17 per 1000 player-hours in floorball (95% CI 0.09–0.32, I2 = 41%), 0.05 per 1000 player-exposures in basketball (95% CI 0.03–0.11, I2 = 98%), and 0.06 per 1000 player-exposures in American football (95% CI 0.05–0.08, I2 = 87%) (Appendices A8-1 and 8-2). There were insufficient studies for field hockey [55], Australian football [62], rugby sevens [41], lacrosse [48], volleyball [56], baseball [56], softball [56] and Gaelic football [77] (Table 1).
Sub-grouping by sport and sex was only possible for soccer and basketball. In soccer, injury incidence was higher in female athletes (0.13 per 1000 player-hours, 95% CI 0.09–0.19, I2 = 52%; 0.07 per 1000 player-exposures, 95% CI 0.05–0.11, I2 = 95%) compared to male athletes (0.04 per 1000 player-hours, 95% CI 0.03–0.05, I2 = 0%; 0.03 per 1000 player-exposures, 95% CI 0.01–0.09, I2 = 95%) (Appendices A8-3 and 8-4). Only the difference between female and male soccer athletes per 1000 player-hours was significant as confirmed by meta-regression (β = − 1.09, 95% CI − 1.38 to − 0.81, p < 0.01) (Appendix B2). Injury incidence was higher in female basketball players (0.11 per 1000 player-exposures, 95% CI 0.06–0.20, I2 = 97%) compared to males (0.03 per 1000 player-exposures, 95% CI 0.02–0.05, I2 = 89%) and this difference was significant (β = − 1.34, 95% CI − 2.25 to − 0.43, p < 0.01) (Appendices A8-5 and B2).
3.5.3 By Age Group
The overall incidence of non-contact ACL injuries in adults was 0.07 per 1000 player-hours (95% CI 0.05–0.10, I2 = 75%) and 0.08 per 1000 player-exposures (95% CI 0.06–0.11, I2 = 97%) (Appendices A9-1 and 9-2). In adolescents, the incidence was 0.19 per 1000 player-hours (95% CI 0.09–0.38, I2 = 57%) and 0.02 per 1000 player-exposures (95% CI 0.01–0.04, I2 = 94%) (Appendices 9-1 and 9-2). Only the difference between adults and adolescents per 1000 player-exposures was significant as confirmed by meta-regression (β = − 1.28, 95% CI − 1.87 to − 0.69, p < 0.01) (Appendix B2).
After sub-grouping by age group and sex, adult injury incidence was 0.11 per 1000 player-hours (95% CI 0.04–0.09, I2 = 74%) and 0.08 per 1000 player-exposures in female athletes (95% CI 0.05–0.11, I2 = 93%), and 0.05 per 1000 player-hours (95% CI 0.03–0.07, I2 = 55%) and 0.06 per 1000 player-exposures (95% CI 0.04–0.09, I2 = 89%) in male athletes (Appendices A9-3 and 9–4). The differences between adult male and female athletes per 1000 player-hours and player-exposures were significant as confirmed by meta-regression (β = − 1.08, 95% CI − 1.35 to − 0.81, p < 0.01 and β = − 0.69, 95% CI − 1.29 to − 0.10, p = 0.02, respectively) (Appendix B2). In adolescents, injury incidence was 0.02 per 1000 player-exposures in male athletes (95% CI 0.01–0.02, I2 = 89%), and 0.28 per 1000 player-hours (95% CI 0.17–0.46, I2 = 26%) and 0.03 per 1000 player-exposures for female athletes (95% CI 0.02–0.06, I2 = 91%) (Appendices A9-5 and A9-6). There were insufficient studies of male adolescent athletes to compare incidence per 1000 player-hours between adolescent male and female athletes [58, 66].
3.5.4 By Participation Level
Overall, the incidence of non-contact ACL injuries in elite-level athletes was 0.06 per 1000 player-hours (95% CI 0.04–0.09, I2 = 68%), in intermediate-level athletes 0.10 per 1000 player-hours (95% CI 0.06–0.18, I2 = 76%) and 0.10 per 1000 player-exposures (95% CI 0.06–0.17, I2 = 98%), and in amateur-level athletes 0.13 per 1000 player-hours (95% CI 0.07–0.24, I2 = 41%) and 0.03 per 1000 player-exposures (95% CI 0.02–0.05, I2 = 96%) (Appendices A10-1 and 10–2). There were insufficient studies of elite-level cohorts to compare incidence per 1000 player-exposures [68]. Only the difference between amateur- and intermediate-level athletes per 1000 player-exposures was significant as confirmed by meta-regression (β = 1.03, 95% CI 0.26–1.79, p < 0.01) (Appendix B2).
After sub-grouping by participation level and sex, the incidence of non-contact ACL injuries in elite-level female athletes was 0.10 per 1000 player-hours (95% CI 0.07–0.14, I2 = 19%) and in male athletes was 0.04 per 1000 player-hours (95% CI 0.03–0.05, I2 = 52%) (Appendix A10-3). There were insufficient studies to perform similar analyses per 1000 player-exposures [68]. The difference between male and female athletes per 1000 player-hours was significant as confirmed by meta-regression (β = − 0.91, 95% CI − 1.31 to − 0.52, p < 0.01) (Appendix B2). At the intermediate-level, injury incidence in females was 0.16 per 1000 player-hours (95% CI 0.12–0.21, I2 = 30%), and in male athletes was 0.04 per 1000 player-hours (95% CI 0.07–0.06, I2 = 0%) and 0.08 per 1000 player-exposures (95% CI 0.04–0.17, I2 = 92%) (Appendices A10-4 and A10-5). There were insufficient studies to meta-analyse data from female intermediate-level athletes [47]. Only the difference between male and female athletes per 1000 player-hours was significant as confirmed by meta-regression (β = − 1.32, 95% CI − 1.85 to − 0.80, p < 0.01) (Appendix B2). At the amateur-level, injury incidence in females was 0.27 per 1000 player-hours (95% CI 0.14–0.51, I2 = 0%) and 0.05 per 1000 player-exposures (95% CI 0.03–0.09, I2 = 95%), and in males was 0.10 per 1000 player-hours (95% CI 0.06–0.18, I2 = 0%) and 0.02 per 1000 player-exposures (95% CI 0.01–0.04, I2 = 95%) (Appendices A10-6 and A10-7).
3.5.5 By Exposure Type
The overall incidence of injury during competition was 0.48 per 1000 player-hours (95% CI 0.32–0.72, I2 = 77%) and 0.32 per 1000 player-exposures (95% CI 0.15–0.70, I2 = 96%), and during training was 0.04 per 1000 player-hours (95% CI 0.02–0.07, I2 = 63%) and 0.02 per 1000 player-exposures (95% CI 0.01–0.05, I2 = 86%) (Appendices A11-1 and A11-2).
After sub-grouping by exposure types and sex, injury incidence in female athletes during competition was 0.67 per 1000 player-hours (95% CI 0.33–1.35, I2 = 75%) and in training was 0.07 per 1000 player-hours (95% CI 0.05–0.10, I2 = 2%) (Appendix A11-3). There were insufficient studies to perform meta-analysis by player-exposures in females [45, 53]. For males, injury incidence was 0.37 per 1000 player-hours (95% CI 0.24–0.59, I2 = 72%) and 0.34 per 1000 player-exposures, 95% CI 0.12–0.99, I2 = 96%) during competition while for training was 0.02 per 1000 player-hours (95% CI 0.01–0.05, I2 = 55%) and 0.03 per 1000 player-exposures (95% CI 0.01–0.06, I2 = 83%). All competition to training comparisons reported above were significant as confirmed by meta-regression (Appendix B2).
3.5.6 Additional Sub-group Analyses
There were sufficient studies to perform a meta-analysis by participation level per 1000 player-hours for female soccer athletes. Injury incidence was higher in intermediate- (0.18 per 1000 player-hours, 95% CI 0.11–0.29, I2 = 57%) compared to elite-level athletes (0.10 per 1000 player-hours, 95% CI 0.07–0.15, I2 = 35%) (Appendix A12). This difference was significant as confirmed by meta-regression (β = 0.44, 95% CI < 0.01–0.88, p = 0.05) (Appendix B2).
4 Discussion
We conducted a systematic review with meta-analysis to estimate the proportion of non-contact to total ACL injuries and describe the incidence of non-contact ACL injuries in team ball-sports. Compared to the two most recent systematic reviews on ACL injury epidemiology, our review captured more ACL injuries, estimated incidence according to player-hours and player-exposures, and performed meta-regression analyses to investigate sources of heterogeneity and to test the influence of sex, age group, sport, participation level and exposure type on effect sizes [1, 9]. Overall, we found that non-contact ACL injuries represented over half of all ACL injuries sustained in team ball-sports. Non-contact ACL injury proportion was higher in female than male athletes in team ball-sports. Injury incidence was higher in females than males with most injuries occurring during competition team ball-sports. Intermediate-level male and female athletes were more likely to sustain non-contact ACL injuries than amateur-level athletes in team ball-sports. Heterogeneity across studies was generally high.
While female athletes are at a greater risk of ACL injuries compared to male athletes [1, 9, 78], this is the first systematic review to confirm that a similar sex disparity also exists for non-contact ACL injury risk. There is no consensus from multi-pronged research investigating the sex disparity in ACL injury rates through anatomical [79], physiological [80] and biomechanical lenses [81, 82], and injury rates in females remain high [1,2,3, 9]. A recent review by Parsons et al. called for ACL injury risk-reduction research to consider the influence of societal [83] and cultural norms of female athletes [84]. Parsons and colleagues provided the example that it is not uncommon for girls to be told to ‘get stronger’ to reduce ACL injury risk, but are not provided with equal opportunity and support to do so [84]. There is a need for a holistic approach to address this injury rate disparity.
Consistent with previous research, athletes were more likely to sustain non-contact ACL injuries in competition than training settings [43, 44, 51, 71]. Competition settings are often associated with additional internal and external stressors, and failure to manage these stressors may increase injury risk [85]. Training sessions are usually conducted in a more controlled environment than competition settings; therefore, it should be easier to reduce non-contact ACL injuries in training [38]. To do so, it seems logical to employ strategies like technique instruction, optimizing workload, and exercise-based IRRPs. However, the purpose of training is to prepare athletes for the physical demands of sport, and a reduction in injury incidence that comes at the expense of team performance may not be acceptable to coaches. While the search continues for the elusive training “sweet-spot” to reduce injury risk while improving performance [86], stakeholders should consider cost-effectiveness analyses and systems thinking approaches to assess injury risk reduction opportunities and challenges, as these are usually unique to each sport and setting [8, 87].
Our findings were inconclusive regarding the influence of sport, age group and participation level on non-contact ACL injury epidemiology in team ball-sports. In relation to the influence of sport, Montalvo et al. previously reported the highest incidence of ACL injuries in high-impact rotational landing (gymnastics, obstacle course race) and contact sports (soccer, basketball) [1]. It is not clear, however, if these differences were significant because meta-regression analyses were not performed in that study. One possible explanation for the lack of difference in our findings could be due to the common non-contact ACL injury scenarios and mechanisms across team ball-sports [4, 18, 88, 89]. In relation to the influence of age group, studies have suggested that children and adolescents are more susceptible to injury compared to adults because of their lower skill levels, physical capacities, and decision-making capabilities [90,91,92]. We only found a significant difference in injury incidence when comparing adults to adolescents by player-exposure but not for incidence by player-hours or proportion. None of the included studies investigated children. Sub-grouping by sex did not reveal any significant findings. With respect to participation level, our findings mirror the current state of evidence that it is not clear if amateur- and intermediate-level athletes are more susceptible to injuries, as found in some cohorts [1, 9], or if elite-level athletes are more susceptible [27, 93]. We did find, however, that intermediate-level male and female athletes were more likely to sustain non-contact ACL injuries than amateur-level athletes. We should caution that our findings on the influence of sport, age group, and participation level were from meta-analyses with high heterogeneity, and further sub-group analyses requiring more studies may be needed to determine the influence of these categorical predictors on non-contact ACL injury epidemiology.
Lastly, in order to fully establish the extent of an injury problem to inform the development of injury risk-reduction strategies, injury epidemiology studies must report injury mechanisms [7]. We had to exclude nearly four times as many studies from our review than those included because they did not report whether the injuries occurred via a direct contact or non-contact mechanism (168 studies excluded vs. 44 included) (Fig. 1). Additionally, authors from 22 out of the 46 included studies had to be contacted because non-contact ACL injury data were not available in the published manuscript [33,34,35,36,37,38,39,40,41,42,43,44, 50, 51, 55, 65, 66, 73,74,75,76,77]. To illustrate the importance of reporting injury mechanisms, the Australian Football League introduced rule changes to limit the run-up of ruckmen at the centre bounce that reduced posterior cruciate ligament (PCL) injury risk by half [94]. They were successful in doing so because they had identified that PCL injuries commonly occurred through knee-to-knee contact mechanisms, and by limiting the run up, ruckmen had lower momentum and were not jumping and lifting their knees up as high during these contests. Without knowledge that most PCL injuries occurred through contact mechanisms, the proposed injury counter-measures would not have been as effective. Therefore, future studies on injury epidemiology should adopt consensus statement guidelines to not just report injury magnitude, but also injury mechanisms and their accompanying definitions [11].
4.1 Limitations
Firstly, there was substantial heterogeneity among the included studies. This is inevitable in meta-analyses of epidemiological studies and does not invalidate our findings [95]. We attempted to investigate sources of heterogeneity via random-effects meta-analytical methods and sub-group analyses. Future research should explore potential sources of heterogeneity not investigated in our review. Next, previous knee and ACL injuries increase the risk of subsequent ACL injuries [96], but detailed information regarding medical history was not available in most included studies and therefore was not considered in this review. Subgrouping according to index versus re-injuries may improve the generalizability of our findings. Another limitation was that non-contact injury mechanisms were mostly defined in the included studies as the absence of direct player-to-player or player-to-surface contact (Table 1). However, these definitions were unclear on whether indirect contact mechanisms were considered. Indirect contact is defined as physical contact not applied directly to the knee, but contributes to the causal chain of events leading to an ACL injury [11]. For example, shoulder contact between soccer players jostling in mid-air for a header can result in an external perturbation of the centre of mass that affects knee landing kinematics and eventuates in an ACL rupture. Up to 44% of ACL injuries could be due to indirect contact mechanisms [4], and these injuries could arguably be prevented through careful drill design that replicates contact events in sport and instruction of proper technique [97]. The inclusion of ACL injuries sustained by indirect contact mechanisms would likely provide a more accurate estimate on the incidence and proportion of injuries that are amenable to exercise-based IRRPs. It is probable that ACL injury data might not be reported in studies where no ACL injuries occurred: these studies should report zero cases to prevent effect size overestimation. This review only included studies investigating team ball-sports and our results should not be generalized to all sports. Lastly, including non-published data might affect the validity and reproducibility of this review, so we used systematic and detailed criteria and processes to maintain transparency throughout this process.
5 Conclusion
Non-contact ACL injuries represented over half of all ACL injuries sustained in team-ball sports. The proportion of non-contact to total ACL injuries and injury incidence was higher in females than males in team ball-sports. Injuries mostly occurred in competition settings in team ball-sports. More research is required to fully understand the influence of sport, age group and participation level on injury proportion and incidence in team ball-sports. Our findings have implications for future ACL epidemiological research in sport, and the development and implementation of effective ACL injury risk reduction efforts in team ball-sports.
References
Montalvo AM, Schneider DK, Webster KE, Yut L, Galloway MT, Heidt RS, et al. Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train. 2019;54(5):472–82.
Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among US high school athletes, 2005/06–2010/11. Med Sci Sports Exerc. 2013;45(3):462.
Roos KG, Wasserman EB, Dalton SL, Gray A, Djoko A, Dompier TP, et al. Epidemiology of 3825 injuries sustained in six seasons of National Collegiate Athletic Association men’s and women’s soccer (2009/2010–2014/2015). Br J Sports Med. 2017;51(13):1029–34.
Della Villa F, Buckthorpe M, Grassi A, Nabiuzzi A, Tosarelli F, Zaffagnini S, et al. Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases. Br J Sports Med. 2020;54(23):1423–32.
Taylor JB, Waxman JP, Richter SJ, Shultz SJ. Evaluation of the effectiveness of anterior cruciate ligament injury prevention programme training components: a systematic review and meta-analysis. Br J Sports Med. 2015;49(2):79–87.
Vriend I, Gouttebarge V, Finch CF, Van Mechelen W, Verhagen EA. Intervention strategies used in sport injury prevention studies: a systematic review identifying studies applying the Haddon matrix. Sports Med. 2017;47(10):2027–43.
Van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. Sports Med. 1992;14(2):82–99.
Fuller CW. Assessing the return on investment of injury prevention procedures in professional football. Sports Med. 2019;49(4):621–9.
Montalvo AM, Schneider DK, Yut L, Webster KE, Beynnon B, Kocher MS, et al. “What’s my risk of sustaining an ACL injury while playing sports?” A systematic review with meta-analysis. Br J Sports Med. 2019;53(16):1003–12.
Brooks JH, Fuller CW. The influence of methodological issues on the results and conclusions from epidemiological studies of sports injuries. Sports Med. 2006;36(6):459–72.
Group IOCIIEC, Bahr R, Clarsen B, Derman W, Dvorak J, Emery CA, et al. International olympic committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sports 2020 (including the STROBE extension for sports injury and illness surveillance (STROBE-SIIS)). Orthop J Sports Med. 2020;8(2):2325967120902908.
Khan T, Alvand A, Prieto-Alhambra D, Culliford DJ, Judge A, Jackson WF, et al. ACL and meniscal injuries increase the risk of primary total knee replacement for osteoarthritis: a matched case–control study using the Clinical Practice Research Datalink (CPRD). Br J Sports Med. 2019;53(15):965–8.
Snoeker B, Turkiewicz A, Magnusson K, Frobell R, Yu D, Peat G, et al. Risk of knee osteoarthritis after different types of knee injuries in young adults: a population-based cohort study. Br J Sports Med. 2020;54(12):725–30.
Hägglund M, Waldén M, Magnusson H, Kristenson K, Bengtsson H, Ekstrand J. Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):738–42.
Eggerding V, Reijman M, Meuffels DE, van Es E, van Arkel E, van den Brand I, et al. ACL reconstruction for all is not cost-effective after acute ACL rupture. Br J Sports Med. 2021 (published online first: 18 March 2021).
Ardern CL, Kvist J, Webster KE. Psychological aspects of anterior cruciate ligament injuries. Oper Tech Sports Med. 2016;24(1):77–83.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, PRISMA, et al. explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2020;2021:372.
Montgomery C, Blackburn J, Withers D, Tierney G, Moran C, Simms C. Mechanisms of ACL injury in professional rugby union: a systematic video analysis of 36 cases. Br J Sports Med. 2018;52(15):994–1001.
Kluczynski MA, Kang JV, Marzo JM, Bisson LJ. Magnetic resonance imaging and intra-articular findings after anterior cruciate ligament injuries in ice hockey versus other sports. Orthop J Sports Med. 2016;4(5):2325967116646534.
Wells GA, Shea B, O’Connell Da, Peterson J, Welch V, Losos M, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford; 2000.
Diemer WM, Winters M, Tol JL, Pas HI, Moen MH. Incidence of acute hamstring injuries in soccer: a systematic review of 13 studies involving more than 3800 athletes with 2 million sport exposure hours. J Orthop Sports Phys Ther. 2021;51(1):27–36.
López-Valenciano A, Raya-González J, Garcia-Gómez JA, Aparicio-Sarmiento A, Sainz de Baranda P, De Ste Croix M, Ayala F (2021) Injury profile in women’s football: A systematic review and meta-analysis. Sports Med 51(3):423–42.
Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Bagos PG, Nikolopoulos GK. Mixed-effects Poisson regression models for meta-analysis of follow-up studies with constant or varying durations. Int J Biostat. 2009;5(1):Article 21.
Spittal MJ, Pirkis J, Gurrin LC. Meta-analysis of incidence rate data in the presence of zero events. BMC Med Res Methodol. 2015;15(1):1–16.
Williams S, Trewartha G, Kemp S, Stokes K. A meta-analysis of injuries in senior men’s professional rugby union. Sports Med. 2013;43(10):1043–55.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67(11):974–8.
Wilson F, Ardern CL, Hartvigsen J, Dane K, Trompeter K, Trease L, et al. Prevalence and risk factors for back pain in sports: a systematic review with meta-analysis. Br J Sports Med. 2021;55:601.
Jongsma HE, Turner C, Kirkbride JB, Jones PB. International incidence of psychotic disorders, 2002–17: a systematic review and meta-analysis. Lancet Public Health. 2019;4(5):e229–44.
Panagioti M, Khan K, Keers RN, Abuzour A, Phipps D, Kontopantelis E, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. BMJ. 2019;366:1–11.
Fuller C, Taylor A, Douglas M, Raftery M. Rugby World Cup 2019 injury surveillance study. S Afr J Sports Med. 2020;32(1):1–6.
Fuller CW, Taylor A, Kemp SP, Raftery M. Rugby world cup 2015: world rugby injury surveillance study. Br J Sports Med. 2017;51(1):51–7.
Fuller CW, Sheerin K, Targett S. Rugby world cup 2011: international rugby board injury surveillance study. Br J Sports Med. 2013;47(18):1184–91.
Fuller CW, Clarke L, Molloy MG. Risk of injury associated with rugby union played on artificial turf. J Sports Sci. 2010;28(5):563–70.
Brooks JH, Fuller C, Kemp S, Reddin DB. A prospective study of injuries and training amongst the England 2003 Rugby World Cup squad. Br J Sports Med. 2005;39(5):288–93.
West SW, Williams S, Kemp SP, Cross MJ, McKay C, Fuller CW, et al. Patterns of training volume and injury risk in elite rugby union: an analysis of 1.5 million hours of training exposure over eleven seasons. J Sports Sci. 2020;38(3):238–47.
Fuller C, Laborde F, Leather R, Molloy MG. International rugby board rugby world cup 2007 injury surveillance study. Br J Sports Med. 2008;42(6):452–9.
Taylor AE, Fuller CW, Molloy MG. Injury surveillance during the 2010 IRB women’s rugby world cup. Br J Sports Med. 2011;45(15):1243–5.
Fuller CW, Taylor A. Ten-season epidemiological study of match injuries in men’s international rugby sevens. J Sports Sci. 2020;38(14):1595–604.
Fuller CW, Taylor A, Raftery M. Eight-season epidemiological study of injuries in men’s international Under-20 rugby tournaments. J Sports Sci. 2018;36(15):1776–83.
Fuller CW, Dick RW, Corlette J, Schmalz R. Comparison of the incidence, nature and cause of injuries sustained on grass and new generation artificial turf by male and female football players. Part 2: training injuries. Br J Sports Med. 2007;41(suppl 1):i27–32.
Fuller CW, Dick RW, Corlette J, Schmalz R. Comparison of the incidence, nature and cause of injuries sustained on grass and new generation artificial turf by male and female football players. Part 1: match injuries. Br J Sports Med. 2007;41(suppl 1):i20–6.
Agel J, Olson DE, Dick R, Arendt EA, Marshall SW, Sikka RS. Descriptive epidemiology of collegiate women’s basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):202.
Dick R, Ferrara MS, Agel J, Courson R, Marshall SW, Hanley MJ, et al. Descriptive epidemiology of collegiate men’s football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):221.
Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33(4):524–31.
Anderson T, Wasserman EB, Shultz SJ. Anterior cruciate ligament injury risk by season period and competition segment: an analysis of National Collegiate Athletic Association injury surveillance data. J Athl Train. 2019;54(7):787–95.
Dallalana RJ, Brooks JH, Kemp SP, Williams AM. The epidemiology of knee injuries in English professional rugby union. Am J Sports Med. 2007;35(5):818–30.
Dönmez G, Korkusuz F, Özçakar L, Karanfil Y, Dursun E, Kudas S, et al. Injuries among recreational football players: results of a prospective cohort study. Clin J Sport Med. 2018;28(3):249–54.
Faude O, Junge A, Kindermann W, Dvorak J. Injuries in female soccer players: a prospective study in the German national league. Am J Sports Med. 2005;33(11):1694–700.
Giza E, Mithöfer K, Farrell L, Zarins B, Gill T. Injuries in women’s professional soccer. Br J Sports Med. 2005;39(4):212–6.
Gupta AS, Pierpoint LA, Comstock RD, Saper MG. Sex-based differences in anterior cruciate ligament injuries among United States High School Soccer Players: an epidemiological study. Orthop J Sports Med. 2020;8(5):2325967120919178.
Hartmut G, Becker A, Walther M, Hess H. Injuries in women’s soccer: a 1-year all players prospective field study of the women’s Bundesliga (German premier league). Clin J Sport Med. 2010;20(4):264–71.
Hollander K, Wellmann K, Zu Eulenburg C, Braumann K-M, Junge A, Zech A. Epidemiology of injuries in outdoor and indoor hockey players over one season: a prospective cohort study. Br J Sports Med. 2018;52(17):1091–6.
Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48(6):810–7.
Krutsch W, Zeman F, Zellner J, Pfeifer C, Nerlich M, Angele P. Increase in ACL and PCL injuries after implementation of a new professional football league. Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2271–9.
Leppänen M, Pasanen K, Kujala UM, Vasankari T, Kannus P, Äyrämö S, et al. Stiff landings are associated with increased ACL injury risk in young female basketball and floorball players. Am J Sports Med. 2017;45(2):386–93.
Leyes JY, Pérez LT, de Olano CC. Lesión del ligamento cruzado anterior en fútbol femenino. Estudio epidemiológico de tres temporadas. Apunts Medicina de l’Esport. 2011;46(171):137–43.
Loughran GJ, Vulpis CT, Murphy JP, Weiner DA, Svoboda SJ, Hinton RY, et al. Incidence of knee injuries on artificial turf versus natural grass in National Collegiate Athletic Association American football: 2004–2005 through 2013–2014 seasons. Am J Sports Med. 2019;47(6):1294–301.
Nilstad A, Andersen TE, Bahr R, Holme I, Steffen K. Risk factors for lower extremity injuries in elite female soccer players. Am J Sports Med. 2014;42(4):940–8.
Orchard J, Seward H, McGivern J, Hood S. Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. Am J Sports Med. 2001;29(2):196–200.
Östenberg A, Roos H. Injury risk factors in female European football. A prospective study of 123 players during one season. Scand J Med Sci Sports. 2000;10(5):279–85.
Pasanen K, Parkkari J, Kannus P, Rossi L, Palvanen M, Natri A, et al. Injury risk in female floorball: a prospective one-season follow-up. Scand J Med Sci Sports. 2008;18(1):49–54.
Pasanen K, Bruun M, Vasankari T, Nurminen M, Frey WO. Injuries during the international floorball tournaments from 2012 to 2015. BMJ Open Sport Exerc Med. 2017;2:e000217.
Pasanen K, Hietamo J, Vasankari T, Kannus P, Heinonen A, Kujala UM, et al. Acute injuries in Finnish junior floorball league players. J Sci Med Sport. 2018;21(3):268–73.
Rekik RN, Tabben M, Eirale C, Landreau P, Bouras R, Wilson MG, et al. ACL injury incidence, severity and patterns in professional male soccer players in a Middle Eastern league. BMJ Open Sport Exerc Med. 2018;4:e000461.
Scranton PE Jr, Whitesel JP, Powell JW, Dormer SG, Heidt RS Jr, Losse G, et al. A review of selected noncontact anterior cruciate ligament injuries in the National Football League. Foot Ankle Int. 1997;18(12):772–6.
Şenişik S, Özgürbüz C, Ergün M, Yüksel O, Taskiran E, İşlegen Ç, et al. Posterior tibial slope as a risk factor for anterior cruciate ligament rupture in soccer players. J Sports Sci Med. 2011;10(4):763.
Waldén M, Hägglund M, Orchard J, Kristenson K, Ekstrand J. Regional differences in injury incidence in European professional football. Scand J Med Sci Sports. 2013;23(4):424–30.
Waldén M, Hägglund M, Magnusson H, Ekstrand J. Anterior cruciate ligament injury in elite football: a prospective three-cohort study. Knee Surg Sports Traumatol Arthrosc. 2011;19(1):11–9.
Webb M, Davis C, Westacott D, Webb R, Price J. Injuries in elite men’s lacrosse: an observational study during the 2010 world championships. Orthop J Sports Med. 2014;2(7):2325967114543444.
West SW, Starling L, Kemp S, Williams S, Cross M, Taylor A, et al. Trends in match injury risk in professional male rugby union: a 16-season review of 10 851 match injuries in the English Premiership (2002–2019): the professional rugby injury surveillance project. Br J Sports Med. 2020;55(12):676.
Whalan M, Lovell R, McCunn R, Sampson JA. The incidence and burden of time loss injury in Australian men’s sub-elite football (soccer): a single season prospective cohort study. J Sci Med Sport. 2019;22(1):42–7.
Willigenburg NW, Borchers JR, Quincy R, Kaeding CC, Hewett TE. Comparison of injuries in American collegiate football and club rugby: a prospective cohort study. Am J Sports Med. 2016;44(3):753–60.
Tondelli E, Boerio C, Andreu M, Antinori S. Impact, incidence and prevalence of musculoskeletal injuries in senior amateur male rugby: epidemiological study. Phys Sportsmed. 2021:1–7.
O’Connor S, Bruce C, Teahan C, McDermott E, Whyte E. Injuries in collegiate ladies Gaelic footballers: a 2-season prospective cohort study. J Sport Rehabil. 2020;30(2):261–6.
Bram JT, Magee LC, Mehta NN, Patel NM, Ganley TJ. Anterior cruciate ligament injury incidence in adolescent athletes: a systematic review and meta-analysis. Am J Sports Med. 2020:0363546520959619.
Chandrashekar N, Slauterbeck J, Hashemi J. Sex-based differences in the anthropometric characteristics of the anterior cruciate ligament and its relation to intercondylar notch geometry: a cadaveric study. Am J Sports Med. 2005;33(10):1492–8.
Shultz SJ, Schmitz RJ, Cameron KL, Ford KR, Grooms DR, Lepley LK, et al. Anterior cruciate ligament research retreat VIII summary statement: an update on injury risk identification and prevention across the anterior cruciate ligament injury continuum, March 14–16, 2019, Greensboro, NC. J Athl Train. 2019;54(9):970–84.
Holden S, Boreham C, Delahunt E. Sex differences in landing biomechanics and postural stability during adolescence: a systematic review with meta-analyses. Sports Med. 2016;46(2):241–53.
Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Jt Surg. 2004;86(8):1601–8.
Gokeler A, Benjaminse A, Della Villa F, Tosarelli F, Verhagen E, Baumeister J. Anterior cruciate ligament injury mechanisms through a neurocognition lens: implications for injury screening. BMJ Open Sport Exerc Med. 2021;7(2): e001091.
Parsons JL, Coen SE, Bekker S. Anterior cruciate ligament injury: towards a gendered environmental approach. Br J Sports Med. 2021 (published online first: 10 March 2021).
Mellalieu SD, Neil R, Hanton S, Fletcher D. Competition stress in sport performers: stressors experienced in the competition environment. J Sports Sci. 2009;27(7):729–44.
Gabbett TJ. The training—injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med. 2016;50(5):273–80.
Bolling C, Mellette J, Pasman HR, Van Mechelen W, Verhagen E. From the safety net to the injury prevention web: applying systems thinking to unravel injury prevention challenges and opportunities in Cirque du Soleil. BMJ Open Sport Exerc Med. 2019;5:e000492.
Waldén M, Krosshaug T, Bjørneboe J, Andersen TE, Faul O, Hägglund M. Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. Br J Sports Med. 2015;49(22):1452–60.
Koga H, Nakamae A, Shima Y, Iwasa J, Myklebust G, Engebretsen L, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38(11):2218–25.
Quatman-Yates CC, Quatman CE, Meszaros AJ, Paterno MV, Hewett TE. A systematic review of sensorimotor function during adolescence: a developmental stage of increased motor awkwardness? Br J Sports Med. 2012;46(9):649–55.
Emery CA, Pasanen K. Current trends in sport injury prevention. Best Pract Res Clin Rheumatol. 2019;33(1):3–15.
Doherty C, Delahunt E, Caulfield B, Hertel J, Ryan J, Bleakley C. The incidence and prevalence of ankle sprain injury: a systematic review and meta-analysis of prospective epidemiological studies. Sports Med. 2014;44(1):123–40.
Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. 2011;45(7):553–8.
Orchard JW, Seward H. Decreased incidence of knee posterior cruciate ligament injury in Australian Football League after ruck rule change. Br J Sports Med. 2009;43(13):1026–30.
Noubiap JJ, Balti EV, Bigna JJ, Echouffo-Tcheugui JB, Kengne AP. Dyslipidaemia in Africa—comment on a recent systematic review–Authors’ reply. Lancet Glob Health. 2019;7(3):e308–9.
Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Consortium M, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43(7):1583–90.
Buckthorpe M. Recommendations for movement re-training after ACL reconstruction. Sports Med. 2021:1–18.
Acknowledgements
Acknowledgement should be made to those authors who responded to our requests for information not included in their published manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
Lionel Chia, Danilo De Oliveira Silva, Matthew Whalan, Marnee J. McKay, Justin Sullivan, Colin W. Fuller and Evangelos Pappas declare that they have no conflicts of interest relevant to the content of this review.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Authors' contributions
All authors contributed to project conception, project planning and interpretation of data. LC conducted the literature search and data synthesis. LC and DS conducted the record screening and data extraction. LC and MW conducted the methodological evaluation. LC drafted the initial manuscript, which was critically revised and approved for submission by all authors. All authors read and approved the final manuscript.
Data availability
Raw data from data analysis are available upon reasonable request by contacting the corresponding author. The data are not publicly available because a portion of it is obtained directly from authors of the included studies, and subsequent approval from these authors is required.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chia, L., De Oliveira Silva, D., Whalan, M. et al. Non-contact Anterior Cruciate Ligament Injury Epidemiology in Team-Ball Sports: A Systematic Review with Meta-analysis by Sex, Age, Sport, Participation Level, and Exposure Type. Sports Med 52, 2447–2467 (2022). https://doi.org/10.1007/s40279-022-01697-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-022-01697-w