Abstract
Objectives
Accurate risk stratification of patients with stage II and III colorectal cancer (CRC) prior to treatment selection enables limited health resources to be efficiently allocated to patients who are likely to benefit from adjuvant chemotherapy. We aimed to investigate the cost-effectiveness of a recently developed deep learning-based prognostic method, Histotyping, from the perspective of the Norwegian healthcare system.
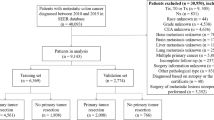
Methods
Two partitioned survival models were developed to assess the cost-effectiveness of Histotyping for two treatment cohorts: patients with CRC stage II and III. For each of the two cohorts, Histotyping was used for risk stratification to assign adjuvant chemotherapy and was compared with the standard of care (SOC) (adjuvant chemotherapy to all patients). Health outcomes measured in the model were quality-adjusted life years (QALYs) and life years (LYs) gained. Deterministic and probabilistic sensitivity analyses were performed to determine the impact of uncertainty. Scenario analyses were performed to assess the impact of the parameters with the greatest uncertainty.
Results
Risk-stratifying patients with CRC stage II and III using Histotyping was dominant (less costly and more effective) compared to SOC. In patients with CRC stage II, the net monetary benefit of Histotyping was 270,934 Norwegian kroners (NOK) (year of valuation is 2021), and the net health benefit of Histotyping was 0.99. In stage III, the net monetary benefit of Histotyping was 195,419 NOK, and the net health benefit of Histotyping was 0.71.
Conclusions
Risk-stratifying patients with CRC using Histotyping prior to the administration of adjuvant chemotherapy is likely to be a cost-effective strategy in Norway.




Similar content being viewed by others
References
GlobalData. Colorectal Cancer: Epidemiology Forecast to 2028. 2019. Contract No.: GDHCER220-19.
Norway CRo. Cancer in Norway 2018—Cancer incidence, mortality, survival and prevalence in Norway. Oslo; 2019. Report No.: 0806-3621.
Crooke H, Kobayashi M, Mitchell B, Nwokeji E, Laurie M, Kamble S, et al. Estimating 1-and 5-year relative survival trends in colorectal cancer (CRC) in the United States: 2004 to 2014. J Clin Oncol. 2018. https://doi.org/10.1200/JCO.2018.36.4_suppl.587.
Edge SB, Byrd DR, Carducci MA, Compton CC, Fritz A, Greene F. AJCC cancer staging manual. New York: Springer; 2010.
Osterman E, Glimelius B. Recurrence risk after up-to-date colon cancer staging, surgery, and pathology: analysis of the entire Swedish population. Dis Colon Rectum. 2018;61(9):1016–25.
Bi WL, Hosny A, Schabath MB, Giger ML, Birkbak NJ, Mehrtash A, et al. Artificial intelligence in cancer imaging: clinical challenges and applications. CA: Cancer J Clin. 2019;69(2):127–57.
Tsikitis VL, Larson DW, Huebner M, Lohse CM, Thompson PA. Predictors of recurrence free survival for patients with stage II and III colon cancer. BMC Cancer. 2014;14(1):1–7.
Copija A, Waniczek D, Witkoś A, Walkiewicz K, Nowakowska-Zajdel E. Clinical significance and prognostic relevance of microsatellite instability in sporadic colorectal cancer patients. Int J Mol Sci. 2017;18(1):107.
Lyu H, Xu T, Brotman D, Mayer-Blackwell B, Cooper M, Daniel M, et al. Overtreatment in the united states. PLoS ONE. 2017;12(9): e0181970.
Shrestha A, Martin C, Burton M, Walters S, Collins K, Wyld L. Quality of life versus length of life considerations in cancer patients: a systematic literature review. Psychooncology. 2019;28(7):1367–80.
Group F-NBW. BEST (Biomarkers, EndpointS, and other Tools) Resource [Internet]. 2016.
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, et al. Colon Cancer, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2021;19(3):329–59.
Argilés G, Tabernero J, Labianca R, Hochhauser D, Salazar R, Iveson T, et al. Localised colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31(10):1291–305.
Team O. The Oncotype® DX Breast Recurrence Score.
Yothers G, O’Connell MJ, Allegra CJ, Kuebler JP, Colangelo LH, Petrelli NJ, Wolmark N. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses. J Clin Oncol. 2011;29(28):3768.
Skrede OJ, De Raedt S, Kleppe A, Hveem TS, Liestøl K, Maddison J, et al. Deep learning for prediction of colorectal cancer outcome: a discovery and validation study. Lancet. 2020;395(10221):350–60.
Philips Z, Bojke L, Sculpher M, Claxton K, Golder S. Good practice guidelines for decision-analytic modelling in health technology assessment. Pharmacoeconomics. 2006;24(4):355–71.
Guidelines for the submission of documentation for single technology assessments (STAs) of medical devices and diagnostic interventions. In: Health NIoP, editor. 2020.
Seo MK, Strong M. A Practical Guide to Modeling and Conducting a Cost-Effectiveness Analysis of Companion Biomarker Tests for Targeted Therapies Using R: Tutorial Paper. PharmacoEconomics. 2021;1–9.
Yang L, Yang J, Kleppe A, Danielsen HE, Kerr DJ. Personalizing adjuvant therapy for patients with colorectal cancer. Nat Rev Clin Oncol. 2023;21:1–13.
Kerr RS, Love S, Segelov E, Johnstone E, Falcon B, Hewett P, et al. Adjuvant capecitabine plus bevacizumab versus capecitabine alone in patients with colorectal cancer (QUASAR 2): an open-label, randomised phase 3 trial. Lancet Oncol. 2016;17(11):1543–57.
Latimer NR. Survival analysis for economic evaluations alongside clinical trials-extrapolation with patient-level data [Internet]. 2013.
Joranger P, Nesbakken A, Hoff G, Sorbye H, Oshaug A, Aas E. Modeling and validating the cost and clinical pathway of colorectal cancer. Med Decis Making. 2015;35(2):255–65.
StatBank. Statistics Norway Mortality Tables. 2019. https://www.ssb.no/en/statbank/table/07902.
Felleskatalogen [The Norwegian Medicines Catalog]: Felleskatalog [The Norwegian Medicines Catalog]; 2020: https://www.felleskatalogen.no/medisin.
DCTD N, NIH, DHHS. Cancer Therapy Evaluation Program, Common Terminology Criteria for Adverse Events v3.0 (CTCAE) 2006.
Capecitabine Accord Felleskatalog2020: https://www.felleskatalogen.no/medisin/capecitabine-accord-accord-586441.
Oxaliplatin Fresenius Kabi Felleskatalog2019: https://www.felleskatalogen.no/medisin/oxaliplatin-fresenius-kabi-fresenius-kabi-568997.
DRG-systemet [DRG-system]. In: Health] HNDo, editor. Oslo: Helsedirektoratet; 2020.
Joranger P, Nesbakken A, Sorbye H, Hoff G, Oshaug A, Aas E. Survival and costs of colorectal cancer treatment and effects of changing treatment strategies: a model approach. Eur J Health Econ. 2020;21(3):321–34.
Bjørnelv GMW, Edwin B, Fretland ÅA, Deb P, Aas E. Till death do us part: the effect of marital status on health care utilization and costs at end-of-life. A register study on all colorectal cancer decedents in Norway between 2009 and 2013. BMC Health Serv Res. 2020;20(1):115.
Ramsey SD, Andersen MR, Etzioni R, Moinpour C, Peacock S, Potosky A, Urban N. Quality of life in survivors of colorectal carcinoma. Cancer. 2000;88(6):1294–303.
Fryback DG, Dasbach EJ, Klein R, Klein BE, Dorn N, Peterson K, Martin PA. The Beaver Dam Health Outcomes Study: initial catalog of health-state quality factors. Med Decis Making. 1993;13(2):89–102.
Magnussen J, Aaserud M, Granaas T, Magelssen M, Syse A, Celius E. På ramme alvor-Alvorlighet og prioritering. Department of Health (p. 71). English summary available from: https://www.regjeringen.no/contentassets/d5da48ca5d1a4b128c72fc5daa3b4fd8/summary_the_magnussen_report_on_severity.pdf. 2015.
Briggs A, Sculpher M, Buxton M. Uncertainty in the economic evaluation of health care technologies: the role of sensitivity analysis. Health Econ. 1994;3(2):95–104.
Hornberger J, Lyman GH, Chien R, Meropol NJ. A multigene prognostic assay for selection of adjuvant chemotherapy in patients with T3, stage II colon cancer: impact on quality-adjusted life expectancy and costs. Value in Health. 2012;15(8):1014–21.
Jongeneel G, Greuter MJ, van Erning FN, Koopman M, Vink GR, Punt CJ, Coupé VM. Model-based effectiveness and cost-effectiveness of risk-based selection strategies for adjuvant chemotherapy in Dutch stage II colon cancer patients. Ther Adv Gastroenterol. 2021;14:1756284821995715.
Alberts SR, Yu TM, Behrens RJ, Renfro LA, Srivastava G, Soori GS, et al. Comparative economics of a 12-gene assay for predicting risk of recurrence in stage II colon cancer. Pharmacoeconomics. 2014;32:1231–43.
To YH, Degeling K, Kosmider S, Wong R, Lee M, Dunn C, et al. Circulating tumour DNA as a potential cost-effective biomarker to reduce adjuvant chemotherapy overtreatment in stage II colorectal cancer. Pharmacoeconomics. 2021;39(8):953–64.
Alarid-Escudero F, Schrag D, Kuntz KM. CDX2 biomarker testing and adjuvant therapy for stage II colon cancer: an exploratory cost-effectiveness analysis. Value in Health. 2022;25(3):409–18.
Kleppe A, Skrede O-J, De Raedt S, Hveem TS, Askautrud HA, Jacobsen JE, et al. A clinical decision support system optimising adjuvant chemotherapy for colorectal cancers by integrating deep learning and pathological staging markers: a development and validation study. Lancet Oncol. 2022;23(9):1221–32.
Jones L, Hawkins N, Westwood M, Wright K, Richardson G, Riemsma R. Systematic review of the clinical effectiveness and cost-effectiveness of capecitabine (Xeloda) for locally advanced and/or metastatic breast cancer. Health Technol Assess (Winchester, England). 2004;8(5):iii–143.
Acknowledgements
Thank you to Dr. Håvard E.G. Danielsen for facilitating and supporting the project and to Dr. Andreas Kleppe for thoughtful input and helpful discussions throughout the data structuring and analysis. Thank you to Dr. Arild Nesbakken and Dr. Ole Kristian Andersen for providing invaluable clinical expertise. We thank Mariann Mathisen of the academic library at Vestfold Hospital Trust for her assistance conducting a thorough and structured literature search. We would also like to thank the QUASAR 2 trial for access to the patient material and data as well as all participating patients.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the Norwegian Research Council through the DoMore Project (259204) and the Bench to Bedside Project (309610).
Conflict of interest
AK, DK, HA, and JEJ report having stocks in DoMore Diagnostics. All other authors declare no competing interests. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Availability of data and material
All necessary data and information are provided in this article.
Ethical approval
Not applicable.
Consent to participate
All authors consent to participate.
Consent for publication
All authors consent for publication.
Code availability
Not applicable.
Author contributions
Study concept and design: AK, DK, MKS, EA, JEJ. Data analysis: AK, DK, MKS. Model development: AK, DK, MKS. Manuscript writing, original draft: AK, DK. Manuscript review and editing: AK, DK, MKS, EA, JC, DK, HA, JEJ. Supervision: MKS
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kenseth, A., Kantorova, D., Seo, M.K. et al. Is Risk-Stratifying Patients with Colorectal Cancer Using a Deep Learning-Based Prognostic Biomarker Cost-Effective?. PharmacoEconomics (2024). https://doi.org/10.1007/s40273-024-01371-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s40273-024-01371-1