Abstract
Background
Socioeconomic status has an important effect on cardiovascular disease (CVD). Data on the economic implications of CVD by socioeconomic status are needed to inform healthcare planning.
Objectives
The aim of this study was to project new-onset CVD and related health economic outcomes in Australia by socioeconomic status from 2021 to 2030.
Methods
A dynamic population model was built to project annual new-onset CVD by socioeconomic quintile in Australians aged 40–79 years from 2021 to 2030. Cardiovascular risk was estimated using the Pooled Cohort Equation (PCE) from Australian-specific data, stratified for each socioeconomic quintile. The model projected years of life lived, quality- adjusted life-years (QALYs), acute healthcare medical costs, and productivity losses due to new-onset CVD. All outcomes were discounted by 5% annually.
Results
PCE estimates showed that 8.4% of people in the most disadvantaged quintile were at high risk of CVD, compared with 3.7% in the least disadvantaged quintile (p < 0.001). From 2021 to 2030, the model projected 32% more cardiovascular events in the most disadvantaged quintile compared with the least disadvantaged (127,070 in SE 1 vs. 96,222 in SE 5). Acute healthcare costs in the most disadvantaged quintile were Australian dollars (AU$) 183 million higher than the least disadvantaged, and the difference in productivity costs was AU$959 million. Removing the equity gap (by applying the cardiovascular risk from the least disadvantaged quintile to the whole population) would prevent 114,822 cardiovascular events and save AU$704 million of healthcare costs and AU$3844 million of lost earnings over the next 10 years.
Conclusion
Our results highlight the pressing need to implement primary prevention interventions to reduce cardiovascular health inequity. This model provides a platform to incorporate socioeconomic status into health economic models by estimating which interventions are likely to yield more benefits in each socioeconomic quintile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cardiovascular disease risk and prevalence is influenced by social determinants of health, including socioeconomic status. |
In this study, we estimated the health and economics impact of new-onset cardiovascular disease in Australia by socioeconomic disadvantage for the next 10 years. |
Over the next 10 years, the most socioeconomically disadvantaged group would have 30,848 extra cardiovascular events compared with the group with the least disadvantage, which will translate to AU$183 million extra healthcare costs. The excess of productivity losses will surpass AU$959 million. Immediate policies are needed to reduce the burden of health inequity in Australia. |
1 Introduction
Cardiovascular disease (CVD) remains the leading cause of death and disability worldwide [1]. In Australia, CVD was the underlying cause for 26% of all deaths in 2018, and 11% of all hospitalisations listed CVD as the principal diagnosis or as an additional diagnosis [2]. The economic burden of CVD in Australia is also substantial, accounting for 9% of total government healthcare expenditure in 2015–2016, which translated to AU$10.4 billion [3].
Social determinants of health, including socioeconomic status, have a major influence on CVD, and the inverse association between socioeconomic status and cardiovascular risk in high-income countries is well described [4,5,6]. Education and income levels, type of professional occupation, and employment status show associations with atherosclerotic risk factors such as smoking, blood pressure, and cholesterol levels [7,8,9]. The persistence of health inequities is pervasive, even in countries with universal healthcare coverage. In Australia, despite the theoretical universality of the healthcare system [10] and the success of some population-level interventions targeting individual risk factors (e.g. smoking) [11], the equity gap remains [12]. In 2017–2018, the Australian National Health Survey (NHS) reported that CVD prevalence, morbidity, and mortality increased substantially with increasing socioeconomic disadvantage [13].
Addressing the impact of socioeconomic status on CVD calls for innovative, structural policies supported by health and economic arguments [14, 15]. Data on the economic implications of CVD by socioeconomic status are needed to inform preventive investments and can drive the agenda for future health financing. In the present study, we quantify the health and economic impact of new-onset CVD in Australia by socioeconomic disadvantage for 2021–2030, which can inform health inequality distribution for cost-effective analyses [16]. Furthermore, we projected the health and economic impacts of a hypothetical targeted intervention that removes the equity gap, highlighting the utility of the model.
2 Methods
2.1 Model Overview and Structure
We estimated new-onset CVD (comprising myocardial infarction [MI] or stroke) by socioeconomic quintile among Australians aged 40–79 years over a 10-year period, from 2021 to 2030. The model projected new-onset cardiovascular events, years of life lived, quality-adjusted life-years (QALYs), direct healthcare medical costs for acute events, and productivity losses due to new-onset CVD. The analysis considered both a healthcare and a societal perspective (comprised of direct healthcare costs and indirect costs including productivity losses).
The dynamic population model comprised two health states: ‘Alive, with no CVD’, and ‘Dead’. All individuals entered the model in the ‘Alive, with no CVD’ state, and, during each yearly cycle, were at risk of experiencing a non-fatal CVD event (including MI or stroke) or dying from cardiovascular or non-cardiovascular causes (electronic supplementary material [ESM] Appendix 1). After having a non-fatal cardiovascular event, individuals were excluded from the model population from the next cycle. The model captured the number of new-onset cardiovascular events (fatal and non-fatal), as well as quality of life and acute medical costs (due to hospitalisations), in the year of occurrence. The dynamic nature of the model meant that any Australian turning 40 years of age within the period 2021–2030 entered the model, while those turning 80 years exited. Immigration rates were also considered. All outcomes were discounted by 5% annually, as per Australian guidelines [17].
Socioeconomic status was measured using the Socio-Economic Indexes for Areas (SEIFA), an indicator of relative socioeconomic disadvantage based on the area of residency [18]. Lower scores indicate more socioeconomic disadvantage, while higher scores indicate less disadvantage. SEIFA is based on a number of variables from the Australian census, such as the highest level of education achieved, the average income levels, and employment rates [18]. For this study, SEIFA deciles were grouped in quintiles, defining five socioeconomic levels (SE 1–SE 5).
2.2 Model Population
The model population was profiled on the latest available demographic data for the Australian population in 2020 [19] (ESM Appendix 2) divided into five quintiles, each representing a socioeconomic quintile, with SE 1 being the lowest socioeconomic quintile (most disadvantaged) and SE 5 being the highest quintile (least disadvantaged). To capture the dynamic nature of the population, projected numbers of Australians turning 40 years of age (including migrants) were added at the commencement of each cycle. Similarly, projected numbers of Australians turning 80 years of age and emigrants were subtracted from the model population with each cycle. The projected population (2021–2030) was estimated from the Australian Bureau of Statistics data [20]. Prevalent CVD rates (defined as a history of MI or stroke) were extracted from the most recent Australian NHS 2017–2018 [13], and individuals with prevalent CVD were excluded from the model baseline population.
2.3 Risk of New-Onset Cardiovascular Disease by Socioeconomic Quintile
Data to estimate cardiovascular risk and to assign socioeconomic quintile were extracted from the Australian NHS 2011–2012, the latest NHS with information on biomarkers [21]. Descriptive statistics were used to summarise general demographic and clinical characteristics for the 2011–2012 NHS population (n = 3,299 with available SEIFA and biomarker data without a history of CVD) (Table 1). Data for age and cholesterol were supplied as categorical variables and recoded into continuous variables using the mid-point of each category.
To estimate cardiovascular risk by socioeconomic quintile, participants from the NHS 2011–2012 were first stratified by their socioeconomic quintile. Following stratification, the cardiovascular risk for each participant was estimated using the Pooled Cohort Equation (PCE) [22]. The algorithm underpinning the PCE is based on age, sex, total cholesterol, high-density lipoprotein cholesterol (HDL-C), systolic blood pressure, smoking status and diabetes status [22]. The PCE algorithm also includes the population baseline survival [22], which was specific for each socioeconomic quintile [23] (ESM Appendix 3).
The PCE has been validated for the Australian population and has shown superior performance over other cardiovascular risk algorithms [24]. Cardiovascular risk as estimated from the PCE was categorised as either low (estimated 10-year risk of CVD < 7.5%), moderate (risk ≥ 7.5% and < 15%) or high (risk ≥ 15%), and within each socioeconomic quintile, the proportion of people in each risk category was estimated. To obtain sex-specific cardiovascular risk, individuals were further stratified by sex (ESM Appendix 4). To determine the probability of CVD for each single year of age, the average cardiovascular risk was calculated for 10-year age groups (i.e. 40–50 years, 50–60 years, etc.) and cubic polynomial equations were fitted on these data (ESM Appendix 5).
Since the PCE only estimates absolute CVD risk in terms of total major adverse cardiovascular events (MACE), in order to estimate specific events Australian hospitalisation data for 2017 were used to determine the relative proportions of non-fatal MI, non-fatal stroke and CVD death. To calculate mortality rates due to non-cardiovascular causes, cardiovascular mortality rates were subtracted from all-cause mortality rates in Australia in 2018 [23]. Age and sex-specific non-cardiovascular mortality data were drawn from the Australian Institute of Health and Welfare General Record of Incidence of Mortality [23] and were not specific by socioeconomic quintile. The resultant transition probabilities are shown in Appendix 6 of the ESM.
2.4 Costs
From a healthcare perspective, the model captured direct acute medical costs due to hospitalisation. The acute costs of non-fatal stroke, non-fatal MI and death from cardiovascular causes were derived from the Australian Refined Diagnosis Related Groups (DRGs; version 8, round 21) for 2017–2018 Australian hospital admissions [25]. Conservatively, we assumed that half of the deaths occurred at home and half in hospital. Although the model projected deaths due to non-CVD causes, these were not included in the costs. All costs were adjusted to 2021 Australian dollars (AU$) using the health price index [26].
From a societal perspective, the model curated productivity losses using the human capital approach [27]. Productivity losses included the cost of absenteeism after a non-fatal event (for the year of the event), but the cost due to workforce dropouts were not incorporated since individuals with prevalent CVD were excluded from the simulation. Presenteeism was not included in the model due to a paucity of available data specific to acute events.
To calculate the cost of absenteeism after an acute non-fatal event, the average number of days of work missed after suffering an event [28, 29] was multiplied by the average daily earnings in Australia [30]. This cost was only applied in the year that the event occurred. Although average daily earnings will vary by socioeconomic disadvantage, this was not considered because average income by socioeconomic quintile is not published. Average salaries in Australia were adjusted for age, sex, and unemployment rates as per the latest 2020 published data [31]. Productivity losses also included the impact of CVD mortality by projecting the cost of premature deaths. The loss of future earnings due to premature CVD mortality was determined using the human capital approach [27] and was adjusted for the model time horizon or until retirement age, whichever came first. For example, if a person had 20 years of productivity remaining but died in 2021, only the first nine years contributed to the estimated loss of future earnings as the model time horizon was until 2030. Retirement age was set at 67 years of age [31].
2.5 Utilities
For the population in the ‘Alive, no CVD’ health state, age- and sex-specific utility scores were derived from a 2016 Australian cross-sectional study, which included more than 2000 participants from the general population [32]. The acute utility score for an MI was 0.70, and 0.63 for stroke [33, 34]. Chronic utilities were 0.80 for MI and 0.72 for stroke [33, 35]. The utility scores were applied to the year in which an acute non-fatal event occurred, as follows: general population utility scores were applied for 6 months, acute utility scores were applied for 3 months, and for the remaining 3 months, a chronic utility score was applied. The method applied to generate utilities has been previously published [36].
2.6 Statistical Analyses
To evaluate the association between socioeconomic quintile and cardiovascular risk factors, linear (for continuous variables) or logistic (for categorical variables) regression analyses were performed (adjusted for age and sex) (ESM Appendix 7). Differences in the proportion of other demographic characteristics (area of residence, income, and education) in each socioeconomic quintile were assessed using Chi-square tests. All analyses were conducted in R software version 4.0.3 (The R Foundation for Statistical Computing, Vienna, Austria) and the model was built using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA). All model inputs are presented in Appendix 8 of the ESM.
2.7 Sensitivity Analyses
To quantify uncertainty, probabilistic sensitivity analyses were performed by running 10,000 iterations of a Monte Carlo simulation. The respective candidate distributions for costs, effects and utilities were selected as per Briggs et al. [37] For each key output, 95% uncertainty intervals were estimated (ESM Appendix 8). In addition, we undertook scenario analyses to estimate the effect of theoretical interventions on health and economic outcomes. In the first scenario, the baseline cardiovascular risk in each socioeconomic quintile was reduced (separately) by 10% (mimicking an untargeted intervention). In the second scenario, the estimated cardiovascular risk obtained for the least disadvantaged quintile was applied to all other socioeconomic quintiles, which would mimic an intervention designed to remove the equity gap. In the last scenario analysis, we modelled the effect of the ‘Walk your Heart Health’ intervention [38], a community-based intervention in marginalised communities in the US. For this scenario, we applied the effect of the intervention on total cholesterol levels and blood pressure to the population in SE 1 and SE 2. Successful participation in the intervention was significantly associated with an odds ratio of 0.9 for hypertension as well as a mean reduction of 0.10 mmol/L of total cholesterol.
3 Results
3.1 Baseline Risk Profiling in the National Health Survey
Age, sex, total cholesterol, and prevalence of type 2 diabetes did not significantly differ by socioeconomic quintile. Systolic blood pressure and smoking rates increased (men and women) and HDL-C decreased (only in women), with increasing socioeconomic disadvantage (Table 1).
Results from cardiovascular risk profiling using the PCE showed that the proportion of people classified as high and moderate risk increased with increasing socioeconomic disadvantage (proportion at high risk from SE 1 to SE 5: 8.4%, 7.3%, 6.3%, 4.3% and 3.7%, respectively; p < 0.001) (Table 2); while the proportion of individuals at low risk decreased with increasing disadvantage (p < 0.001). When the population was stratified by sex, cardiovascular risk in men followed the socioeconomic gradient (i.e. lower risk in higher socioeconomic quintiles), while in women the quintile with the highest proportion at high cardiovascular risk was SE 2, not SE 1.
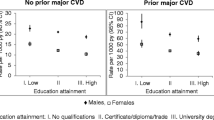
The estimated annual cardiovascular risk in men, by age, followed the social gradient for men 40–70 years of age; however, for the age quintile 70–79 years, SE 3 had the highest estimated rates of CVD. In women, SE 2 had the highest estimated rates of annual CVD for all age groups (Fig. 1 and ESM Appendix 4).
Annual cardiovascular events derived from the PCE and extrapolated for every single year of age, stratified by SE quintile and by sex. SE 1 represents the quintile with the most socioeconomic disadvantage, while SE 5 represents the quintile with the least socioeconomic disadvantage. SE socioeconomic quintile, PCE Pooled Cohort Equation
3.2 Health Outcomes
From 2021 to 2030, the model projected that 595,714 (456,401 non-fatal and 139,313 fatal) cardiovascular events would occur in Australians aged 40–79 years with no prior history of CVD (Table 3). When stratified by socioeconomic disadvantage, SE 2 was projected to accrue the largest health burden, with 133,776 cardiovascular events, followed by SE 1, with 127,070 cardiovascular events (Table 3). Despite quintile SE 1 having a larger proportion of the overall population at high CVD risk, SE 2 was estimated to have the largest burden of new-onset CVD, driven by the higher CVD rates obtained for women in this quintile. The least disadvantaged quintile (SE 5) accrued the lowest number of events, with 96,222 total cardiovascular events (Table 3). This difference translates to 30,848 fewer cardiovascular events in the highest quintile compared with the lowest during the 10-year period, representing a relative difference of 32.4%. When stratified by sex, men in SE 3 would have the highest number of new-onset CVDs (79,329 fatal and non-fatal cardiovascular events), followed by SE 1 (79,025 events). In women, the quintile with the largest burden was SE 2 (59,752 events).
3.3 Years of Life Lived and Quality-Adjusted Life-Years
Over the 10-year period, the model projected 132,588,290 total years of life lived among Australians with no prevalent CVD aged 40–79 years (Table 3). Following the same trend as cardiovascular events, the quintile SE 2 was estimated to accumulate the least number of years of life lived (26,498,033) and SE 5 was estimated to accrue the most years of life lived (26,550,257). Similarly, SE 2 was projected to accrue the least number of QALYs (23,447,375), while SE 5 was projected to accumulate the most (23,495,376). Through the modelled period, individuals in the highest quintile (SE 5) were estimated to accrue 39,026 more QALYs than individuals in the lowest quintile (SE 1).
3.4 Economic Outcomes
From a healthcare perspective, the total healthcare costs from acute cardiovascular events during the 10-year period were projected to be AU$3728 million. Again, the quintile SE 2 incurred the highest healthcare costs, surpassing AU$854 million, while the quintile SE 5 incurred the lowest healthcare costs at AU$605 million. The highest productivity losses due to acute morbidity and mortality were observed in quintile SE 2 (AU$3235 million), while the lowest were observed in quintile SE 5 (AU$2122 million) (Table 3).
3.5 Sensitivity Analyses
Uncertainty intervals resulting from Monte Carlo simulations for key outcomes are presented in Table 3 and Figure 2 as well as Appendix 9 of the ESM. In scenario analyses, reducing the baseline risk of CVD by 10% in each socioeconomic quintile separately showed that, as expected, larger benefits would be obtained in the socioeconomic quintiles with the highest baseline risk. For example, if a 10% reduction in baseline cardiovascular risk was applied to SE 2, 13,265 cardiovascular events would be prevented, with healthcare savings of AU$85 million. In contrast, applying a 10% CVD risk reduction to SE 5 resulted in 9,488 events prevented and healthcare savings of AU$60 million (Table 4).
Applying the CVD risk levels obtained for SE 5 to all remaining SE quintiles (i.e. removing the equity gap) would result in 114,822 less cardiovascular events, 144,688 QALYs gained, and healthcare savings of AU$704 million over the next 10 years (Table 4). In addition, removing the equity gap would save AU$3,844 million to the overall Australian economy in terms of productivity gains. Applying the effect of the targeted intervention ‘Walk your Heart Health’ [38] to SE 1 and SE 2 would prevent 17,919 cardiovascular events and a gain of 22,403 QALYs over the 10-year period, saving more than AU$87 million to the healthcare system and more than AU$541 million to the Australian society in productivity gains (Table 4).
4 Discussion
In this study, we projected new-onset CVD, quality of life, and consequent direct healthcare and productivity costs, stratified by socioeconomic group in Australia. The model showed that over the next 10 years, the most socioeconomically disadvantaged quintile would suffer 30,848 extra cardiovascular events compared with the quintile with the least disadvantage. Individuals in the most disadvantaged quintile will accrue 42,328 fewer years of life lived and 39,026 fewer QALYs than individuals in the least disadvantaged quintile. Similarly, direct healthcare costs in the most disadvantaged quintile will exceed those in the least disadvantaged by AU$183 million, and the excess cost of productivity losses will be AU$959 million. These findings highlight the societal burden of inequity in healthcare outcomes.
Individuals in the most disadvantaged quintile had lower levels of HDL-C, higher systolic blood pressure, and increased rates of smoking, consistent with prior studies in Australia and other high-income countries [39,40,41]. CVD risk profiling using the PCE showed an increasing trend in the proportion of individuals classified as high risk with increasing socioeconomic disadvantage, which was particularly obvious in men compared with women. Among women, SE 2 had the largest proportion of women classified as high risk, instead of SE 1.
This gender difference in the social gradient has been previously reported by the Australian Institute of Health and Welfare. One potential explanation is that while rates of CVD have decreased overall in the last 10 years, the reduction has been more pronounced in males of higher socioeconomic groups, widening the equity gap and making the differences more pronounced [42]. In our model, men in SE 5 had a pronounced decrease in CVD risk relative to the other quintiles, suggesting that in Australia, the protective effect of socioeconomic status on CVD is largely specific to the least disadvantaged group in men. However, the results of our projections estimating SE 2 as the quintile with the largest burden are mainly explained by the increased risk in women from SE 2, especially in those aged over 60 years. Several other factors could explain why SE 2 had worst outcomes, including potential socioeconomic misclassification. Since SEIFA is an area-level score, it does not take into account individual circumstances. The availability of biomarker data in the NHS was limited to 3,299 individuals from a sample of more than 20,000, which could have introduced potential for selection bias. Finally, a recent Australian study analysing consumption of ultra-processed foods reported that the second lowest household income quintile had the higher rates of ultra-processed food consumption in Australia, which could have an impact on CVD risk [43].
Although addressing health inequities requires broader policies outside of healthcare [44], health inequities related to social determinants of health can also be partly addressed through actionable public health policies [45]. The model used in this study allowed us to estimate the potential effects on CVD and economic benefits of preventive healthcare policies tailored to specific socioeconomic groups. For example, we estimated that if the equity gap was removed (i.e. applying the estimated cardiovascular risk obtained for SE 5 to all the quintiles), 114,822 events could be prevented and 144,688 QALYs could be gained. These health gains would translate to AU$704 million in savings for the healthcare system and AU$3,844 million for the Australian economy. While this example represents an incredibly optimistic situation, it is important to contrast these results to that of a non-targeted approach, especially as the feasibility and costs of each strategy are likely to differ.
Previous publications have suggested that policies to improve health outcomes should employ evidence-based and cost-effective interventions to address community-level factors affecting the most disadvantaged socioeconomic groups, rather than targeting behavioural or lifestyle factors that are likely to mostly benefit socioeconomic groups with the least disadvantage [46]. In addition, structural interventions aimed at addressing common risk factors could potentially provide more health and economic gains in the most disadvantaged groups since several risk factors, including smoking, dyslipidaemia, and alcohol consumption, are highest in these groups. Our results also highlight the importance of modelling the distribution of health benefits and including distributional cost-effective analyses in every health technology assessment [47].
The effect of disadvantage on productivity losses is consistent with a previous Australian study, which estimated that the most disadvantaged quintile accounted for 27% of lifetime income loss from CVD, while the least disadvantaged accounted for only 8%, despite an almost threefold difference in median income [48]. These results demonstrate that there is substantial inequity in premature death in Australia [48]. Moreover, Australia’s large size highlights the impact of distance from services (remoteness) on healthcare outcomes, as area of residence was strongly associated with socioeconomic disadvantage, and remoteness has been shown to be associated with both decreased access to healthcare and increased CVD risk, independent of socioeconomic disadvantage [49, 50].
4.1 Strengths and Limitations
Our study has several strengths. This is the first study to project new-onset CVD and health and economic outcomes by socioeconomic status in Australia. The transition probabilities informing the model were derived from a representative primary prevention population in Australia, with costs and utilities also being specific to an Australian setting. Our modelling approach allowed for testing of interventions aimed at different socioeconomic groups and has the potential to serve as a tool for evaluating healthcare policies prior to implementation. The inclusion of health equity into routine health economic evaluations is necessary.
Several limitations also warrant mention. First, we used the 2011–2012 NHS data to derive cardiovascular risk estimates, as this was the latest available NHS that included biomarkers, which may not accurately represent the current distribution of cardiovascular risk in the population. Moreover, the NHS sample of 3299 individuals represents < 1% of the Australian population aged 40–79 years with no history of CVD in 2020, and the number of NHS participants who had available data on biomarkers was lower for groups with higher socioeconomic disadvantage, which could have introduced selection bias. Second, SEIFA is an area-based measure of socioeconomic status and it does not consider discrepancies between the socioeconomic status of individuals and the average for their location, making misclassification a potential concern [21]. As we did not have data on the proportion of the population in each socioeconomic quintile, we assumed equal quintiles across the groups. However, SEIFA measures are widely used as a form of measuring socioeconomic status in social and epidemiological studies and have been validated against other indices. Similarly, the PCE restricts the ability to estimate the effect of important parameters for CVD, such as body mass index and low-density lipoprotein cholesterol. Furthermore, the applicability of PCE to non-White Australians is limited and may not provide an adequate estimate of cardiovascular risk for other population groups. Recent work on the applicability of the PCE has shown less accuracy for non-White populations in the US [51]. Nevertheless, the PCE was shown to have a better prediction performance for the Australian population when compared with other risk algorithms [24]. Third, our model was limited to acute events in a primary prevention population and it did not consider the chronic cost of CVD management or pharmacological treatment, or the potential differences in health service use between the different socioeconomic groups [52]. Given the high costs associated with chronic management of CVD, interventions aimed at the primary prevention population are likely to yield the largest benefits. However, the effect of including chronic disease, rehabilitation services, and other health services use would likely amplify the differences reported in this study and warrants further research. Conversely, not accounting for income differences by socioeconomic quintile and the exclusion of individuals over 79 years of age may have led to underestimation of the cost differences by socioeconomic disadvantage. Finally, this model could not consider changes in projections (immigration, mortality) or cardiovascular risk due to the coronavirus disease 2019 (COVID-19) pandemic.
5 Conclusion
This study projected new-onset CVD, related direct healthcare and productivity costs in Australia, stratified by socioeconomic disadvantage. The magnitude of difference between socioeconomic groups highlights the urgent need to implement structural prevention strategies targeted at disadvantaged groups that will provide net economic benefit. This model provides a platform to incorporate socioeconomic status in cost-effectiveness analyses and to assess which interventions are likely to yield more benefits in each socioeconomic group at the population level.
References
Roth GA, Mensah GA, Fuster V. The global burden of cardiovascular diseases and risks. J Am Coll Cardiol. 2020;76(25):2980–1. https://doi.org/10.1016/j.jacc.2020.11.021.
Australian Institute of Health and Welfare. Cardiovascular Disease In Australia. Canberra: AIHW
Australian Institute of Health and Welfare. Disease expenditure in Australia, 2015-16. https://www.aihw.gov.au/reports/health-welfare-expenditure/disease-expenditure-australia/contents/australian-burden-of-disease-conditions. Accessed 11 Jun 2020.
Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873–98. https://doi.org/10.1161/CIR.0000000000000228.
Kreatsoulas C, Anand SS. The impact of social determinants on cardiovascular disease. Can J Cardiol. 2010;26:8C-13C.
Girolamo CD, Nusselder WJ, Bopp M, et al. Progress in reducing inequalities in cardiovascular disease mortality in Europe. Heart. 2020;106(1):40–9. https://doi.org/10.1136/heartjnl-2019-315129.
Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33(2):221–9. https://doi.org/10.1097/HJH.0000000000000428.
Nordahl H, Rod NH, Frederiksen BL, et al. Education and risk of coronary heart disease: assessment of mediation by behavioral risk factors using the additive hazards model. Eur J Epidemiol. 2013;28(2):149–57. https://doi.org/10.1007/s10654-012-9745-z.
Kelli HM, Mehta A, Tahhan AS, et al. Low educational attainment is a predictor of adverse outcomes in patients with coronary artery disease. J Am Heart Assoc. 2019;8(17):e013165. https://doi.org/10.1161/JAHA.119.013165.
Australian Department of Health. The Australian health system. Published 10 Aug 2018. https://www.health.gov.au/about-us/the-australian-health-system. Accessed 19 Jul 2021.
Riseley K. Report on Smoke-Free Policies in Australia. World Health Organization. pp. 1–12.
Australia’s health 2018: in brief, all is not equal. Australian Institute of Health and Welfare. https://www.aihw.gov.au/reports/australias-health/australias-health-2018-in-brief/contents/all-is-not-equal. Accessed 12 May 2021.
National Health Survey: First results, 2017-18 financial year. Australian Bureau of Statistics. Published 12 Dec 2018. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-first-results/latest-release. Accessed 14 Jan 2021.
Kunst AE. Evaluation of health equity impact of structural policies. Int J Health Serv. 2017;47(3):432–9. https://doi.org/10.1177/0020731417709960.
Townsend B, Friel S, Freeman T, et al. Advancing a health equity agenda across multiple policy domains: a qualitative policy analysis of social, trade and welfare policy. BMJ Open. 2020;10(11):e040180. https://doi.org/10.1136/bmjopen-2020-040180.
Asaria M, Griffin S, Cookson R. Distributional cost-effectiveness analysis. Med Decis Making. 2016;36(1):8–19. https://doi.org/10.1177/0272989X15583266.
Pharmaceutical Benefits Advisory Committee. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (version 4.5). https://pbac.pbs.gov.au/content/information/archived-versions/pbac-guidelines-v4-5.pdf.
Australian Bureau of Statistics. SEIFA. Socio-Economic Indexes for Areas. Published 2011. https://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa. Accessed 11 May 2021.
Australian Bureau of Statistic. National, state and territory population, June 2020. Published 16 Sep 2021. https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release. Accessed 6 Oct 2021.
Australian Bureau of Statistics. Population projections Australia, 2017 (base)-2066. Published 22 Nov 2018. https://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/3222.0Main%20Features42017%20(base)%20-%202066?opendocument&tabname=Summary&prodno=3222.0&issue=2017%20(base)%20-%202066&num=&view=. Accessed 8 Jul 2020.
Australian Bureau of Statistics. Australian National Health Survey, First Results 2011. Published 29 Oct 2012. https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4364.0.55.001Explanatory%20Notes602011-12?OpenDocument. Accessed 8 Jul 2020.
Goff DC, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. Circulation. 2014;129(25 Suppl 2):S49–73. https://doi.org/10.1161/01.cir.0000437741.48606.98.
Australian Institute of Health and Welfare. General Record of Incidence of Mortality (GRIM) data, General Record of Incidence of Mortality (GRIM) data. https://www.aihw.gov.au/reports/life-expectancy-deaths/grim-books/contents/general-record-of-incidence-of-mortality-grim-data. Accessed 30 Jun 2020.
Albarqouni L, Doust JA, Magliano D, Barr EL, Shaw JE, Glasziou PP. External validation and comparison of four cardiovascular risk prediction models with data from the Australian Diabetes, Obesity and Lifestyle study. Med J Aust. 2019;210(4):161–167. https://doi.org/10.5694/mja2.12061
Australian Institute of Health and Welfare 2019. Australian refined diagnosis-related groups (AR-DRG) data cubes, Data cubes. https://www.aihw.gov.au/reports/hospitals/ar-drg-data-cubes/contents/data-cubes. Accessed 30 Jun 2020.
Australian Institute of Health and Welfare 2019. Health Expenditure Australia 2017-18. Australian Government; 2019. https://doi.org/10.25816/5ec5ba12ed174
van den Hout WB. The value of productivity: human-capital versus friction-cost method. Ann Rheum Dis. 2010;69:i89. http://dx.doi.org.ezproxy.lib.monash.edu.au/https://doi.org/10.1136/ard.2009.117150
Worcester MU, Elliott PC, Turner A, et al. Resumption of work after acute coronary syndrome or coronary artery bypass graft surgery. Heart Lung Circ. 2014;23(5):444–53. https://doi.org/10.1016/j.hlc.2013.10.093.
Vyas MV, Hackam DG, Silver FL, Laporte A, Kapral MK. Lost productivity in stroke survivors: an econometrics analysis. Neuroepidemiology. 2016;47(3–4):164–70. https://doi.org/10.1159/000454730.
Australian Bureau of Statistics. Average weekly earnings, Australia. Published 20 February 2020. https://www.abs.gov.au/ausstats/abs@.nsf/mf/6302.0. Accessed 2 Jul 2020.
Australian Bureau of Statistic. Labour Force, Australia, May 2020. Published 18 June 2020. https://www.abs.gov.au/ausstats/abs@.nsf/mf/6202.0. Accessed 14 Jul 2020.
McCaffrey N, Kaambwa B, Currow DC, Ratcliffe J. Health-related quality of life measured using the EQ-5D–5L: South Australian population norms. Health Qual Life Outcomes. 2016;14(1):133. https://doi.org/10.1186/s12955-016-0537-0.
Lewis EF, Li Y, Pfeffer MA, et al. Impact of Cardiovascular events on change in quality of life and utilities in patients after myocardial infarction: A VALIANT Study (Valsartan In Acute Myocardial Infarction). JACC: Heart Failure. 2014;2(2):159-165. https://doi.org/10.1016/j.jchf.2013.12.003
Ali M, MacIsaac R, Quinn TJ, et al. Dependency and health utilities in stroke: data to inform cost-effectiveness analyses. Eur Stroke J. 2017;2(1):70–6. https://doi.org/10.1177/2396987316683780.
Pockett RD, McEwan P, Ray J, et al. Prospective utility study of patients with multiple cardiovascular events. J Med Econ. 2018;21(6):616–21. https://doi.org/10.1080/13696998.2018.1454453.
Marquina C, Talic S, Vargas-Torres S, et al. Future burden of cardiovascular disease in Australia: impact on health and economic outcomes between 2020 and 2029. Eur. J. Prevent. Cardiol. 2021:zwab001. https://doi.org/10.1093/eurjpc/zwab001
Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2006.
Schulz AJ, Israel BA, Mentz GB, et al. Effectiveness of a walking group intervention to promote physical activity and cardiovascular health in predominantly non-Hispanic Black and Hispanic urban neighborhoods: findings from the Walk Your Heart to Health Intervention. Health Educ Behav. 2015;42(3):380–92. https://doi.org/10.1177/1090198114560015.
Paige E, Welsh J, Agostino J, Calabria B, Banks E, Korda RJ. Socioeconomic variation in absolute cardiovascular disease risk and treatment in the Australian population. Prev Med. 2018;114:217–22. https://doi.org/10.1016/j.ypmed.2018.07.011.
Kavanagh A, Bentley RJ, Turrell G, Shaw J, Dunstan D, Subramanian SV. Socioeconomic position, gender, health behaviours and biomarkers of cardiovascular disease and diabetes. Soc Sci Med. 2010;71(6):1150–60. https://doi.org/10.1016/j.socscimed.2010.05.038.
Smurthwaite K. Using geographical convergence of obesity, cardiovascular disease, and type 2 diabetes at the neighborhood level to inform policy and practice. Prev Chronic Dis. 2017;14:E91. https://doi.org/10.5888/pcd14.170170.
Australian Institute of Health and Welfare. Indicators of Socioeconomic Inequalities in Cardiovascular Disease, Diabetes and Chronic Kidney Disease 2019. Canberra, ACT: https://www.aihw.gov.au/reports/chronic-disease/indicators-of-socioeconomic-inequalities-in-cardio/contents/summary. Accessed 8 Jul 2020.
Marchese L, Livingstone MK, Woods JL, Wingrove K, Machado P. Ultra-processed food consumption, socio-demographics and diet quality in Australian adults. Public Health Nutrition. Cambridge Core. Public Health Nutrition. Epub 12 Sep 2021. https://doi.org/10.1017/S1368980021003967
Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes. Circulation. 2018;137(20):2166–78. https://doi.org/10.1161/CIRCULATIONAHA.117.029652.
Sadana R, Blas E. What can public health programs do to improve health equity? Public Health Rep. 2013;128(Suppl 3):12–20.
Brown AF, Ma GX, Miranda J, et al. Structural interventions to reduce and eliminate health disparities. Am J Public Health. 2019;109(Suppl 1):S72–8. https://doi.org/10.2105/AJPH.2018.304844.
Cookson R, Griffin S, Norheim OF, Culyer AJ, Chalkidou K. Distributional cost-effectiveness analysis comes of age. Value Health. 2021;24(1):118–20. https://doi.org/10.1016/j.jval.2020.10.001.
Carter HE, Schofield D, Shrestha R. Productivity costs of cardiovascular disease mortality across disease types and socioeconomic groups. Open Heart. 2019;6(1):e000939. https://doi.org/10.1136/openhrt-2018-000939.
Jacobs J, Peterson KL, Allender S, Alston LV, Nichols M. Regional variation in cardiovascular mortality in Australia 2009–2012: the impact of remoteness and socioeconomic status. Aust N Z J Public Health. 2018;42(5):467–73. https://doi.org/10.1111/1753-6405.12807.
Morton JI, Ilomӓki J, Magliano DJ, Shaw JE. The association of socioeconomic disadvantage and remoteness with receipt of type 2 diabetes medications in Australia: a nationwide registry study. Diabetologia. 2021;64(2):349–60. https://doi.org/10.1007/s00125-020-05304-3.
Yadlowsky S, Hayward RA, Sussman JB, McClelland RL, Min YI, Basu S. Clinical implications of revised pooled cohort equations for estimating atherosclerotic cardiovascular disease risk. Ann Intern Med. 2018;169(1):20–9. https://doi.org/10.7326/M17-3011.
Filc D, Davidovich N, Novack L, Balicer RD. Is socioeconomic status associated with utilization of health care services in a single-payer universal health care system? Int J Equity Health. 2014;13(1):115. https://doi.org/10.1186/s12939-014-0115-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data availability statement
The model is available upon request or through the Open Science Framework data repository (https://osf.io/t3ue8/?view_only=af2cc3ae25044b55a7323fb3f67ab13d).
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Kaitlyn Hastings, Clara Marquina, Jedidiah Morton, Danielle Berkovic, Stella Talic and Zanfina Ademi have no conflicts of interest to declare. Ella Zomer declares grants from Amgen, AstraZeneca, Pfizer and Shire, outside the submitted work. Danny Liew declares previous grants, participation in advisory boards and/or receipt of honoraria from Abbvie, Amgen, Astellas, AstraZeneza, Bristol-Myers Squibb, Edwards Lifesciences, Novartis, Pfizer, Sanofi and Shire, outside the submitted work.
Author contributions
KH contributed to the interpretation of the data and wrote the first draft of the manuscript; CM designed the model, performed the analysis, contributed to the analysis and interpretation of the data and wrote the first draft of the manuscript; JM and EZ contributed to the interpretation of the data and editing of the manuscript; ST, DB and DA contributed to the editing of the manuscript; DL contributed to the conceptualisation of the project and editing of the manuscript; and ZA contributed to design of the model, conceptualisation of the project, interpretation of the data, and editing and revision of the manuscript, and supervised the whole project.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hastings, K., Marquina, C., Morton, J. et al. Projected New-Onset Cardiovascular Disease by Socioeconomic Group in Australia. PharmacoEconomics 40, 449–460 (2022). https://doi.org/10.1007/s40273-021-01127-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-021-01127-1