Abstract
Inborn errors of metabolism (IEMs) are a group of genetic diseases that occur due to the either deficiency of an enzyme involved in a metabolic/biochemical pathway or other disturbances in the metabolic pathway including transport protein or activator protein deficiencies, cofactor deficiencies, organelle biogenesis, maturation or trafficking problems. These disorders are collectively significant due to their substantial impact on both the well-being and survival of affected individuals. In the quest for effective treatments, enzyme replacement therapy (ERT) has emerged as a viable strategy for patients with many of the lysosomal storage disorders (LSD) and enzyme substitution therapy in the rare form of the other inborn errors of metabolism including phenylketonuria and hypophosphatasia. However, a major challenge associated with enzyme infusion in patients with these disorders, mainly LSD, is the development of high antibody titres. Strategies focusing on immunomodulation have shown promise in inducing immune tolerance to ERT, leading to improved overall survival rates. The implementation of immunomodulation concurrent with ERT administration has also resulted in a decreased occurrence of IgG antibody development compared with cases treated solely with ERT. By incorporating the knowledge gained from current approaches and analysing the outcomes of immune tolerance induction (ITI) modalities from clinical and preclinical trials have demonstrated significant improvement in the efficacy of ERT. In this comprehensive review, the progress in ITI modalities is assessed, drawing insights from both clinical and preclinical trials. The focus is on evaluating the advancements in ITI within the context of IEM, specifically addressing LSDs managed through ERT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Enzyme replacement therapy may elicit immune reactions diminishing the therapeutic advantages and potentially compromising patient safety. |
Immune tolerance induction regimes have been used in patients as a prophylactic approach to forestall immune responses in enzyme-replacement-therapy-naïve patients, and as a therapeutic approach to diminish pre-existing antibodies in individuals undergoing enzyme replacement therapy with established immune response. |
It is crucial to identify individuals prone to immune responses, determine the regime and explore innovative immunomodulatory approaches that are antigen-specific and/or target antigens at a higher level to prevent or reverse immune responses. |
1 Introduction
Enzyme replacement therapy (ERT) is the primary treatment for various inborn errors of the metabolism, including lysosomal storage disorders (LSD), and has been used in other inborn errors of metabolism including phenylketonuria (enzyme substitution therapy) and hypophosphatasia (enzyme substitution therapy) recently (Table 1). Recombinant enzymes, derived from human fibroblasts, animal cell lines, or plant cells, are used for ERT [1].
It is crucial to acknowledge that not all patients who undergo ERT will experience immune responses, which can be influenced by factors such as properties of the replacement protein (immunogenicity, particle aggregation, impurities, dose, route of administration, treatment frequency, and structural similarities to antigens), and host-related issues (residual mutant protein, genetic background).
This review aims to overview a comprehensive examination of contemporary approaches in treating patients receiving ERT, delving into the most recent insights regarding immune responses and their effective management. Additionally, it explores the prospective implications for gene replacement therapies in the future treatment landscape.
A comprehensive systematic review encompassing publications on inborn errors of metabolism, including infantile onset Pompe disease (IOPD), Pompe disease, glycogen storage disease type 2, immune tolerance induction, immune modulation, immune response, anti-drug antibodies, enzyme replacement therapy, lysosomal storage diseases, Fabry disease, Gaucher disease, acid sphingomyelinase deficiency, Wolman disease, mucopolysaccharidosis, phenylketonuria, and hypophosphatasia, was conducted to search the immune tolerance induction (ITI). Case reports, guidelines, meta-analyses, clinical trials, randomised controlled trials, reviews, systematic reviews, and multicentre studies were meticulously selected through the PubMed bibliographic database and thoroughly examined.
2 The Mechanism of the Immune Response to Enzyme Replacement Therapy
ERT administration may induce an immune response in individual’s prior enzyme exposure due to the introduction of a structurally different protein, promoting immunogenicity. Key humoral mechanisms involve antigen-presenting cells (APCs) presenting ERT peptides to helper T cells, triggering B cell activation and leading to the production of antibodies, including short-lived IgM and long-lived IgG [2, 3]. The immune system can trigger hypersensitive reactions, such as infusion-associated reactions (IAR), to antigens. Another significant concern is the development of anti-drug antibodies (ADA) in response to enzyme therapy. The presence of residual endogenous enzymes, referred to as cross-reactive immunologic material (CRIM), can impact a patient’s likelihood of antibody generation against the therapeutic protein. CRIM status is extensively discussed in infantile onset Pompe Disease (IOPD) [4]. Although it has been suggested that CRIM-positive patients with residual enzyme activity have lower antibody titres and respond better to ERT, while CRIM-negative patients with severe mutations tend to have high and persistent antibody titres, leading to poor treatment outcomes [4, 5], Desai et al. reported there were no differences in the antibody titres between CRIM-negative and positive IOPD patients. Some CRIM-positive IOPD patients develop high and persistent antibody titres (HSAT; ≥ 51,200) or sustained intermediate titres (SIT; ≥ 12,800 and < 51,200), mirroring the pattern observed in CRIM-negative patients. Within the CRIM-positive IOPD cohort, 32% (12 out of 37) showed the emergence of HSAT/SIT, potentially limiting the response to ERT and impacting clinical outcomes [6]. Notably, it should be emphasised that the magnitude of antibody titres, irrespective of the patient group, did not show significant differences, and, consequently, both groups might experience impediments to the effectiveness of the therapeutic intervention.
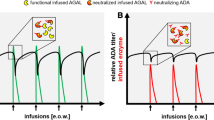
2.1 Anti-drug Antibodies in Patients Receiving ERT
There are primarily two major issues related to ADAs. The first issue is whether the existence of ADAs will give rise to any IARs, and the second concern is whether the presence of ADAs will lead to a reduced treatment effect, or negatively impact the patient’s therapy outcome.
The occurrence of IARs is often associated with the presence of ADAs. Patients with antibodies have a higher risk of experiencing IARs, including anaphylaxis. Immune-mediated IARs are more common in individuals with ADAs [7, 8].
In conditions such as haemophilia A and haemophilia B, allo-immune responses can lead to therapy failure due to antibodies against infused proteins [9]. Elevated antibody titres can hinder the effectiveness of ERT, ultimately impeding the therapeutic outcomes. It was revealed that the clinical outcome might be correlated with the level of the ADAs to ERT and ERT dosage [10]. Quantifying the levels of unbound ADAs revealed that titres could reach saturation during infusions [11]. Berrier et al. reported the HSAT could impede the effect of ERT. Among 20 CRIM-negative patients, 17 exhibited clinically significant IgG antibody titres against rhGAA. Among them, 13 patients developed HSAT with a median peak titre of 204,800 by the 24th week of ERT. Additionally, four patients had SIT with peak titres of 25,600 and 51,200, while three patients had low titres (LT) peaking at 200 (in two patients) and 800 (in 1 patient). Four patients initiated ERT before reaching 1 month of age, and their clinical outcomes varied. Two of these patients did not develop an immune response against rhGAA (patients 18 and 20), whereas the other two exhibited a poor response, leading to unfortunate outcomes with death (two patients) [12].
Mhanni et al. [13] and Hongo et al. [14] reported lack of ERT efficacy due to HSAT in Fabry patients who had markedly increased levels of globotriaosylsphingosine (Lyso-Gb3), which is a specific biomarker commonly used to monitor ERT response even under ERT. It was also suggested that HSAT in IOPD at or below 1:6250 likely did not hold clinical significance. In contrast, titres reaching 1:31,250 and beyond might potentially undermine the effectiveness of ERT at a dosage of 20 mg/kg, and titres exceeding 1:60,000 could be anticipated to interfere with ERT when administered at a dosage of 40 mg/kg [15]. Long-term studies in attenuated mucopolysaccharidosis I (MPS I) patients have shown a gradual decline in ADA levels over time, with some patients even becoming seronegative, indicating the development of natural immune tolerance with prolonged laronidase therapy [16, 17].
3 Immune Tolerance Induction in Enzyme Replacement Therapy
Immune tolerance induction (ITI) is an effective approach to address immunogenicity in ERT. ITI promotes immunological tolerance by exposing the immune system to the therapeutic enzyme. T cells play a crucial role in initiating immune responses, and B cell responses, including antibody production, depend on T cell assistance. Tolerance induction involves balancing the elimination or deactivation of antigen-reactive cells and the emergence of regulatory cells. “Natural” regulatory T cells (nTregs) and induced Tregs (iTregs) play crucial roles in suppressing immune responses against self-antigens. nTregs are autoreactive T cells that circulate in the peripheral immune system, while iTregs are derived from circulating T effector cells. Both types of Tregs contribute to tolerance induction and the prevention of autoimmunity and inflammation [18].
There are three categories of ITI: antigen-specific, antigen non-specific, and delivery of negative/regulatory signals. Antigen-specific therapy involves delivering an antigen in a tolerogenic form, while antigen non-specific therapy blocks signals necessary for immune responses. Regulatory signals can inhibit immune responses, such as using Tregs. Tregs are CD4 T cells expressing forkhead box p3 (Foxp3), CD25, and low CD127 levels, playing an essential role in self-tolerance. Atypical Tregs, lacking Foxp3 expression, also possess immunosuppressive functions through cytokine production [18, 19].
Tregs induced by IVIG treatment exhibit antigen specificity [20] and intravenous immunoglobulin (IVIG) has been shown to trigger the production of natural Tregs [21]. The binding of immunoglobulins to surface receptors involved in antigen processing pathways can induce Tregs [22]. T regulatory cell epitopes (Tregitopes) derived from IgG antibodies have been proposed as an alternative to IVIG. These conserved peptides can bind to major histocompatibility complex class II molecules and activate natural regulatory T cells [23, 24].
Most of the research on ITI has been conducted in patients with IOPD.
Most cases with IOPD have been identified as CRIM-positive [12]. Optimal immune modulation involves identifying suitable candidates prior to treatment, enabling ITI alongside ERT. CRIM-negative patients lack functional GAA enzymes, placing them at high risk for developing ADA. Treating patients in the treatment-naïve stage aims to prevent IARs and the production of HSAT following ERT [25]. Patients classified as CRIM-positive exhibit a lower susceptibility to antibody development, with only 32% reported to develop antibodies, in contrast to CRIM-negative patients, where 85% are documented to develop antibodies. Consequently, the a priori risk of antibody development is reduced in CRIM-positive individuals.
3.1 Different Protocols of Immune Tolerance Induction
There are three approaches for immune modulation of patients treated with enzymes. The optimal condition for immune modulation arises when clinicians can identify suitable candidates before initiating ERT, specifically those who are treatment naïve. This allows for the implementation of ITI concurrently with ERT. This strategy is considered advantageous in preventing the development of HSAT, thereby enhancing the efficacy of the overall treatment process.
In the second approach, clinicians may identify patients at risk of developing an immune response after an early exposure to ERT. In such cases, timely intervention with immune modulation is initiated before the manifestation of HSAT. This proactive approach aims to mitigate the potential immunogenicity associated with ERT and to optimise treatment outcomes.
The third approach involves patients who have already developed HSAT, indicated by antibody titres equal to or exceeding 51,200 at two or more instances, typically occurring at or beyond 6 months of ERT. In this scenario, clinicians may implement immune modulation strategies to address the established immune response and work towards restoring the efficacy of ERT.
Different agents have been used in ITI in patients receiving ERT (Table 2).
3.2 Prophylactic ITI
Prophylactic immunomodulation induction is given to patients alongside ERT to prevent rhGAA antibody.
3.2.1 Transient Low-Dose Methotrexate (TLD-MTX)
Methotrexate (MTX) inhibits the Janus kinase/signal transducer and activator of transcription proteins (JAK/STAT) pathway, essential for immune and inflammatory responses. It reduces immune cell proliferation, including T and B cells, and suppresses pro-inflammatory cytokines. MTX also increases adenosine production, known for its anti-inflammatory properties [26]. TLD-MTX was used for prophylactic and therapeutic use.
Subcutaneous or oral TLD-MTX (0.4 mg/kg) for three cycles alongside rhGAA infusions was administered to 14 IOPD patients. A total of 14 patients were included in the study as TLD-MTX and compared with the 37 CRIM-positive patients who received ERT monotherapy. Among the 14 TLD-MTX recipients (13 CRIM-positive patients and 1 CRIM-negative patients), the median last titre was 150 at a median rhGAA duration of approximately 83 weeks. Only one patient exhibited antibodies within the HSAT range, while another patient had antibodies within the SIT range. In contrast, all other recipients of methotrexate maintained a long-term status, distinguishing them from the responses observed in the ERT monotherapy group who had not received MTX. Among the cohort of 37 IOPD ERT monotherapy patients, in total, 32.4% of the patients developed either SIT or HSAT [27]. Furthermore, in classic infantile patients, the likelihood of antibody formation is established to be influenced by CRIM status, wherein 85% of CRIM-negative patients develop high sustained antibody titres (HSAT), in contrast to 32% of CRIM-positive patients [6, 12]. Consequently, the a priori risk of antibody development is reduced in CRIM-positive individuals. Although the findings suggest that TLD-MTX administration may sustainably reduce anti-rhGAA IgG titres in CRIM-positive IOPD patients [27], TLD-MTX does not completely prevent antibody formation. In the study, the effectiveness of TLD-MTX in CRIM-negative patients was limited due to the presence of one CRIM-negative patient. Further studies with larger cohorts are needed to evaluate the effectiveness of the TLD-MTX either in the CRIM-positive patients and CRIM-negative patients.
A study with TLD-MTX in three individuals with mucopolysaccharidosis I (MPS I) revealed treatment with MTX did not significantly reduce anti-laronidase IgG titres, which remained above the clinically relevant threshold of 1:4000. Antibodies were detected in all participants by week 4, and a relative reduction in titres was observed after hematopoietic stem cell transplantation [28].
3.2.2 Rituximab, Methotrexate and/or IVIG
Rituximab is a monoclonal antibody targeting human CD20, composed of a chimeric mouse–human structure. It binds to CD20, present on various stages of B-cell development, leading to B-cell depletion through antibody-dependent cellular cytotoxicity and complement-dependent cytotoxicity [29]. IVIG is used in ITI to target immune cells and reduce sustained antibody production [30]. IVIG’s immunomodulatory properties at higher doses help deplete B cells and provide passive immunity. However, administering IVIG before rituximab may decrease rituximab’s efficacy due to saturation of neonatal Fc receptors (FcRn) [31]. These drugs were given both as prophylactic and therapeutic management of immunomodulation.
A safety study on 19 CRIM-negative IOPD patients who received prophylactic immunomodulation was conducted with rituximab, MTX, and intravenous immunoglobulin (IVIG) over a period of 285 weeks [32]. MTX (0.4 mg/kg/dose) in three cycles, with each cycle comprising three doses, resulting in a total of nine doses being administered. In contrast, Poelman et al. [33] employed a dosing regimen which involved weekly MTX at a dosage of 1 mg/kg per dose with 40 mg/kg/week ERT. Most patients (15 out of 19) did not reach high IgG antibody titres, while three patients maintained intermediate titres and one achieved HSAT. Most patients experienced B-cell recovery, except for one who continued rituximab treatment [32]. The patients reported by Poelman et al. [33] exhibited different IgG antibody titres: 800,000, 6250, and 200,000. Following discontinuation of rituximab, all three patients showed B-cell recovery, but their IgG antibody titres increased afterwards. However, it is worth noting that all patients remained alive and capable of walking at the conclusion of the study, which might be attributed to the use of a weekly ERT dosage of 40 mg/kg/week. This highlights that, even in the presence of HSAT, ERT could still yield positive clinical outcomes.
Desai et al. [34] conducted a retrospective study on IOPD patients who underwent a short-term ITI therapy. The therapy included rituximab, MTX, and IVIG given over a 5-week period to a total of 34 patients of whom 25 were CRIM negative and 9 were CRIM positive. Among 25 patients, 17 patients were from the study that Kazi et al. reported [32].
In a recent study, 30 CRIM-negative patients received ERT and ITI with rituximab, MTX and IVIG prophylactically. Patients were evaluated according to the initiation of ERT period as an early treatment group (ETG; five patients; ≤ 4 weeks), an intermediate treatment group (ITG; seven patients; > 4 and ≤ 15 weeks), and a late treatment group (LTG; eight patients; > 15 weeks). All of the five patients in the ETG group maintained immune tolerance to ERT with a median follow-up duration of 31 weeks. Among the seven patients in the ITG group, five patients remained immune tolerant to ERT, with four of them continuing to be seronegative and one patient maintaining long-term tolerance. In the LTG group, all patients remained immune tolerant to ERT, with two patients remaining seronegative and six patients maintaining long-term tolerance. None of the patients experienced adverse events related to ITI [35].
A female MPS II patient with a severe phenotype who might exhibit susceptibility to developing elevated and persistent ADA against idursulfase, posing a significant risk that could impede the efficacy of ERT administered an ITI protocol. Rituximab was administered intravenously at a dose of 375 mg/m2 per week for a duration of 4 weeks (total four doses). MTX was administered at a dose of 0.4 mg/kg three times weekly for 3 weeks enterally, amounting to a total of nine doses. IVIG was administered at a dose of 500 mg/kg IV once weekly, for four doses, followed by monthly administrations for a period of 6 months until B-cell/plasma cell recovery was achieved. No significant adverse effects were observed, and after 2.5 years, the patient showed reduced urinary glycosaminoglycan levels and low ADA titres [36].
Rituximab and MTX were used for immune modulation in 9 IOPD patients (8 CRIM-negative, 1 CRIM-positive) among 33 IOPD patients. The regimen included rituximab (375 mg/m2 IV) and MTX [0.4 mg/kg subcutaneously (SC)]. It was observed that only one patient developed anti-IgG antibodies reaching a peak titre of 12,800 when he was 14 months old. Patients received 1 dose of rituximab and 10 doses of MTX. The duration of follow-up was between 6 months to 24 months. Eight patients showed B cell recovery. One patient received ERT as 20 mg/kg every other week, 6 patients received ERT as 20 mg/kg/week for the first 3 months then 20/kg/week every other week, and two patients received ERT as 40 mg/kg/week [37]. It may be suggested that dose level may be an important determinant of the outcome in PD.
Messinger et al. reported that two CRIM-negative patients underwent prophylactic treatment with a brief regimen of rituximab and MTX which was initiated concurrently with rhGAA therapy [38]. The prophylactic ITI regime included rituximab 375 mg/m2/dose weekly for 4 weeks and MTX 0.4 mg/kg subcutaneously 3 times a week for 9–17 doses. One patient received IVIG only once. One patient developed ADA with a titre of 1:1600 but declined to 1:200 after 2 years on ERT without receiving additional ITI. These two patients gained developmental milestones and did not need ventilation support during follow-up, and cardiomyopathy improved. While the authors reported the effectiveness of ITI during a 24-month follow-up period, it should be noted that this duration may not have been sufficient to definitively assess its long-term effectiveness [38]. Although the use of rituximab, MTX and IVIG may show effect on the development of ADA during short course and B cell recovery, in the longer period of follow-up, the recurrence of ADAs is a challenge.
3.2.3 Cyclosporine and Azathioprine
The safety and effectiveness of an immunosuppressive regimen consisting of cyclosporine (CsA) and azathioprine (AzA) was conducted in treatment-naïve MPS I patients with severe symptoms caused by two nonsense mutations [39]. The study included six patients who received immunosuppression prior to laronidase treatment. The goal was to assess ITI based on ADA titres (≤ 3200) after 24 weeks of laronidase treatment. Two cohorts underwent ITI with cyclosporine, azathioprine and low-dose laronidase infusions for different durations. The results showed no evidence of immune tolerance in all three patients in cohort 1, while two out of three patients in cohort 2 received ITI. Patients with lower ADA titres demonstrated greater reductions in urinary glycosaminoglycan excretion [39].
Around 90% of MPS Type I patients develop IgG antibodies within a few months of starting laronidase treatment [40]. Severe MPS I patients with two null mutations are more prone to this response, and higher antibody levels are associated with less reduction in urinary glycosaminoglycans (uGAGs) [41]. There is a need for further studies to observe the effectiveness of the ITI consisting of cyclosporine and azathioprine. Although it might be a limitation in the view of the patients to give regular blood samples to the measurement of cyclosporine level, the safety is followed up by the measurement of cyclosporine level in the blood.
3.2.4 Rituximab, Corticosteroids, Sirolimus or Mycophenolate and IVIG
Mycophenolate inhibits T and B lymphocyte proliferation and reduces immune cell recruitment to inflammation sites. Mycophenolate also depletes tetrahydrobiopterin, decreasing nitric oxide production by inducing nitric oxide synthase. This is crucial as macrophages can generate nitric oxide and superoxide, which can form peroxynitrite and cause tissue damage [42].
In a study reported by Elder [43], infants with PD received methylprednisolone with rituximab and either sirolimus or mycophenolate before starting ERT. B-cell depletion and T-cell immunomodulation successfully eliminated immune responses against the therapeutic enzyme, resulting in improved clinical outcomes. However, the study noted that this approach did not necessarily impact the sustained ability of infants to be ventilator free. They emphasised that initiating immunomodulation before starting ERT was beneficial, as they stated that the ITI protocol was easy to use by allowing for prompt initiation of therapy.
3.3 Therapeutic ITI
Therapeutic use of immune modulation protocols aims to reduce and eliminate the pre-existing ADAs occurring after the administration of ERT.
3.3.1 Rituximab, Methotrexate and/or IVIG
Two patients who were CRIM-negative and had pre-existing anti-GAA antibodies (maximum 1:12,800) but declined during the course received therapeutic treatment involving rituximab, MTX and IVIG. The administration of rituximab consisted of a weekly dose of 375 mg/m2 for a duration of 4 weeks, followed by ongoing maintenance dosing. MTX was administered enterally at a weekly dosage of 0.5 mg/kg along with ERT (alglucosidase alfa 20 mg/kg every other week). Additionally, IVIG was administered every 4 weeks at a dose of 0.5 g/kg in only one patient. The combination of rituximab and MTX resulted in elimination (3 months and 19 months, respectively) of anti-rhGAA antibodies [38]. The patient who had ITI without IVIG was persistently antibody-negative. Two patients gained developmental milestones, having mild infection during follow-up and being ventilator free [38]. The method was previously administered in a CRIM-negative IOPD by Meldelsohn et al., and a maximum 1:1600 level of anti GAA antibody was observed but became negative after 3.5 months of ITI [44]. Markic et al. [45] achieved ITI in a CRIM-positive IOPD patient during ERT using rituximab, MTX and IVIG. This patient had to discontinue ERT due to severe IARs and tested positive for ADA of anti-rhGAA antibodies. Following ITI, cardiomyopathy steadily improved over a 3-year follow-up, despite the patient remaining ventilator dependent with no notable motor skill gains with no detectable antibodies and no adverse reactions associated with ITI.
3.3.2 High-Dose IVIG
IVIG exerts immunomodulatory effects by reducing autoantibodies, inhibiting T cell activation, blocking complement-mediated damage, suppressing inflammatory cytokine production, enhancing corticosteroid sensitivity, and regulating thromboxane A2, endothelin and prostacyclin [46, 47]. IVIG has been used as a part of ITI during prophylactic and therapeutic ITI regimes. In therapeutic ITI regimens high-dose IVIG was used.
Rairikar et al. introduced a new approach for immunomodulation in a CRIM-negative IOPD patient using high-dose IVIG as the primary treatment. The patient had an ineffective ITI regimen with rituximab, MTX and IVIG due to intolerability and infections. High-dose IVIG therapy (1 g/kg) was initiated alongside ERT, initially given weekly and later adjusted to bi-weekly doses. The patient showed clinical improvement with partial motor recovery and tolerated the treatment well with reduced IgG antibodies [48]. It might decrease the recurrence of infections and modulate immune response. Although this regime with only high-dose IVIG may reduce IgG antibodies, it may not lead to complete immune tolerance to ERT. There should be further studies with a large group of patients to evaluate the effectiveness of the high-dose IVIG either alone or with a combination of other therapies.
3.3.3 Bortezomib, Rituximab, Rapamycin and IVIG
Rapamycin inhibits mTORC1, disrupting immune cell signalling, proliferation, and antibody production [49]. It suppresses T-cell proliferation by reducing IL-2 production and affects dendritic cell function, leading to decreased antigen presentation and T-cell priming [50].
Bortezomib is a special proteasomal inhibitor. It has a major role in the suppression of NF-κB signalling leading to a reduction in the release of proinflammatory cytokines and the activity of type I interferons [50]. Its key function in the ITI after HSAT formation following ERT is to reduce in both short-lived and long-lived plasma cells.
In a study by Poelman et al. [51], a rapamycin-based immunomodulation protocol was used in three IOPD patients (two CRIM negative, one CRIM positive). The regimen included rituximab, bortezomib, monthly IVIG and rapamycin [three weekly infusions of RTX 375 mg/m2; six twice-weekly doses of bortezomib 1.3 mg/m2; monthly IVIG (first dose 1.0 g/kg; subsequent doses of 0.5 g/kg), rapamycin at week 4 (10–20 kg, 1.0–1.5 mg/day; 20–30 kg, 1.5–2.0 mg/day; double dose on first day of rapamycin)]. Among these three patients, only one had rituximab, MTX and IVIG dose prophylactically, and after HSAT occurrence, the patient received ITI with this protocol. Anti-rhGAA antibodies were detected in all patients, with varying titres over time. Secondary immunomodulation reduced antibody titres, eliminated infusion-associated reactions, but complete antibody elimination was not achieved. No severe infections were observed [51]. Despite the presence of high antibody titres, the overall outcome of the patients was good, with all individuals surviving, free from ventilator support, and able to walk (two patients) and with normal left ventricular mass index during a follow-up period extending up to 6.6 years. The favourable outcomes observed might be associated with the specific dose administered, set at 40 mg/kg per week in all patients. The outcome underscores that the ultimate result might be influenced by a combination of factors, including antibody titre and the prescribed dose levels [51]. As bortezomib is a special proteasome inhibitor that target both the long-lived and short-lived plasma cells producing antibodies, the combination of bortezomib with other immunomodulatory drugs have positive impact on providing effective ITI in patients who have high and sustained titres of antibody.
3.3.4 Bortezomib, Rituximab, Methotrexate and IVIG
Rituximab, MTX, IVIG and addition of bortezomib to rituximab-resistant HSAT protocol was administered to three patients experiencing severe clinical decline, with the highest observed IgG antibody titres of 204,800, 819,200, and 204,800 by Banugaria et al. [52]. Following multiple cycles of immunomodulation, monthly immunoglobulin (0.4–0.5 g/kg) or monthly immunglobulin (400–500 mg/kg), rituximab (375 mg/m2, IV for 4 weeks), bortezomib (1.3 mg/m2 weekly IV), and MTX (15 mg/m2 SC), all three patients demonstrated a substantial reduction in their IgG antibody titres, reaching 100, 6400, and 3200, respectively. The patients had clinical improvements with no immunosuppression-related infections. In a subsequent study by Kazi et al., it was noted that all three patients maintained low IgG antibody titres at 0, 1600, and 800, with full B cell recovery [53]. Among these patients, two had discontinued immunomodulating, with one patient continued to receive maintenance rituximab and methotrexate, with a significantly reduced frequency of rituximab. This patient had been off rituximab for 41 weeks at the end of the study. These two case reports revealed that the incorporation of bortezomib into the rituximab, MTX and IVIG regimen marked the first successful protocol in eliminating IgG antibodies in individuals with HSAT while achieving immune tolerance. The two patients had peak IgG titres of 819,000 and 102,400, and patients received the same dosage of bortezomib 1.3 mg/m2 weekly (subcutaneously for 4 weeks, folic acid 2.5 mg 6 days/week, weekly oral methotrexate 0.4–0.5 mg/kg and monthly immunoglobulin 0.4 mg/kg IV and rituximab 375 mg/m2 IV for 4 weeks); they did not show clinical improvement although ERT dosage increased and there was a reduction in anti-rhGAA antibody titres [54]. The noteworthy point in the reports might be the disease severity and the close monitoring of the anti-rhGAA antibody titre in the patients. Delayed initiation of immunomodulation therapy diminishes the effectiveness of ERT and may lead to irreversible changes in clinical status, reducing the window for enhancing clinical outcomes.
3.3.5 Plasma Exchange, Rituximab and IVIG
Plasma exchange, or plasmapheresis, is a procedure that removes and replaces plasma in the blood. It helps eliminate harmful substances such as antibodies, reducing the autoimmune response and promoting immune tolerance. Plasma exchange can reduce the levels of anti-GAA antibodies and immune complexes, which may contribute to the development of infusion-associated reactions [55, 56].
Plasma exchange and rituximab were combined in a CRIM-negative IOPD patient with severe IARs. After discontinuing ERT therapy, the patient received plasma exchange and a single dose of rituximab. Anti-recombinant human acid a-glucosidase levels significantly reduced, with enhanced response from rituximab. Deodato et al. [55] also found that a single administration of an immune modulator drug resulted in a faster and positive outcome. They speculated that the immediate response observed in the patient suggests plasma exchange’s potential effectiveness in low antibody titres.
In a CRIM-negative patient, despite the presence of HSAT, the attempt to reduce HSAT through treatment with plasmapheresis and other immune modulatory drugs including cyclophosphamide, rituximab, and an ERT dose of 10 mg/kg every day for 5 days/week showed increased antibody titres from 1:25,600 to 1:204,800 (weeks 78 through 99) with no motor development and no improvement in left ventricular mass index (56). Although plasma exchange was thought of as a potential treatment approach to reduce antibody titres in a faster way, it has no impact on the long-term low antibody titres in patients receiving ERT (Table 3 shows the approaches of the published reports; Table 4 shows the most commonly used prophylactic and therapeutic ITI regimes).
3.4 Preclinical Studies
3.4.1 Oral Tolerance Studies
3.4.1.1 As a Prophylactic ITI
Efforts are underway to develop new ITIs due to adverse effects of current drugs. Antigen-specific immunotherapy, such as peptide-based vaccines, engineered antigen-presenting cells or gene therapy, targets immune response against specific antigens. Oral tolerance induction aims to generate regulatory T cells, suppress immune reactions, and induce clonal energy or deletion. It offers safety and antigen specificity advantages. For instance, oral administration of rhGAA reduces anti-rhGAA antibody levels and induces immune tolerance, as demonstrated by Ohashi et al. in PD mouse models. Practical limitations were noted with high doses of rhGAA needed for immune suppression [57].
3.4.2 Non-depleting Anti-CD3 and Anti CD4 Antibodies
Antigen-targeted immunotherapy employs non-depleting anti-CD3 and anti-CD4 antibodies to target lymphocyte populations, down-regulating CD3 and CD4 receptors on T cells and modulating immune response. These antibodies facilitate the generation and activation of regulatory T-cells, crucial for immune tolerance [58, 59]. These mechanisms contribute to the immunomodulatory effects of non-depleting anti-CD4 antibodies in antigen-targeted therapies.
Therapeutic ITI In a study by Ohashi et al. [60] anti-CD3 antibody administration reduced anti-human GAA antibody levels in mice receiving the enzyme, resulting in lower increases in antibody titres compared with controls upon rhGAA challenge. It also decreased pre-existing antibodies and prevented lethal HSATs while reducing antibody titres in a mouse model of PD. Treatment with anti-CD3 antibodies led to a decrease in CD4+ and CD8+ cell numbers, suggesting their potential for inducing immune tolerance to ERT in PD.
In a comparative study, the control group exhibited high levels of anti-rhGAA antibodies, which remained consistently elevated over time. However, both the MTX group and the three-dose anti-CD4-monoclonal-antibody-treated groups showed significantly reduced levels of anti-rhGAA antibodies after 4 weeks of rhGAA treatment compared with the control group. The study demonstrated that a short-course treatment with non-depleting anti-CD4 monoclonal antibodies effectively induced long-term immune tolerance to ERT in PD mice [61].
3.4.3 Anti-CD4 and Anti-CD8 Monoclonal Antibodies
Different strategies to induce ITI and reduce anti-laronidase IgG antibodies were investigated in MPS I mice. They explored the use of MTX, non-depleting anti-CD4 monoclonal antibodies, non-depleting anti-CD8 monoclonal antibodies and combinations of these treatments. Mice received 10 weekly injections of laronidase and an immune system challenge on day 49. The efficacy of the treatments was compared by measuring anti-laronidase IgG antibody levels. All ERT-treated mice developed antibodies by day 28. The groups receiving monoclonal antibodies showed significantly lower antibody levels on day 70. Two courses of non-depleting anti-CD4 monoclonal antibodies successfully eliminated immune responses in seven out of eight MPS I mice, even after adjuvant stimulation. The study suggests that non-depleting anti-CD4 monoclonal antibodies hold promise for inducing ITI [28].
3.4.4 B-Cell Activating Factor (BAFF) Inhibition or Anti-B Lymphocyte Stimulator (antiBlyS) Antibody
B-cell-activating factor (BAFF) is a cytokine crucial for B cell survival and differentiation [62]. It supports transitional and mature B cells and regulates the maturation of low-affinity autoreactive cells. BAFF influences autoreactive B cell activation, clone selection, plasma cell survival and antibody production. Transgenic mice with high BLyS levels develop autoimmune-like symptoms [63].
BAFF, in conjunction with a proliferation-inducing ligand known as APRIL, plays a crucial role as the primary cytokines responsible for the survival and maturation of B cells. While their impact on T cell survival and functions is less precisely defined, BAFF serves as a vital survival factor, particularly in the maturation of follicular (FO) and marginal zone (MZ) B cells. The absence of BAFF results in inhibition of the maturation, differentiation and survival of B-lymphocytes and the arrest of B-cell maturation at the transitional stage (TR), a noteworthy point as TR B cells are susceptible to clonal deletion and lack responsiveness to T-cell help—essential for immune responses observed during ERT. In essence, BAFF impedes B-cell development at the transitional stages [64].
The Food and Drug Administration (FDA)-approved BAFF inhibitor has shown promising results in alleviating disease manifestations among patients with systemic lupus erythematosus (SLE) [65]. Its efficacy extends beyond clinical observations, as demonstrated in both clinical and murine models, further affirming its positive impact [66,67,68,69].
Infusion-associated reactions, including headache, arthralgia, nasopharyngitis, abdominal pain, nausea, cough, diarrhoea and fever, were more commonly observed in patients receiving BAFF inhibitors compared with placebo group [70, 71]. The psychiatric problems and suicide attempts were evaluated in the patients with SLE receiving BAFF inhibitors and one suicide attempt in the placebo group and one instance of suicidal ideation in the BAFF inhibitor group were observed. Cervical carcinoma was reported in one case receiving a BAFF inhibitor. Although nine patients receiving BAFF inhibitors had depression, six patients in the control group also had depression. The infection rate was found to be similar in both groups and attributed to steroid use [71]. It has been indicated that, in mouse models [72], belimumab may not have a discernible impact on circulating antibodies and may potentially contribute to the development of subtle autoimmune reactions and mild renal immunopathology. This suggests that BAFF might not exert an effect on the circulating antibodies and could be associated with the development of renal autoimmunity.
3.4.4.1 As a Prophylactic ITI
In a study by Doerfler et al. [64], inhibiting BAFF was investigated to prevent antibody formation in a mouse model of PD. They administered a BAFF-neutralising antibody along with GAA ERT to Gaa−/− mice. Anti-BAFF treatment delayed antibody production, increased GAA activity and protected against anaphylaxis. It also resolved antibody formation during an immune response and prevented migration of antibody-secreting cells to the bone marrow.
In a study by Sato et al. [73], ITI was achieved during ERT in a mouse model of FD using the anti-BlyS antibody belimumab. A single administration of belimumab temporarily reduced B cell proportion and IgG antibody levels against recombinant human GLA. By administering a low maintenance dose of belimumab, they achieved immune tolerance in 20% of the mice, although antibody formation could not be prevented. Increasing the maintenance dose of belimumab led to immune tolerance induction in 50% of the mice. The study also suggested that the high maintenance dose of belimumab improved the distribution and clearance of the target molecule, GL-3, in Fabry disease [73].
Although Doerfler [64] and Sato [73] suggested that the agent was safe, these studies were performed in animal models. It has been shown that BAFF inhibitors lead to some complications, including opportunistic infections and psychiatric problems and reduction in IG levels (IgG, IgM and IgA levels) in SLE adult patients [74]. Although BAFF shows promise as a target for rhGAA in IOPD patients, there is a need for studies to reveal effectiveness and safety of the drug as an immunomodulatory drug in patients either for prophylactic or therapeutic approaches.
3.4.5 Rapamycin-Carrying Nanoparticles
Recently the potential benefits of encapsulating rapamycin within nanoparticles (NP) have been investigated for enhanced uptake by antigen-presenting cells and induction of tolerogenic dendritic cells. In clinical trials [75, 76] of refractory gout patients regarding the effectiveness of the rapamycin-carrying NP, it was revealed that it reduced the serum urate levels and prevented ADA formation by the induction of tolerogenic dendritic cells toward the PEGylated uricase antigen [77]. Tolerogenic dendritic cells (DCs) play a role in promoting the generation of anergic (or regulatory) T cells, thereby reducing immunogenicity and extending the activity of PEGylated uricase.
3.4.5.1 As a Prophylactic ITI
In a study using GAA-KO mice undergoing ERT for PD, they compared NP-Rapa with MTX. Co-administration of NP-Rapa with rhGAA resulted in sustained suppression of anti-rhGAA antibodies, improved glycogen clearance in skeletal muscles and enhanced motor function compared with empty NP- or MTX-treated mice. The study suggests that NP-Rapa may have a longer-lasting immunosuppressive effect compared with MTX [78].
3.4.6 Red Blood Cell Based Study
3.4.6.1 As a Prophylactic ITI
Cremel et al. [79] reported a study in mice to demonstrate the immunological tolerance-inducing properties of red blood cells (RBCs) encapsulating the rh-GAA. Mice received intravenous injections of AGA-loaded RBCs and were sensitised to AGA using adjuvant molecules. Compared with control mice receiving free AGA, mice receiving AGA-loaded RBCs showed a significant reduction in the humoral response, even after three AGA stimulations with adjuvants. This specific immunomodulation persisted for at least 2 months without compromising the overall immune response. The delivery of antigens through RBCs demonstrated rapid and potent suppression of the humoral response against AGA within a week. The use of RBC therapy effectively maintained a tolerant state despite immune stimulations, resulting in a significant reduction in the presence of anti-AGA antibodies [79].
3.4.7 Phosphatidylserine-Based Study
3.4.7.1 As a Prophylactic ITI
Schneider et al. [80] demonstrated that liposomes containing phosphatidylserine (PS) can convert an immunogen into a tolerogen. PS, an immune regulatory molecule, exhibits tolerogenic activity when present on the outer leaflet of apoptotic cells. The study showed that rhGAA formed complexes with PS liposomes, and immunisation with PS-rhGAA resulted in a significant reduction in the antibody response against rhGAA. This reduced response persisted even upon re-challenge with free rhGAA [80]. The findings suggest that PS liposomes have the potential to induce tolerance toward therapeutic proteins, making them a valuable tool in immunotherapy.
3.4.8 Bortezomib with a Chaperone
3.4.8.1 As a Prophylactic ITI
The effects of bortezomib, a proteasome inhibitor, was investigated in combination with pharmacological chaperones (PCs) on mutant GAA function in PD. They found that bortezomib treatment improved GAA maturation and activity in patient fibroblasts carrying PC-responsive and PC-unresponsive mutations. The colocalisation of GAA with lysosomal markers also increased after bortezomib treatment. These results suggest that bortezomib, along with PC therapies, has the potential to enhance enzyme activity in specific PD patients. This approach shows promise for improving treatment outcomes in certain patient populations [81].
3.4.9 Mannose 6-Phosphate Conjugation Approach
3.4.9.1 As a Prophylactic ITI
Modification of N-linked carbohydrates with mannose 6-phosphate (M6P) facilitates the uptake of lysosomal enzymes through the high-affinity M6P receptor. ITI was achieved for rhGAA, which contains abundant M6P [82]. However, Vera et al. [83] investigated the induction of immune tolerance to phenylalanine ammonia-lyase in dogs with phenylketonuria using a recombinant form conjugated with M6P. Despite the stable binding and cellular uptake of the conjugated enzyme, dogs did not develop immune tolerance after the induction period. The combination of high-affinity cellular uptake, cyclosporin A, and azathioprine was insufficient to induce immune tolerance to the exogenous protein [83].
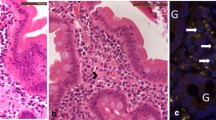
3.4.10 Gene Therapy
Adeno-associated viral vector (AAV)-mediated gene therapy has potential for treating genetic disorders by inducing immune tolerance. In PD mouse models, liver-specific transgene expression evaded immune responses. AAV2/8 vector with the CMV enhancer/beta-actin CB regulatory cassette triggered immune reactions, but an AAV2/1 vector with the cytomegalovirus promoter reduced anti-GAA antibodies and maintained transgene expression [84,85,86]. Liver-specific transgene expression is crucial for mitigating immune responses in PD. Early vector administration may enhance immune tolerance to GAA, highlighting the importance of early intervention. In Fabry mice, liver-specific AAV2 vector administration corrected biochemical abnormalities and induced immune tolerance to α-galactosidase [87]. Similarly, Niemann–Pick mice treated with an AAV2/8 vector containing a liver-specific promoter showed clearance of sphingomyelin accumulations and reduced hepatosplenomegaly and pulmonary inflammation, without antibody production against acid sphingomyelinase [88]. Co-administration of a liver-specific vector and CB promoter-containing vector enhanced efficacy in Niemann–Pick mice, potentially by preventing antibody formation and immune response [89].
In Gaucher disease mice, liver-specific AAV2/8 vector delivery of human glucocerebrosidase prevented glucosylceramide accumulations and Gaucher cell formation in multiple organs. Notably, the treated mice did not develop antibodies upon recombinant glucocerebrosidase challenge, unlike mock-treated mice [90]. Hinderer et al. [91] conducted a study using neonatally tolerant MPS I dog to investigate the intrathecal administration of an AAV9 vector carrying the human IDUA gene for treating MPS I-associated central nervous system symptoms. The dogs received an intravenous injection of AAV8 vector carrying the IDUA gene at 5 days old and an intrathecal injection of AAV9 vector at 1 month old. All animals showed a dose-dependent increase in cerebrospinal fluid IDUA activity, with consistent enzyme expression in the tolerised dogs throughout the 6-month study period. The tolerised animals exhibited significantly lower CSF antibody responses compared with naïve animals, with only two dogs showing detectable antibody titres approximately 20 times lower than those in naïve animals. One dog with the highest antibody titre displayed elevated CSF lymphocytes at day 21, albeit at lower levels than in naïve animals. No clinically significant adverse events were observed [91]. The administration of low-dose therapeutic enzymes targeted to the liver has shown potential in inducing tolerance mediated by Tregs. CD25+ T cells were found to be involved in immune tolerance to rhGAA in GAA-null mice, as depletion of CD25+ cells prevented the maintenance of immune tolerance to rhGAA [92]. Similarly, in Fabry disease mice, a liver-specific AAV2/8 vector induced tolerance to α-galactosidase, and transfer of splenocytes from vector-treated mice prevented the antibody response against α-galactosidase in recipient Fabry mice [87]. These findings collectively support the ability of liver-specific AAV vectors to induce immune tolerance to foreign proteins. The enhanced efficacy of AAV vectors in knockout mouse models relies on Treg-mediated immune tolerance through liver-restricted transgene expression.
Recent gene therapy study revealed the immunomodulatory effect of the ex vivo lentiviral gene (LVG) therapy in mice models. Lentiviral gene therapy to induce immune tolerance by varying the intervals (1, 6 and 12 weeks) between gene therapy and the initiation of ERT were investigated for chimerism and antibody formation in GAA−/− PD mice models. They observed that, although after a 12-week interval, ensuring complete hematopoietic reconstitution post-transplantation, antibody formation in response to ERT was observed. The study included two parts with high lentiviral vector dose (MOI of 20) and low subtherapeutic dose (MOI of 2). Gene therapy using lentivirus at MOI 20 prevented anti-rhGAA antibodies throughout the 10-week treatment (titres < 1:300). Even at a low dose (MOI = 2), anti-rhGAA antibodies were suppressed. It was suggested that HSPC-mediated LVG therapy induced immune tolerance at a subtherapeutic dose. To observe the effect of LVG therapy on anti-rhGAA antibodies, ERT after 1, 6 and 12 weeks of HSPC-mediated LVG therapy revealed that a 1-week interval resulted in lower anti-rhGAA antibody titres (1:3000) in LVG (MOI of 2)-treated mice compared with the 6-week and 12-week intervals (1:30,000), suggesting a potential mitigating effect of ERT when administered shortly after gene therapy. Extended ERT with 14 injections did not induce delayed immune responses, although mice without treatment with LV GAA died due to anaphylactic shock. While chimerism level was low compared with long internal periods, immune tolerance against rhGAA was achieved with a 1-week lead time for LVG therapy before ERT initiation. The benefit of HSPC-mediated LVG therapy for PD is its capacity to induce immune tolerance to the rhGAA protein. This not only facilitates supplemental treatment with ERT in cases where gene therapy may exhibit inadequate efficacy but also serves to prevent antibody formation. Consequently, it likely enhances the clinical response to treatment with either lentiviral gene therapy or ERT [93].
4 Discussion
A range of immunomodulation strategies including both prophylactic and therapeutic approaches have been utilised to establish tolerance to ERT in many LSDs. These immunomodulatory approaches have proven effective not only in preventing or reducing the harmful effects caused by the development of IgG ADAs. Administration of immunomodulation has shown a favourable safety profile obtained from clinical and preclinical studies. To give either prophylactic or therapeutic ITI is a challenging issue to concern. Although administration of prophylactic ITI mainly in CRIM-negative IOPD patients should be considered firstly, determination of CRIM status is sometimes a major concern and starting the treatment early is critical. Although CRIM status is determined by both western blot analysis or molecular analysis, the analysis takes time to reveal the CRIM status. Drawing insights from existing literature, it is evident that the overall effectiveness of current immunomodulation strategies is hindered by several unresolved factors. The immune-tolerising agents are used for the neutralising antibodies against the enzyme, and these are not long-lived drugs for neutralising the antibody during the life. After a period, the neutralising antibodies develop. There are further longer periods of studies to evaluate the effectiveness of the drug duration to enzymes. Bortezomib is used mostly in rheumatological diseases and has a positive effect on long-lived plasma cells by decreasing the titres of ADA with the combination of other immunomodulatory drugs in IOPD patients. The long-term effects of bortezomib as an ITI have not been known. The other unresolved question in immunomodulation protocols might be the need in different types of routes of enzymes. Up to now all protocols have been used for the intravenous route of the enzyme, and all the drugs have been given intravenously; it is not known in the central nervous system. The other question might be the need of immunomodulation for intrathecal or intracerebroventricular administration of enzymes. In tralesinidase alfa treatment study, ADAs against the tralesinidase alfa have been observed, and it was revealed that the serum concentration was higher than the cerebrospinal fluid (CSF) in the part 2 study for 48 weeks. Among the participants, three individuals did not exhibit any detectable ADAs in their serum, while six patients showed an absence of ADAs in CSF. Only three patients demonstrated ADA in CSF at both the 36th and 48th week [94].
While numerous products have demonstrated effectiveness as immune-tolerising agents, there is potential concern about the long-term safety of these agents, particularly in terms of immune suppression. Based on studies, a short course ITI regime (rituximab, IVIG and methotrexate) is safe and has few side effects including infection; some researchers suggested that risk of infection with ITI did not increase [95]. Furthermore, the other beneficial effect is the reduction in allergic reactions with the use of ITI. Notably, the treatment plan outlined by Kazi et al. has demonstrated the highest efficacy in establishing enduring immune tolerance without encountering prolonged toxicity related to the duration of immunosuppression or any hindrance in initiating ERT [32]. Patients subjected to this regimen have displayed immune tolerance, as indicated by the minimal or absent IgG antibody response, full recovery of B cells and without the requirement for continuous immunotherapy. One question is the need of prophylactic ITI in patients with some residual enzyme activity. Based on clinical studies, in the use of prophylactic ITI, there is lack of evidence in the patients with a mild form of the disease who have some residual enzyme activity.
Although the level of ADAs is not strictly correlated with the outcome of patients under ERT, measurement of ADAs during the disease is a suggested approach with the evaluation of clinical outcomes and specific biomarkers to determine the need of therapeutic ITI under ERT. Therapeutic ITI with rituximab, methotrexate and IVIG revealed mostly good and safe responses to therapeutic ITI with improvement in clinical outcome; in some cases, ADAs increased after the ITI regimes leading to clinical decline and to the need for other immunomodulatory drugs.
Most of the other drugs have been used in oncologic and autoinflammatory diseases, and long-term beneficial effects and risks are insufficient in many LSDs, mainly Fabry, Gaucher and MPSs.
The improvements in preclinical studies with new pharmaceutics, mainly gene therapy, will be promising approaches to overcome the development of ADAs and increase the effectiveness of the ERT.
Regarding other aspects of concern, individuals with elevated and sustained IgG levels may exhibit suboptimal responses to ERT, even without neutralising antibodies. Based on studies, the neutralising antibodies are affected by the antibody titres and ERT doses. It is postulated that administering a higher dosage, such as 40 mg/kg/week, may result in a greater availability of antibody-free ERT. Consequently, the neutralising effects of antibodies with a similar titre are anticipated to be less severe compared with patients receiving a lower dosage of 20 mg/kg every other week [96]. To illustrate, van Gelder et al. demonstrated through calculations that an ELISA titre of 1:156,250 could potentially bind up to 54% of the administered enzyme at a 20 mg/kg dosage [15]. Theoretically, under a 40 mg/kg dosage, a comparable binding amount might leave approximately 30 mg/kg accessible for uptake in target tissues [51, 83]. It might be concluded that high ERT dosage significantly enhances survival outcomes by allowing more than the standard dosage to reach target tissues. Consequently, additional research focusing on patients with positive antibodies is warranted.
Personalised medicine is the key point to determine the need of immunomodulation in patients receiving ERT. A recent report suggests that the development of ADAs to rhGAA may be influenced in CRIM-positive IOPD patients potentially linked to the patient’s HLA haplotype. An individualised prediction tool called “individualised T cell epitope measure (iTEM)” has been created; it is characterised by HLA haplotype and GAA pathogenic variants, with the specific T cell epitope composition of the rhGAA sequence [96]. This method could enable clinicians to identify CRIM-positive IOPD and late-onset Pompe patients at a heightened risk of developing HSAT or SIT and decide to administer ITI.
5 Conclusion
The effectiveness of current immunomodulation strategies is constrained due to limited knowledge of the pathological mechanisms, activation and signalling pathways, and affected cell types involved in the immune response to ERT. Future advancements in the identification of new signalling pathways or target cells are crucial for refining and enhancing the effectiveness and safety of future therapeutic approaches. The engineering of ERT to generate non-immunogenic epitopes without compromising effectiveness might also represent a strategic approach. This involves the modification of the therapeutic agent to elicit minimal immune response while preserving its intended efficacy.
Importantly, there is a pressing requirement for the development of innovative methods to induce immune tolerance, particularly through protocols that are specific to antigens and/or exhibit a higher degree of antigen targeting, which stands out as a distinctive approach. This diverges from the conventional use of systemically administered immunosuppressive agents, with the aim of enhancing both efficacy and safety in the induction of immune tolerance. Furthermore, it is imperative to deepen our understanding of the precise mechanisms underlying the development of immune tolerance in patients, especially concerning specific enzymes.
References
Ries M. Enzyme replacement therapy and beyond—in memoriam roscoe O. Brady, M.D. (1923–2016). J Inherit Metab Dis. 2017;40:343–56.
Brooks DA, Kakavanos R, Hopwood JJ. Significance of immune response to enzyme-replacement therapy for patients with a lysosomal storage disorder. Trends Mol Med. 2003;9(10):450–3. https://doi.org/10.1016/j.molmed.2003.08.004.
Banugaria SG, Prater SN, Ng YK, et al. The impact of antibodies on clinical outcomes in diseases treated with therapeutic protein: lessons learned from infantile Pompe disease. Genet Med. 2011;13(8):729–36. https://doi.org/10.1097/GIM.0b013e3182174703.
Kishnani PS, Goldenberg PC, DeArmey SL, et al. Cross-reactive immunologic material status affects treatment outcomes in Pompe disease infants. Mol Genet Metab. 2010;99(1):26–33. https://doi.org/10.1016/j.ymgme.2009.08.003.
Broomfeld A, Jones SA, Hughes SM, et al. The impact of the immune system on the safety and efficiency of enzyme replacement therapy in lysosomal storage disorders. J Inherit Metab Dis. 2016;39(4):499–512.
Desai AK, Kazi ZB, Bali DS, et al. Characterization of immune response in cross-reactive immunological material (CRIM)-positive infantile Pompe disease patients treated with enzyme replacement therapy. Mol Genet Metab Rep. 2019;10(20): 100475. https://doi.org/10.1016/j.ymgmr.2019.100475.
Barbier AJ, Bielefeld B, Whiteman DA, et al. The relationship between anti-idursulfase antibody status and safety and efficacy outcomes in attenuated mucopolysaccharidosis II patients aged 5 years and older treated with intravenous idursulfase. Mol Genet Metab. 2013;110(3):303–10. https://doi.org/10.1016/j.ymgme.2013.08.002.
Emecen Sanli M, Ertoy Karagol HI, Kilic A, et al. First successful concomitant therapy of immune tolerance induction therapy and desensitization in a CRIM-negative infantile Pompe patient. J Pediatr Endocrinol Metab. 2021;35(2):273–7. https://doi.org/10.1515/jpem-2021-0133.
Howard TE, Yanover C, Mahlangu J, et al. Haemophilia management: time to get personal? Haemophilia. 2011;17(5):721–8. https://doi.org/10.1111/j.1365-2516.2011.02517.x.
Lenders M, Neußer LP, Rudnicki M, et al. Dose-dependent effect of enzyme replacement therapy on neutralizing antidrug antibody titers and clinical outcome in patients with Fabry disease. J Am Soc Nephrol. 2018;29:2879–89.
Lenders M, Schmitz B, Brand SM, et al. Characterization of drug-neutralizing antibodies in patients with Fabry disease during infusion. J Allergy Clin Immunol. 2018;141:2289-92.e7.
Berrier KL, Kazi ZB, Prater SN, et al. CRIM-negative infantile Pompe disease: characterization of immune responses in patients treated with ERT monotherapy. Genet Med. 2015;17(11):912–8. https://doi.org/10.1038/gim.2015.6. (Erratum in: Genet Med. 2015 Jul;17(7):596. Rosenburg, Amy S [corrected to Rosenberg, Amy S]. PMID: Messinger 25741864; PMCID: PMC4561024).
Mhanni AA, Auray-Blais C, Boutin M, et al. Therapeutic challenges in two adolescent male patients with Fabry disease and high antibody titres. Mol Genet Metab Rep. 2020;24(24): 100618. https://doi.org/10.1016/j.ymgmr.2020.100618.
Hongo K, Harada T, Fukuro E, et al. Massive accumulation of globotriaosylceramide in various tissues from a Fabry patient with a high antibody titer against alpha-galactosidase A after 6 years of enzyme replacement therapy. Mol Genet Metab Rep. 2020;16(24): 100623. https://doi.org/10.1016/j.ymgmr.2020.100623.
van Gelder CM, Hoogeveen-Westerveld M, Kroos MA, et al. Enzyme therapy and immune response in relation to CRIM status: the Dutch experience in classic infantile Pompe disease. J Inherit Metab Dis. 2015;38(2):305–14. https://doi.org/10.1007/s10545-014-9707-6.
Kakavanos R, Turner CT, Hopwood JJ, et al. Immune tolerance after long-term enzyme-replacement therapy among patients who have mucopolysaccharidosis I. Lancet. 2003;361(9369):1608–13. https://doi.org/10.1016/S0140-6736(03)13311-9.
Clarke LA, Wraith JE, Beck M, et al. Long-term efficacy and safety of laronidase in the treatment of mucopolysaccharidosis I. Pediatrics. 2009;123(1):229–40.
Sakaguchi S, Mikami N, Wing JB, et al. Regulatory T cells and human disease. Annu Rev Immunol. 2020;26(38):541–66. https://doi.org/10.1146/annurev-immunol-042718-041717.
Shevach EM. From vanilla to 28 flavors: multiple varieties of T regulatory cells. Immunity. 2006;25(2):195–201. https://doi.org/10.1016/j.immuni.2006.08.003.
Massoud AH, Kaufman GN, Xue D, et al. Peripherally generated Foxp3 + regulatory T cells mediate the immunomodulatory effects of IVIg in allergic airways disease. J Immunol. 2017;198:2760–71. https://doi.org/10.4049/jimmunol.1502361.
Ephrem A, Chamat S, Miquel C, et al. Expansion of CD4+CD25+ regulatory T cells by intravenous immunoglobulin: a critical factor in controlling experimental autoimmune encephalomyelitis. Blood. 2008;111:715–22. https://doi.org/10.1182/blood2007-03-079947.
Anthony RM, Wermeling F, Karlsson MC, et al. Identification of a receptor required for the antiinflammatory activity of IVIG. Proc Natl Acad Sci USA. 2008;105:19571–8. https://doi.org/10.1073/pnas.0810163105.
De Groot AS, Moise L, McMurry JA, et al. Activation of natural regulatory T cells by IgG Fc–derived peptide “Tregitopes.” Blood. 2008;112:3303–11. https://doi.org/10.1182/blood-2008-02-138073.
De Groot AS, Cousens L, Mingozzi F, et al. Tregitope peptides: the active pharmaceutical ingredient of IVIG? Clin Dev Immunol. 2013;2013:1–6. https://doi.org/10.1155/2013/493138.
Bali DS, Goldstein JL, Banugaria S, et al. Predicting cross-reactive immunological material (CRIM) status in Pompe disease using GAA mutations: lessons learned from 10 years of clinical laboratory testing experience. Am J Med Genet C Semin Med Genet. 2012;160C(1):40–9. https://doi.org/10.1002/ajmg.c.31319.
Alqarni AM, Zeidler MP. How does methotrexate work? Biochem Soc Trans. 2020;48(2):559–67. https://doi.org/10.1042/BST20190803.
Kazi ZB, Desai AK, Troxler RB, et al. An immune tolerance approach using transient low-dose methotrexate in the ERT-naïve setting of patients treated with a therapeutic protein: experience in infantile-onset Pompe disease. Genet Med. 2019;21(4):887–95. https://doi.org/10.1038/s41436-018-0270-7.
Ghosh A, Liao A, O’Leary C, et al. Strategies for the induction of immune tolerance to enzyme replacement therapy in mucopolysaccharidosis Type I. Mol Ther Methods Clin Dev. 2019;2(13):321–33. https://doi.org/10.1016/j.omtm.2019.02.007.
Reff ME, Carner K, Chambers KS, et al. Depletion of B cells in vivo by a chimeric mouse human monoclonal antibody to CD20. Blood. 1994;83(2):435–45.
Schwab I, Nimmerjahn F. Intravenous immunoglobulin therapy: how does IgG modulate the immune system? Nat Rev Immunol. 2013;13(3):176–89. https://doi.org/10.1038/nri3401.
Liu J. Pharmacokinetics of monoclonal antibodies and Fc-fusion proteins. Protein Cell. 2017;9:603–18. https://doi.org/10.1007/s13238-017-0370-6.
Kazi ZB, Desai AK, Berrier KL, et al. Sustained immune tolerance induction in enzyme replacement therapy-treated CRIM-negative patients with infantile Pompe disease. JCI Insight. 2017;2(16): e94328. https://doi.org/10.1172/jci.insight.94328.
Poelman E, Hoogeveen-Westerveld M, Kroos-de Haan MA, et al. High sustained antibody titers in patients with classic infantile pompe disease following immunomodulation at start of enzyme replacement therapy. J Pediatr. 2018;195:236-243.e3. https://doi.org/10.1016/j.jpeds.2017.11.046.
Desai AK, Baloh CH, Sleasman JW, et al. Benefits of prophylactic short-course immune tolerance induction in patients with infantile Pompe disease: demonstration of long-term safety and efficacy in an expanded cohort. Front Immunol. 2020;6(11):1727. https://doi.org/10.3389/fimmu.2020.01727.
Li C, Desai AK, Gupta P, et al. Transforming the clinical outcome in CRIM-negative infantile Pompe disease identified via newborn screening: the benefits of early treatment with enzyme replacement therapy and immune tolerance induction. Genet Med. 2021;23(5):845–55. https://doi.org/10.1038/s41436-020-01080-y.
Julien DC, Woolgar K, Pollard L, et al. Immune modulation for enzyme replacement therapy in a female patient with Hunter syndrome. Front Immunol. 2020;21(11):1000. https://doi.org/10.3389/fimmu.2020.01000.
Broomfield A, Fletcher J, Davison J, et al. Response of 33 UK patients with infantile-onset Pompe disease to enzyme replacement therapy. J Inherit Metab Dis. 2016;39:261–71.
Messinger YH, Mendelsohn NJ, Rhead W, et al. Successful immune tolerance induction to enzyme replacement therapy in CRIM-negative infantile Pompe disease. Genet Med. 2012;14(1):135–42. https://doi.org/10.1038/gim.2011.4.
Giugliani R, Vieira TA, Carvalho CG, et al. Immune tolerance induction for laronidase treatment in mucopolysaccharidosis I. Mol Genet Metab Rep. 2017;13(10):61–6. https://doi.org/10.1016/j.ymgmr.2017.01.004.
Wraith JE, Clarke LA, Beck M, et al. Enzyme replacement therapy for mucopolysaccharidosis I: a randomized, double-blinded, placebo-controlled, multinational study of recombinant human alpha-l-iduronidase (laronidase). J Pediatr. 2004;144(5):581–8. https://doi.org/10.1016/j.jpeds.2004.01.046.
Wraith JE, Beck M, Lane R, et al. Enzyme replacement therapy in patients who have mucopolysaccharidosis I and are younger than 5 years: results of a multinational study of recombinant human alpha-l-iduronidase (laronidase). Pediatrics. 2007;120(1):e37-46. https://doi.org/10.1542/peds.2006-2156.
Allison AC. Mechanisms of action of mycophenolate mofetil. Lupus. 2005;14(Suppl 1):s2-8. https://doi.org/10.1191/0961203305lu2109oa. (PMID: 15803924).
Elder ME, Nayak S, Collins SW, et al. B-Cell depletion and immunomodulation before initiation of enzyme replacement therapy blocks the immune response to acid alpha-glucosidase in infantile-onset Pompe disease. J Pediatr. 2013;163(3):847–54. https://doi.org/10.1016/j.jpeds.2013.03.002. (e1).
Mendelsohn NJ, Messinger YH, Rosenberg AS, et al. Elimination of antibodies to recombinant enzyme in Pompe’s disease. N Engl J Med. 2009;360:194–5.
Markic J, Polic B, Stricevic L, et al. Effects of immune modulation therapy in the first Croatian infant diagnosed with Pompe disease: a 3-year follow-up study. Wien Klin Wochenschr. 2014;126(3–4):133–7. https://doi.org/10.1007/s00508-013-0475-3.
Rossi F. Kazatchkine: antiidiotypes against autoantibodies in pooled normal human polyspecific Ig. J Immunol. 1989;143:4104–9.
Bayry J, Lacroix-Desmazes S, Carbonneil C, et al. Inhibition of maturation and function of dendritic cells by intravenous immunoglobulin. Blood. 2003;101(2):758–65. https://doi.org/10.1182/blood-2002-05-1447.
Rairikar M, Kazi ZB, Desai A, et al. High dose IVIG successfully reduces high rhGAA IgG antibody titers in a CRIM-negative infantile Pompe disease patient. Mol Genet Metab. 2017;122(1–2):76–9. https://doi.org/10.1016/j.ymgme.2017.05.006.
Thomson AW, Turnquist HR, Raimondi G. Immunoregulatory functions of mTOR inhibition. Nat Rev Immunol. 2009;9(5):324–37. https://doi.org/10.1038/nri2546.
Alexander T, Cheng Q, Klotsche J, et al. Proteasome inhibition with bortezomib induces a therapeutically relevant depletion of plasma cells in SLE but does not target their precursors. Eur J Immunol. 2018;48(9):1573–9. https://doi.org/10.1002/eji.201847492.
Poelman E, Hoogeveen-Westerveld M, van den Hout JMP, et al. Effects of immunomodulation in classic infantile Pompe patients with high antibody titers. Orphanet J Rare Dis. 2019;14(1):71. https://doi.org/10.1186/s13023-019-1039-z.
Banugaria SG, Prater SN, McGann JK, et al. Bortezomib in the rapid reduction of high sustained antibody titers in disorders treated with therapeutic protein: lessons learned from Pompe disease. Genet Med. 2013;15:123–31.
Kazi ZB, Prater SN, Kobori JA, et al. Durable and sustained immune tolerance to ERT in Pompe disease with entrenched immune responses. JCI Insight. 2016. https://doi.org/10.1172/jci.insight.86821.
Owens P, Wong M, Bhattacharya K, et al. Infantile-onset Pompe disease: a case series highlighting early clinical features, spectrum of disease severity and treatment response. J Paediatr Child Health. 2018;54:1255–61.
Deodato F, Ginocchio VM, Onofri A, et al. Immune tolerance induced using plasma exchange and rituximab in an infantile Pompe disease patient. J Child Neurol. 2014;29(6):850–4. https://doi.org/10.1177/0883073813485819.
Banugaria SG, Patel TT, Mackey J, et al. Persistence of high sustained antibodies to enzyme replacement therapy despite extensive immunomodulatory therapy in an infant with Pompe disease: need for agents to target antibodysecreting plasma cells. Mol Genet Metab. 2012;105:677–80.
Ohashi T, Iizuka S, Shimada Y, et al. Oral administration of recombinant human acid α-glucosidase reduces specific antibody formation against enzyme in mouse. Mol Genet Metab. 2011;103(1):98–100. https://doi.org/10.1016/j.ymgme.2011.01.009.
Joly MS, Martin RP, Mitra-Kaushik S, et al. Transient low-dose methotrexate generates B regulatory cells that mediate antigen-specific tolerance to alglucosidase alfa. J Immunol. 2014;193(8):3947–58. https://doi.org/10.4049/jimmunol.1303326.
Garman RD, Munroe K, Richards SM. Methotrexate reduces antibody responses to recombinant human alpha-galactosidase A therapy in a mouse model of Fabry disease. Clin Exp Immunol. 2004;137(3):496–502. https://doi.org/10.1111/j.1365-2249.2004.02567.x.
Ohashi T, Iizuka S, Shimada Y, et al. Administration of anti-CD3 antibodies modulates the immune response to an infusion of α-glucosidase in mice. Mol Ther. 2012;20(10):1924–31. https://doi.org/10.1038/mt.2012.133.
Sun B, Banugaria SG, Prater SN, et al. Non-depleting anti-CD4 monoclonal antibody induces immune tolerance to ERT in a murine model of Pompe disease. Mol Genet Metab Rep. 2014;12(1):446–50. https://doi.org/10.1016/j.ymgmr.2014.08.005.
Mackay F, Woodcock SA, Lawton P, et al. Mice transgenic for BAFF develop lymphocytic disorders along with autoimmune manifestations. J Exp Med. 1999;190:1697–710.
Khare SD, Sarosi I, Xia XZ, et al. Severe B cell hyperplasia and autoimmune disease in TALL-1 transgenic mice. Proc Natl Acad Sci USA. 2000;97:3370–5.
Doerfler PA, Nayak S, Herzog RW, et al. BAFF blockade prevents anti-drug antibody formation in a mouse model of Pompe disease. Clin Immunol. 2015;158(2):140–7. https://doi.org/10.1016/j.clim.2015.03.022.
Baker KP, Edwards BM, Main SH, et al. Generation and characterization of LymphoStat-B, a human monoclonal antibody that antagonizes the bioactivities of B lymphocyte stimulator. Arthritis Rheum. 2003;48:3253–65.
Parsons RF, Yu M, Vivek K, et al. Murine islet allograft tolerance upon blockade of the B-lymphocyte stimulator, BLyS/BAFF. Transplantation. 2012;93:676–85.
Gorbacheva V, Ayasoufi K, Fan R, et al. B cell activating factor (BAFF) and a proliferation inducing ligand (APRIL) mediate CD40-independent help by memory CD4 T cells. Am J Transplant. 2015;15:346–57.
Mariño E, Walters SN, Villanueva JE, et al. BAFF regulates activation of self-reactive T cells through B-cell dependent mechanisms and mediates protection in NOD mice. Eur J Immunol. 2014;44:983–93.
Kyaw T, Cui P, Tay C, et al. BAFF receptor mAb treatment ameliorates development and progression of atherosclerosis in hyperlipidemic ApoE(−/−) mice. PLoS ONE. 2013;8: e60430.
Dörner T, Posch MG, Li Y, et al. Treatment of primary Sjögren’s syndrome with ianalumab (VAY736) targeting B cells by BAFF receptor blockade coupled with enhanced, antibody-dependent cellular cytotoxicity. Ann Rheum Dis. 2019;78(5):641–7. https://doi.org/10.1136/annrheumdis-2018-214720.
Zhang F, Bae SC, Bass D, et al. A pivotal phase III, randomised, placebo-controlled study of belimumab in patients with systemic lupus erythematosus located in China, Japan and South Korea. Ann Rheum Dis. 2018;77(3):355–63. https://doi.org/10.1136/annrheumdis-2017-211631.
Jacob CO, Pricop L, Putterman C, et al. Paucity of clinical disease despite serological autoimmunity and kidney pathology in lupusprone New Zealand mixed 2328 mice deficient in BAFF. J Immunol. 2006;177:2671–80.
Sato Y, Ida H, Ohashi T. Anti-BlyS antibody reduces the immune reaction against enzyme and enhances the efficacy of ERTin Fabry disease model mice. Clin Immunol. 2017;178:56–63. https://doi.org/10.1016/j.clim.2017.01.014.
Kirou KA, Dall Era M, Aranow C, et al. Belimumab or anifrolumab for systemic lupus erythematosus? A risk-benefit assessment. Front Immunol. 2022;31(13): 980079. https://doi.org/10.3389/fimmu.2022.980079.
Sands E, Kivitz A, DeHaan W, et al. Tolerogenic nanoparticles mitigate the formation of anti-drug antibodies against pegylated uricase in patients with hyperuricemia. Nat Commun. 2022;13(1):272. https://doi.org/10.1038/s41467-021-27945-7.
Baraf HSB, Khanna PP, Kivitz AJ, et al. The COMPARE head-to-head, randomised-controlled trial of SEL-212 (pegadricase plus rapamycin-containing nanoparticle, ImmTOR™) versus pegloticase for refractory gout. Rheumatology (Oxford). 2023. https://doi.org/10.1093/rheumatology/kead333.
Schlesinger N, Padnick-Silver L, LaMoreaux B. Enhancing the response rate to recombinant uricases in patients with gout. BioDrugs. 2022;36(2):95–103. https://doi.org/10.1007/s40259-022-00517-x.
Lim HH, Yi H, Kishimoto TK, et al. A pilot study on using rapamycin-carrying synthetic vaccine particles (SVP) in conjunction with enzyme replacement therapy to induce immune tolerance in Pompe disease. Mol Genet Metab Rep. 2017;23(13):18–22. https://doi.org/10.1016/j.ymgmr.2017.03.005.
Cremel M, Guerin N, Campello G, et al. Innovative approach in Pompe disease therapy: induction of immune tolerance by antigen-encapsulated red blood cells. Int J Pharm. 2015;491:69–77.
Schneider JL, Balu-Iyer SV. Phosphatidylserine converts immunogenic recombinant human acid alpha-glucosidase to a tolerogenic form in a mouse model of Pompe disease. J Pharm Sci. 2016;105(10):3097–104. https://doi.org/10.1016/j.xphs.2016.06.018.
Shimada Y, Nishimura E, Hoshina H, et al. Proteasome inhibitor bortezomib enhances the activity of multiple mutant forms of lysosomal α-glucosidase in Pompe disease. JIMD Rep. 2015;18:33–9. https://doi.org/10.1007/8904_2014_345.
Dahms NM, Lobel P, Kornfeld S. Mannose 6-phosphate receptors and lysosomal enzyme targeting. J Biol Chem. 1989;264:12115–8.
Vera M, Lester T, Zhao B, et al. Mannose 6-phosphate conjugation is not sufficient to allow induction of immune tolerance to phenylalanine ammonia-lyase in dogs. JIMD Rep. 2013;8:63–72. https://doi.org/10.1007/8904_2012_162.
Franco LM, Sun B, Yang X, et al. Evasion of immune responses to introduced human acid alphaglucosidase by liver-restricted expression in glycogen storage disease type II. Mol Ther. 2005;12:876–84.
Sun B, Zhang H, Franco LM, et al. Correction of glycogen storage disease type II by an adenoassociated virus vector containing a muscle-specific promoter. Mol Ther. 2005;11:889–98.
Mah C, Pacak CA, Cresawn KO, et al. Physiological correction of Pompe disease by systemic delivery of adeno-associated virus serotype 1 vectors. Mol Ther. 2007;15:501–7.
Ziegler RJ, Cherry M, Barbon CM, et al. Correction of the biochemical and functional deficits in Fabry mice following AAV8-mediated hepatic expression of a-galactosidase A. Mol Ther. 2007;15:492–500.
Barbon CM, Ziegler RJ, Li C, et al. AAV8-mediated hepatic expression of acid sphingomyelinase corrects the metabolic defect in the visceral organs of a mouse model of Niemann–Pick disease. Mol Ther. 2005;12:431–40.
Passini MA, Bu J, Fidler JA, et al. Combination brain and systemic injections of AAV provide maximal functional and survival benefits in the Niemann–Pick mouse. Proc Natl Acad Sci USA. 2007;104(22):9505–10. https://doi.org/10.1073/pnas.0703509104.
McEachern KA, Nietupski JB, Chuang WL, et al. AAV8-mediated expression of glucocerebrosidase ameliorates the storage pathology in the visceral organs of a mouse model of Gaucher disease. J Gene Med. 2006;8:719–29.
Hinderer C, Bell P, Louboutin JP, et al. Neonatal tolerance induction enables accurate evaluation of gene therapy for MPS I in a canine model. Mol Genet Metab. 2016;119(1–2):124–30. https://doi.org/10.1016/j.ymgme.2016.06.006.
Sun B, Zhang H, Bird A, et al. Impaired clearance of accumulated lysosomal glycogen in advanced Pompe disease despite high-level vector-mediated transgene expression. J Gene Med. 2009;11(10):913–20. https://doi.org/10.1002/jgm.1372.
Liang Q, Vlaar EC, Catalano F, et al. Lentiviral gene therapy prevents anti-human acid α-glucosidase antibody formation in murine Pompe disease. Mol Ther Methods Clin Dev. 2022;4(25):520–32. https://doi.org/10.1016/j.omtm.2022.04.016.
Muschol N, Koehn A, von Cossel K, et al. A phase I/II study on intracerebroventricular tralesinidase alfa in patients with Sanfilippo syndrome type B. J Clin Investig. 2023;133(2): e165076. https://doi.org/10.1172/JCI165076.
Kishnani PS, Dickson PI, Muldowney L, et al. Immune response to enzyme replacement therapies in lysosomal storage diseases and the role of immune tolerance induction. Mol Genet Metab. 2016;117(2):66–83. https://doi.org/10.1016/j.ymgme.2015.11.001.
De Groot AS, Kazi ZB, Martin RF, et al. HLA- and genotype-based risk assessment model to identify infantile onset Pompe disease patients at high-risk of developing significant anti-drug antibodies (ADA). Clin Immunol. 2019;200:66–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Conflict of interest
Aslı İnci, Fatih S. Ezgü and Leyla Tümer declare that they have no conflicts of interest.
Availability of data and material
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Authors’ contributions
All authors contributed to the design of the review, drafted the review and revised it for important intellectual content. All the authors saw the final version and approved of the version to be submitted.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
İnci, A., Ezgü, F.S. & Tümer, L. Advances in Immune Tolerance Induction in Enzyme Replacement Therapy. Pediatr Drugs 26, 287–308 (2024). https://doi.org/10.1007/s40272-024-00627-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-024-00627-9