Abstract
Background
Respiratory syncytial virus (RSV) causes significant morbidity and mortality in children aged ≤ 5 years and adults aged ≥ 60 years worldwide. Despite this, RSV-specific therapeutic options are limited. Rilematovir is an investigational, orally administered inhibitor of RSV fusion protein-mediated viral entry.
Objective
To establish the antiviral activity, clinical outcomes, safety, and tolerability of rilematovir (low or high dose) in children aged ≥ 28 days and ≤ 3 years with RSV disease.
Methods
CROCuS was a multicenter, international, double-blind, placebo-controlled, randomized, adaptive phase II study, wherein children aged ≥ 28 days and ≤ 3 years with confirmed RSV infection who were either hospitalized (Cohort 1) or treated as outpatients (Cohort 2) were randomized (1:1:1) to receive rilematovir (low or high dose) or placebo. Study treatment was administered daily as an oral suspension from days 1 to 7, with dosing based on weight and age groups. The primary objective was to establish antiviral activity of rilematovir by evaluating the area under the plasma concentration–time curve of RSV viral load in nasal secretions from baseline through day 5. Severity and duration of RSV signs and symptoms and the safety and tolerability of rilematovir were also assessed through day 28 (± 3).
Results
In total, 246 patients were randomized, treated, and included in the safety analysis population (Cohort 1: 147; Cohort 2: 99). Of these, 231 were included in the intent-to-treat-infected analysis population (Cohort 1: 138; Cohort 2: 93). In both cohorts, demographics were generally similar across treatment groups. In both cohorts combined, the difference (95% confidence interval) in the mean area under the plasma concentration–time curve of RSV RNA viral load through day 5 was - 1.25 (- 2.672, 0.164) and - 1.23 (- 2.679, 0.227) log10 copies∙days/mL for the rilematovir low-dose group and the rilematovir high-dose group, respectively, when compared with placebo. The estimated Kaplan–Meier median (95% confidence interval) time to resolution of key RSV symptoms in the rilematovir low-dose, rilematovir high-dose, and placebo groups of Cohort 1 was 6.01 (4.24, 7.25), 5.82 (4.03, 8.18), and 7.05 (5.34, 8.97) days, respectively; in Cohort 2, estimates were 6.45 (4.81, 9.70), 6.26 (5.41, 7.84), and 5.85 (3.90, 8.27) days, respectively. A similar incidence of adverse events was reported in patients treated with rilematovir and placebo in Cohort 1 (rilematovir: 61.9%; placebo: 58.0%) and Cohort 2 (rilematovir: 50.8%; placebo: 47.1%), with most reported as grade 1 or 2 and none leading to study discontinuation. The study was terminated prematurely, as the sponsor made a non-safety-related strategic decision to discontinue rilematovir development prior to full recruitment of Cohort 2.
Conclusions
Data from the combined cohort suggest that rilematovir has a small but favorable antiviral effect of indeterminate clinical relevance compared with placebo, as well as a favorable safety profile. Safe and effective therapeutic options for RSV in infants and young children remain an unmet need.
Clinical Trial Registration
EudraCT Number: 2016-003642-93; ClinicalTrials.gov Identifier: NCT03656510. First posted date: 4 September, 2018.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Despite the significant burden of respiratory syncytial virus, therapeutic options for the disease are limited. |
This study showed that rilematovir, an orally administered therapeutic option for respiratory syncytial virus, was safe and the results suggested a small but favorable antiviral effect of indeterminate clinical relevance in children aged ≥ 28 days and ≤ 3 years. |
Because of a non-safety-related strategic decision by the sponsor, rilematovir development was discontinued. |
Therapeutic options for respiratory syncytial virus remain an unmet need. |
1 Introduction
Respiratory syncytial virus (RSV) is a highly contagious seasonal pathogen that commonly causes bronchiolitis and pneumonia in young children [1]. RSV is responsible for an estimated 33.1 million episodes of acute lower respiratory tract infection, 3.2 million hospitalizations, and 59,600 in-hospital deaths globally each year in children aged ≤ 5 years [2]. Around 90% of children become infected with RSV during their first 2 years of life, and reinfections are frequent [3, 4]. Approximately 1–3% of children are hospitalized because of RSV lower respiratory tract disease in their first year of life, with most hospitalizations occurring in children aged ≤ 6 months [4]. Additionally, among children in the USA aged ≤ 5 years hospitalized because of community-acquired pneumonia, RSV is found in up to 37% of cases, highlighting the significant disease burden of RSV in children [5].
Despite the significant burden of RSV, therapeutic options are limited [6]. Palivizumab [7, 8], a monoclonal antibody targeting the RSV fusion (F) protein, is licensed for the prevention of severe RSV infection; however, its use is restricted to high-risk infants [9]. Nirsevimab, a long-acting monoclonal antibody, has been approved in the European Union and by the US Food and Drug Administration (FDA) for preventing RSV lower respiratory tract disease in newborns and infants [10,11,12]. The FDA also recently approved the first RSV vaccines for use in adults aged ≥ 60 years and women who are pregnant [13, 14]. Several other antiviral agents and monoclonal antibodies are currently in various stages of clinical development for RSV prophylaxis or treatment [15].
At present, there are no approved therapeutic drugs for children with confirmed RSV infection. Rilematovir (JNJ-53718678) is an investigational, orally administered small molecule that binds to the RSV F protein, thereby inhibiting RSV F-mediated fusion of the virus with the cell membrane and viral entry into the cell [16]. Rilematovir has demonstrated antiviral activity against both RSV-A and RSV-B strains in vitro [17], and reduced viral loads were observed in infants (aged > 1 to ≤ 24 months) hospitalized with RSV infection who were treated with rilematovir versus placebo in a phase Ib study, although with a small sample size [18]. While reduced viral loads are an important indicator of antiviral activity, demonstrating a therapeutic benefit requires the evaluation of clinical outcome measures [19]. However, there are currently no standardized clinical outcome measures to evaluate RSV disease severity or the impact of therapeutic interventions. The Pediatric RSV Electronic Severity and Outcome Rating System (PRESORS), a novel clinical outcome measure used in this study, was developed to assess the severity of RSV infections in children [19, 20].
Here, the results of the phase II CROCuS study evaluating the efficacy (with RSV viral load [area under the concentration–time curve (AUC)] from baseline through day 5 as the primary efficacy endpoint) and safety of rilematovir in children aged ≥28 days and ≤3 years with RSV infection are reported.
2 Methods
2.1 Study Design
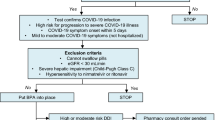
CROCuS (Children’s RSV Outcome Clinical Study; EudraCT Number: 2016-003642-93; ClinicalTrials.gov Identifier: NCT03656510) was a multicenter, double-blind, placebo-controlled, randomized, adaptive phase II study conducted at 176 sites in 22 countries (Fig. 1). The study was conducted from 3 December 2018 (first informed consent signed) to 18 April 2022 (last patient, last visit). The study was terminated prematurely, as the sponsor made a non-safety-related strategic decision to discontinue the development of rilematovir in view of the encountered operational and clinical development challenges.
Study design. C1 Cohort 1, C2 Cohort 2, RSV respiratory syncytial virus. aStudy sites were located in Argentina, Belgium, Brazil, Bulgaria, France, Germany, Hungary, Italy, Japan, Malaysia, Mexico, Poland, Russia, Taiwan, Thailand, South Africa, South Korea, Spain, Sweden, Turkey, UK, and the USA. bScreening and treatment could have occurred on the same day. cThe original estimated sample size for C2 was N = 150, or 50 patients per treatment group. The sample size in C2 was allowed to be increased to a maximum of 300 (100 per treatment group) based on a pre-planned sample size re-estimation after interim analysis 3. dPrior to Protocol Amendment 4, study treatment was administered once daily. After Protocol Amendment 4, study treatment was administered twice daily, with the total daily dose remaining unmodified. eRilematovir dosing and volume of placebo were based on weight (mg/kg) and age group for both cohorts. fC1 after discharge and C2. gIn case of ongoing adverse event(s)
The study design included pre-planned interim analyses (IAs) and adaptive design elements (Table 1 of the Electronic Supplementary Material [ESM]). An independent data monitoring committee was commissioned to review unblinded safety data on a regular basis, as well as data from the IAs, and to make recommendations to the Sponsor Committee. At any point during the study, the independent data monitoring committee had the authority to recommend modifications to the study conduct and/or to safety assessments, including the recommendation to halt a dose arm because of safety concerns.
2.2 Eligibility Criteria
Children aged ≥ 28 days and ≤ 3 years with laboratory-confirmed RSV disease who were otherwise healthy or had a risk factor for severe RSV disease were eligible, provided they could be randomized within 5 days after RSV symptom onset. Laboratory-confirmed RSV disease was defined as RSV positive by molecular or antigen-based testing with one or more symptoms of upper respiratory tract infection (nasal congestion, rhinorrhea, pharyngitis, or otitis media), one or more symptoms of lower respiratory tract infection (increased respiratory effort [as evidenced by subcostal, intercostal, or tracheosternal retractions; grunting; head bobbing; nasal flaring; or tachypnea], abnormal breathing sounds [such as wheezing, rales, or rhonchi], cyanosis, apnea, or cough [cough or wheezing should have been accompanied by one or more additional lower respiratory tract infection sign/symptom]), and one or more systemic/general symptom (feeding difficulties, defined as a < 75% intake of normal food amounts; dehydration; fever; or disturbed sleep or disturbed activity level, including irritability, restlessness, agitation, and decreased responsiveness). Examples of risk factors for severe disease and key exclusion criteria are provided in the ESM.
2.3 Study Procedures
Children presenting to a healthcare facility with symptoms of an acute respiratory illness supporting a diagnosis of RSV infection (e.g., nasal congestion, rhinorrhea, pharyngitis, increased respiratory effort, abnormal breathing sounds [wheezing, rales, or rhonchi], cyanosis, cough, apnea, fever, feeding difficulties, dehydration) were screened. A nasal swab was taken to test for RSV infection if nasal swabs were not taken as part of the standard of care. Enrolled patients who were hospitalized were included in Cohort 1, while those who were treated on an outpatient basis were included in Cohort 2. Within each cohort, patients were centrally randomized (1:1:1) to receive either a low or high dose of rilematovir or placebo, stratified by the time since symptom onset (≤ 3 days, > 3 days to ≤ 5 days) and the presence of risk factors for severe RSV disease. Study treatment was initiated ≤ 4 h post-randomization. Following IA3, a population-enrichment decision was made and enrollment in Cohort 2 was limited to only patients with ≤ 3 days since symptom onset.
Study treatment was administered as a flavored oral suspension (rilematovir active powder reconstituted to 23 mg/mL) for 7 consecutive days, with the total daily dose based on weight (mg/kg) and age group (age group 1: ≥ 28 days and < 3 months; age group 2: ≥ 3 months and < 6 months; age group 3: ≥ 6 months and ≤ 3 years) for each cohort to achieve target exposures established by a phase Ib pharmacokinetic analysis [18]. Analysis of interim data from CROCuS (n = 62; once-daily dosing) yielded exposure metrics (maximum observed concentration at steady state, trough concentration at steady state, and AUC up to 24 h post-dosing at steady state) that confirmed population pharmacokinetic modeling, and simulations predicted exposures indicating that study drug exposure was consistent across the different age groups. Dosing frequency was changed from once to twice daily (Protocol Amendment 4) to mitigate the potential risk of QT interval prolongation, while maintaining the highest potential antiviral effect and minimizing the risk of developing antiviral resistance. While the dosage per administration was reduced by half with the change in dosing frequency, the unmodified total daily dose was expected to result in similar exposures. Patients in the high-dose group received total daily doses of 5.0 mg/kg (0.300–2.2 mL), 6.0 mg/kg (0.375–2.6 mL), or 9.0 mg/kg (0.550–4.0 mL) of study treatment for age groups 1, 2, and 3, respectively; those in the low-dose group received total daily doses of 1.7 mg/kg (0.125–0.725 mL), 2.0 mg/kg (0.125–0.850 mL), or 3.0 mg/kg (0.200–1.3 mL) of study treatment for age groups 1, 2, and 3, respectively (Table 2 of the ESM). Patients in the matching placebo group received high-volume or low-volume placebo in accordance with their weight and age group.
The total study duration was approximately 29 days (screening: day - 1 to day 1; treatment period: day 1 to day 8; follow-up period: day 9 to day 28 [± 3]; Fig. 1). On-site follow-up visits took place on days 14 ± 1 and 21 ± 3; an on-site or telephone follow-up visit took place on day 28 ± 3.
2.4 Study Assessments
Patient demographics and characteristics (e.g., presence of comorbidities or risk factors for severe RSV, RSV symptom duration, and RSV viral load) were collected at screening. The RSV viral load in nasal secretions was measured at a central laboratory (Viroclinics-DDL, Rotterdam, The Netherlands) using a quantitative, real-time, reverse transcription polymerase chain reaction (qRT-PCR) assay on mid-turbinate swab specimens that were collected at screening, daily during treatment, daily from day 9 up to day 13 if patients were still hospitalized (Cohort 1) or symptomatic (patients in Cohort 1 who had been discharged and Cohort 2), and on days 14 and 21. The severity and duration of 12 RSV signs and symptoms, including six key RSV symptoms (breathing problems, tachypnea, tachycardia, retractions, breathing sounds, and cough), were assessed using the PRESORS observer-reported outcome questionnaire (PRESORS ObsRO; Version 7.1) [20], which was completed by caregivers [21] on an electronic device at screening, twice daily (morning and evening) from day 1 to day 14, and once daily (evening) from day 15 to day 21 (Table 3 of the ESM) [20, 21].
2.5 Study Objectives and Endpoints
The primary objective was to establish antiviral activity by assessing the AUC of RSV RNA viral load, as measured by qRT-PCR in nasal swabs, from immediately prior to the first dose of study treatment through day 5. The primary hypothesis was that rilematovir has antiviral activity against RSV, as assessed by a positive dose–response relationship of rilematovir compared with placebo. Selection of the primary antiviral endpoint was based on the early antiviral effect of rilematovir observed in a phase Ib study [18]. The primary efficacy analysis of the study was based on the results of Cohorts 1 and 2 combined, as antiviral activity was expected to be independent of the clinical setting. Secondary objectives included evaluation of the dose–response relationship for antiviral activity, the impact of rilematovir on the clinical course of RSV infection, the emergence of changes in viral genome potentially associated with antiviral resistance, acceptability and palatability, and safety and tolerability.
Secondary virologic endpoints included changes from baseline in RSV viral load over time and the time to first confirmed undetectable RSV RNA viral load (defined as an RSV RNA viral load value less than the lower limit of quantification [LLOQ], target not detected). For the RSV-A qRT-PCR assay, the limit of detection was 620 (2.8 log10) copies/mL, and the LLOQ was 1000 (3 log10) copies/mL. For the RSV-B qRT-PCR assay, the limit of detection was 80 (1.9 log10) copies/mL, and the LLOQ was 250 (2.4 log10) copies/mL. A confirmed undetectable sample was defined as the first of two or more consecutive undetectable samples post-baseline.
Secondary clinical endpoints for Cohort 1 included the time to hospital discharge and time to the end of oxygen supplementation (Methods in ESM). Meanwhile, RSV signs and symptoms (assessed using the PRESORS ObsRO) and medical resource utilization (i.e., need for hospitalization [Cohort 2] or re-hospitalization [Cohort 1] or outpatient encounters during the study) were assessed for both cohorts. During the study, the definition of time to resolution of PRESORS ObsRO key RSV symptoms was evaluated and refined at interim stages to ensure a more suitable, clinically relevant endpoint for further development in phase III studies. The requirement of being free of oxygen, hydration, and feeding supplementation for at least 24 h was added, resulting in the derivation and analysis of the time (hours) from the first dose of study treatment until the first time at which all key RSV symptoms were scored as not present or mild (i.e., “resolved”) after being free of oxygen, hydration, and feeding supplementation for at least 24 h (Table 3 of the ESM). This requirement was added as such supplementation could mask symptom severity.
Acceptability and palatability of rilematovir were assessed by questionnaires completed by caregivers on day 8. Safety and tolerability were assessed by adverse events (AEs), clinical laboratory assessments, electrocardiograms, vital signs, and physical examinations throughout the study. RSV-related complications were identified from reported AEs and classified according to respiratory complications, infectious complications, cardiovascular complications, and acid-base or electrolyte complications. AEs were coded using the Medical Dictionary for Regulatory Activities Version 23.1 [22]. Clinical laboratory assessments were conducted at screening, day 8, and day 21, and, for patients with an onsite visit, on day 28. Laboratory abnormalities were determined according to the Division of Microbiology and Infectious Diseases pediatric toxicity tables (November 2007). Patients’ safety was monitored throughout the study by an independent data monitoring committee.
The emergence of changes in the RSV F gene sequence was evaluated by next-generation sequencing (Illumina, San Diego, CA, USA) of mid-turbinate swab samples collected at baseline and selected post-baseline timepoints (Viroclinics-DDL). Sequencing analyses of RSV-A and RSV-B strains focused on 24 F protein positions of interest for RSV F inhibitors (positions 127, 137, 138, 140, 141, 143, 144, 323, 338, 339, 392, 394, 396, 397, 398, 399, 400, 401, 474, 486, 487, 488, 489, and 517) [17, 23]. Additional information is provided in the ESM.
2.6 Statistical Analysis
All randomized patients who received one or more doses of study treatment were included in the safety analysis population. Efficacy analyses were conducted in the intent-to-treat-infected (ITT-i) analysis population, defined as all randomized patients who received one or more doses of study treatment and who had an RSV RNA viral load of ≥ 1 log10 copies/mL above the LLOQ of the RSV qRT-PCR assay at baseline. Patients’ data were analyzed according to the randomized treatment arm.
The primary analysis and analysis of the dose–response relationship were conducted using a hybrid methodology combining aspects of multiple comparison testing with modeling techniques (Multiple Comparison Procedure-Modeling) [24,25,26], as described in the ESM. The time to the first confirmed undetectable RSV RNA viral load, resolution of key PRESORS ObsRO RSV symptoms, hospital discharge, and the end of oxygen supplementation were estimated using the Kaplan–Meier analysis.
2.7 Sample Size
Assuming a reduction in RSV viral load AUC of 20% compared with placebo, considering a coefficient of variation of 35%, and a one-sided alpha of 2.5%, the power to conclude a dose response using the Multiple Comparison Procedure-Modeling procedure under different assumptions for the dose–response relationship (linear, maximal efficacy, and exponential) was > 90% if data of both cohorts were combined (n = 74 per treatment arm). Therefore, the trial was initially planned to enroll 72 participants in Cohort 1 (n = 24 per treatment arm), and 150 participants in Cohort 2 (n = 50 per treatment arm). During the trial, it was decided to increase the sample size in Cohort 1 to 144 (n = 48 per treatment arm) to enable a more precise estimation of the clinical course endpoints in this hospitalized cohort (Protocol Amendment 1).
As no clinical endpoints for a phase III study had been identified at the time of study design and the association between the antiviral effect and clinical course endpoints was not yet established for RSV, a key secondary objective of this phase II study was the evaluation of clinical course endpoints and their dependence on viral load reductions. Results of this phase II study were meant to inform the discussion on and selection of clinical course endpoints and guide the design for subsequent phase III studies. Therefore, during IA3, a sample size re-estimation was performed to allow an extension of Cohort 2 to confirm and increase the precision of the results of selected clinical course endpoints (Nre-estimated = 210; Table 1 of the ESM). Clinical course endpoints considered were time to resolution of key RSV symptoms (PRESORS ObsRO), incidence of RSV-related complications, and change from baseline in key RSV symptoms (PRESORS ObsRO). The number of patients in Cohort 2 required to limit the conditional “consider” probability (i.e., an inconclusive result at the end of the study) to 20% for clinical endpoints was calculated (up to a maximum of n = 100 per treatment group) using a Go/No-Go approach, with a required confidence of 90% (one-sided) to exclude a predefined target value and/or minimum acceptable value.
3 Results
3.1 Patients
A total of 263 children were screened, and 246 were randomized, treated, and included in the safety analysis population. Of these, 144 patients (98.0%) in Cohort 1 and 98 patients (99.0%) in Cohort 2 completed the study. Figure 2 provides additional details regarding patient disposition and the composition of the safety and ITT-i analysis populations.
Patient disposition. ITT-i intent-to-treat-infected, LLOQ lower limit of quantification, RSV respiratory syncytial virus. aDefined as all randomized patients who received one or more doses of study treatment and who had an RSV RNA viral load of ≥1 log10 copies/mL above the LLOQ of the RSV quantitative real-time reverse transcription polymerase chain reaction assay at baseline. bSponsor’s decision leading to discontinuation of study treatment was because of the non-safety-related strategic decision of premature study termination
All patients in Cohort 1 received once-daily dosing. Patients in Cohort 2 who were enrolled before Protocol Amendment 4 (i.e., approximately 70% of Cohort 2 patients) also received once-daily dosing. The remaining patients in Cohort 2 enrolled after Protocol Amendment 4, wherein the dosing frequency was changed from once-daily to twice-daily dosing, with an unmodified total daily dose.
In the ITT-i analysis population, the median (range) age was 5.54 (1.0, 34.8) months for Cohort 1 and 12.98 (2.0, 35.6) months for Cohort 2 (Table 1). Demographics were similar across treatment groups for both cohorts, except in Cohort 2 where patients in the rilematovir high-dose group were older than those in the rilematovir low-dose and placebo groups. Approximately half of the patients (52.2%) in Cohort 1 had RSV symptoms for > 3 to ≤ 5 days prior to randomization, while most patients (73.1%) in Cohort 2 had RSV symptoms for ≤ 3 days prior to randomization because of the population enrichment decision following IA3. Median baseline RSV viral load values were 6.78 log10 copies/mL for Cohort 1 and 7.43 log10 copies/mL for Cohort 2. Most patients in both cohorts were infected with RSV-A. In Cohort 1, most patients (76.1%) required supplemental oxygen and about one-third (34.8%) required supplemental feeding prior to the first dose of study treatment.
At baseline, 13 patients in Cohort 1 were in the intensive care unit (ICU). Additionally, 11 patients in Cohort 1 required non-invasive or invasive mechanical ventilation at the time of the first dose of study treatment; of these, eight were in the ICU. Baseline imbalances of patients in the ICU and/or receiving mechanical ventilation were observed, especially in patients with ≤ 3 days since symptom onset.
Within the ITT-i analysis population of the combined cohort, demographics were similar across treatment groups. Risk factors for severe RSV disease were present in 18.6% of patients.
3.2 RSV RNA Viral Load
Figure 3 shows RSV RNA viral load (mean ± standard error) change from baseline to day 8 in the combined cohort for the rilematovir low-dose, rilematovir high-dose, and placebo groups and provides the mean (standard deviation) change from baseline at day 5. Changes in the RSV RNA viral load were relatively similar between groups overall (Fig. 3A), in patients with ≤ 3 days since symptom onset (Fig. 3B), and in patients with > 3 and ≤ 5 days since symptom onset (Fig. 3C).
Change in respiratory syncytial virus (RSV) RNA viral load (mean ± standard error [SE]) from baseline to day 8 in the intent-to-treat-infected population for Cohort 1 and Cohort 2 combined (A) overall, (B) in patients with ≤ 3 days since symptom onset, and (C) in patients with > 3 to ≤ 5 days since symptom onset. SD standard deviation
Results of the Multiple Comparison Procedure-Modeling method showed that the maximal efficacy dose–response relationship best fit the data (Table 4 of the ESM), indicating that low-dose and high-dose rilematovir performed equally well to one another and both performed better than placebo. Because of premature study discontinuation, the primary study hypothesis was not tested using a p value combination to correct for the decisions regarding adaptive design elements (i.e., enrichment and sample size re-estimation); however, the unadjusted p value (0.047) assessing Cohort 1 and Cohort 2 combined suggests a favorable antiviral effect of rilematovir compared with placebo. In line with this, the total difference in the mean RSV viral load AUC (95% CI) through day 5 was − 1.24 (− 2.479, − 0.001) log10 copies∙days/mL for the combined rilematovir low-dose and high-dose groups when compared with placebo (Table 5 of the ESM).
In the subgroup of patients with ≤ 3 days since symptom onset, the mean difference (95% CI) in the AUC of RSV RNA viral load through day 5 compared with placebo was - 2.54 (- 4.463, - 0.618) log10 copies∙days/mL for the rilematovir low-dose group, - 1.46 (- 3.480, 0.556) log10 copies∙days/mL for the rilematovir high-dose group, and - 2.00 (- 3.708, - 0.294) log10 copies∙days/mL for the combined rilematovir treatment group. For patients with > 3 days to ≤ 5 days since symptom onset, the mean difference (95% CI) from placebo in the AUC of RSV RNA viral load through day 5 was 0.57 (- 1.552, 2.697), - 0.90 (- 2.992, 1.202), and - 0.16 (- 1.975, 1.653) log10 copies∙days/mL for the rilematovir low-dose, rilematovir high-dose, and combined rilematovir treatment groups, respectively.
3.3 Time to First Confirmed Undetectable RSV RNA Viral Load
In Cohorts 1 and 2 combined, the estimated Kaplan–Meier median (95% CI) time to first confirmed undetectable RSV RNA viral load ranged from 9.73 (7.84, 13.01) days to 13.79 (9.84, 17.73) days across treatment groups (Fig. 4).
3.4 Time to Resolution of Key RSV Symptoms
From baseline to day 8, PRESORS ObsRO assessments were completed for > 90% of patients in Cohort 1 across all treatment groups; completion remained > 80% throughout the study, except for the placebo group at day 21 (57.5%). In Cohort 2, completion remained > 78% for all treatment groups throughout the study, except for the rilematovir low-dose group at day 21 (72.7%). The most common reasons for missing PRESORS ObsRO assessments were caregivers forgetting to complete the assessment (Cohorts 1 and 2) and technical issues with the device (Cohort 2).
In Cohort 1, the estimated Kaplan–Meier median (95% CI) time to resolution of key RSV symptoms ranged from 5.82 (4.03, 8.18) to 7.05 (5.34, 8.97) days across treatment groups (Fig. 5). The estimated Kaplan–Meier median (95% CI) time to resolution of key RSV symptoms ranged from 5.85 (3.90, 8.27) to 6.45 (4.81, 9.70) days in Cohort 2.
Time to resolution of key respiratory syncytial virus symptoms (Pediatric Respiratory Syncytial Virus Electronic Severity and Outcome Rating System observer-reported outcome) in the intent-to-treat-infected analysis population for Cohorts 1 and 2. CI confidence interval, + indicates censoring. aDefined as the time (hours) from the first dose of study treatment until the first time at which all key respiratory syncytial virus symptoms were scored as not present or mild (i.e., “resolved”) after being free of oxygen, hydration, and feeding supplementation for at least 24 hours
In Cohort 1, the estimated Kaplan–Meier median (95% CI) time to resolution of key RSV symptoms after being free of supplementation for at least 24 h ranged from 6.54 (5.18, 8.98) to 8.10 (6.93, 9.92) days across treatment groups, from 5.18 (4.00, 9.81) to 8.97 (6.93, 12.85) days for the subgroup of participants with ≤ 3 days since symptom onset, and from 5.87 (3.93, 8.28) to 7.80 (4.97, 8.65) days for the subgroup of participants with > 3 days and ≤ 5 days since symptom onset (Fig. 1 of the ESM).
3.5 Time to First Hospital Discharge and Time to End of Oxygen Supplementation (Cohort 1)
The estimated Kaplan–Meier median time to the first hospital discharge was similar between treatment groups (Fig. 6A), as was the estimated Kaplan–Meier median time to the end of oxygen supplementation (Fig. 6B).
Time to A hospital discharge and B end of oxygen supplementation for patients in Cohort 1a. CI confidence interval, + indicates censoring. aThe graph in B represents time to the end of oxygen supplementation up to 72 h from first hospital discharge (i.e., excluding oxygen supplementation received during re-hospitalizations that occurred > 72 h after initial hospital discharge)
3.6 Medical Resource Utilization
In Cohort 1, 4.3% of patients in the rilematovir low-dose group, 2.3% in the rilematovir high-dose group, and 6.4% in the placebo group were re-hospitalized during the study following initial hospital discharge. In Cohort 2, 15.2%, 25.0%, and 9.4% of patients in the rilematovir low-dose group, rilematovir high-dose group, and the placebo group, respectively, had medical care encounters during the study period. In total, 6.1% of patients in the rilematovir low-dose group, 14.3% in the rilematovir high-dose group, and 6.3% in the placebo group had hospital inpatient encounters (i.e., hospital inpatient department or visits to the emergency room [> 24 h]). Additional details regarding medical resource utilization are provided in Table 6 of the ESM.
3.7 RSV-related Complications
A summary of RSV-related complications is shown in Table 7 of the ESM. No grade 4 emergent RSV-related complications were reported in Cohort 1. Grade 4 bronchiolitis was reported in one placebo patient of Cohort 2. No emergent RSV-related complications leading to study discontinuation were reported in either cohort. None of the individual emergent RSV-related complications were reported in more than two patients in any treatment group in either cohort.
3.8 Viral Sequencing Analyses
In the combined cohort, emerging amino acid substitutions among the 24 RSV F protein positions of interest were observed post-baseline (during treatment and/or follow-up) in 5.9% (4/68) of patients with sequencing data available in the rilematovir high-dose group (G143S in two patients; D338Y and K399N in one patient each; Table 8 of the ESM); these were not observed in any of the patients with sequencing data available in the rilematovir low-dose (0/72) or placebo (0/76) groups. For all four patients, emerging substitutions were detected in combination with wild type (the amino acid present at baseline). Additional results of baseline viral sequencing analyses are reported in the ESM.
3.9 Acceptability and Palatability
In both cohorts, the majority of caregivers of patients who received rilematovir reported that study treatment was acceptable (Cohort 1: 78.3%; Cohort 2: 88.1%) and those patients took the treatment easily (Cohort 1: 78.3%; Cohort 2: 88.1%; Table 9 of the ESM). For those receiving placebo, 67.6% and 70.8% of participants in Cohorts 1 and 2, respectively, reported that study treatment was acceptable; the same proportions reported that study treatment was easily taken.
3.10 Safety
A similar incidence of AEs was reported in patients treated with rilematovir and placebo in both Cohort 1 (rilematovir: 61.9%; placebo: 58.0%) and Cohort 2 (rilematovir: 50.8%; placebo: 47.1%; Table 2). In both Cohorts 1 and 2, the most common AEs were in the system organ class of infections and infestations, many of which were respiratory in nature. For both cohorts, no AEs leading to study discontinuation were reported, and most AEs across treatment groups were reported as grade 1 (mild) or 2 (moderate).
In Cohort 1, grade 3 AEs were reported in 6.2% of those receiving rilematovir and 8.0% of those receiving placebo; in Cohort 2, grade 3 AEs were reported in 4.6% and 0.0% of those receiving rilematovir and placebo, respectively. None of the grade 3 AEs in either cohort were considered related to study treatment by the investigator. No grade 4 AEs were reported in Cohort 1, while a grade 4 AE (bronchiolitis) was reported in one patient (2.9%) in the placebo group of Cohort 2 that was considered unrelated to the study treatment by the investigator.
Few patients in Cohort 1 or Cohort 2 reported serious AEs, and serious AE frequency was similar between patients treated with rilematovir compared with those receiving placebo. No serious AEs were considered to be related to study treatment by the investigator. Additional safety results, including protocol-defined AEs of interest are reported in the safety section of the ESM.
4 Discussion
This report includes the results of the completed Cohort 1 (hospitalized patients) and prematurely terminated Cohort 2 (outpatients) for the phase II CROCuS study. Results of the primary efficacy analysis, evaluating the effects of rilematovir on the AUC of RSV RNA viral load through day 5 for Cohorts 1 and 2 combined, suggest a small but favorable antiviral effect of indeterminate clinical relevance of rilematovir compared with placebo. In Cohorts 1 and 2 combined, the estimated Kaplan–Meier median time to the first confirmed undetectable RSV RNA viral load was 2.1 and 4.1 days lower in the rilematovir low-dose and high-dose groups, respectively, compared with those receiving placebo. Observed differences in baseline viral load between Cohort 1 and Cohort 2 were accounted for in the primary efficacy analysis for RSV RNA AUC through day 5, as the statistical model included baseline log10 RSV RNA viral load and stratification factors (symptom onset and presence of risk factors for severe RSV disease) as covariates.
Notably, patients with ≤ 3 days since symptom onset showed a numerically greater decrease, resulting in a smaller AUC of RSV RNA viral load through day 5 than those with > 3 days to ≤ 5 days since symptom onset. These findings highlight the limited window of opportunity for effective RSV antiviral therapy, which has been noted in reports of other investigational RSV antiviral drugs [27]. Early intervention may be more critical for RSV F inhibitors as they inhibit the first step (fusion-mediated entry) in the viral replication cycle.
Assessment of several clinically relevant endpoints evaluating the effects of rilematovir on clinical outcomes suggested small or no differences. In Cohort 1, a reduction in the median time to the resolution of key RSV symptoms by 1.04 and 1.23 days was observed in the rilematovir low-dose and high-dose groups, respectively, suggesting a small but favorable clinical effect. However, no effects of rilematovir on the median time to resolution of key RSV symptoms were observed in Cohort 2. This may have been because of the lower baseline symptom severity in this cohort or the insufficient sample size that resulted from the premature termination of the study. In Cohort 1, patients treated with rilematovir low or high dose had a shorter median time of 1.27 and 1.56 days, respectively, to the resolution of key RSV symptoms after being free of supplementation for at least 24 h than those treated with placebo. There were no differences in the median time to hospital discharge nor the time to end of oxygen supplementation between treatment groups of hospitalized children in Cohort 1. A low incidence of re-hospitalization in Cohort 1, inpatient hospitalization in Cohort 2, and RSV-related complications in both cohorts was observed. The difference between the antiviral and clinical effects can possibly be explained by the activation of the inflammatory pathways by RSV, resulting in the clinical signs and symptoms, which typically occurs later than the actual infection. This inflammation cannot be directly inhibited by antiviral agents that target viral entry, such as rilematovir.
Post-baseline emerging amino acid changes at positions of interest within the RSV F protein were only observed in four patients in the rilematovir high-dose group. Substitution G143S, which emerged in two out of the four patients with emerging substitutions, has been associated with resistance to rilematovir in vitro. The impact of K399N or D338Y on the in vitro activity of rilematovir has not been tested, but these substitutions have been associated with reduced susceptibility to presatovir, another RSV F inhibitor [23].
Both rilematovir low-dose and high-dose regimens were safe and well tolerated, with a low incidence of treatment-related AEs and no AEs leading to treatment discontinuation. Furthermore, rilematovir was generally acceptable and easily taken, suggesting palatability of the formulation.
The results of this study should be interpreted cautiously, considering the small sample size of the completed Cohort 1 and incomplete Cohort 2, as well as the subgroups by time since symptom onset. The actual number of outpatients in Cohort 2 (Nactual = 99) was below that of the re-estimated sample size after IA3 (Nre-estimated = 210), thus not allowing firm conclusions to be drawn based on the current analyses. Furthermore, high variability was observed for viral load and clinical endpoints, which might have been influenced in Cohort 1 by the baseline imbalances of patients in the ICU and/or receiving mechanical ventilation.
5 Conclusions
Although there were no safety concerns and data from the combined cohorts suggest that rilematovir had small but favorable antiviral effects compared with placebo, no firm conclusions could be drawn because of the early termination of CROCuS. This termination was driven by a non-safety-related strategic decision by the sponsor to discontinue rilematovir development, which was influenced by challenges in recruiting patients within 3 days of symptom onset, as well as the totality of the clinical efficacy data in the various adult and pediatric populations evaluated thus far. Recruitment for Cohort 2 was also likely impacted by the COVID-19 pandemic, during which time an atypically low RSV circulation was observed [28], combined with more restricted access to healthcare for non-COVID-19-related services [29]. Ultimately, these findings highlight the challenges and need for continued exploration of safe and effective therapeutic options for RSV in infants and young children.
References
Center for Disease Control and Prevention. Respiratory syncytial virus infection (RSV). 2022. https://www.cdc.gov/rsv/index.html. Accessed 19 Dec 2022.
Shi T, McAllister DA, O’Brien KL, Simoes EAF, Madhi SA, Gessner BD, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet. 2017;390:946–58.
Baraldi E, Checcucci Lisi G, Costantino C, Heinrichs JH, Manzoni P, Ricco M, et al. RSV disease in infants and young children: can we see a brighter future? Hum Vaccin Immunother. 2022;18:2079322.
American Academy of Pediatrics. Red book 2018–2021. Report of the Committee of Infectious Diseases. Itasca: American Academy of Pediatrics; 2018.
Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015;372:835–45.
Griffiths C, Drews SJ, Marchant DJ. Respiratory syncytial virus: infection, detection, and new options for prevention and treatment. Clin Microbiol Rev. 2017;30:277–319.
Synagis® (palivizumab) injection, for intramuscular use [package insert]. Waltham: Sobi Inc.; 2021.
European Medicines Agency. Synagis: summary of product characteristic. 2009. https://www.ema.europa.eu/en/documents/product-information/synagis-epar-product-information_en.pdf. Accessed 22 Feb 2023.
Rodriguez-Fernandez R, Mejias A, Ramilo O. Monoclonal antibodies for prevention of respiratory syncytial virus infection. Pediatr Infect Dis J. 2021;40:S35–9.
European Medicines Agency. Beyfortus (nirsevimab) product information. https://www.ema.europa.eu/en/medicines/human/EPAR/beyfortus#product-information-section. Accessed 15 Mar 2023.
Hammitt LL, Dagan R, Yuan Y, Baca Cots M, Bosheva M, Madhi SA, et al. Nirsevimab for prevention of RSV in healthy late-preterm and term infants. N Engl J Med. 2022;386:837–46.
US Food and Drug Administration. FDA approves new drug to prevent RSV in babies and toddlers. 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-new-drug-prevent-rsv-babies-and-toddlers. Accessed 19 Dec 2023.
Vidal VM. “A good day”: FDA approves world’s first RSV vaccine. Nature. 2023;617:234–5.
Pfizer. U.S. FDA approves ABRYSVO™, Pfizer’s vaccine for the prevention of respiratory syncytial virus (RSV) in infants through active immunization of pregnant individuals 32-36 weeks of gestational age. August 21, 2023. https://www.pfizer.com/news/press-release/press-release-detail/us-fda-approves-abrysvotm-pfizers-vaccine-prevention-0#:~:text=%E2%80%9CABRYSVO's%20approval%20as%20the%20first,and%20Chief%20Scientific%20Officer%2C%20Vaccine. Accessed 31 Aug 2023.
Domachowske JB, Anderson EJ, Goldstein M. The future of respiratory syncytial virus disease prevention and treatment. Infect Dis Ther. 2021;10:47–60.
National Center for Biotechnology Information. Rilematovir compound summary. 2022. https://pubchem.ncbi.nlm.nih.gov/compound/Rilematovir. Accessed 19 Dec 2022.
Roymans D, Alnajjar SS, Battles MB, Sitthicharoenchai P, Furmanova-Hollenstein P, Rigaux P, et al. Therapeutic efficacy of a respiratory syncytial virus fusion inhibitor. Nat Commun. 2017;8:167.
Martinón-Torres F, Rusch S, Huntjens D, Remmerie B, Vingerhoets J, McFadyen K, et al. Pharmacokinetics, safety, and antiviral effects of multiple doses of the respiratory syncytial virus (RSV) fusion protein inhibitor, JNJ-53718678, in infants hospitalized with RSV infection: a randomized phase 1b study. Clin Infect Dis. 2020;71:e594-603.
US Food and Drug Administration. Respiratory syncytial virus infection: developing antiviral drugs for prophylaxis and treatment guidance for industry. 2017. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/respiratory-syncytial-virus-infection-developing-antiviral-drugs-prophylaxis-and-treatment-guidance. Accessed 25 May 2023.
Vandendijck Y, Scott J, Heerwegh D, Van Der Elst W, Witek J, Sinha R, et al. Measuring respiratory syncytial virus infection severity in hospitalized children using the Pediatric Respiratory Syncytial Virus Electronic Severity and Outcome Rating System (PRESORS). Influenza Other Respir Virus. 2022;16:1091–100.
Tatlock S, Bentley S, Arbuckle R, Abetz-Webb L, Scott J. Content validation of a caregiver diary to monitor severity and recovery of pediatric patients with respiratory syncytial virus infection. J Patient Rep Outcomes. 2022;6:48.
Medical Dictionary for Regulatory Activities. Introductory guide MedDRA (version 23.1). Geneva: International Council for Harmonisation; 2020.
Porter DP, Guo Y, Perry J, Gossage DL, Watkins TR, Chien JW, et al. Assessment of drug resistance during phase 2b clinical trials of presatovir in adults naturally infected with respiratory syncytial virus. Antimicrob Agents Chemother. 2020;64:e02312-e2319.
Pinheiro J, Bornkamp B, Glimm E, Bretz F. Model-based dose finding under model uncertainty using general parametric models. Stat Med. 2014;33:1646–61.
US Food and Drug Administration. Drug development tools: fit-for-purpose initiative. 2022. https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tools-fit-purpose-initiative. Accessed 19 Dec 2023.
European Medicines Agency. First qualification opinion on a statistical methodology for dose finding released for public consultation. 2013. https://www.ema.europa.eu/en/news/first-qualification-opinion-statistical-methodology-dose-finding-released-public-consultation. Accessed 19 Dec 2023.
DeVincenzo J, Lambkin-Williams R, Wilkinson T, Cehelsky J, Nochur S, Walsh E, et al. A randomized, double-blind, placebo-controlled study of an RNAi-based therapy directed against respiratory syncytial virus. Proc Natl Acad Sci USA. 2010;107:8800–5.
Perez A, Lively JY, Curns A, Weinberg GA, Halasa NB, Staat MA, et al. Respiratory virus surveillance among children with acute respiratory illnesses: new vaccine surveillance network, United States, 2016–2021. MMWR Morb Mortal Wkly Rep. 2022;71:1253–9.
Tuczynska M, Matthews-Kozanecka M, Baum E. Accessibility to non-COVID health services in the world during the COVID-19 pandemic: review. Front Public Health. 2021;9: 760795.
Acknowledgements
We thank the CROCuS Investigators for their contributions to the study. A list of investigators is provided in the ESM. We acknowledge Todd Lustine for contributions to the trial design and safety analyses. We also thank site personnel, patients, and caregivers for their participation in the study. Medical writing and editorial support were provided by Laura Watts, PhD, and William J. Kelley, PhD, of Lumanity Communications Inc. (Yardley, PA, USA).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
The study was sponsored by Janssen Research & Development.
Conflicts of interest/competing interests
Fernando Ferrero, Chien-Yu Lin, Kleber Luz, Tatyana Stoeva, Agnes Nemeth, Cristina Calvo, and Silvina Natalini have no conflicts of interest that are directly relevant to the content of this article. Johannes Liese received study grants for participation in the CROCuS trial. Manuel Gijón has received a public research grant from a public health institution (Instituto de Salud Carlos III, Madrid, Spain) to develop research tasks, with no conflicts of interests with the present study. Teck-Hock Toh received financial support from the study sponsor for travel to an investigator meeting prior to beginning the study. Sofie Deleu, Sarah Rusch, Leen Vijgen, and Mohamed Gamil are employees of Janssen Research & Development and may own stock or stock options. Bohang Chen is a prior employee of Janssen Research & Development and is a current employee of Bristol Myers Squibb. Beatriz López Sánchez is an employee of Janssen Research & Development under the legal entity Janssen Vaccines & Prevention B.V. Illse Leipoldt is an employee of Janssen-Cilag Pharmaceutical South Africa. Dymphy Huntjens is a prior employee of Janssen Research & Development and is a current employee of Priothera SAS and may own stock or stock options. Tristan Baguet is an employee of Janssen Research & Development. Kristi Bertzos is an employee of Janssen Global Services and holds stock options. Marita Stevens is a prior employee of Janssen Research & Development and may own stock or stock options.
Ethics approval
The final trial protocol and amendments were approved by an independent ethics committee or institutional review board at participating sites. The trial was conducted in compliance with the principles of the Declaration of Helsinki and the International Council for Harmonisation Guidelines on Good Clinical Practice.
Consent to participate
Written informed consent was provided by patients’ parents/legal guardians.
Consent for publication
Not applicable.
Availability of data and material
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access (YODA) Project site at http://yoda.yale.edu.
Code availability
Not applicable.
Authors’ contributions
FF, C-YL, JL, KL, TS, AN, MaG, CC, SN, T-HT, SD, BC, SR, BLS, LV, DH, TB, MoG, and MS participated in the conception and design of the study. Material preparation, data collection, and analyses were performed by SD, SR, BLS, IL, LV, KB, and MS. Study center monitoring and data analysis were performed by the sponsor. Medical writers, funded by the sponsor, assisted with manuscript drafting. All authors provided input on previous drafts of the manuscript, approved the final version, and vouch for the accuracy and completeness of the data.
Additional information
Bohang Chen, Dymphy Huntjens, Marita Stevens: Former employees of Janssen Research & Development.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ferrero, F., Lin, CY., Liese, J. et al. CROCuS, a Phase II Study Evaluating the Antiviral Activity, Clinical Outcomes, and Safety of Rilematovir in Children Aged ≥ 28 Days and ≤ 3 Years with Acute Respiratory Tract Infection Due to Respiratory Syncytial Virus. Pediatr Drugs 26, 411–427 (2024). https://doi.org/10.1007/s40272-024-00625-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-024-00625-x