Abstract
Objectives
There was initially insufficient understanding regarding suitable pharmacological treatment for pediatric Coronavirus Disease 2019 (COVID-19) patients. Lopinavir-ritonavir (LPV/r) was originally used for the treatment of Human Immunodeficiency Virus-1 (HIV-1) infection. It was also used in patients with severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome (MERS) with positive results. Nonetheless, results from recent randomized controlled trials and observational studies on COVID-19 patients were unfavorable. We sought to evaluate the clinical outcomes associated with early treatment with LPV/r for pediatric COVID-19 patients.
Study Design
A total of 933 COVID-19 patients aged ≤ 18 years were admitted between 21 January 2020 and 31 January 2021 in Hong Kong. Exposure was receiving LPV/r within the first two days of admission. Time to clinical improvement, hospital discharge, seroconversion and hyperinflammatory syndrome, cumulative costs, and hospital length of stay were assessed. Multivariable Cox proportional hazard and linear models were performed to estimate hazard ratios (HR) and their 95% confidence intervals (CI) of time-to-event and continuous outcomes, respectively.
Results
LPV/r users were associated with longer time to clinical improvement (HR 0.51, 95% CI 0.38–0.70; p < 0.001), hospital discharge (HR 0.51, 95% CI 0.38–0.70; p < 0.001) and seroconversion (HR 0.59, 95% CI 0.43–0.80; p < 0.001) when compared with controls. LPV/r users were also associated with prolonged hospital length of stay (6.99 days, 95% CI 6.23–7.76; p < 0.001) and higher costs at 30 days (US$11,709 vs US$8270; p < 0.001) as opposed to controls.
Conclusion
Early treatment with LPV/r for pediatric COVID-19 patients was associated with longer time to clinical improvement. Our study advocates the recommendation against LPV/r use for pediatric patients across age groups.
Similar content being viewed by others
This territory-wide retrospective observational study aimed to study the clinical outcomes of pediatric COVID-19 patients receiving early treatment with lopinavir-ritonavir (LPV/r). |
Treatment with LPV/r was associated with significantly longer time to clinical improvement, hospital discharge and longer hospital length of stay. |
Our study advocates against the use of LPV/r in pediatric age groups. |
1 Introduction
Coronavirus Disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected over 424 million people as of 23 February 2022 [1]. Although children with COVID-19 are found to exhibit milder clinical manifestations [2], rare but severe complications such as multisystem inflammatory syndrome in children (MIS-C) and infection-induced chilblains [3,4,5] may still pose a threat to the safety of these patients. MIS-C may eventually lead to or exacerbate hyperinflammatory syndrome and subsequent organ damage associated with severe COVID-19 [6, 7]. To date, there is still insufficient understanding regarding suitable pharmacological treatment for pediatric COVID-19 patients.
Together with the ongoing development of novel and specific pharmacological treatment, scientists are also trying to repurpose existing drugs which are approved for treatments of other infections owing to their known safety profile and pharmacology [8, 9]. One of the proposed medications is the cocktail therapy of lopinavir and ritonavir (LPV/r), which originally targeted Human Immunodeficiency Virus-1 (HIV-1). Lopinavir is the effective component which binds to the active site of the viral enzyme 3-chymotrypsin-like protease (3CLpro), inhibiting RNA replication and viral proliferation of HIV-1 [10, 11]. Ritonavir is used to increase the half-life of lopinavir [11, 12]. In addition, LPV/r was selected as a potential candidate for COVID-19 treatment as it was shown to have in vitro activity against severe acute respiratory syndrome coronavirus (SARS-CoV) via the inhibition of 3CLpro [11, 13, 14] and is active against Middle East respiratory syndrome-related coronavirus (MERS-CoV) [8, 13].
However, in the latest guidelines from National Institutes of Health (NIH) and World Health Organization (WHO), based on the results from randomized controlled trials (RCTs) in adult cohorts, administration of LPV/r is not recommended owing to the lack of significant clinical benefits [15, 16]. Three notable RCTs, the LOTUS trial in severe COVID-19 patients, the SOLIDARITY trial by the WHO consortium and the RECOVERY trial with only two pediatric patients out of 4859 patients all found that LPV/r was not associated with shorter time to clinical improvement and/or improved virologic outcomes [9, 17, 18]. However, contradicting results can be found in observational studies showing that LPV/r users are associated with slightly better outcomes [15, 19, 20].
With regards to the pharmacology of LPV/r on SARS-CoV-2, its efficacy in reducing SARS-CoV-2 reproduction was disputed as HIV-1 contains aspartic protease while SARS-CoV-2 contains cysteine protease [8, 21]. Additionally, as pediatric COVID-19 patients exhibit milder symptoms than adults, the potential benefits may not outweigh the possibility of adverse reactions [12, 18, 22, 23]. Moreover, results from the RCTs were inconclusive for the pediatric population as only two patients aged ≤ 18 years were included. Therefore, we conducted this retrospective observational study with the objective to evaluate the clinical outcomes associated with early treatment using LPV/r for children and adolescent patients with COVID-19.
2 Methods
2.1 Data Source and Study Population
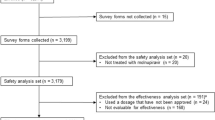
A total of 993 pediatric (aged ≤18 years) patients diagnosed with COVID-19 (defined as positive SARS-CoV-2 viral nucleic acid detected using real-time reverse transcriptase-polymerase chain reaction [RT-PCR] assay, confirmed by the Department of Health Public Health Laboratory) admitted between 21 January 2020 and 31 January 2021 in Hong Kong were identified in our cohort. In Hong Kong, all confirmed COVID-19 cases were admitted for isolation purposes. Anonymous electronic medical records of patients diagnosed with COVID-19 were extracted from the Hong Kong Hospital Authority database.
With reference to the latest version of the Interim Drug Treatment Handbook for COVID-19 patients [24], oral LPV/r was additional to interferon-based regimens, and administered to infants (≥ 14 days of age), children and adolescents with a pediatric dose of lopinavir 300 mg/m2 and ritonavir 75 mg/m2 twice daily for 14 days. Treatment would be discontinued when patients encountered contraindications, serious adverse events, or fulfilled the requirement for hospital discharge [24, 25]. Patients had to meet both of the following two criteria for hospital discharge: (i) clinical conditions improved and afebrile; (ii) with two clinical specimens of the same type (e.g., respiratory or stool) tested negative for nucleic acid of SARS- CoV-2 by RT-PCR taken at least 24 hours apart. For patients who ever tested positive with a stool specimen, two negative stool specimens collected 24 hours apart and a period of 10 days since the onset of illness; or a positive test for SARS-CoV-2 antibody (i.e., anti-receptor binding domain [anti-RBD] immunoglobin G [IgG]/Abbott SARS-CoV-2 IgG) was necessary before release from isolation [25].
2.2 Treatment Exposure and Follow-Up Period
Exposure was defined as receiving LPV/r treatment within the first two days of admission. This reduces the possibility of selection bias from the difference in date of initiation of treatment among patients and immortal time bias from the difference between admission time and treatment initiation [26,27,28]. Patients who had initiated LPV/r after 2 days of hospital admission or did not receive LPV/r at all during hospitalization were classified as the non-exposure group. Patients were observed from the day of admission until in-hospital death, hospital discharge or data cut-off date of 30 April 2021, whichever came first.
2.3 Outcome Definition
WHO clinical progression scale provided a measure of severity from 0 (non-hospitalized, non-infected case) to 10 (dead) for COVID-19 patients [29]. Our primary outcome was defined as time to clinical improvement with regards to the WHO progression scale by at least 1 point. Secondary outcomes were hospital discharge; seroconversion (a composite outcome consisting of having a cycle threshold [Ct] value of ≥ 30 or positive IgG antibody); hyperinflammatory syndrome; hospital length of stay; and cumulative medical cost. The cumulative medical costs were calculated based on the unit cost of medication and healthcare services sourced from the Hong Kong SAR Government Gazette and Hospital Authority (Supplementary Table 1, see electronic supplementary material [ESM]).
2.4 Data Analysis
Descriptive statistics of baseline characteristics between the exposure and non-exposure groups were presented with mean and standard deviation for continuous variables, and count and proportion of categorical variables.
Baseline covariates of patients included duration of LPV/r use and time from admission to LPV/r initiation, age, sex, pre-existing comorbidities, long-term medication use, laboratory parameters, clinical severity measure by the WHO clinical progression scale, and in-hospital pharmacological and non-pharmacological treatments. Pre-existing comorbidities included ADHD, allergic rhinitis, asthma, autism, chronic heart disease, chronic kidney disease, depression, diabetes mellitus, glucose-6-phosphate dehydrogenase (G6PD) deficiency, hypertension, Kawasaki disease, liver disease, malignancy, obesity, vitamin D deficiency, and Charlson’s Comorbidity Index (CCI). Concomitant medications included anticoagulants, antiplatelets, nonsteroidal anti-inflammatory drugs, and insulin. Criteria for COVID-19-associated hyperinflammatory syndrome [30] included macrophage activation, hematological dysfunction, coagulopathy, and hepatic inflammation. Laboratory parameters included were white blood cell, neutrophil, lymphocyte, platelet, lactate dehydrogenase (LDH), creatine kinase, total bilirubin, C-reactive protein (CRP), Ct value, estimated glomerular filtration rate (eGFR), alkaline phosphatase (ALP), alanine transaminase (ALT), and hemoglobin.
To minimize outcome bias due to discrepancy in baseline characteristics between the exposure and control, Inverse Probability of Treatment Weights (IPTW) using the propensity score was applied to balance covariates across treatment groups [31]. A logistic regression model was performed to calculate the propensity scores of each patient in the group and included the aforementioned covariates. After the propensity-score weighting, the balance of baseline covariates between the treatment groups was further assessed using the standardized mean difference (SMD). SMDs of ≤ 0.2 implied sufficient balance between the groups. Missing baseline covariates were addressed with Multiple Imputation by Chained Equations (MICE) and each missing value of laboratory data was imputed 20 times using other variables that may impact the outcome. Supplementary Table 2 lists the data completion rates of baseline characteristics before multiple imputation (see ESM).
Multivariable Cox proportional hazard models were performed to estimate standard hazard ratios (HR) and their 95% confidence intervals (CI) of event outcomes. In addition, time from the index date of admission to hospital discharge, and cumulative direct medical costs incurred between the groups were compared using the linear regression model following the IPTW using the propensity scores for COVID-19 survivors.
Subgroup analyses were conducted on the following: age (0–4, 5–12, and 13–18 years old), sex, and recipient of interferon-β-1b. Sensitivity analyses were also performed on three scenarios: extending the follow-up period to beyond hospital discharge; limiting the follow-up period to a maximum of 90 days; and performing the complete-case approach with the IPTW.
All statistical analyses were performed using STATA Version 16 (StataCorp LP, College Station, TX, USA). p values < 0.05 were considered statistically significant.
3 Results
3.1 Patient Cohort
Among a total of 933 patients aged ≤ 18 years who were admitted with COVID-19 between 21 January 2020 and 31 January 2021 in Hong Kong SAR, China, LPV/r was prescribed in 49 patients for its anti-viral properties. After multiple imputation and propensity score weighting, all the SMDs except for no oxygen therapy were balanced between groups with SMDs ≤ 0.2. The majority of the patients were admitted without oxygen therapy (score 4; 98%). 12 patients in the LPV/r group were also co-administered with interferon-β-1b within two days of admission. Baseline characteristics of the patients and their respective SMDs after multiple imputation and propensity score weighting are summarized in Table 1.
Overall, the median follow-up period of this patient cohort was 14 days and 29,454 person-days. The incidence rates of outcome events by exposure and control groups are presented in Supplementary Table 3 (see ESM).
3.2 Clinical Improvement, Hospital Discharge, and Seroconversion
Early treatment with LPV/r was associated with significantly longer time to clinical improvement as indicated by at least one-point score reduction on the WHO clinical progression scale (HR 0.51, 95% CI 0.38–0.70; p < 0.001), hospital discharge (HR 0.51, 95% CI 0.38–0.70; p < 0.001), seroconversion (HR 0.59, 95% CI 0.43–0.80; p < 0.001), and a longer hospital length of stay (6.99 days, 95% CI 6.23–7.76) when compared with controls (Table 2). Subgroup analyses, presented in Supplementary Table 4 (see ESM), reveal that significant overall results are mainly contributed by patients aged 13–18 years old (clinical improvement, HR 0.39, 95% CI 0.26–0.60, p < 0.001; hospital discharge, HR 0.39, 95% CI 0.26–0.60, p < 0.001; seroconversion, HR 0.47, 95% CI 0.31–0.71, p < 0.001), while sensitivity analyses (Supplementary Table 5, see ESM) are in line with the results for the main analysis. Figure 1a, b illustrate the clinical severity status and changes in WHO clinical progression scale score of LPV/r users and their control counterparts over the follow-up period (days 7, 15, and 30), respectively. A lower proportion of patients on LPV/r were discharged on days 7, 15 and 30 (Fig. 1a) and LPV/r patients had higher scores on day 15 (p < 0.001) and day 30 (p < 0.001) (Fig. 1b) than those in the control group. Kaplan-Meier survival curves for having at least 1-point clinical improvement on the WHO clinical progression scale, and seroconversion, are shown in Fig. 2.
3.3 Hyperinflammatory Syndrome
Insignificant outcomes for hyperinflammatory syndrome (HR 3.54, 95% CI 0.49–25.38) were produced for the main analysis, shown in Table 2. Sensitivity analyses were in line with the main analysis. However, the wide CI values indicate that interpretation should be conducted with caution.
3.4 Cumulative Direct Medical Costs
Figure 1c displays the average cumulative direct medical costs incurred by patients in the exposure and control groups over the 30-day follow-up period. LPV/r users incurred progressively higher costs from index date (US$744 vs US$718, p < 0.001) to day 30 (US$11,709 vs US$8270, p < 0.001) compared with their control counterparts.
4 Discussion
This study has identified a significant association between LPV/r use and longer time to clinical improvement, hospital discharge, seroconversion as well as hospital length of stay for hospitalized mild pediatric COVID-19 cases with early LPV/r use within 2 days of admission. Hyperinflammatory syndrome was implied, and LPV/r use was associated with significantly higher cumulative medical costs than control.
It is well documented that pediatric patients generally exhibit mild symptoms or are asymptomatic when infected and tend to have fewer complications [3,4,5, 32]. An epidemiological study carried out by Dong et al. reported proportions of severe cases do not exceed 11% per age group for pediatric patients aged ≤ 18 years [33], while a systematic review by de Souza et al. reported 82.3% cases were mild to moderate [34]. Results from our cohort supported this observation, with 98% of the cohort admitted with mild-to-moderate COVID-19; the need for mechanical ventilation or mortality were not reported. Additionally, biochemical profiles for pediatric patients were investigated by Bourgeois et al. in an international analysis of electronic health records, showing elevated CRP and LDH, on average, with coagulation abnormalities (D-dimer) yet normal neutrophil and lymphocyte levels [35]. These results are in line with systematic reviews carried out by de Souza et al. and Henry et al., which investigated differences in laboratory parameters between mild and severe pediatric patients as well as those of adults and pediatric patients [34, 36]. Such trends are also in line with our analysis observing elevated LDH but normal values for neutrophil and lymphocyte count at baseline.
LPV/r was considered as one of the candidates for COVID-19 treatment owing to its efficacy exhibited in HIV and potentially in MERS and SARS treatment [37,38,39,40]. Early on during the pandemic in Hong Kong, LPV/r was used as a part of triple therapy for early treatment of COVID-19, consisting of interferon-β-1b and LPV/r ± ribavirin [41]. Additional to LPV/r, dexamethasone and remdesivir have been commonly used in patients with mild-to-moderate symptoms [42,43,44,45].
Consequently, in vitro studies were carried out and showed that lopinavir displays inhibitory activities against SARS-CoV-2. 3CLpro of SARS-CoV-2 was soon realized to be 96.1% identical to the 3CLpro of SARS-CoV-1 [46]. The association between LPV/r use and clinical improvement remains controversial in observational studies usually involving adult patients. A case study in Korea reported viral load reduction and improved clinical symptoms [19], and several other studies pointed towards reduced time to negative SARS-CoV-2 RNA detection, faster resolution of fever, and the effectiveness of LPV in disease recovery [20, 47]. In contrast, a nationwide comparative analysis [48] and the only observational study examining effects of LPV/r on outcomes of hospital length of stay and viral shedding time for mild-to-moderate pediatric COVID-19 patients (LPV/r users n = 23 vs control n = 92) demonstrated longer hospital length of stay and time to negative nasopharyngeal swab test. This observational study was comparable with our study; it had a similar cohort in terms of disease severity and results from both studies shared similarities with poorer outcomes for pediatric LPV/r users.
While there was successful main protease inhibition of SARS-CoV-2 in vitro, evidence is inconclusive on clinical improvement in COVID-19 patients. It was found that LPV can bind to the main protease according to computer simulation and exert an inhibitory effect with half maximal effective concentration (EC50) of 16.4 µmol, with successful inhibition on its cytopathic activity [49]. Lopinavir consistently has a weaker inhibitory effect with SARS-CoV-1 and MERS coronavirus (MERS-CoV) when compared with HIV-1, despite successful inhibition on viral replication of all four viruses [49, 50]. However, such inhibition might not be translated to COVID-19 patients as there have been inconclusive results in clinical improvement and viral loads in the adult cohorts. This indicates a difference between in vivo and in vitro environments; for example, most in vitro methods employ bovine serum in the assay medium [51]. Experiments suggested that lopinavir has a plasma protein binding of > 98%, lowering the plasma concentration of free drug [52]. Therefore, it was hypothesized that lack of plasma protein binding in vitro might overestimate the protease inhibitory effect, explaining lack of improvement as illustrated in our cohort.
A mechanistic explanation for worse outcomes has been hypothesized to be infection-induced cytokine release and oxidative stress suppressing cytochrome P450 enzyme activity and associated gene expression [53, 54]. Moreover, ritonavir’s mechanism of action is CYP3A4 inhibition for lopinavir’s half-life extension [11]; hence, hepatic burden may be exacerbated by both inflammation and LPV/r-associated potential hepatotoxicity [55]. Our results may support this theory as elevated levels of ALP, one of the implied elevated biomarkers in COVID-19 patients with hepatocellular injury [56], were reported at baseline, perhaps indicating pre-admission SARS-CoV-2 infection-induced hepatic injury, hence potentially raising the risk for hyperinflammatory syndrome as an outcome [53, 54]. Despite this, our results for hyperinflammatory syndrome trend towards higher risk but have a wide CI, possibly due to the small number of events. These results should therefore be interpreted with caution [56].
Prior to our study, the LOTUS trial including severe adult COVID-19 patients reported that LPV/r use was not associated with time to clinical improvement and was associated with increased adverse events instead. The RECOVERY trial, which included two pediatric patients after removing the age restriction (> 18 years) from 9 May 2020, has also reported a lack of association between LPV/r use and reduction of 28-day mortality, length of stay, and risk of progressing to invasive mechanical ventilation. The SOLIDARITY trial, with an unknown number of pediatric patients, reported results that are in line with both aforementioned trials, with a joint mortality rate ratio of 1.01 (95% CI 0.91–1.13) [9, 17, 18]. Both the WHO and NIH have discouraged the use of LPV/r for COVID-19 patients owing to its lack of efficacy, with the WHO consulting seven trials containing 7429 adult participants. Hence, pediatric patients might be underrepresented by current guidelines [15, 16]. Therefore, a notable strength of our study is that it contributes to the knowledge on effectiveness of LPV/r for pediatric patients and advocates the recommendation against LPV/r use for pediatric patients across age groups.
Our study is not without its limitations. Firstly, most patients were admitted without oxygen therapy, hence this study could not account for outcomes for severe pediatric COVID-19 cases. Secondly, the exposure population of this study is very limited (n = 49), which could introduce biased results as well as difficulties in yielding significant results when comparing clinical outcomes across different age groups in subgroup analysis. Thirdly, SARS-CoV-2 viral loads were represented by Ct values in this study. Despite a good correlation, direct quantitative measurements of viral loads would have been preferable if available. Fourthly, our study could not investigate the use of LPV/r with other concomitant drugs for COVID-19 due to limited use in this cohort. Lastly, residual confounding may not be fully removed due to the observational nature of this study.
5 Conclusion
Among pediatric patients hospitalized with COVID-19, LPV/r use was associated with longer time to clinical improvement, hospital discharge, seroconversion, and hospital length of stay. A trend towards higher risk of hyperinflammatory syndrome and significantly higher cumulative medical costs than controls was observed. Accordingly, it is advised that clinicians resort to other treatment modalities for pediatric COVID-19 cases; however, studies with longer follow-up periods and larger sample sizes of different clinical severities are necessary to further elucidate the potential role of LPV/r in the deterioration of clinical outcomes.
References
World Health Organisation. WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/. Accessed 23 Feb 2022.
Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr. 2020;109(6):1088–95.
Rubens JH, Akindele NP, Tschudy MM, Sick-Samuels AC. Acute covid-19 and multisystem inflammatory syndrome in children. Bmj. 2021;372
Chua GT, Wong JSC, Lam I, et al. Clinical characteristics and transmission of COVID-19 in children and youths during 3 waves of outbreaks in Hong Kong. JAMA Netw Open. 2021;4(5):e218824–e218824.
Venturini E, Montagnani C, Garazzino S, et al. Treatment of children with COVID-19: position paper of the Italian Society of Pediatric Infectious Disease. Ital J Pediatr. 2020;46(1):1–11.
Kaushik S, Aydin SI, Derespina KR, et al. Multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection: a multi-institutional study from New York City. J Pediatr. 2020;224:24.
Hu B, Huang S, Yin L. The cytokine storm and COVID-19. J Med Virol. 2021;93(1):250–6.
Nutho B, Mahalapbutr P, Hengphasatporn K, et al. Why are lopinavir and ritonavir effective against the newly emerged coronavirus 2019? Atomistic insights into the inhibitory mechanisms. Biochemistry. 2020;59(18):1769–79.
WHO Solidarity Trial Consortium. Repurposed antiviral drugs for COVID-19—interim WHO SOLIDARITY trial results. N Engl J Med. 2021;384(6):497–511.
Sevilla-Castillo F, Roque-Reyes OJ, Romero-Lechuga F, et al. Both chloroquine and lopinavir/ritonavir are ineffective for COVID-19 treatment and combined worsen the pathology: a single-center experience with severely ill patients. BioMed Res Int. 2021;2021
Gao G, Wang A, Wang S, et al. Brief report: retrospective evaluation on the efficacy of lopinavir/ritonavir and chloroquine to treat nonsevere COVID-19 patients. J Acquir Immune Def Syndromes. 2020;85(2):239.
Maciorowski D, Idrissi SZE, Gupta Y, et al. A review of the preclinical and clinical efficacy of Remdesivir, Hydroxychloroquine, and Lopinavir-Ritonavir treatments against COVID-19. SLAS Discov Adv Sci Drug Discov. 2020;25(10):1108–22.
De Wilde AH, Jochmans D, Posthuma CC, et al. Screening of an FDA-approved compound library identifies four small-molecule inhibitors of Middle East respiratory syndrome coronavirus replication in cell culture. Antimicrob Agents Chemother. 2014;58(8):4875–84.
Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323(18):1824–36.
Lopinavir/Ritonavir and Other HIV Protease Inhibitors. Updated 11/02/2021. https://www.covid19treatmentguidelines.nih.gov/therapies/antiviral-therapy/lopinavir-ritonavir-and-other-hiv-protease-inhibitors/. Accessed 13 Aug 2021.
World Health Organization. Therapeutics and COVID-19: Living Guideline (World Health Organization). 2021.
Horby PW, Mafham M, Bell JL, et al. Lopinavir–ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2020;396(10259):1345–52.
Cao B, Wang Y, Wen D, et al. A Trial of Lopinavir–Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 2020;382(19):1787–99.
Lim J, Jeon S, Shin H-Y, et al. Case of the index patient who caused tertiary transmission of coronavirus disease 2019 in Korea: the application of lopinavir/ritonavir for the treatment of COVID-19 pneumonia monitored by quantitative RT-PCR. J Korean Med Sci. 2020;35(6)
Ye XT, Luo YL, Xia SC, et al. Clinical efficacy of lopinavir/ritonavir in the treatment of Coronavirus disease 2019. Eur Rev Med Pharmacol Sci. 2020;24(6):3390–6.
Lin L, Niu G, Zhang X. Influence of lncRNA MALAT1 on septic lung injury in mice through p38 MAPK/p65 NF-κB pathway. Eur Rev Med Pharmacol Sci. 2019;23(3):1296–304.
Shane AL, Sato AI, Kao C, et al. A pediatric infectious diseases perspective of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and novel coronavirus disease 2019 (COVID-19) in children. J Pediatr Infect Dis Soc. 2020;9(5):596–608.
Goldman DL, Aldrich ML, Hagmann SH, et al. Compassionate use of remdesivir in children with severe COVID-19. Pediatrics. 2021;147(5).
Interim Drug Treatment Handbook for COVID-19. Department of Pharmacy, Queen Mary Hospital, Hospital Authority, Hong Kong. 2021.
Updated Consensus Recommendations on Criteria for Releasing Confirmed COVID-19 Patients from Isolation (July 29, 2020) In: Scientific Committee on Emerging and Zoonotic Diseases. Centre for Health Protection, Department of Health, Hong Kong. 2020.
Gupta S, Wang W, Hayek SS, et al. Association between early treatment with tocilizumab and mortality among critically ill patients with COVID-19. JAMA Intern Med. 2021;181(1):41–51. https://doi.org/10.1001/jamainternmed.2020.6252.
Monedero P, Gea A, Castro P, et al. Early corticosteroids are associated with lower mortality in critically ill patients with COVID-19: a cohort study. Crit Care. 2021;25(1):2. https://doi.org/10.1186/s13054-020-03422-3.
Renoux C, Azoulay L, Suissa S. Biases in evaluating the safety and effectiveness of drugs for the treatment of COVID-19: designing real-world evidence studies. Am J Epidemiol. 2021;190(8):1452–6. https://doi.org/10.1093/aje/kwab028.
A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis. 2020;20(8):e192–e197. https://doi.org/10.1016/s1473-3099(20)30483-7.
Webb BJ, Peltan ID, Jensen P, et al. Clinical criteria for COVID-19-associated hyperinflammatory syndrome: a cohort study. Lancet Rheumatol. 2020;2(12):e754–63.
Austin PC. Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biometr J J Math Methods Biosci. 2009;51(1):171–84.
Chiotos K, Hayes M, Kimberlin DW, et al. Multicenter initial guidance on use of antivirals for children with coronavirus disease 2019/severe acute respiratory syndrome coronavirus 2. J Pediatr Infect Dis Soc. 2020;9(6):701–15.
Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 Among Children in China. Pediatrics. 2020;145(6):e20200702.
de Souza TH, Nadal JA, Nogueira RJ, Pereira RM, Brandão MB. Clinical manifestations of children with COVID-19: a systematic review. Pediatr Pulmonol. 2020;55(8):1892–9.
Bourgeois FT, Gutiérrez-Sacristán A, Keller MS, et al. International analysis of electronic health records of children and youth hospitalized with COVID-19 infection in 6 countries. JAMA Netw Open. 2021;4(6):e2112596–e2112596.
Henry BM, Benoit SW, de Oliveira MHS, et al. Laboratory abnormalities in children with mild and severe coronavirus disease 2019 (COVID-19): a pooled analysis and review. Clin Biochem. 2020;81:1–8.
Wood AJJMD, Flexner CMD. HIV-protease inhibitors. N Engl J Med. 1998;338(18):1281–1293.
Chandwani A, Shuter J. Lopinavir/ritonavir in the treatment of HIV-1 infection: a review. Ther Clin Risk Manag. 2008;4(5):1023–33. https://doi.org/10.2147/tcrm.s3285.
Barragan P, Podzamczer D. Lopinavir/ritonavir: a protease inhibitor for HIV-1 treatment. Expert Opin Pharmacother. 2008;9(13):2363–75. https://doi.org/10.1517/14656566.9.13.2363.
Chu C, Cheng V, Hung I, et al. Role of lopinavir/ritonavir in the treatment of SARS: initial virological and clinical findings. Thorax. 2004;59(3):252–6.
Hung IF-N, Lung K-C, Tso EY-K, et al. Triple combination of interferon beta-1b, lopinavir–ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet. 2020;395(10238):1695–1704.
Wong CKH, Lau KTK, Au ICH, Xiong X, Lau EHY, Cowling BJ. Clinical improvement, outcomes, antiviral activity, and costs associated with early treatment with remdesivir for patients with coronavirus disease 2019 (COVID-19). Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab631.
Wong CKH, Au ICH, Cheng WY, et al. Remdesivir use and risks of acute kidney injury and acute liver injury among patients hospitalized with COVID-19: a self-controlled case series study. Aliment Pharmacol Ther. 2022. https://doi.org/10.1111/apt.16894.
Wong CKH, Lau KTK, Au ICH, et al. Optimal timing of remdesivir initiation in hospitalized patients with coronavirus disease 2019 (COVID-19) administered with dexamethasone. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab728.
National Institutes of Health. Therapeutic management of hospitalized adults with COVID-19. Updated 16/12/2021. https://www.covid19treatmentguidelines.nih.gov/management/clinical-management/hospitalized-adults--therapeutic-management/. Accessed 07 Feb 2022.
Meini S, Pagotto A, Longo B, Vendramin I, Pecori D, Tascini C. Role of Lopinavir/Ritonavir in the treatment of Covid-19: a review of current evidence, guideline recommendations, and perspectives. J Clin Med. 2020;9(7):2050.
Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8(4):e21.
Lu J, Zhou A, Zhang X, et al. Safety and efficacy of oral lopinavir/ritonavir in pediatric patients with coronavirus disease: a nationwide comparative analysis. Eur Rev Med Pharmacol Sci. 2021;25(1):549–55.
Karolyi M, Omid S, Pawelka E, et al. High dose lopinavir/ritonavir does not lead to sufficient plasma levels to inhibit SARS-CoV-2 in hospitalized patients with COVID-19. Original research. Front Pharmacol. 2021. https://doi.org/10.3389/fphar.2021.704767.
Wu C-Y, Jan J-T, Ma S-H, et al. Small molecules targeting severe acute respiratory syndrome human coronavirus. Proc Natl Acad Sci. 2004;101(27):10012–7.
Boffito M, Back DJ, Blaschke TF, et al. Protein binding in antiretroviral therapies. AIDS Res Hum Retrovirus. 2003;19(9):825–35.
Croxtall JD, Perry CM. Lopinavir/Ritonavir: a review of its use in the management of HIV-1 infection. Drugs. 2010;70(14):1885–915. https://doi.org/10.2165/11204950-000000000-00000.
Aitken AE, Morgan ET. Gene-specific effects of inflammatory cytokines on cytochrome P450 2C, 2B6 and 3A4 mRNA levels in human hepatocytes. Drug Metab Dispos. 2007;35(9):1687–93. https://doi.org/10.1124/dmd.107.015511.
Cheng PY, Morgan ET. Hepatic cytochrome P450 regulation in disease states. Curr Drug Metab. 2001;2(2):165–83. https://doi.org/10.2174/1389200013338676.
Shehu AI, Lu J, Wang P, et al. Pregnane X receptor activation potentiates ritonavir hepatotoxicity. J Clin Invest. 2019;129(7):2898–903. https://doi.org/10.1172/jci128274.
Deb S, Arrighi S. Potential effects of COVID-19 on cytochrome P450-mediated drug metabolism and disposition in infected patients. Eur J Drug Metabol Pharmacokinet. 2021:1–19.
Acknowledgements
We thank the Hong Kong Hospital Authority for the data provision, and support from the Research Internship Scheme, Li Ka Shing Faculty of Medicine, University of Hong Kong
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Contributors’ Statement
Dr CKHW conceptualized, designed the study, reviewed and revised the manuscript. Mr MCHL, Miss ACYK and Miss AYCL searched literatures, drafted the initial manuscript, reviewed and revised the manuscript. Miss KTKL reviewed and revised the manuscript. Mr ICHA and Mr SHC conducted data analysis, reviewed and revised the manuscript. Miss XX, Mr EHYL and Prof. BJC reviewed and revised the manuscript. Dr MYWK provided clinical input.
Funding/Support
We received financial support from the Health and Medical Research Fund, Food and Health Bureau, Government of the Hong Kong Special Administrative Region, China (Grant no. COVID190210).
Conflict of interest
Dr Wong, Mr Low, Miss Kwok, Miss Lui, Miss Lau, Mr Au, Mr Chung, Miss Xiong, Mr Lau, Prof. Cowling and Dr Kwan have no conflicts of interest to disclose.
Ethical approval and informed consent
The study protocol was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (Reference No. UW 20-493). Given the extraordinary nature of the COVID-19 pandemic, individual patient informed consent was not required for this retrospective cohort study using anonymized data.
Data sharing statement
The data that support the findings of this study were provided by the Hong Kong Hospital Authority. Restrictions apply to the availability of these data, which were used under license for this study. Deidentified individual participant data will not be made available.
Availability of Data and Material
The data that supported the findings of this study were provided by the Hong Kong Hospital Authority but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Hong Kong Hospital Authority.
Consent for publication
All authors contributed to the interpretation of the analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Code availability
All statistical analyses were performed using STATA Version 16 (StataCorp LP, College Station, TX).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wong, C.K.H., Low, M.C.H., Kwok, A.C.Y. et al. Slower Recovery with Early Lopinavir/Ritonavir use in Pediatric COVID-19 Patients: A Retrospective Observational Study. Pediatr Drugs 24, 269–280 (2022). https://doi.org/10.1007/s40272-022-00500-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-022-00500-7