Abstract
Asenapine, administered as a twice-daily (BID) sublingual tablet, is approved in the US as monotherapy for the acute treatment of manic and mixed episodes of bipolar I disorder in children and adolescents aged 10–17 years based on the positive results of one 3-week, double-blind, placebo-controlled study; the recommended dose is 2.5–10 mg BID. Although asenapine has been studied in pediatric patients with schizophrenia, it is not approved for this indication. Asenapine is not approved for pediatric use in bipolar I disorder or schizophrenia in other major markets. To inform clinicians treating psychiatric disorders in pediatric patients, we have summarized the neuropharmacology, pharmacokinetics, clinical trial experience, and clinical use of asenapine in pediatric patients. After rapid absorption through the oral mucosa, the pharmacokinetic profile of asenapine in pediatric patients is similar to that which is observed in adult patients, indicating that the recommended adult dosage does not need to be adjusted for pediatric use. Intake of food and water should be avoided for 10 min after administration. In clinical trials, asenapine was generally safe and well tolerated in pediatric patients with bipolar I disorder and schizophrenia. Serious adverse effects were generally related to worsening of the underlying psychiatric disorder. The most common treatment-emergent adverse events (TEAEs) in both indications were sedation and somnolence. Like some other second-generation antipsychotic agents, weight gain and changes in some metabolic parameters were noted; oral effects (e.g., oral hypoesthesia, dysgeusia, paresthesia) related to sublingual administration did not typically result in treatment discontinuation and were generally transient. Extrapyramidal symptom TEAEs occurred in ≥5% of asenapine-treated patients in the acute and long-term studies in bipolar I disorder and schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Asenapine monotherapy is approved in the US for the acute treatment of manic and mixed episodes of bipolar I disorder in children and adolescents aged 10–17 years. |
Although asenapine has been studied in pediatric patients with schizophrenia, it is not approved for this indication. |
Asenapine is administered twice daily as a fast-dissolving tablet that is placed under the tongue; generally transient oral effects related to sublingual administration (e.g., oral hypoesthesia, dysgeusia, paresthesia) have been observed. |
Absolute bioavailability is markedly decreased if asenapine is swallowed, so it should not be ingested; exposure can also be reduced by food or drink, so eating and drinking should be avoided for at least 10 min after administration. |
Asenapine was generally safe and well tolerated in clinical trials of pediatric patients with bipolar I disorder or schizophrenia; sedation, somnolence, weight gain, and changes in some metabolic parameters have been observed and should be monitored. |
1 Introduction
Psychiatric disorders that are commonly treated with pharmacotherapy in adulthood often have onset in childhood or adolescence [1]. Similar to treatment recommendations for adult patients with schizophrenia or bipolar mania, practice parameters addressing the early onset of these disorders recommend the use of antipsychotic agents as a first-line treatment [2, 3]. The relative scarcity of safety and efficacy information for antipsychotic use in juveniles means that prescribers may have to rely on data from studies in adults to treat their young patients; this lack of information is concerning since antipsychotics may have effects that are developmentally dependent and differ from what is observed in adult patients [4].
Data indicate that 14–28% of adult patients with bipolar disorder experience onset of the illness before the age of 13 years, and 36–38% experience onset between the ages of 13 and 18 years [5, 6]. Early onset of bipolar disorder, which is generally associated with a delay in first treatment and a more pernicious course of illness than later onset illness, is characterized by greater comorbidity with other psychiatric disorders and substance abuse, more mood episodes, more days depressed, shorter periods of euthymia, and higher lifetime risk of suicide attempt [6, 7].
The onset of schizophrenia before the age of 13 years appears to be rare, with a prevalence of approximately 1 in 40,000 [8]. Rates of illness increase during adolescence, with the peak age of onset for schizophrenia cited as ranging from 15 to 30 years [3]. It has been reported that up to 20% of individuals with schizophrenia become ill before the age of 18 years [9], and early onset is associated with poor long-term prognosis, social deficits, and high suicidality [3, 10].
Asenapine is a novel second-generation antipsychotic that is administered twice daily (BID) as a sublingual tablet. As the only second-generation antipsychotic with this unique formulation, asenapine is available as 2.5-, 5-, and 10-mg black-cherry-flavored tablets that dissolve within seconds when placed under the tongue. Rapidly absorbed through the oral mucosa, in adult patients asenapine reaches peak plasma concentration in 30–90 min following a single 5-mg dose, and steady state is reached within 3 days of BID administration [11]. Absolute bioavailability is markedly decreased if asenapine is swallowed, so it should not be ingested; exposure can also be reduced by food or drink, so eating and drinking should be avoided for at least 10 min after administration [11].
US Food and Drug Administration (FDA) approval of asenapine monotherapy in adult patients was based on efficacy demonstrated in two 6-week, double-blind, placebo- and active-controlled studies in schizophrenia [12, 13] and two 3-week, double-blind, placebo- and active-controlled studies in manic or mixed episodes associated with bipolar I disorder [14, 15]. Maintenance efficacy was demonstrated in a 26-week relapse prevention study in schizophrenia [16] and a 26-week relapse prevention study in bipolar I disorder [17]; these studies served as the basis for subsequent indications for maintenance treatment in each disease state in adults [11]. Additional short-term and longer-term studies support the safety and efficacy of asenapine in adult patients with schizophrenia [18, 19] and bipolar I disorder [20,21,22,23]. Asenapine is also approved for the treatment of adults in the European Union (moderate to severe manic episodes associated with bipolar disorder), in Canada (as monotherapy or in combination with lithium or divalproex for manic or mixed episodes associated with bipolar I disorder), in Japan (schizophrenia), and in Australia (schizophrenia, and as monotherapy or in combination with lithium or sodium valproate for acute mania associated with bipolar I disorder and prevention of relapse of manic or mixed episodes in bipolar I disorder).
Clinicians who treat pediatric and adolescent patients with psychiatric disorders should be aware that asenapine is approved in the US as monotherapy for the acute treatment of manic and mixed episodes of bipolar I disorder in children and adolescents aged 10–17 years. Although asenapine has been studied in pediatric patients with schizophrenia, it did not separate from placebo on the primary efficacy parameter in a double-blind randomized trial [24] and is not approved for this indication. Asenapine is not approved for pediatric use in bipolar I disorder or schizophrenia in any other major market. A recent literature search using the terms asenapine, pediatric, adolescent, childhood, bipolar I disorder, and schizophrenia yielded scant results. Consequently, we reviewed and collated the available information on the neuropharmacology, pharmacokinetics, clinical trials, and clinical use of asenapine in pediatric patients to assist clinicians who treat young patients with these disorders.
2 Overview of Asenapine
2.1 Neuropharmacology
Although the mechanism of action for asenapine in schizophrenia and bipolar disorder is unknown, it is suggested to be the result of combined antagonist activity at dopamine (D2) and serotonin (5-HT2A) receptors [11]. The receptor profile of asenapine is complex, and beyond the common features of D2 and 5-HT2A receptor affinity, it is different than other second-generation antipsychotics [25]. Asenapine displays high antagonist activity for other dopamine (D1, D3, and D4), serotonin (5-HT1A, 5-HT1B, 5-HT2B, 5-HT2C, 5-HT5, 5-HT6, and 5-HT7), adrenergic (α1 and α2), and histamine (H1) receptors and moderate antagonistic affinity for the H2 receptor; it has no appreciable affinity for muscarinic receptors. This receptor binding profile may theoretically predict a low propensity for causing anticholinergic effects through low affinity at muscarinic receptors [25, 26]. Conversely, antagonism at the histamine H1 and α1-adrenergic receptors may cause sedation and H1 receptor blockade may be related to weight gain; antagonism of α1-adrenergic receptors may also be associated with cardiovascular effects [25, 26].
2.2 Pharmacokinetic Parameters
2.2.1 Pediatric Pharmacokinetic Studies
Two phase I studies investigated the pharmacokinetic profile of asenapine in pediatric patients [27, 28]; a summary of findings is presented in Table 1. Data from these two studies showed that the pharmacokinetic profile of asenapine in pediatric patients is similar to that in adult patients in other studies [11, 25, 29]. This important clinical characteristic suggests that the recommended adult dosage of asenapine can be given to pediatric and adolescent patients without adjustment [11].
In the first study, 40 adolescent patients (12–17 years of age) with a history of schizophrenia, bipolar disorder, or any condition for which chronic use of antipsychotic medication was warranted received 10 days of double-blind asenapine (1, 3, 5, or 10 mg BID) or matching placebo. Results indicated that asenapine exposure (maximum concentration [C max] and area under the concentration–time curve, 0–12 h [AUC0–12]) tended to increase with increasing doses from 1 mg BID up to and including 5 mg BID, although the increase was slightly less than dose proportional [28]. Lower asenapine exposure was observed in the 10-mg BID dose group than in the 5-mg BID dose group. Although the exact reason for this is unclear, it is possible that patients in this group swallowed a greater portion of the administered dose. Namely, asenapine undergoes significant first-pass metabolism when given orally; first-pass metabolism is minimized when asenapine is administered sublingually and higher plasma asenapine concentrations are achieved [25]. For asenapine metabolites such as desmethylasenapine, exposure (AUC) following either route of administration is expected to be similar. As such, the finding that lower C max and AUC0–12 values for asenapine, but not for desmethylasenapine, were observed in the 10-mg dose group may support the oral ingestion hypothesis. Rapid absorption and an initial rapid decline in plasma concentrations was followed by a slower elimination phase; time to maximum asenapine plasma concentration was ~1 h (range 0.7–1.3 h) and steady state was attained in ~8 days (data on file, Allergan). Multiple sublingual doses of asenapine were safe and well tolerated in adolescent subjects with a disorder that warranted the use of antipsychotic medication [28].
To further investigate the pharmacokinetics of asenapine 10 mg BID in subjects aged 12–17 years and to evaluate asenapine pharmacokinetics in younger subjects (10–11 years of age), a second study was conducted [28]. Thirty pediatric patients (10–17 years of age) with a documented history of psychiatric disorder, including bipolar disorder, schizophrenia, autism, and conduct disorder, participated in this 7-, 8-, or 12-day open-label, sequential group, rising multiple-dose study [27]. Multiple sublingual doses of asenapine 2.5 mg BID, 5 mg BID, or escalating doses up to 10 mg BID were administered to the 10- to 11-year-old subjects; after receiving 5 mg BID on day 1, multiple sublingual doses of asenapine 10 mg BID were administered to the 12- to 17-year-old subjects. Results indicated that asenapine was rapidly absorbed (time to maximum concentration [T max] ~1 h) and had an apparent terminal half-life of ~20 h. At the 10-mg BID dose, exposure to asenapine was similar across the age groups from 10–17 years, but maximum asenapine concentrations were ~30% higher in 10- to 11-year-old subjects compared with the older age group. Asenapine was generally safe and well tolerated in pediatric subjects. Of note, eight events of dystonia were reported in seven subjects (five events in the 10- to 11-year age group receiving 5 mg BID; three events in the 12- to 17-year age group receiving 10 mg BID). As such, a low initial dose (2.5 mg BID) followed by a short up-titration schedule became the recommended dosing schedule to circumvent initial sensitivity to asenapine treatment [11].
Of note in adult subjects, a dosage increase from 5 to 10 mg BID results in less than linear increases in the extent of exposure and C max (1.7 times) [11]. Overall, data from the two designated pediatric studies showed that the pharmacokinetic profile of asenapine in pediatric patients is similar to that in adult patients in other studies [11, 25, 29]. This is an important clinical characteristic that suggests that the recommended adult dosage of asenapine can be given to pediatric and adolescent patients without adjustment [11].
2.2.2 Bioavailability and Metabolism
Given its sublingual method of administration, the bioavailability of asenapine is dependent on various factors including the amount of saliva in the mouth, food and water intake, and dissolving versus ingestion of the tablet. It is particularly important to note that, in adults, the absolute bioavailability of asenapine decreases markedly (to <2%) if it is swallowed [11]; bioavailability can also be reduced by ~12–20% with the intake of water within 2–5 min after administration [25, 30]. Additionally, a high-fat meal immediately before sublingual administration in healthy adults reduced asenapine exposure by 20%; and, when food was given 4 h after asenapine was administered, AUC was reduced by 13% [31]. These effects are likely due to increased clearance of asenapine related to increased hepatic blood flow following food intake and are expected to be similar in pediatric patients. As such, adult and pediatric patients should avoid drinking and eating for 10 min after asenapine is administered [11].
Although asenapine has multiple metabolites, none are active or considered clinically relevant, with asenapine activity predominantly due to the parent drug [25]. The primary metabolic pathways for asenapine are direct glucuronidation by uridine 5′-diphospho-glucuronosyltransferase 1A4 (UGT1A4) and oxidative metabolism by cytochrome P450 (CYP450) isoenzymes (predominantly CYP1A2) [11]. Asenapine is rapidly distributed, has a large volume of distribution, and is highly bound to plasma proteins (95%) [11, 32]. Elimination of asenapine and its metabolites occurs approximately equally via hepatic and renal routes [30].
2.2.3 Population Pharmacokinetics
The population pharmacokinetics of asenapine in pediatric patients has been modeled to determine whether dose adjustments based on differences in age or weight are warranted [28]. Pediatric patient data from the two dedicated phase I pediatric pharmacokinetic studies, one phase III acute study in bipolar I disorder [33], and one phase III acute study in schizophrenia were included in the model (2451 samples from 561 pediatric patients) [24]. The final population pharmacokinetic model was described as a two-compartment model with first-order absorption and first-order elimination. Building on an existing population pharmacokinetic model in adults [34], analyses were conducted using age, body mass index (BMI), gender, race, and dose as covariates. Simulations were performed to determine the effect of covariates on asenapine pharmacokinetics and compare steady-state exposure between pediatric and adult subjects. Results showed no statistically significant differences or clinically meaningful changes in asenapine exposure for age, BMI, race, and gender. Predictive checks indicated that the model adequately described the observed asenapine data and indicated that no dose adjustments are required based on the covariates tested.
2.2.4 Drug–Drug Interactions and Contraindications
Asenapine is a substrate for UGT1A4, CYP1A2, and to a lesser extent CYP3A4 and CYP2D6; it is a weak inhibitor of CYP2D6 [25]. Asenapine does not cause induction of CYP1A2 or CYP3A4. The dose of paroxetine (CYP2D6 substrate and inhibitor) should be reduced by half when it is coadministered with asenapine. When coadministered with a strong CYP1A2 inhibitor (e.g., fluvoxamine), asenapine exposure may be increased, and a dosage reduction may be necessary based on clinical response. However, no asenapine dosage adjustments are required if asenapine is concomitantly administered with imipramine (CYP1A2/2C19/3A4 inhibitor), cimetidine (CYP3A4/2D6/1A2 inhibitor), valproate, lithium, or a CYP34A inducer (e.g., carbamazepine, phenytoin, rifampin) [11]. Asenapine is contraindicated for patients with severe hepatic impairment because exposure was more than 7-fold greater in these patients than in patients with normal hepatic function; however, no dose adjustment is needed in patients with mild or moderate hepatic impairment or in patients with renal impairment [11].
3 Pediatric Clinical Trial Experience
Asenapine has been studied in pediatric and adolescent patients with manic and mixed episodes associated with bipolar I disorder and schizophrenia (paranoid, disorganized, or undifferentiated subtype) (Table 2).
3.1 Bipolar I Disorder
3.1.1 Acute Study
Asenapine was approved for use in pediatric patients with bipolar I disorder based on efficacy and safety demonstrated in one short-term study (ClinicalTrials.gov: NCT01244815) [33]; long-term safety has also been investigated in a 50-week, open-label extension trial (NCT01349907) [35]. The short-term study was a 3-week, double-blind, placebo-controlled, parallel-group trial in pediatric patients with a current manic or mixed episode, with or without psychotic features, associated with bipolar I disorder. Patients were randomized (1:1:1:1) to placebo or asenapine 2.5 mg BID, 5 mg BID, or 10 mg BID; the primary and secondary efficacy measures were change from baseline to day 21 in Young Mania Rating Scale (YMRS) [36] total score and Clinical Global Impressions-Bipolar Version (CGI-BP) [37], respectively.
Study completion was similar among groups (placebo 86.1%; asenapine: 2.5 mg BID 84.6%, 5 mg BID 88.9%, 10 mg BID 87.9%); adverse events (AEs) were the most common reason for discontinuation in each group (placebo 4.0%; asenapine: 2.5 mg BID 6.7%, 5 mg BID 5.1%, 10 mg BID 5.1%). Statistically significant improvement in manic symptoms was demonstrated by the least squares mean difference (LSMD) and associated 95% confidence interval (CI) in YMRS total score at day 21 for each dose of asenapine versus placebo (LSMD [95% CI]: 2.5 mg BID −3.2 [−5.6 to −0.8], p = 0.008; 5 mg BID −5.3 [−7.7 to −2.9], p < 0.001; 10 mg BID −6.2 [−8.6 to −3.8], p < 0.001). The odds ratio (OR) and associated 95% CI for YMRS response (50% total score improvement from baseline) was statistically significant in favor of asenapine versus placebo across the dose groups (asenapine: 2.5 mg BID 1.9 [1.0 to 3.4], p = 0.042, number needed to treat [NNT] 8; 5 mg BID 3.2 [1.7 to 5.8], p < 0.001, NNT 4; 10 mg BID 2.9 [1.6 to 5.3], p < 0.001, NNT 5). Similarly, a greater reduction in severity of illness was shown by statistically significant LSMDs versus placebo in change from CGI-BP baseline for each asenapine group (2.5 mg BID −0.6 [−0.9 to −0.3], p < 0.001; 5 mg BID −0.8 [−1.0 to −0.5], p < 0.001; 10 mg BID −0.7 [−1.0 to −0.4], p < 0.001).
Asenapine was generally safe and well tolerated in pediatric patients who participated in the study. No deaths and few serious adverse events (SAEs) occurred (placebo 3 [3.0%]; asenapine: 2.5 mg BID 0 [0%], 5 mg BID 2 [2.0%], 10 mg BID 2 [2.0%]); all SAEs were related to psychiatric disorders (worsening of bipolar 1 disorder/bipolar disorder [2 placebo patients, 1 asenapine 5.0-mg BID patient, 1 asenapine 10.0-mg BID patient], mania [1 asenapine 5.0-mg BID patient], suicidal behavior and suicidal ideation [2 events in 1 placebo patient], suicide attempt [1 asenapine 10.0-mg BID patient]). AEs occurred with greater frequency in the asenapine groups (2.5 mg BID 76.0%, 5 mg BID 72.7%, 10 mg BID 86.9%) than in the placebo group (55.4%). Some AEs were predefined as events of special interest; of these AEs, incidences of oral hypoesthesia/dysgeusia combined and somnolence/sedation/hypersomnia combined were significantly higher for all three asenapine treatment groups compared with the placebo treatment group (p < 0.05). The incidence of dizziness was greater in the 5-mg BID asenapine treatment group compared with the placebo group (p < 0.05). Of potential clinical consequence, body weight increase ≥7% from baseline was significantly higher in patients in each asenapine treatment group (2.5 mg BID 12.0%, 5 mg BID 8.9%, 10 mg BID 8.0%) compared with patients in the placebo treatment group (1.1%) (p < 0.05 for each group). There were no significant differences between the asenapine and placebo groups for extrapyramidal symptoms (EPS) defined by the narrow risk set, which included akathisia, dyskinesia, dystonia, and Parkinson-like events; similarly, no significant differences between groups were observed for akathisia or insomnia.
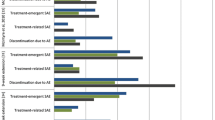
Treatment-emergent AEs (TEAEs) that occurred at an incidence ≥5% and twice the rate of placebo in all three asenapine groups were somnolence, sedation, oral hypoesthesia, oral paresthesia, and increased appetite. The oral TEAEs, which are related to the local anesthetic properties of the sublingual formulation of asenapine, are generally transient and only caused treatment discontinuation in one patient (paresthesia in the 2.5-mg group). Treatment-emergent EPS were reported as AEs for three (3.0%) placebo-treated patients and six (5.8%), five (5.1%), and six (6.1%) asenapine-treated patients in the 2.5-, 5-, and 10-mg BID dose groups, respectively; these AEs were considered mild to moderate in intensity in all but one patient (asenapine 2.5 mg BID: severe akathisia resulting in discontinuation).
Larger mean increases in weight, BMI, fasting cholesterol, triglycerides, fasting glucose, and fasting insulin were seen in asenapine- versus placebo-treated patients (Table 3). A potential dose–response relationship with asenapine was observed for increases in aspartate aminotransferase and alanine aminotransferase. Insulin level shifts >1.2 times the upper limit of normal occurred in greater percentages of asenapine-treated patients (2.5 mg BID 31.8%, 5 mg BID 32.2%, 10 mg BID 24.4%) than in placebo-treated patients (17.7%), suggesting a treatment-related effect.
Suicidal ideation assessed by the Columbia Suicide Severity Rating Scale (C-SSRS) [38] was reported in five (5.0%) placebo patients and five (4.8%), six (6.1%), and eight (8.1%) asenapine-treated patients in the 2.5-, 5-, and 10-mg BID groups, respectively; suicidal behavior was reported by two patients (1 placebo and 1 asenapine 10 mg BID). TEAEs of suicidal ideation were reported in nine patients (1 placebo, 4 asenapine 2.5 mg BID, 1 asenapine 5 mg BID, 3 asenapine 10 mg BID); each TEAE had a corresponding positive C-SSRS response. One SAE of suicidal behavior was reported (placebo patient; discontinued); one suicide attempt, which did not result in study discontinuation and was not considered related to the study drug, was reported in a patient receiving asenapine 10 mg BID.
3.1.2 Long-Term Safety Study
Patients who completed the acute study could enroll in a flexible-dose (2.5–10 mg BID), 50-week, open-label extension study [35]. Although the primary objective of this trial was to assess the long-term safety and tolerability of asenapine, efficacy outcomes were collected, including change from open-label baseline on the YMRS and CGI-BP. Of the 350 patients who completed the acute trial, 322 (92.0%) patients entered the open-label extension and were treated with asenapine; 321 patients were included in the analyses, of whom 80 had been treated with placebo (placebo/asenapine) and 241 had been treated with asenapine (asenapine/asenapine) in the acute trial. A total of 181 (56.4%) patients prematurely discontinued from the study; the most common reasons for discontinuation were AEs (15.0%), nonadherence to the study protocol (14.3%), and withdrawal of consent (11.8%). Overall asenapine exposure ranged from 2 to 380 days, with a mean duration of treatment of 187 days. The mean average daily dose was 12.8 mg for placebo/asenapine patients and 14.1 mg for asenapine/asenapine patients.
No deaths occurred during the trial; SAEs were reported in 22 (6.9%) patients. Most SAEs belonged to the psychiatric disorders class, including suicidal ideation, aggression, bipolar disorder, depression, and agitation. SAEs resulted in the discontinuation of 13 (4.0%) patients (aggression [2 patients], suicidal ideation [3 patients], worsening of attention-deficit/hyperactivity disorder [ADHD], agitation, anxiety, worsening of bipolar disorder, worsening of depression, dystonia, intentional overdose, and suicidal behavior [1 patient each]). Few SAEs were considered by the investigator to be possibly or probably related to treatment (depression/suicidal ideation [1 patient]; swollen tongue [1 patient]; hypersensitivity to asenapine [1 patient]; dystonia [1 patient]).
TEAEs were reported in 83.2% of patients; the most common TEAEs leading to discontinuation were somnolence (1.9%), sedation (1.2%), and fatigue (1.2%). The most commonly reported TEAEs were somnolence (26.8%), weight gain (18.1%), sedation (15.9%), and headache (12.8%); these TEAEs, in addition to dizziness and oral hypoesthesia, occurred more frequently in placebo/asenapine patients than in asenapine/asenapine patients. TEAEs of special interest were also assessed; most of these events also occurred with greater frequency in the placebo/asenapine group versus the asenapine/asenapine group (akathisia 3.8% vs 2.9%; dizziness 11.3% vs 2.5%; oral hypoesthesia/dysgeusia combined 18.8% vs 3.7%; insomnia 2.5% vs 2.5%; EPS [narrow risk set] 7.5% vs 5.8%; somnolence/hypersomnia/sedation combined 60.0% vs 36.5%; weight gain ≥7% from baseline to endpoint 37.3% vs 34.0%). All TEAEs reported for EPS (narrow) were not serious and considered mild or moderate in severity; akathisia led to one treatment discontinuation.
No clinically meaningful changes were noted in the prespecified laboratory parameters of interest (Table 4). Overall mean weight increase from baseline to endpoint was 3.5 kg over a mean duration of approximately 27 weeks of treatment. There were no reported TEAEs of specific hyperglycemia or new-onset diabetes; however, when the broad definition of hyperglycemia/new-onset diabetes was applied (i.e., increased weight, increased appetite, increased blood glucose, central obesity, hyperlipidemia, and loss of consciousness), 73 (22.7%) patients reported TEAEs. There were also two TEAEs of increased blood glucose and six events of increased blood insulin, all of which were considered mild or moderate in intensity. The post-baseline criteria for new-onset metabolic syndrome were met by 18 patients during the extension study; 10 patients who met metabolic syndrome criteria at baseline did not meet the criteria at endpoint and 12 patients met the criteria at both baseline and endpoint.
No suicidal ideation or behavior based on C-SSRS responses was reported for the 295 (91.9%) patients with data (one patient did not have C-SSRS data). Most suicidal ideation was reported as passive or nonspecific ideation; eight patients reported self-injurious behavior without suicidal intent.
Although assessing safety was the primary objective of this extension study, descriptive statistics suggested that improvement in mania was maintained over the course of the extension trial; week 26 was used for efficacy analyses due to limited available week-50 data because of a study protocol amendment. Mean change from open-label baseline to week 26 in YMRS total score was −6.9 points in the total treatment group (observed cases); a greater magnitude of change was seen in the placebo/asenapine group (−13.0 points) than in the asenapine/asenapine group (−4.9 points). Mean change in CGI-BP severity overall score was similar among all treatment groups at week 26 (total treatment group −1.2; placebo/asenapine group −1.8; asenapine/asenapine group −0.9), further suggesting that the effectiveness of asenapine was maintained over the course of treatment.
3.2 Schizophrenia
3.2.1 Acute Study
The efficacy and safety of asenapine in adolescents with schizophrenia (12–17 years of age) were evaluated in an 8-week randomized, double-blind, placebo-controlled trial (NCT01190254) [24]. In the acute study, patients were randomized (1:1:1) to placebo (n = 102), asenapine 2.5 mg BID (n = 98), or asenapine 5 mg BID (n = 106); similar percentages of patients across treatment groups completed the study (placebo 79%; asenapine: 2.5 mg BID 83%, 5 mg BID 79%). The most common reasons for study discontinuation in the 2.5-mg BID and 5-mg BID asenapine groups, respectively, were AEs (6.1% and 7.5%), withdrawal of consent (5.1% and 6.6%), and treatment failure (4.1% and 4.7%).
Although change from baseline to week 8 in Positive and Negative Syndrome Scale (PANSS) [39] total score was numerically greater for asenapine-treated patients compared with placebo-treated patients, the LSMD (95% CI) was not statistically significant for either asenapine dose versus placebo (2.5 mg BID −4.8 [−9.9 to 0.4], p = 0.070, 5 mg BID −5.6 [−10.7 to −0.5], p = 0.064). Some differences in favor of asenapine over placebo were observed on exploratory secondary endpoints including change from baseline in the Clinical Global Impressions–Severity (CGI–S) scale (asenapine 5 mg BID: LSMD [95% CI] −0.3 [−0.6 to −0.0], p = 0.024) and PANSS response, defined as 30% improvement from baseline (placebo 36%; asenapine: 2.5 mg BID 50%, p = 0.028 and 5 mg BID 49%, p = 0.048).
No deaths occurred during the study; the incidence of SAEs was low and similar across treatment groups (placebo 2.9%; asenapine: 2.5 mg BID 3.1%, 5 mg BID 2.8%), with most events related to worsening of schizophrenia. The incidence of TEAEs was higher in the asenapine groups (2.5 mg BID 62.2%, 5 mg BID 67.0%) than in the placebo group (47.1%). AEs resulted in the discontinuation of six patients in the asenapine 2.5-mg BID group (schizophrenia, agitation, depression, auditory hallucination, somnolence, pneumonia [1 patient each]) and eight patients in the 5-mg BID group (worsening schizophrenia [3 patients], insomnia and akathisia, dysgeusia, sedation, polycythemia, abnormal alanine aminotransferase [1 patient each]). The most common TEAEs overall were nervous system events (placebo 13.7%; asenapine: 2.5 mg BID 36.7%, 5 mg BID 48.1%); somnolence and sedation, respectively, occurred in 6.9% and 2.0% of placebo patients, 20.4% and 4.1% of asenapine 2.5-mg BID patients, and 17.0% and 11.3% of asenapine 5-mg BID patients. Oral hypoesthesia occurred more than twice as frequently in asenapine patients (2.5 mg BID 5.1% and 5 mg BID 4.7%) than in placebo patients (1.0%). Predefined AEs of interest that occurred significantly more frequently in at least one asenapine group versus the placebo group were akathisia (placebo 1.0%, asenapine 5 mg BID 6.6%, p < 0.05), dizziness (placebo 1.0%, asenapine 2.5 mg BID 7.1%, p < 0.05), combined somnolence/sedation/hypersomnia (placebo 8.8%, asenapine 2.5 mg BID 24.5%, asenapine 5 mg BID 29.2%, p < 0.05 each), and weight increase ≥7% (placebo 3.1%, asenapine 2.5 mg BID 9.5%, asenapine 5 mg BID 10.1%, p < 0.05 each). AEs likely to be associated with EPS occurred in more asenapine-treated patients (2.5 mg BID 5 [5.1%], 5 mg BID 11 [10.4%]) than placebo-treated patients (4 [3.9%]), but the difference was not statistically significant (p ≥ 0.05).
There were no noteworthy differences between treatment groups in fasting cholesterol, fasting glucose, fasting triglycerides, or HbA1c (Table 5). Mean weight increase was 0.1 kg in the placebo group; in the asenapine 2.5- and 5-mg BID groups, weight increase was 1.3 and 1.4 kg, respectively. Using the hyperglycemia/new-onset diabetes (broad) criteria, potential new-onset diabetes was reported in four (4%) placebo patients, seven (7%) asenapine 2.5-mg BID patients, and seven (7%) asenapine 5-mg BID patients; new-onset metabolic syndrome was reported by one patient in the asenapine 2.5-mg BID group and two patients in the 5-mg BID group. Mean change in laboratory values showed a potential dose response for asenapine in fasting insulin. Mean changes in prolactin were similar among groups; however, prolactin levels meeting the predefined limit of change for a high value (≥1.1 times the upper limit of normal) were more common with asenapine (2.5 mg BID 23%, 5 mg BID 19%) than placebo (13%).
3.2.2 Long-Term Safety Study
Long-term safety and tolerability were assessed in adolescent patients who completed the 8-week acute trial in schizophrenia and continued in a 26-week, open-label, flexible-dose (2.5–5 mg BID) extension trial (NCT01190267) [24]. Although safety was the primary focus of the long-term study, exploratory efficacy findings were also collected. A total of 196 patients participated in the extension study; 62 of these patients had received placebo in the acute study (placebo/asenapine) and 134 patients had received asenapine (asenapine/asenapine). Discontinuations were recorded for 9 (14.5%) placebo/asenapine patients and 32 (23.9%) asenapine/asenapine patients; AEs were the most common reason for discontinuation in both groups (6.5% and 4.5%, respectively; four events were considered SAEs). The mean duration of treatment in the open-label extension was 171 days for placebo/asenapine patients and 163 days for the asenapine/asenapine patients; the mean average daily dose was 9.8 mg for both groups.
One death, which resulted from a fall from a sixth-floor window, occurred in a placebo/asenapine patient; it was determined by the investigator and the patient’s family to be accidental and not related to the study drug. SAEs, including the death, were reported for seven (4%) patients (2 placebo/asenapine, 5 asenapine/asenapine). Six patients were hospitalized due to worsening psychiatric disorders (1 placebo/asenapine patient [aggression and anxiety]; 5 asenapine/asenapine patients [3 with worsening of schizophrenia, 1 with aggression, 1 with agitation]). Consistent with findings from the acute study, somnolence/hypersomnia/sedation combined was the most common TEAE of interest in longer-term treatment (21.4%). Except for the TEAE of weight gain ≥7%, all other TEAEs of interest were reported with greater frequency in placebo/asenapine patients versus asenapine/asenapine patients (akathisia 3.2% vs 1.5%; dizziness 4.8% vs 2.2%; oral hypoesthesia/dysgeusia combined 9.7% vs 0.7%; insomnia 4.8% vs 3.7%; EPS [narrow risk set] 9.7% vs 2.2%; somnolence/hypersomnia/sedation combined 27.4% vs 18.4%; weight gain ≥7% 12.9% vs 14.9%). Somnolence, the most common TEAE in acute treatment, occurred with greater frequency in placebo/asenapine patients (22.6%) than in asenapine/asenapine patients (11.2%); sedation occurred in 5.1% of patients overall (placebo/asenapine 3.2%; asenapine/asenapine 6.0%). Oral hypoesthesia also occurred with greater frequency in placebo/asenapine patients (8.1%) than in asenapine/asenapine patients (0.7%), suggesting a transitory effect.
Mean changes in metabolic parameters were generally modest (Table 6). Mean weight increase was 1.6 kg for patients in the placebo/asenapine group and 1.0 kg for the asenapine/asenapine group. New-onset hyperglycemia/diabetes (broad) occurred in eight (4%) patients, five of whom also met the weight gain ≥7% criterion (asenapine/asenapine group). New-onset metabolic syndrome was also observed in seven patients (2 placebo/asenapine, 5 asenapine/asenapine). Mean changes in prolactin levels during open-label treatment were small; however, prolactin increases ≥1.1 times the upper limit of normal occurred in 32% of placebo/asenapine patients and 31% of asenapine/asenapine patients.
C-SSRS–assessed suicidal ideation was recorded in eight (4%) patients during open-label treatment; none of the events was associated with intent or a formal plan, nor were suicidal behaviors recorded. TEAEs of suicidal ideation were reported for three (1.5%) of these events, and parental consent was withdrawn for six subjects with suicidal ideation.
Numerical improvements in PANSS total and CGI–S scores that were observed in the acute phase of the study were maintained during open-label treatment, suggesting that some treatment effect persisted over the course of the long-term study. From the acute baseline to the extension endpoint, mean change in PANSS total score was −36.7 points for asenapine/asenapine patients and −34.4 points for placebo/asenapine patients. Of the 103 patients who were PANSS responders at the end of double-blind treatment and continued into extension treatment, 79% of patients (placebo/asenapine 76% and asenapine/asenapine 80%) maintained response.
3.3 Asenapine Subgroup and Post Hoc Analyses
Although results of subgroup and post hoc analyses should be interpreted with caution due to inherent limitations associated with this type of analysis, exploratory information about a drug can be informative for clinicians. For example, in subgroup analyses from the acute asenapine bipolar study in pediatric patients [33], the efficacy of asenapine versus placebo (YMRS total score change from baseline to day 21) was not significantly different between patients with and without ADHD, which was the most common comorbid Axis I disorder in the study (54.6% of patients), and between patients with and without concomitant stimulant use. Additionally, efficacy did not differ significantly with respect to patient gender or for patients with bipolar disorder onset before or after the age of 11 years [33]. No noticeable between-group differences in TEAEs were reported.
In post hoc analyses conducted on data from the acute bipolar study, patient body weight and BMI did not strongly influence the efficacy of asenapine; as such, adjusting for body weight or BMI is unlikely to be an effective dosing strategy in adolescent patients [40]. Additional analyses showed that although asenapine-treated patients had significantly greater increases in body weight and BMI compared with placebo-treated patients, weight increases were only slightly greater in asenapine-treated patients with baseline BMI percentiles above the median (1.4–2.2 kg) than in patients with BMI percentiles below the median (1.4–1.7 kg) across the dose range. This suggests that weight gain in pediatric patients treated with asenapine was not substantively correlated to baseline BMI [41]. Asenapine has also been found to be generally effective in pediatric patients with bipolar disorder regardless of the number of previous manic episodes; small sample sizes in these analyses precluded definitive conclusions about differences by dose [42]. Finally, asenapine appeared to be generally effective in subsets of patients with manic episodes as well as in patients with mixed episodes as shown by significantly greater improvements in YMRS total score for asenapine-treated patients compared with placebo-treated patients [43].
4 Dosing and Administration
For bipolar mania monotherapy in pediatric patients aged 10–17 years, the recommended dose is 2.5–10 mg BID, which may be adjusted based on individual response and tolerability [11]. As discussed previously, since initial sensitivity to asenapine and the occurrence of dystonia in some pediatric patients has been noted, a short up-titration period is recommended when treatment is initiated. After starting treatment with the recommended 2.5 mg BID dose, the dose may be increased to 5 mg BID after 3 days and to 10 mg BID after an additional 3 days. Drinking and eating should be avoided for 10 min after asenapine is administered since this can remove drug from the oral cavity and prevent further mucosal absorption [11]. The safety of doses >10 mg BID has not been evaluated in clinical trials; safety and efficacy have not been evaluated in patients with bipolar disorder under the age of 10 years or in patients with schizophrenia under the age of 12 years.
5 Using Asenapine in Pediatric Patients
Asenapine monotherapy is FDA approved for the treatment of bipolar mania in adolescent patients aged 10–17 years; the recommended dosage is 2.5–10 mg BID (Table 7). Asenapine has also been studied in pediatric patients with schizophrenia, but it is not approved for this indication. Asenapine, with its unique sublingual formulation, is absorbed through the oral mucosa when a tablet placed under the tongue completely dissolves, which occurs within seconds. In pediatric patients, sublingual administration may be considered particularly advantageous since difficulty swallowing a pill may make conventional oral tablets less acceptable [44]. Complete instructions for sublingual administration are available in the prescribing information (Table 7) [11]. Patients should be informed that numbness or tingling of the mouth or throat may occur directly after asenapine administration and that these sensations usually resolve within 1 h.
Although swallowing an asenapine tablet is difficult to do because it immediately dissolves under the tongue, absolute bioavailability is markedly decreased if asenapine is swallowed, so it should not be ingested [25]. Asenapine exposure can also be reduced by food or drink, so eating and drinking should be avoided for at least 10 min after administration. Additionally, consumption of a high-fat meal immediately prior to sublingual administration of asenapine has been shown to reduce drug exposure by 20%. Although there is no need to adjust the recommended adult dosage when asenapine is used in pediatric patients, young patients may be more sensitive to dystonia when asenapine is initiated, so a short up-titration is recommended in this population.
Asenapine was generally safe and well tolerated in clinical trials of young patients with bipolar I disorder and schizophrenia. Serious adverse effects were generally related to worsening of the underlying psychiatric disorder, including bipolar disorder, schizophrenia, suicidal ideation, aggression, and agitation. Suicidal ideation was noted in acute and long-term asenapine studies, although most events occurred in patients with a history of suicidal ideation and no deaths from suicide were reported in any asenapine study. Given this vulnerable patient population, the high risk for relapse, and the high suicide attempt rate in young patients with bipolar disorder and schizophrenia [2, 45], close monitoring for worsening of the psychiatric condition and prompt response to signs of suicidality is imperative.
Somnolence and sedation are commonly reported with asenapine. Although antipsychotic-related sedating effects may diminish over time in many patients, sedation can become a persistent issue that affects quality of life for a substantial proportion of patients [46]. Since persistent somnolence and sedation may impair academic and social functioning, clinicians should be aware that these effects may be treatment-limiting in some young patients. Oral effects (hypoesthesia and dysgeusia), which are unique to asenapine and related to sublingual administration, do not typically result in treatment discontinuation and appear to be transient. Additionally, the risk of antipsychotic-related EPS in young patients requires special attention from clinicians when any antipsychotic agent is prescribed. As expected, the incidence of EPS was greater in asenapine- than in placebo-treated patients in pediatric clinical trials, although EPS-related effects were generally considered mild to moderate and resulted in few treatment discontinuations.
Finally, elevations in weight and BMI are commonly seen in young patients treated with a second-generation antipsychotic, although metabolic effects may vary [47]. Weight gain in asenapine-treated patients was accompanied by some metabolic changes, indicating that baseline values for lipid levels, BMI, and glucose levels should be established and regularly monitored during treatment. Counseling in healthy eating and lifestyle should accompany metabolic monitoring to encourage patient involvement in their treatment and overall health.
6 Conclusion
Asenapine is a unique sublingual second-generation antipsychotic that is approved in the US for use in patients with bipolar mania who are 10–17 years of age. In the acute bipolar I disorder trial, improvement in mania was seen for three BID doses of asenapine (2.5, 5, 10 mg) versus placebo. Although results of the acute schizophrenia trial were not robust enough to establish efficacy for asenapine in schizophrenia, valuable information was added to the drug’s safety profile in pediatric patients. Asenapine was generally well tolerated in acute and longer-term treatment of bipolar I disorder and schizophrenia; safety findings were generally consistent across indications, with potentially clinically significant changes in some metabolic parameters and a high incidence of sedation noted. As with any antipsychotic administered to pediatric patients, the use of asenapine should be closely monitored for adequate treatment response and antipsychotic-induced adverse effects.
References
Correll CU, Kratochvil CJ, March JS. Developments in pediatric psychopharmacology: focus on stimulants, antidepressants, and antipsychotics. J Clin Psychiatry. 2011;72(5):655–70.
McClellan J, Kowatch R, Findling RL, Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(1):107–25.
McClellan J, Stock S, American Academy of Child Adolescent Psychiatry Committee on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with schizophrenia. J Am Acad Child Adolesc Psychiatry. 2013;52(9):976–90.
Correll CU, Penzner JB, Parikh UH, Mughal T, Javed T, Carbon M, et al. Recognizing and monitoring adverse events of second-generation antipsychotics in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2006;15(1):177–206.
Leverich GS, Post RM, Keck PE Jr, Altshuler LL, Frye MA, Kupka RW, et al. The poor prognosis of childhood-onset bipolar disorder. J Pediatr. 2007;150(5):485–90.
Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, et al. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry. 2004;55(9):875–81.
Post RM, Leverich GS, Kupka RW, Keck PE Jr, McElroy SL, Altshuler LL, et al. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. J Clin Psychiatry. 2010;71(7):864–72.
Gochman P, Miller R, Rapoport JL. Childhood-onset schizophrenia: the challenge of diagnosis. Curr Psychiatry Rep. 2011;13(5):321–2.
Hrdlicka M, Dudova I. Atypical antipsychotics in the treatment of early-onset schizophrenia. Neuropsychiatr Dis Treat. 2015;11:907–13.
Clemmensen L, Vernal DL, Steinhausen HC. A systematic review of the long-term outcome of early onset schizophrenia. BMC Psychiatry. 2012;12:150.
Saphris [package insert]. Irvine: Allergan, Inc; 2017.
Kane JM, Cohen M, Zhao J, Alphs L, Panagides J. Efficacy and safety of asenapine in a placebo- and haloperidol-controlled trial in patients with acute exacerbation of schizophrenia. J Clin Psychopharmacol. 2010;30(2):106–15.
Potkin SG, Cohen M, Panagides J. Efficacy and tolerability of asenapine in acute schizophrenia: a placebo- and risperidone-controlled trial. J Clin Psychiatry. 2007;68(10):1492–500.
McIntyre RS, Cohen M, Zhao J, Alphs L, Macek TA, Panagides J. A 3-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11(7):673–86.
McIntyre RS, Cohen M, Zhao J, Alphs L, Macek TA, Panagides J. Asenapine in the treatment of acute mania in bipolar I disorder: a randomized, double-blind, placebo-controlled trial. J Affect Disord. 2010;122(1–2):27–38.
Kane JM, Mackle M, Snow-Adami L, Zhao J, Szegedi A, Panagides J. A randomized placebo-controlled trial of asenapine for the prevention of relapse of schizophrenia after long-term treatment. J Clin Psychiatry. 2011;72(3):349–55.
Szegedi A, Durgam S, Mackle M, Yu SY, Wu X, Mathews M, et al. Randomized, double-blind, placebo-controlled trial of asenapine maintenance therapy in adults with an acute manic or mixed episode associated with bipolar I disorder. Am J Psychiatry. https://doi.org/10.1176/appi.ajp.2017.16040419.
Durgam S, Landbloom R, Mackle M, Wu X, Mathews M, Nasrallah H. Exploring the long-term safety of asenapine in adults with schizophrenia in a double-blind, fixed-dose, extension study. Neuropsychiatr Dis Treat. 2017;13:2021–35.
Landbloom R, Mackle M, Wu X, Kelly L, Snow-Adami L, McIntyre RS, et al. Asenapine for the treatment of adults with an acute exacerbation of schizophrenia: results from a randomized, double-blind, fixed-dose, placebo-controlled trial with olanzapine as an active control. CNS Spectr. 2016;08:1–9.
Ketter TA, Durgam S, Landbloom R, Mackle M, Wu X, Mathews M. Long-term safety and tolerability of asenapine: a double-blind, uncontrolled, long-term extension trial in adults with an acute manic or mixed episode associated with bipolar I disorder. J Affect Disord. 2017;01(207):384–92.
Landbloom RL, Mackle M, Wu X, Kelly L, Snow-Adami L, McIntyre RS, et al. Asenapine: Efficacy and safety of 5 and 10 mg bid in a 3-week, randomized, double-blind, placebo-controlled trial in adults with a manic or mixed episode associated with bipolar I disorder. J Affect Disord. 2016;15(190):103–10.
McIntyre RS, Cohen M, Zhao J, Alphs L, Macek TA, Panagides J. Asenapine versus olanzapine in acute mania: a double-blind extension study. Bipolar Disord. 2009;11(8):815–26.
McIntyre RS, Cohen M, Zhao J, Alphs L, Macek TA, Panagides J. Asenapine for long-term treatment of bipolar disorder: a double-blind 40-week extension study. J Affect Disord. 2010;126(3):358–65.
Findling RL, Landbloom RP, Mackle M, Pallozzi W, Braat S, Hundt C, et al. Safety and efficacy from an 8 week double-blind trial and a 26 week open-label extension of asenapine in adolescents with schizophrenia. J Child Adolesc Psychopharmacol. 2015;25(5):384–96.
Citrome L. Asenapine review, part I: chemistry, receptor affinity profile, pharmacokinetics and metabolism. Expert Opin Drug Metab Toxicol. 2014;10(6):893–903.
Shayegan DK, Stahl SM. Atypical antipsychotics: matching receptor profile to individual patient’s clinical profile. CNS Spectr. 2004;9(10 Suppl 11):6–14.
Dogterom P, Riesenberg R, Lesem M, de Greef R, Miltenburg A, Landbloom R, et al. Asenapine pharmacokinetics and tolerability in a pediatric population with a psychotic disorder: influence of dosing regimen. Poster presented at the 59th annual meeting of the American Academy of Child and Adolescent Psychiatry; San Francisco, CA; October 23–28, 2012.
Johnson M, Reddy VP, de Greef R, Findling RL, Carrothers TJ. Population pharmacokinetics of asenapine in pediatric subjects aged 10 to 17 years. Poster presented at the 63rd American Academy of Child Adolescent Psychiatry annual meeting; New York, NY; October 24–29, 2016.
Chapel S, Hutmacher MM, Haig G, Bockbrader H, de Greef R, Preskorn SH, et al. Exposure-response analysis in patients with schizophrenia to assess the effect of asenapine on QTc prolongation. J Clin Pharmacol. 2009;49(11):1297–308.
US Food and Drug Administration. Saphris (Asenapine) Sublingual Tablets. Briefing Book. July 30, 2009. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/PsychopharmacologicDrugsAdvisoryCommittee/UCM173877.pdf. Accessed 30 Aug 2016.
Dogterom P, de Greef R, Peeters PA. The effect of food on the high clearance drug asenapine after sublingual administration to healthy male volunteers. Eur J Clin Pharmacol. 2015;71(1):65–74.
Dogterom P, Timmer C, de Greef R, Spaans E, de Vries D, van Vliet A, et al. Asenapine safety, tolerability, and pharmacokinetics after single and multiple doses in healthy volunteers. Clin Pharmacol Drug Dev. 2012;1(4):131–43.
Findling RL, Landbloom RL, Szegedi A, Koppenhaver J, Braat S, Zhu Q, et al. Asenapine for the acute treatment of pediatric manic or mixed episode of bipolar I disorder. J Am Acad Child Adolesc Psychiatry. 2015;54(12):1032–41.
Prohn M, de Greef R, Chapel S, Kerbusch T. Population pharmacokinetics of asenapine in patients with schizophrenia or bipolar disorder. Eur Neuropsychopharmacol. 2009;9(suppl 3):S542–3 (Abstract).
Findling RL, Landbloom RL, Mackle M, Wu X, Snow-Adami L, Chang K, et al. Long-term safety of asenapine in pediatric patients diagnosed with bipolar I disorder: a 50-week open-label, flexible-dose trial. Pediatr Drugs. 2016;18(5):367–78.
Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35.
Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the Clinical Global Impressions (CGI) Scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 1997;73(3):159–71.
Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–77.
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76.
Findling RL, McIntyre RS, Landbloom RL, Wu X, Durgam S. Body weight did not influence asenapine efficacy in pediatric patients with bipolar I disorder. In: Poster presented at: the 63rd annual meeting of the American Academy of Child & Adolescent Psychiatry; New York, NY; October 24–29, 2016.
Findling RL, Landbloom RL, Wu X, Durgam, S. Weight change by baseline body mass index in asenapine-treated pediatric patients with bipolar I disorder. In: Poster presented at: the 63rd annual meeting of the American Academy of Child & Adolescent Psychiatry; New York, NY; October 24–29, 2016.
McIntyre RS, Findling R, Wu X, Edwards J, Earley W, Gache C. Efficacy of asenapine in relation to the number of prior manic/mixed episodes in pediatric patients with bipolar I disorder. In: Poster presented at: the U.S. Psychiatric & Mental Health Congress; San Antonio, TX; October 21–24.
Gache C, Findling R, McIntyre RS, Suppes T, Landbloom R, Han S-H, Durgam S. Efficacy of asenapine in pediatric patients with manic and mixed episodes of bipolar I disorder. In: Poster presented at: the 169th annual meeting of the American Psychiatric Association; Atlanta, Georgia; May 14–18, 2016.
Lopez FL, Ernest TB, Tuleu C, Gul MO. Formulation approaches to pediatric oral drug delivery: benefits and limitations of current platforms. Expert Opin Drug Deliv. 2015;12(11):1727–40.
Barrett EA, Sundet K, Faerden A, Agartz I, Bratlien U, Romm KL, et al. Suicidality in first episode psychosis is associated with insight and negative beliefs about psychosis. Schizophr Res. 2010;123(2–3):257–62.
Kane JM, Sharif ZA. Atypical antipsychotics: sedation versus efficacy. J Clin Psychiatry. 2008;69(Suppl 1):18–31.
Correll CU, Manu P, Olshanskiy V, Napolitano B, Kane JM, Malhotra AK. Cardiometabolic risk of second-generation antipsychotic medications during first-time use in children and adolescents. JAMA. 2009;302(16):1765–73.
Acknowledgements
Writing assistance and editorial support for this manuscript were provided by Carol Brown, MS, at Prescott Medical Communications Group (Chicago, IL, USA), with support from Allergan (Jersey City, NJ, USA) in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3). All authors had full control of content throughout development of the manuscript and participated in the writing, editing, and approval of this final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Source of funding and material support
Supported by funding from Allergan.
Conflict of interest
Dr. Stepanova receives research support from PsychNostics, LLC. Dr. Grant has no conflicts of interest to disclose. Dr. Findling receives or has received research support, acted as a consultant and/or served on a speaker’s bureau for Actavis, Akili, Alcobra, American Academy of Child & Adolescent Psychiatry, American Psychiatric Press, Bracket, CogCubed, Cognition Group, Coronado Biosciences, Elsevier, Epharma Solutions, Forest, Genentech, GlaxoSmithKline, Guilford Press, Ironshore, Johns Hopkins University Press, KemPharm, Lundbeck, Medgenics, Merck, NIH, Neurim, Novartis, Otsuka, PCORI, Pfizer, Physicians Postgraduate Press, Purdue, Rhodes Pharmaceuticals, Roche, Sage, Shire, Sunovion, Supernus Pharmaceuticals, Syneurx, Takeda, Teva, TouchPoint, Tris, Validus, and WebMD.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Stepanova, E., Grant, B. & Findling, R.L. Asenapine Treatment in Pediatric Patients with Bipolar I Disorder or Schizophrenia: A Review. Pediatr Drugs 20, 121–134 (2018). https://doi.org/10.1007/s40272-017-0274-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-017-0274-9