Abstract
Background and Objective
Medical advancement has enabled children to survive congenital airway anomalies, rare diseases and critical illnesses with medical technology including tracheostomies and long-term ventilation to support breathing. This study aimed to assess (1) the validity of the EQ-TIPS and EQ-5D-Y-3L in children dependent on technology and (2) the impact of caring for these children on the EQ-5D-5L and CarerQoL.
Methods
Caregivers of children aged 1 month to 18 years completed the EQ-TIPS or EQ-5D-Y-3L, Pediatric Quality of Life Inventory (PedsQL) and Paediatric Tracheostomy Health Status Instrument (PTHSI) to reflect the child’s health. In addition, caregivers self-completed the EQ-5D-5L and CarerQoL. Reports of problems on EQ dimensions were compared across age groups with the Fisher’s exact test. Spearman and Pearson’s correlation coefficients and Kruskal–Wallis H-test were used to explore the association between caregiver and child scores, concurrent validity, and known-group validity of the EQ-TIPS and EQ-5D-Y-3L.
Results
Responses from 144 caregivers were collected, 66 for children aged 1 month to 4 years completing EQ-TIPS and 78 for children aged 5–18 years completing EQ-5D-Y-3L. The EQ-TIPS showed a higher report of no problems for social interaction for children aged 1–12 months (p = 0.040) than the older age groups, there were however no differences in the level sum score (LSS) or EQ Visual Analogue Scale scores between the age groups. The EQ-5D-Y-3L showed a significantly less report of problems for mobility (p = 0.013) and usual activities (p = 0.006) for children aged 5–7 years compared with children aged 8–12 and children aged 13–18 years. Similarly, the 5–7 years of age group had a significantly lower EQ-5D-Y-3L LSS compared with the older groups (H = 12.08, p = 0.002). The EQ-TIPS and EQ-5D-Y-3L showed moderate-to-strong associations with the PedsQL. EQ-TIPS median LSS was able to differentiate between groups on the clinical prognosis with a better health-related quality of life (HRQoL) in those where weaning from technology is possible compared with those where weaning is not possible (H = 18.98, p = 0.011). The EQ-5D-Y-3L can discriminate between breathing technology, where those with only a tracheostomy reported better HRQoL (H = 8.92, p = 0.012), and between mild and moderate clinical severity (H = 19.42, p < 0.001). Neither the PedsQL nor the PTHSI was able to discriminate between these groups across the age range. Caregiver and child HRQoL scores showed moderate-to-strong associations.
Conclusions
The EQ-TIPS and EQ-5D-Y-3L showed good validity in children dependent on the technology for breathing. The EQ-TIPS and EQ-5D-Y-3L LSS were all able to differentiate between children with known clinical variables and outperformed both the PedsQL and PTHSI, making them preferable for intervention research. The caregiver scores are associated with the child HRQoL scores and thus a spill-over should be accounted for in any interventions targeting this cohort. It is recommended that future studies investigate the reliability and responsiveness of these measures in children dependent on technology for breathing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Children who are dependent on technology for breathing have decrements in their health-related quality of life. |
The results of this research suggests that the EQ-TIPS and EQ-5D-Y-3L are the most appropriate generic health-related quality-of-life measures for use in children who are dependent on technology for breathing. |
The burden of caring for children who are dependent on breathing for technology and the resultant spill-over of health effects on the caregiver should be accounted for in interventions targeting this cohort. |
1 Introduction
Medical advancement has enabled children to survive congenital airway anomalies, rare diseases and critical illnesses with medical technology including tracheostomies and long-term ventilation to support breathing [1, 2]. A tracheostomy acts as an artificial airway in patients who are unable to maintain a patent airway, often from congenital and acquired airway anomalies or neurological consequences, or for those who may need long-term mechanical ventilation [3]. Furthermore, in children needing intermittent or nocturnal mechanical ventilation, i.e. children with rare neuromuscular conditions, congenital central hypoventilation syndrome and sleep apnoea, less invasive ventilation with mask assistance is supported [2, 4,5,6]. The number of technology-dependent children is increasing globally with the increased use of healthcare services [1]. This necessitates a change in focus in this group from the measurement of mortality to monitoring and improving health-related quality-of-life (HRQoL).
Health-related quality-of-life measures the perceived impact of health on physical, social, psychological/emotional and cognitive function [7, 8]. Health-related quality-of-life measures can be divided into two main categories: disease-specific and generic measures. Disease-specific measures are typically developed to measure the effects of a specific health condition on HRQoL [9]. Although disease-specific measures may be able to more accurately detect clinical changes, their data cannot be compared across disease groups or between disease groups and the general population [10]. Conversely, generic health measures can be used to collect data from both healthy and ill individuals and thus have a wider application allowing comparisons across conditions and interventions [10,11,12,13,14,15,16]. The inclusion of generic HRQoL measures in paediatrics is increasingly used to support patient-centred care in the clinical setting and for health economic decision making [17,18,19]. Children are all dependent on their caregivers with a change in dependence over time. Arguably, the burden of care for children with a health condition is higher than caring for a healthy child creating a spill-over of health between the child and their caregiver [20,21,22]. The burden of caring for children with a health condition and the subsequent health loss of the caregiver can also be measured with condition-specific measures such as the CarerQol [23], Paediatric Tracheostomy Health Status Instrument (PTHSI) [24] and Pediatric Quality of Life Inventory (PedsQL) family impact module [25,26,27] as well as adult generic HRQoL measures. This health spill-over may be particularly pertinent in children dependent on technology in the context of South Africa. Because of resource restraints, home-based nursing assistance cannot be provided and thus parents undergo a home-based tracheostomy and ventilation training programme before being discharged home under their sole care [2, 28]. The training and caring for children dependent on technology for breathing are more admirable in this context as families have additional socioeconomic challenges including poor access to formal housing, water and/or electricity [2].
There is a clear decrement in HRQoL in adult patients with tracheostomies as measured with generic measures including the EQ-5D-3L/5L [29,30,31,32], SF-36 [33, 34] and tracheostomy-specific questionnaires [35,36,37]. Most studies in children dependent on technology for breathing have studied the impact of caregiver or family burden with decrements in HRQoL shown on the PedsQL family impact module [25,26,27] as well as caregiver HRQoL on the SF-36 [38, 39], HUI [4] and the PTHSI [24, 38, 40]. There is a dearth of research investigating generic HRQoL in children dependent on technology for breathing, including tracheostomies or ventilation. This may be a reflection on the lack of clinical specificity or disease symptoms included in generic measures [9]. Considering the increasing prevalence of breathing technology in children with a wide range of health conditions [41] and the potential need for future decision making for funding of this technology [14], research is needed to validate generic HRQoL measures in this group [42]. Previous studies that have included generic HRQoL measures in this group have not focussed on instrument validation but on using the results to describe family impact [3], social and economic burden of care, and comparisons of developmental outcomes [4] and HRQoL [43] to controls. However, the results from self-completion of the PedsQL [3, 5], TAPQoL [4] and KINDL [43] in these studies all show a decrement in HRQoL in older children and adolescents. The disease-specific HRQoL measure, PTHSI, was used in the South African setting to evaluate the health state in children with a tracheostomy and showed a clear decrement in the HRQoL of the child [40]. However, 84% of the sample were decannulated (no longer had a tracheostomy) at the time of the interview, which may have influenced these results .
The EQ-5D-Y-3L is one of the most cited generic preference-weighted HRQoL measures available for young children [44]. It has however not been used to measure HRQoL in children dependent on technology for breathing and requires psychometric validation. The development of a new EuroQol instrument for Toddler and Infant Populations (EQ-TIPS, previously known as the TANDI) [45, 46] now allows the measurement of HRQoL across the age range on EQ instruments (1 month to 18 years). Further evidence is however needed on both the psychometric performance of the measure in this group and the performance of the EQ-TIPS and EQ-5D-Y across the age range. The adult EQ-5D-3L/5L instruments have further been found to be useful in measuring the decrements in health associated with caregiving burden [47,48,49] and spill-over. Previous studies in South Africa have found the general health on the EQ Visual Analogue Scale (VAS) to be strongly associated between the parent and child [47, 48]. It is further anticipated that the burden of caring for children dependent on technology for breathing will result in a higher report of problems with anxiety/depression or mental health [50,51,52].
As such, this study aims to assess the performance of the EQ-5D-Y-3L and EQ-TIPS measures, in children who are dependent on breathing technology, and compare the results to the PedsQL (a generic HRQoL measure) and PTHSI (a disease-specific HRQoL measure for the child and caregiver). Furthermore, the impact of caring for these technology-dependent children is assessed on the EQ-5D-5L, CarerQoL and PTHSI.
2 Methods
2.1 Measures
2.1.1 EQ-5D-Y-3L Proxy Version 1
The EQ-5D-Y-3L Proxy version 1 is recommend for use in children aged 4–18 years and includes five dimensions: mobility, looking after myself, usual activities, having pain or discomfort and feeling worried, sad or unhappy. Each item has three response levels corresponding to ‘no problems’, ‘some problems’ and ‘a lot of problems’. Proxy version 1, which asks the respondent to rate the child’s HRQoL from their own viewpoint was used in this study [53]. The EQ-5D-Y-3L has been validated in the South African population [54] and used across a variety of health conditions [55,56,57,58]
2.1.2 EQ-TIPS
The EQ-TIPS is a proxy report instrument intended for completion, in most cases, by the primary caregiver or parent. The EQ-TIPS includes six dimensions: movement, play, pain, communication, social interaction and eating. Similarly to the EQ-5D-Y-3L, the dimensions are scored on three response levels. The EQ-TIPS has been validated in children aged 1 month to 3 years in the South African population [45, 59]. As the dimensions of the EQ-TIPS were more relevant and out-performed the EQ-5D-Y-3L in 4-year-old children in South Africa [60] the EQ-TIPS age range was extended to 4 years in this study.
2.1.3 EQ-5D-5L
The validated EQ-5D-5L South African version [61] was included to measure the health of the caregiver and determine the impact of caring for a child who is dependent on health technology for breathing. Measurement of HRQoL is similarly measured on five dimensions: mobility, self-care, usual activities, pain or discomfort, and anxiety or depression. These are rated on five levels of severity: no, slight, moderate, severe and unable/extreme.
All EuroQol instruments include a general rating of health on a EQ VAS of 0 (worst health) to 100 (best health) [46, 62]. The three or five levels of each of the EuroQol descriptive systems are expressed with a five- or six-digit code. For example, the EQ-5D-Y-3L health state 11223 describes someone with no problems with mobility, no problems with looking after myself, some problems with usual activities, having some pain or discomfort, and feeling very worried, sad or unhappy. The best health state described by the instrument is coded as 11111, describing ‘no problems’ in each of the dimensions [63]. There are not preference-based scores available for the EQ-5D-Y-3L nor the EQ-5D-5L for South Africa and to date there are no protocols available for valuation of the EQ-TIPS. As such, a level sum score (LSS) was used to describe the responses on the descriptive system where the level labels are treated as numeric data with scores that ranged from 5 to 15 for the EQ-5D-Y-3L, 5 to 25 for the EQ-5D-5L and from 6 to 18 for the EQ-TIPS. The LSS is a crude score that does not account for preference of dimensions or weighting of responses [64, 65] but gives some indication of the performance of the dimensions between the EuroQol instruments. Considering the range of scores between the EQ-5D-Y-3L and EQ-TIPS, the LSS was transformed to a score out of 100 for comparison across the age range (EQ-5D-Y-3L/EQ-TIPS LSS% score). The combination of EQ-5D-Y-3L and EQ-TIPS LSS gives a basic overview of how these instruments may perform across the age range. It is noted that the dimensions are different, and the weighting given to each dimension may differ across the age range and the instruments. A higher LSS and LSS% score indicates a worse HRQoL.
2.1.4 Pediatric Quality of Life Inventory (PedsQL)
The age-appropriate PedsQL 4.0 generic measures for children aged 0–18 years were used for the proxy report. The scales measure HRQoL across five dimensions including physical functioning (and symptoms in infants aged 1–24 months), emotional functioning, social functioning and cognitive/school functioning. Each version has a variable number of items with the questionnaire for 1–12 months including 36 items, 13–24 months including 45 items, 2–4 years including 21 items, and versions for 5–7 years, 8–12 years and 13–18 years including 23 items each. The questionnaire for children aged 2–4 years [60] and for children aged 5–18 years [54] have been validated in the South African population and has shown good concurrent validity with the EQ-TIPS [60] and EQ-5D-Y-3L [56]. It has further been used to measure HRQoL in children with a tracheostomy [3, 5]. Each item is scored on a Likert scale from 0 to 4 (never a problem, almost never, sometimes, often or almost always a problem). Items are reversed scored and transformed to a 0–100 scale: 0 = 100, 1 = 75, 2 = 50, 3 = 25 and 4 = 0. Dimension scores are calculated by a sum of the item scores divided by the total number of items. A total score is similarly generated by summing the dimension scores over the total number of dimensions giving an overall HRQoL score. Scores for scales with more than 50% missing data are not computed. A higher PedsQL score indicates a better HRQoL [66,67,68].
2.1.5 Paediatric Tracheostomy Health Status Instrument (PTHSI)
The PTHSI was developed to capture the HRQoL and clinical characteristics of the caregivers and children with a tracheostomy [24, 35] and has been previously used in the South African population [40]. The caregiver and child HRQoL sections of this measure were completed by the proxy and included three questions about the child and 17 questions about the caregiver. The PTHSI was reverse scored with a higher score indicating a better HRQoL [69].
2.1.6 CarerQoL
The CarerQoL was developed to capture the care-related quality of life for caregivers. It consists of seven items including fulfilment, relationships, mental health, daily activities, financial problems, support and physical health [23]. Response categories include: “no”, “some” and “a lot of”, which are scored as 0, 1 and 2, respectively. The two positive items of fulfilment and support are reverse scored. The item scores are summed for the total score with a range of 0–14 with a higher score indicating a higher burden of care [23].
2.1.7 Clinical Information
Clinical information was completed for the child by the nurse practitioner/doctor and by the researcher from the clinical notes and included the length of time with a tracheostomy and/or ventilation, the primary indication for tracheostomy, co-morbidities, medications and the clinical workload score as described by Seear et al. (Table S1 of the Electronic Supplementary Material [ESM]) [5]. The workload score gives an indication of the clinical burden of caring for a child across five categories: airway and ventilation, prognosis, feeding, activities of daily living and regular daily treatments. In this study, activities of daily living were not scored for children aged 1 month to 4 years as it accounted for toileting and dressing, which may not be appropriate for the developmental age of these children. Thus, the total score for children aged 1 month to 4 years and aged 5–18 years was 42 and 52, respectively. Scores are calculated as a percentage of proportion and interpreted according to Seear et al. as mild (0–33%), moderate (34–66%) and severe (67–100%) [5].
2.2 Procedure
Ethics approval was obtained from the University of Cape Town, Faculty of Health Sciences, Human Research Ethics Committee (HREC 740_2021). The study was carried out in accordance with the Declaration of Helsinki involving human participants [70].
The study setting included a public and private hospital facility who manage children dependent on technology for breathing in both outpatient and inpatient facilities. All children aged 1 month to 18 years, and their caregivers, attending these facilities were eligible for recruitment. Children whose parents or legal guardians were unavailable for consent were excluded from the study.
Children and their caregivers were recruited in-person or telephonically at the time of their routine follow-up appointment or on admission to the hospital. Children and their caregivers were provided with a detailed description of the study and informed consent was obtained from the parent or legal guardian and assent was obtained from children aged over 8 years. All caregivers completed the PedsQL, General Rating of Health, EQ-5D-5L, PTHSI, CarerQoL and sociodemographic information. Caregivers of children aged 1 month to 4 years completed the EQ-TIPS whereas those caring for children aged 5–18 years completed the EQ-5D-Y-3L. Paper and pencil questionnaires and electronic questionnaires were available. Questionnaires were completed in random order to prevent the ordering effect [57]. The clinician attending the child completed the clinical workload form. Caregivers and children were not reimbursed for their participation as no additional costs were incurred for participation in this study.
2.3 Data Analyses and Management
2.3.1 General Performance and Feasibility
The EQ-TIPS and EQ-5D-Y-3L descriptive data and sociodemographic information were summarised in terms of frequency of dimension responses across age groups and for the total sample. The EQ-TIPS and EQ-5D-Y-3L dimension responses were categorised into problems and no problems and compared across the age groups for 1–12 months, 13–24 months, and 2–4 years and compared with the Fisher’s exact test. The ceiling of the EQ-TIPS and EQ-5D-Y-3L was defined as the proportion of children scoring no problems across all six/five dimensions, whereas the floor was calculated as the proportion of those scoring a lot of problems across all dimensions. The ceiling and floor effects were compared by the Fisher’s exact test and the EQ-TIPS LSS and VAS scores were compared by the Kruskal–Wallis H-test between age groups. Key medical and demographic characteristics of the children were compared across the age groups (1–12 months, 13–24 months, 2–4 years, 5–7 years, 8–12 years and 13–18 years) with a one-way analysis of variance and a Bonferroni post-hoc analysis.
2.3.2 Concurrent Validity
The concurrent validity of EQ-TIPS and EQ-5D-Y-3L dimension scores were compared to the PedsQL subscores, summary scores, and total scores and the PTSHI score for the child using Spearman’s correlation. A subgroup analysis by PedsQL age categories was computed for dimension scores. Pearson’s correlations were computed for EQ-TIPS and EQ-5D-Y-3L VAS and LSS scores and corresponding PedsQL scores. Correlation coefficients were interpreted according to Cohen: 0.1–0.29 low association, 0.3–0.49 moderate association and ≥0.5 high association [71].
2.3.3 Known Group Validity
The Kruskal–Wallis H-test was used to compare EQ-TIPS/EQ-5D-Y-3L, PedsQL and PTHSI total scores of children with known clinical or sociodemographic characteristics. As the EQ-TIPS and EQ-5D-Y-3L have a different range of LSS scores, these were calculated as percentages for direct comparisons. Post-hoc pairwise comparisons were computed with Bonferroni correction for multiple comparisons. Characteristics included age groups (1–12 months, 13–24 months, 2–4 years, 5–7 years, 8–12 years and 13–18 years as per the PedsQL questionnaires), gender (female and male), breathing technology (tracheostomy, invasive ventilation [tracheostomy and ventilation], non-invasive ventilation), clinical severity (mild, moderate or severe) and clinical prognosis (good, technology likely permanent; long survival, weaning possible; poor, survival unlikely beyond a year). Clinical severity scores were calculated according to the pre-existing categories developed for the Seear scale with mild (0–33%), moderate (34–66%) and severe (67–100%) [5].
2.3.4 Burden of Caring for Children Who Are Dependent on Technology
Caregiver EQ-5D-5L, CarerQoL and PTHSI scores and sociodemographic scores were summarised in terms of the frequency of dimension responses across the children’s age groups and for the total sample. Median caregiver scores were compared by Kruskal–Wallis H-test according to known sociodemographic characteristics of the caregivers (health condition, number of caregiving hours for the child, number of children in their care and education status) and of the child (child’s age, gender, breathing technology, rating of child’s health, Child’s clinical severity and school attendance). Post-hoc pairwise comparisons were performed with Bonferroni correction for multiple comparisons.
Associations between the caregiver’s scores (EQ-5D-5L VAS and LSS, PTHSI caregiver score, CarerQoL) were calculated with Spearman’s corelation. Association of caregiver scores and caregiver rating of child’s scores (EQ-TIPS/EQ-5D-Y-3L, PedsQL and PTHSI child score) were similarly calculated with Spearman’s correlation. Correlation coefficients were interpreted according to Cohen: 0.1–0.29 low association, 0.3–0.49 moderate association and ≥0.5 high association [71].
The level of statistical significance was set at p ≤ 0.05. A statistical analysis was performed in SPSS Statistics Version 28 (IBM, Armonk, NY, USA).
3 Results
Figure 1 summarises the recruitment and enrolment of participants. The data of 144 children/adolescents have been included for analysis. Reasons for refusal of consent/assent was not collected. Although there were more children in the 0–4 years of age group compared with the 5–18 years of age group recruited during an out-patient visit for acute illness, this was not significantly different (x2 = 4.08, p = 0.130). Participants all withdrew because of time constraints.
3.1 Descriptive Statistics
Table 2 of the ESM describes the child and caregiver characteristics. The patient population had a median age at enrolment of 5.9 years (interquartile range 2.9–9.7 years). Most patients (n = 99, 68.8%) were dependent on only a tracheostomy for breathing and 13.2% (n = 19) of children were reliant on invasive ventilation (both a tracheostomy and ventilation) with a median duration since the tracheostomy insertion of 5.0 months (interquartile range 1.0–23.0 months). To note, 12.5% of these children had been decannulated in the previous 12 months. The indication for technology for breathing is predominantly for upper airway obstruction (n = 85, 59.0%) followed by neuromuscular disease (n = 24.0, 17%) and the need for long-term ventilation (n = 14, 10.0%). The proportion of children living with neuromuscular disease was significantly higher in children aged 13–18 years compared with those in the younger age groups (1 month to 7 years) [F3.459, p = 0.006]. Similarly, children aged 13–18 years were more dependent on non-invasive ventilation than the younger groups (F = 5.84, p < 0.001) [Table 3 of the ESM]. The majority of children who were dependent on non-invasive ventilation were living with neuromuscular disease (n = 17, 65%). The clinical workload was calculated as mild for most children (n = 118, 82%) and the attending clinician scored the majority of the children’s prognoses as “good, with long term survival and possible weaning of technology” (n = 62, 43.1%).
The majority of caregiver were mothers (n = 128, 89.9%) with high school the highest education level attained (n = 84, 58.3%). A quarter of the caregivers (n = 37, 25.7%) reported a health condition most frequently reporting hypertension, asthma and HIV. Caregiver health was not significantly different across the age groups (F = 0.951, p = 0.0.450) [Table 3 of the ESM].
3.2 General Instrument Performance
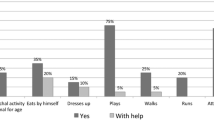
Table 1 shows the distribution of EQ-TIPS dimension scores in total and per age group. Significant differences were found for social interaction with a greater report of no problem for children aged 1–12 months compared with the older two groups. There was notably a higher report of a lot of problems with eating than some problems eating across age groups. There were no significant differences noted between these age groups for key medical and demographic characteristics (Table 3 of the ESM).
The highest report of problems on the EQ-5D-Y-3L (Table 2) was for the dimensions of mobility and looking after myself with the highest report of no problems for usual activities and feeling worried, sad or unhappy. The 5–7 years of age group had a significantly lower EQ-5D-Y-3L LSS than the 8–12 years of age group (H = −16.68, p = 0.17) and 13–18 years of age group (H = 19.53, p = 0.005). This could be attributed to significantly less problems reported in the dimensions of mobility and usual activities and a higher overall ceiling (11111). The 5–7 years of age group had significantly higher dependence on tracheostomy (p < 0.001) and a corresponding lower use of non-invasive ventilation (p = 0.043) when compared with those aged 13–18 years.
3.3 Concurrent Validity
It was hypothesised that all of the EQ-TIPS dimensions, except eating, and the LSS would show a moderate-to-high correlation with the PedsQL total score [60]. Furthermore, it was anticipated that moderate-to-high correlations would be found between corresponding EQ-TIPS and PedsQL dimensions/items of movement and physical functioning; play and physical functioning; pain and physical symptoms social interaction and social functioning; and communication and social functioning [60].
It was hypothesised that EQ-5D-Y-3L dimensions and LSS would show a moderate-to-high correlation with the PedsQL total score [72]. It was further anticipated that moderate-to-high correlations would be found between corresponding EQ-5D-Y-3L and PedsQL dimensions/items of mobility and physical functioning; looking after myself and physical functioning; usual activities and physical functioning/social functioning; pain or discomfort and physical functioning; worried, sad, or unhappy and emotional functioning [72].
All associations between the EQ-5D-Y-3L were strong for the anticipated dimensions and PedsQL scores except for mobility and PedsQL physical functioning (Table 3). The EQ-TIPS dimension, VAS and LSS scores were strongly associated with PedsQL subscores and summary scores. Pain on the EQ-TIPS was associated with physical symptoms, which are only included in the PedsQL 1–12 months and 13–24 months scales. Notably, pain or discomfort was strongly associated with physical and emotional functioning on the EQ-5D-Y-3L but only for physical symptoms on the EQ-TIPS. Although the PedsQL subscore of emotional function did not show a strong association with any of the EQ-TIPS scores across the age range of 0–4 years, on age-group analysis, it showed a moderate association with pain (0–12 months), eating (13–24 months) and social interaction (2–4 years) [Table 4 of the ESM]. PedsQL similarly had moderate associations with all EQ-TIPS dimensions except pain and eating. At an age-group level, the EQ-TIPS dimension of eating was strongly associated with PedsQL scores for children aged 0–12 months and 13–24 months but not aged 2–4 years (Table 4 of the ESM). To note, the PedsQL was only completed by seven and three caregivers of children aged 8–12 years and 13–18 years, respectively, this limited any meaningful age-group comparisons.
The PTHSI score showed low-to-moderate correlations with the EQ-TIPS dimensions of social interaction and communication. The PTHSI and all the PedsQL scores except the physical symptom score and emotional functioning showed moderate correlations. Doing usual activities, looking after myself and the LSS on the EQ-5D-Y-3L for children aged 8–18 years showed a moderate association with the PTHSI score.
3.4 Known Group Validity
Summary scores were compared across the EQ-TIPS, EQ-5D-Y-3L, PedsQL and PTHSI total scores (Table 4). Upper airway obstruction was considered to be the most frequent reason for receiving a tracheostomy with most receiving a tracheostomy under the age of 1 year and decannulated after an average of 22 months [41]. Thus, it was hypothesised that there would be no age-related differences on the EQ-TIPS dimension scores as this group would have similar diagnoses and prognoses. The older age groups (5–18 years) were considered to have chronic or acquired conditions that would lead to dependence on tracheostomy and/or ventilation later in life and for longer periods, for example, neuromuscular disease and traumatic brain injury. [41]. Thus, we expected that the EQ-5D-Y-3L summary and VAS scores would be lower than the corresponding EQ-TIPS scores. Furthermore, the EQ-5D-Y-3L dimension, LSS and VAS scores were anticipated to indicate poorer HRQoL in the oldest age group (13–18 years).
The EQ-5D-Y-3L, PedsQL and PTHSI showed significant differences by age group. There were no significant differences between age and the EQ-TIPS scores. A post-hoc analysis with Bonferroni correction showed the 5–7 years of age group had a significantly lower EQ-5D-Y-3L score than the 8–12 years of age group (H = −16.68, p = 0.017) and 13–18 years of age group (H = 19.53, p = 0.005). The combined EQ-5D-Y-3L/EQ-TIPS LSS% score (H = −38.443, p = 0.021), PedsQL score (H = 44.4, p = 0.009) and PTHSI (H = 48.37, p = 0.001) were significantly lower in the 8–12 years of age groups than those aged 1–12 months. Similarly, the EQ-5D-Y-3L/EQ-TIPS LSS% score (H = −45.72, p = 0.004) and PTHSI (H = 66.89, p < 0.001) were significantly lower in the 13–18 years of age group than those aged 1–12 months. In addition, the PTHSI found significant differences between those aged 13–18 years and those aged 13–24 months (H = −51.531, p < 0.001), 2–4 years (H = 42.39, p = 0.004) and 5–7 years (H = 39.13, p = 0.018) when compared with those aged 1–12 months.
It was anticipated that the scores of all instruments would be able to differentiate between clinically different groups according to the breathing technology, clinical severity and clinical prognosis. It was anticipated that the decrements in HRQoL would be highest for those with invasive ventilation (tracheostomy and ventilator), followed by tracheostomy only and non-invasive ventilation. However, if these breathing technologies were not equally distributed across age groups, the age-related hypotheses may outweigh hypotheses for breathing technologies.
The EQ-TIPS LSS (H = 18.98, p = 0.011) and EQ-5D-Y-3L/EQ-TIPS LSS% score (H = 29.67, p = 0.002) were able to differentiate between the clinical prognosis in this age group with a post-hoc analysis showing that those categorised as “expected long survival, weaning possible” had a significantly lower LSS (indicating better HRQoL) than those rated with “good prognosis, but technology likely to be permanent.” The EQ-5D-Y-3L was able to discriminate between groups who were dependent on different technology, EQ-5D-Y-3L LSS (H = 15.595, p = 0.021) and EQ-5D-Y-3L/EQ-TIPS LSS% (H = 27.65, p = 0.006) score showed that children with only a tracheostomy had a lower score (better HRQoL) than those dependent on non-invasive ventilation, respectively. The EQ-5D-Y-3L and combined EQ-TIPS and EQ-5D-Y-3L LSS showed significant differences between children with mild or moderate clinical severity scores. Neither the PedsQL nor PTHSI was able to differentiate between any clinical indicators.
3.5 Burden of Caring for Children Who Are Dependent on Technology
The individual HRQoL and caregiver burden scores for the EQ-5D-5L, PTHSI and CarerQoL showed that problems on the EQ-5D-5L can mostly be attributed to pain/discomfort (23.9%) and anxiety/depression (35.2%), whereas there were frequently reported problems in all areas of QoL on the PTHSI with a notable 54.2% of caregivers reporting that they have been limited in fulfilling their own needs because of their child’s physical health all of the time. Results from the CarerQoL highlight that 85.4% of caregivers get some or a lot of fulfilment from caring for their children.
Characteristics of the child contributed to significant differences in the caregiver scores (Table 5). Caregivers of children dependent on invasive ventilation (tracheostomy and ventilation) had significantly lower PTHSI and EQ-5D-5L LSS scores (indicating worse HRQoL) than those who were only dependent on a tracheostomy. Similarly, caregivers of children with a moderate clinical severity reported poorer HRQoL on the PTHSI but a similar burden of care on the CarerQoL to those with mild clinical severity. There was a high and significant association between the PTHSI caregiver QoL scores and the EQ-5D-5L LSS score, CarerQoL score, and the EQ-5D-5L LSS and the CarerQoL score (Table 6). The EQ-5D-5L VAS score showed a moderate and significant association with other caregiver scores. When caregiver and child scores were compared, there were moderate and significant associations between all scores except for all child PHTSI scores and the caregiver EQ-5D-5L VAS score and child EQ-5D-Y-3L/EQ-TIPS LSS% score and PedsQL total score and the child Y-5L and caregiver CarerQoL summary score (Table 7).
4 Discussion
EQ-TIPS responses were collected for children aged 1 month to 4 years from their caregivers and the EQ-5D-Y-3L from children aged 5–18 years. These scores were compared to responses on the PedsQL and PTHSI child scores. The EQ-TIPS had a good distribution of responses across all dimensions and for all age groups that were delineated according to the PedsQL modules (1–12 months, 13–24 months and 2–4 years). The only differences in reporting between age groups was for the dimension of social interaction where the 1–12 months of age group had a higher proportion of no problems. This was not seen in previous validations of the instrument from the same geographical area [46, 59] and there were no significant differences in breathing technology, diagnosis or clinical prognosis across these age groups to account for this difference. Thus, this difference may be attributed to the change in the dimension heading from relationships to social interaction following recommendations from the EuroQol group (personal correspondence). The reporting of no problems was significantly higher for mobility and usual activities for children aged 5–7 years. The ceiling for both the EQ-TIPS and EQ-5D-Y-3L (11111/1) was higher than anticipated (>15%) in this group with a known health condition [73]. Although the ceiling decreased as the age of the child increased on both instruments, there was only a significant difference reported for the EQ-5D-Y-3L ceiling effect with the 5–7 years of age group having a higher report of no problems. The lower report of problems and ceiling effect in the 5–7 years of age group may be attributed to the significantly lower incidence of neuromuscular disease and the corresponding lower need for non-invasive ventilation.
The inclusion of pain on the EQ-TIPS and EQ-5D-Y-3L descriptive system is a strength when compared with the PedsQL. The EQ-TIPS pain dimension had a strong association with the PedsQL physical symptoms subscore, which is included in the modules for 1–12 months and 13–24 months only [74], whereas the EQ-5D-Y-3L pain and discomfort dimension had strong associations with PedsQL physical and emotional functioning. The attribution of pain or discomfort to emotional distress has been reported before by children completing the EQ-5D-Y-3L [75]. There were reassuringly strong correlations with the EQ-TIPS dimension scores and the PedsQL scores. There was however only a moderate association of the PedsQL emotional functioning subscore and EQ-TIPS dimensions of social interaction and communication. In the EQ-TIPS development work, social interaction is a strong theoretical construct for mental health and emotional functioning in this young age group [45]. However, more work is suggested for the EQ-TIPS to explore further representation for emotional functioning.
The EQ-TIPS and EQ-5D-Y-3L performed as anticipated when comparing the LSS between the known groups. The EQ VAS was not able to discriminate between any known clinical characteristics of the sample. This may, however, be attributed to the relatively high median score of 90 and the narrow interquartile range of 70–100, which is similar to previous EQ VAS results from the general population in South Africa [46]. The report of better HRQoL on the EQ-TIPS and EQ-5D-Y-3L LSS for children with a tracheostomy compared with those with non-invasive ventilation may be attributed to the fact most children with non-invasive ventilation were living with neuromuscular disease and had a greater physical impairment and thus a lower HRQoL. Reassuringly, there were no significant differences between EQ-TIPS LSS across the child’s age group, gender or sociodemographic variables. The 5–7 years of age group had a significantly higher reported HRQoL on the EQ-5D-Y-3L LSS, which is similarly attributed to the significantly lower proportion of children with neuromuscular disease.
When the entire age range was compared, there were notable differences across the PedsQL, PTHSI and EQ-5D-Y-3L/EQ-TIPS LSS% scores between the youngest and oldest age groups (1–12 months and 8–12 years), which may be attributed to the higher proportion of children with progressive neurological conditions in the older age group. The authors further postulate that older children are expected to develop independence and thus the dependence for medical treatment from the caregivers may have a more notable effect on the HRQoL, as perceived by their caregiver [20]. The EQ-TIPS and EQ-5D-Y-3L were able to differentiate between children with different clinical outcomes, whereas neither the PedsQL nor the disease-specific PTHSI measure was able to. This may have important implications for applications in clinical trials or interventional medicine where you anticipate a change in clinical characteristics. This result further highlights that clinical differences may in some cases be more accurately described by generic HRQoL instruments, such as the EQ-TIPS and EQ-5D-Y-3L, than disease-specific measures, such as the PTHSI. This may be more notable in a group of children with heterogenous health conditions who are all receiving a similar intervention, such as those dependent on technology for breathing.
The disease-specific measure, PTHSI, showed a clear decrement in the HRQoL score as children aged. This may be attributed to the fact that it evaluated items of swimming, playing in the bath and vocal sounds, which may not be as developmentally appropriate for the younger children [40]. The reference to age-appropriate behaviour on the EQ-TIPS seems to be a relative strength as no age-related differences were noted for any of the scores, except at the dimension level for social interaction.
It is noted that there is a spill-over of health between a caregiver and a child with ill health [22, 47, 76], as such, the HRQoL and caregiver burden was measured on the EQ-5D-5L, PTHSI and CarerQoL, respectively. Problems reported on the EQ-5D-5L were in keeping with the population norms for this age group with the highest report of problems for dimensions of pain or discomfort and anxiety or depression and a similar EQ VAS rating [77]. It is however notable that the report of anxiety or depression (35.2%) is more than one and a half times of that reported on international population norms (22%) [77]. This high rate of mental health concerns may be explained by the high caregiver report of their child’s health limiting their own needs on the PTSHI (54.2%). The median PTSHI score was similar to that reported by Din et al. for caregivers in the same setting [40]. Despite the CarerQoL score indicating a high burden of care, most caregivers (85.4%) indicated that they get fulfilment from caring for their children. Further, there is a high association between caregiver EQ-5D-5L LSS, PTHSI and CarerQoL scores, indicating that all measures are sensitive in measuring HRQoL and the burden of caregivers in those caring for children dependent on technology for breathing. The EQ VAS, however, seems to not be a good indicator of spill-over or caregiver burden in this cohort. It was anticipated that the spill-over would be greatest for parents of children with invasive ventilation (tracheostomy and ventilator) followed by a tracheostomy only and then non-invasive ventilation. The study however observed a slightly higher, but not significant, spill-over for children receiving non-invasive ventilation compared with having a tracheostomy only. This is attributed to the higher burden associated with neuromuscular disease in the group receiving non-invasive ventilation.
The caregiver EQ-5D-5L and PTHSI scores were associated with the age of the child with the 5–7 years of age group showing significantly higher caregiver HRQoL, owing to milder disease characteristics in this group. The PTHSI and CarerQoL further showed that children with more severe clinical scores contributed to lower caregiver HRQoL and a higher burden of care, respectively. The caregiver-rated HRQoL scores of the children have a moderate association (EQ-TIPS LSS, EQ-5D-Y-3L LSS and PedsQL score) with the caregiver PTHSI, EQ-5D-5L and CarerQoL scores. This has important implications for economic evaluations of paediatric interventions in children dependent on technology for breathing.
The small sample in each age group and known groups limits the interpretation of these results [78]. The LSS used for the EQ-TIPS, EQ-5D-Y-3L and EQ-5D-5L is a crude representation of the dimension performance and is limited as it does not account for the difference in health profile, for example, 12222 may have the same LSS as 31311 [64, 65]. The EQ-5D-Y-3L and EQ-TIPS include different content in their dimensions and have a different number of dimensions, thus the combination of LSS is intended to give a basic overview of how these instruments may perform across the age range. It is recommended that future mapping work investigate the relationship between these dimensions, and potentially their scores.
5 Conclusions
The EQ-TIPS and EQ-5D-Y-3L showed good validity in children dependent on technology for breathing. The EQ-TIPS and EQ-5D-Y-3L LSS were all able to differentiate between children with known clinical variables and outperformed both the PedsQL and PTHSI, making them preferable for intervention research. Further investigation into the EQ-TIPS dimension of social interaction is warranted for both understanding of the current wording and the appropriateness for young children aged 1–12 months. The caregiver scores are associated with the child HRQoL scores and thus a spill-over should be accounted for in any interventions targeting this cohort. It is recommended that future studies investigate the reliability and responsiveness of these measures in children dependent on technology for breathing. A comparison of HRQoL in children living with neuromuscular disease with and without dependence on technology for breathing may give a more accurate indication of the impact of breathing technology on overall HRQoL.
References
Noyes J. Health and quality of life of ventilator-dependent children. Issues Innov Nurs Pract. 2006;56(4):392–403.
Groenendijk I, Booth J, Van DM, Argent A, Zampoli M. Paediatric tracheostomy and ventilation home care with challenging socio-economic circumstances in South Africa. Int J Pediatr Otorhinolaryngol. 2016;84:161–5.
Westwood EL, Hutchins JV, Thevasagayam R, Road BH. Quality of life in paediatric tracheostomy patients and their caregivers: a cross-sectional study. Int J Pediatr Otorhinolaryngol. 2019;127(March): 109606.
Teng L, Mpaeds T, Marie A, Mrcpch N, Mpaeds SJ, Peng K, et al. Health-related quality of life and developmental outcome of children on home mechanical ventilation in a developing country: a cross-sectional study. Pediatr Pulmonol. 2020;55:3477–86.
Seear M, Kapur A, Wensley D, Morrison K, Behroozi A. The quality of life of home-ventilated children and their primary caregivers plus the associated social and economic burdens: a prospective study. Arch Dis Chil. 2016;101:620–7.
van der Poel LAJ, Booth J, Argent A, van Dijk M, Zampoli M. Home ventilation in South African children: do socioeconomic factors matter? Pediatr Allergy Immunol Pulmonol. 2017;30(3):163–70.
Spieth LE, Harris CV. Assessment of health-related quality of life in children and adolescents: an integrative review. J Pediatr Psychol. 1996;21(2):175–93.
Grange A, Bekker H, Noyes J, Langley P. Adequacy of health-related quality of life measures in children under 5 years old: systematic review. J Adv Nurs. 2007;59(197–220):197–220.
Pal DK. Quality of life assessment in children: a review of conceptual and methodological issues in multidimensional health status measures. J Epidemiol Community Health. 1996;50(4):391–6.
Varni JW, Burwinkle TM, Lane MM. Health-related quality of life measurement in pediatric clinical practice: an appraisal and precept for future research and application. Health Qual Life Outcomes. 2005;3(34):34–43.
Solans M, Pane S, Estrada MD, Serra-Sutton V, Berra S, Herdman M, et al. Health-related quality of life measurement in children and adolescents: a systematic review of generic and disease-specific instruments. Value Health. 2008;11(4):742–64.
Feeny D, Furlong W, Mulhern RK, Barr RD, Hudson M. A framework for assessing health-related quality of life among children with cancer. Int J Cancer Suppl. 1999;12:2–9.
Kaplan RM, Bush JW. Health-related quality of life measurement for evaluation research and policy analysis. Health Psychol. 1982;1(1):61–80.
Torrance GW. Preferences for health outcomes and cost-utility analysis. Am J Manage Care. 1997;3:S8-20.
Garber AM, Phelps CE. Economic foundations of cost-effectiveness analysis. J Health Econ. 1997;16:1–31.
Tengs TO. Cost-effectiveness versus cost-utility analysis of interventions for cancer: does adjusting for health-related quality of life really matter? Value Health. 2004;7(1):70–8.
Matza LS, Patrick DL, Riley A, Alexander J, Rajmil L, Pleil A, Bullinger M. Pediatric patient-reported outcome instruments for research to support medical product labeling: report of the ISPOR PRO good research practices for the assessment of children and adolescents task force. Value Health. 2013;16(4):461–79.
Janssens A, Rogers M, Thompson Coon J, Allen K, Green C, Jenkinson C, et al. A systematic review of generic multidimensional patient-reported outcome measures for children, part II: evaluation of psychometric performance of English-language versions in a general population. Value Health. 2015;18(2):334–45.
Kwon J, Freijser L, Huynh E, Howell M, Chen G, Khan K, et al. Systematic review of conceptual, age, measurement and valuation considerations for generic multidimensional childhood patient-reported outcome measures. Pharmacoeconomics. 2022;40(4):379–431.
Oliveira C, de Silva NT, Ungar WJ, Bayoumi AM, Avitzur Y, Hoch JS, et al. Health-related quality of life in neonates and infants: a conceptual framework. Qual Life Res. 2020;29(5):1159–68.
Bobinac A, van Exel NJA, Rutten FFH, Brouwer WBF. Health effects in significant others: separating family and care-giving effects. Med Decis Making. 2011;31(2):292–8.
Lavelle TA, Wittenberg E, Lamarand K, Prosser LA. Variation in the spillover effects of illness on parents, spouses and children of the chronically ill. Appl J Econ Health Policy. 2014;12(2):117–24.
Brouwer WBF, Van Exel NJA, Van Gorp B, Redekop WK. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res. 2006;15(6):1005–21.
Hopkins C, Whetstone S, Foster T, Blaney S, Morrison G. The impact of paediatric tracheostomy on both patient and parent. Int J Pediatr Ototorhinolaryngol. 2009;73:15–20.
Johnson RF, Brown A, Brooks R. The family impact of having a child with a tracheostomy. Laryngoscope. 2021;131:911–5.
Chandran A, Sikka K, Thakar A, Lodha R, Irugu DVK, Kumar R, et al. The impact of pediatric tracheostomy on the quality of life of caregivers. Int J Pediatr Otorhinolaryngol. 2021;149(July): 110854.
Israelsson-Skogsberg Å, Persson C, Markström A, Hedén L. Children with home mechanical ventilation: parents’ health- related quality of life, family functioning and sleep. Acta Paediatr. 2020;109:1807–14.
Sandler ML, Ayele N, Ncogoza I, Blanchette S, Munhall DS, Marques B, et al. Improving tracheostomy care in resource-limited settings. Ann Otol Rhinol Laryngol. 2020;129(2):181–90.
Salahuddin N, Haider K, Husain SJ, Siddiqui S, Khan FH, Manasia R. Outcome of home mechanical ventilation. J Coll Physicians Surg Pak. 2005;15(7):387–90.
Hung M, Yan Y, Fan P, Lin M, Chen C, Kuo L, et al. Measurement of quality of life using EQ-5D in patients on prolonged mechanical ventilation : comparison of patients, family caregivers, and nurses. Qual Life Res. 2010;19:721–7.
Freeman-Sanderson AL, Togher L, Elkins MR, Phipps PR. Quality of life improves with return of voice in tracheostomy patients in intensive care: an observational study. J Crit Care. 2016;33:186–91.
Gomez-Carballo C, Pedrero S. Long-term outcomes after tracheostomy for COVID-19. Arch Bronconeumol. 2020;57(S2):45–63.
Windisch W. Impact of home mechanical ventilation on health-related quality of life. Eur Respir J. 2008;32:1328–36.
Gul ND, Karadag A. An evaluation of the quality of life in patients with tracheostomy. Pak J Med Sci. 2010;26(2):444–9.
Huttmann SE, Windisch W, Storee JH. Invasive home mechanical ventilation: living conditions and health-related quality of life. Clin Invest. 2015;89:312–21.
Smith KA, Bosch JD, Pelletier G, Mackenzie M, Hoy MY. The development of a tracheostomy-specific quality of life questionnaire: a pilot study. Ann Otol Rhinol Laryngol. 2016;125(8):667–71.
Pandian V, Cole T, Kilonsky D, Holden K, Feller-Kopman DJ, Brower R. Voice-related quality of life increases with a talking tracheostomy tube: a randomized controlled trial. Laryngoscope. 2020;5:1249–55.
Hartnick CJ, Bissell C, Parsons SK. The impact of pediatric tracheotomy on parental caregiver burden and health status. Arch Otolaryngol Head Neck Surg. 2003;129(10):1065–9.
Nauffal DN, Domenech R, Marinez Garcia MA, Compte L, Macian V, Perpina M. Noninvasive positive pressure home ventilation in restrictive disorders: outcome and impact on health-related quality of life. Respir Med. 2002;96:777–83.
Din TF, Mcguire J, Booth J, Lytwynchuk A, Fagan JJ. The assessment of quality of life in children with tracheostomies and their families in a low to middle income country (LMIC ). Int J Pediatr Otorhinolaryngol. 2020;138(August): 110319.
Zenk J, Fyrmpas G, Zimmermann T, Koch M, Constantinidis J, Iro H. Tracheostomy in young patients: indications and long-term outcome. Eur Arch Otorhinolaryngol. 2009;266(5):705–11.
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, et al. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19:539–49.
Noyes J. Comparison of ventilator-dependent child reports of health-related quality of life with parent reports and normative populations. J Adv Nurs. 2007;58(1):1–10.
Kwon J, Smith S, Raghunandan R, Howell M, Huynh E, Kim S, et al. Systematic review of the psychometric performance of generic childhood multi-attribute utility instruments. Appl Health Econ Health Policy. 2023;21(4):559–84.
Verstraete J, Ramma L, Jelsma J. Item generation for a proxy health related quality of life measure in very young children. Health Qual Life Outcomes. 2020;18(1):11.
Verstraete J, Ramma L, Jelsma J. Validity and reliability testing of the Toddler and Infant (TANDI) health related quality of life instrument for very young children. J Patient Rep Outcomes. 2020;4(1):84.
Verstraete J, Ramma L, Jelsma J. Influence of the child’s perceived general health on the primary caregiver’s health status. Health Qual Life Outcomes. 2018;16(1):1–11.
Verstraete J. Does the child’s health influence the caregiver’s health using the EQ-5D instruments ? South Afr J Physiother. 2020;76(1):1343.
Wittenberg E, Ritter GA, Prosser LA. Evidence of spillover of illness among household members: EQ-5D scores from a US population sample. Med Decis Making. 2013;33(2):235–43.
Foster RH, Kozachek S, Stern M, Elsea SH. Caring for the caregivers: an investigation of factors related to well-being among parents caring for a child with smith-magenis syndrome. J Genet Couns. 2010;19(2):187–98.
Gerkensmeyer JE, Johnson C, Scott E, Oruche U, Lindsey LM, Austin JK, et al. Problem-solving intervention for caregivers of children with mental health problems. Arch Psychiatr Nurs. 2013;27(3):112–20.
Zhou T, Yi C, Zhang X, Wang Y. Factors impacting the mental health of the caregivers of children with asthma in China: effects of family socioeconomic status, symptoms control, proneness to shame, and family functioning. Fam Process. 2014;53(4):717–30.
Scott D, Jelsma J. A comparison of the validity of the two EQ-5D-Y proxy version in acutely and chronically ill children in South AFrica: a cross sectional analytical descriptive study: preliminary results. Poster presented at the 33rd Plenary Meeting of the EuroQoL Group; 15-16 September, 2016; Berlin.
Scott D, Ferguson GD, Jelsma J. The use of the EQ-5D-Y health related quality of life outcome measure in children in the Western Cape, South Africa: psychometric properties, feasibility and usefulness: a longitudinal, analytical study. Health Qual Life Outcomes. 2017;15(1):12.
Scott D, Scott C, Jelsma J, Abraham D, Scott D. Validity and feasibility of the self-report EQ-5D-Y as a generic health-related quality of life outcome measure in children and adolescents with juvenile idiopathic arthritis in Western Cape, South Africa. South Afr J Physiother. 2019;75(1):1–9.
Verstraete J, Amien R, Scott D. Comparing the English EQ-5D-Y three-level version with the five-level version in South Africa. Value Health Reg Issues. 2021;30:140–7.
Verstraete J, Amien R, Scott D. Comparing measurement properties of the English EQ-5D-Y 3-Level Version with the 5-Level Version in South Africa. Value Health Region Issues. 2022;30:140–7.
Verstraete J, Scott D. The performance of the EQ-5D-Y-5L compared to the EQ-5D-Y-3L in children and adolescents with cerebral palsy (CP). Dialogues Health. 2022;1(July): 100032.
Verstraete J, Amien R. Cross-cultural adaptation and validation of the EuroQol Toddler and Infant Populations (EQ-TIPS) instrument into Afrikaans for South Africa. Value Health Region Issues. 2023;35:78–86.
Verstraete J, Lloyd AJ, Jelsma J. Performance of the Toddler and Infant (TANDI) health-related quality of life instrument in 3-4-year-old children. Children. 2021;8(920):1–15.
Jelsma J, Maart S. Should additional domains be added to the EQ-5D health-related quality of life instrument for community-based studies? An analytical descriptive study. Popul Health Metrics. 2015;13(1):1–11.
Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res. 2010;19(6):875–86.
EuroQol Research Foundation. EQ-5D-Y user guide version 2.0. Rotterdam; 2020. https://euroqol.org/publications/user-guides.
Lamers L, McDonnell J, Stalmeier PF, Krabbe PF, Busschbach JJ. The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ. 2006;15:1121–32.
Parkin D, Rice N, Devlin N. Statistical analysis of EQ-5D profiles: does the use of value sets bias inference? Med Decis Making. 2010;30(5):556–65.
Boyle SE, Jones GLWS. Quality of life, physical activity, weight status and diet in adolescent school children. Qual Life Res. 2010;19(7):943–54.
Pardo-Guijarro MJ, Woll B, Moya-Martínez P, Martínez-Andrés M, Cortés-Ramírez EE, Martínez-Vizcaíno V. Validity and reliability of the Spanish sign language version of the KIDSCREEN-27 health-related quality of life questionnaire for use in deaf children and adolescents. Gac Sanit. 2013;27(4):318–24.
Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329–41.
Hartnick CJ, Giambra BK, Bissell C, Fitton CM, Cotton RT, Parsons SK. Final validation of the Pediatric Tracheotomy Health Status Instrument (PTHSI). Otolaryngol Head Neck Surg. 2002;126(3):228–33.
World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. J Am Med Assoc. 2013;310(29):2191–4.
Cohen S, Percival A. Prolonged peritoneal dialysis in patients awaiting renal transplantation. Br Med J. 1968;1:409–13.
Verstraete J, Scott D. Comparison of the EQ-5D-Y-5L, EQ-5D-Y-3L and PedsQL in children and adolescents. J Patient Rep Outcomes. 2022. https://doi.org/10.1186/s41687-022-00480-9.
Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
Verstraete J, Lloyd A, Scott D, Jelsma J. How does the EQ-5D-Y proxy version 1 perform in 3, 4 and 5-year-old children? Health Qual Life Outcomes. 2020;18(1):1–10.
Amien R, Scott D, Verstraete J. The validity and reliability of the interviewer-administered EQ-5D-Y-3L version in young children. Health Qual Life Outcomes. 2023. https://doi.org/10.1186/s12955-023-02100-6.
Wittenberg E, Prosser LA. Disutility of illness for caregivers and families: a systematic review of the literature. Pharmacoeconomics. 2013;31(6):489–500.
Szende A, Janssen B, Cabases J. Self-reported population health: an international perspective based on EQ-5D. 2014; p. 212.
Mokkink LB, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, de Vet HCW, et al. COSMIN Study Design checklist for Patient-reported outcome measurement instruments. Amsterdam, The Netherlands. 2019; pp 1–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by University of Cape Town. This study was funded by the EuroQol Research Foundation EQ-426. All views expressed by the authors do not necessarily reflect the views of the EuroQol Group.
Conflicts of Interest
Janine Verstraete receives an honorarium from Merck and is reimbursed for her time on the Younger Populations Working Group of the EuroQol group, receives research grants and is a member of the EuroQol group. Marco Zampoli receives research grants from the EuroQol Group. Christopher Booth, Jane Booth, Shazia Peer, Jessica McGuire, Fiona Kritzinger, Taryn Gray, Noluthando Zibi and Primrose Shabangu have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
Ethics approval was obtained from the University of Cape Town, Faculty of Health Sciences, Human Research Ethics Committee (HREC 740_2021) and institutional approval was obtained from Red Cross War Memorial Children’s Hospital. The study was conducted in accordance with the Declaration of Helsinki.
Consent to Participate
All participants aged older than 8 years provided informed assent to participate in the study. The parents or legal guardians of all children provided informed consent for their own participation and the participation of their child.
Consent for Publication
All participants provided informed assent and their parent or legal guardian provided informed consent to have the findings of this study published.
Availability of Data and Material
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Authors’ Contributions
JV contributed towards the proposal development, conception and design of the study, ethical submission, sourcing of funding, data collection and analysis, discussion and conclusion, and development of the manuscript. MZ contributed to the proposal development and manuscript development. CB, JB, PS and NZ contributed to proposal development, data collection and manuscript development. SP, JM, TG and FK contributed to proposal development and critical revision of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Verstraete, J., Booth, C., Booth, J. et al. Fighting to Breathe and Fighting for Health-Related Quality of Life: Measuring the Impact of Being Dependent on Technology for Breathing on the Child and Their Caregiver. Patient 17, 65–82 (2024). https://doi.org/10.1007/s40271-023-00657-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-023-00657-4