Abstract
Objectives
This study aimed to quantify adult preferences for adjuvant immunotherapy for resected melanoma and the influence of varying levels of key attributes and baseline characteristics.
Methods
A D-efficient design generated 12 choice tasks for two alternative treatments, adjuvant immunotherapy or no adjuvant immunotherapy. Recruitment to the online discrete choice experiment (DCE) occurred via survey dissemination by eight Australian melanoma consumer and professional groups, targeting adults with resected stage III melanoma, considering or having received adjuvant immunotherapy. The DCE included six attributes with two to three levels each, including 3-year risk of recurrence, mild, permanent and fatal adverse events (AEs), drug regimen and annual out-of-pocket costs. A mixed multinomial logit model was used to estimate preferences and calculate marginal rates of substitution and marginal willingness to pay (mWTP).
Results
The DCE was completed by 116 respondents, who chose adjuvant immunotherapy over no adjuvant immunotherapy in 70% of choice tasks. Respondents preferred adjuvant immunotherapy when associated with reduced: probabilities of recurrence, permanent and fatal AEs, and out-of-pocket costs. mWTP for an absolute reduction of 1% in 3-year risk of recurrence was less for respondents with lower rather than higher incomes, AU$794 (US$527) and AU$2190 (US$1454) per year. Respondents accepted an additional 4% chance of a permanent AE to reduce their absolute risk of 3-year recurrence by 1%. Respondents were willing to accept an extra 2% chance of 3-year recurrence to lower their chance of a fatal AE by 1%.
Conclusions
Almost three-quarters of respondents chose adjuvant immunotherapy over no adjuvant immunotherapy, preferring treatment that improved efficacy and safety. Findings may inform decisions about access to adjuvant immunotherapy following surgery for melanoma.
Plain Language Summary
Melanoma is the deadliest type of skin cancer. Treatment for melanoma involves surgery to remove it and can be followed by extra (adjuvant) immunotherapy, a type of drug that uses the body's immune system to fight any leftover melanoma. Immunotherapy can help a person live longer (benefits) but has downsides or side-effects (risks) that may need a person to take daily medication for life. We surveyed people with melanoma to learn what was important to them and which immunotherapy treatment risks were acceptable in order to gain benefits (trade-offs). People preferred treatment that lowered the chance of the melanoma returning and lowered the chance of dying from a treatment side-effect. People accepted an extra 4% (4 per 100) chance of a life-long treatment side-effect to lower the chance of their melanoma returning by 1% (1 per 100). This information will help doctors, nurses and governments to consider what treatment options are available to people with melanoma and their families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Respondents with stage III melanoma prefer adjuvant immunotherapy that reduces their risk of recurrence, reduces treatment adverse events and costs less. |
Almost three-quarters of respondents chose adjuvant immunotherapy over no adjuvant immunotherapy. Preferences were found to statistically differ by the amount of immunotherapy experience and being female; women were significantly less accepting of treatment. Respondents were willing to pay between AU$794 and AU$4266 (US$527–2833) depending on income, for adjuvant immunotherapy per year to reduce their risk of immediate death and recurrence by 1%. |
Health policymakers should consider respondents’ trade-offs and remove financial barriers to enable access to effective therapies. |
1 Introduction
Melanoma incidence continues to increase globally [2]. In Australia, the lifetime risk of melanoma rose from 1 in 46 people in 1982 to an estimated 1 in 15 in 2020 [3]. Over the past decade, advances in treating stage IV metastatic melanoma using checkpoint inhibitor immunotherapy or BRAF-targeted therapy have revolutionised care, with 5-year overall survival now greater than 50% [4, 5]. Such gains have been applied in the adjuvant stage III setting. In an era before immunotherapy, 10-year overall survival for resected stage IIIA–D melanoma was 24–88%, worsening with sub-stage [6].
However, adjuvant checkpoint inhibitor immunotherapy (adjuvant immunotherapy) is associated with possible short- and long-term side-effects, including fatigue, skin rash, arthralgia, diarrhoea, hormone deficiencies (thyroid, pituitary and pancreatic) and other immune-related adverse effects. In the post-operative setting, respondents without active overt residual (metastatic) disease might be reluctant to commence a 12-month regimen of treatment (i.e. adjuvant therapy) to prevent future melanoma recurrence. Previous research suggests around one-tenth of respondents with stage III resected melanoma are reluctant to commence immunotherapy, with a further fifth requiring early cessation of treatment due to toxicity [7]. Additionally, such treatments may be costly, as in Australia adults receiving immunotherapy may have substantial out-of-pocket costs [8]. Therefore, it is imperative to understand and quantify what treatment risks respondents are willing to accept to gain benefits (trade-offs).
Generating meaningful information to inform policy and allocation of healthcare resources requires quantification of respondents’ preferences and should be considered by regulatory agencies [9, 10]. Consistent with prior research from our group, key drivers for respondents with resected stage III melanoma considering adjuvant immunotherapy included extending life, uncertainty about treatment efficacy, appetite for risk, treatment burden and out-of-pocket (OOP) costs [7]. Discrete choice experiments (DCEs) are commonly used to quantify preferences for healthcare services or treatments, exploring the trade-offs respondents are willing to make [11]. A DCE is a series of questions (a survey) showing two or more alternatives, described by a set of attributes (factors) with varying levels. Multiple choice tasks or scenarios are presented to respondents, in which the levels of each attribute are varied. Respondents consider all the information presented in the choice task and are asked to select the alternative they most prefer [12, 13]. This generates a dataset that enables the analyst to quantify preferences, the relative importance of attributes, and trade-offs between attributes for the group as a whole [14].
This study aimed to quantify adults’ preferences for adjuvant checkpoint inhibitor immunotherapy for resected melanoma and the influence of varying levels of key attributes, and baseline characteristics. Additionally, calculation of trade-offs, marginal rates of substitution (MRS) for adjuvant immunotherapy and marginal willingness to pay (mWTP) per year are reported.
2 Methods
2.1 Respondent Recruitment and Setting
Australian adults who self-reported having surgery for resected stage III melanoma were invited to participate in an online DCE about adjuvant immunotherapy. Respondents were excluded if they were younger than 18 years, had stage I–II or stage IV melanoma or did not consent. Respondents did not receive payment for survey completion. The DCE was designed and conducted according to best practice methods [15,16,17,18]. The survey was hosted on the Qualtrics survey platform (version July 2021) and disseminated by eight Australian melanoma consumer and professional groups, including the Melanoma Institute Australia, Melanoma Patients Australia, Melanoma Research Victoria, the Melanoma and Skin Cancer Advocacy Network, Melanoma WA, Skin Cancer Tasmania, Melanoma and Skin Cancer Trials, and the Hunter Melanoma Foundation. All respondents provided written consent, and the Declaration of Helsinki underpinned this study. Data collection occurred between July and September 2021, with ethical approval granted by the Sydney Local Health District Human Research Ethics Committee (HREC/18/RPAH/736).
2.2 Selection of Attributes and Levels
Attributes and levels were informed by existing literature [19,20,21,22,23,24,25,26], focus groups and interviews with respondents with resected stage III melanoma (n = 24) [7], expert consultation, adjuvant immunotherapy trials of resected stage III melanoma, and pilot testing. As per Table 1, the DCE included six attributes with two to three levels each.
2.3 Study Design
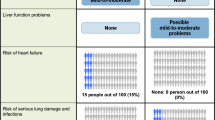
This DCE presented respondents with two treatment alternatives and asked them to choose one or the other. The DCE included an explanation of the choice questions, definitions of the attributes and levels, 12 hypothetical choice tasks and socio-demographic questions. Respondents were provided with a brief description of the choice context, i.e. “As a person with resected stage III melanoma, we ask you to consider treatment with adjuvant immunotherapy, a drug that uses the body’s immune system to fight any leftover melanoma cells” (Fig. 1).
Respondents were provided with a brief description of the choice context: i.e. “As a person with resected stage III melanoma, we ask you to consider treatment with adjuvant immunotherapy, a drug that uses the body’s immune system to fight any leftover melanoma cells.”
A literature review and in-depth discussion with investigators drawing on their clinical knowledge and experience informed the alternatives, attributes and levels included in the choice set. A D-efficient design was generated using Ngene version 1.2.1 software, consisting of two labelled alternatives of 72 choice questions in six blocks of 12 questions. Options consisted of drug treatment (adjuvant immunotherapy) versus no adjuvant immunotherapy. In both scenarios, respondents undergo regular monitoring, including clinical assessments, imaging and blood tests. Respondents’ socio-demographic and clinical factors collected included age, gender, have children (yes/no), education, annual pre-tax household income, melanoma sub-stage and treatment received. Accordingly, the author hypothesised that the following traits might influence treatment choices: age, disease sub-stage, children and income. Respondent characteristics were coded numerically with ‘unknown’ melanoma sub-stage coded as missing data.
As per recommended guidelines, selecting the final six attributes was based on stakeholder feedback and ease of survey completion [15, 27]. Adjuvant immunotherapy trials of respondents with resected stage III melanoma informed the levels for four of the six attributes, namely the chance of 3-year melanoma recurrence and the three treatment toxicity attributes. These included the chance of melanoma recurrence at 3 years (levels 36%, 42%, 50%, 56% or 62%); the chance of a mild adverse event (AE) (levels 0%, 1%, 12% or 37%); the chance of a permanent AE (levels 0%, 1%, 10% or 14%); and the chance of fatal AE (levels 0%, 1% or 3%). For the remaining two attributes, drug regimen (levels 0-, 3- or 4-weekly treatment) was as per approved treatment guidelines [28, 29], and respondent OOP cost (levels AU$0, $750, $1500 or $6000) was informed by focus groups, interviews and the literature [8]. Following extensive consultation with medical oncologists, the levels for no adjuvant immunotherapy AEs (mild, permanent and fatal) were set at 0%.
Annual household income consisted of four categories (≤ AU$43,999, AU$44,000–$87,999, AU$88,000–$175,999 and ≥ AU$176,000) for analysis purposes, splitting categories into two, low-income (combining the two lower-income ranges, ≤ AU$87,999) and high-income (combining the two higher-income ranges, ≥ AU$88,000). The authors hypothesised that respondent OOP costs would likely interact with the annual pre-tax household income; therefore, an interaction between income and cost was created, and coded in the design to respecify the model. Further, a priori, the author hypothesised that respondents would be more likely to prefer adjuvant immunotherapy that meant less frequent treatment (i.e. 4-weekly versus 3-weekly); reduced their chance of recurrence; lowered the number of mild, permanent and fatal AEs; and reduced OOP costs.
The survey design in Ngene included six blocks of 12 choice tasks. The design had two constraints; first, the AU$6,000 ‘out-of-pocket cost per year’ was not displayed for 4-weekly immunotherapy treatments, as more frequent drug delivery (i.e. 3-weekly) was likely to be associated with the higher cost. Second, to address dominance across the alternatives, the ‘chance of melanoma recurrence’ could not be equal (i.e. 50%) across both alternatives. The pilot and main DCE study used this design. Figure 1 provides an example DCE choice question.
2.4 Pilot Study
The DCE was piloted on respondents with resected stage III melanoma (n = 21) to assess face validity and acceptability. Additionally, 10 of the 21 respondents undertaking the pilot study completed face-to-face ‘think aloud’ feedback with the researcher. The ‘think aloud’ process allows respondents to verbalise their thoughts when completing any task [30]. Respondents verbalised their reasoning for choosing choice tasks, discussed their understanding of the questions and the survey look and feel, and confirmed face validity. Examples of survey refinement included revision of clinical terms [e.g. diabetes or hypophysitis (loss of pituitary gland function)] and removal of treatment options (e.g. interferon). The pilot study results generated prior parameter estimates for the main DCE. The pilot results were not included in the main study results; however, six respondents completed the pilot and main study DCEs.
2.5 Analyses
DCE survey analysis assesses the relationship between the choices made and the differences in the attributes used to describe profiles (i.e. the distinct combinations of attributes levels displayed) resulting in those choices [18, 31, 32]. DCE analyses used NLOGIT version 6 software [33]. Analyses initially used a multinomial logit (MNL) model; however, a limitation of this model is the use of the same preference weights (homogeneous) applied to all respondents [16]. Further analyses used mixed multinomial logit (MMNL) models; assumptions accommodated the data’s cross-sectional panel structure and preference heterogeneity, meaning one or more parameter estimates are randomly distributed among individuals [15, 16]. Additionally, the model choice was based around the assumption that error terms were independent and identically distributed, preference heterogeneity and how flexible respondents were about substituting between options [34]. A linear functional form was used, and testing of other functional forms completed; however, they did not improve the model fit. Further, sensitivity analyses of the model specification were considered, resulting in testing the plausible variations in the model assumptions, for example, subgroup analyses. MNL analyses are not presented as they did not add any explanatory value over the final MMNL analyses.
To minimise respondent fatigue, choice sets were limited to 12 per person. Additionally, MMNL model assumptions and the use of NLOGIT software accounted for the non-independence between observations completed by the same respondent [33].
The MMNL expresses the utility to person n from choosing alternative j in choice scenario t:
where β is the weighting of the attributes, ηn is a random term capturing non-observable person-specific variation, such as preferences. The random error ε includes random variation across discrete choices. The following equation expresses the utility function (i.e. the total satisfaction received from consuming a good or service) [35] of the final MMNL model:
Of the six attributes, two categorical attributes were dummy coded and did not reach statistical significance (p > 0.05) in the MNL model (i.e. the chance of mild AEs and drug regimen). The remaining four attributes were treated as continuous (linear) (i.e. the chance of recurrence at 3 years, fatal and permanent AEs, and OOP cost). All 15 parameters were specified as random, and if not statistically significant (i.e. p > 0.05), parameters were re-specified as non-random. The final MMNL model had 12 random parameters (eight normally distributed parameters and four cost parameters that used a constrained triangular distribution) [36] and three non-random parameters. All parameters were specified as main effects, except the cost parameters, which were interacted with low- and high-income categories; the model was run using 10,000 Halton draws. The log-likelihood ratio test, McFadden’s pseudo-R [2] value and normalised Akaike’s information criterion (AIC/N) assessed the goodness of model fit.
Socio-demographic and clinical characteristics hypothesised to influence choices included age, gender, children yes/no and melanoma sub-stage (i.e. American Joint Committee on Cancer, AJCC, 8th edition stage IIIA-D) [6] were interacted in the model with the alternative specific constant. These were added to models, and then removed if the improvement in model fit was not statistically significant (i.e. p > 0.05). Melanoma sub-stage was added to the model as the likelihood of recurrence increases with more extensive disease. Authors hypothesised that as the chance of recurrence increased, so would the preference for immunotherapy. Coefficients of the parameters, and post-estimation odds ratios (OR) with their 95% confidence intervals (CI) and p-values are reported. Odds ratios are interpreted regarding the likelihood of preferring adjuvant immunotherapy per specified change in the level of that attribute. Thus, the smaller the OR, the less likely the respondent is to select treatment per each increase in the level of that attribute (OR < 1); conversely, the larger the OR, the more likely the respondent is to prefer treatment per each decrease in the level of that attribute (OR ≥ 1).
Calculation of the marginal rate of substitution (MRS) and marginal willingness to pay (mWTP) used the delta method (a method used to measure the variability of data, and the variability between variables often used to calculate the 95% confidence intervals) [17]. The MRS was calculated by dividing the coefficients of the attributes of interest by each other, providing information on the rate respondents were willing to trade levels of one attribute for another [37]. Similarly, calculation of the mWTP by dividing the coefficient of an attribute of interest by the cost coefficient, providing an individual’s maximum price to trade levels of that attribute [38]. Cost attributes used a constrained triangular distribution [36]. MRS values for trading the chance of a permanent AE for a reduction in the chance of 3-year recurrence, and the chance of 3-year recurrence for a reduction in the chance of a fatal AE, are reported. mWTP for a 1% lower chance of recurrence and a 1% lower chance of a fatal AE were reported separately for respondents with lower and higher household incomes.
The ESTIMATE checklist informed our approach for reporting a DCE (Table 2) [18].
3 Results
3.1 Respondents
Analysis was undertaken using complete survey data from 116 respondents. We excluded 28 duplicates (more than one response by the same respondent), 35 incomplete responses and 90 surveys from respondents who were ineligible or did not consent (Fig. 2). The final 116 respondents had a median age of 60 years (range 26–82 years); 53% were female, and 79% had received adjuvant immunotherapy. Most respondents (84%) resided in New South Wales or Victoria and were aged 45–64 years (Table 3).
3.2 Mixed Multinomial Logit Model Results (MMNL)
Respondents chose adjuvant immunotherapy over no adjuvant immunotherapy in 70% of the choice tasks. Over a third of respondents (n = 41) always chose drug treatment, i.e. drug treatment was selected in all 12 of the 12 choice tasks. MMNL results suggest respondents were less likely to prefer treatment that increased the absolute risk of recurrence (OR 0.76 per 1% higher risk of recurrence over 3 years, 95% CI 0.70–0.83, p < 0.001); or treatment that had a higher chance of fatal AEs (OR 0.60 per 1% increase in the chance of fatal AE, 95% CI 0.44–0.80, p = 0.006); or treatment that had a higher chance of permanent AEs (OR 0.94 per 1% higher chance of permanent AE, 95% CI 0.89–0.99, p < 0.05). Further, for each $1000 increase in annual OOP costs, respondents with incomes that were low compared to high were less likely to prefer adjuvant immunotherapy, (OR 0.63, 95% CI 0.47–0.85, p < 0.01) and (OR 0.84, 95% CI 0.15–4.86, p = 0.06) (Table 4 and Fig. 3).
Of the respondent characteristics included in the model (age, have children yes/no, melanoma sub-stage and annual household income), preferences were found to statistically differ by gender, with females having a lower preference for immunotherapy than males (OR 0.10, 95% CI 0.02–0.66, p = 0.02) (Table 4).
Further, the model was rerun using subgroups of the sample. Subgroup analyses investigated the preferences of respondents who had received immunotherapy (n = 92) versus those who had not (n = 22). Respondents treated with immunotherapy were grouped into those ceasing immunotherapy because of toxicity (n = 17) versus those who continued treatment (n = 75) (Table 4).
Compared with the total sample, respondents who ceased immunotherapy because of toxicity (n = 17) chose adjuvant immunotherapy treatment over no adjuvant immunotherapy 63% of the time, 7% less than the whole cohort. Other socio-demographic and clinical characteristics were similar for the entire group, except for zero stage IIIA disease, and 10% more respondents reported the highest income level (≥ AU$176,000). Compared with the total sample, preferences for adjuvant immunotherapy were similar, except for a stronger preference to lower the chance of a permanent AE (OR 0.77, 95% CI 0.61–0.96, p = 0.02). For this cohort, the reduction in the likelihood of a fatal AE (OR 0.46, 95% CI 0.15–1.38, p = 0.16), and each $1000 increase in annual OOP costs, were less of a concern with incomes that were lower (OR 1.18, 95% CI 0.74–1.89, p = 0.10) rather than higher (OR 2.08, 95% CI 0.86–5.01, p = 0.94). Further, preferences did not statistically differ by gender (Table 4).
Compared with the total sample, survey respondents that underwent immunotherapy and did not stop it due to toxicity (n = 75), chose adjuvant immunotherapy 76% of the time, which was 6% higher than the total sample. Compared with the whole sample, a reduction in the chance of a permanent AE was of less concern (OR 0.97, 95% CI 0.91–1.04, p = 0.39). Similarly, the acceptability of an increase in the chance of experiencing a mild AE from 1% to 37% concerned this group less (OR 1.17, 95% CI 0.58–2.38, p = 0.66) (Table 4).
For the 22 respondents who did not receive adjuvant immunotherapy, mild, permanent or fatal AE attributes did not significantly affect preferences. Of those not treated with immunotherapy, almost a quarter would have been eligible for treatment (i.e. stage IIIB-D melanoma). Further, preferences did not statistically differ by gender (Table 4).
3.3 Trade-Offs (Marginal Rates of Substitution) and Marginal Willingness-to-Pay Estimates
On average, respondents were willing to accept an additional 4% chance of a permanent AE to reduce their absolute risk of recurrence at 3 years by 1% (95% CI – 10.44 to 23.41). Respondents were willing to accept an extra 2% chance of recurrence at 3 years to lower their chance of a fatal AE by 1% (95% CI – 12.35 to 34.54) (Table 5).
Respondents with lower household income were, on average, willing to pay an extra AU$794 (95% CI – AU$741 to AU$1,745) (US$527, 95% CI – US$492 to US$1159) per year and, for higher income, an additional AU$2190 (95% CI −AU$1651 to AU$4,571) (US$1454, 95% CI – US$1096 to US$13,035) for each 1% reduction in their absolute risk of recurrence at 3 years with adjuvant immunotherapy. Further, respondents with lower income were, on average, willing to pay AU$1531 (95% CI – AU$1527 to AU$8417) (US$1017, 95% CI – US$1014 to US$5589), for a 1% lower chance of fatal AE compared with a higher income, AU$4266 (95% CI – AU$3484 to AU$13,997) (US$2832, 95% CI – US$2314 to US$9295) (Table 5). Additionally, respondents were willing to accept an increase in their likelihood of experiencing a mild AE from 1% to 37% (OR 2.06, 95% CI 1.13–3.78, p = 0.02) in return for adjuvant immunotherapy (Table 4).
4 Discussion
Results suggest that respondents with resected stage III melanoma had an overall preference for adjuvant immunotherapy over no adjuvant immunotherapy, with 70% choosing adjuvant treatment across the choice tasks. Respondents in our sample prefer treatments with an absolute reduction in the risk of recurrence, reduced probabilities of fatal and permanent AEs, and lower yearly OOP costs. However, respondents accepted a substantial increase in their chance of experiencing mild AEs in return for adjuvant immunotherapy. Respondents were willing to trade a slight increase in the chance of a permanent AE to reduce their chance of recurrence at 3 years and a slight increase in the likelihood of 3-year recurrence to lower their chance of a fatal AE.
Subgroup analysis of the 17 respondents who ceased adjuvant immunotherapy for toxicity revealed that lowering the chance of a fatal AE was of less concern; however, this finding may be due to the small sub-sample size. Additionally, despite ceasing treatment because of toxicity (n = 17), this group appeared willing to choose adjuvant immunotherapy over no adjuvant immunotherapy almost as frequently as the total sample, 63% of the time compared with 70% of the time. Further, the 75 respondents who received immunotherapy without cessation because of toxicity chose adjuvant immunotherapy 76% of the time, 6% more than the entire group. This finding suggests respondents receiving immunotherapy treatment without AEs, still chose no adjuvant immunotherapy in almost a quarter of the choice tasks. Preferences were found to statistically differ by gender (p = 0.02), with females having a lower preference for immunotherapy treatment than males. For respondents who had not received immunotherapy treatment, AEs did not drive their treatment choices; suggesting those who have experienced AEs possess additional information to inform decisions.
Prior DCE research confirms that respondents with stage III–IV melanoma prefer to avoid fatal AEs, such as colitis, and permanent AEs, including changes in hormone gland function [23, 24]. Similarly, US respondents with self-reported unresectable or metastatic melanoma preferred to maximise their objective response rate and minimise severe treatment toxicities in the stage IV setting [20]. Further, a conference abstract of an Australian DCE of stage III–IV melanoma respondents asked about single and double immunotherapy and targeted therapy preferences [25]. Likewise, results reported that efficacy attributes were most preferred, and adverse events and higher costs were least preferred. Our results align with prior melanoma research, confirming that respondents never treated with adjuvant immunotherapy had fewer concerns about AEs [21]. Lastly, our findings align with two earlier DCEs reporting patients with resected melanoma selected the ‘no treatment’ option, 32% [26], and 29% of the time [24], compared with 30% in our resected stage III melanoma sample.
Regarding demographic characteristics, females had a significantly lower preference for immunotherapy than males; this differed from prior melanoma DCEs showing preferences for treatment did not differ by gender [21]. Conversely, other cancer research supported our findings of gender differences for cancer treatment, with women with resected stage I–III non-small cell lung cancer more likely to decline adjuvant chemotherapy than men [39]. Additionally, the authors acknowledge that these findings may be relevant in other cancers where adjuvant immunotherapy is routine care.
To our knowledge, this DCE is the first to investigate and publish preferences for adjuvant checkpoint inhibitor immunotherapy alone, for respondents with resected stage III melanoma. Interestingly, respondents preferred to avoid the short-term risk of death from melanoma by lowering their likelihood of experiencing a fatal AE over their longer-term risk of death, such as reducing their chance of recurrence in 3 years. One possible explanation for respondent behaviour may be that recurrence was viewed differently to death. In stage IV melanoma, immunotherapy may be curative, unlike other cancer treatments such as chemotherapy. Therefore, recurrence might not result in death, whereas a fatal AE ensures immediate loss of life. Concordantly, respondents willingly accepted a slight increase in recurrence at 3 years to lower their chance of a deadly AE. Findings may explain the potential trade-offs respondents were willing to accept to lower the likelihood of fatal treatment toxicity and reduce the risk of recurrence.
Given the increasing cost of cancer care, health service providers need to rationalise costly cancer treatments and consider respondent OOP costs. In Australia, the government reimburses adjuvant immunotherapy drug costs for respondents with resected stage III melanoma. However, respondent OOP costs may be considerable, meaning therapy has a financial cost [8]. Consequently, unlike many earlier melanoma DCEs, our study included a respondent OOP cost attribute, as prior qualitative research identified this as an important consideration in treatment decision-making [7].
Further, lower- and higher-income respondents were willing to pay an additional AU$794 (US$527) and AU$2190 (US$1454), per year respectively, for adjuvant immunotherapy to reduce their absolute risk of recurrence at 3 years by 1%. Findings support that governments and healthcare payers should focus on removing respondents’ financial barriers, enabling equitable access to effective treatments that align with respondent preferences, such as adjuvant immunotherapy.
Study limitations include the potential for selection bias as most of the respondents recruited to this study received adjuvant immunotherapy treatment. Additionally, research has shown that respondents prefer what they know instead of the unknown, which may account for most respondents choosing immunotherapy [40]. Second, the authors hypothesised that as the sub-stage of disease increases, so might the preference for adjuvant immunotherapy. Unfortunately, over a quarter of respondents reported their melanoma sub-stage as ‘unknown’, resulting in the coding of these responses as missing data. Such misinformation might contribute to the sub-stage not being statistically significant at the 5% level. Additionally, it is acknowledged that subgroup sample sizes were small. Specifically for the 17 respondents who ceased immunotherapy due to toxicity, the authors accept it is difficult to conclude with certainty these findings, which are at best hypothesis generating and require further research with larger samples, and control for differences in scale [41, 42]. Nevertheless, the design generated a small D-error of 0.001708; the smaller the number, the better the design [16], proving that the sample size was adequate to quantify preferences and identify statistically significant attributes. Further, the attribute levels for AEs for the no adjuvant immunotherapy alternative were assumed to be zero. However, adjuvant trials of checkpoint inhibitor immunotherapy demonstrate that a small percentage of respondents receiving placebo report a substantial number of AEs [43]. Lastly, we did not include tests of internal validity [44].
Globally, rapid changes in the treatment of earlier stage melanoma continue. Findings from two phase 3 randomised clinical trials have demonstrated a significant reduction in the risk of recurrence with anti-PD1 checkpoint inhibitors, with a relative reduction in the risk of recurrence of approximately 40% versus no therapy [43, 45]. These findings have led to the approval of both nivolumab and pembrolizumab to treat adjuvant melanoma. Authors deliberately focused on issues about adjuvant anti-PD1 checkpoint inhibitor immunotherapy for respondents with resected stage III melanoma and the potential trade-offs of treatment benefits and risks. Following the recent results indicating the benefits of adjuvant immunotherapy in high-risk stage II disease, this warrants further research [46]. Additionally, preferences for immunotherapy in stage IV are likely to differ and require further investigation.
5 Conclusions
This DCE is the first to investigate the preferences for adjuvant checkpoint inhibitor immunotherapy for respondents with resected stage III melanoma. Most respondents chose adjuvant immunotherapy over no adjuvant immunotherapy, especially if treatment affords high efficacy and improves safety. Preferences were found to statistically differ by the amount of immunotherapy experience and being female. Further, those reporting treatment toxicities preferred to reduce the risk of permanent AEs.
Evidently, trade-offs demonstrate that respondents accept an increase in the odds of disease recurrence to lower their immediate risk of death. Respondents would trade a higher risk of permanent AEs to reduce their absolute risk of recurrence. Consideration of respondent preferences and trade-offs for adjuvant immunotherapy following surgery for melanoma may assist policymakers regarding access and subsidisation of effective yet expensive treatments.
References
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. https://doi.org/10.1001/jama.2013.281053.
World Health Organization. Global Cancer Observatory 2020. International Agency for Research on Cancer. https://gco.iarc.fr/. Accessed 10 Jan 2022
Australian Institute of Health and Welfare [AIHW]. Cancer in Australia. Accessed 10 Oct 2022. https://www.aihw.gov.au/getmedia/0ea708eb-dd6e-4499-9080-1cc7b5990e64/aihw-can-144.pdf.aspx?inline=true
Robert C, Ribas A, Schachter J, et al. Pembrolizumab versus ipilimumab in advanced melanoma (KEYNOTE-006): post-hoc 5-year results from an open-label, multicentre, randomised, controlled, phase 3 study. Lancet Oncol. 2019;20(9):1239–51. https://doi.org/10.1016/S1470-2045(19)30388-2.
Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2019;381(16):1535–46. https://doi.org/10.1056/NEJMoa1910836.
Gershenwald JE, Scolyer RA, Hess KR, et al. Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(6):472–92. https://doi.org/10.3322/caac.21409.
Livingstone A, Milne D, Dempsey K, et al. Should I have adjuvant immunotherapy? An interview study among adults with resected stage 3 melanoma and their partners. Patient. 2021. https://doi.org/10.1007/s40271-021-00507-1.
Rodriguez-Acevedo AJ, Chan RJ, Olsen CM, Pandeya N, Whiteman DC, Gordon LG. Out-of-pocket medical expenses compared across five years for patients with one of five common cancers in Australia. BMC Cancer. 2021;21(1):1055. https://doi.org/10.1186/s12885-021-08756-x.
Medical Device Innovation Consortium [MDIC]. Patient Centered Benefit-Risk Project Report: A Framework for Incorporating Information on Patient Preferences Regarding Benefit and Risk into Regulatory Assessments of New Medical Technology. Accessed 10 Oct 2022. https://www.fda.gov/media/95591/download.
European Medicines Agency. Regulatory and methodological standards to improve benefit-risk evaluation of medicines. 2014. 10 Oct 2022. https://www.ema.europa.eu/en/documents/report/regulatory-methodological-standards-improve-benefit-risk-evaluation-medicines-workshop-report_en.pdf.
Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32(9):883–902. https://doi.org/10.1007/s40273-014-0170-x.
Train K. Discrete choice methods with simulation. Cambridge University Press; 2003.
Wong YN, Egleston BL, Sachdeva K, et al. Cancer patients’ trade-offs among efficacy, toxicity, and out-of-pocket cost in the curative and noncurative setting. Med Care. 2013;51(9):838–45. https://doi.org/10.1097/MLR.0b013e31829faffd.
Ryan M, Gerard K, Amaya-Amaya M. Using discrete choice experiments to value health and health care. Springer; 2008.
Bridges JFP, Hauber AB, Marshall D, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value in Health. 2011;14:403–13. https://doi.org/10.1016/j.jval.2010.11.013.
Hensher DA, Rose JM, Greene WH. Applied choice analysis. 2nd ed. Cambridge University Press; 2015.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–77. https://doi.org/10.2165/00019053-200826080-00004.
Hauber AB, Gonzalez JM, Groothuis-Oudshoorn CGM, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ISPOR Conjoint Analysis Good Research Practices Task Force. Value Health. 2016;19(4):300–15.
Liu FX, Witt EA, Ebbinghaus S, DiBonaventura BG, Basurto E, Joseph RW. Patient and oncology nurse preferences for the treatment options in advanced melanoma: a discrete choice experiment. Cancer Nurs Jan/Feb. 2019;42(1):E52–9. https://doi.org/10.1097/NCC.0000000000000557.
Liu FX, Witt EA, Ebbinghaus S, et al. Patient and oncologist preferences for attributes of treatments in advanced melanoma: a discrete choice experiment. Patient Prefer Adherence. 2017;11:1389–99. https://doi.org/10.2147/PPA.S140226.
Weilandt J, Diehl K, Schaarschmidt ML, et al. Patient preferences in adjuvant and palliative treatment of advanced melanoma: a discrete choice experiment. Acta Derm Venereol. 2020;100(6):adv0083. https://doi.org/10.2340/00015555-3422.
Livingstone A, Agarwal A, Stockler MR, Menzies AM, Howard K, Morton RL. Preferences for immunotherapy in melanoma: a systematic review. Ann Surg Oncol. 2020;27(2):571–84. https://doi.org/10.1245/s10434-019-07963-y.
Mansfield C, Ndife B, Chen J, Gallaher K, Ghate S. Patient preferences for treatment of metastatic melanoma. Future Oncol. 2019;15(11):1255–68. https://doi.org/10.2217/fon-2018-0871.
Stenehjem DD, Au TH, Ngorsuraches S, et al. Immunotargeted therapy in melanoma: patient, provider preferences, and willingness to pay at an academic cancer center. Melanoma Res. 2019;29(6):626–34. https://doi.org/10.1097/CMR.0000000000000572.
Huynh E, Rose J, Lambides M, Cong K, Herawati L, Cuore MD. Preferences for advanced melanoma immuno-oncology treatments. In: Presented at: Pigment Cell and Melanoma Research; 2018.
Beusterien K, Middleton MR, Wang PF, et al. Patient and physician preferences for treating adjuvant melanoma: a discrete choice experiment. J Cancer Ther. 2017;8(1):37–50. https://doi.org/10.4236/jct.2017.81004.
Trapero-Bertran M, Rodriguez-Martin B, Lopez-Bastida J. What attributes should be included in a discrete choice experiment related to health technologies? A systematic literature review PLoS One. 2019. https://doi.org/10.1371/journal.pone.0219905.
Australian Government. Pharmaceutical Benefits Scheme - Nivolumab. Webpage. Australian Government. 20 August 2020. https://www.pbs.gov.au/medicine/item/10745M-10748Q-10764M-10775D-11143L-11150W-11152Y-11153B-11157F-11158G-11159H-11160J-11411N-11425H-11434T-11435W-11532Y-11543M-11626X-11627Y-11631E-11635J-11636K-11642R-11900H-11906P. Accessed 20 Aug 2020.
Australian Government. Pharmaceutical Benefits Scheme - Pembrolizumab. Webpage. Australian Government. 10 September 2020. https://www.pbs.gov.au/medicine/item/10424P-10436G-10475H-10493G-11330H-11352L-11492W-11494Y-11632F-11646Y-12119W-12120X-12121Y-12122B-12123C-12124D-12125E-12126F-12127G-12128H-12129J-12130K. Accessed 10 Sep 2020.
van Someren M, Barnard Y, Sandberg J. The think aloud method: a practical approach to modelling cognitive processes. Academic Press; 1993.
Reed Johnson F, Lancsar E, Marshall D, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health Jan-Feb. 2013;16(1):3–13. https://doi.org/10.1016/j.jval.2012.08.2223.
Muhlbacher A, Johnson FR. Choice experiments to quantify preferences for health and healthcare: state of the practice. Appl Health Econ Health Policy. 2016;14(3):253–66. https://doi.org/10.1007/s40258-016-0232-7.
Green WH. NLOGIT Version 6 reference guide. Econometric Software Inc. Accessed 6 Sept 2021.
Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past, present and future. Pharmacoeconomics. 2019;37(2):201–26. https://doi.org/10.1007/s40273-018-0734-2.
Morris S, Devlin N, Parkin D, Spencer A. Economic analysis in health care. 2nd ed. Berlin: Wiley; 2012.
Hess S, Train K. Correlation and scale in mixed logit models. Journal of Choice Modelling. 2017;23:1–8.
Mott DJ, Chami N, Tervonen T. Reporting quality of marginal rates of substitution in discrete choice experiments that elicit patient preferences. Value Health. 2020;23(8):979–84.
Varian H. Microeconomic analysis. W.W. Norton; 1992.
Blinman P, Hughes B, Crombie C, et al. Patients’ and doctors’ preferences for adjuvant chemotherapy in resected non-small-cell lung cancer: what makes it worthwhile? Eur J Cancer. 2015;51(12):1529–37.
Salkeld G, Ryan M, Short L. The veil of experience. Do consumers prefer what they know best? Health Econ. 2000;9(3):267–70.
Norton EC, Dowd BE. Log odds and the interpretation of logit models. Health Serv Res. 2018;53(2):859–78. https://doi.org/10.1111/1475-6773.12712.
Lancsar E, Savage E. Deriving welfare measures from discrete choice experiments: inconsistency between current methods and random utility and welfare theory. Health Econ. 2004;13(9):901–7. https://doi.org/10.1002/hec.870.
Eggermont AMM, Blank CU, Mandala M, et al. Adjuvant pembrolizumab versus placebo in resected stage III melanoma. N Engl J Med. 2018;378(19):1789–801. https://doi.org/10.1056/NEJMoa1802357.
Johnson F, Yang J-C, Reed S. The internal validity of discrete choice experiment data: a testing tool for quantitative assessments. Value Health. 2018. https://doi.org/10.1016/j.jval.2018.07.876.
Weber J, Mandala M, Del Vecchio M, et al. Adjuvant nivolumab versus ipilimumab in resected stage III or IV melanoma. N Engl J Med. 2017;377(19):1824–35. https://doi.org/10.1056/NEJMoa1709030.
Luke J, Rutkowski P, Queirolo P, et al. Pembrolizumab versus placebo after complete resection of high-risk stage II melanoma: efficacy and safety results from the KEYNOTE-716 double-blind phase III trial. Ann Oncol. 2021;32(LBA3_PR)(5):S1283–346. https://doi.org/10.1016/annonc/annonc741.
Acknowledgements
The authors would like to thank the research participants and acknowledge the following consumer organisations for survey distribution: the Melanoma Institute Australia, Melanoma Patients Australia, Melanoma Research Victoria, the Melanoma and Skin Cancer Advocacy Network, Melanoma WA, Skin Cancer Tasmania, Melanoma and Skin Cancer Trials, and the Hunter Melanoma Foundation.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Funding for this work was provided by the Australian National Health and Medical Research Council (NHMRC 1168194), Cancer Institute New South Wales, Melanoma Institute Australia, Sydney Catalyst, Nicholas and Helen Moore, and the University of Sydney.
Conflicts of Interest
AL, RLM and KH have no financial disclosures. AMM served on BMS, MSD, Novartis, Roche, Pierre-Fabre and QBiotics advisory boards. GVL is a consultant advisor for Amgen, Array Biopharma, Boehringer Ingelheim, BMS, Hexel AG, Highlight Therapeutics SL, MSD, Novartis, Pierre-Fabre, Provectus, QBiotics, Regeneron Pharmaceuticals and Specialised Therapeutics Australia. MRS received institutional research support from Amgen, Astellas, AstraZeneca, Bayer, Bionomics, BMS, Celgene, Medivation, MSD, Pfizer, Roche, Sanofi and Tilray but did not sit on any advisory boards.
Ethics Approval
The Sydney Local Health District Human Research Ethics Committee (HREC/18/RPAH/736) granted ethics approval.
Consent
All participants provided written consent; the Declaration of Helsinki underpinned this study [1].
Availability of Data and Material
De-identified datasets used and analysed during the current study may be available from the corresponding author if the request falls within the project’s ethics approval.
Author Contributions
AL: conceptualisation, methodology, resources, writing – original draft preparation; KH: supervision, assistance with DCE methodology, writing, critical review/editing; AMM: supervision, assistance with participant recruitment, writing, critical review/editing, GVL: assistance with participant recruitment, critical review/editing; MRS: supervision, writing, critical review/editing, RLM: conceptualisation, supervision, assistance with DCE methodology, resources, writing, critical review/editing.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Livingstone, A., Howard, K., Menzies, A.M. et al. Preferences for Adjuvant Immunotherapy in Adults with Resected Stage III Melanoma—A Discrete Choice Experiment. Patient 16, 497–513 (2023). https://doi.org/10.1007/s40271-023-00635-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-023-00635-w