Abstract
Background
This study quantified how people with diabetes value the unique features of connected insulin pens and related mobile apps, and the underlying reasons for preferring connected versus non-connected insulin pens.
Methods
A discrete choice experiment (DCE) was conducted in the USA and UK to elicit preferences of adults (≥ 18 years) with type 1 or 2 diabetes for attributes of insulin pens. Attributes included device type, dosing support, glucose monitoring, additional app features, and data sharing. Relative attribute importance (RAI) scores were calculated to capture the relative importance of an attribute. Predicted choice probabilities were obtained to compare different profiles for connected and non-connected insulin pens.
Results
The DCE was completed by 540 participants (58.9% male; 90.7% Caucasian; mean age, 58.3 years; 69.4% type 2 diabetes). Participants most valued the possibility of using a connected insulin pen with dosing support and automated dose logging (RAI = 39.9%), followed by automatic transfer of glucose levels (RAI = 29.0%), additional features of tracking diet and physical activity (RAI = 14.6%), data sharing (RAI = 13.6%), and device type (RAI = 2.9%). All profiles of connected insulin pens were preferred over a non-connected pen (p < 0.001), and pen profiles with advanced features were preferred over those without (p < 0.001). Preferences differed by age but not diabetes type, country of residence, or insulin regimen.
Conclusion
People with diabetes in the USA and UK prefer connected over non-connected insulin pens due largely to the availability of automated logging of dose and glucose levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study of adults with diabetes in the USA and UK showed that most (75%) would prefer to inject insulin with an insulin pen connected to a mobile app, rather than with a non-connected insulin pen. |
Most people in the study preferred connected insulin pens over non-connected pens because they can automatically log insulin doses and record glucose levels. |
A minority (9%) remained skeptical of connected insulin pens but could be convinced if the pens offered features beyond insulin dose and glucose logging, while others (16%) would not use any connected insulin pen. |
1 Introduction
A fundamental aim of diabetes treatment is gaining glycemic control to avoid the risk of microvascular, macrovascular, and other complications [1]. Although insulin is effective for managing diabetes and therefore glycemic control [2, 3], insulin dosing is frequently suboptimal because people with diabetes miss or mistime doses or administer the wrong dose [4, 5]. Common reasons for this are forgetfulness, treatment complexity (e.g., dosing decisions and calculation of doses), fear of hypoglycemia, inadequate support, or follow-up by healthcare professionals, feeling overwhelmed by diabetes management, and interference of insulin dosing with daily activities [6,7,8].
Traditionally, people with diabetes have self-managed their disease by keeping a detailed logbook of therapeutic and lifestyle actions, but such records are often incomplete or inaccurate [9, 10]. Wearable glucose meters, mobile apps, and other digital solutions are increasingly used to aid diabetes management and these may improve clinical outcomes [11,12,13]. Hence, more advanced technological aids with added features, such as bolus advisors, are becoming available to optimise insulin delivery, improve adherence, and reduce dosing errors [14]. Offering dosing advice via digital technologies can reduce the cognitive burden and time spent managing insulin therapy [15]. In order to reduce disease burden, current development efforts have been focusing on connected insulin pens [16]. These devices capture insulin dose data and connect to proprietary or external mobile apps, allowing automatic data logging, data integration (e.g., hemoglobin A1c [HbA1c] levels, glucose levels, exercise, and lifestyle factors), and report generation.
Understanding the willingness of people with diabetes to switch from a non-connected to a connected insulin pen and the drivers of such decisions can help tailor the design of diabetes technologies to meet the needs of people using them [17, 18]. For example, a discrete choice experiment (DCE) can be used to elicit the effect that unique features of insulin pens have on the likelihood that people with diabetes would prefer a connected pen over a non-connected pen [19, 20]. Within a DCE this is achieved by repeatedly offering participants the choice between different hypothetical alternatives (e.g., insulin pens). These alternatives are described by a common set of attributes (e.g., pen features). The levels that these attributes take (e.g., availability of a mobile app feature) is systematically varied across choice tasks to ensure that their independent effects on preferences can be identified. Studies to date have focused only on non-connected insulin pens and have shown that people with diabetes value frequency and mode of administration [21,22,23,24]. The current study quantified the relative importance that people with diabetes placed on different features of connected insulin pens and related mobile apps, and predicted the average likelihood of people preferring a connected insulin pen over a non-connected pen.
2 Materials and Methods
2.1 Study Design
A DCE was conducted between March 24 and July 4, 2021, to elicit preferences of adults (aged ≥ 18 years) with diabetes for attributes of connected insulin pens [25, 26]. Following best practices for preference research [25, 27], the study was conducted in three phases: a targeted literature review to identify attributes to include in the DCE, qualitative interviews to inform and test the final design of the DCE, and a main DCE.
Discrete choice experiment participants were recruited via nationally representative online access panels, social media pages, magazines, and newsletters. To be eligible, interested individuals had to have self-reported type 1 (T1D) or type 2 (T2D) diabetes, used a physician-prescribed injectable insulin pen for the past 6 months, be a resident of the USA or UK, and be able to read and speak English. Participants with T1D had to be currently on a multiple daily insulin regimen (basal and bolus or bolus only) and those with T2D had to be currently on either a basal-only or multiple daily insulin regimen (basal and bolus, or bolus only). Individuals were excluded if they had ever used a connected insulin pen system; were currently using an insulin pump, a cartridge insulin pen, a reusable pen, or premix insulin; or were not using a smartphone at the time of screening. Eligibility was assessed using dedicated, pre-tested screening questions to minimize the possibility of including individuals who did not have diabetes or who were otherwise ineligible. Recruitment targeted participants in the USA and UK with quotas of 30% T1D and 70% T2D.
Eligible individuals completed an online survey (Online Resource 1) including a screening questionnaire, an informed consent form, the DCE, health literacy questions, and clinical and demographic questionnaires. Prior to the DCE, participants viewed a video, which introduced the connected insulin pen systems and described the DCE attributes. Health literacy was assessed using a Set of Brief Screening Questions, which consists of three items rated on a 5-point scale from 0 to 4 [28].
The study was approved by Ethical and Independent Review Services (study number 20182-01 for the initial review and 20182-01A for the modified survey following the qualitative interviews). Each participant consented to participate in the study and was remunerated for their time upon completion of either a 90-min qualitative interview or a 30-min online survey.
2.2 Targeted Literature Review
To inform an initial set of attributes for inclusion in the DCE, a literature search was conducted from June 23 to 29, 2020. Two separate search strategies were executed in Ovid to identify quantitative and qualitative studies on digital technologies for diabetes insulin therapy. Five candidate attributes of connected insulin pens (device type, dosing support, glucose monitoring, additional app features, and data sharing) were identified as being potentially relevant to patients with diabetes (see Online Resource 2 for details).
2.3 Qualitative Interviews
Based on the findings of the targeted literature review, an initial questionnaire including DCE choice tasks was developed and tested through telephone interviews (n = 6 with T1D [n = 3 USA, n = 3 UK]; n = 14 with T2D [n = 7 USA, n = 7 UK]) during which participants and interviewers viewed synchronized questionnaire content online. Objectives of the interviews were: (i) to understand patients’ perspectives on unique features of connected insulin pens; (ii) to assess if the candidate DCE attributes were relevant, tradeable, and understandable; and (iii) to test the adequacy of the attribute levels included in the DCE. To ensure that participant input could be adequately reflected, interviews were conducted in two rounds during which the interview guide, survey, and DCE were iteratively updated. Data (a transcribed dialogue) were analyzed with ATLAS.ti version 8 (ATLAS.ti Scientific Software Development GmbH, Berlin, Germany) using a mixture of inductive “bottom-up” and deductive “top-down” approaches. The outcomes of the qualitative analysis from the qualitative interviews were summarized visually in a conceptual map showing the themes and subthemes that participants discussed (Online Resources 3 and 4) and were used to refine the DCE choice task format, update wording of attributes, levels, and other aspects of the questionnaire, and further clarify attribute levels and device descriptions.
Interviews were conducted by two experienced qualitative researchers, lasted approximately 90 min, and consisted of warm-up background questions, a vignette study (Round 1 only), think-aloud interviews, and a closing discussion during which participants could provide open feedback. During the vignette study, participants were shown vignettes and were asked to answer scripted questions read by the interviewer. The first vignette introduced two types of connected insulin pens (Smart Button and SmartPen) that would be able to send dosing information to a mobile app. Smart Button was described as a Bluetooth-enabled cap that can be attached to a disposable insulin pen, and SmartPen was described as a Bluetooth transmitter that is integrated into a disposable insulin pen. The vignette explained that once all insulin in the pen is used or out-of-date, the Smart Button would be removed and attached to a new pen, whereas the Smart Pen would be disposed of. After being given the chance to read the first vignette, participants answered several questions and discussed the pros and cons of the described pens. The second vignette focused on the mobile app and explained that such an app could automatically receive and summarize blood sugar readings as a figure or graph. After being given the chance to review the second vignette, participants answered a series of questions about advantages and disadvantages of automated blood sugar recording and discussed potential features they would like to see in a mobile app. During the think-aloud interviews, participants completed the online survey, provided feedback, and were observed by interviewers.
2.4 Video Development
A video introduced the connected insulin pen systems and described the DCE attributes. The connected insulin pen in the video was an unbranded demonstration device, and screenshots from a test app were used as illustrative examples of app features and feature combinations. The video was developed following the first round of qualitative interviews (n = 7) and tested in the second round of interviews (n = 13). The video lasted 3 min and 17 s, and a USA and UK version was developed.
2.5 DCE Design
The final set of attributes and the corresponding levels are shown in Table 1. A D-efficient DCE design [29] was generated in Ngene version 1.2.1 (ChoiceMetrics Sydney, Australia). The design generated 36 choice tasks that were split into three blocks of equal size. Each survey participant was randomly assigned one block of 12 choice tasks. Each choice task asked participants to choose between a non-connected insulin pen (“opt out”) and two hypothetical connected insulin pens and their corresponding mobile apps. Each pen option was described by distinct levels of each attribute. The order of the “additional features” and “data sharing” attributes was randomized between participants to avoid ordering effects [30, 31]. An example choice task is shown in Fig. 1. The online survey did not allow for questions to be skipped, and only completed surveys were recorded.
2.6 Internal Validity Assessment
A first practice choice task was given prior to the 12 experimental choice tasks to familiarize participants with a DCE format of subsequent choice tasks, and two tasks for testing the internal validity of responses were added following the 12 experimental choice tasks [32]. The two validity tests followed by the DCE choice tasks were a repeated question of choice task 6 as task 14 to test choice stability and a dominance question in which one of the two connected insulin pens was clearly inferior for all attributes to test monotonicity of preferences and participants’ level of engagement with the choice tasks. Participants were considered to have failed the dominance test if they chose the inferior connected insulin pen. Participants were considered to have failed the repeated choice task if their responses to the repeated task differed. Further, participants were considered to avoid trade-offs if their choices in all 12 experimental tasks appeared to be driven by only a single attribute. Serial responders were defined as participants who chose the same connected pen option in all 12 experimental choice tasks. Following convention in the DCE literature, participants were not excluded on the basis of failing internal validity tests to avoid introducing selection bias [27].
2.7 Statistical Analysis
Only the 12 experimental choice tasks were used for the analysis of the DCE data. R version 4.0.2 was used for data management and analyses. All statistical tests were two-sided and used a significance level of 0.05. Comparison of statistical performance across models was based on Bayesian Information Criterion and the adjusted McFadden R2.
A random constant logit (RCL) model was developed and estimated within a random utility maximization framework [33,34,35,36]. This model extended classical multinomial logit models for choice data to account for heterogeneity in participants’ tendency to opt into a connected pen [37]. The model assumed that the T1D and T2D populations are made up of separate groups of people who attach a different value (i.e., utility) to using a non-connected pen compared to a connected pen. Smaller utility associated with a non-connected pen indicated greater desirability of a connected pen. This opt-out behavior was represented by a finite mixture of utility values associated with the non-connected pen, making the RCL a specific case of latent class analysis [38]. The final model specification was selected by estimating the RCL with varying assumptions about the number of groups in the population and choosing the model with the lowest Bayesian information criterion.
Relative attribute importance (RAI) scores were calculated to measure the maximum percentage contribution of an attribute to a preference relative to all other attributes and their levels. Because the automated dosing log was always offered as a default dosing support feature of connected insulin pens, which was to ensure the plausibility of profiles presented in the DCE, the RAI calculation for this feature had to be adjusted. To capture how participants valued an automated dosing log as part of the “dosing support” attribute, the negative average utility (i.e., the estimated constant) associated with a non-connected pen was added to the relative importance associated with dosing log visualization and dose recommendations.
Subgroup-specific RAI scores were obtained based on age (18–44/45–64/≥ 65 years), diabetes type (T1D/T2D), country of residence (USA/UK), and insulin regimen (bolus only/basal only/basal + bolus). Likelihood ratio tests were used to test if accounting for subgroups improved the ability of the RCL to explain choices made in the DCE.
Predicted choice probabilities (PCPs) were obtained to determine likely treatment preferences for “minimal”, “basic”, “extended”, and “advanced” profiles for both types of connected insulin pens to a non-connected insulin pen (Online Resource 5). Predicted choice probabilities were computed in a competitive setting that assumed participants could choose between different pen profiles.
Further details about the analysis and analysis outputs are provided in Online Resource 2.
3 Results
3.1 Participants
The survey was completed by 540 people with diabetes (n = 336 from USA and 204 from UK). The sample size aligns with other DCEs published in the literature, with most studies including between 100 and 600 participants [39]. Slightly more males (58.9%) than females with diabetes participated in the study, and 90.7% of participants were Caucasian (Table 2). The mean age was 58.3 years, and 74.6% had attained at least some level of college education. Most participants had T2D (69.4%), and approximately two-thirds (58.0%) reported that their most recent HbA1c level was > 7.0%. Basal-bolus insulin was used by 53.3% of participants, basal only by 34.3%, and bolus only by 9.3%. Nearly half of participants (47.6%) reported not recording their insulin dosing. Health literacy was considered adequate for 91.1% of participants. Participant characteristics were similar in the USA and UK.
3.2 Experience Using an App for Diabetes
Less than one-third of participants indicated they had experience with using an app for diabetes (28.1%), while 53.0% of participants indicated they had not used an app for diabetes but were willing to try one (Table 3). Among those who had used an app for diabetes, the most commonly reported uses were to track blood sugar (25.2%), share data with healthcare professionals (14.4%), and track the insulin dose (11.1%). Most participants stated that they would share app data with healthcare professionals (88.0%), but 9.6% stated they would not share app data because they were concerned about data privacy, and 4.3% stated that they would rather communicate verbally. Results were similar in each country.
3.3 Overall Preferences for Attributes of Insulin Pens
Comparable to other DCEs [32], 77.6% of participants passed the stability test and 87.4% passed the dominance test. A connected insulin pen was chosen over a non-connected pen in 80.3% of DCE tasks. The estimated model (Online Resource 6) was able to explain the choices that the participants made (adjusted McFadden R2 = 0.390) and identified three opt-in behaviors: technology supporters (74.9%; n = 405), who always chose a connected insulin pen; technology skeptics (8.8%; n = 47), who only chose very competitive connected insulin pens (i.e., pens that include many desirable features); and technology opponents (16.3%; n = 88), who never chose a connected insulin pen.
All attributes significantly affected participants’ valuations of and preferences for an insulin pen. Specifically, visual presentation of automatically logged dose information and dosing advice; app features that allowed people with diabetes to record blood sugar levels manually or automatically; app features that allowed tracking physical activities, food intake, or both; and a feature that allowed sharing data with family, caregivers, and healthcare professionals all increased the likelihood of a connected pen being preferred over alternatives. Although participants valued the ability to share data, they were indifferent about how it was shared. On average, participants preferred a Smart Button (attached to pen) over a SmartPen (integrated within pen).
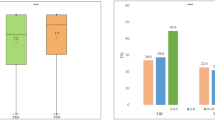
Of the different attributes, participants most valued the possibility of using a connected insulin pen with dosing support and automated dose logging (RAI = 39.9% [95% CI 26.6–53.3%]), followed by the automatic transfer of glucose levels (RAI = 29.0% [95% CI 22.4–35.7%]), additional features of tracking diet and physical activity (RAI = 14.6% [95% CI 10.9–18.3%]), data sharing (RAI = 13.6% [95% CI 10.3–17.0%]), and device type (RAI = 2.9% [95% CI 2.3–3.4%)] (Fig. 2). Based on this, automated dose logging combined with insulin dosing support and glucose monitoring (RAI = 69.0% [95% CI 61.7–76.2%) was 2.2 times more important to participants than all remaining attributes combined (RAI = 31.0% [95% CI 23.8–38.3%]). Similarly, glucose monitoring within the app of the connected insulin pen was approximately as important as the other two non-dosing–related support features together (RAI = 28.2% [95% CI 21.5–34.9%]).
3.4 Comparison of Pen Profiles
All profiles of connected insulin pens were preferred (p < 0.001) over a non-connected pen (Fig. 3). In all cases, connected insulin pens with more advanced app features (e.g., dosing visualization + dosing advice) were preferred over connected insulin pens with fewer or no app features (p < 0.001). A Smart Button with advanced features had the highest likelihood of being preferred (PCP = 23.5% [95% CI 22.5–24.5%]) and was preferred over a SmartPen with identical features (PCP = 21.3% [95% CI 20.4–22.2%]; p < 0.001), and for both pen types, advanced pen profiles were preferred over extended profiles.
3.5 Differences in Preferences between Participant Subgroups
A likelihood ratio test suggested that preferences differed by age (Fig. 4) but not by diabetes type, country of residence, or insulin regimens (Online Resource 7). For example, the availability of physical activity or dietary trackers (additional features) was valued more by participants aged 18–44 years (RAI = 22.7% [95% CI 17.0–28.3%]) than by those aged 45–64 years (RAI = 15.0% [95% CI 10.5–19.5%]; p < 0.05) or those aged ≥ 65 years (RAI = 10.6% [95% CI 6.1–15.1%]; p < 0.01). Conversely, glucose monitoring (all types) was valued less by participants aged 45–64 years (RAI = 26.0% [95% CI 21.4–30.7%]) than by those aged ≥ 65 years (RAI = 34.0% [95% CI 28.0–39.2%]; p < 0.01) but more than by those aged 18–44 years (RAI = 25.6% [95% CI 20.3–30.8%]; p < 0.01).
4 Discussion
To date, quantitative studies on preferences for insulin pens have focused on non-connected devices [21,22,23,24]. This study demonstrated that many people with diabetes prefer a connected insulin pen over a non-connected pen, irrespective of treatment profiles and configurations (e.g., device type). This is highlighted by the finding that approximately two-thirds of participants agreed or strongly agreed with statements that connected insulin pen systems offer improved diabetes management and simpler dose tracking over conventional paper logbooks, in agreement with other studies suggesting that connected insulin pens can increase confidence in diabetes self-management [40]. Despite this strong support for connected insulin pens, however, about one-sixth of participants were reluctant or even averse to switching to a connected insulin pen and preferred a non-connected pen. Observations of similar preference patterns have previously informed behavioral models of technology adaptation [41].
The main drivers for preferring a connected over a non-connected insulin pen were features related to automated insulin dose recording and other dosing support, such as dose history visualization, and the possibility of having glucose monitoring. Being able to track diet and physical activity and to share data were less valued but still considered important. Similarly, surveys of preferences for diabetes self-management mobile apps have shown that people with diabetes highly value being able to track blood glucose, exercise, and diet; receiving assistance with dose calculation; being able to consolidate data across peripheral health devices; and receiving reminders and other assistance to reduce the burden of diabetes self-management [42,43,44,45]. Although these preferences were similar between the two included countries (USA and UK), they differed by age: the importance of glucose monitoring increased with age, while the importance of additional features such as dietary and physical activity trackers decreased with age. Finally, the specific device type allowing connection to a mobile app was a minor driver of preferences, although, on average, a Smart Button was preferred over a SmartPen.
The results of this study suggest that people with diabetes highly value the support that connected insulin pen technologies offer by integrating data on dosing and data collected from glucose monitors [16]. In line with this, another study reported reduced HbA1c levels in people with diabetes using an insulin SmartPen connected via Bluetooth® to a mobile app [46]. Other studies have shown fewer missed doses and improved glucose control in people with diabetes using connected insulin pens [47, 48].
This study benefitted from a best-practice mixed methods design [49,50,51], wherein a targeted literature search was used to select attributes and levels for the DCE, after which the DCE was tested and refined in two rounds of qualitative interviews and then finally used in a main study [49]. In addition, efforts were made to ensure the DCE was clear and accessible. For example, a short video was included to illustrate connected insulin pens and help participants distinguish between attribute levels [52, 53]. This study also benefitted from an analysis method that accounted for differences in opt-in behaviors among the participants, which is important for placing decisions in a real-life context [37]. A limitation, however, was that because this was an online study, participants did not have the opportunity to physically experience and use the connected insulin pens, which may have influenced their preferences. Another limitation of this study was that the participants were identified through a convenience sample drawn from an opt-in panel of adults in the USA and UK who volunteered to participate in healthcare research and who self-reported T1D or T2D with a set quota of basal-bolus and basal only use. The study sample was predominantly (<90%) Caucasian and most participants were well-educated, with approximately 75% having attained at least some college education. A further limitation is that the study excluded patients who had current or prior experience with connected insulin pens. While excluding experienced patients was important to maintain this study’s focus on assessing attributes that would be valued in patients naïve to connected insulin pens, these patient populations may differ. Although screening questions should have excluded individuals who did not have diabetes, and although efforts were made to include participants with both diabetes types, different dosing types, and a sufficient number of non-Caucasian participants, the generalizability of the results to the wider population of people with diabetes remains uncertain.
5 Conclusions
This quantitative study showed that most people with diabetes in the USA and UK preferred connected over non-connected insulin pens. This was due largely to the availability of automated logging of dose from the pen and also app features such as automatic logging of glucose levels, although people with diabetes also valued being able to track diet and physical activity and to share data. Notably, even though the majority of participants were not currently using mobile apps for tracking their diabetes, they would be willing to try.
References
American Diabetes Association. 6. Glycemic targets: standards of Medical Care in Diabetes—2020. Diabetes Care. 2020;43:S66–76.
Guerci B, Chanan N, Kaur S, Jasso-Mosqueda JG, Lew E. Lack of treatment persistence and treatment nonadherence as barriers to glycaemic control in patients with type 2 diabetes. Diabetes Ther. 2019;10(2):437–49.
Doggrell SA, Chan V. Adherence to insulin treatment in diabetes: can it be improved? J Diabetes. 2015;7(3):315–21.
Davies MJ, Gagliardino JJ, Gray LJ, Khunti K, Mohan V, Hughes R. Real-world factors affecting adherence to insulin therapy in patients with type 1 or type 2 diabetes mellitus: a systematic review. Diabet Med. 2013;30(5):512–24.
Munshi MN, Slyne C, Greenberg JM, Greaves T, Lee A, Carl S, et al. Nonadherence to insulin therapy detected by bluetooth-enabled pen cap is associated with poor glycemic control. Diabetes Care. 2019;42(6):1129–31.
Brod M, Pohlman B, Kongso JH. Insulin administration and the impacts of forgetting a dose. Patient. 2014;7(1):63–71.
Smythe K, Saw M, Mak M, Wong VW. Carbohydrate knowledge, lifestyle and insulin: an observational study of their association with glycaemic control in adults with type 1 diabetes. J Hum Nutr Diet. 2018;31(5):597–602.
Yavuz DG, Ozcan S, Deyneli O. Adherence to insulin treatment in insulin-naive type 2 diabetic patients initiated on different insulin regimens. Patient Prefer Adherence. 2015;9:1225–31.
Given JE, O’Kane MJ, Bunting BP, Coates VE. Comparing patient-generated blood glucose diary records with meter memory in diabetes: a systematic review. Diabet Med. 2013;30(8):901–13.
Kazlauskaite R, Soni S, Evans AT, Graham K, Fisher B. Accuracy of self-monitored blood glucose in type 2 diabetes. Diabetes Technol Ther. 2009;11(6):385–92.
Chomutare T, Fernandez-Luque L, Arsand E, Hartvigsen G. Features of mobile diabetes applications: review of the literature and analysis of current applications compared against evidence-based guidelines. J Med Internet Res. 2011;13(3): e65.
Drincic A, Prahalad P, Greenwood D, Klonoff DC. Evidence-based mobile medical applications in diabetes. Endocrinol Metab Clin North Am. 2016;45(4):943–65.
Iyengar V, Wolf A, Brown A, Close K. Challenges in diabetes care: can digital health help address them? Clin Diabetes. 2016;34(3):133–41.
Shan R, Sarkar S, Martin SS. Digital health technology and mobile devices for the management of diabetes mellitus: state of the art. Diabetologia. 2019;62(6):877–87.
Fleming GA, Petrie JR, Bergenstal RM, Holl RW, Peters AL, Heinemann L. Diabetes digital app technology: benefits, challenges, and recommendations. A consensus report by the European Association for the Study of Diabetes (EASD) and the American Diabetes Association (ADA) diabetes technology working group. Diabetes Care. 2020;43(1):250–60.
Sy SL, Munshi MM, Toschi E. Can smart pens help improve diabetes management? J Diabetes Sci Technol. 2020;21:1932296820965600.
National Institute for Health and Care Excellence (NICE). Type 1 diabetes in adults: diagnosis and management. NICE guideline 17. 2015. Updated July 21, 2021. https://www.nice.org.uk/guidance/ng17. Accessed 25 Feb 2022.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2018;61(12):2461–98.
Carson R, Louviere J. A common nomenclature for stated preference elicitation approaches environmental and resource. Economics. 2011;49:539–59.
Soekhai V, de Bekker-Grob EW, Ellis AR, Vass CM. Discrete choice experiments in health economics: past, present and future. Pharmacoeconomics. 2019;37(2):201–26.
Gelhorn HL, Bacci ED, Poon JL, Boye KS, Suzuki S, Babineaux SM. Evaluating preferences for profiles of glucagon-like peptide-1 receptor agonists among injection-naive type 2 diabetes patients in Japan. Patient Prefer Adherence. 2016;10:1337–48.
Gelhorn HL, Poon JL, Davies EW, Paczkowski R, Curtis SE, Boye KS. Evaluating preferences for profiles of GLP-1 receptor agonists among injection-naive type 2 diabetes patients in the UK. Patient Prefer Adherence. 2015;9:1611–22.
Gelhorn HL, Stringer SM, Brooks A, Thompson C, Monz BU, Boye KS, et al. Preferences for medication attributes among patients with type 2 diabetes mellitus in the UK. Diabetes Obes Metab. 2013;15(9):802–9.
Poon JL, Bove KS, Theiu VT, Norrbacka K, Hassan SW, Gelhorn HL. Preferences for attributes of medications among patients with type 2 diabetes: a cross-medication class comparison of injection therapies. Curr Res Diabetes Obes J. 2018;6(5):1–13.
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13.
Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320(7248):1530–3.
Lancsar E, Louviere J. Deleting “irrational” responses from discrete choice experiments: a case of investigating or imposing preferences? Health Econ. 2006;15(8):797–811.
Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588–94.
Reed Johnson F, Lancsar E, Marshall D, Kilambi V, Muhlbacher A, Regier DA, et al. Constructing experimental designs for discrete-choice experiments: report of the ISPOR Conjoint Analysis Experimental Design Good Research Practices Task Force. Value Health. 2013;16(1):3–13.
Carlsson F, Mørkbak M, Olsen S. The first time is the hardest: a test of ordering effects in choice experiments. J Choice Model. 2012;5(2):19–37.
Heidenreich S, Phillips-Beyer A, Flamion B, Ross M, Seo J, Marsh K. Benefit-risk or risk-benefit trade-offs? Another look at attribute ordering effects in a pilot choice experiment. Patient. 2021;14(1):65–74.
Johnson FR, Yang JC, Reed SD. The internal validity of discrete choice experiment data: a testing tool for quantitative assessments. Value Health. 2019;22(2):157–60.
Thurstone LL. A law of comparative judgment. Psychol Rev. 1927;34(4):273–86.
Marschak J. Binary choice constraints on random utility indicators. New Haven: Cowles Foundation for Research in Economics, Yale University; 1959.
McFadden D. Conditional logit analysis of qualitative choice behaviour. New York: Academic Press; 1973.
Manski CF. The structure of random utility models. Theor Decis. 1977;8:229–54.
Campbell D, Erdem S. Including opt-out options in discrete choice experiments: issues to consider. Patient. 2019;12(1):1–14.
Greene WH, Hensher DA. A latent class model for discrete choice analysis: contrasts with mixed logit. Transport Res Part B Methodol. 2003;37(8):681–98.
de Bekker-Grob EW, Donkers B, Jonker MF, Stolk EA. Sample size requirements for discrete-choice experiments in healthcare: a practical guide. Patient. 2015;8(5):373–84.
Heinemann L, Schnell O, Gehr B, Schloot NC, Gorgens SW, Gorgen C. Digital diabetes management: a literature review of smart insulin pens. J Diabetes Sci Technol. 2021;11:1932296820983863.
Beal GM, Bohlen JM. The diffusion process. Increasing understanding of public problems and policies. 1956; 111–21.
Adu MD, Malabu UH, Malau-Aduli AEO, Malau-Aduli BS. Users’ preferences and design recommendations to promote engagements with mobile apps for diabetes self-management: multi-national perspectives. PLoS ONE. 2018;13(12): e0208942.
Baptista S, Trawley S, Pouwer F, Oldenburg B, Wadley G, Speight J. What do adults with type 2 diabetes want from the “perfect” app? Results from the second diabetes MILES: Australia (MILES-2) study. Diabetes Technol Ther. 2019;21(7):393–9.
Knight BA, McIntyre HD, Hickman IJ, Noud M. Qualitative assessment of user experiences of a novel smart phone application designed to support flexible intensive insulin therapy in type 1 diabetes. BMC Med Inform Decis Mak. 2016;15(16):119.
Rafiullah M, David SK. Health apps usage and preferences among Saudi patients with diabetes: a survey. Int J Clin Pract. 2019;73(5): e13345.
Emperra. Scientific evaluation of the ESYSTA® S-T-A-R-T project. 2016. https://www.emperra.com/wp-content/uploads/2020/06/esysta_start_whitepaper_en_2.0.pdf. Accessed 25 Feb 2022.
Adolfsson P, Hartvig NV, Kaas A, Moller JB, Hellman J. Increased time in range and fewer missed bolus injections after introduction of a smart connected insulin pen. Diabetes Technol Ther. 2020;22(10):709–18.
Gomez-Peralta F, Abreu C, Gomez-Rodriguez S, Cruz-Bravo M, Maria-Sanchez C, Poza G, et al. Efficacy of insulclock in patients with poorly controlled type 1 diabetes mellitus: a pilot, randomized clinical trial. Diabetes Technol Ther. 2020;22(9):686–90.
Coast J, Al-Janabi H, Sutton EJ, Horrocks SA, Vosper AJ, Swancutt DR, et al. Using qualitative methods for attribute development for discrete choice experiments: issues and recommendations. Health Econ. 2012;21(6):730–41.
Kløjgaard ME, Bech M, Søgaard R. Designing a stated choice experiment: the value of a qualitative process. J Choice Model. 2012;5(2):1–18.
Ryan M, Watson V, Entwistle V. Rationalising the ‘irrational’: a think aloud study of discrete choice experiment responses. Health Econ. 2009;18(3):321–36.
Vass CM, Davison NJ, Vander Stichele G, Payne K. A picture is worth a thousand words: the role of survey training materials in stated-preference studies. Patient. 2020;13(2):163–73.
Lim SL, Yang JC, Ehrisman J, Havrilesky LJ, Reed SD. Are videos or text better for describing attributes in stated-preference surveys? Patient. 2020;13(4):401–8.
Acknowledgements
Medical writing was provided by Phillip S. Leventhal (Evidera). This study and medical writing were funded by Eli Lilly & Co.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
SH, JS, EA are employees of Evidera by PPD, which was paid by Eli Lilly & Co. for work related to this study. ES is a contractor funded by Eli Lilly & Co. J-L P, EE, RN are employees and shareholders in Eli Lilly & Co.
Funding
This study and medical writing were funded by Eli Lilly & Co.
Author contributions
SH: conceptualization, methodology, writing, supervision; JS: conceptualization, methodology, writing, project administration; EA: formal analysis, writing—review and editing; JLP: conceptualization, methodology, writing—review and editing; ES: conceptualization, methodology, writing—review and editing; EE: conceptualization, methodology, writing—review and editing; RSN: conceptualization, methodology, supervision, project administration, writing—review and editing.
Ethics approval
The study was approved by Ethical and Independent Review Services (nos. 20182-01 and 20182-01A). Upon completion of the study, each participant was remunerated for their time with a cash equivalent in panel currency/voucher.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available as no consent was sought from participants to allow sharing of data with third parties.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Seo, J., Heidenreich, S., Aldalooj, E. et al. Patients’ Preferences for Connected Insulin Pens: A Discrete Choice Experiment Among Patients with Type 1 and Type 2 Diabetes. Patient 16, 127–138 (2023). https://doi.org/10.1007/s40271-022-00610-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-022-00610-x