Abstract
Background
While coronavirus disease 2019 (COVID-19) vaccines have high rates of efficacy, fully vaccinated individuals can become infected with COVID-19. Among this population, symptoms tend to be less severe and shorter lasting. Less is known about how vaccinated individuals who contract COVID-19 experience the disease through patient-reported outcomes (PROs) and how this changes over time.
Objective
The aim of this study was to describe the physical, mental, and social health PROs for fully vaccinated individuals who contracted COVID-19 over a 6-week period.
Design
Prospective design using the Patient-Reported Outcomes Measurement Information System short-form (PROMIS-10) collected through a mobile application-based platform.
Participant
1114 fully vaccinated patients who tested positive for COVID-19 at a large US health system and engaged with the study on or after 1 March 2021 and reported onset of illness prior to 1 November 2021.
Main Measures
Global physical and mental health PROMIS-10 T-scores for the 6-week period, component PROMIS-10 questions for the 6-week period, and component PROMIS-10 questions restricted to a subset of participants for the first month to measure individual recovery were analyzed.
Key Results
Mean global physical and mental health T-scores increased over time and remained within one standard deviation of the population mean. At baseline, at least 40% of participants reported good health for all component questions except Fatigue (25%), and the proportion reporting good health increased over time for all questions, with the largest improvements in Fatigue (25.5 to 67.5%), Pain (59.1 to 82.8%), and Emotional Problems (42.3 to 62.5%). Over the first month, the greatest positive changes in individual recovery were observed for Fatigue (65.0%), Pain (53.0%), and Emotional Problems (41.1%); at least 30% of respondents reported no change in at least one category, and the greatest decreases were for Usual Social Activities (23.9%), Social Satisfaction (23.2%), and Mental Health (21.8%).
Conclusions
This study provides an important step towards better understanding the impact of ‘breakthrough’ COVID-19 infections on clinically engaged, fully vaccinated patients’ physical and mental health to improve support for their treatment and recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Global physical and mental health scores for fully vaccinated patients infected with coronavirus disease 2019 (COVID-19) increased over a 6-week period but remained within one standard deviation of the population mean during this time. |
At least 40% of patients with ‘breakthrough’ COVID-19 infections reported good health at baseline for their physical and mental health in all domains except Fatigue, which was much lower, and all domains improved over time, although recovery was reported to different degrees in different domains. |
Patients’ individual recovery trajectories over the first month varied by domain; patients experienced the greatest improvements in Fatigue, Pain, and Emotional Problems, and the largest declines in Usual Social Activities, Social Satisfaction, and Mental Health; patients who experienced no change over this time generally had PROs that skewed towards more stable good health. |
1 Introduction
As of February 2022, over 70 million people in the United States (US) have been infected with coronavirus disease 2019 (COVID-19) and over 400 million people have been infected worldwide [1, 2]. COVID-19 vaccine development and distribution has been a central strategy to combat the spread and deadly consequences of infection. Extensive data on COVID-19 vaccines, including mRNA-based (Elasomeran: Moderna, and Tozinameran: Pfizer-BioNTech) and viral vector platforms (JNJ-78436735: Janssen Pharmaceuticals Companies of Johnson & Johnson), have demonstrated safety and significant effectiveness in preventing symptomatic infection, severe disease, and hospitalization in clinical trials [3,4,5].
Over 212 million people in the US have been fully vaccinated [6], defined here as receiving two doses of the mRNA vaccines or one dose of the viral vector vaccine. Since vaccine roll-out, research in the real-world setting has evaluated vaccine effectiveness and demonstrated similar results to clinical trials [7,8,9]. For example, a Kaiser Permanente Health System study that examined vaccine effectiveness over 6 months showed a vaccine efficacy against COVID-19 infection of 73% and a reduction of COVID-19-related hospitalizations of 90% after adjusting for previous health care utilization, prior vaccination behavior, demographics, comorbidities, and neighborhood-level socioeconomic status [10]. Multiple other studies have shown similar effects across different populations and demographics [11, 12].
While vaccine effectiveness is clear, so-called ‘breakthrough’ COVID-19 infections do occur in vaccinated populations. Research has found differences in COVID-19 symptoms and symptom duration for vaccinated and non-vaccinated individuals. A study of healthcare workers showed that COVID-19 cases among vaccinated participants were associated with lower mean viral load, reduced risk of febrile symptoms, and shorter (approximately 2.3 days) illness [13]. Additionally, in the UK, one study found that vaccination was associated with reduced odds of almost all 23 symptoms measured, as well as reduced odds of a symptom lasting longer than 28 days [14]. While vaccinated patients tend to have less severe and shorter-lasting symptoms compared with unvaccinated individuals, relatively little is known about the patient-reported outcomes (PROs) for vaccinated individuals who do contract COVID-19.
PROs are important to delivering high-quality clinical care as they measure perceived functional well-being as well as physical and emotional health status directly from the patient [15, 16]. A handful of studies have examined PROs for COVID-19 and shown impacts on outcomes such as pain, fatigue, ability to participate in social activities, quality of life, and mood [17, 18]. This research shows how COVID-19 can impact PROs, but less is known about PROs for vaccinated COVID-19 patients with symptomatic infection. Furthermore, existing research on PROs for individuals with COVID-19 have generally been limited to those requiring hospitalization, been retrospective, and have often been limited to only one timepoint [17, 19,20,21,22,23]. More research is needed to understand PROs and COVID-19 experiences, especially how they change over time for vaccinated patients who contract COVID-19.
In this study, we leverage the ongoing My COVID Diary (MCD) study based out of Providence St. Joseph Health (Providence), a large integrated US health system that spans seven states. MCD uses a mobile application (app)-based platform to provide participants with structured questionnaires and the opportunity to share open-ended text responses to prospectively monitor the patient experience for individuals infected with COVID-19. The goal of this study was to understand and describe the physical, mental, and social health and well-being for fully vaccinated individuals who contracted COVID-19 over a 6-week period. This study contributes to our understanding of COVID-19 infection by increasing knowledge of the experience of breakthrough infections and providing insight for clinicians and health systems to better manage care for COVID-19 patients.
2 Methods
2.1 Study Population
MCD is offered across Providence’s seven-state footprint (Alaska, Oregon, Washington, California, Montana, New Mexico, and Texas). Since August 2020, any patient aged ≥ 18 years testing positive for COVID-19 at a Providence location receives a text inviting them to participate; up to three attempts are made before exiting them from the protocol. If participants consent, they use a mobile e-consent platform (Twistle) to sign up, and are asked to participate for up to 1 year. Enrollment is ongoing, but an average of 12% of those who were sent a message have enrolled. Patients who test positive for COVID-19 outside the Providence system are not eligible to participate in MCD. The full study protocol was approved by Providence St. Joseph Health Institutional Review Board (IRB# 2020000467).
Our study population focuses on fully vaccinated participants who were infected with COVID-19 (Fig. 1). As of March 2021, new MCD participants were asked about their vaccination status, including vaccination dates and number of doses; thus, we consider March 2021 as the study onset. To obtain this population, we first identified MCD participants who reported receiving two doses of vaccine (vaccine type was not tracked in the platform, therefore participants who received the single dose Johnson & Johnson vaccine were ultimately excluded from the study). At the time of this study, vaccine booster doses were not yet widely approved; therefore, booster status was not considered in identifying the study population. Next, we excluded any individuals whose COVID-19 infection occurred within 2 weeks of their last-needed vaccine dose. Finally, participants had to have at least one response to the PROMIS-10 survey (Patient-Reported Outcomes Measurement Information System), the structured PRO questionnaire administered through the platform. The final sample size was 1114 participants who first engaged with MCD on or after 1 March 2021 and reported onset of illness prior to 1 November 2021. The majority of infection dates occurred in August–October (data not shown).
2.2 Data Collection
All data were collected electronically via the mobile app-based platform. At enrollment, details on demographics and infection onset were collected. During their first 6 weeks, participants received weekly prompts to respond to structured surveys. This included the PROMIS-10 (a validated 10-item survey designed to assess PROs for physical, mental, and social health and well-being) [16] and questions about whether they have been to the hospital or emergency department (ED) for COVID-19 in the past 2 days. The platform collected additional information not used in this study.
2.3 Data and Analysis
Data were exported from the platform for cleaning and analysis. Demographic variables were categorized for descriptive analysis. MCD engagement was analyzed by tabulation of unique patients responding within each weekly interval. All survey responses were grouped by individual patient by week, indicating time from infection onset, beginning with ‘Sick Week 1’ representing the first 7 days following infection (i.e., response week was counted from the reported date a patient’s symptoms started, not their enrollment date). All statistical analysis of patient demographics and PROMIS-10 data was performed using R Statistical Software version 4.0.2 and R Studio version 1.3.1093 (The R Foundation for Statistical Computing, Vienna, Austria).
PROMIS-10 survey responses were used to compute a Global Physical Health T-score and a Global Mental Health T-score for each 1-week period. T-score metrics are commonly used for PROMIS-10; a score of 50 represents the general population mean and a 10-point difference represents one standard deviation from that mean, with higher scores representing better functional health and a difference of at least half a standard deviation (5 points) considered clinically meaningful [24, 25]. Global Physical and Mental Health PROMIS-10 scores were summarized statistically and differences in means across demographic categories were evaluated to determine if certain groups were at more risk for adverse outcomes than others. To explore overall trends of Global T-scores over time, we constructed density plots of T-scores for the study population at weeks 2, 4, and 6, which were compared with the reference T-score distributions.
Results from individual PROMIS-10 component questions were also analyzed at each week. Component questions assess the following aspects of both physical and mental health: Physical Health, Mental Health, General Health, Emotional Problems, Everyday Physical Activities, Usual Social Activities, Fatigue, Quality of Life, Pain, and Social Satisfaction. PROMIS-10 questions were reported on a scale of 1–5 except for Pain, which was rated on a scale of 0–10 but recoded to the 1–5 scale for analysis. Low scores (< 3) are considered to be associated with poor health, and high scores (> 3) are considered to be associated with good health [25,26,27]. The proportion of patients reporting favorable health (score > 3) was computed for each question, and trends over time were explored using time-series analysis. Error bands for trends were computed using the standard error for a proportion based on the number of patients responding within each week.
To investigate the recovery experience reported by individual patients during approximately the first month of infection, change in PROMIS-10 scores was computed and analyzed over time. For this analysis, the study population was restricted to participants who reported a first score within 2 weeks following infection and at least one score during the fourth or fifth week following infection (n = 591). Each patient’s first reported score for each question was used as a baseline score (representing their PROs at the beginning of their COVID-19 infection), and the difference between baseline and their week 4 or 5 score was calculated for each question. The distribution of change in score was then summarized for each question as proportions of the study population.
3 Results
3.1 Participants
Participant characteristics are shown in Table 1. The study population was predominantly female (66.0%) and White (78.9%) and was evenly distributed between over and under 50 years of age. Approximately 30% of the study participants reported either hospitalization or an ED visit due to COVID-19 during the study window. The average time from last dose of vaccine to infection was 22.1 weeks.
Overall response rates declined from a maximum 934 at Week 2 to 424 at Week 6 (Table 2), representing 84% of the study population at our peak response rate and 38% of the study population at 6 weeks (accounting for participants who joined the study later and whose sixth week occurred outside the study window). In general, more people responded each week who reported female sex, were aged ≥ 50 years, and did not have a visit to the ED or hospital; however, this pattern aligns with the demographic characteristics of the study population overall.
3.2 Patient-Reported Outcomes Measurement Information System (PROMIS-10) T-Scores
Comparison of reported baseline Global Physical and Mental Health at Week 2 found only small differences in scores between demographic subgroups. Average scores were slightly lower for female participants for both Physical and Mental Health, and for Mental Health for participants under 50 years of age, however all differences in means between the sex and age groups were < 0.5 standard deviations (SDs) of the references’ T-score distributions and were not considered clinically significant. Participants who reported having been hospitalized or having visited the ED for COVID-19 reported significantly lower scores for Physical Health at Week 2 compared with those who did not (42.9 vs. 47.9, 95% confidence interval [CI] 3.5–6.1). For complete results, please see the Appendix (Table 3).
Density plots of Global Physical and Mental Health T-scores are shown for Weeks 2, 4, and 6 (Fig. 2). Each density plot is annotated with the mean score for the given time period (vertical dashed line) and the standard T-score distribution for the general population is overlayed on each graph (dashed curve). Mean Global Health T-scores generally increased over time for both physical and mental health but remained within one SD of the population mean throughout. Over the full 6-week period, the distribution of Global Physical Health T-scores shifted rightward with the mean approaching and then exceeding the mean of the symmetric standard T-score distribution, and with the right tail shortening and the left tail lengthening over time (Fig. 2, left). A similar effect is seen in the density plots of Global Mental Health T-scores with a notable bump in the right tail in the latter timepoints (note the sample size is smaller at this time period) [Fig. 2, right].
Distributions of (a) Global Physical and (b) Mental Health PROMIS-10 scores reported by MCD participants in Weeks 2, 4, and 6 (solid curves). Vertical dashed lines indicate the mean reported score for the given week, and dashed curves represent the standard T-score distribution (mean of 50 and standard deviation of 10) for PROMIS measures on a reference population. PROMIS Patient-Reported Outcomes Measurement Information System, MCD My COVID Diary
3.3 PROMIS-10 Component Scores
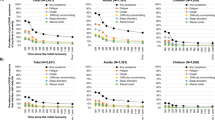
Figure 3 shows trend lines of the percentage of participants responding each week who reported a PROMIS-10 score of 4 or 5 (good health) for each component question. Shaded bands around the trendlines represent the standard error of a proportion based on the response rate each week. At least 40% of participants responding in Week 1 reported baseline scores of 4 or 5 for all questions except for Fatigue (25.5%). Everyday Physical Activities started with the highest percentage with favorable responses (70.9%). Regardless of baseline scores, proportions increased over time for all questions; however, the increase was more dramatic for Fatigue (25.5 to 67.5%), Pain (59.1 to 82.8%), and Emotional Problems (42.3 to 62.5%) over the first 4 weeks, before stabilizing.
Figure 4 shows the change in PROMIS-10 scores over time for a subset of participants (n = 591) who reported a score within 2 weeks following infection and reported at least one score during the fourth or fifth week following infection. For each question, the shades in the associated horizontal bar show the relative proportion of participants reporting the respective change in score. The three questions with the greatest positive change were Fatigue (65.0% > 0), Pain (53.0% > 0), and Emotional Problems (41.1% > 0), while the three questions with the greatest negative change were Usual Social Activities (23.9% < 0), Social Satisfaction (23.2% < 0), and Mental Health (21.8% < 0).
For most components, at least 30% of respondents reported no change over the 1-month period (ranging from 30.5% for Fatigue to 52.6% for Everyday Physical Activities). We examined the distribution of their scores to understand if those reporting no change were maintaining generally good or bad health over the first month. Results show that the distributions of responses for all PROMIS-10 categories, except Fatigue, skewed more towards favorable responses (Fig. 5).
4 Discussion
To better understand the self-reported experience of clinical breakthrough COVID-19 infections, the present study used a prospective design to describe PROs for fully vaccinated COVID-19 patients for 6 weeks following infection. To our knowledge, few existing studies use a prospective design and longitudinal data to examine PROs of individuals infected with COVID-19 [18, 19, 28], and even fewer include fully vaccinated individuals’ experiences [29]. We observed a general increase in mean PROMIS-10 Global Health T-scores over time for both Physical and Mental Health. When examining PROMIS-10 component questions, at least 40% of patients responding in Week 1 reported good health for all questions except Fatigue, for which only 25% reported good health. Regardless of baseline scores, proportions of patients reporting good health increased over time for all component questions. While the observed increase was moderate for most questions, it was dramatic for Fatigue, Pain, and Emotional Problems. For a subset of participants, we also examined how their responses changed over the first month following infection. All categories showed improvements, with the greatest percentage of patients reporting improvement in Fatigue, Pain, and Emotional Problems. The greatest percentages reporting declines were in Usual Social Activities, Social Satisfaction, and Mental Health. When no change was observed, scores skewed towards more favorable responses.
Existing research on unvaccinated COVID-19 patients in outpatient settings follow similar trends, where patients reported improved perceptions of their health and their ability to return to usual activities over 4 weeks, although nearly one-third of patients still had not yet returned to their usual health at this time [28, 30]. Research on vaccinated patients has found even shorter recovery times on average, with 86% of patients reporting a return to usual activities and 76% reporting a return to usual health within 14 days [29]. In comparison with research on hospitalization rates for COVID-19 and on impacts of vaccination on COVID-19 hospitalization, the vaccinated population engaged in this study had a higher-than-expected proportion of ED or hospital visits related to their COVID-19 infection (31%) [4, 31]. This suggests that MCD participation might be correlated with greater likelihood of experiencing COVID-19 symptoms. This is not surprising as all patients invited to participate in MCD were tested in either an acute or outpatient hospital setting. Thus, the PROs presented in this study likely describe a more symptomatic or clinically engaged ‘breakthrough’ COVID-19 infection, which is important knowledge for clinicians caring for vaccinated patients who do have symptomatic disease.
Our data show that the average Physical and Mental Health T-scores remained within one SD of the general population mean, suggesting potentially mild impairment on average that improved over time. However, the density plots clearly show that a small portion of T-scores fell below one SD, indicating that some vaccinated individuals report greater physical and mental health deficits during COVID-19 infection and these deficits can last several weeks after infection. Participants’ general physical and mental health prior to COVID-19 infection is unknown, which would also impact this distribution and interpretation. In general, a PROMIS-10 Global T-score between one and two SDs below the mean indicates moderate symptoms/impairment, and more than two SDs means more severe symptoms/impairment [16, 32]. While cut-offs for clinically meaningful changes in PROMIS scores have not yet been calibrated specifically for COVID-19, generally a shift of 5 points (or 0.5 SDs) is considered clinically meaningful [24, 25, 33]. Some papers have used the threshold of a two- to six-point difference in scores to represent a clinically meaningful change [34]. A handful of studies have measured PROMIS scores in COVID-19 populations, but these early studies are varied based on the population studied, the duration, and the specific focus area [23, 33, 35, 36]. One study that examined changes in PROMIS-10 collected during ambulatory care visits before and after COVID-19 infection found one-quarter of patients had worsening PROMIS-10 Global T-scores over time in the months after their COVID-19 diagnoses [33]. Another study that focused on hospitalized COVID-19 patients six months after discharge reported physical and mental health T-scores of 45.2 and 47.4, respectively [36]. COVID-19 patients who required oxygen reported global physical and mental health T-scores of 43.8 and 47.3, respectively, 1 month after discharge [23]. These studies show the impact that COVID-19 infection can have on patients’ lives even after acute infection, as measured by patient-reported physical and mental health global PROMIS-10 scores; our study expands on this by describing these scores for clinical cases of vaccinated patients infected with COVID-19 and shows how physical and mental health can be impacted.
When examining specific component questions, Fatigue had the greatest initial deficit, with only 25.5% of patients reporting good scores (> 3). However, positive responses to the Fatigue question showed the most rapid increase and negative responses had the smallest proportion of decrease among individual respondents over the first 4–5 weeks of infection. Interestingly, studies on long-term COVID-19 that examine symptoms at different timepoints show that fatigue is one of the most persistent symptoms [17, 21, 22]. While the data reported in this study show rapid improvement in fatigue over the first 4 weeks, after that time the increase tapers off. These results suggest that vaccination might limit long-term symptoms of fatigue but, for a small portion, fatigue may be a protracted symptom of COVID-19 infection. More research is needed to understand the potential long-term impacts, particularly research driven by patients experiencing protracted symptoms that centers their experiences and priorities [37].
Although our overall results show more participants reporting improving global Mental Health scores over time, questions for which the greatest proportion of patients reported a decline over the first 5 weeks were Usual Social Activities, Social Satisfaction, and Mental Health. It is important to note that an even larger proportion of this population saw improvements in these outcomes over that period. However, these data surface the mental and social impacts of COVID-19 infection that may affect some vaccinated individuals. Other research has captured the high mental health burden associated with COVID-19 infection, such as depression, anxiety, stress, panic attacks, and irrational anger, among others [38]. These mental health challenges are impacted by various factors; one of which is the perceived likelihood of survival due to infection severity [38]. While vaccination substantially increases the likelihood of survival, this study furthers our understanding of the mental health impacts of COVID-19 by focusing on the vaccinated population and recognizing that vaccinated patients can also experience mental health challenges.
MCD is still enrolling COVID-19 patients and collecting longitudinal PROs and narrative journal entries for up to 1 year. We plan to leverage these data to continue to explore the COVID-19 experience in the short- and long-term to understand the physical, mental/emotional, and social impacts of infection and recovery in patients’ own words. Additional research using PROs for COVID-19 patients is needed to support a better understanding of treatment and address any downstream consequences of infection, as well as consider broader community needs and recovery. Furthermore, PROs are an important aspect of the continued shift from a fee-for-service to value-based healthcare system that places patient health and well-being at the center of their treatment and care [39]. Having a fuller understanding of individual COVID-19 outcomes and experiences will facilitate the movement towards a value-based healthcare system and more holistic care management.
This study has several key limitations. First, the population is limited to patients infected with COVID-19 who engage in this app-based English-language study through Providence and test positive for COVID-19 at a Providence facility. Thus, the population engaged skews toward people with mobile technology access, willingness to engage in research, access and proximity to care, and who have English proficiency and therefore may not be generalizable to the vaccinated population. For example, the population who engaged was predominately White, even though COVID-19 has disproportionately impacted people of color due to inequitable distribution of social risk factors and treatment when seeking care [40, 41]. It is well-established that people of color have a history of trauma with research that discourages their participation [42, 43]; more efforts are needed to gather PROs for people of color, including culturally appropriate approaches. Participation was high in the first 3 weeks, followed by increasing attrition leading to smaller population sizes in later timepoints. The data also lacked participants’ geographical information, existing comorbidities, or PROs prior to COVID-19 infection, therefore these could not be considered in our analysis. Additionally, we were unable to validate self-reported vaccination status against patients’ medical records due to the MCD design and the IRB approval process. This population had higher than expected hospitalization and ED visits for COVID-19, suggesting that participation in MCD might be correlated with greater symptom severity. Finally, this study focused only on the first 6 weeks after COVID-19 infection; future studies should explore PROs in the vaccinated (and unvaccinated) population beyond this timepoint.
5 Conclusion
Taken together, the results describe the range of physical and mental health impacts of symptomatic COVID-19 infections for vaccinated patients and emphasize the importance of understanding patient-reported physical and mental health experiences as part of treatment and recovery.
References
CDC COVID Data Tracker: Trends in Number of COVID-19 Cases and Deaths in the US Reported to CDC, by State/Territory. Available at: https://covid.cdc.gov/covid-data-tracker/#trends_dailycases. Accessed 10 Feb 2022.
WHO Coronavirus (COVID-19) Dashboard. Available at: https://covid19.who.int/. Accessed 10 Feb 2022.
Baden LR, el Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384:403–16. https://doi.org/10.1056/NEJMoa2035389.
Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. N Engl J Med. 2020;383:2603–15. https://doi.org/10.1056/NEJMoa2034577.
Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384:2187–201. https://doi.org/10.1056/NEJMoa2101544.
CDC COVID Data Tracker: Cumulative Count of Fully Vaccinated People Reported to CDC by Date Administered, United States. Available at: https://covid.cdc.gov/covid-data-tracker/#vaccination-trends_vacctrends-fully-cum. Accessed 10 Feb 2022.
Chodick G, Tene L, Rotem RS, Patalon T, Gazit S, Ben-Tov A, et al. The effectiveness of the two-dose BNT162b2 vaccine: analysis of real-world data. Clin Infect Dis. 2022;74:472–8. https://doi.org/10.1093/cid/ciab438.
Bruxvoort KJ, Sy LS, Qian L, Ackerson BK, Luo Y, Lee GS, et al. Real-world effectiveness of the mRNA-1273 vaccine against COVID-19: interim results from a prospective observational cohort study. Lancet Region Health Am. 2022;6: 100134. https://doi.org/10.1016/j.lana.2021.100134.
Corchado-Garcia J, Hughes T, Cristea-Platon T, Lenehan P, Pawlowski C, et al. Real-world effectiveness of Ad26.COV2.S adenoviral vector vaccine for COVID-19. SSRN Electron J. 2021. https://doi.org/10.2139/ssrn.3835737.
Tartof SY, Slezak JM, Fischer H, Hong V, Ackerson BK, Ranasinghe ON, et al. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: a retrospective cohort study. Lancet. 2021;398(10309):1407–16. https://doi.org/10.1016/S0140-6736(21)02183-8.
Rosenberg ES, Holtgrave DR, Dorabawila V, Conroy M, Greene D, Lutterloh E, et al. New COVID-19 cases and hospitalizations among adults, by vaccination status—New York, May 3–July 25, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1150–5. https://doi.org/10.15585/mmwr.mm7034e1.
Bajema KL, Dahl RM, Prill MM, Meites E, Rodriguez-Barradas MC, Marconi VC, et al. Effectiveness of COVID-19 mRNA vaccines against COVID-19–associated hospitalization—five veterans affairs medical centers, United States, February 1–August 6, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1294–9. https://doi.org/10.15585/mmwr.mm7037e3.
Thompson MG, Burgess JL, Naleway AL, Tyner H, Yoon SK, Meece J, et al. Prevention and attenuation of covid-19 with the BNT162b2 and mRNA-1273 vaccines. N Engl J Med. 2021;385:320–9. https://doi.org/10.1056/NEJMoa2107058.
Antonelli M, Penfold RS, Merino J, Sudre CH, Molteni E, Berry S, et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. Lancet Infect Dis. 2022;22(1):P43-45. https://doi.org/10.1016/S1473-3099(21)00460-6.
Weldring T, Smith SMS. Article commentary: patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights. 2013;6:11093. https://doi.org/10.4137/HSI.S11093.
Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63:1179–94. https://doi.org/10.1016/j.jclinepi.2010.04.011.
Ganesh R, Ghosh AK, Nyman MA, Croghan IT, Grach SL, Anstine CV, et al. PROMIS scales for assessment of persistent post-COVID symptoms: a cross sectional study. J Prim Care Community Health. 2021;12:215013272110304. https://doi.org/10.1177/21501327211030413.
Wong AW, Shah AS, Johnston JC, Carlsten C, Ryerson CJ. Patient-reported outcome measures after COVID-19: a prospective cohort study. Eur Respir J. 2020;56:2003276. https://doi.org/10.1183/13993003.03276-2020.
Shah AS, Ryu MH, Hague CJ, Murphy DT, Johnston JC, Ryerson CJ, et al. Changes in pulmonary function and patient-reported outcomes during COVID-19 recovery: a longitudinal, prospective cohort study. ERJ Open Res. 2021;7:00243–2021. https://doi.org/10.1183/23120541.00243-2021.
Carfì A, Bernabei R, Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603. https://doi.org/10.1001/jama.2020.12603.
Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet. 2021;397:220–32. https://doi.org/10.1016/S0140-6736(20)32656-8.
Jacobs LG, Paleoudis EG, di Bari DL, Nyirenda T, Friedman T, Gupta A, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS ONE. 2020;15(12): e0243882. https://doi.org/10.1371/journal.pone.0243882.
Weerahandi H, Hochman KA, Simon E, Blaum C, Chodosh J, Duan E, et al. Post-discharge health status and symptoms in patients with severe COVID-19. J Gen Intern Med. 2021;36:738–45. https://doi.org/10.1007/s11606-020-06338-4.
U.S. Department of Health and Human Services. Scoring PROMIS Global Short Form Scoring Global Short Form 2010. Available at: https://data.mncm.org/help/faq_documents/0000/0916/Scoring_PROMIS_Global_short_form_8-2014.pdf. Accessed 8 Sep 2022.
US Department of Health and Human Services. PROMIS: Explore Measurement Systems 2022. Available at: https://www.healthmeasures.net/explore-measurement-systems/promis. Accessed 8 Sep 2022.
Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The patient-reported outcomes measurement information system (PROMIS): progress of an NIH roadmap cooperative group during its first two years. Med Care. 2007;45:S3-11. https://doi.org/10.1097/01.mlr.0000258615.42478.55.
Hays RD, Bjorner JB, Dennis AE, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18:873–80. https://doi.org/10.1007/s11136-009-9496-9.
Blair PW, Brown DM, Jang M, Antar AAR, Keruly JC, Bachu VS, et al. The clinical course of COVID-19 in the outpatient setting: a prospective cohort study. Open Forum Infect Dis. 2021;8:7. https://doi.org/10.1093/OFID/OFAB007.
Richard SA, Epsi NJ, Lindholm DA, Malloy AMW, Maves RC, Berjohn CM, et al. COVID-19 patient-reported symptoms using FLU-PRO plus in a cohort study: associations with infecting genotype, vaccine history, and return to health. Open Forum Infect Dis. 2022;9:275. https://doi.org/10.1093/ofid/ofac275.
Tenforde MW, Kim SS, Lindsell CJ, Billig Rose E, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:993–8. https://doi.org/10.15585/mmwr.mm6930e1.
Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. BNT162b2 mRNA covid-19 vaccine in a nationwide mass vaccination setting. N Engl J Med. 2021;384:1412–23. https://doi.org/10.1056/NEJMoa2101765.
Shi Q, Mendoza TR, Cleeland CS. Interpreting patient-reported outcome scores for clinical research and practice. Med Care. 2019;57:S8-12. https://doi.org/10.1097/MLR.0000000000001062.
Lapin B, Katzan IL. Health-related quality of life mildly affected following COVID-19: a retrospective pre-post cohort study with a propensity score-matched control group. J Gen Intern Med. 2022;37:862–9. https://doi.org/10.1007/s11606-021-07340-0.
Terwee CB, Peipert JD, Chapman R, Lai J-S, Terluin B, Cella D, et al. Minimal important change (MIC): a conceptual clarification and systematic review of MIC estimates of PROMIS measures. Qual Life Res. 2021;30:2729–54. https://doi.org/10.1007/s11136-021-02925-y.
Kharbanda R, Ganatra K, Abbasi M, Agarwal V, Gupta L. Patients with idiopathic inflammatory myopathies suffer from worse self-reported PROMIS physical function after COVID-19 infection: an interview-based study from the MyoCite cohort. Clin Rheumatol. 2022;41:2269–72. https://doi.org/10.1007/s10067-022-06204-0.
Horwitz LI, Garry K, Prete AM, Sharma S, Mendoza F, Kahan T, et al. Six-month outcomes in patients hospitalized with severe COVID-19. J Gen Intern Med. 2021;36:3772–7. https://doi.org/10.1007/s11606-021-07032-9.
Ziegler S, Raineri A, Nittas V, Rangelov N, Vollrath F, Britt C, et al. Long COVID citizen scientists: developing a needs-based research agenda by persons affected by long COVID. Patient Patient Center Outcomes Res. 2022;15:565–76. https://doi.org/10.1007/s40271-022-00579-7.
Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, et al. Epidemiology of mental health problems in COVID-19: A review. F1000Res. 2020. https://doi.org/10.12688/f1000research.24457.1.
Squitieri L, Bozic KJ, Pusic AL. The role of patient-reported outcome measures in value-based payment reform. Value Health. 2017;20:834–6. https://doi.org/10.1016/j.jval.2017.02.003.
Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis. 2021;72:703–6. https://doi.org/10.1093/cid/ciaa815.
Bergmans RS, Chambers-Peeple K, Aboul-Hassan D, Dell’Imperio S, Martin A, Wegryn-Jones R, et al. Opportunities to improve long COVID care: implications from semi-structured interviews with black patients. Patient Outcomes Res. 2022. https://doi.org/10.1007/s40271-022-00594-8.
Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underserved. 2010;21:879–97. https://doi.org/10.1353/hpu.0.0323.
George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(2):e16-31. https://doi.org/10.2105/AJPH.2013.301706.
Acknowledgments
The authors would like to acknowledge Bradley Roberts for his support and critical input throughout the My COVID Diary project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author contributions
Conceptualization: KV, DF, BG, NK, AR. Methodology: DF. Formal analysis: DF. Data curation: DF. Writing – original draft preparation: DF, KV. Writing – review and editing: BG, NK, AR. Visualization: DF, BG, NK. Investigation: DF. Funding acquisition: KV. Supervision: KV.
Funding
This study was funded by Providence St. Joseph Health and the Providence St. Joseph Foundation.
Conflicts of interest
Keri Vartanian, Daniel Fish, Benjamin Gronowski, Natalie Kenton, and Ari Robicsek declare that they have no financial or non-financial conflicts of interest.
Ethics approval
The full study protocol was approved by the Providence St. Joseph Health Institutional Review Board (IRB# 2020000467). The study was performed in line with the principles of the Declaration of Helsinki.
Consent to participate
Mobile device-administered informed consent was obtained from all participants included in the study. Participants were informed about their freedom to refuse to participate. Anonymity and confidentiality were maintained throughout the research process.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available due to identifying participant personal and health information. Additionally, data collection is still ongoing. In the future, de-identified portions of the dataset may be made publicly available.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Vartanian, K., Fish, D., Gronowski, B. et al. Patient-Reported Outcomes for Fully Vaccinated COVID-19 Patients Over 6 Weeks: The Experiences of Clinical Breakthrough Cases. Patient 16, 105–116 (2023). https://doi.org/10.1007/s40271-022-00605-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-022-00605-8