Abstract
Background
Uncertainty about the benefits new cancer medicines will deliver in clinical practice risks delaying patient access to new treatment options in countries such as England, where the cost effectiveness of new medicines affects reimbursement decisions. Outcome-based payment (OBP) schemes, whereby the price paid for the drug is linked to patients’ real-world treatment outcome(s) has been put forward as a mechanism to accelerate access. Although OBP schemes have generally focused on clinical outcomes to determine reimbursement, the degree to which these represent the outcomes that are important to patients is unclear.
Objective
To advance the application of OBP we ask, what outcomes do patients with cancer value (most) that might form a practical basis for OBP?
Methods
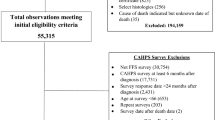
A review of the literature on outcomes in cancer produced a long list of candidates. These were evaluated in a focus group with patients with cancer and were then, in a second focus group, distilled to a shortlist of ten outcomes using a card sort method. The ten outcomes were included in an online survey of patients with cancer and carers, who were asked to rank the importance of each outcome.
Results
The focus groups identified a range of both clinical and functional outcomes that are important to patients. Analyses of the 164 survey responses suggested that the four most important outcomes to patients and carers are survival; progression, relapse or recurrence; post-treatment side effects; and return to normal activities of daily life.
Conclusion
Commissioners of cancer services wishing to instigate an OBP scheme should prioritise collecting data on these outcomes as they are important to patients. Of these, only mortality data are routinely collected within the national health service (NHS). Progression and some morbidity data exist but are not currently linked, creating a challenge for OBP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Outcome-based payment schemes for new medicines should address the outcomes that patients and carers value most. |
The four most important outcomes to patients and carers are survival; progression, relapse or recurrence; post-treatment side effects; and return to normal activities of daily life. |
Only mortality data are routinely collected within the National Health Service; collecting data on the four core outcomes should be prioritised to realise outcome-based payment for some new cancer medicines in future. |
1 Introduction
More than 360,000 people in the UK are diagnosed with cancer each year [1]. Of these, around 28% receive cancer drugs as part of their primary treatment, though this proportion is significantly higher for those diagnosed when their disease is more advanced [2]. To ensure appropriate care for these patients, they need to access new, more effective medicines for their condition.
It is estimated the UK spends around £2 billion each year on cancer medicines [3], and growth in oncology medicines spending globally is expected to increase on average by 10–13% over the next 5 years [4]. Much of the recent and anticipated future growth in spending can be attributed to advances in the development of cancer medicines: in 2005 there were 399 cancer drugs in development in the USA (in clinical trials or awaiting review by the US FDA), whereas today there are an estimated 1120 drugs [5]. Many of these new medicines are more effective than medicines used currently but also more expensive.
Many new treatments are being approved by regulatory agencies, including the European Medicines Agency, with increasingly immature or incomplete data. Approval based on immature or incomplete data can be a particular issue in cases where the patient group is small or where outcomes only become clear beyond the timescale of a clinical trial. There is then uncertainty about the extent of a medicine’s effectiveness. This poses a challenge to patient access, since many countries have an additional step before a licensed cancer drug (one that has regulatory approval) can be made available to patients (either reimbursed publicly or via an insurance scheme). Its comparative clinical effectiveness and—in many healthcare systems, including the UK’s—its cost effectiveness must be evaluated via a process called health technology assessment (HTA).
In England, before a patient has access to a cancer medicine on the National Health Service (NHS), the drug’s clinical and cost effectiveness must be assessed by the National Institute for Health and Care Excellence (NICE), normally using data from clinical trials. Such trials are vital for establishing the safety and efficacy of treatments. Clinical trials data are also used to inform any price negotiations between the drug manufacturer and the NHS. But trial evidence may not reflect the outcomes that will be achieved when medicines are used in a real-world setting, as the trial patients and setting may not reflect routine clinical practice or the mix of patients who are treated. For example, in real-world practice, some patients will have comorbidities along with their cancer, but patients in clinical trials will have been selected to be without such comorbidities [6]. This creates further uncertainty about the cost effectiveness of the new medicines. Together with the uncertainty arising from immaturities or gaps in the clinical trial data, this may lead to delays in patients receiving them.
Approaches to improving patient access are needed that respect the financial constraints on the healthcare system. The Accelerated Access Review (AAR) [7] proposed that NHS England should adopt more flexible pricing mechanisms to assist the swift adoption and reimbursement of products (including medicines) under early access schemes. These offer adjustment options for the price of a medicine in light of the experience of patients treated with it and thereby reduce the risk of overpaying for products that do not deliver the expected benefits in practice, or undervaluing products that deliver transformative long-term benefits for patients that cannot be quantified at the time of HTA.
Cancer Research UK and Greater Manchester Health and Social Care Partnership (GMHSCP) jointly commissioned the authors to explore the possibility of developing a new model of paying for some cancer drugs within the NHS, both in Greater Manchester and at a national level, explicitly on the basis of the outcomes they achieve, and specifically the outcomes that are most important to patients [8, 9]. Outcome-based payment (OBP) aligns a medicine’s cost to the NHS and the payment to its manufacturer with the benefits it delivers for patients in the real world. OBP schemes generally focus on clinical outcomes to determine the extent of disease progression and subsequent reimbursement [10]. However, the degree to which these outcomes are important to patients is unclear.
The aim of this project was to understand the outcomes that patients with cancer value (most). To aid our understanding, we considered the following specific objectives:
-
Using qualitative research approaches, determine which treatment outcomes identified in a literature review are of most importance to patients with cancer.
-
Using a quantitative survey approach, gain a broader understanding and a ranking of what treatment outcomes matter most to patients with cancer and their carers.
2 Methods
We employed a mixed-methods approach to understand what outcomes patients with cancer value. We undertook a rapid evidence assessment to identify outcomes of cancer treatment, including clinical outcomes, patient-reported outcomes and patient experience measures. For space reasons, the methods and results of this literature review are provided in Appendix 1 in the Electronic Supplementary Material (ESM). The key output of the literature review was the synthesis and categorisation of outcomes into an outcomes framework or ‘value flower’ [11], see Fig. 1.Footnote 1 Table 1 provides definitions for the high-level outcomes (the petals of the flower).
Two focus groups were then employed as the first of two approaches to obtaining a patient voice. The second stage was a survey of patients with cancer and carers, which is described later in this section. Focus group participants were identified via a dedicated Cancer Research UK webpage through which patients with cancer could declare their interest in participating directly to the research team. All who declared interest were invited to participate. Participants were paid an honorarium of £30 plus travel expenses up to £50. We closed recruitment on the focus groups when we had ten individuals confirmed for each, as per standard qualitative research practice [12].
The first focus group aimed to identify which types of treatment outcomes among those identified in the literature review are important to patients with cancer, particularly when considering their own cancer drug treatments. In this focus group, participants were specifically asked which of the high-level outcomes shown in Fig. 1 (the flower petals) were most important to them and whether any important outcomes were missing. We emphasised that we were interested in the outcomes of medicines they received, or the expected outcomes of medicines they were offered but declined, during their treatment for cancer. We additionally enquired as to the participants’ ability to rank a set of outcomes, including how many outcomes were optimal to have in a ranking exercise. The focus group was recorded, and the two facilitators also took notes. The analysis was informed by the field notes and the audio recordings.
The first focus group raised concerns that their ability to rank outcomes (in a subsequent survey) would be challenging if there was a large number of outcomes to rank. Therefore, we sought to identify a shorter list to inform a future OBP scheme. Building on the high-level outcomes we presented in the first focus group (as identified in the literature review), supplemented by any additional outcomes identified within the first focus group, a second focus group aimed to identify a more specific list of important treatment outcomes and which were the most important among those. A card sort technique similar to that employed in cognitive psychology was used [13]. Participants were split into pairs and presented with 34 more specific treatment outcomes derived from the high-level outcomes and written on individual A5-sized cards. In their pairs, the participants were asked to order the 34 outcomes into a diamond structure, with the ‘most important’ outcome(s) at the top of the diamond and the ‘least important’ outcome(s) at the bottom. The diamond shape imposed an expectation that there would be more cards placed in the middle and less at the extremes, thus challenging the participants to work together to effectively prioritise. Participants were also invited to highlight any outcomes they felt were missing from this list and to rank them accordingly. They were encouraged to conflate outcomes they thought were similar constructs. This technique reduced the number of outcomes while taking into account the dimensions of quality of life that patients with cancer deemed important. As in the first focus group, participants were asked to reflect on how many outcomes could be included in a future ranking exercise. This focus group was not recorded (because of acoustics), but each pair was facilitated by a study team member who took field notes on the prioritisation process as it was discussed by participants.
Focus group participants appeared to be most comfortable ranking a smaller list of outcomes: ten was chosen for simplicity. The ten chosen were informed by the card sort exercise and our analysis of focus group discussions and guided by our previous review of the literature. This refined shorter list of outcomes was then included in a survey of current and former patients with cancer and current and former carers of someone with cancer. The survey was carried out, during August and September 2018, to gain a broader understanding of what treatment outcomes matter most to patients with cancer and their carers, building on the findings from the focus groups. The survey (using SmartSurvey v4.10.1) was uploaded to the ‘Patient Involvement at Cancer Research UK’ section of the Cancer Research UK website, advertised to patients and carers via a Cancer Research newsletter and promoted on social media. (Consequently, it is not possible to know how many people were aware of the survey, and hence not possible to determine the response rate we obtained.)
Ethical approval for the study was granted by the Biomedical and Health Sciences, Dentistry, Medicine and Natural and Mathematical Sciences Research Ethics Subcommittees (BDM RESC) at King’s College London, UK (ref: LRS-17/18-5723).
The survey questionnaire is available in Appendix 2 of the ESM. Survey respondents were asked, “When being offered a cancer medicine (e.g. chemotherapy, immunotherapy, targeted therapy or hormone therapy), which of the following factors were [or would be] of most importance to you {/the person you care for}? Please order the 10 outcomes from 1 (most important) to 10 (least important)”. The list of ten outcomes, and the justification for that particular list, are set out in Sect. 3. Outcomes were randomly ordered for each respondent to mitigate any framing effect bias.
To estimate importance, the median, interquartile range and mean of the rank score of each outcome were calculated. Caution is always necessary in such analysis because the ranking reflects ordinal rather than cardinal preferences. It takes no account of whether, for example, the outcome ranked 1 was a lot, or only a little, more important than the outcome ranked 2. However, in this case, calculating these measures of average and dispersion, it proved possible to identify a subset of the outcomes that were ranked by most respondents more highly than the rest.
Information was gathered on respondents’ sex, age group and employment status. Respondents were asked whether they were a patient or carer, or both; which cancer(s) they had been diagnosed with; how long since they were last diagnosed with cancer; which treatment(s) they had received for their cancer; and whether the intention of that treatment was to cure or control their cancer. Respondents who reported being a carer were asked to answer with respect to the person they were or had been caring for. Individuals identifying as both a patient and carer were asked to answer as patients. Respondents who reported more than one cancer diagnosis were asked the ‘time since diagnosis’ question in respect of their most recent cancer diagnosis.
3 Results
Both focus group discussions were facilitated by PKL, assisted by JP. The first focus group took place in central Manchester in June 2018, with five participants. This was smaller than planned (N = 10), but the focus group unfortunately coincided with an extremely warm day, wildfires close to Greater Manchester and England’s final group game in the football World Cup 2018. The second focus group took place in central London in July 2018, with four participants. Again, this was smaller than planned (possibly due to the central London location on a summer’s evening) but nonetheless provided useful data as a smaller group, who worked in pairs and went into more depth on the questions. Table 2 details the characteristics of the participants: a mixture of ages and sexes were represented, with females being most represented. Participants drew on experience from a wide range of cancers.
3.1 Outcomes of Importance—Focus Groups
During the first focus group’s discussions, each of the high-level outcome ‘petals’ (Fig. 1) was identified as important to at least one of the participants. It became apparent during discussions that participants were able to differentiate between the outcomes, such that, while all outcomes are important, some outcomes were regarded as more important than others. The one outcome ‘petal’ that was regarded by all participants as the most important was ‘clinical outcomes’, with a particular focus on life extension, “how long I stay alive is the most important outcome for me” [Participant 5, female, breast cancer, 60–69 years].
Quality of life, as captured by the four ‘functioning’ types of outcomes (Fig. 1, pink petals), was also regarded as extremely important, if not as important as life extension for some participants: “quality of life, not just length, is important” [Participant 2, male, prostate cancer, 60–69 years]; “extending life is not the only outcome of importance, it is important to feel useful and that you are benefiting from being around” [Participant 4, female, breast cancer, 60–69 years]; and “it is important to have a sense of agency… [and] a feeling of getting back to normal” [Participant 2, male, prostate cancer, 60–69 years].
Treatment toxicity, particularly some of its side effects, was also important. Participant 1 spoke about wanting to spend time with his grandchild, which he would not be able to do had he undergone chemotherapy because of the impact on his immune system as a treatment side effect. Another participant suggested that the potential side effect of infertility “would be considerably more important for a younger person, particularly if they did not have any children yet” [Participant 4, female, breast cancer, 60–69 years].
Adverse events were also identified as important to participants, with a particular issue being the potential need for reoperation. This highlights one of the difficulties that focus group participants experienced: separating the outcomes they experienced as a result of their drug treatments from outcomes resulting from their continuum of cancer care, for example, their diagnosis through to surgery through to radiotherapy and now their experience of ‘living’ with cancer.
The environment within which the drug is administered was also raised by participants, which comes under the ‘treatment process’ heading in Fig. 1. While some participants would rather receive treatment in the comfort of their own home, others enjoyed being able to socialise with other patients with cancer while receiving treatment in a hospital chemotherapy unit.
Finally, the impact of treatment and the wider cancer experience on family members was also identified as important, which sits under the ‘social functioning’ heading. Participant 3 noted that this was particularly important to her as her family “split for a while” [Participant 3, female, bone cancer, 20–29 years] following the cancer diagnosis.
During the focus group discussion, participants raised the issue of context. That is, the outcomes of most importance depend greatly on the characteristics and context of the individual, the cancer they are being treated for and the drug they are receiving. For example, participants felt that clinical outcomes may be relatively more important for older patients, whereas ‘functioning’ outcomes may be relatively more important to younger patients. This context issue will be important for future research.
The second focus group were tasked with refining and reducing the list of outcomes—aided with a card sort technique undertaken in pairs—to a shorter list of more important outcomes. The positioning of their cards by each pair is illustrated in Figs. 2 and 3. The most important outcomes for each pair are in the top row of the figure and the least important in the bottom row. There is no significance to the relative position of individual outcomes within each row of each figure. Comparing Figs. 2 and 3, it is clear that, although there is consensus across the two pairs with respect to the relative importance of certain outcomes, there is also disagreement about others. Overall, the discussion on outcomes of importance in the pairs can be summarised in five categories: life extension and quality of life, side effects, emotional functioning, impact on family and satisfaction with the treatment.
Pair 2 ranked life extension as an ‘important’ outcome, particularly because of its direct link to hope; without the potential for life extension, hope suffers. Pair 1 also acknowledged the importance of life extension and went on to argue that patients also want a good quality of life. This, they felt, was just as important as life extension; returning to a sense of normality (e.g. returning to normal activities, returning to work, regaining mobility) were good determinants of quality of life. Pair 2 agreed that it is not just about returning to work, for example, but about returning to normality more broadly.
Both pairs agreed that all of the individual outcomes describing side effects could be grouped into broader side effects outcomes. Pair 2 listed the individual side effect outcomes under a single ‘side effects’ category and ranked it as ‘less important’. This was partly because of how well many side effects, particularly pain, are now managed. However, pair 1 argued that there are two distinct types of side effects: short-term, in-treatment side effects and long-term, post-treatment side effects. In-treatment side effects were regarded as ‘less important’ as patients are willing to put up with them if the treatment keeps you alive. Long-term, post-treatment side effects were ranked as important because of their lasting impacts.
Anxiety, depression, lack of hope and lack of confidence were combined by pair 1 and classed as ‘fairly important’. According to participants 6 and 7, these outcomes should all be ‘grouped together and could be included as a sentence [in the survey]’. Pair 2 combined depression, anxiety and social support/loneliness under the emotional wellbeing outcome and ranked these as ‘important’. All of these specific outcomes fall under the wider ‘emotional functioning’ heading in the outcomes flower (Fig. 1), suggesting that the patients with cancer were comfortable viewing these outcomes as a single, wider emotional functioning or emotional wellbeing outcome.
Pair 1 and pair 2 both grouped burden on loved ones and relying on caregiver/family under the ‘impact on family’ outcome. Pair 2 acknowledged that cancer in general is a burden on loved ones, children and parents. They then went on to discuss how the cancer treatment itself could impact on their family, for example through changes in appearance and the impact this could have on a patient’s child. Overall, pair 1 ranked impact on family as ‘important’ but then classed it as ‘out of scope’ because the impact on family comes from the diagnosis and not the treatment.
Satisfaction with treatment was regarded as ‘important’ by pair 2. Participant 9 explained that they wanted to receive their cancer treatment at home but could not because they were unable to inject themselves. It was then suggested that satisfaction might come under quality of care, which could be an outcome in its own right but is not for the most part a consequence of the medicine used and therefore is out of scope for an OBP scheme. Pair 1 argued that satisfaction with the treatment is ‘peripheral’ and therefore ranked it as ‘least important’ compared with the other outcomes.
Finally, pair 2 created a new category, ‘coping’, which includes hearing, speech, tiredness and so on, and ranked it as the ‘most important’ outcome. However, they noted that separating out the role of the medicine from the wider cancer experience would be difficult, an issue identified in the first focus group.
While the most important outcomes appear to differ across the two pairs when comparing Figs. 2 and 3, they both suggest that ‘normality’ is important: returning to normal activities, returning to work, mobility, avoiding recurrence (pair 1) and coping, communicating, sleeping and confidence (pair 2). In terms of outcomes that were least/less important, these are either side effects of the treatment or are consequences of the cancer diagnosis rather than the treatment.
Given discussions in both focus groups and the card sort exercise, together with the participants’ views on the planned ranking task, as well as our previous literature review, we identified the following ten outcomes as of importance to patients with cancer (in no particular order):
-
Long-term after-treatment side effects
-
Infertility
-
Survival
-
Satisfaction with treatment
-
Progression/recurrence
-
Return to normal activities of daily living
-
Emotional wellbeing
-
Having to undergo surgery again
-
Impact on family and caregivers
-
Short-term in-treatment side effects.
3.2 Outcomes of Importance—Survey
The online survey recorded 164 complete responses from patients with cancer and carers to be analysed. The sex, age and employment status at diagnosis of the respondents are shown in Table 3. The large majority (n = 144) of the 164 respondents were female. Among the respondents, the most common age group was 51–60 years (58 respondents), followed by 61–70 years (n = 41) and 41–50 years (n = 38). The great majority (n = 128) of respondents were in employment at the time of the cancer diagnosis (full-time, part-time or self-employed), and six were students (Table 3).
Table 4 details the experiences that respondents had with cancer. The vast majority (n = 144) were patients, with the other 20 identifying as carers. The majority (n = 100) of individuals had experienced breast cancer (either as patients or carers), with lung and bowel/colorectal cancer being the equal second most common, with 16 respondents each. It is worth noting that patients can be diagnosed with more than one cancer. A slight majority (n = 85) of respondents were last diagnosed 1–5 years ago or were caring for someone last diagnosed 1–5 years ago. The majority of respondents had undergone, or cared for someone who had undergone, surgery (n = 127), chemotherapy (n = 117) and/or radiotherapy (n = 111), with a substantial minority receiving hormone therapy (n = 77). Patients typically receive more than one treatment. The purpose of these treatments was curative for the majority (n = 118), with 39 respondents reporting that the treatment was designed to control the cancer rather than cure it.
Respondents were asked to rank the outcomes from 1, most important, to 10, least important. Therefore, the lower the score, the more important the outcome. Table 5 reports the median and interquartile ranges for the ranks (from 1 to 10) accorded to the outcomes by the survey respondents and attributes an overall rank for each outcome according to that median. We also show the mean rank score in the final column of Table 5 to provide a bit more information about the distribution of scores, which is helpful to differentiate when medians and interquartile ranges for two outcomes are the same. The outcomes are accorded an overall rank on the basis of median rank, and where medians are the same ranking by mean rank score.
Across the whole sample, ‘survival’ and ‘progression, relapse or recurrence’ scored noticeably better than the other eight outcomes, with median rank scores of 1 and 2, respectively, and thus appear to be the two most important outcomes. ‘Long-term side effects’ and ‘return to normal activities of daily life’ each had a median rank score of 4 and thus were clearly more highly ranked than the next highest outcome median rank scores, which were 6 for ‘short-term side effects’ and ‘emotional wellbeing’. There is then a relatively small difference in scores amongst the next three outcomes: ‘satisfaction with treatment’, ‘re-surgery’ and ‘impact on family and caregivers’. Finally, the outcome ‘fertility problems’ was clearly ranked lower than all other outcomes in the list of ten.
4 Discussion
The research was undertaken in response to the wish of a commissioner of cancer services in the NHS in England, the GMHSCP and an independent cancer charity, Cancer Research UK, to understand which real-world outcomes patients with cancer value most. The intention of these organisations was to determine whether OBP, based on those particular outcomes of most importance to patients, can practically be implemented in the NHS in Greater Manchester and in England more widely. Further work is being undertaken by GMHSCP and Cancer Research UK to design just such an OBP scheme [8]. The research was therefore aimed at understanding more about the relative importance to patients of different cancer treatment outcomes than about a broader scope regarding which health dimensions are important to patients with cancer irrespective of treatment, or which data might be collected and used to realise OBP for some new cancer medicines in future.
To our knowledge, this is the first study that has sought to understand which outcomes are most important to patients in the context of planning for an OBP scheme. Previous OBP schemes almost exclusively focus on clinical outcomes and therefore are likely driven by what clinicians or industry think are important. While we find that the clinical outcomes such as survival and disease progression are important to patients, other functioning concepts are also important. Our findings are aligned with the literature on clinical decision making. For example, McMullen et al. [14] used interviews and a survey and found that patients reported severity of adverse events as a deterrent to receiving treatment for advanced non-small-cell lung cancer, whereas the major motivator was the potential to extend life. In another study, which reviewed the literature and patient-reported information shared on YouTube, Crawford et al. [15] identified that therapies that could potentially delay progression and extend life were of great importance to patients, particularly in terms of quality-of-life impact and disruption to daily life.
The main limitations of our study are the modest numbers of patients with cancer who participated in the two focus groups and the unbalanced sample of patients with cancer and carers who responded to the online survey, with the number of females and patients with breast cancer being disproportionately high. Focus group discussions were employed to narrow the large number of different cancer outcomes revealed by the literature review to a list of ten that could be tested in a survey of patients and carers. Although it is possible that conducting more focus groups could have led to some different outcomes being included in the list of ten, it seems very unlikely that any such list would have excluded any of the four outcomes that in the event were ranked most highly in the survey process, namely survival; progression, relapse or recurrence; long-term side effects; and return to normal activities of daily life.
The sample of survey respondents contained a disproportionate number with an experience of breast cancer. This is partly because of breast cancer is common and has good survivability, but that does not fully explain the preponderance of respondents with breast cancer. We cannot be sure to what extent the rankings of outcomes would have been different with a more balanced array of cancers experienced. However, as an indication, we have compared, in Fig. 4, the median ranking scores for the patients with breast cancer who responded to the survey with those for the patients with lung cancer and bowel/colorectal, respectively. Sample sizes were too small to compare any other cancer types. There is a notable degree of agreement in rank scores across the three cancer types. Survival and progression were the two most important outcomes among all three cancer type subgroups. Patients with lung cancer and carers (n = 16) ranked return to normal activity as the third most important outcome and long-term side effects fourth, whereas patients with breast (n = 100) and bowel/colorectal cancer (n = 16) and carers ranked long-term side effects as the third most important and return to normal activities fourth. While all cancer types yield the same top four most important outcomes, we acknowledge that the relative stability of the results could change with a broader, more representative sample, for example a sample that included younger individuals may rank fertility concerns much higher.
There were also some differences between respondents according to whether the purpose of their treatment was curative or merely to control progression (results not shown). While the top two outcomes were the same regardless of treatment intent, those patients receiving medicines to control or manage their cancer ranked returning to normal activities above long-term side effects, and emotional wellbeing above short-term side effects; patients who had received (or were receiving) medicines to cure had rankings similar to the sample as a whole. This aligns with the work of Minion et al. [16], who considered the preferences of patients with ovarian cancer and how they differ with treatment intent. The heterogeneity of responses across patients with different experiences confirms the context-specificity issues identified in the focus groups.
Researchers, commissioners or the pharmaceutical industry who are considering an OBP scheme may wish to revisit the issue of context. We were specifically tasked with understanding outcomes for cancer broadly, in order to be generalisable. We hope our methods can be reproduced by others seeking to understand what outcomes are important to patients with other diseases or conditions.
Going forward, our research focuses on four types of outcomes: survival; progression, relapse or recurrence; post-treatment side effects; and return to normal activities of daily life. We wish to go beyond the usual practice in OBP schemes hitherto of focusing on a single outcome measure to determine payment, while being mindful of practical considerations concerning OBP scheme negotiation and the burden of collecting outcome data. We are therefore focusing on the four outcomes that were most highly ranked by patients and were clearly more highly ranked than any of the other ten outcomes.
5 Conclusion
A commissioner of cancer services in England wishing to instigate OBP schemes for new medicines that capture the outcomes that matter most to people affected by cancer might prioritise collecting data on the following four types of outcomes: survival; progression, relapse or recurrence; post-treatment side effects; and return to normal activities of daily life. Of these, only mortality data are currently routinely collected within the NHS in England. Cancer progression and some morbidity data exist but are not currently linked, creating a challenge for OBP. Further work is planned to address how far that challenge might practically be met.
Data Availability Statement
The consent granted by survey respondents limits access to the data to the research team, so it is not possible to publish the data.
Notes
Figure 1 is a reproduction of Figure A2 in Appendix 1.
References
Cancer Research UK. Cancer incidence statistics [Internet]. https://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence.
Cancer Research UK. Cancer diagnosis and treatment statistics [Internet]. https://www.cancerresearchuk.org/health-professional/cancer-statistics/diagnosis-and-treatment.
IQVIA Institute for Human Data Science. Understanding the Dynamics of Drug Expenditure: Shares, Levels, Compositions, and Drivers. 2017.
IQVIA Institute for Human Data Science. Global Oncology Trends 2018: Innovation, Expansion and Disruption. 2018.
Statista. Number of cancer drugs in development in the United States in select years between 2005 and 2018 [Internet]. https://www.statista.com/statistics/268805/number-of-cancer-drugs-in-development-since-2005/.
Devlin NJ, Lorgelly PK. QALYs as a measure of value in cancer. J Cancer Policy. 2017;11:19–25.
Taylor H, Bell J. Accelerated Access review: final report. Review of innovative medicines and medical technologies London: Wellcome Trust. 2016.
Cancer Research UK. Outcome-based payment for cancer drugs [Internet]. https://www.cancerresearchuk.org/about-us/we-develop-policy/our-policy-on-access-to-cancer-treatments/outcome-based-payment-for-cancer-drugs.
Cole A, Cubi-Molla P, Pollard J, Sim D, Sullivan R, Sussex J, Lorgelly P. Making outcome-based payment a reality in the NHS. 2019; OHE, RAND Europe, KCL and Cancer Research UK Research Paper. https://www.ohe.org/publications/making-outcome-based-payment-reality-nhs.
Garrison LP, Towse A. Value-based pricing and reimbursement in personalised healthcare: introduction to the basic health economics. J Pers Med. 2017;7:10.
Lakdawalla DN, Doshi JA, Garrison LP, Phelps CE, Basu A, Danzon PM. Defining elements of value in health care—a health economics approach: an ISPOR Special Task Force report [3]. Value Health. 2018;21:131–9.
Krueger RA. Focus groups: a practical guide for applied research. London: Sage Publications; 2014.
Ravens-Sieberer U, Gosch A, Rajmil L, Erhart M, Bruil J, Duer W, et al. KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Rev Pharmacoecon Outcomes Res. 2005;5:353–64.
McMullen S, Hess LM, Kim ES, Levy B, Mohamed M, Waterhouse D, Wozniak A, Goring S, Müller K, Muehlenbein C, Aggarwal H. Treatment decisions for advanced non-squamous non-small cell lung cancer: patient and physician perspectives on maintenance therapy. Patient Patient Centered Outcomes Res. 2019;12(2):223–33.
Crawford R, Sully K, Conroy R, Johnson C, Doward L, Bell T, Welch V, Peloquin F, Gater A. Patient-centered insights on treatment decision making and living with acute myeloid leukemia and other hematologic cancers. Patient Patient Centered Outcomes Res. 2020;13(1):83–102.
Minion LE, Coleman RL, Alvarez RD, et al. Endpoints in clinical trials: what do patients consider important? A survey of the Ovarian Cancer National Alliance. Gynecol Oncol. 2016;140(2):193–8.
Acknowledgements
The authors acknowledge the contributions of patients with cancer and carers to this study, particularly the focus group participants and those who completed the survey. The authors also thank colleagues from Cancer Research UK, Greater Manchester Health and Social Care Partnership, King’s College London, the Office of Health Economics and RAND Europe who contributed to the delivery of this work and members of the project Steering Group. Please refer to the OHE-RAND Research Report https://www.cancerresearchuk.org/sites/default/files/obp_final_report_pdf.pdf for these individuals’ names.
Author information
Authors and Affiliations
Contributions
DS: conceived the study with input from colleagues from Cancer Research UK and Greater Manchester Health and Social Care Partnership; PKL and JS: designed the study, with assistance from AC, PCM and JP. PCM: conducted the literature review, with assistance from AC. PKL: planned and facilitated the focus groups, with assistance from JP. JP: led the survey data collection, assisted by JS, PKL, AC and PCM. PKL: led the drafting of the article, with assistance from JS, JP and PCM. All the authors revised the article and approved the final version.
Corresponding author
Ethics declarations
Ethics
Ethical approval for the study was granted by the Biomedical and Health Sciences, Dentistry, Medicine and Natural and Mathematical Sciences Research Ethics Subcommittees (BDM RESC) at King’s College London, Ref: LRS-17/18-5723.
Funding
This research was funded by the Cancer Policy Research Centre, Cancer Research UK. Cancer Research UK is a registered charity in England and Wales (1089464), Scotland (SC041666) and the Isle of Man (1103).
Conflict of interest
PCM and AC are employees of the Office of Health Economics, a registered charity, which receives funding from a variety of sources, including the Association of the British Pharmaceutical Industry. PKL was an employee of the Office of Health Economics during the project completion. JS and JP as employees of RAND Europe have undertaken contract research for the Association of the British Pharmaceutical industry and have received grant funding from Cancer Research UK. DS is an employee of Cancer Research UK, funders of the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lorgelly, P., Pollard, J., Cubi-Molla, P. et al. Outcome-Based Payment Schemes: What Outcomes Do Patients with Cancer Value?. Patient 13, 599–610 (2020). https://doi.org/10.1007/s40271-020-00430-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-020-00430-x