Abstract
Background
Vupanorsen is a GalNAc3-conjugated antisense oligonucleotide targeting angiopoietin-like 3 (ANGPTL3) mRNA shown to reduce atherogenic lipoproteins in individuals with dyslipidemia.
Objectives
The aim of this study was to satisfy Chinese regulatory requirements and support ethnic sensitivity assessment by evaluating pharmacokinetics (PK), pharmacodynamics (PD), and safety of vupanorsen in healthy Chinese adults with elevated triglycerides (TG).
Methods
In this phase I, parallel-cohort, open-label study, 18 Chinese adults with elevated fasting TG (≥ 90 mg/dL) were randomized 1:1 to receive a single subcutaneous dose of vupanorsen 80 mg or 160 mg. PK parameters, PD markers (including ANGPTL3, TG, non–high-density lipoprotein cholesterol [non–HDL-C]), and safety were assessed.
Results
Absorption of vupanorsen was rapid (median time to maximum concentration [Tmax]: 2.0 h for both doses), followed by a multiphasic decline (mean terminal half-life 475.9 [80 mg] and 465.2 h [160 mg]). Exposure (area under curve [AUC] and maximum plasma concentration [Cmax]) generally increased in a greater than dose-proportional manner from 80 mg to 160 mg. Time-dependent reductions in ANGPTL3 and lipid parameters were observed. Mean percentage change from baseline for the 80-mg and 160-mg doses, respectively, were – 59.7% and – 69.5% for ANGPTL3, – 41.9% and – 52.5% for TG, and – 23.2% and – 25.4% for non–HDL-C. No serious or severe adverse events (AEs), deaths, or discontinuations due to AEs were reported. Three participants experienced treatment-related AEs; all were mild and resolved by end of study.
Conclusions
This study provided the first clinical vupanorsen data in China. In Chinese participants with elevated TG, PK and PD parameters were consistent with those reported previously in non-Chinese participants, including in Japanese individuals. No safety concerns were noted.
Trial Registration
ClinicalTrials.gov identifier: NCT04916795.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Phase I and II studies have previously demonstrated that vupanorsen results in favorable changes in angiopoietin-like 3 (ANGPTL3), triglycerides (TG), and other lipid parameters in different patient populations. |
This phase I, randomized, parallel-cohort, open-label study of Chinese adults with elevated fasting TG (≥ 90 mg/dL) administered subcutaneous vupanorsen (80 mg or 160 mg) was conducted to satisfy regulatory criteria for medication development in China. |
The pharmacokinetic, pharmacodynamic, and safety profiles of vupanorsen detected in Chinese participants were similar to those previously demonstrated in Western and Japanese populations, and these observations satisfied Chinese regulatory requirements. |
1 Introduction
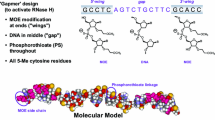
Vupanorsen (also known as PF-07285557, AKCEA-ANGPTL3-LRx, IONIS-ANGPTL3-LRx, ISIS 703802) is a second-generation, tri-N-acetyl galactosamine (GalNAc3)-conjugated 2’O-methoxyethyl antisense oligonucleotide (ASO) that targets angiopoietin-like 3 (ANGPTL3) mRNA [1, 2]. ANGPTL3 protein is an inhibitor of lipoprotein lipase (LPL) and endothelial lipase, which are key enzymes involved in the metabolism of very–low-density lipoprotein (VLDL) and high-density lipoprotein (HDL), respectively [3]. In phase I and II studies in Western populations, subcutaneous (SC) vupanorsen treatment resulted in favorable changes in ANGPTL3, lipids, and lipoprotein profiles, including reductions in triglycerides (TG) and non–high-density lipoprotein cholesterol (non–HDL-C) [4,5,6,7]. The pharmacokinetic (PK) profile of vupanorsen has also been defined in Western and Japanese subjects, with a rapid absorption and distribution phase, and a slow elimination half-life of ~ 3–5 weeks [4, 8, 9]. The PK profile of vupanorsen in these populations is largely consistent with that demonstrated for other GalNAc3-conjugated ASOs (targeting Apo(a), ApoCIII-L, and factor B), which are rapidly absorbed (median time to maximum concentration [Tmax]: ~0.5–5 h) and systemically distributed to target tissues (primarily hepatocytes) [10, 11]. GalNAc3-conjugated ASOs are internalized via asialoglycoprotein receptor-mediated endocytosis resulting in an initial rapid distributional plasma clearance. The ASOs are slowly metabolized by nucleases resulting in an elimination half-life of ~3–5 weeks [10,11,12]. In humans, the exposure (area under curve [AUC] and maximum plasma concentration [Cmax]) of vupanorsen increased approximately dose-proportionally after single-dose administration from 20 to 40 mg, but a greater than dose-proportional increase was observed from 40 to 80 mg and from 80 to 160 mg [4, 9]. Such non-linear PK was also observed for other GalNAc3-conjugated and unconjugated ASOs [10, 13]. However, no previous studies of vupanorsen have been carried out in China.
The Chinese National Medical Products Administration (NMPA) requires that the ethnic differences between Chinese and non-Chinese individuals should be evaluated when considering registration of drugs in China via bridging overseas data [14,15,16]. The current study was designed to investigate the PK, pharmacodynamics (PD), safety, and tolerability of vupanorsen following a single SC 80-mg or 160-mg dose in healthy Chinese adults with elevated TG.
2 Methods
2.1 Study Design
This phase I, randomized, parallel-cohort, open-label study in Chinese adults with elevated fasting TG (≥ 90 mg/dL), but who were otherwise healthy, was conducted between 17 June 2021 and 19 October 2021 at a single site in China (ClinicalTrials.gov identifier: NCT 04916795).
After a ≥ 10-h fast, participants underwent an extended lipid panel test on Day 1 prior to receiving vupanorsen. Enrolled participants were randomized 1:1 to receive a single SC dose of vupanorsen 80 mg or 160 mg. A single-dose design was selected over repeated dosing as the steady-state PK and PD can be predicted from single-dose data [10]. Vupanorsen was administered as an SC injection to the lower quadrant of the abdomen using a pre-filled glass syringe containing 80 mg of study drug. Participants in the vupanorsen 160-mg cohort received two SC injections of vupanorsen 80 mg, which were not administered to the same location on the abdomen.
Following discharge on Day 3, participants returned for an on-site post-treatment evaluation at Days 8, 15, 30, 60, and 90. A total of 90 days was considered the necessary period to allow adequate characterization of the terminal half-life (t½) of vupanorsen.
The study was conducted in compliance with the ethical principles of the Declaration of Helsinki and in compliance with all International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practice Guidelines. In addition, all local regulatory requirements were followed, in particular those affording greater protection to the safety of trial participants. The final protocol, any amendments, and informed consent documentation were reviewed and approved by the Independent Ethics Committee (IEC) at the investigational center. Investigators were required to inform their IEC of the study’s progress and occurrence of any serious and/or unexpected adverse events (AEs).
2.2 Study Participants
Eligible participants were aged 18–65 years and had elevated fasting TG (≥ 90 mg/dL) at screening. Participants were currently residing in mainland China, were born in China, and had both parents of Chinese descent.
Individuals were not eligible if they had evidence of clinically significant hematologic, renal, endocrine, pulmonary, gastrointestinal, cardiovascular, hepatic, psychiatric, neurologic, or allergic disease (including drug allergies, but excluding untreated, asymptomatic, seasonal allergies at the time of dosing), and if they had received any prescription or nonprescription drugs within 7 days or 5 half-lives (whichever was longer) prior to the first dose of study intervention. Participants were also excluded if they had aspartate transaminase (AST) or alanine aminotransferase (ALT) level ≥ 1.25 × upper limit of normal (ULN) or total bilirubin level ≥ 1.5 × ULN.
2.3 Pharmacokinetic Analyses
Blood samples for plasma analysis were collected pre-dose, and then at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 24, and 48 h after dose administration on Day 1. Additional samples were analyzed from follow-up visits on Days 8, 15, 30, 60, and 90. Vupanorsen plasma concentration was measured using a validated electrochemiluminescence method (data on file). PK parameters were determined from plasma concentration–time data using standard noncompartmental methods by an internally validated software system (oNCA version 2.4.33). Vupanorsen plasma PK parameters included overall and dose-normalized AUC, area under the concentration–time curve values (AUC from time 0 to the quantifiable concentration 24 h and 48 h post-dose [AUC24 h and AUC48h], AUC from time 0 to the time of the last quantifiable concentration [AUClast], AUC from time 0 extrapolated to infinite time [AUCinf]), Cmax, Tmax, t½, apparent clearance (CL/F), and apparent volume of distribution (Vz/F).
2.4 Pharmacodynamic Analyses
Blood samples for serum analysis were collected after a ≥ 10-hour fast on Day 1 (pre-dose), Day 2 (24-h post-dose), Day 3 (48-h post-dose), and Days 8, 15, 30, 60, and 90. ANGPTL3 was assessed using a validated enzyme-linked immunosorbent assay (data on file). A lipid panel assessed parameters including TG, low-density lipoprotein cholesterol (LDL-C), HDL-C, very–low-density lipoprotein cholesterol (VLDL-C), non–HDL-C, and total cholesterol.
2.5 Safety Assessments
Safety evaluations included AEs, clinical safety laboratory tests, monitoring vital signs, physical examination, and 12-lead electrocardiogram.
2.6 Statistical Analysis
There was no statistical hypothesis for this study; therefore, the study sample size was chosen based on the need to minimize exposure to humans of a new chemical entity and to fulfill the NMPA requirement for a PK study to support the registration in China. Considering the possibility of participant dropouts/withdrawals, approximately 18 participants (n = 9 per dose group) were required to ensure approximately 16 participants (n = 8 per dose group) were evaluable for the primary endpoint.
PK parameters for vupanorsen following an 80 mg or 160 mg single dose were derived from the concentration–time profiles using standard noncompartmental methods. Actual PK sampling times were used in the derivation of PK parameters. Vupanorsen PK parameters were summarized descriptively for vupanorsen 80 and 160 mg. For dose-normalized AUC and Cmax, box whisker plots for individual participant parameters overlaid with geometric means were generated. Plasma concentrations for vupanorsen were summarized descriptively by dose group and nominal PK sampling time. Median concentration–time plots against nominal sampling time were presented for each vupanorsen dose group. Percentage changes from baseline (%CFB) for PD assessments were summarized for vupanorsen 80 and 160 mg, and nominal sampling time using descriptive statistics.
3 Results
3.1 Participant Characteristics
A total of 18 participants were enrolled and randomized to vupanorsen 80 mg (n = 9) or 160 mg (n = 9) (Table 1). All participants completed the study. The majority of participants were male (n = 15 male vs n = 3 female). The mean ± standard deviation (SD) age of the overall cohort was 33.8 ± 8.0 years, and weight was 70.4 ± 10.6 kg. The mean ± SD body mass index (BMI) was 25.5 ± 3.0 kg/m2 (range 19–29), including six participants in normal range and 12 participants in the overweight range. All participants who received vupanorsen contributed to the PK, PD, and safety analyses.
3.2 Pharmacokinetic Analysis
Absorption of vupanorsen into the systemic circulation following single SC dose of 80 or 160 mg was rapid, with a median Tmax of 2.0 h for both doses (Table 2). Following attainment of Cmax, vupanorsen showed a multiphasic decline characterized by a relatively fast initial distribution phase followed by a slower terminal elimination phase, with mean t½ values of 475.9 h and 465.2 h in the 80-mg and 160-mg dose groups, respectively (Fig. 1).
Median plasma vupanorsen concentration–time profiles from 0 to 48 h post-dose following a single subcutaneous dose of vupanorsen (80 or 160 mg). a Linear scale. b Semi-log scale. Concentration values below the lower limit of quantification have been set to 0. The lower limit of quantification is 0.130 ng/mL
Mean CL/F was 19.6 L/h and 13.4 L/h, and the mean Vz/F was 12,500 L and 8681 L for the 80- and 160-mg doses, respectively. In general, both AUCinf and Cmax appeared to increase in a greater than dose-proportional manner from 80 mg to 160 mg. The inter-participant variability (geometric coefficient of variation) for AUCinf and Cmax was 36–39% and 62–63%, respectively (Table 2). Individual and geometric mean dose-normalized AUCinf and Cmax are given by dose in Fig. 2.
Individual and geometric mean plasma vupanorsen dose-normalized a AUCinf and b Cmax following a single subcutaneous dose of vupanorsen (80 or 160 mg). Dose normalized to a 1-mg dose. Stars represent geometric mean values and circles represent individual participant values. Box plot provides median and 25%/75% quartiles with whiskers to the last point within 1.5 × interquartile range. AUCinf area under the plasma concentration–time profile from time 0 extrapolated to infinite time, Cmax maximum plasma concentration
3.3 Pharmacodynamic Analysis
3.3.1 Change in ANGPTL3
Time-dependent reductions in mean ANGPTL3 were seen following single-dose SC vupanorsen 80 mg or 160 mg, before returning toward baseline values (Fig. 3A and Supplementary Table 1, see electronic supplementary material [ESM]). The maximal %CFB (mean ± SD) was observed on Day 8 in the vupanorsen 80-mg arm (– 59.7 ± 18.7%) and Day 15 in the vupanorsen 160-mg arm (– 69.5 ± 11.7%).
Mean (± SD) %CFB in a ANGPLT3, b triglycerides, c non–HDL-C, d LDL-C, e HDL-C, and f cholesterol over time, and g VLDL-c, following a single subcutaneous administration of vupanorsen (80 or 160 mg). Baseline is defined as the measurements collected on Day 1 prior to dosing or last pre-dose measurement. %CFB percentage change from baseline, ANGPTL3 angiopoietin-like 3, HDL-C high-density lipoprotein cholesterol, LDL-C low-density lipoprotein cholesterol, SD standard deviation
3.3.2 Changes in Lipid Parameters
Time-dependent reductions in mean key lipid parameters were observed following administration of SC vupanorsen 80 mg or 160 mg before returning toward baseline values (Fig. 3 and Supplementary Table 1, see ESM). Maximal %CFB (mean ± SD) in TG was seen on Day 15 (– 41.9 ± 20.0%) in the vupanorsen 80-mg arm and Day 8 (– 52.5 ± 18.2%) in the vupanorsen 160-mg arm (Fig. 3B). For non–HDL-C, maximal %CFB (mean ± SD) was observed on Day 15 in both the vupanorsen 80-mg arm (– 23.2 ± 15.2%) and 160-mg arm (– 25.4 ± 11.2%) (Fig. 3C). Mean time-dependent reductions were also observed in other lipid parameters including cholesterol, HDL-C, LDL-C, and VLDL-C (Fig. 3E–G).
3.4 Safety Summary
No deaths, or serious or severe AEs were reported in either vupanorsen dose group, and there were no discontinuations from the study due to AEs. In the vupanorsen 80-mg treatment arm (n = 9), three (33.0%) participants experienced 10 AEs, of which three (reported in two participants [22.2%]) were considered treatment-related. One participant experienced increased ALT (> 3 × ULN) and AST (< 3 × ULN), and one participant experienced an increase in ALT (< 3 × ULN). All treatment-related AEs were mild in severity and resolved by the end of the study. In the vupanorsen 160-mg treatment arm (n = 9), five (55.6%) participants experienced 11 AEs, and one AE was considered treatment-related. One participant experienced musculoskeletal pain, which was mild in severity and resolved by the end of the study. No AEs of increased ALT or AST were reported in the vupanorsen 160-mg arm. There were no clinically significant changes in vital signs or electrocardiogram results.
4 Discussion
To satisfy Chinese NMPA requirements, this phase I, open-label study was conducted in healthy Chinese adults with elevated fasting TG, and it demonstrated that single-dose SC vupanorsen (80 and 160 mg) had a PK profile typical of GalNAc3-conjugated ASOs [10, 12], and provided time-dependent reductions in mean ANGPTL3 and lipid parameters including TG, non–HDL-C, LDL-C, VLDL-C, and HDL-C. Single-dose vupanorsen 80 mg or 160 mg was also well tolerated in these Chinese individuals with elevated fasting TG, with AEs similar to those reported in non-Chinese individuals [4, 9].
The PK of single-dose vupanorsen has been previously characterized in non-Chinese individuals [4, 9], and this is the first study to provide the PK, PD, and safety data of vupanorsen in participants from China as part of NMPA requirements, and to support ethnic sensitivity comparisons with other populations. In the present study, absorption of vupanorsen was rapid, with a multiphasic decline characterized by a fast initial distribution phase followed by a slower terminal elimination phase. This profile is characteristic of vupanorsen and is similar to that seen in previous phase I studies in non-Chinese individuals [4, 9]. Vupanorsen exposure (AUCinf and Cmax) increased in a greater than dose-proportional manner from 80 mg to 160 mg, which may be due to partial saturation of hepatic uptake of vupanorsen via the asialoglycoprotein receptor, and/or inherent PK variability as a consequence of the limited number of participants in this study. Similar observations have been noted in healthy Japanese adults with elevated TG (≥ 90 mg/dL at screening) and Western adults with elevated TG (between 90 and 150 mg/dL at screening), where vupanorsen exposure also increased in a greater than dose-proportional manner across the single dose 80–160 mg range and 40–80 mg range, respectively [4, 9].
The dose-normalized PK profiles in Asian adults (Chinese [current study] and Japanese [9]) were generally comparable with those observed from a previous phase I trial in healthy Western adults [4]. The distribution ranges of individual dose-normalized PK parameters (including dose-normalized Cmax and AUC24) in Asian and Western adults were generally overlapping, despite Asian adults displaying a mean dose-normalized Cmax approximately two-fold higher than Western adults (single ascending dose cohort and Day 1 of multiple ascending dose cohort) [4, 9]. The apparent difference in mean dose-normalized Cmax in Asian and non-Asian individuals is possibly due to the small sample sizes (N = 9 in this Chinese study, N = 6 in the Japanese study, and N = 36 in the Western study [4, 9]), and/or due to variation in the sample population such as differences in body weight (mean ± SD) between Chinese (70.0 ± 11.0 kg), Japanese (63.8 ± 2.1 kg), and Western (81.8 ± 10.1 kg) adults [4, 9]. Other characteristics of participants across Chinese, Japanese, and Western studies are generally comparable, with participants aged 24–49, 26–61, and 28–65 years, respectively [4, 9], the majority of which are male (n = 7 male vs n = 2 female in this Chinese study; n = 6 males in the Japanese study; and n = 31 male vs n = 5 female in the Western study) [4, 9].
Time-dependent reductions in ANGPTL3 from baseline (%CFB) to Day 15 for 80 mg and 160 mg, respectively, (– 59.7% and – 69.5%), TG (– 41.9% and – 52.5%), and non–HDL-C (− 23.2% and − 25.4%) were in line with those observed in Japanese participants with elevated TG following single-dose vupanorsen (80–160 mg) [9], and also with healthy Western participants (single-dose vupanorsen 80–120 mg) [4]. These observations also help confirm similar PD of vupanorsen regardless of ethnic origin of the study population.
As a drug class, GalNAc3-conjugated ASOs are known to have a consistent absorption, distribution, metabolism, and excretion profile [10]. Factors that may cause ethnic differences in drug PK, such as uptake and efflux transporters, oxidative metabolism, and conjugation, are not thought to be involved in the disposition of ASOs [10, 17]. The similarity of vupanorsen PK profiles between Asian and Western populations demonstrated in the present study supports that there are limited racial or ethnic differences for vupanorsen. Therefore, it may be concluded that there is a limited need for specific studies to determine ethnic differences for ASOs such as vupanorsen, given their known and predictable PK properties, combined with the lack of known factors that may impact ethnic sensitivity. For example, although the elimination half-life of ASOs is generally in weeks rather than days, as demonstrated for vupanorsen in this study and other phase I studies showing a t½ of ~2–5 weeks [4, 9], ASOs do not interact with cytochrome p450 enzymes and ASOs do not bind to drug-binding sites on albumin, and therefore, show limited potential for drug–drug interactions [12]. Thus, metabolism and excretion profiles are relatively consistent across the class [12]. Given these properties, international regulators should consider the need for future ethnic-specific studies with ASOs and consider accepting existing data from other ethnic populations in order to accelerate early clinical development.
Our study should be considered in light of certain limitations, including the limited sample size of 18 participants and the single-dose design. However, our data add to the totality of PK, PD, and safety data together with that from Western and Japanese studies [4, 9], and the predictable PK profile of GalNAc3-ASOs [10] suggests there is no evidence of a clinically significant ethnic difference in PK and PD for vupanorsen. Also, this trial was not placebo-controlled; however, this is of limited concern for the PK findings given that these are objective endpoints. Following review of results from the TRANSLATE-TIMI 70 study in statin-treated participants with dyslipidemia, the vupanorsen development program was discontinued based on the magnitude of non–HDL-C lowering achieved [6]. If global development had continued, the present study would have informed clinical development of vupanorsen in China, facilitating China’s participation in global pivotal studies and providing the necessary evidence to satisfy Chinese NMPA regulatory requirements.
5 Conclusions
This phase I study in Chinese participants with elevated TG demonstrated vupanorsen PK and PD parameters were consistent with those previously reported in non-Chinese populations, and no new safety concerns were noted in these Chinese participants. This study provided the first clinical vupanorsen data from China and satisfied Chinese regulatory requirements to evaluate any ethnic differences between Chinese participants and existing data from non-Chinese populations.
References
Prakash TP, Graham MJ, Yu J, et al. Targeted delivery of antisense oligonucleotides to hepatocytes using triantennary N-acetyl galactosamine improves potency 10-fold in mice. Nucleic Acids Res. 2014;42(13):8796–807. https://doi.org/10.1093/nar/gku531.
Insight Adis. Vupanorsen - Ionis Pharmaceuticals/Pfizer. Updated 18 Feb 2022. https://adisinsight.springer.com/drugs/800049006 Accessed 23 Feb 2022.
Kersten S. Angiopoietin-like 3 in lipoprotein metabolism. Nat Rev Endocrinol. 2017;13(12):731–9. https://doi.org/10.1038/nrendo.2017.119.
Graham MJ, Lee RG, Brandt TA, et al. Cardiovascular and metabolic effects of ANGPTL3 antisense oligonucleotides. N Engl J Med. 2017;377(3):222–32. https://doi.org/10.1056/NEJMoa1701329.
Gaudet D, Karwatowska-Prokopczuk E, Baum SJ, et al. Vupanorsen, an N-acetyl galactosamine-conjugated antisense drug to ANGPTL3 mRNA, lowers triglycerides and atherogenic lipoproteins in patients with diabetes, hepatic steatosis, and hypertriglyceridaemia. Eur Heart J. 2020;41(40):3936–45. https://doi.org/10.1093/eurheartj/ehaa689.
Bergmark BA, Marston NA, Bramson CR, et al. Effect of vupanorsen on non-high-density lipoprotein cholesterol levels in statin-treated patients with elevated cholesterol: TRANSLATE-TIMI 70. Circulation. 2022;145(18):1377–86. https://doi.org/10.1161/circulationaha.122.059266.
Foss-Freitas MC, Akinci B, Neidert A, et al. Selective targeting of angiopoietin-like 3 (ANGPTL3) with vupanorsen for the treatment of patients with familial partial lipodystrophy (FPLD): results of a proof-of-concept study. Lipids Health Dis. 2021;20(1):174. https://doi.org/10.1186/s12944-021-01589-4.
Lai Y, Chu X, Di L, et al. Recent advances in the translation of drug metabolism and pharmacokinetics science for drug discovery and development. Acta Pharm Sin B. 2022;12(6):2751–77. https://doi.org/10.1016/j.apsb.2022.03.009.
Fukuhara K, Furihata K, Matsuoka N, et al. A multi-purpose Japanese phase I study in the global development of vupanorsen: Randomized, placebo-controlled, single-ascending dose study in adults. Clin Transl Sci. 2023;16(5):886–97. https://doi.org/10.1111/cts.13498.
Wang Y, Yu RZ, Henry S, et al. Pharmacokinetics and clinical pharmacology considerations of GalNAc3-conjugated antisense oligonucleotides. Expert Opin Drug Metab Toxicol. 2019;15(6):475–85. https://doi.org/10.1080/17425255.2019.1621838.
Cui H, Zhu X, Li S, et al. Liver-targeted delivery of oligonucleotides with N-acetylgalactosamine conjugation. ACS Omega. 2021;6(25):16259–65. https://doi.org/10.1021/acsomega.1c01755.
Crooke ST, Baker BF, Xia S, et al. Integrated assessment of the clinical performance of GalNAc3-conjugated 2’-O-methoxyethyl chimeric antisense oligonucleotides: I. Human volunteer experience. Nucleic Acid Ther. 2019;29(1):16–32. https://doi.org/10.1089/nat.2018.0753.
Han K, Ito H, Elston R, et al. Comparison of pharmacokinetics of the GalNAc-conjugated antisense oligonucleotide GSK3389404 in participants with chronic hepatitis B infection across the Asia-Pacific Region. Antimicrob Agents Chemother. 2023;67(1): e0090022. https://doi.org/10.1128/aac.00900-22.
National Medical Products Administration. Main responsibilities of the National Medical Products Administration. 2022 http://english.nmpa.gov.cn/2019-07/18/c_377587.htm Accessed 27 July 2022.
National Medical Products Administration. Clinical technical requirements for drugs marketed overseas but not marketed in China. 2020 http://english.nmpa.gov.cn/2020-11/18/c_568155.htm Accessed 27 July 2022.
Tang W, Huang Y, Zhou D, et al. Evolving drug regulatory landscape in China: a clinical pharmacology perspective. Clin Transl Sci. 2021;14(4):1222–30. https://doi.org/10.1111/cts.12987.
Geary RS. Antisense oligonucleotide pharmacokinetics and metabolism. Expert Opin Drug Metab Toxicol. 2009;5(4):381–91. https://doi.org/10.1517/17425250902877680.
Acknowledgements
The authors thank all individuals who participated in this study. Medical writing support was provided by Jake Evans, PhD, and Karen Burrows, MPhil, of Engage Scientific Solutions (Horsham UK) and was funded by Pfizer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Pfizer.
Conflicts of Interest
XW, JY, and XM are employees of Huashan Hospital, Fudan University, Shanghai, China. No honorarium was paid for this study. BG, XH, CZ, HK, CB, SGT, and JL are employees of Pfizer and may own stock or stock options. JW was a full-time employee of Pfizer at the time of the manuscript development and may own stock or options.
Ethics Approval
The study was conducted in compliance with the ethical principles of the Declaration of Helsinki and in compliance with all International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use Good Clinical Practice Guidelines. In addition, all local regulatory requirements were followed, in particular those affording greater protection to the safety of trial participants. The final protocol, any amendments, and informed consent documentation were reviewed and approved by the Independent Ethics Committee (IEC) at the investigational center (HIRB approval 2021-070). Investigators were required to inform their IEC of the study’s progress and occurrence of any serious and/or unexpected adverse events.
Consent to Participate
All participants gave written informed consent prior to initiation of the study.
Availability of data and material
Upon request, and subject to review, Pfizer will provide the data that support the findings of this study. Subject to certain criteria, conditions, and exceptions, Pfizer may also provide access to the related individual de-identified participant data. See https://www.pfizer.com/science/clinical-trials/trial-data-and-results for more information.
Author Contributions
All authors contributed to the analysis, design, and implementation of the study. All authors contributed to the analysis of the results and critically reviewed and approved the manuscript for submission.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wu, X., Yu, J., Ge, B. et al. A Randomized, Open-Label, Phase I, Single-Dose Study of Antisense Oligonucleotide, Vupanorsen, in Chinese Adults with Elevated Triglycerides. Drugs R D (2024). https://doi.org/10.1007/s40268-024-00467-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s40268-024-00467-5