Abstract
Background and Objective
Oral linezolid is often used as alternative therapy for intravenous vancomycin. According to the current guidelines, no dose adjustment has to be made in case of renal impairment. Nevertheless, in our hospital we have seen several patients with renal impairment who developed linezolid-induced thrombocytopenia when linezolid was taken in the standard dose. In this case series and review we want to emphasize the necessity of reviewing the Dutch and international guidelines.
Methods
We describe five cases with renal impairment that developed linezolid-induced thrombocytopenia in our hospital. A PubMed literature review was conducted to identify other cases and find the optimal dosing regimen for these patients.
Results
Our cases join a long list of cases and available literature about linezolid-induced thrombocytopenia in patients with renal impairment. Less linezolid-induced thrombocytopenia was found, both in our cases and in the literature, after dose reduction of 50%. High linezolid trough concentrations were associated with a higher risk of linezolid-induced thrombocytopenia. Besides renal impairment, other risk factors for developing linezolid-induced thrombocytopenia were also identified, such as low body weight, high daily dose/kg, higher age, longer duration of therapy, low baseline count, malignity, low-dose aspirin and interacting co-medication.
Conclusion
Re-evaluation of the current dose advice is necessary. We advocate for a standard dose reduction to 50% after 2 days of standard dosing for all patients with an estimated glomerular filtration of <60 mL/min/1.73 m2. Besides this, therapeutic drug monitoring and thrombocytes monitoring may be executed weekly when patients have renal impairment or other risk factors for developing linezolid-induced thrombocytopenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Several patients with renal impairment have developed linezolid-induced thrombocytopenia. |
Standard dose reduction to 50% after 2 days of linezolid treatment may be advised. |
Monitoring of thrombocyte levels and linezolid trough concentrations weekly may be recommended. |
1 Introduction
Linezolid is a synthetic antibacterial agent from the class of oxazolidinones. It is effective against most Gram-positive bacteria including methicillin-resistant Staphylococcus aureus, penicillin-resistant Streptococcus pneumoniae and vancomycin-resistant enterococcus (VRE). It is used to treat infections like pneumonia, skin infections and (off-label) periprosthetic infections. Linezolid has a unique mechanism of action; it binds to the bacterial 50S ribosomal subunit and prevents the formation of the 70S subunit complex, which results in the inhibition of protein synthesis. Its effect is time-dependent and in general bacteriostatic, but in most streptococci bactericidal [1].
After oral administration, the bioavailability of linezolid is approximately 100%. The volume of distribution is approximately 0.5 L/kg. It is metabolized both enzymatically and nonenzymatically into several metabolites. The two major metabolites are aminoethoxyacetic acid (PNU-142300) and hydroxyethyl glycine (PNU-142586). Both metabolites have no antibacterial activity. The major route of elimination is glomerular filtration. At steady state the mean recovery in excreta is about 94%, of which 30% is unchanged in the urine, 55% as metabolites in the urine and 9% in the faeces [2].
Because of its good bioavailability and effectiveness against VRE, oral linezolid is often used as an oral alternative for intravenous targeted vancomycin therapy. Especially for patients who no longer have an indication for hospitalization, changing to oral linezolid therapy is a way to discharge patients earlier. Additionally, oral linezolid therapy is cheaper because a central venous catheter does not need to be inserted and no home care organisation is required to administer the intravenous therapy.
A common side effect of linezolid is myelosuppression and linezolid-induced thrombocytopenia (LIT), defined as a thrombocyte count of <150*109/L. The mechanism remains unclear, but it could possibly be immune-mediated, or a result of drug-induced bone marrow suppression [3]. LIT is often dose dependent and generally occurs after 2 or 3 weeks of treatment. This means that theoretically the side effect can be prevented by monitoring thrombocytes and linezolid trough concentrations [4]. Patients treated with linezolid at home are at risk for these side effects when there is no frequent monitoring.
Several studies have shown a correlation between LIT and renal impairment in patients treated with linezolid [5,6,7,8,9,10,11]. Despite this, the current guidelines still advise to maintain the standard linezolid dose (600 mg twice daily) in case of renal impairment [25]. Over the last 3 years we have encountered several suspected cases of LIT in patients with renal impairment, who are described in this paper. In addition, we performed a review of the current literature regarding this condition in order to find a safe and effective dose for linezolid in patients with renal impairment, to support our advocacy for reviewing the current Dutch and international guidelines.
2 Case Reports
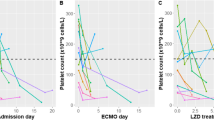
Over the years 2019–2022, we treated 37 patients for >4 days with linezolid in our hospital. From these patients, 12 had renal impairment, defined as estimated glomerular filtration (eGFR) (Chronic Kidney Disease – Epidemiology Collaboration [CKD-EPI] equation) <50 mL/min/1.73 m2. Five of them (42%) developed thrombocytopenia after start of linezolid therapy. In comparison, only 20% of the patients with a normal renal function developed thrombocytopenia during linezolid treatment. All five patients were classified with a Naranjo score between 5 and 8, which means that the causality of the adverse reaction is considered ‘probable’. The key characteristics of each case are described in Table 1. Relevant comedication can be found in Table 3. Samples for linezolid trough concentrations were all drawn within 2 h before the next dose.
2.1 Case 1
Case 1 is a 76-year-old man with a history of diabetes mellitus type 1 and renal impairment with an eGFR (CKD-EPI) of 30 mL/min/1.73 m2. He was re-admitted to the hospital because of a wound infection after osteosynthesis for a lower leg fracture. Enterococcus faecium was cultured and vancomycin IV was started. After 11 days, at discharge, vancomycin was switched to oral linezolid 600 mg twice daily. The thrombocyte count was 450*109/L at the day of discharge. At day 20 after the start of linezolid, the thrombocyte count had dropped to 63*109/L. Six days later he was suffering a severe nose bleeding that required blood transfusion. The linezolid trough concentration was 26.6 mg/L and linezolid was stopped. At day 30 the thrombocytes dropped to 46*109/L and recovered to 160*109/L 4 days later.
2.2 Case 2
Case 2 is a 59-year-old woman with a history of diabetes type 1, renal impairment, haemodialysis and a kidney transplant in 2009 with an eGFR (CKD-EPI) of ±30 mL/min/1.73 m2. She was admitted to the hospital because of a persistent septic arthritis of the knee. Arthroscopic debridement of the knee followed, and ceftriaxone was started as initial broad spectrum antibiotic treatment. Bacterial cultures showed a Corynebacterium striatum and vancomycin IV was started. After 2 weeks vancomycin was replaced by oral linezolid 600 mg twice daily. Three days after the start of linezolid, the linezolid trough concentration was 25.4 mg/L, which led to a dose reduction to 600 mg once daily on day 10. On day 15 the thrombocyte count dropped from a baseline of 400*109/L at the beginning of the linezolid therapy to 120*109/L and it was decided to cease the linezolid. Thrombocytes recovered to 340*109/L within 3 weeks.
2.3 Case 3
Case 3 is a 65-year-old woman with diabetes mellitus type 2, a pertrochanteric femur fracture, treated with an intramedullary nail, and renal impairment with an eGFR (CKD-EPI) of about 50 mL/min/1.73 m2. She was admitted because of a cut out of the intramedullary osteosynthesis land necrosis of the femoral head. The fixation nail was removed and a Corynebacterium striatum, Proteus mirabilis and Staphylococcus epidermis were cultured. Vancomycin IV and cefuroxime IV were started. After 3 weeks of treatment, this therapy was replaced by oral ciprofloxacin 750 mg and oral linezolid 600 mg, both twice daily. At baseline the thrombocyte count was 300*109/L. Linezolid was continued for 2 weeks, during which time the renal function remained stable and thrombocytes and linezolid trough concentrations were not measured. Because of blurry vision, a suspected adverse event of linezolid, the linezolid was replaced with vancomycin IV for 11 days. The adverse event was not confirmed, and vancomycin was switched back to linezolid. The renal function remained stable, and the thrombocyte count was 380*109/L. At day 12 after the restart, the linezolid trough concentration was 14.6 mg/L. At day 16 the thrombocytes had reduced to 89*109/L, which resulted in linezolid therapy cessation one day later. Thrombocytes further decreased to 53*109/L at day 24 but recovered to 260*109/L at day 35. Renal function remained stable during the antibiotic treatment. A hip prosthesis was never implanted because of mental and physical impairments.
2.4 Case 4
Case 4 is a 49-year-old man with a history of diabetes type 2, hypertension and autosomal dominant polycystic kidney disease leading to terminal renal failure treated with haemodialysis. He was admitted to the hospital because of infected liver cysts. In blood cultures an Enterococcus faecium was found. He was initially treated with vancomycin IV and at discharge switched to oral linezolid 600 mg twice daily. Trough concentrations were monitored before dialysis and were 7.1 and 15 mg/L at day 6 and 11, respectively, after the switch to linezolid. Based on the last trough concentration, the dose was reduced to 600 mg once daily. This resulted in a trough concentration of 5.2 mg/L at day 18. At day 20, he was admitted to the hospital again with cold shivers and a Campylobacter was found in the blood cultures. The linezolid was stopped, and vancomycin was started. His thrombocyte level had dropped from a baseline of 200*109/L to 85*109/L at day 21. At day 25 the thrombocytes recovered to 220*109/L.
2.5 Case 5
Case 5 is a 76-year-old woman with hypertension and an eGFR (CKD-EPI) of about 50 mL/min/1.73 m2. She was admitted to the hospital because of a periprosthetic hip joint infection. The hip prosthesis was explanted. A Staphylococcus epidermidis was cultured and treated with vancomycin IV for 10 days. Vancomycin was stopped and linezolid 600 mg twice daily was started orally. Linezolid trough concentration at day 5 after the switch to linezolid was 7.5 mg/L, after which the linezolid dose was reduced to 600 mg once daily on day 8. Her eGFR (CKD-EPI) had dropped to 40 mL/min/1.73 m2 at day 7 and linezolid was stopped at day 12. At day 13 the thrombocytes dropped from a baseline of 180*10^9/L to 86*10^9/L. Thrombocytes and renal function recovered at day 20 to 160*109/L and 50 mL/min/1.73 m2, respectively. Treatment was continued with vancomycin IV. The total hip was re-implanted successfully after 2 months.
3 Discussion
In this cases series, we have described five cases of patients with impaired renal function who probably developed LIT. Also, a high linezolid trough concentration (above the therapeutic range of 2–8 mg/L) was measured in four of these patients. Our cases substantiate the list of already published cases (Table 2). Overall, in the current literature, LIT is described in 42.9–78.6% of patients with renal impairment compared with 5.6–42.9% in patients with a normal renal function [12,13,14,15,16,17,18,19,20,21,22]. As the definition of renal impairment is described differently through the literature, a direct comparison is not possible.
The manufacturer of linezolid advises not to reduce the dose in case of renal impairment. This advice is based on studies showing no difference between the area under the concentration–time curve (AUC) of linezolid in patients with a normal renal function and with renal impairment. Exposure to the two main linezolid metabolites was reported to be higher (10-fold), but not included in the dose advice, as the clinical relevance was not clear. Nevertheless, it does warn to be cautious when the eGFR is <30 mL/min [24]. The dose advice is similar to the manufacturers’ and based on the manufacturers’ advice and only one small study [25]. In this small, single-dose pharmacokinetics study, no different linezolid clearance was found in patients with renal impairment compared with healthy patients with CLCR >80 mL/min. Moreover, toxicity and longer exposure to linezolid were not monitored, so possible accumulation of linezolid was not studied. It is remarkable that despite the many reports of LIT and available literature, the dosing advice for patients with renal impairment has remained the same.
Even though the higher blood concentrations of the two main metabolites (PNU-142300 and PNU-142586) have been considered irrelevant, it could be a possible explanation for linezolid toxicity in patients with renal impairment. The metabolite concentrations were 3.3- and 2.8-fold higher in patients with renal impairment (eGFR <60 mL/min/1.73 m2) than in patients without renal impairment, respectively [26]. And a 7- to 8-fold increase in exposure to the two metabolites was found in patients with severe renal impairment <30 mL/min [27]. As no other specific studies are available about the toxicity of the two metabolites, further research is needed to investigate the involvement of the metabolites.
Our cases show that in daily practice, when a patient shows symptoms of LIT, linezolid is often stopped, with the thrombocyte level subsequently recovering in approximately 7 days. This could be explained by the lifetime of a thrombocyte, which is about 8 days. A dose reduction of 50% after the occurrence of thrombocytopenia has resulted in recovery of the thrombocyte count and adequate infection treatment [9, 11]. An early dose reduction may avoid adverse events and unnecessary treatment withdrawal of linezolid in patients with renal impairment. Patient-specific dose advice is needed.
In four of our cases, high linezolid trough concentrations (>10 mg/L) were measured. Linezolid trough concentrations of >7.5–8.2 mg/L are associated with a higher risk of developing LIT [4, 28,29,30,31,32]. These findings suggest that linezolid exposure in patients with renal impairment is higher and a dose adjustment is justified. In simulations, an initial fixed dose of linezolid 600 mg twice daily for 2 days followed by 300 mg twice daily leads to an effective therapeutic concentration with the optimal balance of safety and efficacy in a patient with a clearance of 60 mL/min [18]. This study was conducted in an Asian population, so differences with the Caucasian population should be taken into consideration. The maximized attainment of therapeutic trough concentrations in Caucasian patients with renal impairment has been identified with Monte Carlo simulations. For patients with an eGFR <30 mL/min, the probability for linezolid trough concentrations to be within the therapeutic range (2–8 mg/L) is 33% for 600 mg twice daily, 64% when dosed at 300 mg twice daily and 55% when dosed at 600 mg once daily. At a dose of 600 mg twice daily, 65% of these patients have a probability for linezolid trough concentrations to be above this range. For 300 mg twice daily, this is 26% and for 600 mg once daily, 13%. Both dose reductions in patients with eGFR <30 mL/min result in a probability of attaining linezolid trough concentrations within the therapeutic range that is comparable to the dose of 600 mg twice daily in patients with an eGFR >90 mL/min (60% probability of attaining linezolid trough concentrations within the therapeutic range and 19% probability to be above this range) [12]. Moreover, a formula has been proposed to calculate the required dose to achieve the target trough concentration based on the renal function: initial daily dose (mg/day) = CL × AUC24= (0.0258 × CLCr + 2.03) × (18.2 × Cmin + 134.4), based on a target AUC24 of 200 µg*h/mL [4]. Also, in patients undergoing haemodialysis, a dose reduction to 300 mg twice daily or 600 mg once daily has led to a linezolid trough concentration just before haemodialysis of 20.6 mg/L and 6.0 mg/L, respectively. Compared with a standard dose of 600 mg twice daily, less LIT was seen in this population [33]. This suggests that a dose reduction to 600 mg once daily is also appropriate in haemodialysis patients.
It is remarkable that in 21% of the patients with good renal function, no trough concentration >2 mg/L is reached with 600 mg twice daily [12], and that a creatinine clearance >100 mL/min is associated with linezolid underexposure [34, 35]. Also, in the case of Tsuji et al. [9], the patient developed LIT despite having a 50% dose reduction from start of treatment. Pea et al. [35] found a strong and significant association between high linezolid trough concentrations and renal clearance <40 mL/min, but no significant linear correlation between linezolid trough concentrations and renal function in general [35]. This suggests that high linezolid trough concentrations can only partially be explained by renal impairment and that there are several other risk factors that contribute to a large inter-individual variability [36]. Identified risk factors are low body weight of <60 kg [21], daily dose >18.75–22 mg/kg [21, 22], age >75 years [37], duration of therapy >7–14 days [20, 21, 38], baseline platelet count <150–200 *103/mm3 [22, 38], malignity [37], low-dose aspirin [38] and concomitant use of interacting medication like caspofungin or levofloxacin (higher linezolid trough concentrations) [21]. Remarkably, all of our described cases had used linezolid for >7 days, suggesting accumulation plays an important role in the development of LIT in patients with renal impairment. An overview of all the risk factors that applied to our cases can be found in Tables 1 and 3.
Several studies have shown therapeutic drug monitoring (TDM) to be a useful tool to monitor the linezolid trough concentrations and to prevent LIT [9, 12, 17, 18, 39]. Especially for patients with multiple risk factors, additional TDM next to a standard dose reduction in case of renal impairment may contribute to the prevention of high linezolid blood levels.
Currently, linezolid is only available as a 2 mg/mL infusion fluid and as a 600 mg tablet in the Netherlands. The tablet has no score line to split into equal doses, hence it can only be administered in the reduced dose of 600 mg once daily. The infusion fluid (2 mg/mL) can also be taken orally, but because of the low concentration, a large volume has to be taken. Besides this, the infusion fluid contains a lot of glucose (45.7 mg/mL), which could cause stomach problems. To be able to optimize dosing by TDM, doses smaller than 600 mg are needed, which makes it necessary to develop an alternative dose or dosage form. This can be done by a specialized pharmacy.
4 Conclusion
The large amount of available literature describing LIT in patients with renal impairment, and studies about the optimal linezolid dose in these patients, make it necessary to re-evaluate the current dosing advice. A dose reduction to 600 mg/day in patients with eGFR <60 mL/min/1.73 m2 (also in haemodialysis patients), after 2 days of standard dosing, may lead to effective trough concentrations with less LIT, but further research is necessary to confirm this. In addition, we also advocate for TDM and thrombocytes monitoring 1 week after therapy initiation, followed by monitoring of both parameters weekly, in all patients with renal impairment or other risk factors such as low body weight, high daily dose/kg, higher age, longer duration of therapy, low baseline count, malignity, low-dose aspirin and interacting co-medication. In order to optimally implement TDM-based dosing, a suitable smaller dosage form should be available. Further prospective studies should be encouraged to determine the effects of dosing according to TDM on the occurrence of LIT in the real population and to determine the toxicity of the two main metabolites.
References
Swaney SM, Aoki H, Ganoza MC, Shinabarger DL. The oxazolidinone linezolid inhibits initiation of protein synthesis in bacteria. Antimicrob Agents Chemother. 1998;42(12):3251–5. https://doi.org/10.1128/AAC.42.12.3251.
Slatter J, et al. Pharmacokinetics, metabolism, and excretion of linezolid following an oral dose of [14 C]linezolid to healthy human subjects. Am Soc Pharmacol Exp Ther. 2001;29(8):1136–45.
Bernstein WB, Trotta RF, Rector JT, Tjaden JA, Barile AJ. Mechanisms for linezolid-induced anemia and thrombocytopenia. Ann Pharmacother. 2003;37(4):517–20. https://doi.org/10.1345/aph.1C361.
Matsumoto K, et al. Analysis of thrombocytopenic effects and population pharmacokinetics of linezolid: a dosage strategy according to the trough concentration target and renal function in adult patients. Int J Antimicrob Agents. 2014;44(3):242–7. https://doi.org/10.1016/j.ijantimicag.2014.05.010.
Cossu AP, Musu M, Mura P, De Giudici LM, Finco G. Linezolid-induced thrombocytopenia in impaired renal function: Is it time for a dose adjustment? A case report and review of literature. Eur J Clin Pharmacol. 2014;70(1):23–8. https://doi.org/10.1007/s00228-013-1585-6.
Lam S. Linezolid-associated thrombocytopenia. Consult Pharm. 2012;27(7):504–8. https://doi.org/10.4140/TCP.n.2012.504.
Esposito L, Kamar N, Guilbeau-Frugier C, Mehrenberger M, Modesto A, Rostaing L. Linezolid-induced interstitial nephritis in a kidney-transplant patient. Clin Nephrol. 2007;68(11):327–9. https://doi.org/10.5414/CNP68327.
Navarroza RV, Zamora LD, Navarra SV. Serotonin syndrome masquerading as disease flare in lupus nephritis with end-stage renal disease. Int J Rheum Dis. 2019;22(10):1933–6. https://doi.org/10.1111/1756-185X.13683.
Tsuji Y, et al. Treatment of mediastinitis due to methicillin-resistant staphylococcus aureus in a renal dysfunction patient undergoing adjustments to the linezolid dose. Intern Med. 2015;54(2):235–9. https://doi.org/10.2169/internalmedicine.54.2292.
Berenguer N, Ferrández O, Barbosa F, Urbina O, Espona M, Grau S. Long-term treatment with linezolid in a patient with osteomyelitis undergoing hemodialysis. J Chemother. 2012;24(4):226–8. https://doi.org/10.1179/1973947812Y.0000000014.
Taguchi K, et al. A reduced linezolid dosage maintains favorable efficacy with minimal hematologic toxicity in a methicillin-resistant Staphylococcus aureus-infected patient with renal insufficiency. Scand J Infect Dis. 2013;45(1):77–80. https://doi.org/10.3109/00365548.2012.708783.
Crass RL, Cojutti PG, Pai MP, Pea F. Reappraisal of linezolid dosing in renal impairment to improve safety. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/AAC.00605-19.
Wu V-C, et al. High frequency of linezolid-associated thrombocytopenia and anemia among patients with end-stage renal disease. Infect Dis Soc Am. 2005;42:66–72. https://doi.org/10.1086/498509.
Jones SJ, Nichols KR, DeYoung HL, Cox EG, Knoderer CA. Linezolid-associated thrombocytopenia in children with renal impairment. J Pediatric Infect Dis Soc. 2015;4(3):272–5. https://doi.org/10.1093/jpids/piu035.
Lin Y-H, et al. High frequency of linezolid-associated thrombocytopenia among patients with renal insufficiency. Int J Antimicrob Agents. 2006;28(4):345–51. https://doi.org/10.1016/j.ijantimicag.2006.04.017.
Moraza L, Leache L, Aquerreta I, Ortega A. Linezolid-induced haematological toxicity. Farm Hosp. 2015;39(6):320–32. https://doi.org/10.7399/fh.2015.39.6.8305.
Shi C, et al. Effect of renal function on the risk of thrombocytopaenia in patients receiving linezolid therapy: a systematic review and meta-analysis. Br J Clin Pharmacol. 2022;88(2):464–75. https://doi.org/10.1111/bcp.14965.
Kawasuji H, et al. Proposal of initial and maintenance dosing regimens with linezolid for renal impairment patients. BMC Pharmacol Toxicol. 2021;22(1):13. https://doi.org/10.1186/s40360-021-00479-w.
Lima LS, Brito ECA, Mattos K, Parisotto EB, Perdomo RT, Weber SS. A retrospective cohort study to screen linezolid-induced thrombocytopenia in adult patients hospitalized in the Midwestern Region of Brazil. Hematol Transfus Cell Ther. 2020;42(3):230–7. https://doi.org/10.1016/j.htct.2019.07.004.
Hirano R, Sakamoto Y, Tachibana N, Ohnishi M. Retrospective analysis of the risk factors for linezolid-induced thrombocytopenia in adult Japanese patients. Int J Clin Pharm. 2014;36(4):795–9. https://doi.org/10.1007/s11096-014-9961-6.
Chen C, et al. Risk factors for thrombocytopenia in adult chinese patients receiving linezolid therapy. Curr Ther Res Clin Exp. 2012;73(6):195–206. https://doi.org/10.1016/j.curtheres.2012.07.002.
Niwa T, et al. Retrospective cohort chart review study of factors associated with the development of thrombocytopenia in adult Japanese patients who received intravenous linezolid therapy. Clin Ther. 2009;31(10):2126–33. https://doi.org/10.1016/j.clinthera.2009.10.017.
Xiao B, Deng P, Jin H, Wang H, Cao Y. Lactic acidosis and thrombocytopenia associated with linezolid therapy: a case report. Am J Case Reports. 2018;19:1117–20. https://doi.org/10.12659/AJCR.911362.
“SPC Linezolid.” Accessed: Jan. 23, 2023. Available: https://www.geneesmiddeleninformatiebank.nl/smpc/h115279_smpc.pdf
Brier ME, et al. Pharmacokinetics of linezolid in subjects with renal dysfunction. Antimicrob Agents Chemother. 2003;47(9):2775–80. https://doi.org/10.1128/AAC.47.9.2775-2780.2003.
Souza E, Crass RL, Felton J, Hanaya K, Pai MP. Accumulation of major linezolid metabolites in patients with renal impairment. Antimicrob Agents Chemother. 2020. https://doi.org/10.1128/AAC.00027-20.
MacGowan AP. Pharmacokinetic and pharmacodynamic profile of linezolid in healthy volunteers and patients with Gram-positive infections. J Antimicrob Chemother. 2003. https://doi.org/10.1093/jac/dkg248.
Matsumoto K, et al. Higher linezolid exposure and higher frequency of thrombocytopenia in patients with renal dysfunction. Int J Antimicrob Agents. 2010;36(2):179–81. https://doi.org/10.1016/j.ijantimicag.2010.02.019.
Tsuji Y, et al. Thrombocytopenia and anemia caused by a persistent high linezolid concentration in patients with renal dysfunction. J Infect Chemother. 2011;17(1):70–5. https://doi.org/10.1007/s10156-010-0080-6.
Hiraki Y, Tsuji Y, Matsumoto K, Morita K, Kamimura H, Karube Y. Influence of linezolid clearance on the induction of thrombocytopenia and reduction of hemoglobin. Am J Med Sci. 2011;342(6):456–60. https://doi.org/10.1097/MAJ.0b013e318218cf18.
Nukui Y, et al. High plasma linezolid concentration and impaired renal function affect development of linezolid-induced thrombocytopenia. J Antimicrob Chemother. 2013;68(9):2128–33. https://doi.org/10.1093/jac/dkt133.
Cattaneo D, et al. Linezolid plasma concentrations and occurrence of drug-related haematological toxicity in patients with Gram-positive infections. Int J Antimicrob Agents. 2013;41(6):586–9. https://doi.org/10.1016/j.ijantimicag.2013.02.020.
Kawasuji H, et al. Initially reduced linezolid dosing regimen to prevent thrombocytopenia in hemodialysis patients. Antibiotics Basel. 2021. https://doi.org/10.3390/antibiotics10050496.
Fang J, et al. Does the conventional dosage of linezolid necessitate therapeutic drug monitoring?—Experience from a prospective observational study. Ann Transl Med. 2020;8(7):493–493. https://doi.org/10.21037/atm.2020.03.207.
Pea F, Cojutti PG, Baraldo M. A 10-year experience of Therapeutic Drug Monitoring (TDM) of linezolid in a hospital-wide population of patients receiving conventional dosing: Is there enough evidence for suggesting TDM in the majority of patients? Basic Clin Pharmacol Toxicol. 2017;121(4):303–8. https://doi.org/10.1111/bcpt.12797.
Cattaneo D, Gervasoni C, Cozzi V, Castoldi S, Baldelli S, Clementi E. Therapeutic drug management of linezolid: a missed opportunity for clinicians? Int J Antimicrob Agents. 2016;48(6):728–31. https://doi.org/10.1016/j.ijantimicag.2016.08.023.
González-Del Castillo J, et al. Predictive score of haematological toxicity in patients treated with linezolid. Eur J Clin Microbiol Infect Dis. 2017;36(8):1511–7. https://doi.org/10.1007/s10096-017-2960-5.
Choi GW, et al. Risk factors for linezolid-induced thrombocytopenia in patients without haemato-oncologic diseases. Basic Clin Pharmacol Toxicol. 2019;124(2):228–34. https://doi.org/10.1111/bcpt.13123.
Rao GG, et al. Therapeutic drug monitoring can improve linezolid dosing regimens in current clinical practice: a review of linezolid pharmacokinetics and pharmacodynamics. Ther Drug Monit. 2020;42(1):83–92. https://doi.org/10.1097/FTD.0000000000000710.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Not applicable.
Conflict of Interest
All authors have declared no conflicts of interest.
Ethics Approval
Not applicable.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
The participants have consented to the submission of the case report to the journal.
Availability of Data and Material Code
The original data is available on request.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SRE Laarhuis. The first draft of the manuscript was written by SRE Laarhuis and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Laarhuis, S.R.E., Kerskes, C.H.M., Nijziel, M.R. et al. Linezolid-Induced Thrombocytopenia in Patients with Renal Impairment: A Case Series, Review and Dose Advice. Drugs R D 24, 109–115 (2024). https://doi.org/10.1007/s40268-024-00458-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-024-00458-6