Abstract
Introduction
In Germany, incidence rates of basal cell (BCC) and squamous cell carcinoma (SCC) rose significantly from 1998 to 2010. Ultraviolet (UV) light exposure, immunosuppressants and drugs with photosensitising potential are known to increase the risk to develop BCC and SCC. The aim of our study was to analyse the adverse drug reaction (ADR) reports from Germany referring to BCC and SCC and to compare them to BCC and SCC occurring in the general population.
Methods
We analysed all validated spontaneous ADR reports referring to BCC (n = 191) and SCC (n = 75) from Germany contained in the European ADR database EudraVigilance prior to 6 March 2019. These reports were compared to 1,267,210 BCC and 476,903 SCC cases from the German Centre for Cancer Registry Data recorded from 2006 to 2018.
Results
The number of BCC and SCC reports as well as the BCC and SCC incidences in the registry increased in the analysed time period. Patients with drug-associated BCC (60 years) and SCC (64 years) were younger than patients with BCC (72 years) and SCC (76 years) in the registry. In 57.1 and 60.0% of BCC and SCC reports immunosuppressants were reported as suspected. The reported suspected drug was assumed to possess a photosensitising potential in 41.9 and 44.0% of BCC and SCC reports.
Conclusions
In Germany, drug-associated BCC and SCC occurred at a younger age than in the general population. The results underline the necessity for skin cancer screening of patients treated with immunosuppressants or with drugs with photosensitising potential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The number of adverse drug reaction reports for basal (BCC) and squamous cell carcinomas (SCC) and their incidences in the registry increased. |
Immunosuppressants were most frequently suspected. |
1 Introduction
Non-melanoma skin cancer (NMSC) is the main term for various skin cancers such as basal (BCC) and squamous cell carcinomas (SCC), cutaneous lymphomas or Merkel cell carcinoma. However, it mainly refers to BCC and SCC, which account for about 70 and 30% of NMSC, respectively [1, 2].
NMSC is the most common cancer in the world [3, 4]. In Germany, incidence rates rose significantly from 43.1 cases/100,000 in 1998 to 105.2 cases/100,000 in 2010 with age-standardised incidence rates being higher for men than for women [5].
Ultraviolet (UV) radiation is considered the primary risk factor, playing a major role in around 50–70% of SCC and 50–90% of BCC in fair-skinned people [4]. Further risk factors are a previous history of (multiple) skin cancers [6], long-lasting inflammatory processes or long-lasting skin lesions [7], as well as life-style factors such as alcohol consumption [8]. Occurrence of BCC and SCC has also been reported as an adverse drug reaction (ADR) to immunosuppressants [1] and hydrochlorothiazide [9], probably owing to immunosuppressive and photosensitising mechanisms, respectively.
Our first aim was to analyse the number of and the characteristics reported in ADR reports from Germany referring to BCC and SCC contained in the European ADR database EudraVigilance. Secondly, we wanted to investigate whether the reported characteristics differed between reports referring to BCC and SCC. We also analysed the proportion of reports referring to immunosuppessants and drugs with photosensitising potential. Thirdly, we compared the characteristics reported in BCC and SCC reports to those reported in BCC and SCC cases from the German Cancer Registry in order to identify potential drug-associated characteristics. Fourth, the number of reports for the most frequently reported drugs in BCC and SCC reports were considered in relation to their number of prescriptions.
2 Material and Methods
2.1 EudraVigilance
ADRs (definition and seriousness described in [10,11,12]) can be reported by healthcare professionals (e.g. physicians, pharmacists) who are obliged by their professional conduct code to report ADRs or non-healthcare professionals (e.g. consumers) [10,11,12]. All ADR reports received from one of the member states of the European Economic Area are stored in EudraVigilance, the ADR database of the European Medicines Agency. In EudraVigilance, ADRs are coded in accordance with MedDRA terminology and drugs with the EudraVigilance medicinal product dictionary [13, 14].
2.2 Identification and Validation of Adverse Drug Reaction (ADR) Reports Referring to Basal (BCC) and Squamous (SCC) Cell Carcinomas
We identified all spontaneous ADR reports from Germany contained in EudraVigilance received from the start of the database up to 6th March 2019, with an ADR coded in the standardised MedDRA query (SMQ) [14] level 2 “skin malignant tumours (narrow)” (n = 1101) (see Fig. 1 flow chart). The identified 1101 ADR reports were assessed with regard to the causal relationship and the completeness of the ADR reports by one of three board‐certified specialists in dermatology or a pharmacist. In order to harmonise the assessment, ten randomly selected ADR reports were initially assessed together, using the WHO criteria [15] for the assessment of causal relationship and the VigiGrade completeness score [16] to assess the quality of the reports (see below). Any uncertainties in the assessment were discussed together in regular meetings and decided on consensus. Only ADR reports with a quantifiable time to onset information between the intake of a drug and the skin cancer and with an at least possible causal relationship were considered for further analyses (n = 565, 51.3%). Data from the individual reports (n = 565) were selected and the reports were assigned to one or more types of skin tumours [melanoma, basal cell carcinoma, squamous cell carcinoma and other skin tumours (incl. not assignable)]. Among these n = 565 validated reports, n = 191 reports and n = 75 reports were assigned to BCC and SCC. Sixteen cases were assigned to both BCC and SCC. From here on, we will refer to BCC and SCC identified in the ADR database as "reports", distinguishing from those identified in the cancer registry as "cases".
An evaluation of the melanoma reports has already been published [17].
2.3 Completeness Score
A published score (VigiGrade [16]) was applied to measure the quality of documentation of BCC and SCC reports (completeness score > 0.8 “well documented”). Its calculation [16]) was modified [18] as it was not computed for every reported drug-ADR pair (in case more than one ADR had been reported) but only for BCCs and SCCs. The calculated completeness score was 0.68 [95% confidence interval (CI) 0.65–0.77] for BCC and 0.73 (95% CI 0.68-0.77) for SCC reports. Most of the penalties were given for missing exact time to onset (TTO) information, for example month and year were reported (= quantifiable TTO) but not the exact day of occurrence.
2.4 Descriptive Analyses of the Validated BCC and SCC Reports
The validated BCC and SCC reports were analysed with regard to the (1) patients’ demographics, (2) drugs most frequently reported as suspected, (3) proportion of patients with autoimmune diseases, (4) proportion of reports referring to drugs with immunosuppressants and drugs with photosensitising potential, (5) seriousness of ADR reports, (6) annual numbers of reports, (7) location of BCC and SCC, and (8) TTO between drug intake and occurrence of the BCC or SCC. Furthermore, sex-stratified analyses were performed.
Information about family history of any tumour (4.0%, n = 10), UV exposure (15.6%, n = 39) and skin type (7.6%, n = 19) were rarely reported, and are thus not presented in our results.
The documented seriousness of an ADR report follows the legal definition [11]. An ADR report is classified as serious if the reported ADR was life-threatening, led to or prolonged hospitalisation, led to death or disabilities, or caused a congenital anomaly. The seriousness based on the legal definition is not equal to the clinical definition of severity of an ADR.
Patients were classified as patients with autoimmune diseases if at least one of the following diseases was reported in the patients’ history or as indication for drug therapy: multiple sclerosis, psoriasis, Crohn’s disease, ulcerative colitis or arthritis (all forms). Note that, since the history of the patients or the indication of drug therapies were not always provided, not all patients with autoimmune diseases may have been identified.
The assignment of immunosuppressants reported as suspected was based on the Anatomic Therapeutical Classification (ATC) code L04A [19]. For the evaluation of patients treated with drugs with immunosuppressive effects in the past or concomitantly, all drugs with potentially immunosuppressive effects were considered.
Furthermore, the drugs with photosensitising potential were identified based on information in the summary of product characteristics (SmPC) or literature. Note that concomitant or past exposure to drugs with photosensitising potential was not considered.
2.5 The Number of ADR Reports per Inhabitants
The number of inhabitants in Germany in total and stratified by age and sex for each of the years 1995–2018 was extracted from the Genesis database of the German Federal Statistical Office [20]. The number of BCC and SCC reports per 10 million inhabitants was calculated by
(number of BCC/SCC reports per year (stratified by age and gender)/number of inhabitants per year (stratified by age and gender)) × 10,000,000
2.6 Prescription Data
Prescription data were provided by the Research Institute for Ambulatory Health Care in Germany [21]. The provided data include all outpatient drug prescriptions for patients with statutory health insurances (approximately 80–90% of the German population) dispensed in German pharmacies from 2009 onwards. Reporting rates were calculated by the number of reports for the five most frequently reported drugs in BCC and SCC reports divided by their number of prescriptions. Note that inpatient prescriptions were not considered.
2.7 Data from the German Cancer Registry
Population-based cancer registration in Germany is organized by the federal states, and data are transmitted annually to the Centre for Cancer Registry at the Robert Koch Institute (RKI) [22]. National incidence rates for BCC and SCC were estimated from 2006 to 2018 (presented in Fig. 2) based on selected registries with a presumed high completeness for NMSC. In contrast, proportions of tumour locations (presented in Table 2; see also Online Supplemental Material (OSM) Tables S1 and S2) are based on all BCC and SCC cases notified between 2006 and 2018.
2.8 Statistical Analysis
Means with standard deviations (SDs) and medians with interquartile ranges (IQRs) were calculated for patients’ age. Frequency distributions with percentages were calculated for all other criteria. Odds ratios (ORs) with 95% CIs were calculated for the comparative analysis of BCC and SCC reports. If the lower CI exceeded 1 the analysed characteristic was considered to be more frequently reported in BCC reports. If the upper CI was smaller than 1 the analysed characteristic was considered to be more frequently reported in SCC reports.
2.9 Ethics Approval and Data Availability
The study was approved by the local ethics committee of the Medical Faculty of Bonn (file no, 100/21). Due to data privacy requirements and the EudraVigilance access policy [23], the complete individual pseudonymised case reports are not available to the readership. Researchers can perform the same analysis in the EudraVigilance. Although different levels of access are granted for different stakeholders [23], even with the lowest level of access analyses of aggregated data are possible. For further information regarding the processing of personal data in the context of the operation of EudraVigilance Human, we refer to the European Medicines Agency’s Data Protection Notice for EudraVigilance Human [24].
3 Results
3.1 Baseline and Comparative Analysis of BCC and SCC Reports
In the analysed period of time 191 BCC and 75 SCC reports were identified (ratio: 2.5:1). Patients in the BCC reports (median: 60.0 years) were approximately 4 years younger than patients in SCC reports (median: 64.0 years). Female sex was clearly more often reported in BCC compared to SCC reports (OR: 3.1 [1.7–5.5]) (Table 1).
Autoimmune diseases in the patient history or as an indication for drug therapy were more often reported in BCC (56.5%) compared to SCC reports (38.7%) (OR: 2.1 [1.2–3.6]). In contrast, prior non-skin-related tumours were less often documented for patients of BCC than SCC reports (OR: 0.3 [0.1–0.6]).
At the aggregated drug class level more than half of BCC (57.1%) and SCC (60.0%) reports referred to immunosuppressants as suspected drugs. The second most frequently reported drug classes were thiazides (12.6%) in BCC and other antineoplastic agents (24.0%) in SCC reports. In comparison, immunostimulants were more often suspected (OR: 5.9 [0.8–45.3]) and other antineoplastic agents (OR: 0.2 [0.1–0.5]) as well as corticosteroids (OR: 0.2 [0.1–0.9]) less often suspected in BCC than SCC reports.
On the drug substance level, fingolimod was most often reported as suspected in BCC reports (13.6%), and more often suspected in BCC compared to SCC reports (OR: 3.8 [1.1–12.9]), as well as etanercept (6.8%, OR: 5.4 [0.7–42.1]). In contrast, adalimumab was most frequently suspected in SCC reports (12.0%, OR: 1.0 [0.4–2.2]). Lenalidomide, one of the second most frequently reported drugs in SCC reports, was clearly more often reported in SCC than BCC reports (10.7%, OR: 0.0 [0.0–0.4]). Hydrochlorothiazide, the other second most common suspected drug in SCC reports (10.7%), also ranked second in BCC reports (13.1%) (OR: 1.3 [0.5–2.9]).
More patients in SCC reports (41.3%) took drugs with immunosuppressive effects in the past or concomitantly than patients in BCC reports (32.5%). In this respect, corticosteroids (22.7%, OR: 0.4 [0.2–0.9]) were most often and more often used by patients with SCC, and immunosuppressants (16.2%) by patients with BCC. Additionally, other antineoplastics (OR: 0.2 [0.0–0.6]) and alkalysing agents (OR: 0.1 [0.0–0.5]) were more frequently taken in the past or concomitantly by patients in SCC than in BCC reports. The distribution of drugs with photosensitising potential reported as suspected was almost equal between BCC and SCC reports.
Almost all reports were designated as serious according to the legal definition (BCC: 99.0%; SCC: 97.3%). Notably, the seriousness criterion death was coded more frequently in reports referring to SCC than BCC (OR: 0.3 [0.1–0.8]).
3.2 Annual Number of Reports
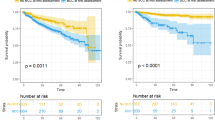
The BCC/SCC ratio was 2.5:1 in the reports and 2.8:1 in the cases. Per 10 million inhabitants, the annual number of BCC and SCC reports increased in the analysed period of time with several peaks. These peaks may be related to specific substances (Fig. 2). As an example, in 2013 roughly one-third of the BCC and SCC reports referred to fingolimod (33.3% (6/18)) and adalimumab (36.3% (4/11)) and in 2018 hydrochlorothiazide was most frequently reported in BCC (37.5% (12/32) and SCC (50.0% (6/12)) reports. Likewise, the incidences for BCC and SCC cases increased from 2006 to 2018.
Basal (BCC) and squamous cell carcinoma (SCC): Annual number of BCC/SCC reports and BCC/SCC incidences per 10 million inhabitants. The figure shows the annual number of BCC and SCC reports per 10 million inhabitants and the BCC and SCC incidences per 10 million inhabitants from the cases of the German cancer registry. First reports referring to BCCs and SCCs were received in 1997 and 2002, respectively. Data from the German cancer registry were available from 2006 onwards. The vertical line marks the year 2008. In July 2008, a reimbursed skin cancer screening was implemented in Germany
3.3 Age- and Sex-Stratified Analyses of BCC and SCC Reports
An increased number of reports per 10 million inhabitants and an increase of the incidences per 10 million person-years was observed from 25- and 45-year-olds onwards for BCC and SCC, respectively (Fig. 3). In patients below 60 years (except for age class 15–19 years), the number of BCC reports per females was higher than the number of BCC reports per males. The opposite was seen for patients above 60 years. Likewise, the BCC incidences of cases were higher for females below 60 years and lower for females above 60 years compared to males of the same age. A higher number of SCC reports per females was only seen for patients aged 30–34 years. Likewise, higher SCC incidences for cases for females were only observed for 25- to 39-year-olds.
3.4 Characteristics in BCC and SCC Reports and Cases
The proportion of females was higher in BCC reports (56.5%) than in BCC cases (48.7%). For SCC fewer females were included in reports (29.3%) than in cases (41.6%). In the BCC and SCC cases, the proportion of males (BCC: 51.3%, SCC: 58.4%) exceeded the proportion of females (BCC: 48.7%, SCC: 41.6%). As already seen in the reports, patients with BCC (median age: 72.0 years) were also younger than patients with SCC (median age: 76.0 years) in the cases (Fig. 2; Table 2). Patients with BCC (median age: 60.0 years) and SCC (median age: 64.0 years) in the reports were approximately 10 years younger than patients in the cases. Differences were more pronounced in females than in males.
In reports and cases, BCCs and SCCs were mostly located in the face of the patient. Trunk was the second most frequently reported location in BCC reports and cases, while upper and lower extremities and oral cavity ranked second in SCC reports and cases, respectively. With regard to sex, differences in proportions of reported locations of BCC and SCC were observed between the reports and the cases (OSM Resource 1).
3.5 Time to Onset Analyses of BCC and SCC Stratified by Drugs
The median time to onset (TTO) from the start of drug therapy to the occurrence was shorter for SCC (788 days) than for BCC (1117.5 days) (Table 5). Both BCC (2044 days) and SCC (2143 days) associated with drugs with photosensitising potential occurred later than BCC (930 days) and SCC (811 days) associated with immunosuppressants. Differences in the TTO analyses were observed for the five drugs most frequently reported as suspected in BCC and SCC reports (Fig. 4). Etanercept (immunosuppressive drug)-associated BCC occurred earlier, mostly within the first 2 years of drug therapy. In contrast, hydrochlorothiazide (photosensitising potential)-associated BCC had the longest TTO and occurred mostly after 3–12 years after start of drug therapy. In SCC reports, lenalidomide (immunosuppressive drug)-associated SCC occurred earlier and most of them within the first 2 years of drug therapy. The longest TTO with 17–25 years was detected for azathioprine (immunosuppressive and photosensitising potential)-associated SCC.
Time to onset of BCC: fingolimod 893.0 [365.0–1278.0], hydrochlorothiazide 893.0 [365.0–1278.0], adalimumab 1157.5 [478.8–1511.5], cyclosporine 2389.5 [1584.3–3818.0], etanercept 426.0 [231.0–610.0]
Time to onset of SCC: adalimumab 1021.0 [503.0–1665.0], hydrochlorothiazide 1892.5 [1078.8–4473.8], lenalidomide 449.0 [297.5–546.5], azathioprine 6881.0 [6173.0–9125.0], cyclosporine 1320.0 [608.8–3691.8]
3.6 Reporting Rates for the Drugs Most Frequently Reported as Suspected in BCC and SCC Reports
In relation to the number of prescriptions, the highest reporting rate was found for fingolimod (median: 3.9), followed by adalimumab (median: 1.6) for BCC and for lenalidomide (median: 1.0) followed by adalimumab (median: 0.2) for SCC (Table 6). BCC and SCC were only rarely reported in relation to the huge number of hydrochlorothiazide prescriptions.
Calculated reporting rates (number of reports/number of drug prescriptions) for the five drugs most frequently reported as suspected in BCC and SCC reports are shown. For the analyses the number of reports for the time frame 2009–2018 was determined since drug prescription data was only available from 2009 onwards
4 Discussion
In the present study spontaneous ADR reports referring to BCC and SCC were analysed with regard to various characteristics and considered in relation to the number of drug prescriptions and BCC and SCC cases from the Centre of Cancer Registry in Germany. Several factors were identified that might be associated with BCC and SCC occurrence in our reports such as use of immunosuppressants and drugs with photosensitising potential.
4.1 Annual Number of Reports and Number of Cases
In literature [25], the ratio of BCC/SCC (4:1) was higher than in our reports and cases (2.5:1 and 2.8:1). Differences in the study designs might account for these differences.
As in our analysis, an increase of BCC and SCC incidences was also seen in studies from other countries [25,26,27,28]. Several reasons may impact on the increase of BCC and SCC, such as (1) higher exposure to sunlight, (2) artificial UV radiation (especially younger females), (3) increase of older people in the population (demographical change), (4) changes in drug therapies (e.g. more common use of immunosuppressants), (5) improved diagnostic tools, (6) campaigns for regular skin cancer screening. Consistent with the latter, a nationwide skin cancer-screening program was implemented in Germany in 2008, which might have led to the increases of reports and incidences after 2008 in our analysis, as also confirmed for BCC by Eiseman et al. [29].
Furthermore, specific factors such as authorisations of new drugs or drug indications, as well as drug safety alerts might have influenced the annual number of reports, as also observed by others [30, 31]. This might explain the higher numbers of (1) fingolimod-associated BCCs in 2013 (authorised in 2011) [32], (2) adalimumab-associated SCCs in 2013 (authorised for ulcerative colitis in 2012) [33], and (3) hydrochlorothiazide-associated BCCs and SCCs in 2018 and 2019 (drug safety alerts in 2018) [34].
4.2 Descriptive and Comparative Analyses of Demographic Parameters and Tumour Locations
As also seen in other studies, patients with SCC were older than patients with BCC [28, 35]. Cumulative sun exposure, which increases with rising age, is discussed as a risk factor for SCC [36]. In contrast, extensive and intermittent sun exposure at a younger age is assumed to be associated with a higher risk of BCC occurrence.
Differences in the female/male ratio for BCC and SCC were detected between our reports and our cases. In the literature, a higher risk of BCC and SCC for males than for females was described [25, 29]. In our analysis, differences in drug exposures by underlying diseases requiring treatment with sex preferences might have influenced the proportion of females and males. As an example, the prevalence for psoriasis is slightly higher for males than for females in Germany [37]. In contrast, more females than males suffer from multiple sclerosis in Germany [38].
Consistent with other studies [25, 26, 28, 39], BCCs and SCCs were most frequently located in the face, followed by the trunk and upper extremities. In fact, BCCs and SCCs occur more often on sun-exposed body sites since sun exposure is one of the major risk factors [25]. The higher proportion of SCCs located on lower extremities including the hips compared to BCCs was also observed in studies from Poland [28] and the Netherlands [39], and may indicate that for certain SCCs located on rarely sun-exposed areas of the bodies other risk factors, for example, chronic inflammation may apply.
4.3 Autoimmune Diseases, Immunosuppressants and Drugs with Photosensitising Potential
In the literature, an increased risk to develop NMSC compared to the general population is discussed for some autoimmune diseases such as rheumatoid arthritis and psoriasis [40,41,42]. For multiple sclerosis no higher risk compared to the general population was reported [43, 44], but certain subtypes (e.g. relapsing multiple sclerosis) are reported as having a higher risk [45]. However, the treatment of these autoimmune diseases might also impact on NMSC development [41, 42]. Furthermore, treatment of psoriasis with UV light (PUVA or UVB) in the past or concomitantly is known to increase the risk of NMSC occurrence [25]. In this respect, the recommended regular skin screening for patients with some of these autoimmune diseases or patients treated with specific drugs (e.g. fingolimod, PUVA) might have led to a higher detection rate of NMSC in these patients in our analysis.
Immunosuppressants, which are used to treat autoimmune diseases, were the most frequently suspected drugs in our BCC and SCC reports. A tumour-promoting effect of immunosuppressants is already known for patients under effective immunosuppression following transplantation [25].
With regard to drugs with photosensitising potential, an increased UV sensitivity may lead to more severe sunburns, and, thus to a higher risk of developing NMSC [46, 47]. Notably, we considered only the drugs reported as suspected but not used concomitantly. In addition, a short time treatment or concomitant treatment with drugs with photosensitising potential in the past or at the time of reporting might have been under-reported. Likewise, the drugs dominating in our analysis are usually used long term, such as hydrochlorothiazide, which was the most frequently reported drug with photosensitising potential.
4.4 Analysis of Time to Onset
Patient-related risk factors that may account for the shorter TTO of SCC compared to BCC are older age, the higher proportion of patients with previous tumours, and the more frequent use of antineoplastic agents in patients with SCC compared to BCC. BCC and SCC associated with immunosuppressants occurred earlier compared to those associated with drugs with photosensitising potential. This might be related to the treated autoimmune disease itself or a tumour-promoting effect of immunosuppressants [25]. In contrast, the longer TTO for BCC and SCC associated with drugs with photosensitising potential such as hydrochlorothiazide and azathioprine (also acting as an immunosuppressive agent) in our analysis may rather suggest a tumour-initiating instead of an tumour-promoting effect. In addition, it may also reflect a higher risk of NMSC after cumulative exposure [9, 47]. Furthermore, drug-specific differences in the potential to induce BCC and SCC or with regard to their pathophysiological mechanisms (e.g. immunosuppression) have to be considered.
4.5 Number of Reports in Relation to the Number of Drug Prescriptions
In BCC reports, the highest reporting rate was found for fingolimod, followed by adalimumab and etanercept. In SCC reports, reporting rates were highest for lenalidomide and adalimumab. BCCs are listed as common (SCC rare) ADRs for fingolimod [32], which is in line with the higher reporting rate and the higher number of reports for BCC compared to SCC. For patients with multiple myelomas treated with lenalidomide, the SmPC lists a more common severe type of SCC but not for BCC [48]. Severe types might be more often reported, explaining the higher proportion of lenalidomide-associated SCC compared to BCC in our analysis. Others found a higher proportion of adalimumab-associated BCC than SCC [49], which matches our analysis of reporting rates. In contrast, in the SmPC BCC and SCC are both listed as frequent ADRs for adalimumab [50]. In the SmPC of etanercept, NMSC are reported to occur uncommonly. As in our analysis, others also observed a higher proportion of etanercept-associated BCC than SCC [51].
4.6 Strengths and Limitations
The advantages of analyses in spontaneous reporting databases are the inclusion of (1) ADRs that occur in everyday life, (2) patients with comorbidities, and (3) ADRs (e.g. BCC, SCC) that may occur after long-term treatment [12]. In order to contextualize the results, comparative analyses to BCC and SCC from the German cancer registry were performed.
Two of the major limitations of our analysis are the unknown amount of under-reporting and the lack of matching exact patient-related exposure data [12]. In addition, a detection bias (e.g. skin cancer screening recommended for specific drugs) may have affected our results. Note that the applied doses of the immunosuppressants was not investigated, which may also impact on the occurrence of NMSC. Furthermore, it was demonstrated that a previous history of multiple skin cancers is a risk factor for developing subsequent skin cancer [6]. In our study only a small number of patients reported information regarding a previous history of cancer, thus under-reporting of the patients’ history cannot be excluded. Also, the subtype of BCC and SCC may play a role, which we could not investigate in our study. Under-coverage may also apply to the data from the Centre of Cancer Registry in Germany since BCC and SCC might be under-reported in particular in ambulant settings. The patients in the reports may also have been included as cases in the registry. However, due to the small number of patients in the reports compared to the cases, this should not influence our comparative analyses. The prescription data used do not include data of privately insured patients, inpatient prescriptions as well as over-the-counter drugs.
4.7 Conclusion
It has to be considered that drug-associated BCC and SCC may occur at a younger age than BCC and SCC in the general population. Our results support the recommendation of a regular skin screening of patients treated with immunosuppressants and with drugs with photosensitising potential. Likewise, our study underlines the importance of sun protective measures especially if patients are treated with drugs of photosensitising potential. Further research is needed to analyse if the drug-stratified differences are related to differences in pathophysiological mechanisms or to differences in the treated patient populations.
References
Didona D, Paolino G, Bottoni U, et al. Non melanoma skin cancer pathogenesis overview. Biomedicines. 2018;6(1):6.
Zink A. Nichtmelanozytärer Hautkrebs. Hautarzt. 2017;68(11):919–28.
Madan V, Lear JT, Szeimies RM. Non-melanoma skin cancer. Lancet. 2010;375(9715):673–85.
John SM, Trakatelli M, Gehring R, et al. CONSENSUS REPORT: recognizing non-melanoma skin cancer, including actinic keratosis, as an occupational disease—a call to action. J Eur Acad Dermatol Venereol. 2016;30(Suppl 3):38–45.
Rudolph C, Schnoor M, Eisemann N, et al. Incidence trends of nonmelanoma skin cancer in Germany from 1998 to 2010. J Dtsch Dermatol Ges. 2015;13(8):788–97.
Ciążyńska M, Pabianek M, Sławińska M, et al. Risk factors and clinicopathological features for developing a subsequent primary cutaneous squamous and basal cell carcinomas. Cancers. 2022;14(13):3069.
Chlebicka I, Jastrząb B, Stefaniak A, et al. Basal cell carcinoma secondary to trauma: a 3-year experience of the single center. Adv Clin Exp Med. 2021;30(1):83–6.
Wu S, Li WQ, Qureshi AA, et al. Alcohol consumption and risk of cutaneous basal cell carcinoma in women and men: 3 prospective cohort studies. Am J Clin Nutr. 2015;102(5):1158–66.
Arnspang Pedersen S, Gaist D, Alba Johannesdottir Schmidt S, et al. Hydrochlorothiazide use and risk of nonmelanoma skin cancer: a nationwide case-control study from Denmark. J Am Acad Dermatol. 2018;78(4):673–81.
European Medicines Ageny (EMA). Guideline on good pharmacovigilance practices (GVP) Module VI—collection, management and submission of reports of suspected adverse reactions to medicinal products (Rev 2). 2017. https://www.ema.europa.eu/en/documents/regulatory-procedural-guideline/guideline-good-pharmacovigilance-practices-gvp-module-vi-collection-management-submission-reports_en.pdf.
European Medicines Agency (EMA). Guideline on good pharmacovigilance practices (GVP) Annex I—definitions (Rev 4). 2017. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-good-pharmacovigilance-practices-annex-i-definitions-rev-4_en.pdf.
Dubrall D, Schmid M, Alesik E, et al. Frequent adverse drug reactions, and medication groups under suspicion. Dtsch Arztebl Int. 2018;115(23):393–400.
European Medicines Agency. EudraVigilance. https://www.ema.europa.eu/en/human-regulatory/research-development/pharmacovigilance/eudravigilance.
Medical Dicitionary for Regulatory Activities (MedDRA). https://www.meddra.org/.
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000;356(9237):1255–9.
Bergvall T, Noren GN, Lindquist M. vigiGrade: a tool to identify well-documented individual case reports and highlight systematic data quality issues. Drug Saf. 2014;37(1):65–77.
Sachs B, Dubrall D, Kraywinkel K, et al. Descriptive analysis of 179 German reports of melanoma reported to an adverse drug reaction database as a drug-related adverse effect, and comparison with melanoma cases contained in German cancer registries. Clin Exp Dermatol. 2022;47(6):1078–87.
Dubrall D, Just KS, Schmid M, et al. Adverse drug reactions in older adults: a retrospective comparative analysis of spontaneous reports to the German Federal Institute for Drugs and Medical Devices. BMC Pharmacol Toxicol. 2020;21:25.
Federal Institute for Drug and Medical Devices. ATC-Classification. https://www.bfarm.de/EN/Code-systems/Classifications/ATC/_node.html;jsessionid=758DAADCD2CAA6BEC2F21CBB49C13B12.intranet671.
German Federal Statistical Office. Genesis-Online. https://www.destatis.de/EN/Themes/Economic-Sectors-Enterprises/Services/database-teaser.html.
Research Institute for Ambulatory Health Care in Germany. https://www.zi.de/.
Robert Koch Institute (RKI). Zentrum für Krebsregisterdaten. Malignes Melanom der Haut. Available at: https://www.krebsdaten.de/Krebs/DE/Content/Krebsarten/Melanom/melanom_node.html.
EudraVigilance. Access to EudraVigilance. https://www.ema.europa.eu/en/human-regulatory/research-development/pharmacovigilance/eudravigilance/access-eudravigilance-data.
European Medicines Agency (EMA). European Medicines Agency’s Data Protection Notice for EudraVigilance Human (EV). https://www.ema.europa.eu/en/documents/other/european-medicines-agencys-data-protection-notice-eudravigilance-human-ev_en.pdf.
Wang H, Diepgen TL. The epidemiology of basal cell and squamous cell carcinoma. In: Molecular mechanisms of basal cell and squamous cell carcinomas. Boston: Medical Intelligence Unit, Springer; 2006.
Flohil SC, Seubring I, van Rossum MM, et al. Trends in Basal cell carcinoma incidence rates: a 37-year Dutch observational study. J Invest Dermatol. 2013;133(4):913–8.
Bath-Hextall F, Leonardi-Bee J, Smith C, et al. Trends in incidence of skin basal cell carcinoma. Additional evidence from a UK primary care database study. Int J Cancer. 2007;121:2105–8.
Ciazynska M, Kaminska-Winciorek G, Lange D, et al. The incidence and clinical analysis of non‑melanoma skin cancer. Sci Rep. 2021;11(1):4337.
Eisemann N, Waldmann A, Geller AC, et al. Non-melanoma skin cancer incidence and impact of skin cancer screening on incidence. J Invest Dermatol. 2014;134(1):43–50.
Pariente A, Gregoire F, Fourrier-Reglat A, et al. Impact of safety alerts on measures of disproportionality in spontaneous reporting databases: the notoriety bias. Drug Saf. 2007;30(10):381–8.
Hartnell NR, Wilson JP. Replication of the Weber effect using postmarketing adverse event reports voluntarily submitted to the United States Food and Drug Administration. Pharmacotherapy. 2004;24(6):743–9.
European Medicines Agency. Fingolimod authorization. https://www.ema.europa.eu/en/medicines/human/EPAR/gilenya.
European Medicines Agency. Adalimumab authorization. https://www.ema.europa.eu/en/medicines/human/EPAR/humira.
Federal Institute for Drugs and Medical Devices. Rote-hand-brief hydrochlorothiazide. https://www.bfarm.de/SharedDocs/Risikoinformationen/Pharmakovigilanz/DE/RHB/2018/rhb-hydrochlorothiazid.html.
Muzic JG, Schmid AR, Wright AC, et al. Incidence and trends of basal cell carcinoma and cutaneous squamous cell carcinoma: a population-based study in Olmsted County, Minnesota, 2000–2010. Mayo Clin Proc. 2017;92(6):890–8.
Leiter U, Garbe C. Epidemiology of melanoma and nonmelanoma skin cancer—the role of sunlight. In: Reichrath J, editor. Sunlight, vitamin D and skin cancer advances in experimental medicine and biology, vol. 624. New York: Springer; 2008. https://doi.org/10.1007/978-0-387-77574-6_8.
Sewerin P, Brinks R, Schneider M, et al. Prevalence and incidence of psoriasis and psoriatic arthritis. Ann Rheum Dis. 2019;78:286–7.
Höer A, Schiffhorst G, Zimmermann A, et al. Multiple sclerosis in Germany: data analysis of administrative prevalence and healthcare delivery in the statutory health system. BMC Health Serv Res. 2014;14:381.
Hollestein LM, de Vries E, Nijsten T. Trends of cutaneous squamous cell carcinoma in the Netherlands: increased incidence rates, but stable relative survival and mortality 1989–2008. Eur J Cancer. 2012;48:2046–53.
Mellemkjaer L, Linet MS, Gridley G, et al. Rheumatoid arthritis and cancer risk. Eur J Cancer. 1996;32A(10):1753–7.
Raaschou P, Simard JF, Hagelberg CA, et al. Rheumatoid arthritis, anti-tumour necrosis factor treatment, and risk of squamous cell and basal cell skin cancer: cohort study based on nationwide prospectively recorded data from Sweden. BMJ. 2016;352: i262.
deShazo R, Soltani-Arabshahi R, Krishnasamy S, et al. Non-melanoma skin cancer risk among patients in the Psoriasis Longitudinal Assessment and Registry (PSOLAR). J Drugs Dermatol. 2019;18(10):1059–60.
Norgaard M, Veres K, Didden EM, et al. Multiple sclerosis and cancer incidence: a Danish nationwide cohort study. Mult Scler Relat Disord. 2019;28:81–5.
Lebrun C, Debouverie M, Vermersch P, et al. Cancer risk and impact of disease-modifying treatments in patients with multiple sclerosis. Mult Scler. 2008;14:399–405.
Kingwell E, Bajdik C, Phillips N, et al. Cancer risk in multiple sclerosis: findings from British Columbia, Canada. Brain. 2012;135(10):2973–9.
Karagas MR, Stukel TA, Umland V, et al. Reported use of photosensitizing medications and basal cell and squamous cell carcinoma of the skin: results of a population-based case–control study. J Invest Dermatol. 2007;127:2901–3.
Su KA, Habel LA, Achacoso NS, et al. Photosensitizing antihypertensive drug use and risk of cutaneous squamous cell carcinoma. Br J Dermatol. 2018;179(5):1088–94.
European Medicines Agency (EMA). Lenalidomide product information. https://www.ema.europa.eu/en/medicines/human/EPAR/revlimid.
Mercer LK, Green AC, Galloway JB, et al. The influence of anti-TNF therapy upon incidence of keratinocyte skin cancer in patients with rheumatoid arthritis: longitudinal results from the British Society for Rheumatology Biologics Register. Ann Rheum Dis. 2012;71:869–74.
European Medicines Agency (EMA). Adalimumab product information. https://www.ema.europa.eu/en/documents/product-information/amgevita-epar-product-information_en.pdf#:~:text=Each%20single%20dose%20pre-filled%20pen%20contains%2040%20mg,the%20full%20list%20of%20excipients%2C%20see%20section%206.1.
European Medicines Agency (EMA). Etanercept product information. https://www.ema.europa.eu/en/documents/product-information/nepexto-epar-product-information_en.pdf.
Acknowledgements
The authors would like to thank the ADR database research team of BfArM’s pharmacovigilance department for their excellent support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding sources
The project is funded by the German Federal Institute for Drugs and Medical Devices’ (BfArM) own resources and by the Institute for Medical Biometry, Informatics, and Epidemiology (IMBIE), University Hospital of Bonn, Germany (V-2020.2/68502/2020-2024).
Conflict of interest
The authors have no conflicts of interest.
Ethics approval
The study was approved by the local ethics committee of the Medical Faculty of Bonn (file no. 100/21).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data set generated and/or analysed during the current study are not publicly available due data privacy requirements. For further information regarding the processing of personal data in the context of the operation of EudraVigilance Human we refer to the European Medicines Agency’s Data Protection Notice for EudraVigilance Human [24]. Researchers and/or readers who are interested can perform the same analyses in the ADR database EudraVigilance of the European Medicines Agency (EMA) (public access: http://www.adrreports.eu/en/index.html). However, different levels of access are granted for different stakeholders.
Code availability
Not applicable.
Author contributions
BS, DD, WF-B and JB contributed to the study conception and design and performed the causality assessment of the ADR reports. Case identification in the ADR database and data analysis was performed by DD. Statistical analyses were performed by DD and MS. KK provided the data of the cancer registry. The first draft of the manuscript was written by DD and BS. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Additional information
Disclaimer The information and views set out in this article are those of the authors and do not necessarily reflect the official opinion of the German Federal Institute for Drugs and Medical Devices.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Dubrall, D., Sachs, B., Kraywinkel, K. et al. Analyses of Basal and Squamous Cell Carcinoma Reported as an Adverse Drug Reaction and Comparison with Cases from the Cancer Registry from Germany. Drugs R D 23, 21–33 (2023). https://doi.org/10.1007/s40268-022-00407-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-022-00407-1