Abstract
On 2 June, 2021, the US Food and Drug Administration approved ibrexafungerp (formerly MK-3118 and SCY-078) for the treatment of vulvovaginal candidiasis, also known as vaginal yeast infection. Ibrexafungerp is the first drug approved in a novel antifungal class in more than two decades, and the Food and Drug Administration’s decision was based on positive results from two pivotal phase III studies in which oral ibrexafungerp proved both safe and effective in patients with vulvovaginal candidiasis. The decision was also based on substantial preclinical and clinical work in both the pharmacokinetics and pharmacodynamics of ibrexafungerp. This paper reviews that research and looks ahead to explore how this novel antifungal agent may be used in the future to address the expanding problem of drug-resistant mycotic infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Ibrexafungerp is the first drug approved in a novel antifungal class in more than 20 years. |
Ibrexafungerp is now approved for the treatment of vulvovaginal candidiasis. |
Ibrexafungerp has activity against a variety of multidrug-resistant fungi, including Candida auris. |
Ibrexafungerp is under investigation for a variety of invasive conditions, including fungemia, to be used alone or in combination with other antimicrobial agents. |
1 Introduction
The rapid emergence of drug-resistant fungal pathogens poses an expanding threat to public health. Treatment strategies are limited and new drugs are urgently needed. Ibrexafungerp (originally known as MK-3118) is a semi-synthetic, orally bioavailable antifungal derivative of the echinocandin enfumafungin [1, 2]. Echinocandins are fungicidal against yeast and fungistatic against molds and serve as first-line agents for treating many severe invasive mycotic infections [3,4,5]. This class of drugs alters the integrity of the fungal cell wall via the inhibition of the synthesis of (1→3)-β-d-glucan [6, 7]. However, US Food and Drug Administration (FDA)-approved echinocandins are only available in intravenous formulations, which limits their use in the treatment of less severe fungal infections, such as vulovaginal candidiasis, or as step-down agents [8].
Ibrexafungerp is a first-in-class triterpenoid antifungal agent that is available in an oral formulation. Similar to echinocandins, ibrexafungerp inhibits (1→3)-β-d-glucan synthase, a key component of the fungal cell wall, and has both in vitro and in vivo activity against a variety of clinically relevant fungal species, including the yeast Candida and the mold Aspergillus [9, 10]. However, the full spectrum of activity of ibrexafungerp is not yet known, especially against invasive mold infections such as mucormycosis, scedosporiosis, and fusariosis.
Although there are a number of novel antifungal agents in development, ibrexafungerp received attention in the early stages of clinical development because the drug is in a distinct class of antifungal agents and retains in vitro activity against both echinocandin-resistant and triazole-resistant strains of pathogenic fungi, making it an attractive agent to address the escalating problem of drug-resistant invasive fungal infections [11,12,13].
2 Pharmacokinetics and Pharmacodynamics
2.1 Preclinical Studies
Pfaller and colleagues evaluated the activity of ibrexafungerp against more than 100 clinical isolates of Candida spp., including C. albicans, C. glabrata, and C. kruseii, using CLSI and EUCAST broth microdilution methods. Ibrexafungerp was active against all species tested in vitro and demonstrated similar efficacy to caspofungin, a widely used antifungal drug [14]. Importantly, the drug also showed efficacy against strains of Candida that were inherently resistant to echinocandins and triazoles. The difference between caspofungin and ibrexafungerp was most pronounced in strains of Candida harboring FKS1 and FKS2 mutations.
Lepak et al. subsequently performed an initial pharmacodynamic evaluation of ibrexafungerp in a neutropenic murine model of invasive candidiasis [15]. Mean free area under the concentration–time curve (AUC)/minimum inhibitory concentration (MIC) values associated with a 1-log kill endpoint against Candida albicans, Candida glabrata, and Candida parapsilosis were not statistically different between species but were lower than those observed for echinocandins.
Building on this work, Wring and colleagues performed single-dose pharmacokinetic studies in rats, mice, and dogs to characterize bioavailability and potential dosing regimens [16]. The drug was well absorbed across species, demonstrating good oral bioavailability in mice (> 51%), rats (45%), and dogs (35%). Ibrexafungerp also revealed a low level of clearance in rodents representing approximately 10–15% of hepatic blood flow; estimates for the terminal elimination-phase half-life ranged from 5.5 to 8.7 h in rodents to ∼ 9.3 h in dogs, suggesting once-daily dosing would be appropriate in humans.
Murine studies compared dose-dependent steady-state exposure in plasma and kidney tissue after twice-daily treatment for 1 week. These models that use the reduction in the fungal tissue burden of an intervention vs an untreated control as a measure of antifungal efficacy in vivo. The mean plasma ibrexafungerp steady-state AUC from 0 to 24 h required for efficacy in mice was 15.4 ± 2.21 μM·h (11.2 ± 1.61 μg/mL·h), and the corresponding total drug AUC/MIC ratio was 373 ± 54. Ibrexafungerp exposure in kidney tissue exceeded plasma by more than 20-fold for the AUC from 0 h to infinity and maximum concentration. The free AUC/MIC found in blood was actually lower than for echinocandins, possibly because of higher kidney/plasma exposures.
An in vivo pharmacodynamic evaluation with ibrexafungerp in a neutropenic murine model of invasive candidiasis has also been performed against C. albicans, C. parapsilosis, and C. glabrata [15]. Oral doses of 3.125–200 mg/kg of ibrexafungerp produced peak concentrations of 0.04–2.66 μg/mL, AUC from 0 to 24 h of 0.61–41.10 μg·h/mL, and AUC from 0 h to infinity values of 0.68–40.31 μg·h/mL. The pharmacodynamic index AUC/MIC was explored by using total AUC and free AUC drug concentrations; maximum responses were 4.0, 4.0, and 4.3 log10 colony-forming units/kidney reductions for C. albicans, C. glabrata, and C. parapsilosis. Taken together, these findings suggested that the drug would be suitable for trials in humans.
2.2 Phase I Trials
A single-center, open-label phase I study of healthy subjects was performed to assess the drug–drug interaction potential between ibrexafungerp and the immunomodulator tacrolimus, which is commonly used in renal transplant recipients, and may predispose patients to invasive fungal infection [17]. An important finding was that co-administration of tacrolimus and ibrexafungerp had no effect on the maximum blood concentrations of tacrolimus. There was also no change in the maximum concentration of tacrolimus in plasma and a 1.4-fold increase in total AUC, suggesting that a dose adjustment for tacrolimus may not be warranted when combined with ibrexafungerp.
Another phase I, open-label, crossover study of ibrexafungerp was performed to evaluate the pharmacokinetic parameters of rosiglitazone, a sensitive substrate of cytochrome P450 2C8 metabolism [18,19,20]. Subjects were randomized to a single oral rosiglitazone 4-mg dose alone on day 1 or a SCY-078 1250-mg loading dose on day 1 followed by a once-daily SCY-078 750-mg dose for an additional 7 days with co-administration of a single oral rosiglitazone 4-mg dose on day 3, before alternating following a ≥ 10-day washout. This study had an important finding: maximum concentration values for rosiglitazone and its metabolite, N-desmethylrosiglitazone, were unaffected by co-administration with ibrexafungerp, suggesting a low risk for interaction of ibrexafungerp with drugs metabolized via the cytochrome P450 family of enzymes. Given these encouraging findings, ibrexafungerp advanced to phase II studies.
2.3 Phase II Trials
A multicenter, open-label phase II study of patients with documented invasive candidiasis randomized subjects to receive step-down therapy in one of three treatment arms: two dosing regimens of oral ibrexafungerp or standard of care following initial echinocandin therapy [21]. Twenty-seven subjects enrolled: seven people received ibrexafungerp 500 mg, seven received ibrexafungerp 750 mg, and eight received the standard of care following echinocandin therapy.
Satisfactory response rates were reported among all groups: 86% (n = 6) in the ibrexafungerp 750-mg arm vs 71% (n = 5) in both ibrexafungerp 500-mg and standard of care treatment arms. All treatment regimens were well tolerated. A population pharmacokinetic analysis revealed that the ibrexafungerp 750-mg regimen leads to target exposure in approximately 85% of the population, suggesting that this dosage would be appropriate for further investigation.
Building on this work, a phase II, randomized, double-blind, dose-finding study was done to compare ibrexafungerp to fluconazole in women with vulvovaginal candidiasis [22]. The clinical cure (52 vs 58%) and mycological eradication (63 vs 63%) rates were similar for both drugs. Importantly, 1 month after diagnosis, clinical cure rates (70 vs 50%) were higher for the ibrexafungerp group than the fluconazole group, setting the stage for pivotal phase III studies, which are reviewed below.
2.4 Phase III Trials
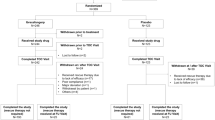
The FDA approved ibrexafungerp after two successful randomized, double-blind, placebo-controlled, phase clinical trials, VANISH 303 and VANISH 306 [23, 24]. In VANISH 303, clinical cure, mycological eradication, and clinical improvement at day 25 were 51 vs 29%, 50 vs 19%, and 64 vs 37% in the ibrexafungerp group compared with placebo [11, 25]. In VANISH 306, 188 patients with acute vulvovaginal candidiasis were randomized to receive ibrexafungerp or placebo in a 2:1 ratio [9]. The primary endpoint of the trial was clinical cure rate, defined as the complete resolution of all signs and symptoms at the test-of-cure visit on day 10. Clinical cure, mycological eradication, and clinical improvement were 63 vs 44%, 59 vs 30%, and 72 vs 55% in the ibrexafungerp group compared with placebo [26]. The FDA approval occurred 2 months after these results were reported.
3 Future Directions
The widespread use of immunosuppressants and immunomodulators in clinical practice has expanded the population of patients with immune impairment who are susceptible to invasive fungal infections [27, 28]. For the past two decades, there have only been three major classes of antifungal agents (polyenes, triazoles, and echinocandins) and their use has been diminished by the emergence of drug-resistant fungal species [29,30,31]. Better treatment options are urgently needed.
Ibrexafungerp is an orally bioavailable, first-in-class, structurally novel, triterpene antifungal with potent in vitro and in vivo activity against a variety of clinically relevant fungal pathogens including both yeasts and molds [17, 21, 32, 33]. The drug was recently approved for the treatment of vulvovaginal candidiasis and recent work suggests the agent may be useful to treat other mycotic diseases, including multidrug-resistant infections, endemic mycoses, and emerging fungal pathogens [34]. A unique property of this drug is its solubility at lower pH, which facilitates penetration into acidic environments, creating opportunities for novel treatment approaches [11, 34, 35]. An intravenous formulation is also in development.
Ibrexafungerp may also be useful in the treatment of organisms that have acquired resistance to existing fungal agents. Candida auris is an emerging pathogen that was discovered in Japan in 2008 and has rapidly spread around the world, and it has been described in the popular press as a fungal “superbug” because it may demonstrate resistance to all three major classes of antifungal agents [36, 37]. The in vitro activity and in vivo efficacy of ibrexafungerp against C. auris was recently tested by broth microdilution against more than 50 C. auris isolates [38]. Neutropenic mice were intravenously infected with this organism, and a 1-week treatment course was initiated with ibrexafungerp, caspofungin, or fluconazole. Pathogen burden was evaluated by renal colony counts on day 8 and on day 21. Throughout the study, ibrexafungerp demonstrated consistent activity with MICs between 0.25 and 2 μg/mL against all isolates of C. auris. Crucially, a survival difference was noted in mice treated with the elevated doses of ibrexafungerp as compared with other drugs.
The key finding in this study is that ibrexafungerp is effective in vivo against C. auris even when appropriate therapy is not initiated promptly. This matters because the diagnosis of human fungal pathogens is sometimes delayed owing to limitations in molecular diagnostics [27, 39]. Although preclinical comparison studies are limited, this study serves as a proof of principle that ibrexafungerp may be a useful treatment option in clinical practice for an emerging fungal pathogen that is often resistant to existing treatment options, although further studies in humans are needed [40].
Additional phase III studies of ibrexafungerp are ongoing. A multicenter, randomized, double-blind phase III study (NCT04029116) is currently underway to investigate the efficacy of ibrexafungerp in women with recurrent vulvovaginal candidiasis [11]. Another phase III, open-label, single-arm study (NCT03059992) is investigating the efficacy of ibrexafungerp in patients with invasive candidiasis and aspergillosis as well as endemic mycoses such as blastomycosis, coccidioidomycosis, and histoplasmosis [11].
Some drug-resistant fungi, such as aspergillosis, may require combination therapy. There may also be a role for ibrexafungerp in combination with other antifungal agents. Petraitis and colleagues investigated the in vitro activity and in vivo efficacy of ibrexafungerp in combination with isavuconazole against invasive pulmonary aspergillosis [41]. The combination of ibrexafungerp and isavuconazole in in vitro studies resulted in additive and synergistic interactions against Aspergillus spp., decreased pulmonary injury, reduced mycotic burden, lower GMI and (1→3)-β-d-glucan levels, and prolonged survival in comparison to antifungal monotherapy [42]. Other combinations may prove similarly effective [31, 43].
The oral bioavailability of ibrexafungerp presents yet another avenue for its potential use in clinical practice as a stepdown agent. Many patients with invasive fungal infections are treated with intravenous agents while hospitalized and may be transitioned to an oral agent upon discharge [44, 45]. Future studies will undoubtedly explore ibrexafungerp as an oral option for patients who have been partially treated for an invasive fungal infection with an intravenous agent and no longer require hospitalization. The remarkable bioavailability of the drug may give clinicians newfound flexibility.
In the future, ibrexafungerp may be used to treat a variety of fungal infections, including those attributed to resistant organisms, and it may be use alone or in combination with other drugs to treat a variety of invasive fungal pathogens [12, 46]. We do not yet know the full potential of this novel antifungal agent, but FDA approval in June 2021 serves as an important milestone. A new class of antifungal agents has finally arrived.
References
Pfaller MA, Messer SA, Motyl MR, Jones RN, Castanheira M. Activity of MK-3118, a new oral glucan synthase inhibitor, tested against Candida spp. by two international methods (CLSI and EUCAST). J Antimicrob Chemother. 2013;68(4):858–63.
Hector RF, Bierer DE. New β-glucan inhibitors as antifungal drugs. Expert Opin Ther Pat. 2011;21(10):1597–610.
Denning DW. Echinocandins and pneumocandins: a new antifungal class with a novel mode of action. J Antimicrob Chemother. 1997;40(5):611–4.
Espinel-Ingroff A. Comparison of In vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 (L-743,872) and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J Clin Microbiol. 1998;36(10):2950–6.
Cornely OA, Schmitz K, Aisenbrey S. The first echinocandin: caspofungin. Mycoses. 2002;45(Suppl. 3):56–60.
Denning DW. Echinocandin antifungal drugs. Lancet. 2003;362(9390):1142–51.
Kontoyiannis DP, Hachem R, Lewis RE, Rivero GA, Torres HA, Thornby J, et al. Efficacy and toxicity of caspofungin in combination with liposomal amphotericin B as primary or salvage treatment of invasive aspergillosis in patients with hematologic malignancies. Cancer. 2003;98(2):292–9.
Wiederhold NP. The antifungal arsenal: alternative drugs and future targets. Int J Antimicrob Agents. 2018;51(3):333–9.
Apgar JM, Wilkening RR, Parker DL, Meng D, Wildonger KJ, Sperbeck D, et al. Ibrexafungerp: an orally active β-1,3-glucan synthesis inhibitor. Bioorg Med Chem Lett. 2021;32:127661.
Chu S, Long L, McCormick TS, Borroto-Esoda K, Barat S, Ghannoum MA. A second-generation fungerp analog, SCY-247, shows potent in vivo activity in a Murine model of hematogenously disseminated Candida albicans. Antimicrob Agents Chemother. 2021;65(3):e01989-20. https://doi.org/10.1128/AAC.01989-20.
Jallow S, Govender NP. Ibrexafungerp: a first-in-class oral triterpenoid glucan synthase inhibitor. J Fungi (Basel). 2021;7(3).
Lee A. Ibrexafungerp: first approval. Drugs. 2021;81(12):1445–50.
Mesquida A, Vicente T, Reigadas E, Palomo M, Sánchez-Carrillo C, Muñoz P, et al. In vitro activity of ibrexafungerp and comparators against Candida albicans genotypes from vaginal samples and blood cultures. Clin Microbiol Infect. 2021;27(6):915.e5-8.
Pfaller MA, Messer SA, Motyl MR, Jones RN, Castanheira M. In vitro activity of a new oral glucan synthase inhibitor (MK-3118) tested against Aspergillus spp. by CLSI and EUCAST broth microdilution methods. Antimicrob Agents Chemother. 2013;57(2):1065–8.
Lepak AJ, Marchillo K, Andes DR. Pharmacodynamic target evaluation of a novel oral glucan synthase inhibitor, SCY-078 (MK-3118), using an in vivo murine invasive candidiasis model. Antimicrob Agents Chemother. 2015;59(2):1265–72.
Wring SA, Randolph R, Park S, Abruzzo G, Chen Q, Flattery A, et al. Preclinical pharmacokinetics and pharmacodynamic target of SCY-078, a first-in-class orally active antifungal glucan synthesis inhibitor, in murine models of disseminated candidiasis. Antimicrob Agents Chemother. 2017;61(4):e02068-e2116.
Wring S, Murphy G, Atiee G, Corr C, Hyman M, Willett M, et al. Clinical pharmacokinetics and drug–drug interaction potential for coadministered SCY-078, an oral fungicidal glucan synthase inhibitor, and tacrolimus. Clin Pharmacol Drug Dev. 2019;8(1):60–9.
Wring S, Murphy G, Atiee G, Corr C, Hyman M, Willett M, et al. Lack of impact by SCY-078, a first-in-class oral fungicidal glucan synthase inhibitor, on the pharmacokinetics of rosiglitazone, a substrate for CYP450 2C8, supports the low risk for clinically relevant metabolic drug–drug interactions. J Clin Pharmacol. 2018;58(10):1305–13.
Hruska MW, Amico JA, Langaee TY, Ferrell RE, Fitzgerald SM, Frye RF. The effect of trimethoprim on CYP2C8 mediated rosiglitazone metabolism in human liver microsomes and healthy subjects. Br J Clin Pharmacol. 2005;59(1):70–9.
Niemi M, Backman JT, Neuvonen PJ. Effects of trimethoprim and rifampin on the pharmacokinetics of the cytochrome P450 2C8 substrate rosiglitazone. Clin Pharmacol Ther. 2004;76(3):239–49.
Spec A, Pullman J, Thompson GR, Powderly WG, Tobin EH, Vazquez J, et al. MSG-10: a phase 2 study of oral ibrexafungerp (SCY-078) following initial echinocandin therapy in non-neutropenic patients with invasive candidiasis. J Antimicrob Chemother. 2019;74(10):3056–62.
Azie N, Angulo D, Dehn B, Sobel JD. Oral ibrexafungerp: an investigational agent for the treatment of vulvovaginal candidiasis. Expert Opin Investig Drugs. 2020;29(9):893–900.
Colombo RE, Vazquez JA. An evaluation of ibrexafungerp for the treatment of invasive candidiasis: the evidence to date. Expert Opin Pharmacother. 2021;22(7):797–807.
Gamal A, Chu S, McCormick TS, Borroto-Esoda K, Angulo D, Ghannoum MA. Ibrexafungerp, a novel oral triterpenoid antifungal in development: overview of antifungal activity against. Front Cell Infect Microbiol. 2021;11:642358.
Giacobbe DR, Magnasco L, Sepulcri C, Mikulska M, Koehler P, Cornely OA, et al. Recent advances and future perspectives in the pharmacological treatment of Candida auris infections. Expert Rev Clin Pharmacol. 2021;14(10):1205–10.
Seiler GT, Ostrosky-Zeichner L. Investigational agents for the treatment of resistant yeasts and molds. Curr Fungal Infect Rep. 2021:1–12.
McCarthy MW, Aguilar-Zapata D, Petraitis V, Walsh TJ. Diagnosis, classification, and therapeutic interventions for sinopulmonary aspergillosis. Expert Rev Respir Med. 2017;11(3):229–38.
McCarthy MW, Denning DW, Walsh TJ. Future research priorities in fungal resistance. J Infect Dis. 2017;216(Suppl_3):S484–92.
McCarthy MW, Kontoyiannis DP, Cornely OA, Perfect JR, Walsh TJ. Novel agents and drug targets to meet the challenges of resistant fungi. J Infect Dis. 2017;216(Suppl_3):S474–83.
McCarthy MW, Walsh TJ. Drug development challenges and strategies to address emerging and resistant fungal pathogens. Expert Rev Anti Infect Ther. 2017;15(6):577–84.
McCarthy MW, Walsh TJ. Drugs currently under investigation for the treatment of invasive candidiasis. Expert Opin Investig Drugs. 2017;26(7):825–31.
Ghannoum M, Long L, Isham N, Hager C, Wilson R, Borroto-Esoda K, et al. Activity of a novel 1,3-beta-d-glucan synthase inhibitor, ibrexafungerp (formerly SCY-078), against Candida glabrata. Antimicrob Agents Chemother. 2019;62(12):e01510-e1519.
Nunnally NS, Etienne KA, Angulo D, Lockhart SR, Berkow EL. Activity of ibrexafungerp, a novel glucan synthase inhibitor against Candida glabrata isolates with FKS mutations. Antimicrob Agents Chemother. 2019;63(11):e01692-e1719.
Sobel JD, Borroto-Esoda K, Azie N, Angulo D. In vitro pH activity of ibrexafungerp against fluconazole-susceptible and -resistant Candida isolates from women with vulvovaginal candidiasis. Antimicrob Agents Chemother. 2021;65(8):e0056221.
Larkin EL, Long L, Isham N, Borroto-Esoda K, Barat S, Angulo D, et al. A novel 1,3-beta-d-glucan inhibitor, ibrexafungerp (formerly SCY-078), shows potent activity in the lower pH environment of vulvovaginitis. Antimicrob Agents Chemother. 2019;63(5):e02611-e2618.
Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H. Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol Immunol. 2009;53(1):41–4.
Lee WG, Shin JH, Uh Y, Kang MG, Kim SH, Park KH, et al. First three reported cases of nosocomial fungemia caused by Candida auris. J Clin Microbiol. 2011;49(9):3139–42.
Wiederhold NP, Najvar LK, Olivo M, Morris KN, Patterson HP, Catano G, et al. Ibrexafungerp demonstrates in vitro activity against fluconazole-resistant Candida auris and in vivo efficacy with delayed initiation of therapy in an experimental model of invasive candidiasis. Antimicrob Agents Chemother. 2021;65(6):e02694-e2720.
McCarthy M, Rosengart A, Schuetz AN, Kontoyiannis DP, Walsh TJ. Mold infections of the central nervous system. N Engl J Med. 2014;371(2):150–60.
McCarthy M. Hospital transmitted Candida auris infections confirmed in the US. BMJ. 2016;355:i5978.
Petraitis V, Petraitiene R, Katragkou A, Maung BBW, Naing E, Kavaliauskas P, et al. Combination therapy with ibrexafungerp (formerly SCY-078), a first-in-class triterpenoid inhibitor of (1→3)-β-d-glucan synthesis, and isavuconazole for treatment of experimental invasive pulmonary aspergillosis. Antimicrob Agents Chemother. 2020;64(6):e02429-e2519.
Walsh TJ, Petraitiene R, Petraitis V. Modeling invasive aspergillosis: how close are predicted antifungal targets? J Fungi (Basel). 2020;6(4):198.
Katragkou A, McCarthy M, Meletiadis J, Petraitis V, Moradi PW, Strauss GE, et al. In vitro combination of isavuconazole with micafungin or amphotericin B deoxycholate against medically important molds. Antimicrob Agents Chemother. 2014;58(11):6934–7.
Quindós G, Gil-Alonso S, Marcos-Arias C, Sevillano E, Mateo E, Jauregizar N, et al. Therapeutic tools for oral candidiasis: current and new antifungal drugs. Med Oral Patol Oral Cir Bucal. 2019;24(2):e172–80.
Król J, Nawrot U, Bartoszewicz M. Anti-candidal activity of selected analgesic drugs used alone and in combination with fluconazole, itraconazole, voriconazole, posaconazole and isavuconazole. J Mycol Med. 2018;28(2):327–31.
Waterer G. Advances in anti-fungal therapies. Mycopathologia. 2021;186(5):665–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the preparation of this article.
Conflict of interest
Dr. McCarthy has nothing to declare and reports no conflicts of interests associated with this article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
McCarthy, M.W. Pharmacokinetics and Pharmacodynamics of Ibrexafungerp. Drugs R D 22, 9–13 (2022). https://doi.org/10.1007/s40268-021-00376-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-021-00376-x