Abstract
The decision to prescribe anticoagulant therapy must consider the balance between reducing the risk of thromboembolic events and increasing the risk of bleeding. Although assessments of net clinical outcomes with oral anticoagulants are not new, this article presents an evaluation of benefit–risk by considering only events of substantial and comparable clinical relevance (i.e., events with serious long-term sequelae likely to have irreversible consequences, including death). This is based on the concept of the number of patients who need to be treated to elicit one beneficial [number needed to treat (NNT)] or harmful [number needed to harm (NNH)] event. The approach is illustrated using data from phase III trials of rivaroxaban, selected because it has the broadest range of approved indications of the novel oral anticoagulants. For example, in the ATLAS ACS 2 TIMI 51 trial of rivaroxaban plus standard antiplatelet therapy following an acute coronary syndrome event, the current analysis demonstrates that 63 patients need to be treated (over 24 months) to prevent one all-cause mortality event compared with placebo (NNT = 63). Conversely, 500 patients need to be treated to cause one additional intracranial hemorrhage (NNH = 500). The most relevant and clinically meaningful assessment of benefit–risk may therefore be achieved by focusing only on events of greatest concern to patients and physicians, namely those with (potentially) long-lasting, severe consequences. Although there are clear limitations to this type of analysis, rivaroxaban appears to demonstrate a broadly favorable benefit–risk profile across multiple clinical indications.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Clinically meaningful assessment of the benefit–risk of anticoagulant therapy may be achieved by focusing on efficacy and safety events that have the potential for long-lasting, severe consequences. |
The benefit–risk profile of rivaroxaban was assessed by calculating the number of patients needed to treat and the number needed to harm based on the results of phase III clinical trials. |
Rivaroxaban demonstrates a broadly favorable benefit–risk profile across multiple clinical indications. |
1 Introduction
Anticoagulant drugs are the mainstay therapy for the prevention and treatment of venous thromboembolism (VTE) and for stroke prevention in patients with non-valvular atrial fibrillation (AF). Parenteral anticoagulation (with unfractionated heparin, low molecular weight heparins, or fondaparinux) is frequently used for short-term prophylaxis and acute treatment of VTE [1]. However, these parenteral anticoagulants are not generally utilized for longer-term prophylaxis or treatment (except in cancer patients), for which oral anticoagulation is most commonly used. Until recently, vitamin K antagonists (VKAs; e.g., warfarin) were the only option for long-term oral anticoagulant therapy. VKAs are highly effective, significantly reducing the risk of stroke by ~60 % in patients with AF compared with placebo or no treatment; by contrast, antiplatelet agents are associated with a non-significant reduction in AF-related stroke of ~20 % [2]. Despite their therapeutic benefits, VKAs carry certain risks: the risk of major bleeding associated with warfarin use is estimated at between 1 and 3 % per year [3], and may be as high as 7 % per year in elderly patients with AF [4].
In addition to the risk of major bleeding, VKA use also presents a range of practical challenges, including a narrow therapeutic window and considerable inter- and intra-patient variability in dose response. These limitations necessitate routine coagulation monitoring and dose adjustment to ensure that an international normalized ratio (INR) of 2.0–3.0 is maintained [5, 6]. VKAs also interact with a range of food and drugs, resulting in an increased or decreased INR, in turn corresponding to increased risks of bleeding or thrombus formation, respectively [5, 6]. In recent years, novel oral anticoagulants (NOACs) that directly target specific components of the coagulation cascade have been developed and approved for use in a variety of indications. These include the direct activated Factor X (Factor Xa) inhibitors rivaroxaban, apixaban, and edoxaban, and the direct thrombin inhibitor dabigatran etexilate. These agents offer a number of potential advantages over VKAs, including fewer food and drug interactions and more predictable pharmacokinetics and pharmacodynamics, negating the need for routine coagulation monitoring [7, 8].
All anticoagulants, including the NOACs, increase the risk of bleeding. Therefore, their use requires careful consideration of the benefits and risks involved (i.e., risk of thromboembolic events vs. risk of bleeding events). Historically, various methods have been used to estimate benefit–risk; for example, clinical trials often report a net clinical benefit (NCB) endpoint. This is generally a composite endpoint comprising individual efficacy and safety endpoints, with the idea that the lowest rate observed reflects the optimal balance of efficacy versus safety. However, within an indication there is no consistent definition of a composite NCB endpoint, and therefore these endpoints can differ between trials. Furthermore, it is not always clear if the individual efficacy and safety endpoints included in the composite have similar clinical impact.
A useful alternative to conceptualize and compare benefits and risks between treatment modalities is the number needed (NN) approach. This can be either an NN to treat [NNT; the number of patients who must be treated to prevent one efficacy (e.g., thromboembolic or ischemic) event] or NN to harm [NNH; the number of patients who must be treated to accrue one additional adverse safety (e.g., bleeding) event] relative to the comparator therapy (usually the standard of care in any particular indication). NNT and NNH can provide a straightforward method of assessing the benefit–risk profile of one therapy versus another in a clinically relevant manner. Furthermore, such assessments conducted across different indications versus the standard of care may provide useful insights into the overall clinical potential of a particular drug.
Because thromboembolic and bleeding events vary in severity, occur in a variety of sites, and are associated with a correspondingly wide range of clinical outcomes, assessing the benefit–risk balance of NOAC therapy can be difficult. Furthermore, event rates vary according to clinical indication. From a clinical perspective, the most important events to consider are those with serious long-term sequelae; i.e., events likely to have irreversible consequences, such as stroke, pulmonary embolism (PE) resulting in pulmonary hypertension, intracranial hemorrhage (ICH), myocardial infarction (MI), bowel ischemia, or fatal events. Conversely, although other serious events (e.g., a major gastrointestinal hemorrhage) require medical intervention, they may well resolve with no long-term consequences. It may be reasonable to assume that both physicians and patients would prefer to avoid events with serious long-term consequences, even at the expense of serious events without long-term consequences. Such an approach echoes that adopted by the US Food and Drug Administration (FDA) in its consideration of the lower dose of dabigatran for use in patients with AF, where the lower dose was associated with fewer bleeding events, but more ischemic events, than the higher dose [9]. One approach to assessing benefit–risk could therefore be to consider only the events with the greatest clinical impact; i.e., those likely to have serious long-term sequelae or irreversible consequences. From a pragmatic perspective, events with lower clinical severity can be considered to have insufficient ‘weight’ to warrant consideration in a benefit–risk evaluation. For example, comparing a reduction in the risk of stroke with an increase in the risk of ICH is a clinically meaningful comparison, whereas comparing a reduction in the risk of stroke with the risk of a manageable episode of epistaxis is not. Stratification of outcomes in this way highlights the importance of comparing efficacy and safety outcomes of similar gravity when undertaking a benefit–risk evaluation.
The NNT and NNH for efficacy and safety endpoints of similar clinical severity can be applied. For example, Levitan et al. [10] conducted a detailed benefit–risk assessment of rivaroxaban versus enoxaparin for the prevention of VTE after total hip replacement (THR) or total knee replacement (TKR). In this study, NCB was interpreted as the difference between the number of efficacy events prevented and the number of safety events caused. In practice, this could be calculated as the number of events per patient over a given time, or as a rate; e.g., events per patient per year.
2 Methods
2.1 Selection of Novel Oral Anticoagulant for Study: Rivaroxaban
Rivaroxaban exerts its anticoagulant effect by directly inhibiting Factor Xa, thereby reducing the conversion of prothrombin to thrombin [11]. Owing to a high oral bioavailability (80–100 %) and predictable pharmacokinetic and pharmacodynamic properties, it can be given orally in a fixed dosing regimen without the need for routine coagulation monitoring or dose adjustment [11]. The rapid absorption of rivaroxaban ensures that maximum plasma concentrations are reached within 2–4 h of tablet intake, with moderate variability in pharmacokinetic parameters between individuals [12]. One-third of the drug is eliminated renally as unchanged drug. The remaining two-thirds is metabolized in the liver—half of which is excreted via the hepatobiliary route and half by the renal route [11].
Rivaroxaban currently has regulatory approval across the greatest number of indications of all the NOACs. In the EU and the USA, rivaroxaban is approved for the prevention of VTE in adults undergoing elective hip or knee replacement surgery, the treatment of deep vein thrombosis (DVT) and PE and the prevention of recurrent DVT/PE, and the prevention of stroke and systemic embolism in patients with non-valvular AF with one or more risk factors. These risk factors include congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, or prior stroke or transient ischemic attack. More recently, in the EU, rivaroxaban [co-administered with acetylsalicylic acid (ASA) alone or with ASA plus clopidogrel or ticlopidine] was approved for the prevention of atherothrombotic events in adult patients after an acute coronary syndrome (ACS) with elevated biomarkers [8]. In Japan, rivaroxaban is approved for stroke prevention in patients with non-valvular AF, but at a reduced dose [15 mg once daily (10 mg in patients with creatinine clearance 30–49 mL/min)] compared with the corresponding EU and US indications [13].
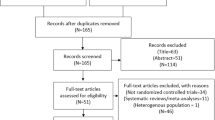
2.2 Literature Search Strategy
A PubMed literature search with the keywords ‘anticoagulants’, ‘rivaroxaban’, ‘hemorrhage’, ‘thromboembolism’ was performed in August 2013 to identify articles. Articles were deemed to be relevant for review if they were clinical trials investigating use of rivaroxaban. Only phase III trials were selected, because phase I and II trials were not powered to assess both efficacy and safety in the patient population, and phase I studies had only been performed in healthy volunteers. Field trials were also excluded because of concerns over inconsistencies in the endpoint definitions used. The author was of the opinion that a meta-analysis would not be an appropriate approach to compare clinical trials that had varying endpoint definitions and a diverse range of patient populations. Additionally, studies may have been duplicated if they were included as both meta-analyses and individual studies. The analysis in this article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by the author.
2.3 Endpoint Selection and Number Needed to Treat/Number Needed to Harm Calculation
The specific endpoints chosen were those that would fulfil the criteria of potentially long-lasting clinical impact and had been investigated in the selected clinical trials. In particular, they represented outcomes that could potentially lead to life-changing consequences. As illustrated in Table 1, the endpoints assessed varied according to indication—efficacy endpoints with fatal or life-changing outcomes included all-cause mortality, non-fatal PE, recurrent DVT, stroke, systemic embolism, and MI. The safety endpoints with potential for long-lasting clinical impact assessed included fatal bleeding and major bleeding into a critical organ. For clarity, composite endpoints, although a common assessment in clinical trials, are not included here. DVT is included because it is a significant risk factor for PE, including fatal PE. For the same reason, proximal DVT is shown (when data are available) because it carries a greater risk of PE than distal DVT [14].
Calculation of absolute risk difference (ARD) was performed by deducting the endpoint event rate of the standard of care from the rate seen with rivaroxaban treatment. Both the NNT and NNH are calculated as the reciprocal of the ARD between two treatments [15]. Although it is feasible to estimate confidence intervals if the difference in event rates between two treatments is not statistically significant [15], the null hypothesis cannot be rejected. In other words, in the absence of statistical significance, it is not possible to conclude that an observed difference is due to anything other than chance. Therefore, estimates of NNT and NNH have been provided only when there is a significant difference in outcome rates between the treatment groups.
In this article, NNT and NNH analyses—using rivaroxaban as an example and based on outcomes of similar, potentially long-lasting clinical severity—are presented for each of the aforementioned approved indications, to facilitate conceptualization of this benefit–risk approach for evaluating a NOAC versus standard of care.
3 Results
A total of nine phase III randomized controlled studies relating to rivaroxaban were identified from the literature search. These studies are grouped according to therapeutic indication below.
3.1 Prevention of Deep Vein Thrombosis After Total Knee or Hip Replacement
Patients undergoing THR or TKR require prophylactic anticoagulant therapy; the current recommendation is that this therapy should be continued for up to 35 days after surgery [16]. Rivaroxaban was approved for the prevention of VTE in patients undergoing elective THR or TKR in Canada and Europe in 2008, and in the USA in 2011. These approvals were based on the results of the phase III RECORD (REgulation of Coagulation in orthopaedic surgery to prevent Deep venous thrombosis and pulmonary embolism) program, which compared rivaroxaban (10 mg once daily) with the standard of care (the low molecular weight heparin enoxaparin) in four clinical trials. In RECORD1 and RECORD3, enoxaparin was administered at the 40 mg once daily dose started preoperatively [17, 18]. In RECORD4, a predominantly North American trial, enoxaparin was given at a dose of 30 mg twice daily [19]. RECORD2, which compared rivaroxaban 10 mg once daily (given for 31–39 days) with enoxaparin 40 mg once daily (given for 10–14 days) in patients undergoing elective THR [19], was not a drug–drug comparison but rather a regimen–regimen comparison, and is therefore not discussed further. RECORD1 enrolled patients undergoing elective THR and evaluated 31–39 days of rivaroxaban versus the same period of enoxaparin. RECORD3 and RECORD4 included patients undergoing elective TKR and evaluated 10–14 days of thromboprophylaxis with rivaroxaban or enoxaparin.
Efficacy events with (potentially) long-lasting consequences collected in the RECORD program included death, PE, and proximal DVT. Comparable bleeding events reported in the RECORD studies were fatal bleeding and major bleeding into a critical organ, defined as retroperitoneal, intracranial, intraocular, or intraspinal bleeding [17, 19].
Table 2 summarizes the event rates and absolute risk reductions for efficacy and bleeding events with (potentially) long-lasting consequences that were considered in RECORD1, RECORD3, and RECORD4 during the ‘on-treatment’ period for each study [17–19]. One question that was immediately apparent was whether to use observed event rates, irrespective of rivaroxaban versus enoxaparin statistical significance, or whether event rates should be deemed similar in the absence of statistical significance (several types of event occurred with a frequency of <1 % because only a few events were observed). Therefore, to minimize the possibility of erroneous conclusions owing to chance variations, NNTs were calculated only when statistical significance was demonstrated. These considerations were carried forward to the benefit–risk evaluations conducted for the other indications discussed.
In all three trials, rivaroxaban significantly reduced the incidence of the primary efficacy endpoint (composite of DVT, non-fatal PE, and all-cause death). Rates of major bleeding were low (<1.0 % in each treatment group), with no significant difference in rates across treatment groups. These endpoints are not shown in Table 2 because, as discussed earlier, the primary efficacy endpoint is a composite and ‘major bleeding’ includes events that are not necessarily associated with a risk of long-term sequelae. A review of events with (potentially) long-lasting consequences shows that many of the differences between treatment groups did not attain statistical significance (Table 2), probably owing to the low numbers of events for these individual endpoints. However, rates of bleeding events with (potentially) long-lasting consequences were consistently low at ≤0.1 %, suggesting an NNH of approximately 1000. Conversely, with the exception of a slight, non-significant increase in PE (0.2 %) in RECORD1, ARDs for efficacy reductions consistently favored rivaroxaban, albeit with few significant differences. Furthermore, calculations of NNT and NNH for the non-significant ARDs in Table 2 (not shown) yielded results broadly consistent with previous estimates of NNT for the composite of symptomatic VTE and all-cause death, and for non-fatal major bleeding [10].
Therefore, when rivaroxaban is used for the prevention of VTE after THR or TKR, the overall data suggested a benefit–risk profile that was at least similar to, and possibly better than, enoxaparin with regard to events with (potentially) long-lasting consequences. This conclusion is also consistent with the results for the primary efficacy and safety outcomes.
3.2 Treatment of Venous Thromboembolism and Prevention of Recurrent Venous Thromboembolism
The management of VTE consists of two phases: an acute phase to address the existing clot and a long-term secondary prevention phase intended to prevent recurrence. Standard treatment includes an initial period of treatment with a low molecular weight heparin, followed by treatment with a VKA. Phase II studies in patients with acute VTE indicated that a single-drug approach with rivaroxaban was possible, with the use of an initial phase of greater intensity followed by a lower dose for longer-term secondary prevention [20, 21]. Hence, the protocol taken forward for phase III evaluation was rivaroxaban 15 mg twice daily for 3 weeks followed by 20 mg once daily for the secondary prevention phase. The phase III evaluation of rivaroxaban for the treatment and prevention of recurrent VTE included two pivotal trials: EINSTEIN DVT [22] and EINSTEIN PE [23]. In both of these trials, the primary efficacy endpoint was a composite of symptomatic recurrent DVT and symptomatic fatal or non-fatal PE. The former study enrolled patients with acute symptomatic DVT but without symptomatic PE, whereas the latter enrolled patients with acute symptomatic PE, with or without DVT. The (EINSTEIN EXT) study included patients from EINSTEIN DVT and EINSTEIN PE, as well as patients from routine care, who had confirmed symptomatic DVT or PE and who had been treated for 6–12 months with either a VKA or rivaroxaban. Patients were randomly assigned to receive continued treatment with rivaroxaban or placebo [22].
The EINSTEIN DVT and EINSTEIN PE trials used identical study designs, treatment regimens, and outcome definitions to allow a pre-specified pooled analysis to be conducted on patient-level data [24]. This analysis was performed to permit greater precision in the estimation of efficacy and safety endpoints. Efficacy and safety events with (potentially) long-lasting consequences obtained for this indication are listed in Table 1, and results for these events, from the pooled analysis, are shown in Table 3 [22–24].
Unfortunately, separate rates for distal and proximal recurrent DVT have not been published, and therefore total rates for recurrent DVT are shown. Examination of the data in Table 3 suggested a broad overall similarity in benefit versus risk for events with (potentially) long-lasting consequences. However, no p values for the ARDs for these outcomes were reported in the pooled analysis, although observed values suggest NNTs of 313 for recurrent DVT and 244 for critical-site bleeding (Table 3).
These results were consistent with the finding of non-inferiority of rivaroxaban for efficacy in both the EINSTEIN DVT and EINSTEIN PE trials and the low and similar rates of major bleeding in EINSTEIN DVT, compared with standard treatment. However, the rate of major bleeding in EINSTEIN PE was significantly lower with rivaroxaban (hazard ratio 0.49; p = 0.003). Major bleeding was also significantly reduced in the pooled analysis compared with standard treatment, driven mainly by reductions in ICH (5 vs. 13) and retroperitoneal bleeding (1 vs. 8), as well as reductions in gastrointestinal bleeding (15 vs. 26) [24]. Furthermore, both trials evaluated an NCB endpoint; this was the composite of VTE and major bleeding. In EINSTEIN DVT, this was significantly reduced with rivaroxaban versus standard therapy (hazard ratio 0.67; p = 0.03); in EINSTEIN PE, the difference between treatment groups was not significant. In the continued-treatment EINSTEIN EXT study, rivaroxaban demonstrated superior efficacy compared with placebo (hazard ratio 0.18; p < 0.001), and a similar rate of major bleeding (4 vs. 0 events; p = 0.11).
3.3 Reducing the Risk of Stroke in Non-Valvular Atrial Fibrillation
The ROCKET AF (Rivaroxaban Once daily oral direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation) study was a large, randomized evaluation of the efficacy and safety of rivaroxaban versus warfarin in reducing the risk of stroke in patients with non-valvular AF [25]. Over 14,000 patients with a mean CHADS2 (congestive heart failure, hypertension, age ≥ 75 years, diabetes mellitus, stroke, or transient ischemic attack (2 points)) score of 3.5 were randomized to either rivaroxaban 20 mg once daily (15 mg once daily in patients with moderate renal impairment; i.e., creatinine clearance 30–49 mL/min) or dose-adjusted warfarin (target INR 2.0–3.0). The primary efficacy endpoint was stroke or systemic embolism, and the principal safety outcome was the composite of major and non-major clinically relevant bleeding. The study was designed to assess non-inferiority of rivaroxaban compared with standard treatment. Superiority testing was performed after the successful demonstration of non-inferiority. The median duration of assigned therapy was 590 days, and the median follow-up period was 707 days. To best reflect the balance between different therapies during actual use, the data presented for this benefit–risk evaluation are taken from the on-treatment analyses. J-ROCKET AF (Japan Rivaroxaban Once Daily, Oral, Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation) was a separate trial specifically for Japanese patients with AF, because they were not included in the global ROCKET AF study. Patients enrolled in J-ROCKET AF received lower doses of rivaroxaban (15 mg once daily; 10 mg once daily in patients with moderate renal impairment) and dose-adjusted warfarin (target INR 2.0–3.0 in patients <70 years or 1.6–2.6 in patients aged ≥70 years) than patients in the global study [26]. The primary efficacy and safety endpoints were the same in both studies.
Efficacy and safety events with (potentially) long-lasting consequences evaluated for benefit–risk for stroke risk reduction are shown in Table 1; these include stroke, systemic embolism, MI, and all-cause death. Safety outcomes included fatal bleeding and bleeding into a critical site (bleeding into intracranial, intraspinal, intraocular, pericardial, intra-articular, intramuscular with compartment syndrome, or retroperitoneal sites [25]). In the ROCKET AF trial, hemorrhagic stroke was counted as both an efficacy event and a safety event. To clearly distinguish between efficacy and safety events, hemorrhagic stroke was not included in the efficacy evaluation (Table 4) [25]. Conversely, critical-site bleeding included ICH, which in turn included hemorrhagic stroke. Inspection of the data for efficacy and safety events with (potentially) long-lasting consequences (Table 4) shows a reduction in event rates with rivaroxaban versus warfarin for all efficacy endpoints, although statistical significance was only attained for reduction in systemic embolism. However, the rates of both critical-site hemorrhages and fatal bleeding are significantly reduced with rivaroxaban compared with warfarin. The ARD for all-cause death exceeded that for systemic embolism but did not attain statistical significance (p = 0.07). Had it been significant, the NNT would have been 294, similar to the NNTs for fatal bleeding (NNT = 333) and critical-site bleeding (NNT = 250) (Table 4). In J-ROCKET AF statistical significance was not reported or not obtained for efficacy and safety endpoints (Table 4).
These data clearly indicate a favorable benefit–risk balance for rivaroxaban versus warfarin for most serious events when used to reduce the risk of stroke in patients with AF.
3.4 Secondary Prevention After Acute Coronary Syndrome
Rivaroxaban 2.5 mg twice daily, co-administered with ASA alone or ASA plus clopidogrel or ticlopidine, is approved in Europe for the prevention of atherothrombotic events in adult patients with elevated cardiac biomarkers after an ACS [8]. The approval was based on the results of the phase III ATLAS ACS 2 TIMI 51 (Anti-Xa Therapy to Lower cardiovascular events in Addition to standard therapy in Subjects with Acute Coronary Syndrome–Thrombolysis in Myocardial Infarction 51) trial [27], in which over 15,500 patients with a recent ACS were randomized (<7 days after hospital admission) to 2.5 or 5 mg rivaroxaban twice daily, or to placebo in addition to the standard of care at the time (low-dose ASA with or without a thienopyridine, selected prior to randomization) for up to 31 months after the index event (mean duration: 13.1 months). Dose selection for this phase III study was based on the earlier results of the phase II dose-finding ATLAS ACS TIMI 46 study [28]. The primary efficacy endpoint for the ATLAS ACS 2 TIMI 51 trial was the composite of cardiovascular death, MI, or stroke. The principal safety outcome was thrombolysis in MI major bleeding not related to coronary artery bypass grafting. At the time the study was initiated, ticagrelor and prasugrel were not available, and therefore the specified antiplatelet agents were restricted to ASA with or without a thienopyridine (i.e., clopidogrel or ticlopidine).
Events with (potentially) long-lasting consequences evaluated for the use of rivaroxaban for secondary prevention after an ACS are listed in Table 1. These include MI, stroke, and death for efficacy events, and critical-site bleeding (intracranial, intraspinal, intraocular, pericardial, intra-articular, intramuscular with compartment syndrome, or retroperitoneal bleeding [29]) and fatal bleeding for safety events. Unfortunately, data for critical-site bleeding per se are yet to be published, and therefore data for ICH are shown in lieu. Furthermore, to minimize the impact of including hemorrhagic stroke under both stroke and ICH, ischemic stroke only is shown under efficacy. Because only the 2.5 mg twice-daily dose was approved for clinical use, the benefit–risk evaluation presented in Table 5 is based solely on data for this dosing regimen [27].
Corresponding results for events with (potentially) long-lasting consequences are shown in Table 5 and combine data for both strata [background therapy of ASA alone (Stratum 1) or ASA plus a thienopyridine (clopidogrel or ticlopidine) (Stratum 2)]. In total, 93 % of patients received dual antiplatelet therapy rather than ASA alone [28].
The data in Table 5 demonstrate an overall favorable benefit–risk profile for rivaroxaban with regard to events with (potentially) long-lasting consequences. Results for ischemic stroke, MI, and fatal bleeding are broadly similar between rivaroxaban and placebo groups. Although the incidence of ICH is significantly increased with rivaroxaban, the NNH (500 per 24 months) is markedly higher than the NNT (63 per 24 months) for all-cause death. In other words, the increased risk of ICH appears to be more than offset by the significant decrease in all-cause death, especially when the lack of any increase in fatal bleeding is also considered.
4 Discussion
Anticoagulant therapy poses a risk of increased bleeding, the most feared manifestation of which is ICH [30]. As such, it is not always clear whether the benefit of anticoagulant therapy—i.e., the reduction of thromboembolic events—is ‘worth’ the increased risk of bleeding. To balance benefit against risk, physicians are faced with a need to consider which kinds of efficacy events can be reduced and which kinds of bleeding events are likely to be increased. This article has presented an approach to this problem by focusing solely on those events with a significant risk of mortality or long-term morbidity. Therefore, the evaluation of benefit–risk is reduced to the consideration of just those events of the greatest clinical severity (i.e., those likely to have serious long-term consequences for the patient). By contrast, events that, although serious, are likely to resolve fully are not considered in this approach. For example, a major gastrointestinal hemorrhage, if not fatal, has a good probability of full resolution despite the need for substantial medical intervention at the time. Conversely, ICH has a high case–fatality rate and, if not fatal, usually results in significant disability and morbidity. Essentially, this viewpoint can be construed as an adaptation of the maxim ‘first do no harm’, with ‘harm’ here referring to long-lasting consequences. The approach has been illustrated with clinical trial data for rivaroxaban because this drug has the greatest number of approved indications among the NOACs. However, the same approach should be applicable to assessing benefit–risk for any anticoagulant.
On the basis of available data, although the results presented on VTE prevention after elective THR or TKR indicate that events with (potentially) long-lasting consequences were too infrequent to generate statistically significant differences between treatment groups for any of the efficacy outcomes, all efficacy ARDs (with one exception) favored rivaroxaban (Table 2). Corresponding bleeding events (fatal or critical organ bleeding) occurred in no more than 0.13 % of patients. However, absolute risk reductions for efficacy events with rivaroxaban versus enoxaparin generally exceeded this figure, suggesting that the benefit–risk balance for rivaroxaban regarding events with (potentially) long-lasting consequences was at least similar to that of enoxaparin and may even be better, although larger studies are required to confirm such a conclusion. Additional results (Table 3) suggest that, for events with (potentially) long-lasting consequences, rivaroxaban has a broadly similar benefit–risk balance versus an active comparator in the treatment and secondary prevention of VTE.
Rivaroxaban also has a favorable benefit–risk balance versus an active comparator when used for stroke risk reduction in patients with AF. All ARDs, for both efficacy and safety, favored rivaroxaban, which demonstrated an NNT of approximately 300 per year for the prevention of one fatality or one critical-site bleeding event: 294 per year for the prevention of all-cause death, 250 per year for the prevention of a critical-site bleeding event, or 333 per year for the prevention of a fatal bleeding event (Table 4). A favorable benefit–risk balance was also observed versus placebo for the reduction of recurrent events after ACS, with the NNT for a reduction in all-cause death markedly lower than the NNH for an increase in ICH (Table 5).
5 Limitations of the Study
There are several limitations associated with the approach taken in this study. First, analysis of selected endpoints is restricted to those for which published data are available. In some instances, only one endpoint was usable, as was the case for ICH in lieu of critical-site bleeding in the ACS evaluation (Table 5).
Second, this article has adopted the conservative approach of estimating NNT/NNH only when the rate difference between treatment groups for the particular endpoint was statistically significant, as opposed to calculating NNT/NNH on the basis of observed rate differences irrespective of statistical significance. This was done to minimize the possibility of an erroneous conclusion owing to chance variation. However, the result is that the effect of events occurring at a lower rate may be underestimated because statistical significance may not have been achieved, even if a larger study would have demonstrated significance. This concern is exacerbated when considering benefit–risk evaluations using data from subgroup analyses of clinical trials. Additionally, particular subgroups may have a different level of risk for events relative to the overall population.
A related concern is that only six of the 31 ARDs presented in Tables 2, 3, 4 and 5 were reported as statistically significant, perhaps owing to patient numbers being too low, or simply because p values were not reported in the publication. However, non-significant differences between therapies also suggest that the two therapies have similar outcomes for a number of endpoints.
Third, it should be noted that for rate-based ARDs (Tables 4, 5), different methods may be employed for calculating the NNT [31] depending on the data available.
Fourth, although minor events may not directly result in long-term consequences, they may persuade some patients to discontinue anticoagulant therapy, resulting in an increased risk of thromboembolic events.
Finally, the illustrative benefit–risk evaluations presented in this article are based on phase III clinical trial data. The extent to which such study data correspond to event rates seen in routine clinical practice remains to be confirmed.
Although other methods have been used for assessing benefit–risk (e.g., use of composite NCB endpoints), the NNT method remains a simple-to-understand approach for visualizing the clinical impact of various therapeutic interventions because it permits a direct comparison of the ‘benefit’ effect (NNT) and the ‘risk’ effect (NNH), providing the comparison is for events of similar clinical impact. Of note, these comparisons are based on population-level data and may or may not be appropriate for the clinical situation of individual patients.
6 Conclusions
In the case of rivaroxaban, the approach described in this article suggests a broadly favorable benefit–risk profile across multiple clinical indications for those events of the greatest clinical impact, and therefore the greatest concern to patients. Despite its limitations, this approach offers a potentially useful addition to the difficult task of assessing the benefit–risk of anticoagulant therapy, and may also inform discussions on issues such as formulary acceptance for rivaroxaban and other multi-indication anticoagulants.
Overall, this approach has the potential to contribute to the ongoing debate on how best to optimize anticoagulant therapy and how to limit the occurrence of the most serious events for patients.
References
Fareed J, Adiguzel C, Thethi I. Differentiation of parenteral anticoagulants in the prevention and treatment of venous thromboembolism. Thromb J. 2011;9(1):5.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146(12):857–67.
Linkins LA. Bleeding risks associated with vitamin K antagonists. Blood Rev. 2013;27(3):111–8.
Akwaa F, Spyropoulos AC. Treatment of bleeding complications when using oral anticoagulants for prevention of strokes. Curr Treat Options Cardiovasc Med. 2013;15(3):288–98.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians evidence-based clinical practice guidelines (8th Edition). Chest. 2008;133(6 Suppl):160S–98S.
Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti G. Oral anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):44S–88S.
Janssen Pharmaceuticals Inc. Xarelto® prescribing information. 2015. http://www.xareltohcp.com/sites/default/files/pdf/xarelto_0.pdf. Accessed 9 June 2015.
Bayer Pharma AG. Xarelto® summary of product characteristics. 2015. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000944/WC500057108.pdf. Accessed 15 July 2015.
Beasley BN, Unger EF, Temple R. Anticoagulant options—why the FDA approved a higher but not a lower dose of dabigatran. N Engl J Med. 2011;364(19):1788–90.
Levitan B, Yuan Z, Turpie AGG, Friedman RJ, Homering M, Berlin JA, et al. Benefit–risk assessment of rivaroxaban versus enoxaparin for the prevention of venous thromboembolism after total hip or knee arthroplasty. Vasc Health Risk Manag. 2014;10:157–67.
Kreutz R. Pharmacodynamic and pharmacokinetic basics of rivaroxaban. Fundam Clin Pharmacol. 2012;26(1):27–32.
Mueck W, Stampfuss J, Kubitza D, Becka M. Clinical pharmacokinetic and pharmacodynamic profile of rivaroxaban. Clin Pharmacokinet. 2014;53(1):1–16.
Okata T, Toyoda K, Okamoto A, Miyata T, Nagatsuka K, Minematsu K. Anticoagulation intensity of rivaroxaban for stroke patients at a special low dosage in Japan. PLoS One. 2014;9(11):e113641.
Bates SM, Jaeschke R, Stevens SM, Goodacre S, Wells PS, Stevenson MD, et al. American College of Chest Physicians. Diagnosis of DVT: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e351S–e418S.
Altman DG. Confidence intervals for the number needed to treat. BMJ. 1998;317(7168):1309–12.
Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. American College of Chest Physicians. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e278S–e325S.
Eriksson BI, Borris LC, Friedman RJ, Haas S, Huisman MV, Kakkar AK, et al. RECORD1 Study Group. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008;358(26):2765–75.
Lassen MR, Ageno W, Borris LC, Lieberman JR, Rosencher N, Bandel TJ, et al. RECORD3 Investigators. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med. 2008;358(26):2776–86.
Turpie AGG, Lassen MR, Davidson BL, Bauer KA, Gent M, Kwong LM, et al. RECORD4 Investigators. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD4): a randomised trial. Lancet. 2009;373(9676):1673–80.
Agnelli G, Gallus A, Goldhaber SZ, Haas S, Huisman MV, Hull RD, et al. ODIXa-DVT Study Investigators. Treatment of proximal deep-vein thrombosis with the oral direct Factor Xa inhibitor rivaroxaban (BAY 59-7939): the ODIXa-DVT (Oral Direct Factor Xa Inhibitor BAY 59-7939 in patients with acute symptomatic Deep-Vein Thrombosis) study. Circulation. 2007;116(2):180–7.
Buller HR, Lensing AWA, Prins MH, Agnelli G, Cohen A, Gallus AS, et al. Einstein-DVT Dose-Ranging Study investigators. A dose-ranging study evaluating once-daily oral administration of the Factor Xa inhibitor rivaroxaban in the treatment of patients with acute symptomatic deep vein thrombosis: the Einstein-DVT Dose-Ranging Study. Blood. 2008;112(6):2242–7.
The EINSTEIN Investigators Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363(26):2499–510.
The EINSTEIN–PE Investigators. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366(14):1287–1297.
Prins MH, Lensing AWA, Bauersachs R, van Bellen B, Bounameaux H, Brighton TA, et al. EINSTEIN Investigators. Oral rivaroxaban versus standard therapy for the treatment of symptomatic venous thromboembolism: a pooled analysis of the EINSTEIN-DVT and PE randomized studies. Thromb J. 2013;11(1):21.
Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Hori M, Matsumoto M, Tanahashi N, Momomura S, Uchiyama S, Goto S, et al. J-ROCKET AF study investigators. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation—the J-ROCKET AF study. Circ J. 2012;76(9):2104–11.
Mega JL, Braunwald E, Wiviott SD, Bassand JP, Bhatt DL, Bode C, et al. ATLAS ACS 2–TIMI 51 Investigators. Rivaroxaban in patients with a recent acute coronary syndrome. N Engl J Med. 2012;366(1):9–19.
Mega JL, Braunwald E, Mohanavelu S, Burton P, Poulter R, Misselwitz F, et al. ATLAS ACS-TIMI 46 study group. Rivaroxaban versus placebo in patients with acute coronary syndromes (ATLAS ACS-TIMI 46): a randomised, double-blind, phase II trial. Lancet. 2009;374:29–38.
Gibson CM, Mega JL, Burton P, Goto S, Verheugt F, Bode C, et al. Rationale and design of the Anti-Xa Therapy to Lower cardiovascular events in Addition to standard therapy in Subjects with Acute Coronary Syndrome-Thrombolysis in Myocardial Infarction 51 (ATLAS-ACS 2 TIMI 51) trial: a randomized, double-blind, placebo-controlled study to evaluate the efficacy and safety of rivaroxaban in subjects with acute coronary syndrome. Am Heart J. 2011;161(5):815–21.
Paciaroni M, Agnelli G. Should oral anticoagulants be restarted after warfarin-associated cerebral haemorrhage in patients with atrial fibrillation? Thromb Haemost. 2014;111(1):14–8.
Altman DG, Andersen PK. Calculating the number needed to treat for trials where the outcome is time to an event. BMJ. 1999;319(7223):1492–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The analysis in this article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by the author.
Acknowledgments
The author would like to acknowledge Jo Luscombe of Chameleon Communications International Ltd, who provided medical writing services with funding from Bayer HealthCare Pharmaceuticals and Janssen Scientific Affairs, LLC. The named author meets the ICMJE (International Committee of Medical Journal Editors) criteria for authorship for this manuscript, takes responsibility for the integrity of the work as a whole, and has given final approval to the version to be published.
Conflict of interest
Professor Ageno received honoraria from Bayer, Boehringer Ingelheim, Daiichi Sankyo, Bristol-Myers Squibb, and Pfizer for participation in Advisory Boards and support for attendance at educational and scientific meetings.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ageno, W. Rivaroxaban: An Evaluation of its Cardiovascular Benefit–Risk Profile Across Indications Based on Numbers Needed to Treat or Harm, and on Clinically Meaningful Endpoint Comparisons. Drugs R D 15, 295–306 (2015). https://doi.org/10.1007/s40268-015-0105-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-015-0105-9