Abstract
Objective
Gabapentin is being investigated as a potential treatment for occasional disturbed sleep. This study assessed the pharmacokinetics and tolerability of gabapentin 500 mg and the commonly prescribed sedative/hypnotic zolpidem tartrate 10 mg, administered separately and in combination.
Methods
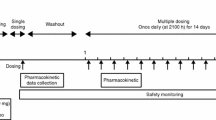
Forty healthy participants (19 male, 21 female) were randomized into this three-period crossover study [mean (range) age 34.1 (18–45) years, weight 68.3 (51.4–92.7) kg; 60 % white]. Participants were dosed with gabapentin alone (n = 39), zolpidem tartrate alone (n = 38), and the combination (gabapentin + zolpidem) (n = 38) over three treatment periods, which were separated by ≥7 days. Blood samples were collected pre-dose and 0.5, 1, 1.5, 2, 3, 4, 6, 8, 10, 12, 18, 24 and 36 h post-dose. Plasma concentrations of each drug were assayed using validated methods. Pharmacokinetic parameters were estimated from plasma concentration–time data using standard non-compartmental methods.
Results
For gabapentin + zolpidem combination versus gabapentin alone, mean pharmacokinetic parameters were peak plasma concentration (C max) 4.61 versus 4.72 µg/mL, time to Cmax (t max) 4.63 versus 3.64 h and the area under plasma concentration–time curve extrapolated to infinity (AUC0–∞) 53.4 versus 51.0 µg h/mL. For the combination versus zolpidem alone, mean pharmacokinetic parameters were C max 154 versus 138 ng/mL, t max 1.45 versus 1.84 h and AUC0–∞ 912 versus 854 ng h/mL. The 90 % confidence intervals for C max (rate of absorption) and AUC0–∞ (extent of absorption) comparing the combination versus single drug administration fell within the 80–125 % range accepted for bioequivalence. All treatments were well tolerated.
Conclusion
The pharmacokinetics of gabapentin 500 mg and zolpidem tartrate 10 mg are unaffected when both drugs are taken simultaneously, compared with each drug taken alone.
Similar content being viewed by others
1. This bioequivalence study demonstrates that the pharmacokinetic properties of gabapentin 500 mg and zolpidem tartrate 10 mg are unaffected when both treatments are taken simultaneously, compared with each drug taken alone, in healthy participants. |
2. Both treatments were well tolerated when taken alone and in combination, in a population of healthy participants. |
1 Introduction
Gabapentin was first developed to treat seizure disorders and neuropathic pain, and is now being investigated as a potential sleep aid for occasional disturbed sleep. Studies suggest that low-dose gabapentin (250 mg [1, 2] and 500 mg [2]) can improve objective and subjective measures of sleep in adults using a model of occasional disturbed sleep [1, 2]. The exact mechanism by which gabapentin improves sleep is unknown, but is likely related to its well-characterized binding affinity to the α2δ subunit of voltage-activated calcium channels, and subsequent modulatory effects on neurotransmitter release [3, 4]. The pharmacokinetic profile of gabapentin as an immediate-release formulation has been well defined across the therapeutic dose range (300–1,800 mg/day, with a recommended dose of 900–1,800 mg/day for approved indications). For example, after single-dose oral administration (300 or 600 mg) [5–7], gabapentin reaches peak plasma concentration (C max) in 2–3 h [time to reach C max (t max)] [5, 8], and with multiple dosing, achieves steady state within 24–48 h [8]. Plasma concentrations of gabapentin do not increase proportionally with increasing doses owing to absorption in only a limited segment of the small intestine. Gabapentin is eliminated unchanged through the kidney, with a terminal half-life (t ½) of 5–7 h [8]. Gabapentin is largely unaffected by alteration in hepatic function or cytochrome P450 (CYP450) activity [6, 9], and there are few known drug–drug interactions, including no interaction observed with other antiepileptic drugs (lamotrigine, vigabatrin or oxcarbazepine) [10] or with a contraceptive regimen of norethindrone acetate and ethinyl estradiol [11]. The most common adverse events (AEs) observed following treatment with gabapentin (900–1,800 mg/day) (not seen at an equivalent frequency among placebo-treated patients) were dizziness, somnolence and peripheral edema in adults with post-herpetic neuralgia, and somnolence, dizziness, ataxia, fatigue and nystagmus in adults with partial seizures with and without secondary generalization [12]. Gabapentin’s overall pharmacokinetic and pharmacodynamic profile makes for a predictable and well-tolerated drug.
There is potential for individuals with sleep disturbances to self-medicate with multiple sleep products. Zolpidem, an imidazopyridine agent, is widely prescribed for the short-term management of insomnia [13]. Zolpidem demonstrates preferential affinity for GABAA receptors containing the α1 subunit [14]. It is absorbed rapidly, with bioavailability of 70 %, and reaches C max in <1 h [15]. Zolpidem shows linear pharmacokinetics across the 5 to 20-mg therapeutic dose range. In addition, zolpidem is rapidly metabolized before being eliminated primarily in bile, urine and feces [15, 16]. Because metabolism occurs via successive CYP450 enzymes, zolpidem has a high potential for drug–drug interactions with agents that inhibit or induce CYP450 enzymes. Although gabapentin is not metabolized via the CYP450 pathway [17], there is potential for co-administration with gabapentin, and therefore, any potential effects of zolpidem on the pharmacokinetic properties of gabapentin, and vice versa, warrant investigation. The aim of this study was to evaluate a potential drug–drug interaction of gabapentin with zolpidem in healthy participants, when administered individually and in combination.
2 Methods
2.1 Study Design
Participants were randomized in an open-label, three-period crossover design to single-dose gabapentin (500 mg), zolpidem tartrate (10 mg), and the combination (gabapentin 500 mg + zolpidem tartrate 10 mg), between November 5 and 21, 2001. There was a minimum of 7 days between treatment periods. Eligibility was determined at screening. Blood and urine tests were conducted and analyzed at screening and at each visit. The study was conducted in compliance with the Declaration of Helsinki and the International Conference on Harmonisation Good Clinical Practice Guidelines. Protocol, consent documents and protocol amendments were all approved by the relevant institutional review board at participating centers. The study is not registered on http://clinicaltrials.gov.
2.2 Participants
All participants provided written, informed consent prior to randomization. Healthy men and women (of non-child-bearing potential or those using an acceptable contraceptive) aged ≥18 years and weighing 50–100 kg (110–220 lbs) were recruited. Participants were considered healthy if they had no clinically relevant abnormalities on physical examination. Standard exclusion criteria were imposed, including, but not limited to, participants with a known sensitivity to either drug; a positive pregnancy test on screening; a history of drug or alcohol abuse; or on physical examination, any clinically significant disease or abnormality that was deemed likely to affect the properties of either drug under investigation.
2.3 Analysis of Plasma Samples
Venous blood (210 mL per participant) was collected in heparinized collection tubes pre-dose (0 h) and at 0.5, 1, 1.5, 2, 3, 4, 6, 8, 10, 12, 18, 24 and 36 h post-dose. Samples were centrifuged and the plasma stored in labeled, screw-capped, polypropylene tubes at −20 °C within 1 h of collection. Gabapentin plasma concentrations were determined by validated liquid chromatography tandem mass spectrometry methods using 1-(amino-methyl)-cycloheptaneacetic acid (PD0403609-0000) as an internal standard (BioAssay Laboratories, Houston, TX, USA). The analytical range for detection of gabapentin was 0.025–10.0 µg/mL, with precision [% coefficient of variation (CV)] ≤15.5 % and accuracy [% relative error (RE)] of 0.2–6.7 %. Zolpidem plasma concentrations were determined by a validated high-throughput liquid chromatography (HPLC) with fluorescence detection, using trazodone as an internal standard (Covance Laboratories, Inc., Madison, WI, USA). The analytical range of detection for zolpidem was 1.00–400 ng/mL, with precision (% CV) ≤14 % and accuracy (% RE) of 2.0–5.0 %.
2.4 Pharmacokinetic Parameters
Non-compartmental methods were employed to estimate pharmacokinetic parameters. The C max and t max were observed directly from the plasma concentration–time profile of each participant. The area under the concentration–time curve from time zero to time of last quantifiable concentration (tlqc) (AUC0–tlqc) was evaluated using the linear trapezoidal method. The area was extrapolated to infinity, AUC0–∞, using standard methods. The t ½ was calculated using the terminal rate constant determined from the terminal log-linear phase of the concentration–time profile. Pharmacokinetic analyses were carried out using WinNonlin® software Pro Version 2.1. Quality control samples were used in each analytical run to ensure data quality. Data were reviewed and accepted by quality-control specialists before being used for pharmacokinetic analyses.
2.5 Safety and Tolerability
All randomized participants were evaluated for safety. Safety evaluations were conducted throughout the study and included monitoring of AEs, vital signs, 12-lead electrocardiograms, and physical examination including blood pressure, respiratory, and pulse rate. Laboratory tests were conducted at screening only.
2.6 Statistical Analyses
A sample size of 36 participants completing the study was estimated on the basis of estimates of intra-subject CV for zolpidem 10 mg, which is larger than that for gabapentin [18, 19]. The sample size provided at least 80 % power to demonstrate bioequivalence with respect to AUC0–∞ and C max, assuming a CV of 33 % and no underlying difference between the combination and each drug administered alone.
Pharmacokinetic analyses were based on participants who completed each treatment period. Log-transformed AUC0–∞ and C max were analyzed using analysis of variance (ANOVA) with treatment sequence, period and treatment as fixed effects and subject-within-sequence as a random effect. Results from the ANOVA were used to calculate 90 % confidence intervals (CIs) for the ratios (test/reference) of least-squares mean treatment values, where administration of gabapentin and zolpidem together was the test treatment and administration of gabapentin alone and zolpidem alone were the reference treatments. Lack of an interaction was concluded if the estimated 90 % CIs for the ratios (test/reference) of adjusted means for both AUC0–∞ and C max fell within the 80–125 % accepted range for bioequivalence.
3 Results
3.1 Study Population
Forty participants were enrolled and randomized. Thirty-six participants completed the study with no protocol deviations. Three participants were withdrawn because of positive urine drug screens (one prior to the second treatment period and two prior to the third treatment period), and one participant did not return for the third treatment period. Because of these withdrawals, 39 participants received gabapentin (500 mg), 38 received zolpidem tartrate (10 mg), and 38 received the combination and were included in the pharmacokinetic analyses (Table 1). During the study, no participant took or received concomitant therapy that was judged to have the potential to affect pharmacokinetic parameters.
3.2 Pharmacokinetic Analyses
The mean plasma concentration–time profiles for gabapentin and zolpidem following administration alone or in combination are shown in Figs. 1 and 2, respectively. For gabapentin + zolpidem combination versus gabapentin alone, the mean pharmacokinetic parameters were C max 4.61 versus 4.72 µg/mL, t max 4.63 versus 3.64 h and AUC0–∞ 53.4 versus 51.0 µg h/mL (Table 2). The 90 % CIs for the treatment ratio of C max (92.0–102.0) and AUC0–∞ (99.0–109.0) for the combination versus gabapentin alone were within the 80–125 % range accepted for bioequivalence (Table 2). For the combination versus zolpidem alone, the mean pharmacokinetic parameters were C max 154.0 versus 138.0 ng/mL, t max 1.45 versus 1.84 h and AUC0–∞ 912.0 versus 854.0 ng h/mL (Table 3). The 90 % CIs for the treatment ratio of C max (104.0–118.0) and AUC0–∞ (98.1–112.0) for the combination versus zolpidem alone were within the 80–125 % range accepted for bioequivalence (Table 3). The t ½ of gabapentin or zolpidem was also similar when administered alone versus in combination, and averaged ~5.5 h for gabapentin and 3.4 h for zolpidem.
3.3 Safety and Tolerability
Co-administration of gabapentin and zolpidem was well tolerated. Five participants reported seven treatment-emergent AEs; all were mild in severity (Table 4). No deaths, serious or severe AEs, or discontinuations due to AEs were reported. In addition, no clinically significant changes in vital signs were recorded pre- versus post-study.
4 Discussion
Gabapentin is being investigated as a potential sleep aid for occasional disturbed sleep on the basis of clinical evidence from healthy volunteers and patients with insomnia [1, 2, 20–23]. The present study demonstrated that the pharmacokinetics of gabapentin (500 mg) and a commonly prescribed prescription sleep aid, zolpidem tartrate (10 mg), were unaffected when both drugs were administered simultaneously, compared with each drug taken alone. In addition, both drugs at the doses stated were well tolerated when taken alone or in combination in this group of healthy individuals.
Zolpidem is widely prescribed in clinical practice for short-term management of insomnia, and is generally safe and well tolerated [24, 25]. Although not recommended, the nature of occasional sleep disturbance may result in individuals self-medicating with multiple sleep aids to improve sleep [26, 27]. Of concern, many prescription sleep aids are associated with significant residual next-day effects due to long half-lives [28], which could be further prolonged with a change to the pharmacokinetic elimination parameters. Our data demonstrate that administration of gabapentin with zolpidem was bioequivalent to administration of gabapentin alone, as the 90 % CIs for C max (rate of absorption) and AUC0–∞ (extent of absorption) comparing single drug administration versus each drug administered in combination were within the 80–125 % range accepted for bioequivalence. Bioequivalence was also achieved for administration of zolpidem with gabapentin versus zolpidem alone. In addition, administration of gabapentin or zolpidem alone or in combination did not change the t ½ for either drug. Therefore, no prolonging of next-day effects of zolpidem would be expected, although pharmacodynamic studies would be needed to confirm this assumption. Overall, our study found no new safety signals for single-dose use of these two drugs when co-administered.
Our observations also support what is known about the pharmacokinetic properties of both drugs, as drug–drug interactions would not be expected between gabapentin and zolpidem. For example, zolpidem is metabolized via CYP3A4, and acts as a mild mechanism-based inactivator of human CYP3A in vitro [29, 30]. In contrast, gabapentin is non-metabolized and is eliminated renally primarily as unchanged drug, showing plasma clearance that is proportional to creatinine clearance [6]. It should be noted that the present study was conducted in a small study population of healthy individuals, using only a single dose, and should be interpreted in light of this. In addition, our observations might not be extrapolated to elderly participants, or those with reduced renal function, as data have shown that age-related changes in renal function can alter the pharmacokinetics of gabapentin [31, 32].
5 Conclusions
The pharmacokinetic properties of gabapentin 500 mg and zolpidem tartrate 10 mg are unaffected when both treatments are taken simultaneously, compared with each treatment taken alone. All treatments were well tolerated when taken alone or in combination in this study population.
References
Furey SA, Hull SG, Leibowitz MT, Jayawardena S, Roth T. A randomized, double-blind, placebo-controlled, multicenter, 28-day, polysomnographic study of gabapentin in transient insomnia induced by sleep phase advance. J Clin Sleep Med. 2014;10:1101–9.
Rosenberg RP, Hull SG, Lankford DA, Mayleben DW, Seiden DJ, Furey SA, et al. A randomized, double-blind, single-dose, placebo-controlled, multicenter, polysomnographic study of gabapentin in transient insomnia induced by sleep phase advance. J Clin Sleep Med. 2014;10:1093–100.
Gee NS, Brown JP, Dissanayake VU, Offord J, Thurlow R, Woodruff GN. The novel anticonvulsant drug, gabapentin (Neurontin), binds to the alpha2delta subunit of a calcium channel. J Biol Chem. 1996;271:5768–76.
Taylor CP. Mechanisms of analgesia by gabapentin and pregabalin—calcium channel alpha2-delta [Cavalpha2-delta] ligands. Pain. 2009;142:13–6.
Bockbrader HN, Wesche D, Miller R, Chapel S, Janiczek N, Burger P. A comparison of the pharmacokinetics and pharmacodynamics of pregabalin and gabapentin. Clin Pharmacokinet. 2010;49:661–9.
Beydoun A, Uthman BM, Sackellares JC. Gabapentin: pharmacokinetics, efficacy, and safety. Clin Neuropharmacol. 1995;18:469–81.
Berry DJ, Beran RG, Plunkeft MJ, Clarke LA, Hung WT. The absorption of gabapentin following high dose escalation. Seizure. 2003;12:28–36.
Striano P, Striano S. Gabapentin: a Ca2+ channel alpha 2-delta ligand far beyond epilepsy therapy. Drugs Today (Barc). 2008;44:353–68.
Elwes RD, Binnie CD. Clinical pharmacokinetics of newer antiepileptic drugs. Lamotrigine, vigabatrin, gabapentin and oxcarbazepine. Clin Pharmacokinet. 1996;30:403–15.
Riva R, Albani F, Contin M, Baruzzi A. Pharmacokinetic interactions between antiepileptic drugs. Clinical considerations. Clin Pharmacokinet. 1996;31:470–93.
Eldon MA, Underwood BA, Randinitis EJ, Sedman AJ. Gabapentin does not interact with a contraceptive regimen of norethindrone acetate and ethinyl estradiol. Neurology. 1998;50:1146–8.
Pfizer Inc. Neurontin® US. Physician Prescribing Information. 2014. http://labeling.pfizer.com/ShowLabeling.aspx?id=630. Accessed 21 Nov 2014.
Dang A, Garg A, Rataboli PV. Role of zolpidem in the management of insomnia. CNS Neurosci Ther. 2011;17:387–97.
Pritchett DB, Seeburg PH. Gamma-aminobutyric acidA receptor alpha 5-subunit creates novel type II benzodiazepine receptor pharmacology. J Neurochem. 1990;54:1802–4.
Salva P, Costa J. Clinical pharmacokinetics and pharmacodynamics of zolpidem. Therapeutic implications. Clin Pharmacokinet. 1995;29:142–53.
Langtry HD, Benfield P. Zolpidem. A review of its pharmacodynamic and pharmacokinetic properties and therapeutic potential. Drugs. 1990;40:291–313.
McLean MJ. Clinical pharmacokinetics of gabapentin. Neurology. 1994;44:S17–22.
Gidal BE, Radulovic LL, Kruger S, Rutecki P, Pitterle M, Bockbrader HN. Inter- and intra-subject variability in gabapentin absorption and absolute bioavailability. Epilepsy Res. 2000;40:123–7.
Greenblatt DJ, Harmatz JS, von Moltke LL, Ehrenberg BL, Harrel L, Corbett K, et al. Comparative kinetics and dynamics of zaleplon, zolpidem, and placebo. Clin Pharmacol Ther. 1998;64:553–61.
Bazil CW, Battista J, Basner RC. Gabapentin improves sleep in the presence of alcohol. J Clin Sleep Med. 2005;1:284–7.
Legros B, Bazil CW. Effects of antiepileptic drugs on sleep architecture: a pilot study. Sleep Med. 2003;4:51–5.
Foldvary-Schaefer N, De Leon Sanchez I, Karafa M, Mascha E, Dinner D, Morris HH. Gabapentin increases slow-wave sleep in normal adults. Epilepsia. 2002;43:1493–7.
Lo HS, Yang CM, Lo HG, Lee CY, Ting H, Tzang BS. Treatment effects of gabapentin for primary insomnia. Clin Neuropharmacol. 2010;33:84–90.
Darcourt G, Pringuey D, Salliere D, Lavoisy J. The safety and tolerability of zolpidem-an update. J Psychopharmacol. 1999;13:81–93.
Zammit G. Comparative tolerability of newer agents for insomnia. Drug Saf. 2009;32:735–48.
Amoako EP, Richardson-Campbell L, Kennedy-Malone L. Self-medication with over-the-counter drugs among elderly adults. J Gerontol Nurs. 2003;29:10–5.
Bergmann JF. Self-medication: from European regulatory directives to therapeutic strategy. Fundam Clin Pharmacol. 2003;17:275–80.
Katayose Y, Aritake S, Kitamura S, Enomoto M, Hida A, Takahashi K, et al. Carryover effect on next-day sleepiness and psychomotor performance of nighttime administered antihistaminic drugs: a randomized controlled trial. Hum Psychopharmacol. 2012;27:428–36.
Polasek TM, Sadagopal JS, Elliot DJ, Miners JO. In vitro-in vivo extrapolation of zolpidem as a perpetrator of metabolic interactions involving CYP3A. Eur J Clin Pharmacol. 2010;66:275–83.
Desager JP, Hulhoven R, Harvengt C, Hermann P, Guillet P, Thiercelin JF. Possible interactions between zolpidem, a new sleep inducer and chlorpromazine, a phenothiazine neuroleptic. Psychopharmacology. 1988;96:63–6.
Blum RA, Comstock TJ, Sica DA, Schultz RW, Keller E, Reetze P, et al. Pharmacokinetics of gabapentin in subjects with various degrees of renal function. Clin Pharmacol Ther. 1994;56:154–9.
Boyd RA, Turck D, Abel RB, Sedman AJ, Bockbrader HN. Effects of age and gender on single-dose pharmacokinetics of gabapentin. Epilepsia. 1999;40:474–9.
Acknowledgments
This study was sponsored by Pfizer Inc. Medical writing support was provided by Karen Burrows, MPhil, of Engage Scientific Solutions, and was funded by Pfizer Inc.
Disclosures
Dr. Galitz has no conflict of interest. Drs. S. Jayawardena and S.A. Furey are full-time employees of, and hold stock options in, Pfizer Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Galitz, L.A., Jayawardena, S. & Furey, S.A. Pharmacokinetic Effects of Simultaneous Administration of Single-Dose Gabapentin 500 mg and Zolpidem Tartrate 10 mg in Healthy Volunteers: A Randomized, Open-Label, Crossover Trial. Drugs R D 15, 71–77 (2015). https://doi.org/10.1007/s40268-014-0079-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-014-0079-z