Abstract
Desidustat (Oxemia™), a hypoxia-inducible factor prolyl hydroxylase inhibitor, is a promising new oral alternative to injectable erythropoiesis-stimulating agents (ESAs) for the treatment of anaemia in patients with chronic kidney disease (CKD). Desidustat is approved in India for adults with CKD who are either not on dialysis or on dialysis. It is administered orally three times a week and dosage should be individualised based on the haemoglobin response of the patient. In clinical trials in patients with non-dialysis-dependent and dialysis-dependent CKD, desidustat was non-inferior to darbepoetin alfa and epoetin alfa, respectively, in increasing haemoglobin levels. Desidustat was generally well tolerated in clinical trials of up to 24 weeks and had a broadly similar tolerability and safety profile to darbepoetin alfa and epoetin alfa. The most common adverse events with desidustat were peripheral oedema in patients with non-dialysis-dependent CKD, and pyrexia, increased blood potassium, nausea and chills in patients with dialysis-dependent CKD.
Plain Language Summary
The current standard of care for the treatment of anaemia in patients with chronic kidney disease (CKD) is an injectable erythropoiesis-stimulating agent (ESA) and iron supplementation. However, some patients are hypo-responsive (resistant) to ESAs and there are concerns around their cardiovascular safety at high doses. This has led to the development of hypoxia-inducible factor prolyl hydroxylase inhibitors (HIF-PHIs), which correct anaemia by modulating the expression of genes that control red blood cell production. Desidustat (Oxemia™), an oral HIF-PHI administered three times a week, is approved in India for the treatment of anaemia in adults with CKD who are either not on dialysis or on dialysis. In clinical trials, desidustat was non-inferior to ESAs in increasing haemoglobin levels in patients with non-dialysis-dependent and dialysis-dependent CKD. Desidustat was generally well tolerated in clinical trials of up to 24 weeks, with similar incidences of adverse events compared with ESAs. Thus, desidustat is a promising new oral alternative to injectable ESAs for the treatment of anaemia in patients with CKD.

Similar content being viewed by others
References
Hanna RM, Streja E, Kalantar-Zadeh K. Burden of anemia in chronic kidney disease: beyond erythropoietin. Adv Ther. 2021;38(1):52–75.
National Health Mission. National iron plus initiative guidelines for control of iron deficiency anaemia. 2013. https://www.nhm.gov.in/. Accessed 26 Jun 2023.
Joharapurkar AA, Pandya VB, Patel VJ, et al. Prolyl hydroxylase inhibitors: a breakthrough in the therapy of anemia associated with chronic diseases. J Med Chem. 2018;61(16):6964–82.
Kile M, Sudchada P. Current treatment practices for anemia in patients with chronic kidney disease and future opportunities with hypoxia-inducible factor prolyl hydroxylase inhibitors: a narrative review. Int Urol Nephrol. 2021;53(2):283–90.
Yap DYH, McMahon LP, Hao CM, et al. Recommendations by the Asian Pacific Society of Nephrology (APSN) on the appropriate use of HIF-PH inhibitors. Nephrology (Carlton). 2021;26(2):105–18.
Weir MR. Managing anemia across the stages of kidney disease in those hyporesponsive to erythropoiesis-stimulating agents. Am J Nephrol. 2021;52(6):450–66.
Hanna R, Rastogi A. Anemia management in peritoneal dialysis. In: Rastogi A, Lerma EV, Bargman JM, editors. Applied peritoneal dialysis: improving patient outcomes. Cham: Springer International Publishing; 2021. p. 233–45.
Zydus Lifesciences Ltd. OxemiaTM (desidustat): summary of product characteristics. Ahmedabad: Zydus Lifesciences Ltd; 2022.
Zydus Lifesciences Ltd. Zydus to launch OxemiaTM (desidustat) a breakthrough treatment for anemia in patients suffering from chronic kidney disease (CKD) [media release]. 07 Mar 2022. www.zyduslife.com/.
Zydus Lifesciences Ltd. OxemiaTM pack insert - desidustat tablet 25 mg and 50 mg. Ahmedabad: Zydus Lifesciences Ltd; 2022.
Zydus Lifesciences Ltd. OxemiaTM pack insert - desidustat tablet 100 mg. Ahmedabad: Zydus Lifesciences Ltd.; 2022.
Kansagra KA, Parmar D, Jani RH, et al. Phase I clinical study of ZYAN1, a novel prolyl-hydroxylase (PHD) inhibitor to evaluate the safety, tolerability, and pharmacokinetics following oral administration in healthy volunteers. Clin Pharmacokinet. 2018;57(1):87–102.
Sanghani NS, Haase VH. Hypoxia-inducible factor activators in renal anemia: current clinical experience. Adv Chronic Kidney Dis. 2019;26(4):253–66.
Jain MR, Joharapurkar AA, Pandya V, et al. Pharmacological characterization of ZYAN1, a novel prolyl hydroxylase inhibitor for the treatment of anemia. Drug Res (Stuttg). 2016;66(2):107–12.
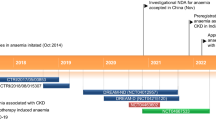
Parmar DV, Kansagra KA, Patel JC, et al. Outcomes of desidustat treatment in people with anemia and chronic kidney disease: a phase 2 study. Am J Nephrol. 2019;49(6):470–8.
Agrawal D, Varade D, Shah H, et al. Desidustat in anemia due to non-dialysis-dependent chronic kidney disease: a phase 3 study (DREAM-ND). Am J Nephrol. 2022;53(5):352–60.
Gang S, Khetan P, Varade D, et al. Desidustat in anemia due to dialysis-dependent chronic kidney disease: a phase 3 study (DREAM-D). Am J Nephrol. 2022;53(5):343–51.
Kansagra KA, Parmar D, Jain MR, et al. Pharmacokinetics of oral ZYAN1 across Indian and Australian healthy subjects [abstract no. PUB700]. J Am Soc Nephrol. 2017;28:1142.
Kansagra K. Comparison of pharmacokinetic parameters of desidustat in pre-dialysis chronic kidney disease Indian patients and Australian healthy volunteers [abstract no. MON-319]. Kidney Int Rep. 2019;4(Suppl 7):S430–1.
Patel H, Modi N, Chaudhari J, et al. Nonclinical pharmacokinetic evaluation of desidustat: a novel prolyl hydroxylase inhibitor for the treatment of anemia. Eur J Drug Metab Pharmacokinet. 2022;47(5):725–40.
Gupta N, Wish JB. Hypoxia-inducible factor prolyl hydroxylase inhibitors: a potential new treatment for anemia in patients with CKD. Am J Kidney Dis. 2017;69(6):815–26.
Semenza GL. Oxygen sensing, hypoxia-inducible factors, and disease pathophysiology. Annu Rev Pathol. 2014;9:47–71.
Sugahara M, Tanaka T, Nangaku M. Future perspectives of anemia management in chronic kidney disease using hypoxia-inducible factor-prolyl hydroxylase inhibitors. Pharmacol Ther. 2022;239:108272.
US National Institutes of Health. ClinicalTrials.gov identifier NCT05515367. 2023. https://www.clinicaltrials.gov/. Accessed 26 Jun 2023.
Borawski B, Malyszko JS, Kwiatkowska M, et al. Current status of renal anemia pharmacotherapy-what can we offer today. J Clin Med. 2021;10(18):4149.
Chen H, Cheng Q, Wang J, et al. Long-term efficacy and safety of hypoxia-inducible factor prolyl hydroxylase inhibitors in anaemia of chronic kidney disease: a meta-analysis including 13,146 patients. J Clin Pharm Ther. 2021;46(4):999–1009.
Wen T, Zhang X, Wang Z, et al. Hypoxia-inducible factor prolyl hydroxylase inhibitors in patients with renal anemia: a meta-analysis of randomized trials. Nephron. 2020;144(11):572–82.
Wang B, Yin Q, Han YC, et al. Effect of hypoxia-inducible factor-prolyl hydroxylase inhibitors on anemia in patients with CKD: a meta-analysis of randomized controlled trials including 2804 patients. Ren Fail. 2020;42(1):912–25.
Zheng Q, Yang H, Sun L, et al. Efficacy and safety of HIF prolyl-hydroxylase inhibitor vs epoetin and darbepoetin for anemia in chronic kidney disease patients not undergoing dialysis: a network meta-analysis. Pharmacol Res. 2020;159:1–9.
Yang J, Xing J, Zhu X, et al. Effects of hypoxia-inducible factor-prolyl hydroxylase inhibitors vs. erythropoiesis-stimulating agents on iron metabolism in non-dialysis-dependent anemic patients with CKD: a network meta-analysis. Front Endocrinol. 2023;14:1131516.
Chen D, Niu Y, Liu F, et al. Safety of HIF prolyl hydroxylase inhibitors for anemia in dialysis patients: a systematic review and network meta-analysis. Front Pharmacol. 2023;14:1163908.
Acknowledgements
The manuscript was reviewed by: A. Gundroo, Division of Nephrology, Department of Internal Medicine, The Ohio State University Wexner Medical Center, Columbus, OH, USA; F. Locatelli, Department of Nephrology, Dialysis & Renal Transplant, Alessandro Manzoni Hospital, Lecco, Italy; J. B. Wish, Division of Nephrology, Indiana University Health, Indianapolis, IN, USA. During the peer review process, Zydus Lifesciences Ltd, the marketing authorization holder of desidustat, was also offered an opportunity to provide a scientific accuracy review of their data. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and conflict of interest
Tina Nie and Yahiya Syed are salaried employees of Adis International Ltd/Springer Nature and declare no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethical approval, Consent to participate, Consent for publication, Availability of data and material, Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nie, T., Syed, Y.Y. Desidustat in anaemia in patients with chronic kidney disease: a profile of its use. Drugs Ther Perspect 39, 279–286 (2023). https://doi.org/10.1007/s40267-023-01012-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-023-01012-1