Abstract
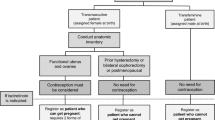
Transmasculine patients receiving testosterone as gender-affirming masculinizing hormone therapy commonly experience hormonal acne as an adverse effect. In some patients, acne is severe and persistent, detrimentally impacting mental health. In order to provide culturally competent and comprehensive dermatological care to transgender and non-binary patients, clinicians need to be aware of the unique concerns of these patients and act to ensure an inclusive clinical experience. While treatment options for acne are similar to those in cisgender patients, possible interactions between acne treatments and gender-affirming therapies or transition goals must be considered. As many acne medications have teratogenic potential, contraceptive needs should be assessed; exogenous testosterone therapy is neither a reliable form of contraception nor a contraindication to contraception. Recent changes to US FDA iPLEDGE requirements may make isotretinoin treatment more accessible to transmasculine patients with severe or treatment-refractory acne.
Similar content being viewed by others
References
Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend. 2012;13(4):165–232.
Radi R, Gold S, Acosta JP, et al. Treating acne in transgender persons receiving testosterone: a practical guide. Am J Clin Dermatol. 2022;23(2):219–29.
Motosko CC, Zakhem GA, Pomeranz MK, et al. Acne: a side-effect of masculinizing hormonal therapy in transgender patients. Br J Dermatol. 2019;180(1):26–30.
Thoreson N, Park JA, Grasso C, et al. Incidence and factors associated with acne among transgender patients receiving masculinizing hormone therapy. JAMA Dermatol. 2021;157(3):290–5.
Yeung H, Ragmanauskaite L, Zhang Q, et al. Prevalence of moderate to severe acne in transgender adults: a cross-sectional survey. J Am Acad Dermatol. 2020;83(5):1450–2.
Wierckx K, Peer F, Verhaeghe E, et al. Short- and long-term clinical skin effects of testosterone treatment in trans men. J Sex Med. 2014;11:222–9.
Ragmanauskaite L, Kahn B, Ly B, et al. Acne and the lesbian, gay, bisexual, or transgender teenager. Dermatol Clin. 2020;38(2):219–26.
Rowniak S, Bolt L, Sharifi C. Effect of cross-sex hormones on the quality of life, depression and anxiety of transgender individuals: a quantitative systematic review. JBI Database Syst Rev Implement Rep. 2019;17(9):1826–54.
Braun H, Zhang Q, Getahun D, et al. Moderate-to-severe acne and mental health symptoms in transmasculine persons who have received testosterone. JAMA Dermatol. 2021;157(3):344–6.
Ogé LK, Broussard A, Marshall MD. Acne vulgaris: diagnosis and treatment. Am Fam Physician. 2019;100(8):475–84.
Krempasky C, Harris M, Abern L, et al. Contraception across the transmasculine spectrum. Am J Obstet Gynecol. 2020;222:134–43.
Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945–73.
Safer JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):168–71.
Kcomt L, Gorey KM, Barrett BJ, et al. Healthcare avoidance due to anticipated discrimination among transgender people: a call to create trans-affirmative environments. SSM Popul Health. 2020;11: 100608.
Markovic L, McDermott DT, Stefanac S, et al. Experiences and interactions with the healthcare system in transgender and non-binary patients in Austria: an exploratory cross-sectional study. Int J Environ Res Public Health. 2021;18(13):6895.
Yeung H, Luk KM, Chen SC, et al. Dermatologic care for lesbian, gay, bisexual, and transgender persons: terminology, demographics, health disparities, and approaches to care. J Am Acad Dermatol. 2019;80:581–9.
Tan J, Thiboutot D, Popp G, et al. Randomized phase 3 evaluation of trifarotene 50 μg/g cream treatment of moderate facial and truncal acne. J Am Acad Dermatol. 2019;80(6):1691–9.
Leyden J, Stein-Gold L, Weiss J. Why topical retinoids are mainstay of therapy for acne. Dermatol Ther (Heidelb). 2017;7:293–304.
Chien AL, Qi J, Rainer B, et al. Treatment of acne in pregnancy. J Am Board Fam Med. 2016;29:254–62.
Hebert A, Thiboutot D, Stein Gold L, et al. Efficacy and safety of topical clascoterone cream, 1%, for treatment in patients with facial acne: two phase 3 randomized clinical trials. JAMA Dermatol. 2020;156(6):621–30.
Peitzmeier SM, Silberholz J, Gardner IH, et al. Time to first onset of chest binding-related symptoms in transgender youth. Pediatrics. 2021;147(3): e20200728.
iPLEDGE. iPLEDGE®: commited to pregnancy prevention. 2021. https://ipledgeprogram.com/. Accessed 6 Sep 2022.
Yeung H, Chen SC, Katz KA, et al. Prescribing isotretinoin in the United States for transgender individuals: ethical considerations. J Am Acad Dermatol. 2016;75:648–51.
US Food and Drug Administration. iPLEDGE risk evaluation and mitigation strategy (REMS). 2022. https://www.fda.gov/. Accessed 6 Sep 2022.
Giltay EJ, Gooren LJG. Effects of sex steroid deprivation/administration on hair growth and skin sebum production in transsexual males and females. J Clin Endocrinol Metab. 2000;85(8):2913–21.
Strauss JS, Leyden JJ, Lucky AW, et al. A randomized trial of the efficacy of a new micronized formulation versus a standard formulation of isotretinoin in patients with severe recalcitrant nodular acne. J Am Acad Dermatol. 2001;45:187–95.
Turrion-Merino L, Urech-Garcia-de-la-Vega M, Miguel-Gomez L, et al. Severe acne in female-to-male transgender patients. JAMA Dermatol. 2015;151(11):1260–1.
Campos-Muñoz L, López-De Lara D, Rodríguez-Rojo ML, et al. Transgender adolescents and acne: a cases series. Pediatr Dermatol. 2018;35:e155–8.
Huang YC, Cheng YC. Isotretinoin treatment for acne and risk of depression: a systematic review and meta-analysis. J Am Acad Dermatol. 2017;76(6):1068–76.
Campos-Muñoz L, López-De Lara D, Conde-Taboada A, et al. Depression in transgender adolescents under treatment with isotretinoin. Clin Exp Dermatol. 2020;45(5):615–6.
Kane S, Admani S. COVID-19 pandemic leading to the accelerated development of a virtual health model for isotretinoin. J Dermatol Nurses Assoc. 2021;13(1):54–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Authorship and conflict of interest
Y. N. Lamb is a salaried employee of Adis International Ltd/Springer Nature and declares no relevant conflicts of interest. All authors contributed to the review and are responsible for the article content.
Ethics approval, Consent to participate, Consent for publication, Availability of data and material, Code availability
Not applicable.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lamb, Y.N. Approach the treatment of acne in transgender patients with sensitivity and awareness. Drugs Ther Perspect 38, 472–477 (2022). https://doi.org/10.1007/s40267-022-00949-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-022-00949-z