Abstract
Background
Adverse drug events associated with medication errors (MEs) are three times higher in children than in adults. To reduce MEs in children, studies have reported the advantage of clinical pharmacist implementations, but a thorough overview of dedicated activities has not yet been clearly described.
Objectives
The objective of this systematic review was to establish an international overview of clinical pharmacy services (CPS) practiced by pharmacists for pediatric inpatients.
Methods
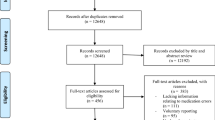
Two databases were searched for original articles published from January 2000 to 2019. Additionally, a manual hand search was conducted. Studies dealing with CPS performed by pharmacists for pediatric inpatients were included. General and geographical data, method, design, and population characteristics of studies were extracted. The primary outcome was to quantify and describe pediatric CPS. Secondary outcomes were to quantify the presence of an age range analysis and impact evaluation. Six validated checklists were used to assess the quality of studies included.
Results
After a full-text review, 42 studies were included. Among the 15 CPS reported, pharmaceutical interventions for prescriptions, medication reconciliation, interactions with medical and paramedical teams, ward round participation, and patient therapeutic education were the most frequently detailed. Only eight studies considered age interpretation. The principal limitation was the heterogeneity of studies.
Conclusion
This work provides a basis for harmonizing the deployment of pediatric CPS in hospital to improve patient safety. Because pharmacists’ time resources are limited, CPS should be prioritized according to hospital population, service organization, and needs evaluation.



Similar content being viewed by others
References
Miller RR. History of clinical pharmacy and clinical pharmacology. J Clin Pharmacol. 1981;21:195–7.
Kaboli PJ, Hoth AB, McClimon BJ, et al. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med. 2006;166:955.
Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114–20.
Choonara I, Conroy S. Unlicensed and off-label drug use in children: implications for safety. Drug Saf. 2002;25:1–5.
Lago P, Bizzarri G, Scalzotto F, et al. Use of FMEA analysis to reduce risk of errors in prescribing and administering drugs in paediatric wards: a quality improvement report. BMJ Open. 2012;2:e001249.
Fortescue EB, Kaushal R, Landrigan CP, et al. Prioritizing strategies for preventing medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2003;111:722–9.
Bhatt-Mehta V, Buck ML, Chung AM, et al. Recommendations for meeting the pediatric patient’s need for a clinical pharmacist: a joint opinion of the Pediatrics Practice and Research Network of the American College of Clinical Pharmacy and the Pediatric Pharmacy Advocacy Group. Pharmacother J Hum Pharmacol Drug Ther. 2013;33:243–51.
Rinke ML, Bundy DG, Velasquez CA, et al. Interventions to reduce pediatric medication errors: a systematic review. Pediatrics. 2014;134:338–60.
Levine SR, Cohen MR, Blanchard NR, et al. Guidelines for preventing medication errors in pediatrics. J Pediatr Pharmacol Ther. 2001;6:426–42.
Wong I. Ways to reduce drug dose calculation errors in children. J Health Serv Res Policy. 2010;15:68–70.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Munn Z, Moola S, Lisy K, et al. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and incidence data. Int J Evid Based Heal. 2015;13:147–53.
Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute; 2017. https://reviewersmanual.joannabriggs.org/. Accessed 30 May 2019.
Tufanaru C, Munn Z, Aromataris E, et al. Chapter 3: systematic reviews of effectiveness. In: Aromataris E, Munn Z, editors. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute; 2017. https://reviewersmanual.joannabriggs.org/. Accessed 28 May 2019.
Drovandi A, Robertson K, Tucker M, et al. A systematic review of clinical pharmacist interventions in paediatric hospital patients. Eur J Pediatr. 2018;177:1139–48.
Prot-Labarthe S, Lavoie A, Bourdon O, et al. Étude pilote sur la mise en place des soins pharmaceutiques dans le service de pédiatrie générale d’un hôpital français Collaboration et comparaison franco-québécoise. Arch Pédiatrie. 2007;14:345–53.
Nguyen V, Sarik DA, Dejos MC, et al. Development of an interprofessional pharmacist-nurse navigation pediatric discharge program. J Pediatr Pharmacol Ther. 2018;23:320–8.
Ramadaniati HU, Lee YP, Hughes JD. The difference in pharmacists’ interventions across the diverse settings in a children’s hospital. PLoS ONE. 2014. https://doi.org/10.1371/journal.pone.0110168.
Zobell JT, Schwab E, Collingridge DS, et al. Impact of pharmacy services on cystic fibrosis medication adherence. Pediatr Pulmonol. 2017;52:1006–12.
Zhang C, Zhang L, Huang L, et al. Clinical pharmacists on medical care of pediatric inpatients: a single-center randomized controlled trial. PLoS ONE. 2012;7:e30856.
Cunningham KJ. Analysis of clinical interventions and the impact of pediatric pharmacists on medication error prevention in a teaching hospital. J Pediatr Pharmacol Ther. 2012;17:365–73.
Virani A, Crown N. The impact of a clinical pharmacist on patient and economic outcomes in a child and adolescent mental health unit. Can J Hosp Pharm. 2003;56:158–62.
Moffett BS, Mott AR, Nelson DP, et al. Medication dosing and renal insufficiency in a pediatric cardiac intensive care unit: impact of pharmacist consultation. Pediatr Cardiol. 2008;29:744–8.
Prot-Labarthe S, Di Paolo ER, Lavoie A, et al. Pediatric drug-related problems: a multicenter study in four French-speaking countries. Int J Clin Pharm. 2013;35:251–9.
Carthon CE, Hall RC, Maxwell PR, et al. Impact of a pharmacist-led vaccine recommendation program for pediatric kidney transplant candidates. Pediatr Transplant. 2017;21:e12989.
Abrogoua D, Békégnran C, Gro B, et al. Assessment of a clinical pharmacy activity in a pediatric inpatient department in Cote D′ivoire. J Basic Clin Pharm. 2017;8:15.
Fernández-Llamazares CM, Pozas M, Feal B, et al. Profile of prescribing errors detected by clinical pharmacists in paediatric hospitals in Spain. Int J Clin Pharm. 2013;35:638–46.
Echarri-Martínez L, Fernández-Llamazares CM, Manrique-Rodríguez S, et al. Pharmaceutical care in paediatric intensive care unit: activities and interdisciplinary learning in a Spanish hospital. Eur J Hosp Pharm. 2012;19:416–22.
Abu Farha R, Abu Hammour K, Al-Jamei S, et al. The prevalence and clinical seriousness of medication discrepancies identified upon hospital admission of pediatric patients. BMC Health Serv Res. 2018;18(1):966.
Huynh C, Wong ICK, Tomlin S, et al. An evaluation of paediatric medicines reconciliation at hospital discharge into the community: paediatric medicines reconciliation discharge. Int J Pharm Pract. 2016;24:196–202.
Tripathi S, Crabtree HM, Fryer KR, et al. Impact of clinical pharmacist on the pediatric intensive care practice: an 11-year tertiary center experience. J Pediatr Pharmacol Ther JPPT Off J PPAG. 2015;20:290–8.
Fernández-Llamazares CM, Calleja-Hernandez MA, Manrique-Rodriguez S, et al. Impact of clinical pharmacist interventions in reducing paediatric prescribing errors. Arch Dis Child. 2012;97:564–8.
Stone BL, Boehme S, Mundorff MB, et al. Hospital admission medication reconciliation in medically complex children: an observational study. Arch Dis Child. 2010;95(4):250–5.
Coffey M, Mack L, Streitenberger K, et al. Prevalence and clinical significance of medication discrepancies at pediatric hospital admission. Acad Pediatr. 2009;9:360-365.e1.
Wang JK, Herzog NS, Kaushal R, et al. Prevention of pediatric medication errors by hospital pharmacists and the potential benefit of computerized physician order entry. Pediatrics. 2007;119:e77-85.
Kaushal R, Bates DW, Abramson EL, et al. Unit-based clinical pharmacists’ prevention of serious medication errors in pediatric inpatients. Am J Health Syst Pharm. 2008;65:1254–60.
Nguyen-Ha P-T, Howrie D, Crowley K, et al. A quality assessment of a collaborative model of a pediatric antimicrobial stewardship program. Pediatrics. 2016;137:e20150316–e20150316.
Rogers J, Pai V, Merandi J, et al. Impact of a pharmacy student–driven medication delivery service at hospital discharge. Am J Health Syst Pharm. 2017;74:S24–9.
Shah D, Manzi S. Pharmacist outpatient prescription review in the emergency department. Pediatr Emerg Care. 2018;34:497–500.
Marconi GP, Claudius I. Impact of an emergency department pharmacy on medication omission and delay. Pediatr Emerg Care. 2012;28:30–3.
Lehnbom EC, Li L, Prgomet M, et al. Little things matter: a time and motion study of pharmacists’ activities in a paediatric hospital. Stud Health Technol Inform. 2016;227:80–6.
Provine AD, Simmons EM, Bhagat PH. Establishment and evaluation of pharmacist-managed admission medication history and reconciliation process for pediatric patients. J Pediatr Pharmacol Ther. 2014;19:98–102.
Maat B, Au YS, Bollen CW, et al. Clinical pharmacy interventions in paediatric electronic prescriptions. Arch Dis Child. 2013;98:222–7.
Dersch-Mills D, Hugel K, Nystrom M. Completeness of information sources used to prepare best possible medication histories for pediatric patients. Can J Hosp Pharm. 2011;64:10–5.
Lake N, Nawer H, Wagner D. Piloting medication histories in a pediatric postanesthesia care unit. J Perianesth Nurs. 2019;34(1):117–23.
Angoulvant F, Rouault A, Prot-Labarthe S, et al. Randomized controlled trial of parent therapeutic education on antibiotics to improve parent satisfaction and attitudes in a pediatric emergency department. PLoS ONE. 2013;8:e75590.
Malfará M, Pernassi M, Aragon D, et al. Impact of the clinical pharmacist interventions on prevention of pharmacotherapy related problems in the paediatric intensive care unit. Int J Clin Pharm. 2018;40:513–9.
Bahnasawy SM, El Wakeel LM, Beblawy NE, et al. Clinical pharmacist-provided services in iron-overloaded beta-thalassaemia major children: a new insight into patient care. Basic Clin Pharmacol Toxicol. 2017;120:354–9.
Okumura LM, da Silva DM, Comarella L. Relation between safe use of medicines and clinical pharmacy services at pediatric intensive care units. Rev Paul Pediatr Engl Ed. 2016;34:397–402.
Prot-Labarthe S, Therrien R, Demanche C, et al. Pharmaceutical care in an inpatient pediatric hematopoietic stem cell transplant service. J Oncol Pharm Pract Off Publ Int Soc Oncol Pharm Pract. 2008;14:147–52.
Krupicka MI, Bratton SL, Sonnenthal K, et al. Impact of a pediatric clinical pharmacist in the pediatric intensive care unit. Crit Care Med. 2002;30:919–21.
Christiansen SR, Morgan JA, Hilmas E, et al. Impact of a prescription review program on the accuracy and safety of discharge prescriptions in a pediatric hospital setting. J Pediatr Pharmacol Ther JPPT Off J PPAG. 2008;13:226–32.
Huynh C, Tomlin S, Jani Y, et al. An evaluation of the epidemiology of medication discrepancies and clinical significance of medicines reconciliation in children admitted to hospital. Arch Dis Child. 2016;101:67–71.
Terry DRP, Solanki GA, Sinclair AG, et al. Clinical significance of medication reconciliation in children admitted to a UK pediatric hospital: observational study of neurosurgical patients. Pediatr Drugs. 2010;12:331–7.
Cies JJ, Varlotta L. Clinical pharmacist impact on care, length of stay, and cost in pediatric cystic fibrosis (CF) patients: pharmacist impact in pediatric CF. Pediatr Pulmonol. 2013;48:1190–4.
Alagha HZ, Badary OA, Ibrahim HM, et al. Reducing prescribing errors in the paediatric intensive care unit: an experience from Egypt: prescribing errors in a PICU. Acta Paediatr. 2011;100:e169–74.
Nguyen M-NR, Mosel C, Grzeskowiak LE. Interventions to reduce medication errors in neonatal care: a systematic review. Ther Adv Drug Saf. 2018;9:123–55.
Horace A, Ahmed F. Polypharmacy in pediatric patients and opportunities for pharmacists’; involvement. Integr Pharm Res Pract. 2015;4:113.
Huynh C, Wong ICK, Tomlin S, et al. Medication discrepancies at transitions in pediatrics: a review of the literature. Pediatr Drugs. 2013;15:203–15.
Mueller SK, Sponsler KC, Kripalani S, et al. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012;172(14):1057–69.
Bédard P, Tardif L, Ferland A, et al. A medication reconciliation form and its impact on the medical record in a paediatric hospital: medication reconciliation in a paediatric hospital. J Eval Clin Pract. 2011;17:222–7.
American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians, Transitions Clinical Report Authoring Group. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128:182–200.
Kaushal R, Goldmann DA, Keohane CA, et al. Adverse drug events in pediatric outpatients. Ambul Pediatr. 2007;7:383–9.
Varnell CD, Rich KL, Nichols M, et al. Assessing barriers to adherence in routine clinical care for pediatric kidney transplant patients. Pediatr Transplant. 2017;21:e13027.
El-Rachidi S, Larochelle JM, Morgan JA. Pharmacists and pediatric medication adherence: bridging the gap. Hosp Pharm. 2017;52:124–31.
Sleath B, Bush PJ, Pradel FG. Communicating with children about medicines: a pharmacist’s perspective. Am J Health-Syst Pharm AJHP Off J Am Soc Health-Syst Pharm. 2003;60:604–7.
Saseen JJ, Ripley TL, Bondi D, et al. ACCP clinical pharmacist competencies. Pharmacother J Hum Pharmacol Drug Ther. 2017;37:630–6.
Bellomo R, Bagshaw SM. Evidence-based medicine: classifying the evidence from clinical trials–the need to consider other dimensions. Crit Care Lond Engl. 2006;10:232.
Chan C, Woo R, Seto W, et al. Medication reconciliation in pediatric cardiology performed by a pharmacy technician: a prospective cohort comparison study. Can J Hosp Pharm. 2015;68:8–15.
McDonald D, Mansukhani R, Kokotajlo S, et al. Effect of nursing education on optimization of medication reconciliation in the pediatric emergency department. J Pediatr Pharmacol Ther. 2018;23:203–8.
Small L, Schuman A, Reiter PD. Training program for pharmacists in pediatric emergencies. Am J Health Syst Pharm. 2008;65:649–54.
Kennedy MJ, Phan H, Benavides S, et al. The role of the pediatric pharmacist in personalized medicine and clinical pharmacogenomics for children: pediatric pharmacogenomics working group. J Pediatr Pharmacol Ther JPPT Off J PPAG. 2011;16:118–22.
Lampkin SJ, Gildon B, Benavides S, et al. Considerations for providing ambulatory pharmacy services for pediatric patients. J Pediatr Pharmacol Ther. 2018;23:4–17.
Acknowledgements
The author thanks Dr Clarisse Roux (pharmacist in Nîmes University Hospital) for her review of the manuscript and the critical contributions of Dr Philippe Cestac (pharmacist in Toulouse University Hospital) and Dr Gaëlle de Barry (pharmacist in Montpellier University Hospital).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Conflict of interest
Irène Maffre, Géraldine Leguelinel-Blache, and Ian Soulairol have no conflicts of interest that are directly relevant to the content of this article.
Availability of data and material
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Author contributions
Irène Maffre wrote the initial manuscript and revised the manuscript, conducted the article inclusion process, collected the data, performed the statistical and results analyses, co-performed quality analysis of included studies and co-wrote the methodology of the review. Ian Soulairol critically reviewed the manuscript, co-wrote the methodology of the protocol, co-performed quality analysis of included studies, supervised and planned the review, and verified the statistical analysis. Géraldine Leguelinel-Blache critically reviewed the manuscript, supervised the methodology of the protocol, and planned the study. All authors read and approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Rights and permissions
About this article
Cite this article
Maffre, I., Leguelinel-Blache, G. & Soulairol, I. A systematic review of clinical pharmacy services in pediatric inpatients. Drugs Ther Perspect 37, 363–375 (2021). https://doi.org/10.1007/s40267-021-00845-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-021-00845-y