Abstract
Background
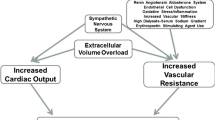
Hypertension is highly prevalent and poorly controlled among hemodialysis patients. However, published information regarding the management and control of hypertension among Pakistani hemodialysis patients is scarce.
Objective
Our objective was to evaluate the pharmacotherapeutic management and control of hypertension and associated factors in hemodialysis patients at a tertiary-care hospital.
Materials and methods
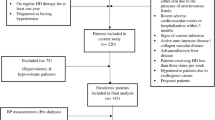
Eligible hypertensive hemodialysis patients enrolled at the Balochistan Institute of Nephrology-Urology Quetta, Pakistan, between 1 July 2017 and 30 November 2019 were retrospectively followed for 6 months after the baseline hemodialysis session. Collected data were analyzed using SPSS version 20, and odds ratios (ORs) were calculated. Patients with mean pre-dialysis blood pressure (BP) < 140/90 and post-dialysis BP < 130/80 mmHg in the final month of study were classified as being at target BP.
Results
A total of 237 hypertensive hemodialysis patients were included in the analysis. The mean age of patients was 42.8 ± 13.2 years, and most (78.9%) had at least one comorbidity. In the final month of the study, only 68 patients (28.7%) were at target BP. Patients were treated with a median of two antihypertensive drugs (range 1–5). Calcium-channel blockers (CCBs) were the most commonly prescribed antihypertensive (54.4%), followed by angiotensin-receptor blockers (53.2%) and diuretics (42.2%). In multivariate binary logistic regression analysis, the use of diuretics (OR 0.50; 95% CI 0.27–0.95), CCBs (OR 2.90; 95% CI 1.35–6.20), β-blockers (OR 2.9; 95% CI 1.30–6.73), and α/β-blockers (OR 2.75; 95% CI 1.26–5.98) was significantly associated with hypertension control.
Conclusion
Hypertension control was suboptimal at the study site. A notable proportion of patients were receiving diuretics despite guidelines discouraging their use. The use of β-blockers, α-β-blockers, and CCBs was associated with hypertension control.
Similar content being viewed by others
Data availability
All data are publically available.
References
Salem MM. Hypertension in the hemodialysis population: a survey of 649 patients. Am J Kid Dis. 1995;26:461–8.
Hypertension, by DOPPS country and cross-section. 2006. https://www.dopps.org/annualreport/archives/DOPPSAR2009/html/MCOMHTN_c_TAB2009.htm
Agarwal R. Epidemiology of interdialytic ambulatory hypertension and the role of volume excess. Am J Nephrol. 2011;34:381–90.
Khan A, Khan AH, Adnan AS, et al. Hypertension control among euvolemic hypertensive hemodialysis patients in Malaysia: a prospective follow-up study. J Pharm Policy Pract. 2019;12:10.
Amar J, Vernier I, Rossignol E, et al. Nocturnal blood pressure and 24-hour pulse pressure are potent indicators of mortality in hemodialysis patients. Kidney Int. 2000;57:2485–91.
Agarwal R. Blood pressure and mortality among hemodialysis patients. Hypertension. 2010;55:762–8.
Bansal N, McCulloch CE, Rahman M, et al. Blood pressure and risk of all-cause mortality in advanced chronic kidney disease and hemodialysis: the chronic renal insufficiency cohort study. Hypertension. 2015;65:93–100.
Sarafidis PA, Persu A, Agarwal R, et al. Hypertension in dialysis patients: a consensus document by the European Renal and Cardiovascular Medicine (EURECA-m) working group of the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) and the Hypertension and the Kidney working group of the European Society of Hypertension (ESH). Nephrol Dial Transpl. 2017;32:620–40.
Machnik A, Neuhofer W, Jantsch J, et al. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C–dependent buffering mechanism. Nat Med. 2009;15:545.
Kelley K, Light RP, Agarwal R. Trended cosinor change model for analyzing hemodynamic rhythm patterns in hemodialysis patients. Hypertension. 2007;50(1):143–50.
Heerspink HJL, Ninomiya T, Zoungas S, et al. Effect of lowering blood pressure on cardiovascular events and mortality in patients on dialysis: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2009;373:1009–155.
Agarwal R, Sinha AD. Cardiovascular protection with antihypertensive drugs in dialysis patients: systematic review and meta-analysis. Hypertension. 2009;53:860–6.
Agarwal R, Flynn J, Pogue V, et al. Assessment and management of hypertension in patients on dialysis. J Am Soc Nephrol. 2014;25:1630–46.
Denker MG, Cohen DL. Antihypertensive medications in end-stage renal disease. Sem Dial. 2015;28:330–6.
Inrig JK. Antihypertensive agents in hemodialysis patients: a current perspective. Sem Dial. 2010;23:290–7.
Hayashi SY, Seeberger A, Lind B, et al. Acute effects of low and high intravenous doses of furosemide on myocardial function in anuric haemodialysis patients: a tissue Doppler study. Nephrol Dial Transpl. 2007;23:1355–61.
Zoccali C, Mallamaci F, Parlongo S, et al. Plasma norepinephrine predicts survival and incident cardiovascular events in patients with end-stage renal disease. Circulation. 2002;105:1354–9.
Jadoul M, Thumma J, Fuller DS, et al. Modifiable practices associated with sudden death among hemodialysis patients in the dialysis outcomes and practice patterns study. Clin J Am Soc Nephrol. 2012;7:765–74.
Cice G, Ferrara L, D’Andrea A, et al. Carvedilol increases two-year survivalin dialysis patients with dilated cardiomyopathy: a prospective, placebo-controlled trial. J Am Coll Cardiol. 2003;41(9):1438–44.
Agarwal R, Sinha AD, Pappas MK, et al. Hypertension in hemodialysis patients treated with atenolol or lisinopril: a randomized controlled trial. Nephrol Dial Transpl. 2014;29:672–81.
Pakistan Bureau of Statistics. Government of Pakistan. Provisional summary results of the 6th population and housing census 2017. Islamabad: Pakistan Bureau of Statistics; 2018.
Hasan M, Sutradhar I, Gupta RD, et al. Prevalence of chronic kidney disease in South Asia: a systematic review. BMC Nephrol. 2018;19:291.
Chaudhry A. Alarming increase in end-stage kidney disease. Lahore: Dawn Newspaper; 2017.
The Kidney Foundation. Dialysis registry of Pakistan 2014. Karachi: The Kidney Foundation; 2014.
Ahmad N, Hassan Y, Tangiisuran B, et al. Guidelines adherence and hypertension control in an outpatient cardiology clinic in Malaysia. Trop J Pharm Res. 2012;11:665–72.
Ahmad N, Hassan Y, Tangiisuran B, et al. Guidelines adherence and hypertension control at a tertiary hospital in Malaysia. J Eval Clin Pract. 2013;19:798–804.
Pallant J. SPSS survival manual: a step-by-step guide to data analysis using SPSS version 15. Nova Iorque: McGraw Hill; 2007.
Pedrini L, Winter A, Cerino F, et al. Clinical outcomes of hemodialysis patients in a public-private partnership care framework in Italy: a retrospective cohort study. BMC Nephrol. 2019;20:35.
Yang W-C, Hwang S-J. Taiwan Society of Nephrology. Incidence, prevalence and mortality trends of dialysis end-stage renal disease in Taiwan from 1990 to 2001: the impact of national health insurance. Nephrol Dial Transpl. 2008;23(12):3977–82.
Jafar TH. The growing burden of chronic kidney disease in Pakistan. N Eng J Med. 2006;354:995–7.
Ahmad K, Jafar TH. Prevalence and determinants of blood pressure screening in Pakistan. J Hypertens. 2005;23:1979–84.
Agarwal R, Nissenson AR, Batlle D, et al. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med. 2003;115(4):291–7.
Miller LM, Hopman WM, Garland JS, et al. Cardioprotective medication use in hemodialysis patients. Can J Cardiol. 2006;22(9):755–60.
Levin NW, Kotanko P, Eckardt KU, et al. Blood pressure in chronic kidney disease stage 5D: report from a kidney disease: improving global outcomes controversies conference. Kidney Int. 2010;77(4):273–84.
Georgianos PI, Agarwal R. Pharmacotherapy of hypertension in chronic dialysis patients. Clin J Am Soc Nephrol. 2016;11(11):2062–75.
Zannad F, Kessler M, Lehert P, et al. Prevention of cardiovascular events in end-stage renal disease: results of a randomized trial of fosinopril and implications for future studies. Kidney Int. 2006;70(7):1318–24.
Knoll GA, Shagal A, Nair RC, et al. Renin-angiotensin system blockade and the risk of hyperkalemia in chronic hemodialysis patients. Am J Med. 2002;112(2):110–4.
Converse RL Jr, Jacobsen TN, Toto RD, et al. Sympathetic overactivity in patients with chronic renal failure. N Eng J Med. 1992;327:1912–8.
London GM, Marchais S, Guerin A, et al. Salt and water retention and calcium blockade in uremia. Circulation. 1990;82(1):105–13.
Tepel M, Hopfenmueller W, Scholze A, et al. Effect of amlodipine on cardiovascular events in hypertensive haemodialysis patients. Nephrol Dial Transpl. 2008;23(11):3605–12.
Vasco RF, Moyses RM, Zatz R, et al. Furosemide increases the risk of hyperparathyroidism in chronic kidney disease. Am J Nephrol. 2016;43(6):421–30.
Sibbel S, Walker AG, Colson C, et al. Association of continuation of loop diuretics at hemodialysis initiation with clinical outcomes. Clin J Am Soc Nephrol. 2019;14(1):95–102.
Bragg-Gresham JL, Fissell RB, Mason NA, et al. Diuretic use, residual renal function, and mortality among hemodialysis patients in the Dialysis Outcomes and Practice Pattern Study (DOPPS). Am J Kid Dis. 2007;49(3):426–31.
Taler SJ, Agarwal R, Bakris GL, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for management of blood pressure in CKD. Clin J Am Soc Nephrol. 2013;62(2):201–13.
Tapolyai M, Forró M, Lengvárszky Z, et al. Dialysis patients who smoke are more hypertensive, more fluid overloaded and take more antihypertensive medications than nonsmokers. Ren Fail. 2020;42(1):413–8.
Acknowledgements
The authors acknowledge the record keeping and supportive staff of Balochistan Institute of Nephrology-Urology Quetta for their help in conducting this study.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
G, NA, and AW conceptualized the study. G collected the data. G, MA, Asad K and NA analyzed the data and wrote the manuscript. All authors critically reviewed the manuscript. NA also supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
Gulalai, Nafees Ahmad, Abdul Wahid, Amjad Khan, Muhammad Atif, and Asad Khan have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
The study was approved by the Research and Ethics Committee of the Faculty of Pharmacy and Health Sciences, and permission to conduct the study was granted by BINUQ.
Rights and permissions
About this article
Cite this article
Gulalai, Ahmad, N., Wahid, A. et al. Evaluation of management and factors associated with hypertension control in hemodialysis patients at a tertiary-care hospital in Pakistan. Drugs Ther Perspect 36, 396–403 (2020). https://doi.org/10.1007/s40267-020-00763-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40267-020-00763-5