Abstract
Background
Older patients are often underrepresented in clinical trials owing to exclusionary comorbidities, which are more common with age. Chemotherapy is poorly tolerated in older comorbid advanced cutaneous squamous cell carcinoma (CSCC) patients; however, little is known on the efficacy and tolerability of immune-checkpoint inhibitors (ICIs) in this population. To our knowledge, this is the largest dedicated report on a cohort of older patients with advanced CSCC treated with immunotherapy to date.
Objective
The aim was to report outcomes of ICI use in a real-world older cohort with advanced CSCC.
Patients and Methods
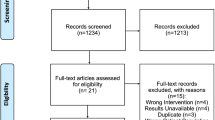
A single-centre retrospective audit of all patients treated via an access scheme providing ICIs to patients with advanced CSCC was conducted. Participants were ≥ 70 years of age and had advanced CSCC not amenable to curative surgery or radiotherapy. Best overall response rate (ORR), 12-month overall survival (OS) and progression-free survival (PFS), and toxicity rates were assessed.
Results
A total of 53 patients were analysed. The median age was 81.8 years (range 70.1–96.8); 81% were male; 34% were immunocompromised; and 34% had an Eastern Cooperative Oncology Group (ECOG) performance status score of ≥ 2. The ORR was 57%, and 12-month OS and PFS were 63% (95% confidence interval [CI] 44–78) and 41% (95% CI 25–57), respectively. Thirty-two per cent developed an immune-related adverse event (irAE), but only two patients experienced a grade 3 irAE, with no treatment-related deaths. Higher ECOG score was associated with worse OS and PFS. No significant association was identified for increasing age, sex, Charlson Comorbidity Index score, or immunocompromised status.
Conclusions
ICIs have demonstrated efficacy and have an acceptable safety profile among older patients with advanced CSCC, with comparable efficacy to what has been demonstrated in current clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study highlights immunotherapy can be safely given to appropriately selected older patients with advanced cutaneous squamous cell carcinoma, with a potential for similar treatment outcomes to what has been reported in trial populations. |
This study also reinforced an important role for Eastern Cooperative Oncology Group (ECOG) performance status in the selection of older patients fit for treatment. |
1 Introduction
Cutaneous squamous cell carcinoma (CSCC) is one of the most common malignancies in Australia owing to high levels of ultraviolet-light (UV) exposure, an outdoors culture, and a large Caucasian population [1]. CSCC is reported to account for around 20% of non-melanomatous skin cancers and has an increasing incidence in older populations, particularly in men over the age of 80 years [2, 3]. CSCC is more common in older patients owing to cumulative UV-radiation exposure, with rates 5–10 times higher in those aged over 75 years [4]. Immune-checkpoint inhibitors (ICIs) have become the standard of care for the management of patients with advanced CSCC who cannot be cured with surgery or radiotherapy. Responses can be seen in 50% of patients as per the Response Evaluation Criteria in Solid Tumors (RECIST1.1) [5], with evidence of durable control and manageable toxicity [6,7,8,9]. It is well established that older patients are under-represented in clinical trials owing to comorbidity, frailty, and a poorer overall performance status, resulting in this population failing to meet the stringent inclusion criteria of clinical trials. Patients aged 80 years or older have historically comprised only 4% of the clinical trial population [10, 11], which is a striking disparity given around 50% of all cancers and 70% of cancer deaths occur in those aged over 65 years [12, 13]. This is particularly relevant for advanced CSCC, with the cemiplimab registrational study having a median cohort age of 71 years and median ages of 77 and 79 years reported in the real-world population studies from France and Italy, respectively [14, 15].
Historically, there has been concern that older patients face an unfavourably skewed risk-to-benefit ratio when treated with chemotherapy. Age-related organ functional decline, comorbidity, decreased functional reserves, and a focus on quality of life are all legitimate concerns in this population. ICIs are generally thought to be more tolerable than chemotherapy. However, immune-related adverse events (irAEs) may still result in hospitalisation and pose significant risk to those with a compromised functional reserve. Higher Charlson Comorbidity Index (CCI) scores, for example, have correlated with poorer survival outcomes in cancer patients [16, 17]. There is, however, growing literature that ICIs can be effectively and safely administered in older patients [11, 18]. In this report, we focus on older patients (≥ 70 years), including poorer performance status and immunocompromised patients and incorporating CCI data to better understand the tolerability and efficacy of ICIs in a real-world older population with advanced CSCC.
2 Patients and Methods
2.1 Patients
This was a single-centre, retrospective study performed at the Peter MacCallum Cancer Centre. Eligible patients included those with locally advanced (not amenable to curative radiotherapy or surgery) or metastatic CSCC who received cemiplimab 350 mg/3-weekly via an access scheme. A small number of patients who self-funded pembrolizumab therapy prior to access scheme availability were also included. All patients were deemed ineligible to participate in available clinical trials at the time of ICI commencement. All locoregionally advanced cases required documentation that the patient was not eligible for curative radiotherapy or surgery. Participants were eligible for the access programme if they had an Eastern Cooperative Oncology Group (ECOG) performance status of ≤ 1; however, poorer ECOG patients who were deemed fit by the treating physician to receive ICIs were permitted. For this study, patients were eligible for analysis if they received at least one cycle of ICI and were ≥ 70 years of age. The first patient commenced treatment in August 2017 and the last patient February 2022. The date of last of follow-up was 9 June 2022. ICIs were continued until unacceptable toxicity, progression, or death from any cause, or according to patient/physician decision.
This study was approved by the Human Research Ethics Committee of the Peter MacCallum Cancer Centre, Melbourne, Australia, with a waiver for consent granted.
2.2 Data Collection and Statistical Analyses
Data collected included basic demographics, disease extent, reason for trial ineligibility, disease response assessments, and toxicity. Immunocompromised status was clinician assessed and could be as a result of disease (i.e. haematological malignancy), medication (systemic immunosuppressive treatment or prednisolone dosages > 10 mg daily or equivalent for > 1 month), or both. The primary endpoint was the best overall response rate (ORR) as determined by a hierarchical assessment of RECIST1.1 [5], World Health Organization (WHO) clinical response criteria [19], and Positron Emission Tomography Response Criteria (PERCIST1.0) [20] on fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT). Overall survival (OS) was defined from commencement of ICI until the time of death from any cause. Progression-free survival (PFS) was measured from the date of commencement of ICI until first documented progression at any site or death from any cause. Toxicity was reported as per Common Terminology Criteria for Adverse Events version 5 (CTCAE v5). The CCI (including cancer diagnosis) was used to calculate comorbidity in patients.
Descriptive statistics were used to present baseline characteristics, and the Kaplan-Meier method was used to describe OS and PFS. A Cox proportional hazard model was used to assess the effect of selected clinico-pathological features on OS and PFS. The Fisher exact test was used to assess whether autoimmune disease and immunocompromised status were associated with irAE grade ≥ 2. Statistical analyses were performed in R version 4.2.1
3 Results
3.1 Patient Characteristics
A total of 53 patients were identified for analysis. The median age was 81.8 years (range 70.1–96.8), the majority were male (81%, n = 43), and 34% (n = 18) had an ECOG score of ≥ 2 (Table 1). The majority of CSCC originated in the head and neck (89%, n = 47). The cohort was comorbid, with a median CCI score of 9 and 34% (n = 18) being immunocompromised. Thirteen patients had a concurrent haematological malignancy, and four out of six patients with autoimmune disease were requiring immunosuppression to control their autoimmune condition at the time of ICI commencement. One patient had a history of immune thrombocytopenic purpura and polymyalgia rheumatica; however, their disease was controlled and not requiring immunosuppressive therapy. Another patient previously developed pneumonitis in the setting of prior immunotherapy for a lung malignancy. The pneumonitis was in remission, and they were off steroid therapy at the time of ICI commencement. Most patients (n = 51) received cemiplimab, and all patients who had advanced disease received immunotherapy as first-line systemic therapy. Forty-seven per cent (n = 25) had prior radiotherapy, and 70% (n = 37) had prior surgery for their primary disease, respectively. Whilst one patient in the cohort had a history of a prior renal transplant, they did not have an active graft at the time of ICI commencement and were no longer receiving transplant immunosuppression.
3.2 Efficacy
The ORR as per the hierarchical response assessment was 57% (26/46), with 33% (n = 15) of patients achieving a complete response and 24% (n = 11) a partial response. Only eight patients recorded progressive disease as their best response (Table 2). Immunocompromised patients (n = 18) experienced a lower ORR of 47% (7/15) compared with immunocompetent patients (61%, 19/31).
Figure 1 demonstrates a complete response that occurred in a 77-year-old patient with painful metastatic CSCC to the right neck. After 15 cycles of cemiplimab, they achieved a partial metabolic response. They now remain pain-free and in complete metabolic response after 21 cycles.
a Baseline FDG-PET/CT demonstrating avid right neck CSCC mass in an older patient. b Following 15 cycles of cemiplimab, a partial metabolic response was achieved. c After 19 cycles of cemiplimab, a complete metabolic response was observed. CSCC cutaneous squamous cell carcinoma, FDG-PET/CT fluorodeoxyglucose positron emission tomography/computed tomography
3.3 Survival
The median duration of follow-up for this cohort was 9.1 months. The 12-month OS and PFS were 63% (95% confidence interval [CI] 44–78) and 41% (95% CI 25–57), respectively (Fig. 2).
In Cox regression analysis, poorer ECOG score was associated with worse OS and PFS (Table 3, Fig. 3). No significant association with OS and PFS was identified for increasing age, sex, CCI score, or immunocompromised status. Figure 4 demonstrates the Kaplan–Meier curves for OS and PFS in immunocompromised versus immunocompetent patients.
At the time of study follow-up, 17 patients (32%) had died. However, only six patients died as a direct result of their advanced CSCC.
3.4 Toxicity
Immune-related adverse events (irAEs) occurred in 32% (n = 17) of patients. Eleven per cent (n = 6) discontinued treatment because of treatment-related toxicity. Two patients experienced grade 3 irAEs: one patient experienced grade 3 skin toxicity and the other patient myocarditis and colitis. Rheumatological irAEs included polymyalgia rheumatica (n = 3), inflammatory arthropathy (n = 2), and myositis (n = 1), and one patient experienced a flare of their original vasculitis. All three endocrine irAEs were thyroiditis. There were no treatment-related deaths (Table 4).
Six patients in this study had autoimmune disease at the time of ICI commencement. This included three patients with rheumatoid arthritis, one with vasculitis, one with pneumonitis after receiving immunotherapy for a prior lung malignancy, and one with immune thrombocytopenic purpura and polymyalgia rheumatica. All six patients subsequently experienced an irAE; however, only three patients experienced a flare of their original autoimmune disease. These three patients had vasculitis, polymyalgia rheumatica, and rheumatoid arthritis, respectively. None of these patients died as a result of their toxicity.
Whilst numbers are small, the presence of autoimmune disease did correlate with grade 2 or higher irAEs (p < 0.001), whilst an immunocompromised status did not (p = 0.101).
4 Discussion
This study supports the use of ICIs in older patients with advanced CSCC as an effective treatment option, with achievement of excellent response rates and an acceptable toxicity profile, similar to reports in younger trial populations [6, 9]. In our study, ICIs achieved an ORR of 57%, with 12-month OS and PFS of 63% and 41%, respectively. Of note, these 12-month survival statistics are lower than what was reported in the original phase 2 cemiplimab trial [6] (12-month OS 81% and PFS 53%), but are considerably higher than what would be expected with other treatment options such as chemotherapy or cetuximab (median OS 8.1 months, median PFS 4.1 months) [21]. As we only included patients ≥ 70 years, the median age of our patients of 81.8 years is higher than that for the key registrational studies (pembrolizumab 72 years, cemiplimab 71 years) and other real-world reports [6, 9, 14, 15]. Thus, the higher median age should be taken into consideration when reviewing the survival data for our study, as we are reporting on an older, frail, and comorbid population. Despite 17 patients in this cohort having died at study follow-up, most (n = 11) died from causes independent of their CSCC and its treatment. Our findings add to the growing literature base supporting the use of ICIs as a tolerable and effective treatment option for older patients [14, 15].
Our cohort is noteworthy for including a high proportion of ECOG ≥ 2 (n = 18, 34%) and immunocompromised (n = 18, 34%) patients. Strippoli et al. reported on a cohort of 30 older patients with advanced CSCC treated with cemiplimab and demonstrated an ORR of 76.7% (n = 23), including nine complete responses. The median PFS and OS were 16 and 18 months, respectively [22]. This Italian cohort included a predominance of patients with locally advanced disease (83.3%), which is in contrast to our predominantly metastatic cohort (73.6%). The Italian cohort also had fewer patients with poorer performance status and less immunocompromised patients, which may have contributed to the observed higher responses than those described in our report. A similar real-world report in a Canadian cohort reported a higher 12-month PFS (58.1%) and OS (76.7%) than we identified in our cohort. However, it must be noted that our cohort included patients with a median age of 81.8 years in contrast to 75.4 years in this study. Additionally, we had a higher number of ECOG 2 and 3 patients (34% vs 28%) [23].
ECOG performance status is an established prognostic marker in patients with advanced malignancies and correlates with OS [24]. A good performance status (ECOG ≤ 1) has thus become an important inclusion criterion for most clinical trials. However, whether as a consequence of their diagnosis, comorbidity, and/or age, patients with advanced cancer frequently have ECOG scores of ≥ 2, which requires the clinician to extrapolate findings from trial-eligible populations. In this study, we demonstrate that ECOG 0 and 1 patients derive benefit from ICIs; however, for ECOG ≥ 2 patients this benefit is markedly less, with a 12-month OS less than 40%. This finding is important to note when balancing discussions on the benefit of treatment relative to risks or impact on quality of life. Whilst ECOG 2 patients are still likely to derive benefit from the use of ICIs for their advanced CSCC, this benefit does appear smaller than for those with a better ECOG score. This highlights the pertinent role ECOG still plays in treatment decision making.
Despite all our participants being aged ≥ 70 years, we identified comparable toxicity to what was seen in the registrational ICI studies, with most irAEs being low grade. This is noteworthy given there are often concerns regarding the safety and tolerability of systemic cancer therapies in older patients. We also noted that although six of our patients with an autoimmune disease experienced an irAE, only three patients experienced an autoimmune disease-related flare. Of the 11 patients with autoimmune disease reported on by Baggi et al. in an Italian cohort, eight experienced an adverse event, but only two had to discontinue treatment from the toxicity [15]. Overall, whilst these numbers are small, there is growing retrospective data in this space for other tumour types demonstrating that ICIs can be safely given in certain patients with autoimmune disease and that irAEs or flares of autoimmune disease may even be associated with better efficacy [25].
The CCI represents a validated and widely recognised index of comorbidity that is frequently used in cancer studies [26, 27]. A large audit of colorectal cancer patients in the South Australian Cancer Registry, for example, found that increasing comorbidity was associated with increased cancer-specific and other cause mortality [28], and in head and neck malignancies, higher CCI values are associated with poorer OS [29]. Whilst our cohort was comorbid (mean CCI 8.5), we did not identify any association between CCI and OS or PFS in univariate analysis. Comorbidity was not evaluated in univariate or multivariate survival analyses for the other large real-world publications, but Strippoli et al. did report that having no comorbidity was associated with a more favourable ORR [14, 15, 22]. Comorbid patients are more likely to have compromised functional reserves, and thus there is a theoretical concern that these patients will face higher morbidity and mortality from immune-related toxicity, as has historically been seen with chemotherapy. For example, in the prospective MOST study, looking at patients aged ≥ 70 years who received chemotherapy for colon cancer, authors reported that during the first 500 days, 49.5% of patients experienced grade 3–4 toxicity and 30% of patients died [30]. However, despite our cohort being both comorbid and older, there were no patient deaths from treatment-related toxicity and the overall safety profile appeared acceptable.
There were 14 patients in our cohort who had locoregionally advanced disease. For many cases of locoregionally advanced CSCC, radiotherapy remains a treatment option; however, it too comes with the potential for toxicity. Whilst all patients included in this study were required to have a multidisciplinary discussion to ensure curative radiotherapy was not an option for them, there is growing interest in the use of ICIs in those for whom the morbidity of radiotherapy is deemed unacceptable. For example, there are now reports of ICIs in periorbital CSCC resulting in deep and durable responses in patients who declined curative surgery and/or radiotherapy due to concerns around the loss of their vision [31]. A single-centre retrospective review on the outcomes of radiotherapy for CSCC of the head and neck region reported radiotherapy could be well tolerated in an older cohort with CSCC without a significant impact on quality of life [2]. However, the toxicities associated with radiation can differ significantly in the aesthetically sensitive region of the head and neck based on the precise location treated, with common toxicities such as dermatitis, skin fibrosis, and alopecia to more specific toxicities such as ocular toxicity, mucositis, and xerostomia [32]. Thus a strong collaborative and multidisciplinary approach in the management of advanced CSCC remains paramount.
The limitations of this study include its retrospective nature, variation in imaging modality used for tumour assessment, lack of central review of imaging and disease assessments, and that imaging assessment intervals occurred as per standard of care, thus reducing the precision of PFS estimates. Additionally, whilst this study is, to the best of our knowledge, the largest real-world report in an older cohort with advanced CSCC treated with ICIs, it is still limited by its small sample size, and thus definitive conclusions cannot be reached.
Our study demonstrates that ICIs can be considered as an acceptable treatment option in select older patients with advanced CSCC. This is particularly noteworthy given this older cohort consisted of a large number of comorbid, frail, and immunocompromised patients. The results of this study also reinforce the importance of ECOG score in selecting older advanced CSCC patients for ICIs.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Haehl E, Rühle A, Klink R, Kalckreuth T, Sprave T, Gkika E, et al. The value of primary and adjuvant radiotherapy for cutaneous squamous cell carcinomas of the head-and-neck region in the elderly. Radiat Oncol. 2021;16(1):105.
Keim U, Katalinic A, Holleczek B, Wakkee M, Garbe C, Leiter U. Incidence, mortality and trends of cutaneous squamous cell carcinoma in Germany, the Netherlands, and Scotland. Eur J Cancer. 2023;183:60–8.
Thai AA, Lim AM, Solomon BJ, Rischin D. Biology and treatment advances in cutaneous squamous cell carcinoma. Cancers (Basel). 2021;13(22):5645.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Migden MR, Rischin D, Schmults CD, Guminski A, Hauschild A, Lewis KD, et al. PD-1 blockade with cemiplimab in advanced cutaneous squamous-cell carcinoma. N Engl J Med. 2018;379(4):341–51.
Rischin D, Migden MR, Lim AM, Schmults CD, Khushalani NI, Hughes BGM, et al. Phase 2 study of cemiplimab in patients with metastatic cutaneous squamous cell carcinoma: primary analysis of fixed-dosing, long-term outcome of weight-based dosing. J Immunother Cancer. 2020;8(1): e000775.
Rischin D, Khushalani NI, Schmults CD, Guminski A, Chang ALS, Lewis KD, et al. Integrated analysis of a phase 2 study of cemiplimab in advanced cutaneous squamous cell carcinoma: extended follow-up of outcomes and quality of life analysis. J Immunother Cancer. 2021;9(8): e002757.
Grob JJ, Gonzalez R, Basset-Seguin N, Vornicova O, Schachter J, Joshi A, et al. Pembrolizumab monotherapy for recurrent or metastatic cutaneous squamous cell carcinoma: a single-arm phase II trial (KEYNOTE-629). J Clin Oncol. 2020;38(25):2916–25.
Sedrak MS, Mohile SG, Sun V, Sun CL, Chen BT, Li D, et al. Barriers to clinical trial enrollment of older adults with cancer: a qualitative study of the perceptions of community and academic oncologists. J Geriatr Oncol. 2020;11(2):327–34.
Nebhan CA, Cortellini A, Ma W, Ganta T, Song H, Ye F, et al. Clinical outcomes and toxic effects of single-agent immune checkpoint inhibitors among patients aged 80 years or older with cancer: a multicenter international cohort study. JAMA Oncol. 2021;7(12):1856–61.
Yancik R, Ries LA. Cancer in older persons: an international issue in an aging world. Semin Oncol. 2004;31(2):128–36.
Lichtman SM. Therapy insight: therapeutic challenges in the treatment of elderly cancer patients. Nat Clin Pract Oncol. 2006;3(2):86–93.
Hober C, Fredeau L, Pham-Ledard A, Boubaya M, Herms F, Celerier P, et al. Cemiplimab for locally advanced and metastatic cutaneous squamous-cell carcinomas: real-life experience from the French CAREPI study group. Cancers (Basel). 2021;13(14):3547.
Baggi A, Quaglino P, Rubatto M, Depenni R, Guida M, Ascierto PA, et al. Real world data of cemiplimab in locally advanced and metastatic cutaneous squamous cell carcinoma. Eur J Cancer. 2021;157:250–8.
Salas M, Henderson M, Sundararajan M, Tu N, Islam Z, Ebeid M, et al. Use of comorbidity indices in patients with any cancer, breast cancer, and human epidermal growth factor receptor-2-positive breast cancer: a systematic review. PLoS ONE. 2021;16(6): e0252925.
Zhao L, Leung L-H, Wang J, Li H, Che J, Liu L, et al. Association between Charlson comorbidity index score and outcome in patients with stage IIIB-IV non-small cell lung cancer. BMC Pulm Med. 2017;17(1):112.
Johns AC, Wei L, Grogan M, Hoyd R, Bridges JFP, Patel SH, et al. Checkpoint inhibitor immunotherapy toxicity and overall survival among older adults with advanced cancer. J Geriatr Oncol. 2021;12(5):813–9.
World Health Organization. WHO handbook for reporting results of cancer treatment (WHO Offset Publication no 48). Geneva: WHO, 1979. https://apps.who.int/iris/bitstream/handle/10665/37200/WHO_OFFSET_48.pdf?sequence=1&isAllowed=y. Accessed Oct 2023.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):122s–50s.
Maubec E, Petrow P, Scheer-Senyarich I, Duvillard P, Lacroix L, Gelly J, et al. Phase II study of cetuximab as first-line single-drug therapy in patients with unresectable squamous cell carcinoma of the skin. J Clin Oncol. 2011;29(25):3419–26.
Strippoli S, Fanizzi A, Quaresmini D, Nardone A, Armenio A, Figliuolo F, et al. Cemiplimab in an elderly frail population of patients with locally advanced or metastatic cutaneous squamous cell carcinoma: a single-center real-life experience from Italy. Front Oncol. 2021;11: 686308.
Koch Hein EC, Vilbert M, Hirsch I, Fernando Ribeiro M, Muniz TP, Fournier C, et al. Immune checkpoint inhibitors in advanced cutaneous squamous cell carcinoma: real-world experience from a Canadian Comprehensive Cancer Centre. Cancers (Basel). 2023;15(17):4312.
Jang RW, Caraiscos VB, Swami N, Banerjee S, Mak E, Kaya E, et al. Simple prognostic model for patients with advanced cancer based on performance status. J Oncol Pract. 2014;10(5):e335–41.
Rakshit S, Molina JR. Immunotherapy in patients with autoimmune disease. J Thorac Dis. 2020;12(11):7032–8.
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM. How to measure comorbidity. A critical review of available methods. J Clin Epidemiol. 2003;56(3):221–9.
Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012;50(12):1109–18.
Pule ML, Buckley E, Niyonsenga T, Roder D. The effects of comorbidity on colorectal cancer mortality in an Australian cancer population. Sci Rep. 2019;9(1):8580.
Habbous S, Harland LT, La Delfa A, Fadhel E, Xu W, Liu FF, et al. Comorbidity and prognosis in head and neck cancers: differences by subsite, stage, and human papillomavirus status. Head Neck. 2014;36(6):802–10.
Retornaz F, Guillem O, Rousseau F, Morvan F, Rinaldi Y, Nahon S, et al. Predicting chemotherapy toxicity and death in older adults with colon cancer: results of MOST study. Oncologist. 2020;25(1):e85–93.
McLean LS, Lim AM, Webb A, Cavanagh K, Thai A, Magarey M, et al. Immunotherapy to avoid orbital exenteration in patients with cutaneous squamous cell carcinoma. Front Oncol. 2021;11: 796197.
Majeed H, Gupta V. Adverse Effects of Radiation Therapy 2023 [Available from https://www.ncbi.nlm.nih.gov/books/NBK563259/.]
Acknowledgements
Cemiplimab was provided via a Sanofi Managed Access Program. Sanofi was not involved in the design, collection, analysis, interpretation, or reporting of the data, but was given the opportunity to review the publication prior to submission. The decision to submit for publication was made by the authors independently. Luke S. McLean would like to acknowledge the support of a National Health and Medical Research Council (NHMRC) post-graduate research scholarship. This study was presented in abstract and poster form at the Society for Immunotherapy of Cancer Annual Meeting in 2022.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This study was funded by an NHMRC Investigator Grant (APP1175929) held by Danny Rischin.
Conflict of Interest
Author Luke S. Mclean has received speaker honorarium and conference registration support from Sanofi and travel support/conference registration support from Merck, Sharpe & Dohme. Author Annette M. Lim provides uncompensated consultancy for Eisai and receives salary support from a Peter MacCallum Cancer Centre Discovery Partner Fellowship and institutional support from Sanofi/Regeneron Pharmaceuticals. Author Alesha A. Thai has received honorarium and is an advisory board member with BMS, Merck, La Roche Posay, and Akesobio. Author Danny Rischin is a member of trial steering committees and/or advisory boards (all uncompensated)—MSD, GSK, Regeneron, and Sanofi. He receives institutional trial funding from Merck Sharp & Dohme, Decibel Therapeutics, Bristol-Myers Squibb, GSK, Roche, Regeneron, Kura Oncology, and ALX Oncology. Author Mathias Bressel has no conflicts of interest that might be relevant to the contents of this article.
Ethics Approval/Consent to Participate/Consent to Publication
This retrospective study was approved by the Human Research Ethics Committee (HREC) (HREC/68865/PMCC) of the Peter MacCallum Cancer Centre, Melbourne, Australia, with a waiver for patient consent granted.
Availability of Data and Material
The datasets generated during and/or analysed during the current study are not authorised to be publicly available under the current ethics approval. However, any queries regarding the datasets generated and analysed for this project may be directed to the corresponding author.
Code Availability
Any queries regarding the code used for the analyses in this study may be directed to the corresponding author.
Authors’ Contributions
Authors LSM, AML, AAT, and DR contributed to the study concept and design. LSM and MB contributed to the data collection and analysis. The first draft of the manuscript was written by LSM. All authors commented on previous versions of the manuscript and read and approved the final version.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
McLean, L.S., Lim, A.M., Bressel, M. et al. Real-World Experience of Immune-Checkpoint Inhibitors in Older Patients with Advanced Cutaneous Squamous Cell Carcinoma. Drugs Aging 41, 271–281 (2024). https://doi.org/10.1007/s40266-024-01095-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-024-01095-z