Abstract
Background
Improving or maintaining quality of life (QoL) is an important aim for caring for people with dementia living in residential aged care facilities (RACFs).
Objectives
This study aimed to investigate the effect of a specific intervention, the Medication Management Consultancy (MMC), on the QoL of residents of RACFs in Western Australia, and to examine the association between psychotropic medications and QoL.
Methods
A before-after study was conducted. Staff from four RACFs participated in the MMC, and 56 residents with dementia from these RACFs were included. The MMC consisted of an online interactive staff education training course comprising educational videos, and a case study encompassing non-pharmacological strategies, person-centred care for behavioural and psychological symptoms of dementia (BPSD), and strategies to reduce the use of antipsychotics. Following the training, posters, reference cards, reminder stickers, administration of the Older Age Psychotropic Quiz (OAPQ), and 30-min video conferences with action groups in RACFs were utilised. At baseline (T0), QoL, neuropsychiatric symptoms (NPS) and staff distress, cognition, and activities of daily living were assessed by QoL in Alzheimer’s Disease (QoL-AD), Neuropsychiatric Inventory–Questionnaire (NPI-Q), Standardised Mini-Mental State Examination (SMMSE) and Bristol Activity of Daily Living Scale (BADLS), respectively, and repeated at 6 (T1) and 12 months (T2). Medication data were obtained from residents’ medication charts.
Results
At baseline, of the 56 participants, 33 completed the study. Compared with baseline (31.2, 95% confidence interval [CI] 28.9–33.6), QoL significantly improved at 6 months (33.5, 95% CI 30.9–36.0; p < 0.001) but not from baseline to 12 months (31.09, 95% CI 28.5–33.7; p = 0.58). The NPI-Q severity (residents) significantly improved from 9 (interquartile range [IQR] 11) at T0 to 6 (IQR 9.5) at T1 (p = 0.014) and to 7 (IQR 11) at T2 (p = 0.026). The medians of NPI-Q distress (staff) significantly improved from 12 (IQR 13.5) at T0 to 8 (IQR 9) at T1 (p = 0.013) and to 6 (IQR 11.5) at T2 (p = 0.018). Monthly doses of antipsychotics declined significantly by 51.8% at 6 months (p = 0.003) and by 43.5% at 12 months (p = 0.003); antidepressant doses declined significantly by 25.4% at 6 months (p = 0.013) and by 39.4% at 12 months (p = 0.016); benzodiazepines doses remained stable. QoL and use of psychotropics, age, sex, NPI-severity, and BADLS were not correlated.
Conclusion
The MMC was associated with improvement in QoL, NPS, staff distress, and reduction in monthly use of antipsychotics and antidepressants among RACF residents. There was no correlation between improved QoL and reduction in use of psychotropic medications, but due to the limitations of our study, this should be confirmed in additional studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The Medication Management Consultancy (MMC) intervention was associated with improved quality of life (QoL) of residents in Australian residential aged care facilities (RACFs) despite the lack of an association between QoL and psychotropic medication use, indicating the importance of non-pharmacological strategies in the care of RACF residents with dementia. |
The MMC was associated with a significant decrease in neuropsychiatric symptoms and staff distress, and a reduction in the use of antipsychotics and antidepressants over 12 months, but not benzodiazepines. |
Reduction in the use of antipsychotics and antidepressants was not associated with a negative effect on residents and care staff following the intervention, which may reassure health care workers who may be concerned of its adverse effect on residents. |
1 Introduction
Dementia is the second leading cause of death in Australia. Over half (53%) of all people in residential aged care facilities (RACFs) are diagnosed with dementia, a condition marked by psychiatric symptoms and decline in cognition [1]. It is estimated that more than 90% of people living with dementia (PWD) experience one or more psychiatric symptoms, such as psychosis, sleep disturbance, anxiety, apathy, and depressed mood, that adversely affect their psychological and behavioural function, and overall quality of life (QoL) [2]. These conditions are collectively known as neuropsychiatric symptoms (NPS) [3]. In most circumstances, person-centred, non-pharmacological approaches are the recommended first-line measures to prevent and manage most NPS [4], such as light therapy, aromatherapy, music therapy, massage, pet therapy, reminiscence therapy and meaningful activities [5]. Pharmacological options should only be considered when first-line treatments are ineffective at reducing NPS, or when there is a safety risk to residents and/or caregivers [6]. There are several reasons for minimising the use of medication for NPS. First, dementia is usually associated with multimorbidity, therefore PWD frequently experience polypharmacy. In addition, age-related pharmacokinetic and pharmacodynamic changes enhance the potential risk for inappropriate use of medications due to drug-disease or drug-syndrome interactions, and undesirable drug–drug interactions [7]. All these increase the complexity of optimisation of medication in PWD [8].
Psychotropic medications, particularly antipsychotics, antidepressants, and benzodiazepines, are often used in Australian RACFs to manage NPS, despite their modest effectiveness and considerable adverse effects [9, 10]. The proportion of RACF residents in Australia regularly prescribed at least one antipsychotic medication ranges from 13 to 42% depending on the RACF, and an average of 26% has not declined in the last 20 years [11]. The Royal Commission into Aged Care Quality and Safety highlighted the overuse of psychotropic medications in Australia’s aged care system, identifying this as being an urgent issue that needs to be addressed immediately [12]. Although psychotropics may help reduce NPS in certain circumstances, severe adverse reactions, including cerebrovascular events and death, have been associated with psychotropics when used for the proposed indication, and their overall benefits, relative to harm, remain uncertain [13].
Maintaining or improving QoL of PWD who reside in RACFs is a major priority for clinicians and policymakers [14]. The World Health Organization (WHO) has defined QoL as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards, and concerns. It is a broad ranging concept affected in a complex way by the person’s physical health, psychological state, level of independence, social relationships, personal beliefs and their relationship to salient features of their environment” [15].
The effect of psychotropic medications on QoL when used for NPS is uncertain. In one study of 288 RACF residents with moderate to severe dementia, psychotropic medications adversely affected QoL (as measured by the Quality of Life for People with Dementia [QUALIDEM] questionnaire) [16]. Conversely, in the study by Ballard et al. of 187 PWD with NPS in RACFs, cessation of antipsychotics negatively affected QoL when assessed using the Dementia Quality of Life measure (DEMQOL)-proxy domains for negative emotions and appearance. However, the negative effect was reversed with increased social interaction and staff training in person-centred care [17]. A systematic review and meta-analysis of several types of interventions that aimed to reduce inappropriate use of medication in RACFs, including psychotropics, found a limited effect on QoL, although medication appropriateness was improved [8].
In view of these incongruent findings, the effects of psychotropics on QoL in PWD experiencing NPS warrant thorough investigation. Adequate knowledge regarding dementia and increased self-efficacy among RACF staff in responding to NPS is associated with positive outcomes for residents [18]. Therefore, we hypothesised that an educational intervention may result in more judicious and appropriate management of NPS, which eventually improves QoL.
The objectives of this study were to (1) investigate the effect of an educational intervention on QoL of PWD; and (2) examine the association between psychotropic medications and QoL among PWD residing in RACFs.
2 Methods
2.1 Study Design
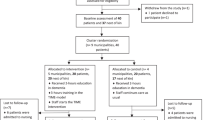
This study, conducted between 25 November 2019 and 11 May 2021, was a subset of a larger cluster randomised control trial (CRCT) involving 11 RACFs consisting of five intervention sites (comprising the intervention group) and six control sites receiving usual care (control group) [19]. Each cluster was randomised to receive the intervention or usual care. Due to difficulties associated with one RACF (n = 24 residents), including multiple managers in a short period, staff shortage, staff turnover, and ongoing accreditation of the facility (resulting in an inability to recruit residents), only four of the five RACFs in the intervention group were enrolled in this substudy of the CRCT. Moreover, the lack of recruitment of residents from control group RACFs was due to the before-after study design in a single group of residents. Therefore, all participants were recruited from the four RACFs in the intervention group.
2.2 Participants and Setting
A power calculation using G*Power (version 3.1.3; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) [20] was performed. Assuming p = 0.05, a power of 80%, and an effect size of 0.5, the required sample size was calculated to be 34.
The inclusion criteria for this study were age ≥ 65 years, diagnosed with dementia, permanent residents of RACFs in Australia, and ability to either consent to be part of the study or have a proxy (a close family member) who could provide consent on behalf of participants. Participants who were transferred, developed severe diseases, or died during the study were excluded from further analysis.
2.3 Intervention
The Medication Management Consultancy (MMC) is a support service for RACF staff enabling them to understand NPS and reduce the use of psychotropic medications among residents at the facility [21]. The MMC is administered by Dementia Training Australia (DTA), a consortium of universities and a peak dementia advocacy body. Detailed information about the intervention has been published elsewhere [19]. Briefly, it is a 6-month programme that consists of initial training followed by a facilitated intervention. The interventional training, delivered online with videos and a case study, encompasses person-centred care, non-pharmacological strategies for NPS, and strategies to minimise the use of psychotropics. Upon receiving training, DTA consultants conduct video conference meetings with key care staff at the RACF every 2–4 weeks to develop, implement, and evaluate strategies to review psychotropic use for NPS management. Participants were assessed at baseline (T0) and again at 6 (T1) and 12 months (T2) after initiating the MMC intervention.
2.4 Ethics
Ethical approval was obtained from the University of Western Australia Human Research Ethics Committee prior to the commencement of the study (Reference RA/4/20/4792). The study is registered on the Australian New Zealand Clinical Trials registry (at https://anzctr.org.au ACTRN12620000268943). The participants and/or their proxy (close families) were informed about the study and written consent was obtained. All participants could withdraw from the study at any time without any reprisals.
2.5 Assessment of Psychotropic Drug Use
Antipsychotics, antidepressants, and benzodiazepines are the three classes of psychotropic drugs most frequently used for NPS treatment in Australia [22]. All antipsychotics, antidepressants, and benzodiazepines were classified according to the Anatomical Therapeutic Chemical (ATC) classification system [23], and their doses and frequency of administration recorded. For each participant, the doses of antipsychotics, antidepressants, and benzodiazepines were first retrieved from participants’ medical files, and then converted to olanzapine, fluoxetine, and diazepam equivalents, respectively [24,25,26]. The total equivalent dose per month per participant per drug class was calculated based on the following formula: strength of specific medication × number of doses per day divided by the defined daily dose (DDD), which is defined by the WHO as the assumed average maintenance dose per day for a drug used for its main indication in adults [27]. The total dose equivalents for each medication were calculated and added together if the resident took more than one agent in the same psychotropic class.
2.6 Assessment of Quality of Life (QoL)
The researcher (HA) administered the QoL in Alzheimer’s Disease (QoL-AD), a short, valid, and reliable measure [28] for all participants to measure their QoL. All study participants responded to the QoL-AD and the interview was carried out with the resident without the involvement of either the family or caregiver.
The 13 items of the QoL-AD include physical health, energy level, mood level, living situation, memory, family, marriage, friends, self as a whole, ability to do chores, ability to do things for fun, money, and life as a whole [28] The participants chose one of four options and scored it from poor (1 point), fair (2 points), good (3 points), to excellent (4 points), giving a possible total score range from 13 to 52, with higher scores representing better QoL [29] for PWD. The study researcher assessed QoL at T0, T1, and T2.
2.7 Assessment of Neuropsychiatric Symptoms
NPS exhibited by participants in the study was measured by care staff at RACFs using the Neuropsychiatric Inventory–Questionnaire version (NPI-Q). The NPI-Q was used in preference to the NPI nursing home version (NPI-NH) due to staff time implications. The 12 NPI-Q domains include delusions, hallucination, agitation/aggression, depression/dysphoria, anxiety, elation/euphoria, apathy/indifference, disinhibition, irritability/lability, motor disturbance, night-time behaviours, and appetite/eating [30].
Care staff distress scores were obtained using the NPI-Q by rating the frequency of occurrence of a specific behaviour domain and the level of severity (1 = mild, 2 = moderate, 3 = severe). Staff rated their distress ranging from 0 to 5 points (0 = no distress, to 5 = very severe distress) for each positive neuropsychiatric domain, and the total NPI-Q score for residents is calculated independently of that of NPI-Q staff.
The maximum overall score was the sum of the severity (36 points) and distress (60 points) scores, with higher scores representing more serious symptoms and greater distress for the caregiver. The professional caregiver assessed NPI-Q at T0, T1, and T2.
2.8 Cognition Assessment
The researcher (HA) assessed cognitive impairment using the Standardised Mini-Mental State Examination (SMMSE), whose total score ranged from 0 (worst) to 30 (best) [31] at T0, T1, and T2.
2.9 Activity of Daily Living Assessment
The participant’s ability to carry out daily activities such as dressing, using transport and preparing food was assessed using the 20-item Bristol Activity of Daily Living Scale (BADLS) questionnaire [32]. The BADLS total score ranges from 0 (totally independent) to the maximum score of 60 (totally dependent). This assessment was administered by the researcher (HA) and rated by care staff at the RACFs at T0, T1 and T2.
2.9.1 Data Collection
Data on age, sex and drugs were retrieved from participants’ medical files. Data on participants’ use of psychotropic drugs of interest (antipsychotics, antidepressants, and benzodiazepines) were collected at T0, T1, and T2. QoL, NPI-Q, NPI-distress, SMMSE, and BADLS were reassessed at T1 and T2 timepoints.
2.9.2 Statistical Analysis
The Shapiro–Wilk W test was performed to test the normality of variables. The distribution of each variable was examined by inspecting histograms, quantile–quantile (Q–Q) and box plots. Normally distributed continuous data were presented as mean and mean change, and non-parametric variables were presented as median and interquartile range (IQR). Categorical variables were expressed as percentages. Difference in baseline variables between residents with full follow-up and residents who were lost to follow-up were compared using Chi-square tests.
Associations between psychotropic medications and variables (QoL, NPI-Q severity, NPI-Q distress, SMMSE, BADLS scores) were tested using Spearman’s rho.
QoL outcome scores were normally distributed and Student’s t tests were used to examine the differences between QoL at T0, T1, and T2. Factors associated with the QoL-AD were investigated by bivariate analysis (Wilcoxon rank tests or Spearman’s rho as appropriate). The results are presented with their associated 95% confidence intervals. For all analyses, p < 0.05 was considered statistically significant.
All analyses were performed using IBM SPSS Statistics, version 27 (IBM Corporation, Armonk, NY, USA).
3 Results
Of the 56 participants enrolled at baseline, 33 (58.9%) completed the study to yield data for three time points (T0, T1 and T2). There were 13 deaths, 3 were transferred, and 7 were hospitalised with severe disease. The baseline characteristics of the study participants are presented in Table 1. The average age of the participants was 80.2 years and participants were predominantly male (60.7%).
Following the intervention, there was a significant improvement in the mean QoL score from baseline (31.2, 95% CI 28.9–33.6) to T1 (33.5, 95% CI 30.9–36.0, p < 0.001; mean percentage change = +7.1) (Fig. 1).
There was a non-significant reduction in QoL score between baseline and 12 months (31.09, 95% CI 28.512–33.669, p = 0.58; mean percentage change = − 0.5).
A significant correlation between NPI-severity and antipsychotic use was noted at baseline (r = 0.612, p < 0.001), with more severe NPS correlated with greater use of antipsychotics. An overall improvement in NPI-severity and NPI-distress was noted. The medians of NPI-Q severity (residents) improved from 9 (IQR 11) at T0 to 6 (IQR 9.5) at T1 (p = 0.014) and to 7 (IQR 11) at T2 (p = 0.026). The medians of NPI-Q distress (staff) improved from 12 (IQR 13.5) at T0 to 8 (IQR 9) at T1 (p = 0.013) and to 6 (IQR 11.5) at T2 (p = 0.018). A strong correlation was found between NPI-Q severity (residents) and NPI-Q distress (staff) at T2 (r = 0.75, p Spearman’s rho < 0.001).
There were no significant associations between QoL and total equivalent doses (mg) of psychotropics/month, as well as age, sex, NPI, and BADLS (Table 2).
When measured as the monthly median equivalent dose (mg), the use of antipsychotics and antidepressants declined significantly—antipsychotics by 51.8% between T0 and T1, and by 43.5% between T1 and T2; antidepressant doses decreased by 25.4% and 39.4% between T0 and T1, and T1 and T2, respectively (Table 3). However, the use of benzodiazepines remained stable between T0 and T1, and declined by 33% between T1 and T2, albeit very few residents used benzodiazepines (Table 3).
The proportion of participants using antipsychotic medications significantly decreased from T0 to T1, but increased between T1 and T2. However, the proportion of participants using antidepressants decreased throughout the study period. Benzodiazepine use remained stable from T0 to T1, but decreased non-significantly between T1 and T2 (Table 3).
4 Discussion
This study aimed to evaluate the effect of the MMC on QoL of PWD in RACFs and psychotropic medication use within this population. The results indicate that the MMC is associated with an improvement in the QoL of PWD in RACFs, and a concurrent decrease in antipsychotic and antidepressant use, although the QoL improvement was significant only at 6 months. Our results suggest that the MMC potentially led staff to use non-pharmacological approaches for NPS, which reduced reliance on potentially harmful antipsychotics and antidepressants, while encouraging person-centred care. Hence, the QoL of residents improved independent of the reduction in medications. These findings strongly support practice guidelines and principles of care for PWD, which recommend non-pharmacological interventions for managing NPS in preference to psychotropic medications [33]. The implementation of such guidelines requires staff education and support, and our findings indicate that programmes such as the MMC have substantial potential to improve outcomes for PWD living in RACFs.
The MMC successfully reduced antipsychotic and antidepressant use but did not reduce the benzodiazepine doses over 12 months. This may be attributed to the fact that the main focus of the MMC intervention was antipsychotic use. Additionally, the sample size may not be sufficient to detect changes in the monthly dose of benzodiazepine use.
In the current study, the cessation of psychotropic medications was not associated with lower QoL among PWD in RACFs; rather, a short-term improvement in QoL was identified. The results of previous studies in this area have varied. A systematic review and meta-analysis reported that interventions that reduced psychotropic medication use in this population had no clear effect on residents’ QoL [8]. The study by Ito et al. of 431 residents with and without dementia [34] reported greater impairment of QoL with increased psychotropic drug use, independent of NPS severity. In that study, increased antidepressant use was associated with greater QoL in people with mild and moderate stages of dementia. However, unlike our study, the study by Ito et al. did not use data on the DDD of the psychotropic drugs, and included all residents with and without dementia. Hence, unlike our study, which only involved PWD, the QoL measures used by Ito et al. were of limited validity in those without cognitive impairment and its findings are somewhat questionable.
In a cross-sectional study of 541 participants with high levels of cognitive impairment and dementia from 17 Australian RACFs, Harrison et al. reported that greater use of psychotropic medications was associated with lower QoL, despite no significant correlation between the two variables [35]. While that study used Dementia QoL-Proxy (DEMQOL) to measure QoLs, which is subject to proxy bias, its findings are broadly consistent with those of the current study whereby the MMC intervention was associated with improved QoL while decreasing antipsychotic and antidepressant drug use. The Well-being and Health for People with Dementia (WHELD) intervention for residents with dementia was implemented in 69 UK nursing homes [36]. Following a 9-month intervention that focused on person-centred care training for care staff, antipsychotic review, and social interactions, there was a statistically significant improvement in QoL (DEMQOL-Proxy Z score 2.82, p = 0.0042; mean difference 2.54, standard error of the mean 0.88, 95% CI 0.81–4.28) compared with usual treatment. However, WHELD did not reduce antipsychotic use [36]. In contrast, we found a reduction in antipsychotic use in addition to QoL improvement.
The positive outcomes from the MMC intervention evaluated in this study support the premise that individualised, non-pharmacological approaches to NPS management may positively influence QoL of PWD living in RACFs. The MMC intervention robustly promotes person-centred care, activities, and social interactions, all of which are known to significantly improve QoL among PWD [36]. No specific non-pharmacological approaches were implemented in our study; rather, the MMC team promoted the use of individualised meaningful activities based on the information about the residents possessed by the RACF staff. Some of the non-pharmacological strategies utilised in the MMC that were previously reported from staff in our qualitative study [19] included small group activities, painting, listening to music, having casual conversations, and communicating with the residents. These interventions facilitated by RACF staff were straightforward to implement within the RACF’s capacity with regard to staffing levels and/or cost.
Reduction in care staff distress was a benefit realised through the intervention, which complemented the positive outcomes achieved for the RACF residents in our study. An educational behaviour change intervention for staff and medication review for PWD reported similar results in a qualitative study undertaken in the UK [37].
The significant correlation between severity of NPS manifested by participants and care staff distress at 12 months is not surprising, considering that caregivers’ distress and burden increase with residents’ NPS [38,39,40]. However, an important finding of this study was the significant reduction in distress among care staff and residents’ NPS over the course of 12 months, which may reassure clinicians that the reduction/cessation of psychotropic medication may not adversely affect residents, and in fact might affect RACF staff in a positive manner. This is in concordance with earlier studies that showed care staff distress due to resident’s NPS may contribute to enhanced psychotropic prescription [41]. Overall, our results are in line with the recommendation that non-pharmacological approaches be considered as first-line treatment due to the lower risk of adverse effects [34]. The findings indicate that the MMC intervention could serve as a component of the clinical management tool kit for PWD in RACFs.
This study also illustrates the need for ongoing staff support to maintain positive outcomes for PWD. The reduction in QoL scores at 12 months, although not significant, supports the sustainability of the intervention, as the intervention had ceased 6 months earlier. This emphasises the need for regular reinforcement of educational intervention programmes to achieve the desired effect among existing RACF staff, and train new staff following turnover. When conducted on an annual basis, the MMC educational intervention may be valuable for improving or maintaining residents’ QoL in a sustainable manner. While the effect of the coronavirus disease 2019 (COVID-19) pandemic and subsequent lockdown may have partly accounted for the decline in QoL at 12 months, previous studies in this area support the need for ongoing reinforcement to sustain positive outcomes [36, 42].
This study has several strengths, including a before-after study of 1-year duration, involving the MMC educational intervention to evaluate its impact on QoL, which is a clinically important outcome for older people. Second, confounding by indication is possible, although appears unlikely in our study because of the lack of association between psychotropic medications and QoL. Third, compared with other studies, the rate of retention of participants in our study was high. Lastly, we examined the impact of educational intervention on QoL in RACFs, which, despite its importance, is a neglected domain of research and investigated in a few studies.
This study is not without limitations. First, the generalisability of our findings may be affected by the participation of residents who were all from the same state in Australia, and were selected for inclusion by staff. Second, more females are affected by dementia than males worldwide (female-to-male ratio 1·69 [1·64–1·73]) [43], yet the majority of participants in our study were male, which may limit the generalisability of our findings.
Third, demographic differences between the groups at baseline and the loss to follow-up may lead to selection bias, and, consequently, there is a threat to the internal validity. Fourth, the use of a subset of clusters included in CRCT (four RACFs) may limit interpretation of the study results.
Fifth, the sample size was small due to the lack of parallel group controls and the challenges faced with recruiting RACFs and their residents. Sixth, staff turnover and the limitations due to the lockdown associated with the COVID-19 pandemic may have affected proper implementation of the intervention. Lastly, any heterogeneity in the prevalence of psychotropic medications between RACFs may have affected the outcome and must be considered.
5 Conclusions
The MMC for care staff helped achieve an optimal QoL for PWD living in RACFs. NPS, staff distress, and reduction in monthly use of antipsychotics and antidepressants among RACF residents following the intervention was noted. There was no correlation between improved QoL and reduction in the use of psychotropic medications, which may reflect the limitations of our study, and this should be confirmed in additional studies. Sustainable non-pharmacological approaches to manage NPS and improve the QoL of PWD in RACFs should be part of future programmes designed for this vulnerable population.
References
Australian Institute of Health and Welfare. Dementia. Canberra (ACT): Australian Institute of Health and Welfare. 2020. Available at: https://www.aihw.gov.au/reports/australias-health/dementia. Accessed 15 Mar 2021.
Bessey LJ, Walaszek A. Management of behavioral and psychological symptoms of dementia. Curr Psychiatry Rep. 2019;21(8):1–11. https://doi.org/10.1007/s11920-019-1049-5.
Phan SV, Osae S, Morgan JC, Inyang M, Fagan SC. Neuropsychiatric symptoms in dementia: considerations for pharmacotherapy in the USA. Drugs R&D. 2019;19(2):93–115. https://doi.org/10.1007/s40268-019-0272-1.
Loi SM, Eratne D, Kelso W, Velakoulis D, Looi JC. Alzheimer disease: non-pharmacological and pharmacological management of cognition and neuropsychiatric symptoms. Australas Psychiatry. 2018;26(4):358–65. https://doi.org/10.1177/1039856218766123.
Scales K, Zimmerman S, Miller SJ. Evidence-based nonpharmacological practices to address behavioral and psychological symptoms of dementia. Gerontologist. 2018;58(Suppl 1):S88–102. https://doi.org/10.1093/geront/gnx167.
McDermott CL, Gruenewald DA. Pharmacologic management of agitation in patients with dementia. Curr Geriatr Rep. 2019;8(1):1–11. https://doi.org/10.1007/s13670-019-0269-1.
Ruangritchankul S, Peel NM, Hanjani LS, Gray LC. Drug related problems in older adults living with dementia. PLoS One. 2020;15(7):e0236830. https://doi.org/10.1371/journal.pone.0236830.
Almutairi H, Stafford A, Etherton-Beer C, Flicker L. Optimisation of medications used in residential aged care facilities: a systematic review and meta-analysis of randomised controlled trials. BMC Geriatr. 2020;20(1):1–19. https://doi.org/10.1186/s12877-020-01634-4.
Westbury J, Gee P, Ling T, Kitsos A, Peterson G. More action needed: Psychotropic prescribing in Australian residential aged care. Aust N Z J Psychiatry. 2019;53(2):136–47. https://doi.org/10.1177/0004867418758919.
Almutairi H, Stafford A, Etherton-Beer C, Flicker L. Pattern of prescription of psychotropics (antipsychotics, antidepressants and benzodiazepines) in Western Australian residential aged care facilities. IMJ. 2021;51(12):2140–3. https://doi.org/10.1111/imj.15608.
Westaway K, Sluggett J, Alderman C, Moffat A, Procter N, Roughead E. The extent of antipsychotic use in Australian residential aged care facilities and interventions shown to be effective in reducing antipsychotic use: a literature review. Dementia. 2020;19(4):1189–202. https://doi.org/10.1177/1471301218795792.
Commonwealth of Australia: Royal Commission into Aged Care Quality and Safety. Interim Report. Commonwealth of Australia. https://agedcare.royalcommission.gov.au/sites/default/files/2020-02/interim-report-volume-1.pdf. Assessed 31 Oct 2019
Gerlach LB, Kales HC. Pharmacological management of neuropsychiatric symptoms of Dementia. Curr Treat Options Psych. 2020;7(4):489–507. https://doi.org/10.1007/s40501-020-00233-9.
Commonwealth of Australia: Royal Commission into Aged Care Quality and Safety. Final Report. Commonwealth of Australia. Available at: https://agedcare.royalcommission.gov.au/publications/final-report-list-recommendations. Accessed 2 Mar 2022
World Health Organisation. Programme on mental health. Geneva: World Health Organisation; 1998.
Wetzels R, Zuidema SU, de Jonghe JF, Verhey FR, Koopmans R. Determinants of quality of life in nursing home residents with dementia. Dement Geriatr Cogn Disord. 2010;29(3):189–97. https://doi.org/10.1159/000280437.
Ballard C, Orrell M, Sun Y, Moniz-Cook E, Stafford J, Whitaker R, et al. Impact of antipsychotic review and non-pharmacological intervention on health-related quality of life in people with dementia living in care homes: WHELD—a factorial cluster randomised controlled trial. Int J Geriatr Psychiatry. 2017;32(10):1094–103. https://doi.org/10.1002/gps.4572.
Bauer M, Fetherstonhaugh D, Haesler E, Beattie E, Hill KD, Poulos CJ. The impact of nurse and care staff education on the functional ability and quality of life of people living with dementia in aged care: a systematic review. Nurse Educ Today. 2018;67:27–45. https://doi.org/10.1016/j.nedt.2018.04.019.
Almutairi H, Stafford A, Etherton-Beer C, Flicker L, Saunders R. Aged care staff perceptions of an online training program for responsive behaviours of residents with dementia. Austalas J Ageing. 2021;20(1):1–19. https://doi.org/10.1111/ajag.13015.
Faul F, Erdfelder E, Lang AG, et al. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91. https://doi.org/10.3758/BF03193146.
Dementia Training Australia. Medication Management Consultancy Australia: Dementia Training Australia. 2021. https://dta.com.au/medication-management-consultancy/. Accessed 12 Apr 2021
Commonwealth of Australia: Royal Commission into Aged Care Quality and Safety. Psychotropic medications used in Australia—information for aged care. Commonwealth of Australia. https://www.agedcarequality.gov.au/sites/default/files/media/acqsc_psychotropic_medications_v11.pdf. Accessed 8 Mar 2021.
World Health Organisation (WHO) Collaborating Center for Drug Statistics Methodology. Anatomical Therapeutic Chemical Classification System. ATC/DDD Index. 2021. http://www.whocc.no/atc_ddd_index/. Accessed 8 Mar 2021
Leucht S, Samara M, Heres S, Davis JM. Dose equivalents for antipsychotic drugs: the DDD method. Schizophr Bull. 2016;42(Suppl 1):S90–4. https://doi.org/10.1093/schbul/sbv167.
Hayasaka Y, Purgato M, Magni LR, Ogawa Y, Takeshima N, Cipriani A, et al. Dose equivalents of antidepressants: evidence-based recommendations from randomized controlled trials. Affect Disord. 2015;180:179–84. https://doi.org/10.1016/j.jad.2015.03.021.
Drug and Alcohol Services South Australia. Benzodiazepines: information for GPs. 2014. https://www.sahealth.sa.gov.au/wps/wcm/connect/dbd6d500407749f193d6bb222b2948cf/Benzodiazepines+-+GPs-DASSA-August2014.pdf?MOD=AJPERES. Accessed 3 Mar 2021
World Health Organisation (WHO) Collaborating Centre for Drug Statistics Methodology. Norwegian Institute of Public Health. ATC/ DDD Index. https://www.whocc.no/atc_ddd_index/. Accessed 3 Mar 2021
Thorgrimsen L, Selwood A, Spector A, Royan L, de Madariaga LM, Woods R, et al. Whose quality of life is it anyway? The validity and reliability of the Quality of Life-Alzheimer’s Disease (QoL-AD) scale. Alzheimer Dis Assoc Disord. 2003;17(4):201–8. https://doi.org/10.1097/00002093-200310000-00002.
Torisson G, Stavenow L, Minthon L, Londos E. Reliability, validity and clinical correlates of the Quality of Life in Alzheimer’s disease (QoL-AD) scale in medical inpatients. Health Qual Life Outcomes. 2016;14(1):90. https://doi.org/10.1186/s12955-016-0493-8.
Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44(12):2308–14. https://doi.org/10.1212/wnl.44.12.2308.
Molloy DW, Standish TI. A guide to the standardized Mini-Mental State Examination. Int Psychogeriatr. 1997;9(Suppl 1):87–94. https://doi.org/10.1093/ageing/25.2.113.
Bucks RS, Ashworth D, Wilcock G, Siegfried K. Assessment of activities of daily living in dementia: development of the Bristol Activities of Daily Living Scale. Age Ageing. 1996;25(2):113–20. https://doi.org/10.1093/ageing/25.2.113.
Guideline Adaptation Committee: Clinical Practice Guidelines and Principles of Care for People with Dementia. 2016: Guideline Adaptation Committee. https://cdpc.sydney.edu.au/wp-content/uploads/2019/06/CDPC-Dementia-Guidelines_WEB.pdf. Accessed 3 Mar 2021.
Ito E, Berge LI, Husebo BS, Nouchi R, Sandvik RK. The negative impact of psychotropic drug use on quality of life in nursing home patients at different stages of dementia: cross-sectional analyses from the COSMOS Trial. J Am Med Dir Assoc. 2020;21(11):1623–8. https://doi.org/10.1016/j.jamda.2020.03.028.
Harrison SL, Bradley C, Milte R, Liu E, O’Donnell LK, Hilmer SN, et al. Psychotropic medications in older people in residential care facilities and associations with quality of life: a cross-sectional study. BMC Geriatr. 2018;18(1):1–8. https://doi.org/10.1186/s12877-018-0752-0.
Ballard C, Corbett A, Orrell M, Williams G, Moniz-Cook E, Romeo R, et al. Impact of person-centred care training and person-centred activities on quality of life, agitation, and antipsychotic use in people with dementia living in nursing homes: a cluster-randomised controlled trial. PLoS Med. 2018;15(2): e1002500. https://doi.org/10.1371/journal.pmed.1002500.
Maidment ID, Damery S, Campbell N, Seare N, Fox C, Iliffe S, et al. Medication review plus person-centred care: a feasibility study of a pharmacy-health psychology dual intervention to improve care for people living with dementia. BMC Psychiatry. 2018;18(1):1–11. https://doi.org/10.1186/s12888-018-1907-4.
Terum TM, Testad I, Rongve A, Aarsland D, Svendsboe E, Andersen JR. The association between specific neuropsychiatric disturbances in people with Alzheimer’s disease and dementia with Lewy bodies and carer distress. Int J Geriatr. 2019;34(10):1421–3. https://doi.org/10.1002/gps.5134.
Chen CT, Chang C-C, Chang W-N, Tsai N-W, Huang C-C, Chang Y-T, et al. Neuropsychiatric symptoms in Alzheimer’s disease: associations with caregiver burden and treatment outcomes. QJM Int J Med. 2017;110(9):565–70. https://doi.org/10.1093/qjmed/hcx077.
Aerts L, Cations M, Harrison F, Jessop T, Shell A, Chenoweth L, et al. Why deprescribing antipsychotics in older people with dementia in long-term care is not always successful: Insights from the HALT study. Int J Geriatr Psychiatry. 2019;34(11):1572–81. https://doi.org/10.1002/gps.5167.
Smeets CH, Gerritsen DL, Zuidema SU, Teerenstra S, van der Spek K, Smalbrugge M, et al. Psychotropic drug prescription for nursing home residents with dementia: prevalence and associations with non-resident-related factors. Aging Ment Health. 2018;22(9):1244–52. https://doi.org/10.1080/13607863.2017.1348469.
Westbury J, Tichelaar L, Peterson G, Gee P, Jackson S. A 12-month follow-up study of “RedUSe”: a trial aimed at reducing antipsychotic and benzodiazepine use in nursing homes. Int Psychogeriatr. 2011;23(8):1260–9. https://doi.org/10.1017/S1041610211000421.
Nichols E, Steinmetz JD, Vollset SE, Fukutaki K, Chalek J, Abd-Allah F, et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health. 2022;7(2):e105–25. https://doi.org/10.1016/S2468-2667(21)00249-8.
Acknowledgements
The involvement of DTA in facilitating this research is acknowledged with gratitude. DTA is supported by the Australian Government.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Hend Almutairi is supported by the University of Western Australia International Fee Scholarship (UIFS) and University Postgraduate Award (UPA). Leon Flicker is supported by a Medical Research Future Fund Next Generation Clinical Researchers Practitioner Fellowship no. 1155669. The funding sources had no role in the design of the study; collection, analysis, and interpretation of data; review or writing the manuscript; and decision to submit the manuscript for publication.
Conflicts of interest
Hend Almutairi, Christopher Etherton-Beer, and Leon Flicker declare that they have no conflicts of interest. Andrew Stafford was a former Director of DTA and remains engaged with the organisation as a periodic consultant.
Ethics approval
Ethical approval was obtained from the University of Western Australia Human Research Ethics Committee prior to the commencement of the study (reference RA/4/20/4792).
Consent to participate
Informed consent was obtained from all individual participants, or their close family member, included in the study.
Consent for publication
All authors approved the current manuscript for publication. All participants and or their family provided consent for publication of de-identified data.
Availability of data and material
The datasets generated and/or analysed during the current study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
Author contributions
Study conception and design: HA, AS, CE, LF. Analysis and interpretation of data: HA and LF. The first draft of the manuscript was written by HA. All authors critically revised, commented on the drafts, and read and approved the final version of the manuscript and agree to be accountable for the work presented.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Almutairi, H., Stafford, A., Etherton-Beer, C. et al. Association of Psychotropic Education with Quality of Life: A Before-After Study in Residential Aged Care Facilities. Drugs Aging 39, 949–958 (2022). https://doi.org/10.1007/s40266-022-00982-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-022-00982-7