Abstract
Insomnia is a pervasive sleep disorder affecting numerous patients across diverse demographical populations and comorbid disease states. Contributing factors are often a complex interaction of biological, psychological, and social components, requiring a multifaceted approach in terms of both diagnosis and management. In the setting of Alzheimer’s disease, insomnia is an even more complicated issue, with a higher overall prevalence than in the general population, greater complexity of contributing etiologies, and differences in diagnosis (at times based on caregiver observation of sleep disruption rather than subjective complaints by the individual with the disorder), and requiring more discretion in terms of treatment, particularly in regard to adverse effect profile concerns. There also is growing evidence of the bidirectional nature of sleep disruption and Alzheimer’s disease, with insomnia potentially contributing to disease progression, making the condition even more paramount to address. The objective of this review was to provide the clinician with an overview of treatment strategies that may have value in the treatment of disturbed sleep in Alzheimer’s disease. Nonpharmacological approaches to treatment should be exhausted foremost; however, pharmacotherapy may be needed in certain clinical scenarios, which can be a challenge for clinicians given the paucity of evidence and guidelines for treatment in the subpopulation of Alzheimer’s disease. Agents such as sedating antidepressants, melatonin, and site-specific γ-aminobutyric acid agonists are often employed based on historical usage but are not necessarily supported by high-quality trials. Newer agents such as dual orexin receptor antagonists have demonstrated some promise but still need further evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sleep disruption/insomnia in Alzheimer’s disease can be challenging to manage clinically. |
Work-up and treatment approaches should include consideration of all potential contributing factors to sleep disruption, with correction of issues through behavioral and nonpharmacological interventions whenever applicable first and foremost. |
Pharmacotherapy should be utilized on an individual basis with careful regard for the balance of risk and benefit. |
More high-quality trials are still needed for the evaluation of efficacy and safety of available pharmacological agents, particularly in the setting of Alzheimer’s disease. |
Potential benefit on cognitive function from improving the quality of sleep in Alzheimer’s disease remains somewhat uncertain, but would provide a coveted outcome if further established. |
1 Overview
Insomnia, defined as difficulty falling asleep, staying asleep, or waking up too early, along with resulting negative daytime consequences and functional impairment, is a widespread occurrence in the general population with point-prevalence estimates of 5–30% of individuals with the condition at any one time [1]. It often connotes a subjective complaint in people without dementia and has been associated with numerous physical and mental health consequences, along with significant quality-of-life concerns [2]. In the setting of Alzheimer’s disease (AD), the prevalence of insomnia is estimated to be even higher than that in the overall population, at around 40% [3, 4], and can present even more challenges in terms of management. In addition, the potentially sleep-related temporally specific behavioral agitation demonstrated by some patients, often subsumed under the rubric of “sundowning,” [5] represents a particularly acute management problem for a subset of dementia cases [6] and likely constitutes a syndrome extending beyond a diagnosis of insomnia per se. The perspective of insomnia as a purely subjective complaint must be modified to some extent when describing the sleep of people with dementia since caregiver observations of sleep difficulties in the individual with dementia may also meet the diagnostic criteria of the International Classification of Sleep Disorders 3rd Edition [7]. Symptoms may be supported or inferred at times by objective measures of sleep disruption, typically in the form of actigraphy, video presentation, and/or polysomnography (PSG).
AD is one of the most common forms of dementia, impacting up to 10% of the population aged > 65 years [8]. In 2010, the estimated number of patients aged > 65 years with AD was 4.7 million in the United States alone, with a projection to increase to 13.8 million by 2050 [9]. The neurodegenerative disease is thought to result from the accumulation of misfolded β-amyloid (Aβ) protein, which then has the propensity to conglomerate into plaque formation, along with concomitant aggregation of hyperphosphorylated tau proteins into neurofibrillary tangles, leading to disruption of neuronal structure and function. This results in progressive memory impairment and cognitive deficits, along with a multitude of negative sleep consequences, including increased fragmentation, disruption of circadian processes, and reduction in rapid eye movement (REM) sleep and sleep spindle quantity, thought in part to be due to disturbance of sleep-related neuronal structures, such as the suprachiasmatic nucleus (SCN) and lateral hypothalamus [10,11,12,13].
Elderly patients already often have worsened sleep quality because of the impact of other sleep-disruptive medical conditions, medications, mercurial living situations, less exercise, and weakened circadian entrainment through reduced social and photic zeitgebers [14]. It is estimated that close to 50% of elderly patients have some degree of trouble falling or staying asleep [15]. If we consider these contributors to symptoms of insomnia based on Spielman’s “3P” model, which dissects components negatively influencing sleep into predisposing, precipitating, or perpetuating factors [16], it is evident as to why this often occurs, with many different potentially sleep-disruptive scenarios being possible with increased age across biological, psychological, and behavioral realms. While there is often overlap between factors in the “3P” model as to the role they play in a patient’s insomnia, it is important to note that structural and functional neuronal abnormalities seen in AD have the potential to be predisposing, precipitating, and perpetuating constituents. It is also pertinent to note that, although behavioral interventions such as cognitive behavioral therapy for insomnia (CBT-i) can resolve or improve many of the contributors to symptoms of insomnia, they may not be able to overcome the sleep disruption caused by architectural changes in the brain as seen in conditions such as AD.
Even with “normal” aging mechanisms, PSG reveals a decrease in slow-wave sleep (SWS), delta-power, sleep efficiency (SE), and an increase in comorbid sleep disorders such as sleep-disordered breathing and periodic limb movements of sleep [17]. The added alterations of neuronal structure in AD can further exacerbate sleep disruption, resulting in an amplified worsening of sleep parameters already seen in aging [18]. Behavioral observations of sleep in an AD special care unit observed that this worsening of sleep was associated with the severity of dementia [19]. In prior PSG studies, patients with AD compared with controls demonstrated an increased wake time by up to 52%, increased number of awakenings by 36%, and reduced SWS by about 22% [20]. REM sleep (as a proportion of time asleep) has been demonstrated to decrease as the severity of dementia increases [21], and a low quantity of REM sleep has been shown to predict incident dementia in a community-based population [22]. Sleep disruption, background electroencephalogram (EEG) slowing, and changes in EEG amplitude are so prevalent in AD that EEG changes have been suggested as a biomarker for diagnosis [23, 24]. In addition, medications used to treat many of the comorbidities seen in patients with AD have the potential to disrupt sleep.
2 Consequences of Sleep Disruption
The consequences of insomnia are numerous. Sleep deprivation in general has been associated with a decrease in vigilance, memory proficiency, executive function, and reaction time, all of which are often areas already subjected to diminished performance with aging [25]. In addition to the cognitive consequences and evident quality-of-life impact, difficulty with falling asleep has been cited as having an increased risk ratio of cardiovascular disease of 1.47–3.90 [26]. Total sleep time (TST) of < 5 h has been associated with a 2.5 times increased incidence of diabetes and increased risk of cancers such as prostate cancer [27, 28]. In the elderly, insomnia has also been linked to increased rates of depression and suicide [29, 30].
Although sleep disturbance in dementia conventionally has been considered an outcome of the primary neurodegenerative processes [12], there is growing provocative evidence that insomnia and sleep disruption may also contribute to dementia pathophysiology, particularly in AD, creating a bidirectional issue. For example, in humans, sleep disruption as measured by actigraphy demonstrated an increased risk of developing AD in a large prospective cohort [31]. In murine models, worsening of sleep/wake cycles along with alteration of brain interstitial fluid (ISF) Aβ diurnal fluctuations were seen with plaque formation [32]. Brain ISF Aβ levels were also shown to be increased in patients with sleep deprivation and orexin administration [33]. Studies demonstrated that SWS disruption resulted in an increase in measured cerebrospinal fluid (CSF) Aβ levels [34]. A similar association between poor sleep quality and elevated Aβ has been noted in descriptive cross-sectional studies, regardless of whether sleep quality was measured via self-report [35], wrist actigraphy [36], or polysomnography [37]. However, data are also conflicting as to the extent that severely restricted sleep (5 nights in a row limited to 4 h in bed) had minimal impact on Aβ isoforms in normal middle-aged adults [38]. A full understanding of these results may reflect the interaction of sleep with genetic risk. Positive correlation between actigraphically assessed disturbed sleep measured ante-mortem and more severe postmortem Aβ neuropathology may be moderated by the presence of apolipoprotein E4 [39].
Tau itself may prove to be a valid marker for the impact of sleep loss on AD. Descriptive human studies have shown poor sleep to be associated with elevated CSF tau protein [35, 40], though not without at least some conflicting data [34]. Nonetheless, imaging studies with positron emission tomography examining tau activity in the amygdala and various cortical regions demonstrated a correlation with lower slow-wave spectral power and a similar association in relation to higher CSF t-Tau and p-Tau181 [41]. Finally, sleep deprivation in mice has been associated with the spread of tau pathology [42].
Such potential bidirectional relationships between sleep disruption/deprivation and AD highlight the importance of therapeutic options targeting sleep symptoms in AD, not only for quality of life and the numerous health benefits associated with adequate sleep but also perhaps to deter the progression of the underlying pathophysiology itself [31, 43]. It is important to point out that, despite exciting research linking AD biomarkers to sleep disruption, none of the intervention trials reviewed in this article have employed such markers as diagnostic entry criteria into such trials, and nor have they examined such biomarkers as outcomes of clinical trials.
3 Caregiver Impact
Of the many challenges facing those with recognized or incipient AD and their families, caregiver burden is a prominent feature. The task of taking care of elderly individuals with dementia can put a strain on relationship dynamics and cause considerable emotional stress and burnout [44, 45]. Sleep disruption has been cited as compounding the burden on caregivers, leading to frustration and strained relationships at a significant life period, and at times even resulting in suboptimal care [46, 47]. Some evidence has even suggested that sleep disturbance in individuals with dementia hastens the ultimate decision of institutionalization [48], and obtaining overnight care in the home may forestall nursing home placement [49]. Because AD is often a disease that impacts upon the entire family, the role of caregiver burden should be considered in evaluating the risk/benefit ratios of treatments and makes finding solutions to disruption of sleep in people with AD of even greater importance. Caregiver input should be considered during history taking and evaluation of treatment plans because those with known or unrecognized dementia have the potential to underestimate symptoms [50], and studies demonstrated that subjective measures and sleep questionnaires often underestimated sleep quality, even in early stages of AD [51].
4 Treatment of Insomnia in Alzheimer’s Disease
Therapeutic goals should be targeted at improving symptoms and quality of life. Because of the associated consequences of sleep disruption, cognitive and health improvements may be appreciated. As mentioned, slowing of disease progression through a decrease in Aβ and neurofibrillary tangles may at least be plausible as per recent data as cited. Given a known association between daytime sleepiness in AD and lower quality of life [52], an outcome of improved daytime alertness and functionality may represent a reasonable goal of treatment. At least one pharmacologic intervention study in nondemented elderly people demonstrated that napping was significantly decreased following improved nocturnal sleep quality [53]. However, increasing daytime alertness in patients with dementia can sometimes impact on caregiving in unexpected ways. For example, the daytime respite afforded the caregiver when the patient with dementia naps may be welcome, and its disappearance is potentially viewed unfavorably.
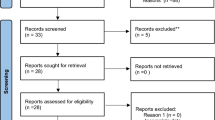
Paramount to management is a thorough sleep and medical history, including assessment of other comorbidities, medications, and environmental factors, along with the diagnosis and treatment of any accompanying sleep disorders. While PSG is not necessarily indicated for the diagnosis of insomnia, it may be warranted if suspicion for other sleep disorders, such as obstructive sleep apnea (OSA) or REM behavior disorder (RBD), is present, both of which have been suggested to potentially occur at a higher rate in AD and could play a role in symptoms of insomnia as well as cognitive decline [54, 55]. Current knowledge regarding whether OSA and/or RBD are more prevalent in AD remains somewhat moot [56, 57], but there is little doubt that they may be comorbid conditions in many patients with AD and contribute to disability or functional decline. Some data suggest that sleep issues may be more salient in dementia with Lewy bodies (DLB) relative to AD (56), but treatment considerations in DLB (and broadly defined Parkinsonism) are separate topics in their own right [58]. Restless leg syndrome (RLS) and periodic limb movement disorder (PLMD) of sleep are also highly present in the elderly population because of anemia (due to both dietary insufficiency and/or gastrointestinal malabsorption/loss), medication side effects, or genetics and should be addressed along with other underlying conditions contributing to insomnia such as comorbid mood and medical disorders. RLS may also be an unrecognized cause of nocturnal agitation and wandering in some individuals with dementia [59]. When considering therapeutic options, it is important to keep in mind that with age comes a change in functional reserves, pharmacodynamics, and concerns about polypharmacy, making dosing windows even more attenuated [60]. To address these issues by reference to the current literature, we performed an extensive review of empirically based studies, as well as systematically conducted meta-analyses, by focusing on key medical subject heading terms. Searches were conducted using PubMed and Cochrane Central Register of Controlled Trials databases and included the terms Alzheimer’s disease, Alzheimer’s, dementia, cognitive impairment, sleep disruption, insomnia, and pharmacotherapy.
5 Nonpharmacological Therapy
It is crucial to emphasize that behavioral interventions should always be considered in the first line for insomnia. They may have more sustained efficacy and possess a significantly superior side effect profile to that of pharmacotherapy for insomnia [61]. A recent comprehensive review of nonpharmacologic interventions for sleep in nursing home patients further emphasized the potential value of intensive, multicomponent behavioral treatments involving varied daytime activities, restriction of daytime napping opportunities, and mitigation of night-time interruptions by staff [62]. While our aim is primarily to review pharmacotherapy options, nonpharmacological interventions should be fundamental to management, with supplementation with pharmacological agents when appropriate for refractory or specific cases [63]. That being said, sleep disturbance in the setting of AD, with its discussed alteration in neuronal architecture, may indeed fall into a clinical scenario where pharmacological agents need to at least be considered. In addition, even though nonpharmacological interventions are, overall, considered to be beneficial, the heterogeneity of data collection and outcome reporting methods make clinical deductions and implementation strategies somewhat unclear and imprecise at times [62].
5.1 Sleep Hygiene/Lifestyle Changes
Improvements in sleep hygiene may be impactful in sleep disturbance in cases of dementia [64]. Exercise has been shown not only to aid with the ability to sleep but also to increase function and delay institutionalization in individuals with AD [64]. The American Academy of Sleep Medicine (AASM) does not recommend sleep hygiene as a sole therapeutic measure in insomnia in the general population, but it may have a role in therapy in patients with AD where treatment options may be limited. Given the favorable risk profile, sleep hygiene and lifestyle modification should be considered in most cases [65]. Observational studies of nursing home patients with severe dementia indicated that excessive daytime napping was associated with relatively more disrupted sleep the following night, implying that restriction of daytime napping might have beneficial effects [66]. However, the complexity of the situation is underscored by the parallel observation that poor sleep continuity at night was associated with daytime napping the following day. Hence, the implementation of daytime sleep restriction in individuals with dementia may be challenging.
5.2 Cognitive Behavioral Therapy for Insomnia
CBT-i has been shown to be an effective treatment modality to improve sleep quality [67] and is typically considered part of first-line therapy for insomnia in the general population [68]. A Cochrane review concluded that, in adults aged > 60 years with sleep problems, CBT-i is effective, particularly for sleep maintenance [67]. In the elderly, CBT-i has been shown to be superior to pharmacotherapy in terms of efficacy and sustained benefit in multiple randomized, placebo-controlled studies [69, 70]. A two‐arm randomized controlled trial (RCT) on CBT-i in people with mild cognitive impairment (MCI) and insomnia demonstrated significant improvement in sleep onset latency (SOL), SE, wake after sleep onset (WASO), and insomnia severity, along with notable effect sizes in subjects receiving CBT-i compared with controls [71]. CBT-i has been shown to improve cognitive function in older adults with MCI [71] and is currently being evaluated to see whether it has the ability to reduce Aβ deposition [72].
5.3 Bright Light Therapy
It has been established that there is weakening of circadian mechanisms in AD, thought to potentially be due in part to architectural changes impacting the SCN [73], manifested primarily by neuronal volume loss rather than Aβ deposition specifically. Such loss makes modulators of circadian rhythm, such as light and melatonin, of particular interest as therapeutic agents. In an RCT (NITE-AD) of 36 patients with AD, daily bright light therapy (2500 lux) administered for at least 1 h before bed, in conjunction with sleep hygiene and daily walking, demonstrated a decrease in the number of nocturnal awakenings and WASO maintained at 6-month follow-up [74]. In another RCT, the use of morning light (2500 lx) alone in 50 patients with AD was not found to be clinically beneficial on its own but improved sleep and daytime function in conjunction with melatonin supplementation [75]. Still another group also found a modest improvement in sleep quality in people with dementia with daytime light therapy (1000 lx) administered between 9 a.m. and 6 p.m., with augmented benefit with the addition of melatonin [76]. Despite some reports of symptom improvement and theoretical plausible mechanistic benefit, the limited data and evidence led a 2014 Cochrane review to report insufficient evidence to recommend bright light therapy alone for treatment of sleep disturbance in people with dementia [77]. Dosing across studies ranged from 2500 to 10,000 lx administered at various times of day for 1–2 h with a treatment duration ranging from 10 days to 2 months. It has been suggested that difficulty of implementation at controlled doses and the complexity of timing of administration make therapeutic utilization challenging and in need of further refinement [78]. A 2016 systematic review and meta-analysis demonstrated a significant small-to-medium effect size for sleep problems in AD with light therapy, with greater effect seen with greater intensity light, although that review also noted difficulties in precision because of the heterogeneity across studies in timing, frequency, and strength (i.e., illumination intensity of treatment) [79]. Moderators of the effects of enhanced illumination may include features such as wavelength of administered light, but these features remain poorly defined at this time [80]. A still more recent study [81] used a 4-week lighting intervention with alterations in intensity between day and evening light (350–750 lx in treatment vs. 110–200 lx for control) tailored to residents’ preferred locales in assisted living environments relative to control lighting in a crossover design. This study demonstrated benefits in caregivers’ rating of sleep quality, depression, and agitation, although no effect was seen with actigraphic measures of sleep. However, an uncontrolled 25-week extension [82] of the active lighting condition did result in significant improvement not only in caregiver-rated sleep but also in actigraphically measured SE. The latter result implies that phototherapy for disturbed sleep in AD may require a particularly long trial period.
6 Pharmacological Therapy
6.1 Melatonin
Melatonin is endogenously formed in the pineal gland and secreted via input from the SCN, which derives much of its signal from light exposure. It plays a large role in modulating circadian rhythm and has become a common supplement used in treating sleep disorders. Melatonin has shown efficacy in the general elderly population for sleep disruption [83], although its role as a therapeutic agent in AD remains more in question.
There has been discussion of the role of mitochondrial oxidative stress in plaque formation [84], along with data suggesting circadian disruption as an integral associative factor in AD [85]. These possible etiological contributors make melatonin intriguing as a potential therapeutic agent for sleep disruption in AD, with the supplement having potential antioxidative and chronobiologic properties [86]. Positive effects were seen in transgenic AD mouse models, where melatonin demonstrated the ability to reduce measured memory deficits and decrease apoptotic neurons and projected Aβ deposit trajectory [87, 88].
Studies in humans thus far have not yielded quite the same level of optimism as seen in mouse models, although results from small lower-quality studies have shown some benefit, though not without limitations. In an uncontrolled retrospective study of patients with AD, melatonin 9 mg resulted in improvement in subjective sleep, reduction of sundowning behavior, and lack of decline in cognitive function testing over a period of 22–35 months [89]. Several other case reports and small open-label trials described benefits on subjective sleep characteristics and cognitive function [86], but data quality is limiting. Much of the available literature highlights the need for placebo-controlled studies, particularly when evaluating therapeutics for insomnia where the risk of placebo effect is substantial.
Current perspectives on melatonin dosing suggest that lower doses (generally < 5 mg) are more effective for circadian phase shifting, whereas sedative/hypnotic effects, if any, may only be apparent at higher doses [90]. However, the several randomized placebo-controlled studies that do exist on melatonin and sleep parameters in patients with AD failed to show significant benefit from melatonin therapy (across a relatively wide range of dosages of 1.5–10 mg) on nocturnal characteristics outside of occasional nonsignificant trends [86, 91,92,93]. One multicenter study did demonstrate a nonsignificant tendency towards improvement in WASO and SOL and a significant small benefit in caregiver-reported patient sleep quality with extended-release melatonin 2.5 mg compared with placebo [92]. An RCT of people with dementia and sleep disturbance found very modest improvements in sleep onset and TST compared with controls with melatonin 2.5 mg (in addition to light therapy) as measured by actigraphy [76]. A randomized double-blinded parallel-group study in patients with mild-to-moderate AD (n = 60 completing analysis, with n = 13 in insomnia subpopulation) evaluated prolonged-release melatonin 2 mg as an adjunctive treatment to cognitive therapy compared with placebo. The study demonstrated a significant reduction in decline on cognitive measures assessed via the Instrumental Activities of Daily Living and Mini-Mental State Examination (MMSE) (p = 0.044), both for patients with AD overall and in the insomnia subpopulation, compared with controls over a 24-week period. Objective sleep diary measures and Pittsburgh Sleep Quality Index components also improved significantly in both the overall AD group and in the insomnia subtype patients with prolonged-acting melatonin compared with placebo. Both cognitive and sleep benefits were somewhat more pronounced in the insomnia subgroup [94].
Melatonin generally seems fairly well tolerated with minimal adverse effects (AEs) in most studies, somewhat limiting the downside of therapy. One study suggested a subjective increase in aggression and mood disturbance with melatonin. This was not seen when melatonin and light therapy were combined (a somewhat increased benefit was also noted) [76].
Despite the potential role of melatonin in sleep disturbances in AD, a recent Cochrane review on pharmacotherapy for insomnia in the setting of dementia, of which the majority of populations under study carried a clinical (c.f., biomarker) diagnosis of AD, reported low-certainty evidence that melatonin ≤ 10 mg had little or no positive impact on sleep parameters over an 8- to 10-week span in patients with AD [95]. They reported no significant AE concerns with melatonin. Some evidence suggests an improvement in sundowning behavior and daytime function with melatonin, which—along with a seemingly favorable side effect profile—may make melatonin worthy of consideration in certain clinical settings; however, overall, more high-quality studies are needed [86]. Several factors may limit its use, including the complexity of naturally occurring melatonin regulation and secretion in terms of timing and light exposure influence. Variation in the preparation of dietary supplements, including but not limited to melatonin [96], and significant placebo effects further obscure the therapeutic role of melatonin.
6.2 Melatonin Receptor Agonists
Ramelteon is a melatonin receptor agonist with an affinity for MT1 and MT2 receptors that retains interest as a therapeutic option in people with sleep disturbances for similar reasons as melatonin [97]. Interestingly, in transgenic murine models, ramelteon failed to show the reduction of neuropathic biomarkers and cognitive improvement in AD mice that melatonin demonstrated [98]. In RCTs, ramelteon did demonstrate significantly improved SOL and TST in elderly people without AD [99]; however, data in the setting of AD are limited [86]. A sponsored RCT of ramelteon in patients with AD was undertaken in 2007, with results remaining unpublished [95]. A few case reports cite subjective benefits in AD [100], but the overall evidence is sparse. AE data seem comparable to those for melatonin [95]. Of note, in Aβ(1–42) injected rat models, there was some benefit of melatonin receptor agonist piromelatine on cognitive function [101]. The agent is at present undergoing phase II clinical trials to determine safety and efficacy in patients with mild AD and insomnia (NCT#02615002).
6.3 Benzodiazepines/Site-Specific Gamma-Aminobutyric Acid Agonists
Hypnotics such as benzodiazepines and nonbenzodiazepine receptor site-specific γ-aminobutyric acid (GABA) agonists (the so-called “z-drugs,” including zolpidem, zaleplon, zopiclone, and eszopiclone) are some of the more commonly prescribed sleep agents for the general population worldwide. With concern over sedation, fall risk, genesis of parasomnias, and impact on cognitive function, they should be considered only for short-term use, are recommended to be employed with caution in the elderly, and are not recommended in patients with AD. Part of the suggested restrictions on the use of older benzodiazepine hypnotics, as well as the “z-drugs,” is derived undoubtedly from a series of observational and case–control studies procured from healthcare administrative databases that demonstrated an increased risk for AD (or other forms of dementia) with these medication classes [102,103,104]. A 2016 systematic review and meta-analysis concluded there was a 78% increased risk with use [105]. Although such analyses certainly suggest caution on the part of prescribers, limitations of these administrative databases must be acknowledged. First, adequate control over the wide array of psychiatric and/or medical comorbidities known to be associated with both poor sleep and incident dementia is often partial or incomplete [102,103,104, 106, 107]. Second, a diagnosis of AD rendered from an administrative database is not typically based on disease biomarkers, neuroimaging, or even standardized psychometrics that are required to achieve an adequate and valid diagnosis, though some cohort studies include such measurements [107]. Third, such associations with these drug classes should show clear graded associations by either frequency of usage and/or cumulative daily dose, and often they do not [108]. Fourth, not all analyses report associations between the use of these drug classes and AD [109, 110]. Fifth, a compelling neurobiologic rationale explaining how GABA agonism might inflict cumulative neuronal and/or glial damage leading to a cascade of accelerated protein misfolding appears largely lacking at this time.
Distinct from incident AD, presumably deriving from over years to decades of use, other more immediate adverse outcomes such as falls have been associated with the “z-drugs.” In nonbenzodiazepine receptor agonists, a recent study of people with a diagnosis of dementia demonstrated that, at high doses in particular, there is at least as great a risk of falls, fractures, and strokes as there is with benzodiazepines [111]. The concern regarding a high degree of AEs (e.g., hip fracture, all-cause mortality) was echoed in a subsequent analysis [112], although, interestingly, this study found no evidence of worsening of dementia in two separate dementia cohorts. The American Geriatrics Society Beers criteria cite both benzodiazepines and nonbenzodiazepine GABA receptor agonists as potentially inappropriate for use in elderly people because of their risk profile [113]. However, some recent reviews presented a more tempered perspective on AEs of nonbenzodiazepines receptor agonists, noting that over a quarter-century of use and tens of millions of doses taken in elderly people may imply that short-term use at appropriate dosing may be suitable in some cases [114]. Recent analyses of prescriptions derived from both commercial [115] and Medicare [116] databases suggested historical trends towards lower usage of zolpidem and the other “z-drugs” for sleep, suggesting a strong influence of the Beers criteria and existing observational studies in clinical practice.
Apart from the aforementioned pharmacoepidemiologic considerations, the efficacy of this class of medication, specifically demonstrated in the setting of RCTs among well-characterized AD, remains poorly researched. A small pilot study (n = 7) of patients with AD and difficulty sleeping reported no benefit in sleep characteristics as measured by actigraphy with the benzodiazepine derivative triazolam 0.125 mg [117]. A systematic review reported no improvement in sleep quality with benzodiazepines in the setting of AD [118]. A recent Cochrane review could not identify a single, well-conducted RCT studying either traditional benzodiazepine hypnotics or site-specific GABAergic hypnotics for sleep in AD [95].
6.4 Orexin Receptor Antagonists
One of the newer classes of agents for insomnia is dual orexin receptor antagonists (DORAs), which the US FDA has approved for both sleep onset and sleep maintenance. Their mechanism of action is exerted through blockage of OX1 and OX2 receptors and the influence of wake-promoting neuropeptides orexin A and B. Although data on the relationship between orexin and AD are conflicting, some evidence has suggested dysregulation of the orexin system due to lateral hypothalamus disruption as a contributor to sleep symptomatology [119]. Higher levels of orexin in the CSF of individuals with AD with more severe disease has been noted, along with worsened SE and higher WASO [40], potentially pointing to a mechanistic consideration of DORAs. Although comparable studies in humans are still needed, mice models have shown that intracerebroventricular infusion of dual orexin antagonist almorexant decreased ISF levels of Aβ and increased TST by 10%. Several other studies supported the potential role of orexin in AD, with trials of orexin antagonist suvorexant demonstrating efficacy. In a recent phase III randomized, double-blinded, placebo-controlled PSG study in patients (n = 285) with mild-to-moderate probable AD, an objective improvement of 73 min of TST from baseline compared with 45 min for placebo (28-minute difference; p < 0.01) over the course of 4 weeks was seen with suvorexant [120]. The benefit in sleep time was more prominent in the latter third of the night. Sleep architecture was otherwise unchanged from that with placebo. Next-day somnolence was reported in 4.2% of patients (compared with 1.4% with placebo), and four falls in three patients (2.1% of total) were recorded in the suvorexant group (vs. 0 in placebo). In 2020, shortly after this clinical trial was concluded, the FDA approved suvorexant for treatment of insomnia in patients with mild-to-moderate AD, making it one of the only agents approved specifically for this indication. Case series have also reported suvorexant as having a favorable impact on symptoms of nocturnal delirium in patients with AD [121]. A phase III RCT is currently being conducted on suvorexant 20 mg to test for a possible diminished rate of Aβ accumulation in the brain with therapy (NCT #04629547).
In 2019, the FDA approved lemborexant for the treatment of insomnia in adults. Studies have since begun to investigate its use in the setting of AD for treatment of irregular sleep-wake disorder. Thus far, a phase II dose-defining proof-of-concept, randomized, double-blinded, placebo-controlled trial on the efficacy and safety of lemborexant has been conducted. Patients (n = 62) were randomized to placebo or lemborexant 2.5, 5, 10, or 15 mg and studied over the course of 4 weeks. Reduction of movement from baseline during the least active 5-h period over 24 h on actigraphy was significant compared with placebo for all doses except 10 mg. Relative amplitude of rest-activity rhythm measured was significantly reduced with 5 and 15 mg compared with placebo, which the authors suggested represents the agent improving distinction between night and day. The mean duration of sleep bouts occurring during the day was significantly decreased from baseline for 5 and 15 mg compared with placebo. No serious treatment-related AEs were noted, and there was no worsening of cognitive function as measured by MMSE and the Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog) [122], a widely used scale for assessing cognition in AD.
A third DORA, daridorexant, has not yet been approved in the USA but has shown promising results in a randomized, dose-finding, crossover design in elderly (nondemented) people and has also shown some positive PSG results indicating improvement in sleep metrics [123].
A Cochrane review found moderate-certainty support for orexin receptor antagonists increasing TST and decreasing WASO but little or unclear impact on total number of awakenings, SOL, or mean duration of sleep segments, and reported AEs were probably no more common than with placebo in patients with mild-to-moderate AD [95].
6.5 Selective Serotonin Reuptake Inhibitors/Tricyclic Antidepressants
Antidepressants have historically been used to treat insomnia because of their potential sedative properties. They may have the added benefit of treating commonly associated mood disorders, which in turn may also improve sleep. Antidepressants, particularly tricyclic antidepressants (TCAs), are concerning for their cholinergic effect, potentially worsening accompanying symptoms of AD.
6.5.1 Trazodone
Trazodone is a phenylpiperazine compound antidepressant with dose-dependent action preventing serotonin reuptake and blocking 5HT2A, H1, and adrenergic receptors, leading to sedation [124]. It has a long history of off-label use for the treatment of insomnia. Trazodone has demonstrated, at least in the general population, the potential to decrease N1 and REM sleep and increase SWS [125], although its efficacy in increasing sleep onset and duration have been debated. Questions regarding efficacy and its AE profile resulted in the AASM clinical guidelines on insomnia management not recommending trazodone for insomnia [126]. The benefits of increased SWS may in theory confer benefit on disease pathology in AD, with reduced SWS being correlated with higher Aβ levels [127]. In a double-blinded, placebo-controlled study (N = 30), patients with AD taking trazodone 50 mg noted an average of 42.5 min more sleep than with placebo measured via actigraphy over a 2-week period [128]. No serious AEs were reported. Based on this study, a Cochrane review reported low confidence that in moderate-to-severe AD, trazodone 50 mg may improve SE and TST over the course of 2 weeks [95]. A recent historical analysis of commercial payors in the USA over the period of 2011–2018 indicated that low-dose (< 150 mg) trazodone prescriptions increased over time, whereas zolpidem prescriptions fell substantially over that same historical period [115].
Trazodone may offer some benefit on cognitive symptoms. In a recent retrospective study, matched-control patients with AD not taking trazodone declined 2.4 times faster on the MMSE than the 25 patients taking trazodone (p = 0.038), although there were limitations inherent to the study being retrospective [129]. It was unclear mechanistically whether this reduction in decline was due to improvement in sleep parameters. Short-term cognitive impact has not been observed [130], but overall data suggest that short-term trazodone may offer benefits in TST and may provide some cognitive function value in the long term, potentially making it a drug worth further investigation.
6.5.2 Doxepin
TCAs can exert sedation via H1 receptor antagonism. Doxepin at low doses (3 or 6 mg) typically prescribed for insomnia is highly selective of H1 receptors with minimal impact on cholinergic receptors [131], making its side effect profile more advantageous than other TCAs for sleep. Because of this, it is the only TCA that the FDA has approved (specific to those low doses) for use for insomnia [132] and carries a weak recommendation for use in the general population from the AASM [126]. It has been demonstrated to decrease WASO and increase TST and SE in the elderly and increase stage 2 sleep with minimal impact on other stages, including REM, while displaying a side effect profile similar to that of placebo [133]. In murine models, doxepin reduced the cognitive issues imposed by injection of Aβ(1–42) compared with placebo [134], but thus far human studies in the setting of AD have been lacking.
6.5.3 Mirtazapine
Mirtazapine is an atypical antidepressant that acts as an α2 antagonist and has antihistaminergic and antiserotonergic (5-HT2A, 5-HT2C) properties. It has sedative qualities attributed largely to strong H1 receptor inverse agonism and has been used off label for the treatment of insomnia. In a small open-label study, mirtazapine was reported to potentially confer some benefit in agitation in people with AD [135]. Case studies have also reported improvements in sleep disturbance in patients with AD with the use of mirtazapine [136]. However, in a double-blinded, placebo-controlled pilot study, mirtazapine 15 mg had no significant effect on SE or duration compared with placebo or significant impact on cognitive function as measured by the MMSE and the Katz scale. Daytime sleepiness was increased in the mirtazapine group compared with controls; otherwise, the AE profile was similar between groups [137].
6.6 Sodium Oxybate
Sodium oxybate, the salt of γ-hydroxybutyric acid (GHB), is used to treat narcolepsy with cataplexy (along with treatment of alcohol withdrawal and use as an anesthetic agent in parts of Europe). Its mechanism of action is somewhat unclear, but it is generally thought to exert effects on GABA receptors inciting sedation, deep sleep, and potentially neuroprotection [138]. In mouse models, it was demonstrated that GHB administration reduced Aβ levels and improved cognitive deficits, with the proposed mechanism of acting via upregulation of neprilysin, a metalloprotease thought to play a role in degrading Aβ [139]. Sodium oxybate has the known AEs of headache, sedation, and respiratory depression; however, given the mouse model results and novel pathway of action, increased exploration in future studies may be warranted. A recent clinical trial of this agent in the setting of Parkinson’s disease demonstrated that it had a high occurrence of mild side effects but was overall tolerable with no patients withdrawing from the study [140], although this study may represent a somewhat younger population (mean age 62 years, standard deviation 11.1) than that of AD. Despite theoretical proposed mechanisms of benefit of sodium oxybate in AD, thus far evaluation in this population has been limited. A clinical trial was initiated to test the feasibility and safety of sodium oxybate in patients with AD, but the study was terminated in 2010 and is currently listed as the protocol being under revision (NCT# 00706186).
6.7 Acetylcholinesterase Inhibitors
Although acetylcholinesterase inhibitors are not thought to alter disease trajectory, they are commonly used as standard of care in the treatment of AD for cognitive symptoms, which generates interest in their impact on the sleep profile. Sleep parameters were measured in patients with AD receiving acetylcholinesterase inhibitors (donepezil n = 41, galantamine n = 15, rivastigmine n = 8) or no treatment (n = 12), and no statistical difference between groups was reported in terms of WASO, TST, REM, SWS percentage, apnea/hypopnea index, or periodic limb movement index (PLMI) [141]. Some evidence has suggested a possible increase in REM sleep with acetylcholinesterase inhibitors, which in theory may improve cognition, but there exists some discrepancy between the data [141, 142]. Cross-sectional assessment of patients with AD receiving rivastigmine (n = 60), donepezil (n = 58), and extended-release galantamine (n = 52) noted no difference in sleep duration compared with patients not on acetylcholinesterase inhibitors [50]. Acetylcholinesterase inhibitors have been noted to increase nightmares in case reports in AD [143, 144] and are associated with higher concurrent usage of sedative/hypnotic class medication, perhaps as a consequence of the sleep disturbance caused by such dream-disturbed sleep [12]. Within the class, some data, including from a randomized, double-blinded, parallel pilot study, suggested galantamine may be the preferable agent from a sleep standpoint, although the overall benefit on symptoms is still overall generally underwhelming [145, 146].
6.8 Memantine
Memantine is an N-methyl-d-aspartic acid (NMDA) receptor antagonist that is generally considered second line for treatment of cognitive symptoms in AD to acetylcholinesterase inhibitors; however, it is still commonly prescribed. In a cross-sectional study of patients with AD, 52 patients on memantine demonstrated longer sleep time than those not taking the drug (9.52 ± 1.9 h vs. 8.82 ± 1.8 h; p = 0.02), an effect not seen with acetylcholinesterase inhibitors [50]. It is important to keep in mind that only association and not causation can be deduced from cross-sectional studies. In an open-label prospective study (n = 12), memantine demonstrated statistically significant improvements in TST, SE, number of awakenings, and PLMI as measured on PSG [147]; however, as this was an uncontrolled study, and given the high comorbidity of PLMD in the sample (PLMI of 22.5/h at baseline), the implication of the results is hard to determine.
6.9 Antihistamines
First-generation antihistamines, such as diphenhydramine and doxylamine, are commonly used as over-the-counter and off-label treatments for insomnia. As discussed, many sedating medications, such as antidepressants, exert their sedative effect through antihistaminergic properties. Their mechanism involves blocking response of H1 receptors either through antagonism or inverse agonism. Generally, the AASM does not recommend antihistamines for use for insomnia in even the general population because of the questionable balance of efficacy versus the AEs [126]. Many of the salient negative consequences of these agents are due to their significant anticholinergic properties, which can cause dry mouth, urinary retention, constipation, agitation, memory issues, and delirium. Published literature has also associated antihistamines (both first-generation antihistamines and TCAs) with an increased risk of dementia [148]. Given these factors, the Beers criteria cite antihistamines as potentially inappropriate for use in elderly people, and they should likely be avoided if possible in the setting of AD [113].
6.10 Antipsychotics
Antipsychotics, although not typically used specifically for the indication of insomnia, are known to possess sedating qualities. They are thought to exert impacts on sleep via antiadrenergic, antidopaminergic, and/or antihistaminergic mechanisms. In essence, their use in people with dementia as de facto hypnotic agents embraces their sedative side effects in lieu of a more direct mechanism of action on circuits controlling sleep/wakefulness [12]. In 5-week open-label study comparing haloperidol and quetiapine in subjects with AD by actigraphy (n = 11 per treatment group), quetiapine decreased the total time of nocturnal wake bouts compared with baseline (p = 0.023), whereas patients in the haloperidol group demonstrated longer immobile phases during sleep compared with baseline (p = 0.01) [149]. In cross-sectional analysis, patients on quetiapine (n = 42), risperidone (n = 10), or olanzapine (n = 1) demonstrated an increased duration of sleep compared with those not taking such an agent (9.55 ± 2.1 h vs. 8.81 ± 1.8 h; p = 0.0095). Although studies such as this imply that certain antipsychotics may have a role in ameliorating disturbed sleep or nocturnal agitation in people with dementia, meta-analyses [150, 151] suggest higher mortality rates and a greater likelihood of cardiovascular/cerebrovascular events when used in such populations. In 2005 and 2008, the FDA issued “black box” warnings of their use in dementia, further supported by a more recent case–control analysis examining each antipsychotic individually [152]. The Beers criteria recommend avoiding antipsychotics in the elderly outside of treatment for schizophrenia or bipolar depression because of the side effect profile [113].
6.11 Herbal Remedies
Although herbal remedies are generally not recommended in the USA, they are more routinely utilized for sleep ailments in East Asia. Jangwonhwan is a boiled mushroom and plant blend (particularly Panax ginseng) traditionally used to achieve mild sedation in people with cognitive dysfunction. In mouse models, it has been demonstrated to potentially reduce both Aβ levels and plaque deposits [153], although no further data have become available regarding its use in either animal or human studies. The traditional Chinese herbal compound Yi-Zhi-An-Shen is currently undergoing clinical trials investigating the effect on ADAS-Cog and sleep quality. The herb is hypothesized to have benefits because of its favorable alteration of gut microbiome [154].
Yokukansan (Yi-Gan San) is a precisely formulated herbal composite that has been used in Japan as a potential agent to improve sleep and psychological and behavioral issues in people with dementia, with a few case reports suggesting benefit in AD [155]. It has been suggested that it produces an ameliorating effect on sleep via impact on GABA-A receptors and neuroprotection [156]. In an open-label trial in Japan, 13 patients (12 with AD, one with frontotemporal dementia) treated with the compound demonstrated significant improvements in Sleep Disorder Inventory, caregiver distress score, and WASO as measured by actigraphy. No AEs were reported [157]. Beneficial effects of Yokukansan in RBD have also been described [158]. Although data on its impact on sleep are limited, the compound has undergone several RCTs in Japan with generally positive results for behavioral and psychological symptoms associated with dementia, and it is listed as grade C1 (recommended regardless of insufficient scientific evidence) for use in sleep disorders by the Japanese Society of Neurology [156]. However, subsequent meta-analysis did not find significant benefit in the AD population [159].
Several low-quality studies suggested that valerian root (Valeriana officinalis) has sleep-enhancing properties [160]. A systematic review determined valerian was relatively safe but did not have enough evidence of benefit to suggest use as a sleep aid [161], although updated review and meta-analysis suggested some benefit if quality of supplementation is ensured [162]. Given the paucity of data and concern for efficacy versus its side effect profile, the AASM recommends against use of valerian as a treatment for insomnia [126]. In the setting of AD, there remains even less evidence and more reservation.
While herbal pharmacotherapy is generally not recommended because of questionable efficacy, significant concern for unvalidated side effect profiles, dosing inconsistencies, and potential to interact with other medications, there may be some utility of certain components warranting further evaluation. With the concern of AEs being even greater in people with AD, herbal therapy should be used with caution until more data are available. As is the case for melatonin, herbal products in the USA are considered dietary supplements by the FDA and fall within the purview of the 1994 Dietary Supplement and Health Education Act (DSHEA). As such, if a given product does not claim to cure disease but limits itself to “structure/function claims,” it is exempt from the more stringent quality assurance requirements stipulated by the FDA for medication. This essentially allows for a wide latitude of quality assurance for products entering the US market as sleep-promoting agents since these are not considered curative but rather are viewed as promoting better sleep as a health function.
6.12 Tryptophan
Tryptophan has been considered for insomnia therapy; however, most of the data on the amino acid have yielded very little evidence to suggest its use. Studies have typically been conducted in younger populations, with minimal data on the impact on the elderly in general [160]. There has been discussion mechanistically of the potential role of tryptophan in sleep in AD [163, 164] because of it being a substrate for melatonin and serotonin, but to date no significant data have been published demonstrating any therapeutic benefit in AD. Usage of tryptophan in the USA has decreased since cases of eosinophilia-myalgia syndrome (EMS) associated with a Japanese manufacturer were reported several decades ago [165], further reiterating issues related to the 1994 DSHEA regulations and issues related to measured purity and concentration of dietary supplements mentioned previously. Few cases of EMS have been reported over the last 15 years [166]. A precursor to tryptophan, 5-hydroxy-L-tryptophan can be obtained as a dietary supplement, but its efficacy for disturbed sleep has not been tested in AD.
6.13 Cannabidiol/Tetrahydrocannabinol
There is some recent suggestion that cannabidiol/tetrahydrocannabinol (CBD/THC) may offer some short-term improvement in sleep characteristics, although long term it may in fact impact negatively on sleep [167]. It has been proposed that CBD may have neuroprotective effects via its impact on peroxisome proliferator-activated receptor gamma and subsequently Aβ clearance [168]. A recent translational study suggested improvements in cognition in familial AD mice with CBD due to upregulation of interleukin 33 and triggering receptors expressed on myeloid cells 2 (TREM2), which play a role in phagocytosis and reduction of inflammation associated with plaque formation [169]. Several small case series have suggested utility of dronabinol for nocturnal agitation in people with dementia [170] and for dream enactment behavior [171], but controlled trials have yet to occur. Quality data supporting CBD/THC compounds in AD with sleep disruption remain sparse.
6.14 Aromatherapy
Anecdotal evidence has suggested that certain scents (e.g., lavender, lemon balm, cedar) may have mildly sedating properties when used in agitated people with dementia [172]. Few of these studies have examined sleep or specifically targeted nocturnal agitation as an outcome. A recent Cochrane review suggested that the quality of these studies was uniformly poor and that no firm evidence in support of aromatherapy currently exists [173]. A major methodologic issue in this research is that impaired olfaction, often quite conspicuous in dementia, makes the results of such trials difficult to interpret.
7 Limitations
When it comes to therapeutics for insomnia, at present there is a scarcity of well-controlled and validated studies available to guide clinical decisions, making the already formidable task of treating insomnia in AD even more of a challenge. More RCTs are needed to evaluate both the efficacy and the safety of pharmacological treatments. Given the significant impact of placebo effect inherent in insomnia treatments, more effort is required to evaluate therapies compared to placebo. Measures used in existing studies are often conducted by subjective recording of data from people with dementia and caregiver or investigator observations, all of which have value, but highlight the need for more directly verifiable objective data. Currently, the objective measures that do exist often take the form of somewhat surrogate measures of sleep disruption, such as actigraphy, which may be less valid in dementia populations and subject to innumerable procedural problems when used as an outcome in an RCT [174]. While there is no perfect solution, and often not logistically feasible, more objective improvements in sleep parameters documented via PSG would be highly beneficial, from both scientific and regulatory perspectives. Dosing of agents needs to be further clarified, especially in the AD population, where a narrow therapeutic window already exists because of concomitant medications, medical pathology, and compromised physiological reserves. Among community-dwelling Medicare recipients with dementia using multiple psychotropics, the most commonly used psychoactive medications included gabapentin, trazodone, and quetiapine [116], and much of the dosing was nocturnal, potentially to induce and/or maintain sleep. None of these medications have been subject to adequate clinical trial testing as hypnotics.
8 Conclusion
Insomnia in the setting of AD presents a unique and complex disease entity both to diagnose and manage. It can clearly extend far beyond the impaired sleep that accompanies aging per se for large segments of the elderly population. Many individuals with AD, along with at times caregivers, suffer both in terms of quality of life and potential health consequences because of a lack of control of symptoms. With sleep disruption also appearing to play a possibly significant but modifiable role in the progression of the disease, augmentation of the evidence regarding treatment modalities is paramount, particularly with prevalence of the disorder projected to increase in the future. Behavioral interventions should be considered first line due to their preferred side effect profile compared with that of pharmacotherapy; however, many pharmacological agents with differing mechanisms are at the disposal of clinicians as adjunctive therapy or in cases where dementia limits the feasibility of behavioral solutions. Historically used treatments may offer some benefit but generally have not been well supported in the literature in the setting of AD. DORAs appear to be one class of agents engendering greater optimism based on current evidence but would benefit from further investigation supporting use and monitoring risk/benefit measures. Suvorexant is approved by the FDA for use in insomnia in mild-to-moderate AD, and several other agents hold plausible mechanistic benefit with some evidence in the literature backing their use. However, a recent Cochrane review on pharmacotherapy in AD concluded that there was an overall lack of evidence to guide decision making [95].
Treatment should be individualized to patients’ and caregivers’ needs and goals, with caution and monitoring of AEs of medication, particularly sedation, in a population of people with dementia who are already at an increased risk for falls and cognitive concerns. The complexity of contributing etiologies to sleep disruption in AD make generalized treatment protocols difficult. Better qualification of optimal clinical candidates and scenarios for utilization of pharmacotherapy along with additional tools to aid in decision making in regard to choice of agent may enhance treatment outcomes. For example, it may be that sleep disturbance associated with alterations in any given AD biomarker may yield a relatively better (or worse) response to a particular intervention. Further high-quality studies on the current agents for insomnia are needed overall, with an even greater need for evaluation in the biomarker-characterized populations of people with dementia. Meaningful improvements in cognition in RCTs of a sedative/hypnotic class agent in AD may well represent the ultimate aim for future work in this area. Overall, continued research and guidelines on treatments are needed as progression is made towards easing the impact of sleep disruption associated with insomnia in the setting of AD.
References
Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5 Suppl):S7-10.
Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep disorders and sleep deprivation: an unmet public health problem. Washington (DC): National Academies Press (US); 2006.
Carpenter BD, Strauss M, Patterson MB. Sleep disturbances in community-dwelling patients with Alzheimer’s disease. Clin Gerontol. 1996;16(2):35–49.
Zhao QF, et al. The prevalence of neuropsychiatric symptoms in Alzheimer’s disease: Systematic review and meta-analysis. J Affect Disord. 2016;190:264–71.
Bliwise DL, et al. Sleep and “sundowning” in nursing home patients with dementia. Psychiatry Res. 1993;48(3):277–92.
McGaffigan S, Bliwise DL. The treatment of sundowning. A selective review of pharmacological and nonpharmacological studies. Drugs Aging. 1997;10(1):10–7.
AASM AAOSM. International classification of sleep disorders. 3rd edn. 2014.
Mander BA, et al. Sleep: a novel mechanistic pathway, biomarker, and treatment target in the pathology of Alzheimer’s disease? Trends Neurosci. 2016;39(8):552–66.
Hebert LE, et al. Alzheimer disease in the United States (2010–2050) estimated using the 2010 census. Neurology. 2013;80(19):1778–83.
Rauchs G, et al. Is there a link between sleep changes and memory in Alzheimer’s disease? NeuroReport. 2008;19(11):1159–62.
Andre C, Chetelat G, Rauchs G. Sleep-disordered breathing and Alzheimer’s disease biomarkers in older adults. Med Sci (Paris). 2020;36(10):833–5.
Bliwise DL. Sleep disorders in Alzheimer’s disease and other dementias. Clin Cornerstone. 2004;6(Suppl 1A):S16-28.
Ballard C, et al. Alzheimer’s disease. Lancet. 2011;377(9770):1019–31.
Ancoli-Israel S, et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep. 1997;20(1):18–23.
Crowley K. Sleep and sleep disorders in older adults. Neuropsychol Rev. 2011;21(1):41–53.
Spielman AJ, Nunes J, Glovinsky PB. Insomnia. Neurol Clin. 1996;14(3):513–43.
Bliwise DL. Sleep in normal aging and dementia. Sleep. 1993;16(1):40–81.
Borges CR, et al. Alzheimer’s disease and sleep disturbances: a review. Arq Neuropsiquiatr. 2019;77(11):815–24.
Bliwise DL, et al. Observed sleep/wakefulness and severity of dementia in an Alzheimer’s disease special care unit. J Gerontol A Biol Sci Med Sci. 1995;50(6):M303–6.
Vitiello MV, et al. Sleep disturbances in patients with mild-stage Alzheimer’s disease. J Gerontol. 1990;45(4):M131–8.
Vitiello MV, et al. Rapid eye movement sleep measures of Alzheimer’s-type dementia patients and optimally healthy aged individuals. Biol Psychiatry. 1984;19(5):721–34.
Pase MP, et al. Sleep architecture and the risk of incident dementia in the community. Neurology. 2017;89(12):1244–50.
Al-Nuaimi AH, et al. Changes in the EEG amplitude as a biomarker for early detection of Alzheimer’s disease. Annu Int Conf IEEE Eng Med Biol Soc. 2016;2016:993–6.
Cassani R, et al. Systematic review on resting-state EEG for Alzheimer’s disease diagnosis and progression assessment. Dis Markers. 2018;2018:5174815.
Dzierzewski JM, Dautovich N, Ravyts S. Sleep and cognition in older adults. Sleep Med Clin. 2018;13(1):93–106.
Schwartz S, et al. Insomnia and heart disease: a review of epidemiologic studies. J Psychosom Res. 1999;47(4):313–33.
Gottlieb DJ, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863–7.
Sigurdardottir LG, et al. Sleep disruption among older men and risk of prostate cancer. Cancer Epidemiol Biomark Prev. 2013;22(5):872–9.
Jaussent I, et al. Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep. 2011;34(8):1103–10.
Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):e1160–7.
Lim AS, et al. Sleep fragmentation and the risk of incident Alzheimer’s disease and cognitive decline in older persons. Sleep. 2013;36(7):1027–32.
Roh JH, et al. Disruption of the sleep-wake cycle and diurnal fluctuation of beta-amyloid in mice with Alzheimer’s disease pathology. Sci Transl Med. 2012;4(150):150ra122.
Kang JE, et al. Amyloid-beta dynamics are regulated by orexin and the sleep-wake cycle. Science. 2009;326(5955):1005–7.
Ju YS, et al. Slow wave sleep disruption increases cerebrospinal fluid amyloid-beta levels. Brain. 2017;140(8):2104–11.
Sprecher KE, et al. Poor sleep is associated with CSF biomarkers of amyloid pathology in cognitively normal adults. Neurology. 2017;89(5):445–53.
Ju YE, et al. Sleep quality and preclinical Alzheimer disease. JAMA Neurol. 2013;70(5):587–93.
Varga AW, et al. Reduced slow-wave sleep is associated with high cerebrospinal fluid Abeta42 levels in cognitively normal elderly. Sleep. 2016;39(11):2041–8.
Olsson M, et al. Sleep deprivation and cerebrospinal fluid biomarkers for Alzheimer’s disease. Sleep. 2018. https://doi.org/10.1093/sleep/zsy025.
Lim AS, et al. Modification of the relationship of the apolipoprotein E epsilon4 allele to the risk of Alzheimer disease and neurofibrillary tangle density by sleep. JAMA Neurol. 2013;70(12):1544–51.
Liguori C, et al. Orexinergic system dysregulation, sleep impairment, and cognitive decline in Alzheimer disease. JAMA Neurol. 2014;71(12):1498–505.
Lucey BP, et al. Reduced non-rapid eye movement sleep is associated with tau pathology in early Alzheimer’s disease. Sci Transl Med. 2019;11(474):6550.
Holth JK, et al. The sleep-wake cycle regulates brain interstitial fluid tau in mice and CSF tau in humans. Science. 2019;363(6429):880–4.
Ju YE, Lucey BP, Holtzman DM. Sleep and Alzheimer disease pathology–a bidirectional relationship. Nat Rev Neurol. 2014;10(2):115–9.
Dawood S. Caregiver burden, quality of life and vulnerability towards psychopathology in caregivers of patients with dementia/Alzheimer’s disease. J Coll Physicians Surg Pak. 2016;26(11):892–5.
Pudelewicz A, Talarska D, Baczyk G. Burden of caregivers of patients with Alzheimer’s disease. Scand J Caring Sci. 2019;33(2):336–41.
Donaldson C, Tarrier N, Burns A. Determinants of carer stress in Alzheimer’s disease. Int J Geriatr Psychiatry. 1998;13(4):248–56.
McCurry SM, et al. Factors associated with caregiver reports of sleep disturbances in persons with dementia. Am J Geriatr Psychiatry. 2006;14(2):112–20.
Pollak CP, et al. Sleep problems in the community elderly as predictors of death and nursing home placement. J Community Health. 1990;15(2):123–35.
Gaugler JE, et al. Predictors of institutionalization of cognitively impaired elders: family help and the timing of placement. J Gerontol B Psychol Sci Soc Sci. 2000;55(4):P247–55.
de Oliveira FF, et al. Assessment of sleep satisfaction in patients with dementia due to Alzheimer’s disease. J Clin Neurosci. 2014;21(12):2112–7.
Most EI, et al. Discrepancy between subjective and objective sleep disturbances in early- and moderate-stage Alzheimer disease. Am J Geriatr Psychiatry. 2012;20(6):460–7.
Lee JH, et al. Daytime sleepiness and functional impairment in Alzheimer disease. Am J Geriatr Psychiatry. 2007;15(7):620–6.
Scharf M, et al. A 2-week efficacy and safety study of eszopiclone in elderly patients with primary insomnia. Sleep. 2005;28(6):720–7.
Andrade AG, et al. The relationship between obstructive sleep apnea and Alzheimer’s disease. J Alzheimers Dis. 2018;64(s1):S255–70.
Zhang F, et al. Rapid eye movement sleep behavior disorder and neurodegenerative diseases: an update. Aging Dis. 2020;11(2):315–26.
Bliwise DL, et al. Sleep disturbance in dementia with Lewy bodies and Alzheimer’s disease: a multicenter analysis. Dement Geriatr Cogn Disord. 2011;31(3):239–46.
Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Perspect Psychol Sci. 2015;10(1):97–137.
Trotti LM, Bliwise DL. Treatment of the sleep disorders associated with Parkinson’s disease. Neurotherapeutics. 2014;11(1):68–77.
Richards KC, et al. Nighttime agitation in persons with dementia as a manifestation of restless legs syndrome. J Am Med Dir Assoc. 2021;22(7):1410–4.
Marengoni A, Nobili A, Onder G. Best practices for drug prescribing in older adults: a call for action. Drugs Aging. 2015;32(11):887–90.
Mitchell MD, et al. Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC Fam Pract. 2012;13:40.
Wilfling D, et al. Characteristics of multicomponent, nonpharmacological interventions to reduce or avoid sleep disturbances in nursing home residents: a systematic review. Int Psychogeriatr. 2021;33(3):245–73.
Zdanys KF, Steffens DC. Sleep disturbances in the elderly. Psychiatr Clin N Am. 2015;38(4):723–41.
Shub D, Darvishi R, Kunik ME. Non-pharmacologic treatment of insomnia in persons with dementia. Geriatrics. 2009;64(2):22–6.
Boeve BF, Silber MH, Ferman TJ. Current management of sleep disturbances in dementia. Curr Neurol Neurosci Rep. 2002;2(2):169–77.
Bliwise DL, et al. Systematic 24-hr behavioral observations of sleep and wakefulness in a skilled-care nursing facility. Psychol Aging. 1990;5(1):16–24.
Montgomery P, Dennis J. Cognitive behavioural interventions for sleep problems in adults aged 60+. Cochrane Database Syst Rev. 2003;1:CD003161.
Schutte-Rodin S, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4(5):487–504.
Morin CM, et al. Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. JAMA. 1999;281(11):991–9.
Sivertsen B, et al. Cognitive behavioral therapy vs zopiclone for treatment of chronic primary insomnia in older adults: a randomized controlled trial. JAMA. 2006;295(24):2851–8.
Cassidy-Eagle E, et al. Neuropsychological functioning in older adults with mild cognitive impairment and insomnia randomized to CBT-I or control group. Clin Gerontol. 2018;41(2):136–44.
Siengsukon CF, et al. Cognitive behavioral therapy for insomnia to enhance cognitive function and reduce the rate of Abeta deposition in older adults with symptoms of insomnia: a single-site randomized pilot clinical trial protocol. Contemp Clin Trials. 2020;99:106190.
Uddin MS, et al. Circadian and sleep dysfunction in Alzheimer’s disease. Ageing Res Rev. 2020;60:101046.
McCurry SM, et al. Nighttime insomnia treatment and education for Alzheimer’s disease: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(5):793–802.
Dowling GA, et al. Melatonin and bright-light treatment for rest-activity disruption in institutionalized patients with Alzheimer’s disease. J Am Geriatr Soc. 2008;56(2):239–46.
Riemersma-van der Lek RF, et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA. 2008;299(22):2642–55.
Forbes D, et al. Light therapy for improving cognition, activities of daily living, sleep, challenging behaviour, and psychiatric disturbances in dementia. Cochrane Database Syst Rev. 2014;2:CD003946.
Urrestarazu E, Iriarte J. Clinical management of sleep disturbances in Alzheimer’s disease: current and emerging strategies. Nat Sci Sleep. 2016;8:21–33.
van Maanen A, et al. The effects of light therapy on sleep problems: a systematic review and meta-analysis. Sleep Med Rev. 2016;29:52–62.
Mitolo M, et al. Effects of light treatment on sleep, cognition, mood, and behavior in Alzheimer’s disease: a systematic review. Dement Geriatr Cogn Disord. 2018;46(5–6):371–84.
Figueiro MG, et al. Effects of a tailored lighting intervention on sleep quality, rest-activity, mood, and behavior in older adults with Alzheimer disease and related dementias: a randomized clinical trial. J Clin Sleep Med. 2019;15(12):1757–67.
Figueiro MG, et al. Long-term, all-day exposure to circadian-effective light improves sleep, mood, and behavior in persons with dementia. J Alzheimers Dis Rep. 2020;4(1):297–312.
Olde Rikkert MG, Rigaud AS. Melatonin in elderly patients with insomnia.A systematic review. Z Gerontol Geriatr. 2001;34(6):491–7.
Mancuso M, et al. Clinical features and pathogenesis of Alzheimer’s disease: involvement of mitochondria and mitochondrial DNA. Adv Exp Med Biol. 2010;685:34–44.
Musiek ES, Xiong DD, Holtzman DM. Sleep, circadian rhythms, and the pathogenesis of Alzheimer disease. Exp Mol Med. 2015;47:e148.
Srinivasan V, et al. Melatonin and its agonist ramelteon in Alzheimer’s disease: possible therapeutic value. Int J Alzheimers Dis. 2010;2011:741974.
Feng Z, et al. Melatonin alleviates behavioral deficits associated with apoptosis and cholinergic system dysfunction in the APP 695 transgenic mouse model of Alzheimer’s disease. J Pineal Res. 2004;37(2):129–36.
Matsubara E, et al. Melatonin increases survival and inhibits oxidative and amyloid pathology in a transgenic model of Alzheimer’s disease. J Neurochem. 2003;85(5):1101–8.
Brusco LI, Marquez M, Cardinali DP. Melatonin treatment stabilizes chronobiologic and cognitive symptoms in Alzheimer’s disease. Neuro Endocrinol Lett. 2000;21(1):39–42.
Hardeland R. Divergent importance of chronobiological considerations in high- and low-dose melatonin therapies. Diseases. 2021;9(1):18.
Serfaty M, et al. Double blind randomised placebo controlled trial of low dose melatonin for sleep disorders in dementia. Int J Geriatr Psychiatry. 2002;17(12):1120–7.
Singer C, et al. A multicenter, placebo-controlled trial of melatonin for sleep disturbance in Alzheimer’s disease. Sleep. 2003;26(7):893–901.
Gehrman PR, et al. Melatonin fails to improve sleep or agitation in double-blind randomized placebo-controlled trial of institutionalized patients with Alzheimer disease. Am J Geriatr Psychiatry. 2009;17(2):166–9.
Wade AG, et al. Add-on prolonged-release melatonin for cognitive function and sleep in mild to moderate Alzheimer’s disease: a 6-month, randomized, placebo-controlled, multicenter trial. Clin Interv Aging. 2014;9:947–61.
McCleery J, Sharpley AL. Pharmacotherapies for sleep disturbances in dementia. Cochrane Database Syst Rev. 2020;11:CD009178.
Erland LA, Saxena PK. Melatonin natural health products and supplements: presence of serotonin and significant variability of melatonin content. J Clin Sleep Med. 2017;13(2):275–81.
Kato K, et al. Neurochemical properties of ramelteon (TAK-375), a selective MT1/MT2 receptor agonist. Neuropharmacology. 2005;48(2):301–10.
McKenna JT, et al. Chronic ramelteon treatment in a mouse model of Alzheimer’s disease. Arch Ital Biol. 2012;150(1):5–14.
Roth T, et al. Effects of ramelteon on patient-reported sleep latency in older adults with chronic insomnia. Sleep Med. 2006;7(4):312–8.
Asano M, et al. Effects of ramelteon on refractory behavioral and psychological symptoms of dementia in Alzheimer disease. J Clin Psychopharmacol. 2013;33(4):579–81.
He P, et al. A novel melatonin agonist Neu-P11 facilitates memory performance and improves cognitive impairment in a rat model of Alzheimer’ disease. Horm Behav. 2013;64(1):1–7.
Wu CS, et al. The association between dementia and long-term use of benzodiazepine in the elderly: nested case-control study using claims data. Am J Geriatr Psychiatry. 2009;17(7):614–20.
de Gage SB, et al. Benzodiazepine use and risk of Alzheimer’s disease: case-control study. Bmj-Br Med J. 2014;349:g5205.
Lee J, et al. Use of sedative-hypnotics and the risk of Alzheimer’s dementia: a retrospective cohort study. PLoS ONE. 2018;13(9):e0204413.
Islam MM, et al. Benzodiazepine use and risk of dementia in the elderly population: a systematic review and meta-analysis. Neuroepidemiology. 2016;47(3–4):181–91.
Cheng HT, et al. The association between the use of Zolpidem and the risk of Alzheimer’s disease among older people. J Am Geriatr Soc. 2017;65(11):2488–95.
Billioti de Gage S, et al. Benzodiazepine use and risk of dementia: prospective population based study. BMJ. 2012;345:e6231.
Gray SL, et al. Benzodiazepine use and risk of incident dementia or cognitive decline: prospective population based study. BMJ. 2016;352:i90.
Bietry FA, et al. Benzodiazepine use and risk of developing Alzheimer’s disease: a case-control study based on Swiss claims data. CNS Drugs. 2017;31(3):245–51.
Imfeld P, et al. Benzodiazepine use and risk of developing Alzheimer’s disease or vascular dementia: a case-control analysis. Drug Saf. 2015;38(10):909–19.
Richardson K, et al. Adverse effects of Z-drugs for sleep disturbance in people living with dementia: a population-based cohort study. BMC Med. 2020;18(1):351.
Richardson K, et al. Non-benzodiazepine hypnotic use for sleep disturbance in people aged over 55 years living with dementia: a series of cohort studies. Health Technol Assess. 2021;25(1):1–202.
By the American Geriatrics Society Beers Criteria Update Expert P. American Geriatrics Society 2019 Updated AGS Beers Criteria(R) for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019;67(4):674–94.
Machado FV, et al. More than a quarter century of the most prescribed sleeping pill: systematic review of Zolpidem use by older adults. Exp Gerontol. 2020;136:110962.
Wong J, et al. Trends in dispensing of Zolpidem and low-dose trazodone among commercially insured adults in the United States, 2011–2018. JAMA. 2020;324(21):2211–3.
Maust DT, et al. Prevalence of central nervous system-active polypharmacy among older adults with dementia in the US. JAMA. 2021;325(10):952–61.
McCarten JR, et al. Triazolam in Alzheimer’s disease: pilot study on sleep and memory effects. Pharmacol Biochem Behav. 1995;52(2):447–52.
Defrancesco M, et al. Use of benzodiazepines in Alzheimer’s disease: a systematic review of literature. Int J Neuropsychopharmacol. 2015;18(10):pyv055.
Gabelle A, et al. Cerebrospinal fluid levels of orexin-A and histamine, and sleep profile within the Alzheimer process. Neurobiol Aging. 2017;53:59–66.
Herring WJ, et al. Polysomnographic assessment of suvorexant in patients with probable Alzheimer’s disease dementia and insomnia: a randomized trial. Alzheimers Dement. 2020;16(3):541–51.
Hanazawa T, Kamijo Y. Effect of Suvorexant on nocturnal delirium in elderly patients with Alzheimer’s disease: a case-series study. Clin Psychopharmacol Neurosci. 2019;17(4):547–50.
Moline M, et al. Safety and efficacy of Lemborexant in patients with irregular sleep-wake rhythm disorder and Alzheimer’s disease dementia: results from a phase 2 randomized clinical trial. J Prev Alzheimers Dis. 2021;8(1):7–18.
Zammit G, et al. Daridorexant, a new dual orexin receptor antagonist, in elderly subjects with insomnia disorder. Neurology. 2020;94(21):e2222–32.
Stahl SM. Mechanism of action of trazodone: a multifunctional drug. CNS Spectr. 2009;14(10):536–46.
Montgomery I, et al. Trazodone enhances sleep in subjective quality but not in objective duration. Br J Clin Pharmacol. 1983;16(2):139–44.
Sateia MJ, et al. Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2017;13(2):307–49.
Mander BA, et al. beta-amyloid disrupts human NREM slow waves and related hippocampus-dependent memory consolidation. Nat Neurosci. 2015;18(7):1051–7.
Camargos EF, et al. Trazodone improves sleep parameters in Alzheimer disease patients: a randomized, double-blind, and placebo-controlled study. Am J Geriatr Psychiatry. 2014;22(12):1565–74.
La AL, et al. Long-term trazodone use and cognition: a potential therapeutic role for slow-wave sleep enhancers. J Alzheimers Dis. 2019;67(3):911–21.
Ferini-Strambi L, et al. Therapy for insomnia and circadian rhythm disorder in Alzheimer disease. Curr Treat Options Neurol. 2020;22(2):4.
Weber J, et al. Low-dose doxepin: in the treatment of insomnia. CNS Drugs. 2010;24(8):713–20.
Lie JD, et al. Pharmacological treatment of insomnia. P T. 2015;40(11):759–71.
Scharf M, et al. Efficacy and safety of doxepin 1 mg, 3 mg, and 6 mg in elderly patients with primary insomnia: a randomized, double-blind, placebo-controlled crossover study. J Clin Psychiatry. 2008;69(10):1557–64.
Bu J, Zu H. Mechanism underlying the effects of doxepin on beta-amyloid -induced memory impairment in rats. Iran J Basic Med Sci. 2017;20(9):1044–9.
Cakir S, Kulaksizoglu IB. The efficacy of mirtazapine in agitated patients with Alzheimer’s disease: a 12-week open-label pilot study. Neuropsychiatr Dis Treat. 2008;4(5):963–6.
Raji MA, Brady SR. Mirtazapine for treatment of depression and comorbidities in Alzheimer disease. Ann Pharmacother. 2001;35(9):1024–7.
Scoralick FM, et al. Mirtazapine does not improve sleep disorders in Alzheimer’s disease: results from a double-blind, placebo-controlled pilot study. Psychogeriatrics. 2017;17(2):89–96.
Maitre M, Klein C, Mensah-Nyagan AG. A proposed preventive role for Gamma-hydroxybutyrate (Xyrem(R)) in Alzheimer’s disease. Alzheimers Res Ther. 2016;8:37.
Klein C, et al. gamma-Hydroxybutyrate (Xyrem) ameliorates clinical symptoms and neuropathology in a mouse model of Alzheimer’s disease. Neurobiol Aging. 2015;36(2):832–44.
Buchele F, et al. Sodium Oxybate for excessive daytime sleepiness and sleep disturbance in Parkinson disease: a randomized clinical trial. JAMA Neurol. 2018;75(1):114–8.
Cooke JR, et al. Acetylcholinesterase inhibitors and sleep architecture in patients with Alzheimer’s disease. Drugs Aging. 2006;23(6):503–11.
Schredl M, et al. Donepezil-induced REM sleep augmentation enhances memory performance in elderly, healthy persons. Exp Gerontol. 2001;36(2):353–61.
Ross JS, Shua-Haim JR. Aricept-induced nightmares in Alzheimer’s disease: 2 case reports. J Am Geriatr Soc. 1998;46(1):119–20.
Stahl SM, et al. Examination of nighttime sleep-related problems during double-blind, placebo-controlled trials of galantamine in patients with Alzheimer’s disease. Curr Med Res Opin. 2004;20(4):517–24.
Naharci MI, et al. Galantamine improves sleep quality in patients with dementia. Acta Neurol Belg. 2015;115(4):563–8.
Ancoli-Israel S, et al. Effects of galantamine versus donepezil on sleep in patients with mild to moderate Alzheimer disease and their caregivers: a double-blind, head-to-head, randomized pilot study. Alzheimer Dis Assoc Disord. 2005;19(4):240–5.
Ishikawa I, et al. The effect of memantine on sleep architecture and psychiatric symptoms in patients with Alzheimer’s disease. Acta Neuropsychiatr. 2016;28(3):157–64.
Gray SL, et al. Cumulative use of strong anticholinergics and incident dementia: a prospective cohort study. JAMA Intern Med. 2015;175(3):401–7.
Savaskan E, et al. Treatment of behavioural, cognitive and circadian rest-activity cycle disturbances in Alzheimer’s disease: haloperidol vs. quetiapine. Int J Neuropsychopharmacol. 2006;9(5):507–16.
Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia—meta-analysis of randomized placebo-controlled trials. Jama-J Am Med Assoc. 2005;294(15):1934–43.
Schneider LS, Dagerman K, Insel PS. Efficacy and adverse effects of atypical antipsychotics for dementia: meta-analysis of randomized, placebo-controlled trials. Am J Geriatr Psychiatry. 2006;14(3):191–210.
Maust DT, et al. Antipsychotics, other psychotropics, and the risk of death in patients with dementia: number needed to harm. JAMA Psychiat. 2015;72(5):438–45.
Seo JS, et al. Oriental medicine Jangwonhwan reduces Abeta(1–42) level and beta-amyloid deposition in the brain of Tg-APPswe/PS1dE9 mouse model of Alzheimer disease. J Ethnopharmacol. 2010;128(1):206–12.
Yue S, et al. Effectiveness of Yi-Zhi-An-Shen granules on cognition and sleep quality in older adults with amnestic mild cognitive impairment: protocol for a randomized, double-blind, placebo-controlled trial. Trials. 2019;20(1):518.
Niitsu T, Okamoto H, Iyo M. Behavioural and psychological symptoms of dementia in an Alzheimer’s disease case successfully treated with natural medicine: association with gonadotropins. Psychogeriatrics. 2013;13(2):124–7.
Okamoto H, et al. Yokukan-san: a review of the evidence for use of this Kampo herbal formula in dementia and psychiatric conditions. Neuropsychiatr Dis Treat. 2014;10:1727–42.
Hayashi Y, et al. An open-label trial of Yokukansan on sleep disturbance in Alzheimer’s disease and other dementia. J Prev Alzheimers Dis. 2015;2(3):172–7.
Matsui K, et al. Effect of Yokukansan for the treatment of idiopathic rapid eye movement sleep behavior disorder: a retrospective analysis of consecutive patients. J Clin Sleep Med. 2019;15(8):1173–8.
Matsunaga S, Kishi T, Iwata N. Yokukansan in the treatment of behavioral and psychological symptoms of dementia: an updated meta-analysis of randomized controlled trials. J Alzheimers Dis. 2016;54(2):635–43.
Abad VC, Guilleminault C. Insomnia in elderly patients: recommendations for pharmacological management. Drugs Aging. 2018;35(9):791–817.
Taibi DM, et al. A systematic review of valerian as a sleep aid: safe but not effective. Sleep Med Rev. 2007;11(3):209–30.
Shinjyo N, Waddell G, Green J. Valerian root in treating sleep problems and associated disorders-a systematic review and meta-analysis. J Evid Based Integr Med. 2020. https://doi.org/10.1177/2515690X20967323.
Widner B, Ledochowski M, Fuchs D. Sleep disturbances and tryptophan in patients with Alzheimer’s disease. Lancet. 2000;355(9205):755–6.
Maurizi CP. The therapeutic potential for tryptophan and melatonin: possible roles in depression, sleep, Alzheimer’s disease and abnormal aging. Med Hypotheses. 1990;31(3):233–42.
Hertzman PA, et al. Association of the eosinophilia-myalgia syndrome with the ingestion of tryptophan. N Engl J Med. 1990;322(13):869–73.
Allen JA, et al. Post-epidemic eosinophilia-myalgia syndrome associated with L-tryptophan. Arthritis Rheum. 2011;63(11):3633–9.
Babson KA, Sottile J, Morabito D. Cannabis, cannabinoids, and sleep: a review of the literature. Curr Psychiatry Rep. 2017;19(4):23.
Elsaid S, Kloiber S, Le Foll B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog Mol Biol Transl Sci. 2019;167:25–75.
Khodadadi H, et al. Cannabidiol ameliorates cognitive function via regulation of IL-33 and TREM2 upregulation in a murine model of Alzheimer’s disease. J Alzheimers Dis. 2021;80:973–7.
Walther S, et al. Delta-9-tetrahydrocannabinol for nighttime agitation in severe dementia. Psychopharmacology. 2006;185(4):524–8.
Chagas MH, et al. Cannabidiol can improve complex sleep-related behaviours associated with rapid eye movement sleep behaviour disorder in Parkinson’s disease patients: a case series. J Clin Pharm Ther. 2014;39(5):564–6.
Olley R, Morales A. Systematic review of evidence underpinning non-pharmacological therapies in dementia. Aust Health Rev. 2018;42(4):361–9.
Ball EL, et al. Aromatherapy for dementia. Cochrane Database Syst Rev. 2020;8:CD003150.
Svetnik V, Wang T-C, Ceesay P, et al. Pilot evaluation of a consumer wearable actigraphy device in a clinical polysomnography trial of suvorexant for treating insomnia in patients with Alzheimer’s disease. J Sleep Res. 2021. https://doi.org/10.1111/jsr.13328.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was accepted by the authors in support of this publication.
Conflicts of interest
Joshua Roland, MD, has no conflicts of interest to disclose. Donald Bliwise, PhD, has been a consultant to Eisai, Ferring, Huxley, and Merck.
Ethics approval
Not applicable.
Consent
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author contributions
Manuscript first draft: JR. Final manuscript: all authors. Authors approve of the final version for publication.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Roland, J.P., Bliwise, D.L. Impact of Pharmacotherapy on Insomnia in Patients with Alzheimer’s Disease. Drugs Aging 38, 951–966 (2021). https://doi.org/10.1007/s40266-021-00891-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-021-00891-1