Abstract
Background
Medication for elderly patients is often complex and problematic. Several criteria for classifying inappropriate prescribing exist. In 2010, the Swedish National Board of Health and Welfare published the document “Indicators of appropriate drug therapy in the elderly” as a guideline for improving prescribing for the elderly.
Objective
The aim of this study was to assess trends in the prescription of inappropriate drug therapy in the elderly in Sweden from 2006 to 2013 using national quality indicators for drug treatment.
Methods
Individual-based data on dispensed prescription drugs for the entire Swedish population aged ≥65 years during eight 3-month periods from 2006 to 2013 were accumulated. The data were extracted from the Swedish Prescribed Drug Register. Eight drug-specific quality indicators were monitored.
Results
For the entire population studied (n = 1,828,283 in 2013), six of the eight indicators showed an improvement according to the guidelines; the remaining two indicators (drugs with anticholinergic effects and excessive polypharmacy) remained relatively unchanged. For the subgroup aged 65–74 years, three indicators showed an improvement, four indicators remained relatively unchanged (e.g. propiomazine, and oxazepam) and one showed an undesirable trend (anticholinergic drugs) according to guidelines. For the older group (aged ≥75 years), all indicators except excessive polypharmacy showed improvement.
Conclusion
According to the quality indicators used, the extent of inappropriate drug therapy in the elderly decreased from 2006 to 2013 in Sweden. Thus, prescribers appear to be more likely to change their prescribing patterns for the elderly than previously assumed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
According to the quality indicators used, the extent of inappropriate drug therapy in the elderly decreased from 2006 to 2013 in Sweden. |
Prescribers appear to be more likely to change their prescribing patterns for the elderly than previously assumed. |
1 Background
Medication for older people (those aged ≥65 years) is often perceived as complex and problematic, and various efforts have been made to improve drug therapy for the elderly, primarily by trying to avoid drugs deemed to be ‘inappropriate’ [1].
Several documents listing criteria for classifying inappropriate prescriptions have been offered. Almost all of these focus on the use of specific drugs by individual elderly patients, e.g. Beers’ criteria [2], the Improving Prescribing in the Elderly Tool (IPET) [3], the Screening Tool of Older persons’ Potentially inappropriate Prescriptions (STOPP) [4], McLeod’s criteria [5], and the Medication Appropriateness Index (MAI) [6]. Some studies have used a combination of several of the more well-known criteria [7].
The widely recognized MAI and Beers’ criteria were published in the early 1990s. The MAI measures the overall prescription quality in ten areas, without specifying which drugs are to be avoided [6]. Originally, Beers’ criteria included a list of drugs to be avoided only in the elderly nursing home population [2] but they were then modified to include community-dwelling elderly [8] and were later updated [9].
In 2003, the Swedish National Board of Health and Welfare issued a proposal based on international developments in the field [2, 5, 8–12] presenting indicators that could be used to evaluate the quality of drug use by the elderly in Sweden [13]. The intention was that the indicators should be applied under a variety of circumstances in order to improve the drug therapy of elderly patients: by supporting the prescription of drugs to the elderly, when monitoring prescribing patterns, and in national monitoring and epidemiological studies. The indicators also enabled investigation of the relationships between drug prescription processes, outcomes and costs over time.
In 2009, a proposal for an updated, expanded version of the quality indicators was presented and in 2010, “Indicators of appropriate drug therapy in the elderly” was published [14] (Table 1). Two groups of quality indicators were provided in the document: drug-specific and diagnosis-specific. Some of these indicators are suitable for use in the analysis of registers of dispensed drugs in large populations. It is important to underline that the drug-specific indicators are defined in terms of the number of recipients of the drug as a percentage of the entire elderly population and are therefore primarily relevant on a population level only. Furthermore, because of the increased sensitivity to drugs with greater age, these indicators are most applicable for the group aged over 75 years [14].
The establishment of the national Swedish Prescribed Drug Register in 2005 enabled analysis of the utilization of dispensed prescription drugs for the entire population [15]. The register provides individual data that can be used for exploring and analyzing the quality of drug use in the elderly for the whole of Sweden. These individual-based data can also be applied in longitudinal studies of the development of drug therapies for the elderly.
The Swedish Prescribed Drug Register has been used in studies of drug treatment in the elderly since 2005 [16–18]. Unfortunately, over the years, the focus of these reports has shifted from drug use among different age groups to housing types, time periods and measuring methods. Consequently, the results are not comparable over time. Thus, no long-term trends concerning these indicators of quality have been reported, and the need for an investigation in this area is apparent.
2 Objective
The aim of this study was to assess trends in the prescription of inappropriate drug therapy in the elderly in Sweden from 2006 to 2013 using national quality indicators for drug treatment.
3 Methods
To assess changes in the extent of appropriate drug therapy for older people in a national population, we employed a list of drug-specific quality indicators from the publication “Indicators of appropriate drug therapy in the elderly” [14], obtained from the Swedish National Board of Health and Welfare, and individual-based data on dispensed prescription drugs in the entire Swedish population aged ≥65 years over eight 3-month periods (January, February and March) for the period 2006–2013. The data were extracted from the Swedish Prescribed Drug Register [15]. With the assumption that the level of primary non-adherence was unchanged for the drugs included in the indicators during the study period, we used the data on dispensed prescription drugs as proxy for changes in prescription patterns during the study period.
The individual data relating to dispensed prescription drugs were processed without the original personal identification numbers of the recipients; all data were anonymous. Instead, a unique temporary individual identifier, specifying year of birth, was applied and the study population was stratified by age (in 5-year groups). The results are presented with respect to the number of individuals per age group in the Swedish population during the corresponding periods.
The number of individuals and the number of dispensed prescription drugs per individual were recorded; a drug was defined as a chemical entity or substance or combination of substances from the fifth level in the Anatomical Therapeutic Chemical (ATC) classification system [19].
3.1 Indicators
We selected all the eight (out of 34) drug-specific indicators from the publication “Indicators of appropriate drug therapy in the elderly” that were suitable for application to the register and did not require complementary information from patients’ medical records. The selected indicators belonged to three categories of drugs (A, B and C below) that can be considered universally applicable to the elderly.
3.1.1 Category A: Drugs that Older People Should Avoid Unless There are Special Reasons Not to Do So
The guidelines state that the number of elderly patients who use these medications (as a percentage of the total elderly population) should be as low as possible.
-
Long-acting benzodiazepines: ATC code N05BA01 (diazepam), N05CD02 (nitrazepam), N05CD03 (flunitrazepam)
-
Drugs with anticholinergic effects: ATC code A03AB (glycopyrrolate), A03BA (e.g. atropine), A03BB (e.g. butylscopolamine), A04AD (scopolamine), C01BA (disopyramide), G04BD (e.g. oxybutynin), N02AG (e.g. morphine), N04A (e.g. trihexyphenidyl), N05AA (levomepromazine), N05AF03 (chlorprotixene), N05AH02 (clozapine), N05BB01 (hydroxyzine), N06AA (e.g. clomipramine), R06AA02 (dimenhydrinate), R06AB (e.g. chlorpheniramine), R06AD (e.g. alimemazine), R06AX02 (cyproheptadine)
-
Tramadol: ATC code N02AX02
-
Propiomazine: ATC code N05CM06
3.1.2 Category B: Polypharmacy
The guidelines state that the number of elderly patients receiving polypharmacy should be as low as possible.
-
Excessive polypharmacy is defined as concomitant treatment with ten or more drugs regularly or as needed.
-
Polypharmacy is also defined as concomitant treatment with three or more psychotropic drugs [from one or more ATC groups N05A (e.g. clozapine), N05B (e.g. diazepam), N05C (e.g. zolpidem), N06 (e.g. fluoxetine)] regularly or as needed.
3.1.3 Category C: Specific Psychotropic Drugs
The guidelines state that:
-
Of all elderly patients treated with tranquilizers (N05B), the proportion (percentage) who use oxazepam (N05BA04) in preference to other alternatives in N05B should be as high as possible.
-
Of all elderly patients treated with hypnotics or sedatives (N05C), the proportion who use zopiclone (N05CF01) in preference to other alternatives in N05C should be as high as possible.
3.2 Comparability of Data
Since ten or more dispensed drugs during a 3-month period is the most widely used definition of excessive polypharmacy [20–23], comparisons with other studies were possible. As a rule, the filling of one prescription covers consumption for a 3-month period in Sweden. To achieve comparability between indicators and over the years, we selected the same periods for analyses of all the selected indicators.
3.3 Swedish Prescribed Drug Register
The Swedish Prescribed Drug Register [15] provides records for the entire Swedish population and covers approximately 82 % of all defined daily doses (DDDs) of medications dispensed in Sweden. The register does not include data on over-the-counter (OTC) medications (13 %), in-hospital medications (4 %), or non-institutional care medications (1 % of all DDDs distributed in Sweden). The register is also not complete with regard to vaccines or non-dose-dispensed drugs in nursing homes.
The Swedish Prescribed Drug Register is individual-based and contains data on dispensed outpatient prescriptions from all Swedish pharmacies from 1 July 2005. The registration of dispensed drugs is mandatory in Sweden. The following data were used in our study: the dispensed drug (substance), date of dispensing, age, and unique identifier (personal identification number) of the patient.
3.4 Study Population
The study population included all individuals aged ≥65 years during eight 3-month periods (January, February and March) from 2006 to 2013. The number of participants increased by 16.2 % from quarter (Q) 1 in 2006 to Q1 in 2013. The largest increase (39.8 %) occurred in the group aged 65–69 years. The group aged 80–84 years decreased by 4.4 %. The number of individuals in the group aged 65–79 years increased by 22.6 %, and the group aged ≥80 years increased by 1.9 % (Table 2).
The group aged ≥100 years was excluded from the graphic representations of the eight indicators because of the small numbers of individuals involved (n = 1,836, representing 0.1 % of the study population in 2013).
Sums and frequencies were calculated using Microsoft Excel, version 2010 (14.0.6126.5000) SP 1 MSO (14.0.6129.5000), (Microsoft Corporation, Redmond, WA, USA).
The study was approved by the Swedish Regional Ethical Review Board in Linköping.
4 Results
4.1 Drugs that Older People Should Avoid
4.1.1 Long-Acting Benzodiazepines
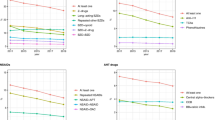
The number of elderly people for whom long-acting benzodiazepines were dispensed, given as a percentage of the total population aged ≥65 years, decreased from 3.5 % to 1.7 % (−52.2 %) in the period Q1 2006 to Q1 2013. The proportion decreased consistently over the study period and occurred in all age groups, with the greatest decrease seen in the oldest group (95–99 years; −58.5 %; Fig. 1).
4.1.2 Drugs with Anticholinergic Effects
The number of elderly people for whom drugs with anticholinergic effects were dispensed, given as a percentage of the total elderly population, decreased marginally during the study period, from 1.5 % to 1.4 % (−1.2).
There were decreases in the groups aged ≥80 years, with the largest decrease in the oldest group (95–99 years; −35.6 %). In the groups aged 65–69 years and 70–74 years, the proportion increased by 28.2 and 16.9 %, respectively (Fig. 2).
4.1.3 Propiomazine
The number of elderly people for whom propiomazine was dispensed, given as a percentage of the total elderly population, decreased from 2.7 % to 2.0 % (−24.4 %) during the study period (Fig. 3).The decrease was consistent over the study period. The proportion decreased in all age groups, except for the group aged 65–69 years. The largest decrease was seen in the oldest group (95–99 years; −55.5 %).
4.1.4 Tramadol
The number of elderly people for whom tramadol was dispensed, given as a percentage of the total elderly population, decreased from 3.9 % to 2.3 % (−41.1 %) during the study period (Fig. 3).
The proportion decreased in all age groups, with the largest decrease seen in the oldest group (95–99 years; −65.3 %). The greatest reduction occurred between Q1 2012 and Q1 2013 (−19.3 %).
4.2 Polypharmacy
4.2.1 Excessive Polypharmacy
The number of elderly people receiving excessive polypharmacy (ten or more concurrent prescription drugs dispensed regularly or as required), given as a percentage of the total elderly population, decreased marginally during Q1 2006 to Q1 2013, from 10.1 % to 10.0 % (−1.2 %) (Fig. 4). The difference between age groups was marginal.
4.2.2 Three or More Concurrent Psychotropic Drugs
The number of elderly people for whom three or more concurrent psychotropic drugs were dispensed, given as a percentage of the total elderly population, decreased from 3.5 % to 3.1 % (−11.0 %) during the study period (Fig. 4).
4.3 Individual Psychotropic Drugs
4.3.1 Oxazepam
The number of elderly patients for whom oxazepam was dispensed, given as a percentage of the total elderly population receiving any tranquilizer, increased from 59.9 % to 63.6 % (+6.2 %) over the period from Q1 2006 to Q1 2013 (Fig. 5). The largest increase was seen in the three oldest groups (85–89 years, 90–94 years, and 95–99 years; +11.8, +12.4, and +11.0 %, respectively).
The proportion of elderly individuals in Sweden (aged ≥65 years) receiving tranquilizers for whom oxazepam was dispensed, and the proportion of elderly individuals in Sweden (aged ≥65 years) receiving hypnotics or sedatives for whom zopiclone was dispensed, over the period Q1 2006 to Q1 2013. Q1 Quarter 1
4.3.2 Zopiclone
The number of elderly patients for whom zopiclone was dispensed, given as a percentage of the total elderly population receiving any hypnotic or sedative, increased from 42.6 % to 53.9 % (+26.5 %) during the study period (Fig. 5). The increase was consistent over the study period. The largest increase was seen in the oldest groups (85–89 years, 90–94 years, and 95–99 years; +32.8, +34.4 and +46.4 %, respectively).
5 Discussion
We found that the extent of inappropriate drug therapy for the elderly (≥65 years of age) improved, according to the national guidelines for this age group, over the period 2006–2013 in Sweden. The positive trend was more pronounced for those aged ≥75 years. Considering that the medication requirements for older patients are commonly described as increasingly complex and problematic, this improvement was unexpected, and offers hope.
5.1 Long-Term Trends
The changes to the indicators were relatively constant during the course of the study, particularly for the reduction in prescribing of long-acting benzodiazepines and the increase in prescribing of zopiclone. Similarly, the absence of change in the indicators for drugs with anticholinergic effects and excessive polypharmacy was stable during the whole period.
Our results displayed no clear link between the addition of an indicator to the Swedish guidelines and changes to prescribing patterns. For example, the indicator drugs with anticholinergic effects has changed only marginally since it was added to the guidelines in 2003, and the indicators involving the use of tramadol, propiomazine, oxazepam and zopiclone were already changing in the appropriate direction before their introduction to the guidelines proposal in 2009.
Our findings confirm that, for most of the indicators, there is an ongoing long-term change in the patterns of prescribing. It appears likely that the current debate on drug therapy for the elderly has increased prescribers’ knowledge of inappropriate drugs and contributed to the changes to quality indicators. However, it remains unresolved whether the observed trends were the result of changes to the guidelines or whether the guidelines are merely reflecting a change in prescribing practice that was already occurring.
It also remains uncertain whether specific interventions introduced with the aim of affecting the indicators have in fact had any effect. In 2012, the Swedish government offered to reward counties managing to decrease the indicators of inappropriate drugs by 10 % in patients aged ≥65 years. Two of the 21 counties succeeded at the time [24] but the long-term effects of the intervention remain to be seen.
Our results also suggest that some indicators may have reached a level from which it is difficult to achieve any further progress. This could be because there are few or no alternative therapies available. It could also be the existence of other opposite treatment recommendations, e.g. the Swedish Medical Product Agency state that the use of drugs with anticholinergic effects are probably too low today [25].
With respect to the indicator excessive polypharmacy, while it may be possible to reduce or alter the use of one or two specific drugs, it is difficult to reduce the overall level of polypharmacy since there are many associated factors at a population level, e.g. increasing life expectancy, development of new therapies, increasing use of preventive strategies, and medical guidelines [26].
5.2 Comparison with Other Studies
The Swedish Association of Local Authorities and Regions and The National Board of Health and Welfare present the report “Quality and Efficiency in Swedish Health Care” every year. Unfortunately, the indicators, monitored age groups and methods of analysis have been altered through the years, resulting in non-comparable data. Thus, there have been no other reports of long-term trends in drug prescribing for the elderly in Sweden. However, official publications have discussed the difficulties associated with achieving change and the perception of stagnation in the process of reducing inappropriate medication to the elderly [27].
Long-term trends in inappropriate prescribing in the elderly have also been poorly investigated internationally [28], and the available studies often describe non-comparable sets of medications and use different measurement tools to estimate the overall prevalence of inappropriate prescribing [29, 30]. Nonetheless, studies have indicated, in line with our results, a slight decrease in the use of potentially inappropriate drugs by elderly patients [28, 31–33].
Our findings that excessive polypharmacy has remained at a constant level during the study period are not consistent with results from official Swedish reports [34, 35]. Although the methods of measurement have changed over the years and may have contributed to the decline, the reports claim that the proportion of the elderly receiving excessive polypharmacy has been reduced. In contrast, a short-term study has indicated that the proportion of elderly receiving excessive polypharmacy in Sweden increased over the period from 2005 to 2008 [36]. The general trend internationally also indicates an increasing prevalence of polypharmacy [37–41]. However, an increasing prevalence of polypharmacy does not necessarily imply increasing inappropriate prescribing among the elderly. Instead, increased prevalence of polypharmacy can actually be combined with reduced inappropriate prescribing [28].
5.3 Strengths and Weaknesses of the Study
The study does not cover all the national indicators of appropriate drug therapies in the elderly. Analysis of other drug- and diagnosis-specific indicators would have required access to the patients’ medical records for gathering complementary information records.
Since the indicators of quality chosen by the Swedish National Board of Health and Welfare are ‘national standards’ in the study population, we have not addressed their possible strengths and weaknesses compared with other quality indicators, despite the availability of alternative choices and the ongoing debate concerning the validity, relevance, measurability, interpretability, and uniqueness of different indicators.
As the study included all individuals in the population, we were able to avoid known problems associated with sampling, recall, interviews, and confidence levels. On the other hand, using registered data on dispensed drugs as an estimate of drug use could result in either over- or under-estimation of actual drug use.
5.4 Unanswered Questions and Future Research
For patients aged 65–74 years, three of eight indicators showed improvement over the 8-year period. During the same period, the number of individuals in this age group increased by 32 %, whereas the number of individuals aged ≥75 years hardly increased at all. It remains to be seen whether the overall positive trends in drug-specific quality indicators for all elderly will continue when the increasing number of individuals currently aged <75 years become older.
During the study period, the prescribing of several drugs included in the indicators declined and it is assumed that other alternative medications have been prescribed instead. The prescribing of alternative drugs and its clinical implications for patients remains to be studied in detail, e.g. the use of other opiates when the prescribing of tramadol declined.
6 Conclusions
According to the quality indicators used, the extent of inappropriate drug therapy in the elderly decreased from 2006 to 2013 in Sweden. This improvement was especially evident in the oldest patients, although this group still had the highest proportion of inappropriate drug use.
Overall, the results indicate that prescribers appear to be more likely to change their prescribing patterns for the elderly than previously assumed.
References
Shelton PS, Fritsch MA, Scott MA. Assessing medication appropriateness in the elderly: a review of available measures. Drugs Aging. 2000;16(6):437–50.
Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing home residents. UCLA Division of Geriatric Medicine. Arch Intern Med. 1991;151(9):1825–32.
Naugler CT, Brymer C, Stolee P, Arcese ZA. Development and validation of an improving prescribing in the elderly tool. Can J Clin Pharmacol. 2000;7(2):103–7.
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72–83.
McLeod PJ, Huang AR, Tamblyn RM, Gayton DC. Defining inappropriate practices in prescribing for elderly people: a national consensus panel. CMAJ. 1997;156(3):385–91.
Hanlon JT, Schmader KE, Samsa GP, Weinberger M, Uttech KM, Lewis IK, et al. A method for assessing drug therapy appropriateness. J Clin Epidemiol. 1992;45(10):1045–51.
Klarin I, Wimo A, Fastbom J. The association of inappropriate drug use with hospitalisation and mortality: a population-based study of the very old. Drugs Aging. 2005;22(1):69–82.
Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly: an update. Arch Intern Med. 1997;157(14):1531–6.
Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–24.
Oborne CA, Batty GM, Maskrey V, Swift CG, Jackson SH. Development of prescribing indicators for elderly medical inpatients. Br J Clin Pharmacol. 1997;43(1):91–7.
Oborne CA, Hooper R, Swift CG, Jackson SH. Explicit, evidence-based criteria to assess the quality of prescribing to elderly nursing home residents. Age Ageing. 2003;32(1):102–8.
van Dijk KN, Pont LG, de Vries CS, Franken M, Brouwers JR, de Jong-van den Berg LT. Prescribing indicators for evaluating drug use in nursing homes. Ann Pharmacother. 2003;37(7–8):1136–41.
Indicators for evaluation of drug therapy in the elderly. The National Board of Health and Welfare; 2003, 76. http://www.socialstyrelsen.se/publikationer2003/2003-110-20.
Indicators of good drug therapy in the elderly. The National Board of Health and Welfare; 2010, 96. http://www.socialstyrelsen.se/publikationer2010/2010-6-29.
Wettermark B, Hammar N, Fored CM, Leimanis A, Otterblad Olausson P, Bergman U, et al. The new Swedish Prescribed Drug Register: opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007;16(7):726–35.
Lesen E, Andersson K, Petzold M, Carlsten A. Socioeconomic determinants of psychotropic drug utilisation among elderly: a national population-based cross-sectional study. BMC Public Health. 2010;10:118.
Johnell K, Fastbom J. The use of benzodiazpines and related drugs amongst older people in Sweden: associated factors and concomitant use of other psychotropics. Int J Geriatr Psych. 2009;24(7):731–8.
Hovstadius B, Petersson G. Adherence, therapeutic intensity, and the number of dispensed drugs. Pharmacoepidemiol Drug Saf. 2011;20(12):1255–61.
WHO Collaborating Centre for Drug Statistics Methodology, Guidelines for ATC classification and DDD assignment 2014. Oslo, 2013. http://www.whocc.no/filearchive/publications/2014_guidelines.pdf
Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287(3):337–44.
Haider SI, Johnell K, Weitoft GR, Thorslund M, Fastbom J. The influence of educational level on polypharmacy and inappropriate drug use: a register-based study of more than 600,000 older people. J Am Geriatr Soc. 2009;57(1):62–9.
Bjerrum L, Sogaard J, Hallas J, Kragstrup J. Polypharmacy: correlations with sex, age and drug regimen: a prescription database study. Eur J Clin Pharmacol. 1998;54(3):197–202.
Flaherty JH, Perry HM 3rd, Lynchard GS, Morley JE. Polypharmacy and hospitalization among older home care patients. J Gerontol A Biol Sci Med Sci. 2000;55(10):M554–9.
Sammanhållen vård och omsorg om de mest sjuka äldre 2012: the Swedish National Board of Health and Welfare; 2012. http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18892/2012-11-16.pdf.
Swedish Medical Product Agency. Treatment recommendations. 2011.
Hovstadius B, Petersson G. Factors leading to excessive polypharmacy. Clin Geriatr Med. 2012;28(2):159–72.
Improving life for sick elderly: performing in 2012. Swedish Association of Local Authorities and Regions; 2012. http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/18892/2012-11-16.pdf
Lapi F, Pozzi C, Mazzaglia G, Ungar A, Fumagalli S, Marchionni N, et al. Epidemiology of suboptimal prescribing in older, community dwellers: a two-wave, population-based survey in Dicomano, Italy. Drugs Aging. 2009;26(12):1029–38.
Opondo D, Eslami S, Visscher S, de Rooij SE, Verheij R, Korevaar JC, et al. Inappropriateness of medication prescriptions to elderly patients in the primary care setting: a systematic review. PloS one. 2012;7(8):e43617.
Dimitrow MS, Airaksinen MS, Kivela SL, Lyles A, Leikola SN. Comparison of prescribing criteria to evaluate the appropriateness of drug treatment in individuals aged 65 and older: a systematic review. J Am Geriatr Soc. 2011;59(8):1521–30.
Stuart B, Kamal-Bahl S, Briesacher B, Lee E, Doshi J, Zuckerman IH, et al. Trends in the prescription of inappropriate drugs for the elderly between 1995 and 1999. Am J Geriatr Pharmacother. 2003;1(2):61–74.
Pugh MJ, Hanlon JT, Wang CP, Semla T, Burk M, Amuan ME, et al. Trends in use of high-risk medications for older veterans: 2004 to 2006. J Am Geriatr Soc. 2011;59(10):1891–8.
Zimmermann T, Kaduszkiewicz H, van den Bussche H, Schon G, Brettschneider C, Konig HH, et al. Potentially inappropriate medication in elderly primary care patients: a retrospective, longitudinal analysis. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz. 2013;56(7):941–9.
Quality and Efficiency in Swedish Health Care: regional comparisons 2009. Swedish Association of Local Authorities and Regions; 2009: p. 255.
National Drug Strategy. Stockholm: Government Offices; 2011. http://www.regeringen.se/content/1/c6/17/38/05/f10289bc.pdf
Hovstadius B, Hovstadius K, Astrand B, Petersson G. Increasing polypharmacy: an individual-based study of the Swedish population 2005–2008. BMC Clin Pharmacol. 2010;10:16.
Veehof L, Stewart R, Haaijer-Ruskamp F, Jong BM. The development of polypharmacy: a longitudinal study. Fam Pract. 2000;17(3):261–7.
Gorard DA. Escalating polypharmacy. QJM. 2006;99(11):797–800.
Haider SI, Johnell K, Thorslund M, Fastbom J. Trends in polypharmacy and potential drug–drug interactions across educational groups in elderly patients in Sweden for the period 1992–2002. Int J Clin Pharmacol Ther. 2007;45(12):643–53.
Linjakumpu T, Hartikainen S, Klaukka T, Veijola J, Kivela SL, Isoaho R. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol. 2002;55(8):809–17.
Jyrkka J, Vartiainen L, Hartikainen S, Sulkava R, Enlund H. Increasing use of medicines in elderly persons: a five-year follow-up of the Kuopio 75+Study. Eur J Clin Pharmacol. 2006;62(2):151–8.
Acknowledgments
Bo Hovstadius, Göran Petersson, Lina Hellström and Lisa Ericson declare no competing interests. We wish to thank Helena Schiöler, of the Swedish Board for Health and Welfare, for assistance with data gathering and statistical procedures associated with the Swedish prescribed drug register. Ellen Vinge, MD, PhD, and Stephan Quittenbaum, MD, are acknowledged for valuable comments on the manuscript. The study was financed by grants from the Kamprad Family Foundation for Entrepreneurship, Research and Charity. The study was designed and conducted independently of the Kamprad Family Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Hovstadius, B., Petersson, G., Hellström, L. et al. Trends in Inappropriate Drug Therapy Prescription in the Elderly in Sweden from 2006 to 2013: Assessment Using National Indicators. Drugs Aging 31, 379–386 (2014). https://doi.org/10.1007/s40266-014-0165-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-014-0165-5