Abstract
Surgery for Crohn’s disease (CD) is not curative, as postoperative recurrence (POR) after ileocolonic resection is the rule in the absence of prophylactic treatment. In the present article, we critically review available data on the role of anti-tumour necrosis factor (TNF) agents and new biologics (including vedolizumab and ustekinumab) in the prevention and treatment of POR after surgery in CD. Several studies (summarised in various meta-analyses) have confirmed the efficacy of anti-TNFs in the prevention of POR. We identified 37 studies, including 1863 CD patients, with mean endoscopic POR at 6–12 months of 29%. Only few randomised controlled trials (RCTs) have directly compared thiopurines and anti-TNFs, with controversial results, although the superiority of the latter is supported by several meta-analyses. Infliximab and adalimumab seem equally effective. The combination of anti-TNFs and immunosuppressives should be considered in patients previously exposed to anti-TNFs. Several studies have shown that anti-TNFs remain an effective option to prevent POR also in patients with anti-TNF failure before surgery. In fact, the use of the same anti-TNF before and after surgery might be effective for the prevention of POR. Prophylactic anti-TNF treatment, once started, should be continued long term. Anti-TNFs are also effective for the treatment of established POR. Retreatment with anti-TNFs for POR is a valid strategy even after their preoperative failure. In six studies (including 156 patients) evaluating vedolizumab, mean endoscopic POR at 6–12 months was 41%. The non-randomised comparison of anti-TNFs and vedolizumab has provided controversial results. One placebo-controlled RCT confirmed that vedolizumab is quite effective in preventing POR in CD patients with increased risk of recurrence. Seven studies (including 162 patients) evaluated ustekinumab, with a mean endoscopic POR at 6–12 months of 41%. The comparative efficacy of ustekinumab and anti-TNFs is still unclear. Ustekinumab and vedolizumab seem to be equally effective, although the experience is very limited. In conclusion, to date, anti-TNFs are the most effective agents in preventing and treating POR in CD. Anti-TNFs remain an effective option to prevent POR also in patients with anti-TNF failure before surgery. Vedolizumab seems to be quite effective in the prevention of POR in patients with increased risk of recurrence. Ustekinumab is probably also effective in the postoperative setting, although the comparative efficacy with anti-TNFs or vedolizumab is still unclear.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Anti-TNFs seem to be the most effective agents in preventing and treating postoperative recurrence in Crohn’s disease. These agents remain an effective option in patients with anti-TNF failure before surgery. |
Vedolizumab seems to be quite effective in the prevention of postoperative recurrence. |
Ustekinumab is probably also effective in the postoperative setting, although the comparative efficacy with anti-TNFs or vedolizumab is still unclear. |
1 Introduction
Crohn’s disease (CD) is a type of inflammatory bowel disease, which frequently leads to bowel damage and consequent disability. The increasing arsenal of treatment options and the growing utilisation of biologics have been associated with a reduction in the frequency of surgical resection [1]. Nonetheless, surgery remains an important treatment modality in patients with obstructive symptoms, penetrating complications, or medically refractory disease. Although a considerable number of patients necessitate surgery for CD, it is important not to perceive surgery as a failure in the treatment of the disease. Instead, surgery should be regarded as a fundamental component of a comprehensive, multidisciplinary approach to managing patients with CD.
Unfortunately, after surgery a high percentage of patients develop new lesions in intestinal segments previously unaffected by the disease, a phenomenon known as postoperative recurrence (POR) [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17]. Postoperative recurrence typically presents a continuum of characteristics from histologic findings to endoscopic lesions and clinical presentation. Thus, mucosal lesions (usually assessed by ileocolonoscopy and named endoscopic POR) generally develop early after surgery—within a few months—and generally precede the development of digestive symptoms (named clinical POR). Once POR is established, a proportion of patients will require new surgical resections (surgical POR) because of refractory or complicated disease, with the additional risk of losing intestinal functions. Since the severity of endoscopic POR correlates fairly well with the likelihood of developing clinical POR in the near future [18], endoscopic POR is commonly used as a surrogate marker for the risk of clinical POR in clinical trials, and drives therapeutic decisions in clinical practice.
Thus, although surgery can effectively address complications related to CD, ultimately these approaches are not curative: up to 90% of patients will demonstrate endoscopic POR in the neo-terminal ileum within 12 months of surgery, and within three years, endoscopic POR is almost universal [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17]. Clinical POR is present in up to 50% of patients within five postoperative years [19], and a repeat intestinal resection is required in 25% of patients within five years and 35% within 10 years [20]. Patients with CD with a previous bowel resection should therefore be evaluated, monitored, and treated appropriately, to prevent irreversible intestinal loss.
The efficacy of several drugs for the prevention of POR has been assessed [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17]. Mesalamine is ineffective, or at most minimally effective, for preventing endoscopic POR [9, 21,22,23,24,25,26,27,28]. Imidazole antibiotics are associated with lower short-term POR rates, but the effect is not sustained in the long term [29]. Regarding thiopurines, a meta-analysis published in 2009 concluded that purine analogues reduced clinical and overall endoscopic POR, but they were not effective in the prevention of severe endoscopic POR [30]. Also in 2009, a Cochrane review identified the association of azathioprine/mercaptopurine with significantly reduced risk of clinical and endoscopic POR, when compared with placebo [22]. More recently (2014) a systematic review concluded that evidence for routine use of azathioprine/mercaptopurine treatment in postoperative CD was heterogeneous and unconvincing [31]. A later network meta-analysis concluded that thiopurines showed greater efficacy in terms of clinical and endoscopic POR prophylaxis compared with 5-aminosalicylates or placebo, but with a higher incidence of adverse events [25]. A more recent updated Cochrane analysis concluded—with moderate certainty—that azathioprine and mercaptopurine were superior to placebo for maintenance of surgically induced remission of CD [32]. Finally, according to a recent network meta-analysis, thiopurines can be considered superior to placebo in preventing endoscopic POR [28]. Nevertheless, it should be noted that some of the classical studies evaluating these drugs included low, very likely sub-therapeutic, doses of thiopurines. In summary, thiopurines appear to be effective in reducing POR in CD, but with modest efficacy.
Current international guidelines on the postoperative management of CD recommend primary prevention of POR based on risk factors, including generally all patients except those with pure fibrotic and short ileal stenosis [29, 33, 34]. Both European and American guidelines recommend starting prophylactic postoperative medication with thiopurines or anti-tumour necrosis factor (TNF) agents in CD patients at high risk of POR [29, 33], with the most consistent risk factors being smoking, prior intestinal resection, and penetrating disease behaviour [35].
Despite the effectiveness of anti-TNF treatment in (non-operated) CD, many patients fail this strategy. The introduction of newer biological agents with novel mechanisms of action, namely vedolizumab and ustekinumab, has increased medical options for disease control [36]. However, little is known about the efficacy of anti-TNFs and these newer biological agents in the POR setting. In this context, the aim of the present article was to critically assess, through a comprehensive narrative review, available data on the role of anti-TNF agents and new biologics (including vedolizumab and ustekinumab) in the prevention and treatment of POR after surgery in CD.
2 Approach to the Literature
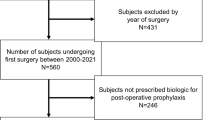
An electronic search was performed in PubMed up to February 2023 using the following algorithm: (post-operative OR postoperative OR "post operative" OR "ileocolic resection" OR "ileo-colic resection" OR "ileocolonic resection" OR "ileo-colonic resection") AND recurrence AND Crohn's AND (biologic OR biologics OR biological OR "anti-tumor necrosis factor" OR "anti-tumour necrosis factor" OR anti-TNF OR infliximab OR adalimumab OR golimumab OR certolizumab OR vedolizumab OR ustekinumab). Up to February 2023, 421 articles were retrieved with this search strategy. In addition, the reference lists of the selected articles, systematic reviews and meta-analyses, were reviewed to identify additional studies of potential interest. Articles published in any language were included. If a study was duplicated, the most recent one fulfilling the inclusion criteria was included.
3 Anti-TNF Agents
3.1 Efficacy of Anti-TNF Agents in the Prevention of Postoperative Recurrence (POR)
Several studies have evaluated the efficacy of anti-TNF agents for the prevention of POR in CD patients. Our main outcome of interest in the present review was endoscopic POR (defined as a Rutgeerts’ score of ≥ i2 on ileocolonoscopy), as this is robust and reproducible, and prevention of endoscopic POR is a strong surrogate measure of surgical POR the future [18]. Thus, the rate of endoscopic POR in the studies evaluating the efficacy of anti-TNF agents is summarised in Table 1 [37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. Some studies were excluded from this table because no detailed information was available to calculate endoscopic POR [73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95], another one was not considered because low infliximab doses were prescribed [96], and finally, a study was excluded because it represented a sub-analysis of an already included study [97]. In total, 37 studies were identified, including 1863 patients. Most were observational studies, mainly retrospective. The anti-TNF agents evaluated were infliximab (in most of the studies) and adalimumab (less frequently), while certolizumab was only assessed in one study. From data included in Table 1, the mean endoscopic POR at 6–12 months in patients receiving prophylactic anti-TNF treatment was 29% (weighted mean; 95% confidence interval [CI] 27–31%).i. RCTs on the efficacy of anti-TNF agents in the prevention of POR
Only a few randomised controlled trials (RCTs) have directly compared the efficacy of anti-TNF agents versus placebo (or mesalamine) in the context of POR [39, 41, 47, 52] as summarised below.
In 2009, Regueiro et al published the first RCT comparing infliximab against placebo for the prevention of POR in CD [39]. The authors randomly assigned 24 patients with CD and previous ileocolonic resection to receive either infliximab (5 mg/kg), first administered within 4 weeks of surgery and continuously for one year, or placebo. The rate of endoscopic POR at one year (the primary endpoint) was significantly lower in the infliximab group (1 of 11 patients; 9.1%) compared with the placebo group (11 of 13 patients; 85%).
In the study by Yoshida et al, published in 2012, 31 CD patients who had ileocolic resection within the previous 4 weeks were randomly assigned to scheduled infliximab at 5 mg/kg intravenously every eight weeks for 36 months (n = 15) or without infliximab (control, n = 16) [41]. The primary endpoint was clinical remission, but endoscopic POR was also evaluated. At 12 and 36 months, 100% and 93% of patients in the infliximab group were in clinical remission, respectively, versus 69% and 56% in the control arm (a statistically significant difference). Furthermore, the infliximab group achieved higher endoscopic remission (absence of endoscopic POR) at 12 months, 79% versus 19%.
Savarino et al evaluated, for the first time in an RCT, whether the administration of adalimumab after resective intestinal surgery reduced POR [47]. Fifty-one patients with CD and previous ileocolonic resection were randomly assigned to receive, after two weeks from surgery, adalimumab at the dose of 40 mg every two weeks or mesalamine, and they were followed-up for two years. The rate of endoscopic POR was significantly lower in the adalimumab group (6.3%) compared with the mesalamine group (83%). There was also a significantly lower proportion of patients with clinical POR in the adalimumab group (12%) compared with the mesalamine group (50%).
Finally, the “Prospective, Multicentre, Randomized, Double-Blind, Placebo-Controlled Trial Comparing Remicade (infliximab) and Placebo in the Prevention of Recurrence in Crohn's Disease Patients Undergoing Surgical Resection Who Are at an Increased Risk of Recurrence” (PREVENT) study, a landmark RCT assessing POR after anti-TNF therapy compared to placebo, was published in 2016 [52]. In this pioneer trial, CD patients with at least one risk factor for POR were randomised to receive infliximab (5 mg/kg every 8 weeks without the usual initial induction sequence) or placebo within 45 days of surgery. The primary endpoint was clinical POR, defined as a composite outcome consisting of a Crohn’s Disease Activity Index (CDAI) score > 200 and a ≥ 70-point increase from baseline, and endoscopic POR (Rutgeerts’ score ≥ i2, determined by a central reader) before or at Week 76. Endoscopic POR was a secondary outcome in this trial. Fewer patients in the infliximab group had clinical POR compared to the placebo group, but the difference was not statistically significant (13% vs 20%). However, the comparison for endoscopic POR did show clear superiority of infliximab (22% vs 51%). Of note, only 18% of patients with endoscopic POR also had recurrence based on the CDAI, which emphasises the well-known limitations of symptom-based scores in the postoperative setting [52].
Although the seminal PREVENT study showed the benefit of infliximab in reducing endoscopic POR, the differing results with regard to clinical and endoscopic POR resulted in a failure to achieve the primary composite endpoint, which in turn resulted in premature termination of the study, thereby likely precluding enough time for clinical complications to develop [98]. In addition, this study used every 8-week dosing for infliximab without induction; conceivably the 3-dose induction could have led to even lower POR rates [13, 15]. Another particularity of the PREVENT study is that only 17% of patients received concomitant immunosuppressive drugs (such as thiopurines). Finally, infliximab might have been started as late as 45 days after resection, when early endoscopic POR may have already been present.ii. Meta-analyses on the efficacy of anti-TNF agents in the prevention of POR
Several meta-analyses including studies evaluating the efficacy of anti-TNF agents for the prevention of POR in CD have been performed so far, and are summarised in Table 2 [12, 25, 26, 28, 99,100,101,102,103,104,105,106,107,108,109,110].
3.1.1 Other Studies on the Efficacy of Anti-TNF Agents in the Prevention of POR
Other studies, despite not being randomised-controlled, have provided relevant information on the role of anti-TNF agents in the prevention of POR. Shinagawa et al performed a sub-analysis within their large multicentre retrospective analysis of 1871 patients with CD who underwent intestinal resection before and after anti-TNF therapy was introduced in Japan in 2002 [111]. In the overall multivariable analysis, the postoperative use of anti-TNF therapy was associated with a lower need of surgery in the future.
Some surveys have assessed the clinical practice of POR management. Nguyen et al examined the clinical practice in the USA through a web-based survey sent to all members of the American Gastroenterological Association (AGA) and the American College of Gastroenterology [112]. In high-risk patients, 65% offered medical prophylaxis—most often biologics—immediately after surgery. In addition, an 11-question survey was distributed among gastroenterologists attending the European Crohn’s and Colitis Organisation (ECCO) congress [113]. With regard to the class of drug, the number of POR risk factors influenced the choice of treatment favouring biologics over thiopurines in 58% of respondents. In this group, 58% would consider directly starting a biologic if ≥ 2 risk factors were present, while 42% would make this choice only for ≥ 3 risk factors.
Regarding safety of anti-TNF agents specifically in the prevention of POR scenario, a meta-analysis comparing infliximab with non-biological agents, was unable to demonstrate any difference in adverse events [103]. Even when comparing infliximab with placebo, there were no differences in safety [114]. Moreover, a more recent meta-analysis showed that initiating postoperative anti-TNF therapy was not associated with an increased rate of adverse events [102].
In summary, several studies (summarised in various meta-analyses) have shown the efficacy of anti-TNF agents in the prevention of POR in CD patients, with a mean rate of endoscopic POR at 6–12 months of “only” approximately 30%. However, only a few RCTs have compared the efficacy of anti-TNF agents versus placebo (or mesalamine) in the context of POR.
3.2 Anti-TNFs Versus Thiopurines in the Prevention of POR
The superiority of anti-TNF agents over thiopurines for the prevention of POR after ileocolonic resection remains controversial. In fact, available guidelines do not express a clear preference for either agent in postoperative CD patients [29, 33]. For patients with surgically induced remission of CD, the AGA guideline suggests using anti-TNF therapy and/or thiopurines over other agents [33]; however, it acknowledges that “there is low-quality evidence favouring anti-TNF agents over thiopurines for reducing disease recurrence, with possibly a large effect size”; and it also points out that “the choice between anti-TNF and thiopurine monotherapy for preventing disease recurrence should include assessment of the patient’s risk of disease recurrence and risk-benefit considerations in the context of patients’ values and preferences” [33]. On the other hand, the ECCO guideline states that “to prevent POR the drugs of choice are thiopurines or anti-TNFs”; however, it is also mentioned, “although data are limited, anti-TNFs are the most effective treatment according to indirect comparisons” [29].
3.2.1 RCTs on the Efficacy of Anti-TNF Agents Versus Thiopurines in the Prevention of POR
Few RCTs with small sample sizes have directly compared the efficacy of thiopurines and anti-TNF agents in the postoperative setting [47, 48, 56], as summarised below.
Armuzzi et al conducted the first prospective RCT comparing clinical and endoscopic POR in patients treated with either infliximab or with azathioprine after curative resection for ileocecal CD [48]. In a small sample of 22 patients with defined high risk for POR, the authors found that there were no significant difference between the groups in terms of endoscopic POR (40% in the azathioprine group vs 9% in the infliximab group, p = 0.14). Obviously, this lack of statistically significant difference may be simply due to the small sample size and the consequent low statistical power.
Savarino et al conducted an RCT involving 51 patients comparing adalimumab with azathioprine (or mesalamine) [47]. Two years after surgery, the rate of endoscopic POR was significantly lower in adalimumab-treated patients (6.3%) compared with those receiving azathioprine (65%).
Finally, López-Sanromán conducted a 52-week RCT in which 84 patients with ileocolonic resection were randomised to either adalimumab or to azathioprine, both associated with metronidazole [56]. The primary endpoint was endoscopic POR at one year, as evaluated by a blinded central reader. Treatment discontinuation was significantly less frequent in the adalimumab (4.4%) than in the azathioprine group (23%). According to the intention-to-treat analysis, therapy failed in 23/39 (59%) patients in the azathioprine group and in 19/45 (42%) patients in the adalimumab group (p = 0.12). Although the authors concluded that adalimumab did not demonstrate a better efficacy than azathioprine for prophylaxis of POR, it may be argued that the almost 20% difference found between the two treatment strategies in this study might be clinically relevant, although not statistically significant probably due the low statistical power consequence of the small sample size. Finally, it should be noted that, in this study, the study drugs were administered to consecutive unselected patients, both with low and high risk of POR; this is a key feature, as benign short indolent stenosis was the only condition excluded in this study, while the populations of other studies are usually limited to patients at high risk of POR.
Some relevant conclusions can be extracted from the “Postoperative Crohn’s endoscopic recurrence” (POCER) trial, although the randomisation was designed to compare two postoperative management strategies (endoscopy vs no endoscopy, and not anti-TNF vs thiopurines) [50, 115]. Patients at high risk of POR (smokers, perforating disease, at least second operation) were treated after resection with thiopurines, while thiopurine-intolerant patients received adalimumab. Thus, the number of adalimumab-treated patients was determined by the rate of thiopurine intolerance. Nonetheless, the patient cohort was prospectively well defined, the groups were comparable in relation to their characteristics including previous drug therapy, and endoscopic assessment was blind to treatment. In summary, endoscopic POR occurred in 33 of 73 (45%) thiopurine- versus 6 of 28 (21%) adalimumab-treated patients. Therefore, the authors concluded that, in patients at high risk of POR, adalimumab was superior to thiopurines in preventing early disease recurrence.
3.2.2 Meta-analyses on the Efficacy of Anti-TNF Agents Versus Thiopurines in the Prevention of POR
As previously mentioned, several meta-analyses of studies evaluating the efficacy of anti-TNF agents for the prevention of POR in CD have been performed (Table 2). Some included studies also with a treatment arm with thiopurines so we could extract some conclusions on the relative effectiveness of anti-TNF versus thiopurines. The most recent meta-analysis concluded that biologics were more effective over non-biological treatments in preventing endoscopic, severe endoscopic, and clinical POR without increasing the frequency of adverse events [12]. Moreover, the conclusion of a superiority of anti-TNF over thiopurines in preventing POR is supported by several network meta-analyses [25, 26, 28, 100,101,102, 104, 106].
However, interpretation of results from meta-analyses (including network meta-analyses) is hindered by heterogeneity of included studies, with differences in: (1) type of anti-TNF (infliximab, adalimumab); (2) dose and regimen of the anti-TNF (induction plus maintenance vs only maintenance dose); (3) use of concomitant medication (mainly thiopurines); (4) previous use of anti-TNF (naïve or non-naïve); (5) number and type of risk factors for POR; (6) outcome definitions (including a Rutgeerts’ score of i2 in most of the cases, but also Rutgeerts’ i3 in some, and even CDAI or Harvey-Bradshaw Index in others); and (7) length of follow-up, among others.
To overcome the disadvantages of network analyses of published data, Beelen et al performed a meta-analysis of individual participant data, to compare the effect of thiopurines and anti-TNF agents [110]. Randomised controlled trials investigating thiopurines and/or anti-TNF agents after ileocolonic resection were included. Primary outcome was endoscopic POR (Rutgeerts’ score ≥ i2). In their meta-analysis, 645 patients from six studies were included. Three of the studies directly compared thiopurines and anti-TNF therapy [48, 50, 56], and three studies compared one of both therapies (either anti-TNF or thiopurines) with placebo or mesalamine [52, 116, 117]. In the total population, a superior effect was demonstrated for anti-TNF agents compared with thiopurine for the prevention of endoscopic POR (relative risk, 0.52; 95% CI, 0.33–0.80) and also clinical POR (relative risk, 0.50; 95% CI, 0.26–0.96). The advantage of anti-TNF agents as compared with thiopurines was observed both in the low- and high-risk groups (i.e., in those patients previously exposed to anti-TNF agents and/or with penetrating disease behaviour).
Finally, when choosing between thiopurines and anti-TNF agents for the prevention of POR, not only efficacy results but also additional factors should be considered. Thus, thiopurines have evident advantages over anti-TNF agents with regard to costs and oral administration route [56]. On the contrary, a major limitation of thiopurines is their balance between safety and efficacy relative to TNF antagonists [56].
In summary, although only few RCTs have directly compared the efficacy of thiopurines and anti-TNF agents in the postoperative setting, with somewhat controversial results, the superiority of anti-TNF over thiopurines, even in low-risk patients, is supported by several meta-analyses (including network meta-analyses and an individual participant data meta-analysis).
3.3 Indications for Anti-TNF Agents in the Prevention of POR
Prophylactic medication for prevention of POR in CD is preferably tailored on individual risk stratification, followed by endoscopy at six months to decide potential treatment escalation [29, 33, 34]. Several risk factors have been identified that enable stratification of individuals at high or low risk for POR after resection surgery. These factors are often divided into patient-related, disease-related, and surgery-related risk factors [14]. Smoking has been consistently identified as the main patient-related risk factor for POR [118]. However, evidence is inconclusive for other patient-related factors such as age, sex, and age at disease onset, whereas genetic factors have not been well studied [14]. With respect to disease-related factors, those include duration of CD prior to first surgery, history of previous CD surgery, extent of gastrointestinal tract involvement, the presence of perianal disease, and complications of CD including penetrating, fistulising, and stricturing CD [10, 13, 14, 29, 33, 34, 50, 119].
It should be highlighted that, although identifying patients who are at higher risk for POR is considered paramount in managing postoperative CD, there is no validated score based on clinical features capable of predicting these outcomes. In fact, risk factors for POR have never been prospectively validated and guidelines differ in the definition of a patient at high risk for recurrence, with the British Society of Gastroenterology requiring the presence of at least two risk factors [34], whilst the AGA and the ECCO mandate the presence of a single risk factor [29, 33]. According to the ECCO, the following are considered predictors of early POR after ileocolonic resection: smoking, prior intestinal surgery, penetrating disease at index surgery, perianal location, granulomas in resection specimen, and myenteric plexitis [29]. Of these, the three most frequently considered in the literature are smoking, prior surgery, and penetrating disease [92], which seem a sensible choice. As previously noted, the main patient-related risk factor is smoking [118]. In addition, a history of previous bowel resection seems to justify the indication of preventive postoperative therapy, given the greater risk of short bowel syndrome if POR occurs [120]. Finally, it also seems reasonable that the presence of fistulising disease, the most severe CD phenotype, constitutes an indication for preventive treatment. From another perspective, except for CD patients with a short resection indicated for fibrotic small bowel stenosis and with no previous resections, preventive treatment (with thiopurines or anti-TNF agents) should be started after surgery [2, 120].
The landmark POCER trial stratified individuals after resection surgery into low or high risk of POR by categorising individuals who smoked, had perforating disease, or had history of at least one previous resection as high-risk (and therefore candidates for postoperative preventive treatment), while those who did not have these risk factors were deemed at low risk [115]. The POCER trial suggested that a treat-to-target strategy (with ileocolonoscopy at six months and treatment step-up if POR was detected) was superior to a symptoms-driven approach in patients at high risk of recurrence, irrespective of the initiation of the prescribed immune-prophylaxis immediately after surgery. If there is endoscopic POR upon the 6- to 12-month ileocolonoscopy, medical therapy should be modified or intensified [121]. Patients receiving thiopurines can be switched to an anti-TNF agent or an anti-TNF agent can be added to their regimen. Patients who are already taking anti-TNF can be switched to another anti-TNF agent or to another biological agent.
However, although prophylactic immunosuppression after surgery in CD patients with several POR risk factors seems appropriate, data are missing about the proper approach for patients with only one risk factor for POR. Immunosuppressive/biological medications are not free of side effects and some still present a non-negligible cost for health care systems. Some observations favour step-up treatment guided by early endoscopic evaluation with prophylactic treatment reserved for carefully selected high-risk patients, in order to avoid potential overtreatment of a significant number of patients [122]. In this respect, in a very recent study, CD patients with only one risk factor for POR (including previous intestinal resection, extensive small intestine resection, fistulising phenotype, history of perianal disease, and active smoking), were retrospectively included [123]. Two groups were formed based on whether immunosuppression was started immediately after surgery (“prophylaxis group”) or guided by endoscopy (“endoscopy-driven group”). No differences between the immune-prophylaxis and the endoscopy-driven approach were found regarding any endoscopic POR, although a statistical beta error cannot be excluded due to the small sample size of the study. The authors concluded, nevertheless, that, in operated CD patients with only one risk factor for POR, immediate immune-prophylaxis does not decrease the rate of early clinical and endoscopic POR [123].
Summarising, the majority of CD patients who currently undergo surgery in clinical practice are at a high risk of POR [50, 115, 124, 125]. Therefore, prophylactic treatment with either thiopurines or anti-TNFs is recommended by current guidelines in the presence of at least one of the abovementioned clinical risk factors. The key question then is to decide whether to choose thiopurines or anti-TNFs as first-line in these patients. Both alternatives are considered valid by European and American guidelines [29, 33]. Traditionally, it has been considered that patients should begin with azathioprine/mercaptopurine, and reserve anti-TNFs for cases of intolerance or failure of thiopurines. However, the relatively low efficacy of thiopurines and the greater efficacy of anti-TNF treatment in this scenario (see above) raise the possibility that these latter agents may be the treatment of choice for any patient with at least one risk factor. Furthermore, most patients requiring surgery have previously failed treatment with thiopurines and/or biologics, so the anti-TNF option seems even more appropriate. Taking all together, it seems that indication of thiopurines could be restricted to exceptional cases.
3.4 Infliximab Versus Adalimumab in the Prevention of POR
The benefit on preventing POR appears to be class specific since adalimumab has shown similar efficacy results to infliximab. The rate of endoscopic POR in the studies evaluating the efficacy of infliximab in particular, calculated from a total of 429 patients from studies included in Table 1, is 24% (95% CI, 20–28%). The respective figure for adalimumab (378 patients) is very similar, 28% (95% CI, 23–32%). Furthermore, some studies have evaluated, in the same protocol, the POR with both infliximab and adalimumab, without finding statistically significant differences [49, 51, 53, 62, 64].
In the first and only randomised study comparing infliximab and adalimumab, Tursi et al assessed POR after one year of treatment with both anti-TNFs as postoperative prophylaxis in 20 CD patients with a high risk of recurrence [49]. Among the ten patients treated with infliximab, two (20%) had endoscopic POR compared to one (10%) in the group of ten adalimumab patients (a non-statistically significant difference, although the sample size of the study may be relatively small to assess statistical significance). Finally, several meta-analyses (including some network meta-analyses) have confirmed similar efficacy of both anti-TNF agents for the prevention of POR [12, 101, 106,107,108].
In summary, infliximab and adalimumab seem to be equally effective in the prevention of POR in CD patients.
3.5 Anti-TNF Combination Therapy (Plus Thiopurines) Versus Monotherapy in the Prevention of POR
Administration of thiopurines increases infliximab levels, reduces immunogenicity, and increases efficacy of infliximab in non-operated patients with CD [126] and ulcerative colitis [127]. In the postoperative scenario, some retrospective cohort studies have compared the efficacy of infliximab monotherapy and combination treatment with thiopurines in preventing POR after surgery and have demonstrated that the use of concomitant thiopurine was correlated with the continuation of infliximab treatment [77]. More recently, the endoscopic POR rate after treatment with thiopurines, infliximab, and the combination of both has been reported to be 34%, 20%, and 0%, respectively, confirming that combination treatment is superior to monotherapy for preventing POR [125]. In this respect, in the PREVENT trial, anti-drug antibodies were detected in 16% of patients, all receiving infliximab monotherapy [52].
Of note, one recent study has shown that, in patients exposed to anti-TNFs prior to the surgery, combination with anti-TNF and immunosuppressive agents was more effective than anti-TNF monotherapy to prevent endoscopic POR [69]. Thus, combination with anti-TNF and immunosuppressive agents should be considered in patients previously exposed to anti-TNF, particularly in those in whom an immune response to biologics has already occurred [17]. However, in anti-TNF–naïve patients, no difference was found in POR rates between patients with or without concomitant immunosuppressive therapy, in agreement with other reports [64]. Therefore, the use of combination therapy could be supported by the higher risk of immunogenicity in patients previously exposed to at least one anti-TNF [128].
In summary, combination with anti-TNF and immunosuppressive agents should be considered in patients previously exposed to anti-TNF, particularly in those with previous loss of response to these agents.
3.6 Timing of Anti-TNF Initiation—for the Prevention of POR—After Surgical Resection
Timing of anti-TNF initiation after intestinal resection (top-down vs step-up) has not been established. The potential risks of step-up management (not initiating anti-TNF immediately after resection but only if endoscopic POR is confirmed at control colonoscopy several months later) include higher rate of endoscopic POR that cannot be rescued by therapeutic escalation at six months and then leads to higher risk of clinical POR and progression of bowel damage. On the other hand, top-down strategy (prescribing anti-TNF immediately after resection) could over-expose some patients to biologics.
In the study by Buisson et al, the top-down strategy led to a lower rate of endoscopic POR and higher proportion of endoscopic remission at six months compared with the step-up approach [71]. Although the authors did not observe any significant superiority between these two strategies regarding long-term outcomes, sub-group analyses in patients without endoscopic POR at six months demonstrated that top-down management was a better option than step-up approach to prevent clinical POR and progression of bowel damage. It is noteworthy that therapeutic intensification in case of early endoscopic POR at six months did not rescue all the patients, highlighting how preventing this early reoccurrence of endoscopic lesion is a key point in the management of CD postoperative period. Accordingly, the authors concluded that top-down strategy should be the preferred management to prevent short- and long-term POR and is recommended to treat all the patients with anti-TNFs after surgery except those without any of the established risk factors.
In cases with anti-TNF treatment initiation after surgery (top-down strategy), some authors have compared the precise starting time—early versus late—of the biologic for preventing POR after ileocecal resection [72]. After adjusting for factors associated with POR, compared with no anti-TNF prophylaxis, the initiation of an anti-TNF agent within four weeks following resection was associated with a reduction in POR. Prior studies have suggested that histologic CD activity can commence within a week of faecal continuity restoration [129]. Thus, timely administration of anti-inflammatory (biological) therapies within four weeks of surgery may be critical to halting the progression to endoscopic lesions.
In this respect, some investigators have identified the frequency of delay and risk factors associated with a deferral in the initiation of prophylactic post-surgical anti-TNF therapy in high-risk CD patients [130]. Of note, a substantial number of delays in initiating postoperative prophylactic biological therapy was identified in high-risk patients: approximately 70% had a greater than 4-week delay, and 60% a greater than 8-week delay in post-surgical biological prophylaxis. Care at an inflammatory bowel disease centre was associated with timely therapy. The authors concluded, therefore, that consultation with inflammatory bowel disease-specialised providers should be considered in peri-surgical irritable bowel disease (IBD) care [130], emphasising the importance of multidisciplinary care in the management of CD patients [131].
D’Amico et al investigated the impact of postoperative biological therapy on the incidence of endoscopic POR and long-term outcomes in CD patients [95]. About one-third of patients were treated with biologics at baseline colonoscopy. A higher rate of endoscopic POR was detected in patients without biological therapy at the time of colonoscopy compared with those treated (81% vs 45%). Additionally, a significant difference in the rate of long-term negative outcomes was also detected between the two study arms. Particularly, patients on biological therapy had a lower risk of hospitalisation and surgery compared with those not treated. The authors concluded that operated patients could benefit from early treatment with biological drugs as soon as they have passed the postoperative setting regardless of endoscopic disease recurrence or risk factors.
It seems obvious that further prospective studies are necessary to confirm whether all operated CD patients should be treated with biological agents postoperatively regardless of endoscopic activity and risk factors. In this respect, a Phase 4 RCT, the SOPRANO-CD study (“Prevention of Postoperative Endoscopic Recurrence With Endoscopy driven Versus Systematic Biological Therapy”; NCT05169593), will enrol approximately 300 operated CD patients with at least one risk factor for POR in order to evaluate the rate of endoscopic POR and the need for unscheduled treatment adaptation; a group of patients will be treated with biological agents immediately after surgery, and a second arm will receive endoscopy-driven induction of biological therapy. The results of this study are eagerly awaited.
3.7 Efficacy of Anti-TNF Agents, After Their Pre-surgical Failure, in the Prevention of POR
Anti-TNF therapy is frequently used in the treatment of refractory CD. Unfortunately, primary or secondary treatment failure of anti-TNF treatment is not uncommon [36, 132]. Therefore, in clinical practice, a substantial portion of patients who receive anti-TNF agents after surgery have been exposed to these agents prior to surgery. As the number of patients who do not respond to multiple biologics and require surgery increases, the decision regarding postoperative treatment will become more complex. In this respect, it is not clear whether patients who undergo intestinal resection after anti-TNF failure would benefit from reinstitution of anti-TNF therapy to prevent POR, as only a few studies have evaluated the effectiveness in this scenario [13, 69].
Some studies have reported that anti-TNF agents are less effective for the prevention of POR in patients with previous exposure to anti-TNFs, compared with those naïve to these agents [55, 59, 62, 69, 111]. This may be simply due to a primary pharmacodynamic failure to anti-TNF agents, suggesting that a reasonable approach to prevent POR would be choosing a biologic with an alternative mechanism of action (non-TNF related) in those who had failed an anti-TNF agent [17].
Supporting this idea, Collins et al showed that previous exposure to two or more anti-TNF agents was a risk factor for CD endoscopic POR [55]. In the study by Hiraoka et al, CD patients who underwent intestinal resection and received anti-TNF agents after surgery were divided into two groups according to the presence or absence of preoperative anti-TNF treatment; endoscopic POR was more frequently observed in the anti-TNF restart group than in the anti-TNF–naïve group (68% vs 14%), concluding that a change to different classes of biologics should be considered for those patients [62]. More recently, Shinagawa et al evaluated patients with CD who underwent intestinal resection before and after anti-TNF therapy was introduced in Japan (in 2002) [111]. After stratifying patients by anti-TNF exposure prior to surgery, the postoperative administration of anti-TNF was found to be effective in the biologic-naïve group, but not in the group that failed anti-TNF therapy before operation. However, it should be stressed that the aforementioned studies have some relevant limitations. First, they have a retrospective design. Second, the timing of endoscopic follow-up after surgery differed between patients. Last, anti-drug antibodies, which may be one of the reasons of the ineffectiveness of postoperative anti-TNF treatment, were not measured.
The lower efficacy of restarting anti-TNF agents after surgery in the aforementioned studies raises the question about whether dose optimisation (intensification) of treatment post-surgery could increase the efficacy of postoperative anti-TNF treatment. In the study by Hiraoka et al, half of the patients who showed endoscopic POR after surgery did indeed respond to intensification of treatment, although endoscopic remission was not obtained in most of the patients and some required additional surgery [62]. In fact, treatment intensification for patients with endoscopic POR in the anti-TNF restart group showed limited responses, with less than 10% of patients achieving endoscopic remission.
However, other investigators have reached opposite conclusions, that is, that anti-TNF remains an effective option to prevent POR for patients operated upon with previous anti-TNF failure. In other words, they suggest that, for patients with CD who receive anti-TNF agents preoperatively, continuing their use after surgery could be recommended. Sakuraba et al showed that the rate of maintained remission in the post-operative setting was similar between those who were naïve to infliximab therapy and those who continued on this treatment after surgery [77]. Likewise, in the study by de Barcelos et al, preoperative therapy with infliximab or adalimumab did not affect the incidence of endoscopic POR [84]. Similarly, a recent prospective study evaluating risk factors for POR, failed to find any effect of prior anti-TNF exposure on efficacy [61]. More recently, Cañete et al observed no relationship between previous exposure to anti-TNFs and success at preventing POR [64]. In the study by Beelen et al, the advantage of anti-TNF agents as compared with thiopurines was observed not only in low- but also in high-risk patients, i.e., in those previously exposed to anti-TNF agents [110]. Finally, Yu et al [70] reviewed patients who had undergone the first intestinal resection due to CD and divided them into two groups: TNF inhibitor users in both the preoperative and postoperative periods, and TNF inhibitor users only in the preoperative period; the rates of surgical and endoscopic POR were not different between either group.
As the presence of intestinal complications is known to be one of the risk factors of the lower efficacy of anti-TNF agents, the requirement for surgery early after initiation of anti-TNF treatment may not indicate primary ineffectiveness of the agent but insufficient effectiveness owing to the presence of intestinal complications, thereby explaining the favourable results in the post-operative scenario despite previous anti-TNF failure [133]. Therefore, in these patients, removal of intestinal complications by surgery might “reconstitute” the efficacy of anti-TNF agents. Others have tried to explain it by arguing that anti-TNF treatment shortly after surgery, when there are still no signs of active disease, could interfere with the initial pathogenic mechanisms of tissue damage, changing the natural evolution of the disease. Based on these results, some authors have suggested maintaining the anti-TNF treatment if these agents were used preoperatively, and then performing early screening to evaluate and adjust medications. This strategy might spare further possible biological treatment options in the future.
Nevertheless, the main limitation of the previously reviewed studies is that a control group, treated with a different biological agent than an anti-TNF, was not included. Preoperative anti-TNF therapy requirement might simply be a surrogate marker of a more severe, refractory disease (to any treatment) before surgery, therefore not necessarily implying a worse response when readministering anti-TNF treatment (compared with other alternatives, such as a non–anti-TNF biological agent). In fact, both vedolizumab and ustekinumab have generally been shown to also be less effective in anti-TNF exposed patients [36]. Unfortunately, the two main strategies used to treat a patient with primary non-response to an anti-TNF agent—switching to a second anti-TNF or swapping to vedolizumab/ustekinumab—have not been properly compared [36].
Recently, some studies have compared the efficacy of anti-TNF with that of other biologics to prevent POR. Yanai et al reported that continuation of anti-TNF treatment after surgery resulted in a similar rate of endoscopic POR as swapping to a different mechanism of action [67]. On the other hand, Le Cosquer et al included CD patients who underwent bowel resection after failure of at least one anti-TNF treatment [68]. Among the 119 patients included, 71 received an anti-TNF (26 infliximab, 45 adalimumab) and 25 another biologics (18 ustekinumab, 7 vedolizumab) to prevent POR. Rates of POR at two years were lower (24%) in patients treated with anti-TNFs than in the others (45%).
In summary, although some studies have reported that anti-TNF agents are less effective for the prevention of POR in patients with previous exposure to anti-TNFs (compared with those naïve to these agents), several other investigations have shown that anti-TNF treatment remains an effective option to prevent POR also in patients operated upon with previous anti-TNF failure, suggesting that the previous failure to these agents does not necessarily imply that a drug with another mechanism of action (such as vedolizumab or ustekinumab) should be prescribed.
3.8 After One Anti-TNF Failure Before Surgery, Is It Better to Readminister the Same Anti-TNF Agent or to Switch to a Different Anti-TNF to Prevent POR?
When dealing with POR, both patients and treating physicians can face the dilemma of choosing between the same anti-TNF agent or switching to a different anti-TNF agent. Theoretically, it seems reasonable to think that once a first anti-TNF agent has failed preoperatively, the chances of response after prescribing the same anti-TNF should be lower. A pharmacokinetic mechanism could explain the failure when prescribing the same anti-TNF after surgery. Thus, it is known that most cases with a secondary loss of response are associated with the development of anti-drug antibodies [134]. The anti-drug antibodies developed prior to surgery to a specific anti-TNF agent probably also work against the same anti-TNF after surgery. Therefore, those who initially responded to anti-TNF agents but subsequently lost the response (and required surgery) are, theoretically, expected to develop POR despite administering the same anti-TNF treatment postoperatively [135].
However, some studies have suggested the opposite, i.e., that the consistent use of the same anti-TNF agent before and after the surgery may be effective in the prevention of POR. In a clinical trial evaluating the prophylaxis of POR, three patients used the same anti-TNF (infliximab) before and after surgery and none had clinical POR one year after surgery [39]. In another study, the efficacy of the consistent versus switched anti-TNF approaches in patients with (already) recurrent CD after ileocolonic resection was compared [79]. During the median follow-up of 1.5 years, 17% of patients in the consistent group and a similar figure (19%) in the switched group required the repeat resection of ileocolonic anastomosis. Nevertheless, this last study was observational, retrospective, had a small sample size, and serum drug levels and antibody concentrations were not routinely measured. In any case, these results support the speculation that bowel resection surgery may change the body’s “immune thermostat”, resulting in a renewed ability to respond to (the same) medical therapy [79].
In summary, although theoretically, it might be thought that once a first anti-TNF agent has failed preoperatively, a different anti-TNF agent should be prescribed, some studies have suggested that the consistent use of the same anti-TNF agent before and after the surgery may be effective in the prevention of postoperative POR, and therefore could be considered a valid option.
3.9 Anti-TNF Regimen (Dose and Induction) in the Prevention of POR
In theory, low-dose infliximab–treated patients could develop sub-therapeutic trough levels, and anti-infliximab antibodies, and might lose response to therapy. To verify this hypothesis in the post-operative setting, infliximab pharmacokinetics and clinical/endoscopic response were checked in a group of five patients in endoscopic remission after one year of therapy with infliximab 3 mg/kg [96]. In these low-dose–treated patients, after 18 additional months of therapy, endoscopy continued to show mucosal remission and no patients developed clinical POR, despite having lower trough levels compared to those treated with 5 mg/kg. Obviously, due to the very small sample size of this study, these results should be considered with caution, and standard doses of anti-TNF should be used for the time being. Finally, it is unknown whether the usual initial induction regimen (e.g., infliximab at 0, 2 and 6 weeks) should be used when starting an anti-TNF in the post-operative setting to prevent POR [39], since some authors have administered from the beginning infliximab at 8-week intervals without any initial induction dose [41].
3.10 Therapeutic Drug Monitoring and POR
Higher concentrations of anti-TNF drugs are associated with better outcomes, including clinical remission and mucosal healing, in patients with active luminal CD [136]. Similarly, some studies have found that higher serum drug concentrations of anti-TNFs are associated with reduced rates of POR after ileocolonic resection [58, 97, 137,138,139]. As a paradigmatic example, the PREVENT trial evaluated almost 300 patients who had an ileocolonic resection for CD and received either infliximab or placebo [52]. Inverse correlation between serum infliximab concentrations and POR rates was found (i.e., the higher the concentration, the lower the rates of POR). In detail, pharmacokinetic data from the PREVENT trial showed that higher infliximab drug concentration quintiles were associated with lower endoscopic POR rates, and the lowest POR rates were in the highest quintile (> 7.7 μg/mL). The lack of a clear plateau suggests that the optimal drug concentration required to prevent POR may not yet be clearly delineated. Of patients with adequate drug concentrations (≥ 4.2 μg/mL), 20% had endoscopic POR compared with 36% with inadequate drug concentrations [52]. This could provide a rationale for the use of proactive drug monitoring in the postoperative setting in order to improve long-term outcomes.
Similarly, a recent systematic review, including studies which assessed infliximab concentrations and endoscopic POR in CD, confirmed higher concentrations mostly associated with lower POR rates [140]. However, this meta-analysis has important methodological limitations: only four studies were included, with low or moderate methodological quality, and several problems such as non-blinding as well as a restricted and often heterogeneous population sample; furthermore, the interval between dosage of infliximab serum levels and colonoscopy also varied in different studies. Taken together, these issues limit the evaluation of results, which therefore should be interpreted with caution [140].
Other studies have shown opposite results. A sub-analysis from the POCER trial, including 52 patients with serum concentrations of adalimumab measured after ileocolic resection, showed that patients in endoscopic remission had similar adalimumab concentrations compared to those with POR [141]. Also, there were no statistically significant differences when adalimumab concentrations were compared between each different Rutgeerts’ score category (i0 to i4) [141]. In another study, patients were treated with low-dose infliximab (3 mg/kg) postoperatively to prevent endoscopic POR, and all patients remained in clinical and endoscopic remission for an average of 18 months following surgery, despite sub-therapeutic infliximab drug concentrations (mean 2.0 μg/mL) [96]. In the study by Fay et al, although lower infliximab trough concentrations were associated with endoscopic POR, this same association was not observed for adalimumab-treated patients [58]. Moreover, despite the significant difference between groups with or without POR in some studies previously mentioned, low infliximab concentrations were still observed in many patients without POR, supporting the hypothesis that the actual threshold in the postoperative scenario can be somewhat different than in non-operated luminal CD: in addition, it is possible that relatively low infliximab levels are sufficient to control anastomotic inflammation. Anyway, it has been suggested that, in patients who have had resection of all gross disease and are started on anti-TNF prophylaxis in a timely manner, the role of therapeutic drug monitoring may be more limited due to the lack of drug clearance from inflammatory burden consumption [16].
In summary, the role of therapeutic drug monitoring in the prevention of POR is unclear (as it is also unclear the cut-off point to define high/low trough levels, which could be slightly different than in luminal disease), and RCTs with adequate methodological quality are warranted to clarify this topic.
3.11 Can Anti-TNF Treatment Ever be Stopped When Prescribed for the Prevention of POR?
A clinically relevant question is whether, after having prescribed anti-TNF for prevention of POR, stopping anti-TNF treatment after some time (e.g. one year) post-surgery in patients in clinical and endoscopic remission leads to recurrence [142,143,144].
In their pioneer study, Regueiro et al randomly assigned 24 patients with CD who had undergone ileocolonic resection to receive infliximab or placebo for one year and demonstrated that infliximab prevented endoscopic POR [39]. At the end of the trial, 11 patients were offered open-label continuation of infliximab; eight of the 11 patients elected to stop the drug and all eight patients had endoscopic POR at one year, and more than 60% (5 of 8) had to undergo another surgery within 5 years, despite restarting immunosuppressive therapy; while three patients of the previous infliximab arm decided to continue with infliximab and remained well without signs of endoscopic or clinical relapse.
In another study, 12 patients who started infliximab after surgery were still free of clinical and endoscopic POR of CD three years later [40]; however, discontinuation of infliximab led to endoscopic POR after four months in 10 of 12 patients (83%). Fortunately, remission was achieved after re-treating all 10 patients with infliximab.
Finally, in a recent postoperative study, nearly three-quarters of the infliximab patients stopped treatment at one year after resection while in complete endoscopic remission; all of these patients subsequently experienced endoscopic POR and most required additional surgery [145]. Twelve patients with endoscopic POR, all of whom were treated for 12 months with placebo in the context of the initial randomised postoperative prevention trial, were initiated on anti-TNF therapy; 7 of 12 patients (58%) achieved endoscopic and clinical remission after reinitiating anti-TNF therapy, whereas 5 of 12 (42%) ultimately needed another surgical resection [145].
In summary, CD POR shortly after discontinuing anti-TNF therapy indicates a lack of long-term effects or reversal of the pathophysiological mechanisms of CD. Consequently, patients with a high risk for POR (those where an anti-TNF has been prescribed) need some form of long-term immunosuppressive therapy to prevent relapse of disease thereby probably benefiting from long-term anti-TNF maintenance.
3.12 Cost Effectiveness of Anti-TNF Treatment to Prevent POR
A decision analysis model examining the cost effectiveness of the various strategies to identify the appropriateness of therapies for patients in differing risk strata could serve an important role in informing clinical practice and decision making.
In 2011, Ananthakrishnan et al developed the first analytic decision model in the postoperative setting, comprising five strategies: no treatment, azathioprine, antibiotics, upfront infliximab, and tailored infliximab (which consisted of no upfront therapy with initiation of this agent only in patients with severe endoscopic POR at six months) [146]. Upfront infliximab was the most efficacious strategy but was not cost effective. Reserving infliximab use for high-risk patients with early endoscopic POR was more cost effective than upfront use in all patients. However, there were no trial data on the efficacy of infliximab in preventing POR beyond one year to inform such a model. Thus, it is possible that over a longer follow-up period, the upfront infliximab arm may accrue more health benefits, rendering it cost effective. Furthermore, it should be considered that this study was published in 2001, when anti-TNF biosimilars (much cheaper) were not available.
One year later, in 2012, Doherty et al published a cost-effectiveness analysis reporting that thiopurine drugs had the most favourable incremental cost-effectiveness ratio (ICER) in the prevention of clinical POR up to one-year post-surgery [147]. Infliximab yielded marginally higher quality-adjusted life years (QALYs) compared to all strategies.
More recently, in 2017, Candia et al assessed whether postoperative management should be based on biological therapy alone or combined with thiopurines, and whether the therapy should be started immediately after surgery or guided by either endoscopic or clinical POR [148]. A Markov model was developed to estimate expected health outcomes in QALYs and costs (in Canadian dollars) accrued by hypothetical patients with high recurrence risk after ileocolic resection. According to this decision analysis, thiopurines immediately after surgery and addition of anti-TNF agents guided by endoscopic POR was the optimal strategy of post-operative management in patients with CD; however, the high cost of administering biologics to all patients rendered it not cost effective in the vast majority of scenarios.
A relevant limitation of all aforementioned studies is that the main analysis did not take into consideration the expiration of patent protection of biologics and the general introduction of biosimilar drugs. In this respect, considering that the main advantage of biosimilars is their cost, some authors have conducted a re-analysis of the data addressing this point. If biosimilar drugs had the same effect as biologics and their cost were lower than 44% of the current cost (estimated in 2017), the optimal strategy would be combination therapy with anti-TNF and thiopurines agents immediately post-surgery [148].
In summary, the cost effectiveness of anti-TNF treatment to prevent POR is still unclear, mainly because the profile of patients to whom they should be administered has not been definitively established and because the studies were carried out at a time when biosimilars were not available.
3.13 Efficacy of Anti-TNF Agents for the Treatment (Not for the Prevention) of POR
Approximately 50% of patients without primary prevention of POR will need rescue therapy within the first year after surgery [120]. Furthermore, even in patients who start thiopurines early after surgery, endoscopic POR occurs in up to 40% within one year [120].
Mesalamine has demonstrated a very limited efficacy for the treatment of POR [120]. Thiopurines, although useful, are hampered by a high rate of intolerance and their slow mechanism of action, and thus they may not be the most suitable option in patients with already existing clinical POR. Therefore, biological agents seem to be the best potential choice in this clinical scenario.
However, in contrast to relatively abundant data on anti-TNF agents for the prevention of POR, data regarding treatment of POR with anti-TNF therapy are scarce [43, 145, 149,150,151,152] as summarised below.
Yamamoto et al showed, as early as in 2009, that 75% of patients starting infliximab six months after surgery for endoscopic POR improved endoscopic inflammation compared with 38% of azathioprine- and 0% of mesalamine-treated patients [149]. Furthermore, complete mucosal healing was achieved in 38% of patients on infliximab when compared with 13% of those receiving azathioprine and 0% of mesalamine-treated patients. Accordingly, the mucosal interleukin (IL)-1β, IL-6, and TNF levels significantly decreased in the infliximab group, while they increased in the mesalamine group, and did not change in the azathioprine group.
In 2012, Papamichael et al reported results from a cohort of 15 CD patients with endoscopic POR six months after surgery and consecutive treatment with adalimumab [43]. After 24 months of therapy, 60% of patients were in endoscopic remission, although 27% experienced clinical POR and 13% needed surgery. In the study by Sorrentino et al, 69% of CD patients had endoscopic improvement and 54% had complete mucosal healing after receiving infliximab for six-month POR [150].
More recently, a multicentre, retrospective study of patients with CD who underwent therapy with anti-TNF agents for endoscopic POR (Rutgeerts’ score > i1) was published by Cañete et al [152]. A total of 179 patients were included: 83 were treated with infliximab and 96 with adalimumab. Endoscopic improvement was observed in 61%, including 42% who achieved endoscopic remission (Rutgeerts’ score < i2). Concomitant use of thiopurines and treatment with infliximab (vs adalimumab) were associated with endoscopic improvement and remission; these results were confirmed in a propensity-matched score analysis.
It is not known whether initiating anti-TNF treatment immediately after surgery prevents future CD complications and surgery more effectively than waiting to treat endoscopic POR. In the study by Regueiro et al, all patients who initiated infliximab within four weeks of surgery and continued long-term treatment avoided additional surgery [145]. In contrast, 58% of the initially placebo-treated patients who started infliximab in response to one-year endoscopic POR had improvement in endoscopic inflammation, but nearly one-half required additional surgery. The authors also found that patients with less severe endoscopic POR responded better to the initiation of infliximab. Thus, in patients with a Rutgeerts’ score of i2 endoscopic remission was induced, whereas no i4 patients and only two of the i3 patients had endoscopic improvement. Furthermore, all patients with i4 scores and half of the i3 patients required another surgery despite initiation of infliximab [145].
The influence of the moment at which treatment with anti-TNFs is started on its efficacy is also not well known. An attractive explanation for the apparently weaker efficacy of anti-TNFs when given later after surgery could be related to the actual mechanism of action of TNF. Recent data suggest that this cytokine may control the fine balance between T regulatory (Treg) cells and T helper 17 (Th17) effector cells, which in turn may critically regulate mucosal repair and destruction [150]. Thus, blockade of TNF immediately after surgery could afford a favourable Treg/Th17 ratio and block inflammation altogether. However, anti-TNF treatment would be less effective once a renewed immune reaction and florid inflammation have been induced after surgery [150].
Finally, the efficacy of anti-TNF treatment in patients with POR and associated complications, typically stenosing phenotype, is unknown. In the study by Freeman et al, anti-TNF treatment was used in three gastrointestinal partial obstruction cases: two with complete relief and one with partial response [151].
In summary, it seems that anti-TNF agents are effective not only for the prevention but also for the treatment of established POR. Whether treating already established endoscopic POR would approach the consistently high endoscopic remission rate seen in the studies initiating anti-TNF treatment within one month of surgery (that is, as prophylaxis of POR) is still unknown, although the aforementioned efficacy figures reached in treatment studies seem to be somewhat lower.
3.14 Efficacy of Anti-TNF Agents, After Their Pre-surgical Failure, in the Treatment of POR
It could be speculated that, when a previous anti-TNF treatment has failed before surgery, these same agents would be less effective to treat POR after surgery. Although most studies assessing the efficacy of anti-TNF agents to treat POR have included a low percentage of patients who failed anti-TNF preoperatively [149, 150, 152], this does not seem to be the case, as a beneficial effect of anti-TNF therapy for POR has been demonstrated in more than 50% of the patients. Assa et al reported on 53 patients with CD who underwent intestinal resection and were treated with anti-TNF agents postoperatively [153]. Patients were stratified to those with preoperative anti-TNF pharmacodynamic failure (i.e., despite adequate drug levels) and those with no preoperative anti-TNF treatment. Unexpectedly, no significant differences were observed at 14 weeks and 12 months of postoperative anti-TNF treatment, including endoscopic remission rate: mucosal healing was observed in 50% for pharmacodynamic failure, and in 45% in controls. Similarly, in the study by Cañete et al previously mentioned, exposure to anti-TNF agents before the index surgery was not associated with a lower efficacy of anti-TNF therapy once POR occurred [152].
More recently, a real-world cohort study was performed on 66 CD patients who underwent ileocecal resection after anti-TNF therapy failure (it should be emphasised that all patients had received these agents preoperatively), and who were retreated with anti-TNF therapy for symptomatic POR [154]. A strength of this study is that it included detailed sub-analyses, depending on the nature of preoperative anti-TNF failure (primary non-response, secondary loss of response, intolerance), retreatment with the same versus different anti-TNF agent, and preoperative exposure to one versus more than one anti-TNF agents. Remarkably, no differences in treatment failure were found with regard to the nature of preoperative anti-TNF failure, switch of anti-TNF agent, and number of preoperative anti-TNF agents.
The fact that the retreatment with anti-TNF therapy is an effective strategy for POR might be explained by the definition of preoperative failure. Some patients might have symptoms due to fibro-stenotic structure or too severe lesions to benefit (before surgery) from medical treatment. After surgery and removal of most severe (or fibro-stenotic) lesions, those patients might respond to anti-TNF [68]. On the other hand, the extreme burden of tissue TNF within severely inflamed tissue in the pre-surgical setting may result in failure of anti-TNF antibodies to neutralise local TNF production [155]. A recent study has shown that response to anti-TNF therapy is associated with the number of TNF expressing cells in the mucosa [156]. In an interesting study, Yarur et al demonstrated that in moderate-to-severely inflamed tissue from adult patients with IBD, the anti-TNF to TNF ratio was lower, implying that there was insufficient drug to neutralise TNF [155]. Moreover, severely inflamed tissue had a lower drug level compared with samples with mild-to-moderate inflammation, resulting in high serum-to-tissue anti-TNF ratio. A plausible explanation for this finding is that in severely inflamed tissue with high inflammatory burden, local high levels of TNF serve as a sink for anti-TNF antibodies, and that tissue injury and local hypoxia might further limit drug penetrance to its target [153]. In this case, intestinal resection of the severely inflamed segment may restore efficacy of traditional biological therapy such as anti-TNF agents. Although retreatment with anti-TNF therapy may be an effective strategy for POR, it has been shown that treatment of established mucosal lesions appears less effective when compared with earlier, preventive strategies [150, 157]. In this respect, recent studies indicate that Treg differentiation and function may play a significant role in the pathogenesis of CD [158]. Thus, it is possible that, by restoring Treg function/number, infliximab could prevent POR. However, infliximab could be less effective in restoring mucosal integrity when a local inflammatory response has already started and spread in the intestinal mucosa [158, 159]. Furthermore, a potential delay in the initiation of anti-TNF treatment may result in a lower response rate in established lesions compared with upfront use before the development of significant POR. In a follow-up to their trial, Regueiro et al found a higher rate of clinical POR in patients started on infliximab at one year after surgery compared with those who used infliximab from the immediate postoperative period [39].
Finally, some studies have shown that treatment is more effective in patients receiving anti-TNF in combination with an immunomodulator compared to patients receiving infliximab/adalimumab monotherapy [154]. This observation is in line with previous data, which suggest that immunomodulators may need to be started or continued in IBD patients upon initiation of anti-TNF therapy, based on the presumption that immunosuppressive therapy is expected to substantially improve efficacy, increase serum drug concentrations, and reduce immunogenicity [126, 127, 154].
In summary, retreatment with anti-TNF therapy for POR is a valid strategy even after preoperative failure. However, this biological treatment will probably be less effective when mucosal lesions are already present (compared with preventive strategies).
4 Biological Agents Other Than Anti-TNFs
In recent years, there has been greater use and interest in newer biologics, e.g., vedolizumab and ustekinumab, to prevent POR. A survey study of gastroenterologists attending the 2019 ECCO congress found that 62% and 56% of gastroenterologists with access to vedolizumab and ustekinumab, respectively, would prescribe these drugs in the postoperative setting [113]. The authors of this report noted that this was an “unexpectedly high” percentage of physicians who would already consider these biologics as reliable treatment despite little published data [113]. Generally, these newer biologics are reserved for patients who have failed anti-TNF agents or are contraindicated to them [14, 160].
4.1 Vedolizumab
Vedolizumab is a selective humanised immunoglobulin G1 monoclonal antibody to α4β7 integrin that blocks lymphocyte trafficking to gut mucosa [161, 162]. Both RCTs and observational studies have shown the efficacy of vedolizumab to induce clinical and endoscopic remission in patients who were naïve to, and who previously failed anti-TNF agents [163, 164]. Vedolizumab is increasingly used as postoperative prophylactic treatment for CD patients, especially in those at high risk for POR [63].
It has been suggested that the use of vedolizumab in the postoperative setting could have an underlying pathophysiological rationale: the presence of submucosal lymphocytic plexitis in the proximal surgical margin has been associated with higher risk for POR after ileocolonic resection [165]. Vedolizumab is able to block lymphocytic trafficking among myenteric and submucosal plexus, including those of the perioperative bowel, in a context where the inflammatory burden has been markedly reduced by surgery.
The efficacy of vedolizumab to prevent endoscopic POR is summarised in Table 3 [63, 67, 68, 72, 166,167,168]. In total, 6 studies were identified, including 156 patients—all were observational studies. From data included in Table 3, the mean endoscopic POR at 6–12 months was 41% (95% CI from 33 to 49%).
In 2018, Yamada et al compared the risk of POR between patients receiving vedolizumab and anti-TNF agents in the postoperative setting [63]. Based on propensity score-matched, patients treated with vedolizumab had a higher rate of endoscopic POR than those treated with anti-TNF agents (25% vs 66%). In fact, vedolizumab use was the only factor independently associated with an increased risk of endoscopic POR in the multivariate analysis.
More recently, Yanai et al compared anti-TNF therapy (224 patients) to vedolizumab (39 patients) and ustekinumab (34 patients) to prevent POR in a real-world setting [67]. As expected, patients treated with vedolizumab and ustekinumab were more biologic experienced, with higher rates of previous surgery. Endoscopic POR rates by treatment groups were 40% for anti-TNF, 33% for vedolizumab, and 62% for ustekinumab. However, after controlling for confounders with propensity score matching, the risk of endoscopic POR within one year of the three drugs was comparable.
Axelrad et al compared biologic type for preventing POR after ileocecal resection [72]. Prophylaxis with vedolizumab (as with ustekinumab) was not associated with a reduction in POR compared with patients who did not receive prophylaxis, although the sample size of this study was quite limited (27 patients).
Finally, vedolizumab has recently been compared with ustekinumab in the postoperative setting in a multicentre study based on the Spanish ENEIDA registry, showing similar results with both biological agents [166] (this relevant study will be discussed in detail in the next section focused on ustekinumab).
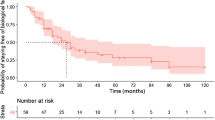
However, the findings from the studies evaluating the efficacy of the new biologics in the prevention of POR, and especially comparing vedolizumab and ustekinumab, should be interpreted with caution for a number of reasons that will be reviewed in the next section. In particular, as there are probably relevant differences in the background characteristics of the patients treated with vedolizumab and anti-TNF agents, further investigation including randomised-controlled trials is required before recommending the use of vedolizumab in preventing CD POR. In this respect, a placebo-controlled RCT, the REPREVIO trial, has just been completed (REPREVIO; EudraCT 2015-000555-24) [167, 168]. In this multicentre study, patients who had an ileocolonic resection and who had at least one risk factor for POR (e.g., active smoking, at least one previous resection, surgery for a perforating complication, or previous exposure to anti-TNFs) were randomly assigned to receive vedolizumab 300 mg (n = 43) or placebo (n = 37) at Weeks 0, 8, 16, and 24 after surgery. Patients underwent ileocolonoscopy six months after surgery. Eighteen patients in the vedolizumab group had a Rutgeerts’ score of i0 (i.e., were in endoscopic remission) at Week 24 versus only one in the placebo group; 3 had a Rutgeerts’ score of i1 (vs 5 in the placebo group), 12 had a Rutgeerts' score of i2a (vs 8), and 7 had a Rutgeerts’ score of i2b (vs 6); of note, no patients in the vedolizumab group had a Rutgeerts’ score of i3 (vs 6 in the placebo), and only 3 had a Rutgeerts' score of i4 (vs 11 in the placebo). In summary, patients in the vedolizumab group had a 78% chance of having a lower Rutgeerts’ score than patients in the placebo group. From this study it can be concluded that starting vedolizumab within 4 weeks of ileocolonic resection is highly effective to reduce both the incidence and the severity of POR in CD patients with increased risk of recurrence.
A recent meta-analysis investigated and compared the efficacy of different biologics for POR prevention [12]. First, vedolizumab prevented endoscopic POR in a similar manner to non-biological treatments. Second, among the various types of biologics, anti-TNF agents were more effective than vedolizumab in preventing endoscopic POR, although only 2 studies with a total of only 100 patients were included in this meta-analysis.
Finally, the efficacy of vedolizumab for the treatment (not for the prevention) of POR has recently been evaluated. Macaluso et al included 58 CD patients with a baseline colonoscopy at 6–12 months from the ileocolonic resection showing endoscopic POR and treated them with vedolizumab [169]. Endoscopic success (defined as reduction of at least one point of Rutgeerts’ score) was reported in 48% of patients. Clinical failure was reported in 19% of patients at one year, and in 33% at the end of follow-up. A new resection was required in 7 patients (12%). Therefore, vedolizumab may be considered as an effective option, not only for the prevention of POR, but also for its treatment.
4.2 Ustekinumab
Ustekinumab, an antagonist of the p40 subunit shared by the IL‐12 and IL‐23, has shown a higher effectiveness than placebo in patients with luminal moderate‐to‐severe CD [170]. Both RCTs and observational studies have demonstrated the efficacy of ustekinumab to induce clinical and endoscopic remission in patients with CD [171, 172]. Thus, this biological agent may also be effective in the prevention of POR.
In a recent multicentre Spanish study evaluating the use of new (non–anti-TNF) biological agents in the postoperative setting, a larger number of patients treated with ustekinumab than with vedolizumab for the prevention of POR was reported, despite the fact that the latter was licensed for CD two years earlier [166]. It has been speculated that this could be because some physicians believe that vedolizumab works less effectively in ileal disease (based on differences in T cell trafficking in the ileum and the colon [173]) or because the supposedly delayed onset of vedolizumab action may prompt the use of ustekinumab instead of vedolizumab for the prevention of POR [166].
The rate of endoscopic POR in the studies evaluating the efficacy of ustekinumab in the postoperative setting is summarised in Table 4 [67, 68, 71, 72, 166, 174, 175]. In total, seven studies, all observational and included 162 patients, were identified. From data included in Table 4, the mean endoscopic POR at 6–12 months was 41% (95% CI 33–49%). This figure was exactly the same as that calculated for vedolizumab (see above, Table 3).
In a French study, ustekinumab was compared to azathioprine using propensity score matching, and was found to be associated with lower rates of recurrence: endoscopic POR (Rutgeerts’ index ≥ i2) at six months was 28% versus 54% [175]. In a US study, Axelrad et al compared biologic type for preventing POR in CD patients after ileocecal resection [72]; prophylaxis with ustekinumab (as with vedolizumab) was not associated with a reduction in POR compared with those patients who did not receive prophylaxis, although the sample size of this study was small (28 patients).
Very recently, ustekinumab has been compared with vedolizumab in the postoperative setting. In the study by Mañosa et al, CD patients in whom one of these two biological agents was prescribed for the prevention of POR within three months of ileocolonic resection were identified in the Spanish ENEIDA registry [166]. Forty patients were treated with ustekinumab and 25 with vedolizumab. Most (80%) had at least one risk factor for POR (prior resections, active smoking, perianal disease, or penetrating disease behaviour), and all the patients had been previously exposed to anti-TNF therapy. The cumulative probability of clinical POR at 12 months after surgery was similar for ustekinumab and for vedolizumab: 32% and 30%, respectively. Endoscopic assessment within the first 18 months after surgery was available for most (70–80%) of the patients, the rate of endoscopic POR was again similar: 42% for ustekinumab and 40% for vedolizumab. Nevertheless, these figures should be taken with caution due to the shorter median follow-up in the ustekinumab group. Finally, one patient treated with ustekinumab and two with vedolizumab underwent a new intestinal resection. Therefore, the authors concluded that ustekinumab and vedolizumab seem to be (equally) effective in the prevention of POR in patients at high risk, with observed endoscopic POR rates close to those previously reported for anti-TNF agents.
Finally, some studies have evaluated the efficacy of ustekinumab for the treatment (not for the prevention) of POR. In the previously mentioned study by Macaluso et al, 44 patients started ustekinumab for the management of POR [176]. Only five patients (11%) were naïve to biologics, while most had previous failure to one (61%), two (16%), or even three (11%) biologics. Endoscopic success (defined as reduction of at least one point of Rutgeerts’ score) was reported in 22 out of 44 (50%) patients, of whom 12 (27%) achieved a Rutgeerts’ score i0 or i1, suggesting that ustekinumab could be a promising option for the treatment of POR of CD.
A recent meta-analysis investigated the efficacy of different biological agents in the postoperative setting and showed that ustekinumab prevented endoscopic POR in a similar manner to non-biological treatments [12]. Subsequently, two studies directly compared the efficacy of ustekinumab to other biologics for the prevention of POR and found that anti-TNF agents performed more efficiently than ustekinumab.
4.3 Limitations of Studies Assessing the Efficacy of Vedolizumab and Ustekinumab in the Prevention of POR
The conclusions from the studies (and also meta-analyses) comparing the efficacy of several biological agents (anti-TNFs vs ustekinumab vs vedolizumab) in the postoperative setting should be taken with caution as these studies have relevant methodological limitations summarised below.
1) Most of the studies are retrospective.
2) No head-to-head RCT has been conducted comparing two biological agents.
3) Sample sizes are generally small.
4) There is a high risk of potential residual confounding despite multivariable modelling (or propensity matched analysis), particularly as individuals receiving a specific biologic could have more severe disease as judged by more patients with multiple prior resections and often second-line therapy to a previous biologic. In this respect, patients receiving vedolizumab or ustekinumab have almost universally been previously treated with biologics, most commonly at least one anti-TNF agent, which may indicate that they had a more medical refractory disease. Unfortunately, no degree of statistical adjustment can fully resolve the potential for residual confounding [13].
5) Some authors have used the Simple Endoscopic Score (SES-CD) rather than the Rutgeerts’ score to define endoscopic POR, to simultaneously assess the degree of inflammation in the ileum and colon; however, unlike the Rutgeerts’ score, SES-CD has not been correlated with a risk of clinical POR.
6) Finally, the majority of the patients have been treated postoperatively without an induction dosing of the biological agent, which may have reduced the effect of all these treatments.
5 Conclusions
Despite multiple advances in the medical treatment of CD, a significant proportion of patients ultimately require surgical resection at some point during their disease course. Unfortunately, surgery is not curative, and POR after ileocolonic resection is very common in the absence of prophylactic treatment. Therefore, the prevention of POR is a high priority. However, until now, traditional drugs have been either ineffective (i.e., mesalamine) or poorly effective (i.e., thiopurines) in preventing POR.
Several studies (summarised in various meta-analyses) have shown the efficacy of anti-TNF agents in the prevention of POR in CD patients (Table 2). We identified 37 studies, including 1863 patients receiving prophylactic anti-TNF treatment, and the calculated mean endoscopic POR at 6–12 months was “only” 29% (Table 1). Although only few RCTs have directly compared the efficacy of thiopurines and anti-TNF agents in the postoperative setting, with somewhat controversial results, the superiority of the latter is supported by several meta-analyses. Infliximab and adalimumab seem to be equally effective in this scenario. The combination of anti-TNF and immunosuppressive agents should be considered in patients previously exposed to anti-TNFs, particularly in those with previous loss of response to these agents. Although some studies have reported that anti-TNFs are less effective for the prevention of POR in patients with previous exposure to anti-TNFs, others have shown that these agents remain an effective option to prevent POR also in patients operated upon with previous anti-TNF failure. Although theoretically, it may be reasonable to assume that once a first anti-TNF agent has failed preoperatively, a different anti-TNF should be prescribed, some studies have suggested that the consistent use of the same anti-TNF agent before and after the surgery may be effective in the prevention or POR. The role of therapeutic drug monitoring in the prevention of POR is unclear. Discontinuing anti-TNF agents in postoperative patients in remission is followed by rapid POR in the majority of them; therefore, prophylactic anti-TNF treatment should be continued in the long term. The cost effectiveness of anti-TNF treatment to prevent POR is still unclear, mainly because data on biosimilars have not been considered. Anti-TNF agents are effective not only for the prevention but also for the treatment of established POR. Finally, retreatment with anti-TNF therapy for POR is a valid strategy even after preoperative failure to these agents.
Regarding vedolizumab, six studies (including 156 patients) have evaluated the efficacy of this biological agent in the prevention of POR, and mean endoscopic POR at 6–12 months was calculated to be 41% (Table 3). The non-randomised comparison of anti-TNFs and vedolizumab in the postoperative setting has yielded controversial results, with some studies suggesting an advantage of one drug or another. Very recently, the first and only placebo-controlled RCT (REPREVIO trial) has confirmed that vedolizumab is quite effective in reducing both the incidence and the severity of POR in CD patients with increased risk of recurrence.
With respect to ustekinumab, seven studies (including 162 patients) have evaluated its efficacy to prevent POR, with a mean endoscopic POR at 6–12 months of 41% (Table 4), exactly the same figure as that calculated for vedolizumab. The comparative efficacy of ustekinumab against anti-TNF agents in the prevention of POR is still unclear. Ustekinumab and vedolizumab seem to be (equally) effective in the prevention of POR in patients at high risk, although the comparative experience is very limited. Further investigation of larger populations in an RCT is required to compare the efficacy of these two biological agents against anti-TNFs (and between themselves) in the postoperative setting.
References
Tsai L, Ma C, Dulai PS, Prokop LJ, Eisenstein S, Ramamoorthy SL, et al. Contemporary risk of surgery in patients with ulcerative colitis and Crohn's disease: a meta-analysis of population-based cohorts. Clin Gastroenterol Hepatol. 2021;19(10):2031–45 e11.
Nos P, Domenech E. Postoperative Crohn’s disease recurrence: a practical approach. World J Gastroenterol. 2008;14(36):5540–8.
Yamamoto T. Prevention of recurrence after surgery for Crohn’s disease: efficacy of infliximab. World J Gastroenterol. 2010;16(43):5405–10.
Buisson A, Chevaux JB, Bommelaer G, Peyrin-Biroulet L. Diagnosis, prevention and treatment of postoperative Crohn’s disease recurrence. Dig Liver Dis. 2012;44(6):453–60.
Buisson A, Chevaux JB, Allen PB, Bommelaer G, Peyrin-Biroulet L. Review article: the natural history of postoperative Crohn’s disease recurrence. Aliment Pharmacol Ther. 2012;35(6):625–33.
Frolkis AD, Dykeman J, Negron ME, Debruyn J, Jette N, Fiest KM, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145(5):996–1006.
Michetti P. Postsurgical prophylaxis in Crohn’s disease: which patients, which agents? Dig Dis (Basel, Switzerland). 2015;33(Suppl 1):78–81.
Lightner AL, Shen B. Perioperative use of immunosuppressive medications in patients with Crohn’s disease in the new “biological era.” Gastroenterol Rep. 2017;5(3):165–77.
Schlussel AT, Cherng NB, Alavi K. Current trends and challenges in the postoperative medical management of Crohn’s disease: a systematic review. Am J Surg. 2017;214(5):931–7.
Barnes EL. Postoperative Crohn’s disease management. Curr Opin Gastroenterol. 2020;36(4):277–83.
Vuitton L, Peyrin-Biroulet L. Pharmacological prevention of postoperative recurrence in Crohn’s disease. Drugs. 2020;80(4):385–99.
Liu C, Li N, Zhan S, Tian Z, Wu D, Li T, et al. Anti -TNFα agents in preventing the postoperative recurrence of Crohn’s disease: do they still play a role in the biological era? Expert Opin Biol Ther. 2021;21(11):1509–24.
Hanzel J, Drobne D. Contemporary management of postoperative Crohn's disease after ileocolonic resection. J Clin Med. 2022;11(22).
Lee KE, Cantrell S, Shen B, Faye AS. Post-operative prevention and monitoring of Crohn's disease recurrence. Gastroenterol Rep. 2022;10:goac070.
Dasharathy SS, Limketkai BN, Sauk JS. What’s new in the postoperative management of Crohn’s disease? Dig Dis Sci. 2022;67(8):3508–17.
Shah RS, Click BH. Medical therapies for postoperative Crohn’s disease. Ther Adv Gastroenterol. 2021;14:1756284821993581.
Battat R, Sandborn WJ. Advances in the comprehensive management of postoperative Crohn’s disease. Clin Gastroenterol Hepatol. 2022;20(7):1436–49.
Rutgeerts P, Geboes K, Vantrappen G, Beyls J, Kerremans R, Hiele M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology. 1990;99(4):956–63.
Greenstein AJ, Sachar DB, Pasternack BS, Janowitz HD. Reoperation and recurrence in Crohn’s colitis and ileocolitis crude and cumulative rates. N Engl J Med. 1975;293(14):685–90.
Frolkis AD, Lipton DS, Fiest KM, Negron ME, Dykeman J, deBruyn J, et al. Cumulative incidence of second intestinal resection in Crohn’s disease: a systematic review and meta-analysis of population-based studies. Am J Gastroenterol. 2014;109(11):1739–48.
Camma C, Giunta M, Rosselli M, Cottone M. Mesalamine in the maintenance treatment of Crohn’s disease: a meta-analysis adjusted for confounding variables. Gastroenterology. 1997;113(5):1465–73.
Doherty G, Bennett G, Patil S, Cheifetz A, Moss AC. Interventions for prevention of post-operative recurrence of Crohn's disease. Cochrane Database Syst Rev. 2009;7(4):Cd006873.
Cottone M, Camma C. Mesalamine and relapse prevention in Crohn’s disease. Gastroenterology. 2000;119(2):597.
Ford AC, Khan KJ, Talley NJ, Moayyedi P. 5-aminosalicylates prevent relapse of Crohn’s disease after surgically induced remission: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(3):413–20.
Yang Z, Ye X, Wu Q, Wu K, Fan D. A network meta-analysis on the efficacy of 5-aminosalicylates, immunomodulators and biologics for the prevention of postoperative recurrence in Crohn’s disease. Int J Surg (London, England). 2014;12(5):516–22.
Singh S, Garg SK, Pardi DS, Wang Z, Murad MH, Loftus EV Jr. Comparative efficacy of pharmacologic interventions in preventing relapse of Crohn's disease after surgery: a systematic review and network meta-analysis. Gastroenterology. 2015;148(1):64–76.e2 (quiz e14).
Lim WC, Wang Y, MacDonald JK, Hanauer S. Aminosalicylates for induction of remission or response in Crohn's disease. Cochrane Database Syst Rev. 2016;7(7):CD008870.
Burr NE, Hall B, Hamlin PJ, Selinger CP, Ford AC, O’Connor A. Systematic review and network meta-analysis of medical therapies to prevent recurrence of post-operative Crohn’s disease. J Crohns Colitis. 2019;13(6):693–701.
Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, Lakatos PL, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 2: surgical management and special situations. J Crohns Colitis. 2017;11(2):135–49.
Peyrin-Biroulet L, Deltenre P, Ardizzone S, D’Haens G, Hanauer SB, Herfarth H, et al. Azathioprine and 6-mercaptopurine for the prevention of postoperative recurrence in Crohn’s disease: a meta-analysis. Am J Gastroenterol. 2009;104(8):2089–96.
Jones GR, Kennedy NA, Lees CW, Arnott ID, Satsangi J. Systematic review: The use of thiopurines or anti-TNF in post-operative Crohn’s disease maintenance–progress and prospects. Aliment Pharmacol Ther. 2014;39(11):1253–65.
Gjuladin-Hellon T, Iheozor-Ejiofor Z, Gordon M, Akobeng AK. Azathioprine and 6-mercaptopurine for maintenance of surgically-induced remission in Crohn's disease. Cochrane Database Syst Rev. 2019;8(8):CD010233.
Nguyen GC, Loftus EV Jr, Hirano I, Falck-Ytter Y, Singh S, Sultan S, et al. American Gastroenterological Association institute guideline on the management of Crohn’s disease after surgical resection. Gastroenterology. 2017;152(1):271–5.
Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, Limdi JK, et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019;68(Suppl 3):s1–106.
Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg. 2000;231(1):38–45.
Gisbert JP, Chaparro M. Primary failure to an anti-TNF agent in inflammatory bowel disease: switch (to a second anti-TNF agent) or swap (for another mechanism of action)? J Clin Med. 2021;10(22).
Sorrentino D, Terrosu G, Avellini C, Beltrami CA, Bresadola V, Toso F. Prevention of postoperative recurrence of Crohn’s disease by infliximab. Eur J Gastroenterol Hepatol. 2006;18(4):457–9.
Sorrentino D, Terrosu G, Avellini C, Maiero S. Infliximab with low-dose methotrexate for prevention of postsurgical recurrence of ileocolonic Crohn disease. Arch Intern Med. 2007;167(16):1804–7.
Regueiro M, Schraut W, Baidoo L, Kip KE, Sepulveda AR, Pesci M, et al. Infliximab prevents Crohn's disease recurrence after ileal resection. Gastroenterology. 2009;136(2):441–50.e1 (quiz 716).
Sorrentino D, Paviotti A, Terrosu G, Avellini C, Geraci M, Zarifi D. Low-dose maintenance therapy with infliximab prevents postsurgical recurrence of Crohn's disease. Clin Gastroenterol Hepatol. 2010;8(7):591–9 e1 (quiz e78–9).
Yoshida K, Fukunaga K, Ikeuchi H, Kamikozuru K, Hida N, Ohda Y, et al. Scheduled infliximab monotherapy to prevent recurrence of Crohn’s disease following ileocolic or ileal resection: a 3-year prospective randomized open trial. Inflamm Bowel Dis. 2012;18(9):1617–23.
Aguas M, Bastida G, Cerrillo E, Beltrán B, Iborra M, Sánchez-Montes C, et al. Adalimumab in prevention of postoperative recurrence of Crohn’s disease in high-risk patients. World J Gastroenterol. 2012;18(32):4391–8.
Papamichael K, Archavlis E, Lariou C, Mantzaris GJ. Adalimumab for the prevention and/or treatment of post-operative recurrence of Crohn’s disease: a prospective, two-year, single center, pilot study. J Crohns Colitis. 2012;6(9):924–31.
Sakuraba A, Sato T, Matsukawa H, Okamoto S, Takaishi H, Ogata H, et al. The use of infliximab in the prevention of postsurgical recurrence in polysurgery Crohn’s disease patients: a pilot open-labeled prospective study. Int J Colorectal Dis. 2012;27(7):947–52.
Savarino E, Dulbecco P, Bodini G, Assandri L, Savarino V. Prevention of postoperative recurrence of Crohn’s disease by Adalimumab: a case series. Eur J Gastroenterol Hepatol. 2012;24(4):468–70.
Kotze PG, Yamamoto T. Infliximab versus azathioprine to prevent postoperative recurrence in Crohn’s disease: are all controversial issues defined? J Crohns Colitis. 2013;7(12): e698.
Savarino E, Bodini G, Dulbecco P, Assandri L, Bruzzone L, Mazza F, et al. Adalimumab is more effective than azathioprine and mesalamine at preventing postoperative recurrence of Crohn’s disease: a randomized controlled trial. Am J Gastroenterol. 2013;108(11):1731–42.
Armuzzi A, Felice C, Papa A, Marzo M, Pugliese D, Andrisani G, et al. Prevention of postoperative recurrence with azathioprine or infliximab in patients with Crohn’s disease: an open-label pilot study. J Crohns Colitis. 2013;7(12):e623–9.
Tursi A, Elisei W, Picchio M, Zampaletta C, Pelecca G, Faggiani R, et al. Comparison of the effectiveness of infliximab and adalimumab in preventing postoperative recurrence in patients with Crohn’s disease: an open-label, pilot study. Tech Coloproctol. 2014;18(11):1041–6.
De Cruz P, Kamm MA, Hamilton AL, Ritchie KJ, Krejany EO, Gorelik A, et al. Efficacy of thiopurines and adalimumab in preventing Crohn’s disease recurrence in high-risk patients—a POCER study analysis. Aliment Pharmacol Ther. 2015;42(7):867–79.
Kotze PG, Yamamoto T, Danese S, Suzuki Y, Teixeira FV, de Albuquerque IC, et al. Direct retrospective comparison of adalimumab and infliximab in preventing early postoperative endoscopic recurrence after ileocaecal resection for crohn’s disease: results from the MULTIPER database. J Crohns Colitis. 2015;9(7):541–7.
Regueiro M, Feagan BG, Zou B, Johanns J, Blank MA, Chevrier M, et al. Infliximab reduces endoscopic, but not clinical, recurrence of Crohn’s disease after ileocolonic resection. Gastroenterology. 2016;150(7):1568–78.
Preda CM, Fulger LE, Negreanu L, Manuc M, Sandra I, Diculescu MM. Adalimumab versus infliximab in treating post-operative recurrence of Crohn’s disease: a national cohort study. Revista espanola de enfermedades digestivas : organo oficial de la Sociedad Espanola de Patologia Digestiva. 2016;108(10):642–7.
Takeshima F, Yoshikawa D, Higashi S, Morisaki T, Oda H, Ikeda M, et al. Clinical efficacy of adalimumab in Crohn’s disease: a real practice observational study in Japan. BMC Gastroenterol. 2016;16(1):82.
Collins M, Sarter H, Gower-Rousseau C, Koriche D, Libier L, Nachury M, et al. Previous exposure to multiple anti-TNF is associated with decreased efficiency in preventing postoperative Crohn’s disease recurrence. J Crohns Colitis. 2017;11(3):281–8.
López-Sanromán A, Vera-Mendoza I, Domènech E, Taxonera C, Vega Ruiz V, Marín-Jiménez I, et al. Adalimumab vs azathioprine in the prevention of postoperative Crohn's disease recurrence. A GETECCU randomised trial. J Crohn's Colitis. 2017;11(11):1293–301.
Allocca M, Landi R, Bonovas S, Fiorino G, Papa A, Spinelli A, et al. Effectiveness of mesalazine, thiopurines and tumour necrosis factor antagonists in preventing post-operative Crohn’s disease recurrence in a real-life setting. Digestion. 2017;96(3):166–72.
Fay S, Ungar B, Paul S, Levartovsky A, Yavzori M, Fudim E, et al. The association between drug levels and endoscopic recurrence in postoperative patients with Crohn’s disease treated with tumor necrosis factor inhibitors. Inflamm Bowel Dis. 2017;23(11):1924–9.
Asada T, Nakayama G, Tanaka C, Kobayashi D, Ezaka K, Hattori N, et al. Postoperative adalimumab maintenance therapy for Japanese patients with Crohn’s disease: a single-center, single-arm phase II trial (CCOG-1107 study). Surg Today. 2018;48(6):609–17.
Fukushima K, Sugita A, Futami K, Takahashi KI, Motoya S, Kimura H, et al. Postoperative therapy with infliximab for Crohn’s disease: a 2-year prospective randomized multicenter study in Japan. Surg Today. 2018;48(6):584–90.
Auzolle C, Nancey S, Tran-Minh ML, Buisson A, Pariente B, Stefanescu C, et al. Male gender, active smoking and previous intestinal resection are risk factors for post-operative endoscopic recurrence in Crohn’s disease: results from a prospective cohort study. Aliment Pharmacol Ther. 2018;48(9):924–32.
Hiraoka S, Takashima S, Kondo Y, Inokuchi T, Sugihara Y, Takahara M, et al. Efficacy of restarting anti-tumor necrosis factor α agents after surgery in patients with Crohn’s disease. Intest Res. 2018;16(1):75–82.
Yamada A, Komaki Y, Patel N, Komaki F, Pekow J, Dalal S, et al. The use of vedolizumab in preventing postoperative recurrence of Crohn’s disease. Inflamm Bowel Dis. 2018;24(3):502–9.
Cañete F, Mañosa M, Casanova MJ, González-Sueyro RC, Barrio J, Bermejo F, et al. Adalimumab or infliximab for the prevention of early postoperative recurrence of Crohn disease: results From the ENEIDA Registry. Inflamm Bowel Dis. 2019;25(11):1862–70.
Maggiori L, Brouquet A, Zerbib P, Lefevre JH, Denost Q, Germain A, et al. Penetrating Crohn disease is not associated with a higher risk of recurrence after surgery: a prospective nationwide cohort conducted by the Getaid Chirurgie Group. Ann Surg. 2019;270(5):827–34.
Rivière P, Vermeire S, Irles-Depe M, Van Assche G, Rutgeerts P, Denost Q, et al. Rates of postoperative recurrence of Crohn’s disease and effects of immunosuppressive and biologic therapies. Clin Gastroenterol Hepatol. 2021;19(4):713-20.e1.
Yanai H, Kagramanova A, Knyazev O, Sabino J, Haenen S, Mantzaris GJ, et al. Endoscopic postoperative recurrence in Crohn’s disease after curative ileocecal resection with early prophylaxis by anti-TNF, vedolizumab or ustekinumab: a real-world multicentre European study. J Crohns Colitis. 2022;16(12):1882–92.
Le Cosquer G, Altwegg R, Rivière P, Bournet B, Boivineau L, Poullenot F, et al. Prevention of post-operative recurrence of Crohn's disease among patients with prior anti-TNFα failure: a retrospective multicenter study. Dig Liver Dis. 2022 (In press).
Buisson A, Cannon L, Umanskiy K, Hurst RD, Hyman NH, Sakuraba A, et al. Factors associated with anti-tumor necrosis factor effectiveness to prevent postoperative recurrence in Crohn’s disease. Intest Res. 2022;20(3):303–12.
Yu J, Hyun HK, Park J, Kang EA, Park SJ, Park JJ, et al. Continued postoperative use of tumor necrosis factor-α inhibitors for the prevention of Crohn’s disease recurrence. Gut Liver. 2022;16(3):414–22.
Buisson A, Blanco L, Manlay L, Reymond M, Dapoigny M, Rouquette O, et al. Top-down versus step-up strategies to prevent postoperative recurrence in Crohn’s disease. Inflamm Bowel Dis. 2022;7(29):185–94.
Axelrad JE, Li T, Bachour SP, Nakamura TI, Shah R, Sachs MC, et al. Early initiation of antitumor necrosis factor therapy reduces postoperative recurrence of Crohn's disease following ileocecal resection. Inflamm Bowel Dis (In press).
Malireddy K, Larson DW, Sandborn WJ, Loftus EV, Faubion WA, Pardi DS, et al. Recurrence and impact of postoperative prophylaxis in laparoscopically treated primary ileocolic Crohn disease. Arch Surg (Chicago, Ill: 1960). 2010;145(1):42–7.
Yamamoto T, Bamba T, Umegae S, Matsumoto K. The impact of early endoscopic lesions on the clinical course of patients following ileocolonic resection for Crohn’s disease: a 5-year prospective cohort study. United Eur Gastroenterol J. 2013;1(4):294–8.
Araki T, Uchida K, Okita Y, Fujikawa H, Inoue M, Ohi M, et al. Impact of postoperative infliximab maintenance therapy on preventing the surgical recurrence of Crohn’s disease: a single-center paired case-control study. Surg Today. 2014;44(2):291–6.
González-Lama Y, Blázquez I, Suárez CJ, Oliva B, Matallana V, Calvo M, et al. Impact of endoscopic monitoring in postoperative Crohn’s disease patients already receiving pharmacological prevention of recurrence. Revista espanola de enfermedades digestivas : organo oficial de la Sociedad Espanola de Patologia Digestiva. 2015;107(10):586–90.
Sakuraba A, Okamoto S, Matsuoka K, Sato T, Naganuma M, Hisamatsu T, et al. Combination therapy with infliximab and thiopurine compared to infliximab monotherapy in maintaining remission of postoperative Crohn’s disease. Digestion. 2015;91(3):233–8.
Kjeldsen J, Nielsen J, Larsen MD, Qvist N, Nørgård BM. Postoperative use of anti-TNF-α agents in patients with Crohn’s disease and risk of reoperation—a nationwide cohort study. Inflamm Bowel Dis. 2016;22(3):599–606.
Li Y, Stocchi L, Rui Y, Remzi FH, Shen B. Comparable outcomes of the consistent use versus switched use of anti- tumor necrosis factor agents in postoperative recurrent Crohn’s disease following ileocolonic resection. Int J Colorectal Dis. 2016;31(11):1751–8.
O’Connor A, Hamlin PJ, Taylor J, Selinger C, Scott N, Ford AC. Postoperative prophylaxis in Crohn’s disease after intestinal resection: a retrospective analysis. Frontline Gastroenterol. 2017;8(3):203–9.
Kusaka J, Shiga H, Kuroha M, Kimura T, Kakuta Y, Endo K, et al. Risk factors associated with postoperative recurrence and repeat surgery in Japanese patients with Crohn’s disease. Int J Colorectal Dis. 2017;32(10):1407–13.
Yang KM, Yu CS, Lee JL, Kim CW, Yoon YS, Park IJ, et al. Risk factors for postoperative recurrence after primary bowel resection in patients with Crohn’s disease. World J Gastroenterol. 2017;23(38):7016–24.
Araki T, Okita Y, Kondo S, Hiro J, Toiyama Y, Inoue M, et al. Risk factors for recurrence of Crohn’s disease requiring surgery in patients receiving post-operative anti-tumor necrosis factor maintenance therapy. J Anus Rectum Colon. 2017;1(1):15–21.
de Barcelos IF, Kotze PG, Spinelli A, Suzuki Y, Teixeira FV, de Albuquerque IC, et al. Factors affecting the incidence of early endoscopic recurrence after ileocolonic resection for Crohn’s disease: a multicentre observational study. Colorectal Dis. 2017;19(1):O39-o45.
Jouvin I, Lefevre JH, Creavin B, Pitel S, Chafai N, Tiret E, et al. Postoperative morbidity risks following ileocolic resection for Crohn’s disease treated with anti-TNF alpha therapy: a retrospective study of 360 patients. Inflamm Bowel Dis. 2018;24(2):422–32.
Chen ZX, Chen YL, Huang XM, Lin XT, He XW, Lan P. Risk factors for recurrence after bowel resection for Crohn’s disease. World J Gastrointest Pharmacol Ther. 2019;10(4):67–74.
Kline BP, Weaver T, Brinton DL Jr, Harris L, Yochum GS, Berg AS, et al. Clinical and genetic factors impact time to surgical recurrence after ileocolectomy for Crohn’s disease. Ann Surg. 2021;274(2):346–51.
Zeng L, Meng WJ, Wen ZH, Chen YL, Wang YF, Tang CW. Management and outcomes of surgical patients with intestinal Behçet’s disease and Crohn’s disease in southwest China. World J Clin Cases. 2021;9(16):3858–68.
Kamel S, Sakr M, Hamed W, Eltabbakh M, Sherief A, Rashad H, et al. Characterization of Crohn's disease patients in Egypt: risk factors for postoperative recurrence (a cohort study). Ann Med Surg (2012). 2021;69:102781.
Guo MY, Sun XY, Wu B, Chen XF, Zhang HM, Zhang MM, et al. Reoperation rate and related factors in patients with Crohn’s disease. Zhonghua Yi Xue Za Zhi. 2021;101(22):1683–9.
Thin LWY, Picardo S, Sooben S, Murray K, Ryan J, Wallace MH. Ileocolonic end-to-end anastomoses in crohn’s disease increase the risk of early post-operative endoscopic recurrence in those undergoing an emergency resection. J Gastrointest Surg. 2021;25(1):241–51.
Arkenbosch JHC, Beelen EMJ, Dijkstra G, Romberg-Camps M, Duijvestein M, Hoentjen F, et al. Prophylactic medication for the prevention of endoscopic recurrence in Crohn’s disease: a prospective study based on clinical risk stratification. J Crohns Colitis. 2023;12(17):221–30.
Azzam N, AlRuthia Y, Al Thaher A, Almadi M, Alharbi O, Altuwaijri M, et al. Rate and risk factors of postoperative endoscopic recurrence of moderate- to high-risk Crohn’s disease patients—a real-world experience from a Middle Eastern cohort. Saudi J Gastroenterol. 2022;28(3):201–8.
Arkenbosch JHC, Mak JWY, Ho JCL, Beelen EMJ, Erler NS, Hoentjen F, et al. Indications, postoperative management, and long-term prognosis of Crohn’s disease after ileocecal resection: a multicenter study comparing the east and west. Inflamm Bowel Dis. 2022;28(Suppl 2):S16-s24.
D’Amico F, Tasopoulou O, Fiorino G, Zilli A, Furfaro F, Allocca M, et al. Early biological therapy in operated Crohn’s disease patients is associated with a lower rate of endoscopic recurrence and improved long-term outcomes: a single-center experience. Inflamm Bowel Dis. 2023;28(29):539–47.
Sorrentino D, Marino M, Dassopoulos T, Zarifi D, Del Bianco T. Low dose infliximab for prevention of postoperative recurrence of Crohn’s disease: long term follow-up and impact of infliximab trough levels and antibodies to infliximab. PLoS ONE. 2015;10(12): e0144900.
Bodini G, Savarino V, Peyrin-Biroulet L, de Cassan C, Dulbecco P, Baldissarro I, et al. Low serum trough levels are associated with post-surgical recurrence in Crohn’s disease patients undergoing prophylaxis with adalimumab. Dig Liver Dis. 2014;46(11):1043–6.
Ghosh S, D’Haens G. Is an ounce of prevention worth a pound of cure: postoperative recurrence of Crohn’s disease? Gastroenterology. 2016;150(7):1521–4.
van Loo ES, Dijkstra G, Ploeg RJ, Nieuwenhuijs VB. Prevention of postoperative recurrence of Crohn’s disease. J Crohns Colitis. 2012;6(6):637–46.
Nguyen DL, Solaimani P, Nguyen ET, Jamal MM, Bechtold ML. Antitumor necrosis factor α is more effective than conventional medical therapy for the prevention of postoperative recurrence of Crohn’s disease: a meta-analysis. Eur J Gastroenterol Hepatol. 2014;26(10):1152–9.
Carla-Moreau A, Paul S, Roblin X, Genin C, Peyrin-Biroulet L. Prevention and treatment of postoperative Crohn’s disease recurrence with anti-TNF therapy: a meta-analysis of controlled trials. Dig Liver Dis. 2015;47(3):191–6.
Zhao Y, Ma T, Chen YF, He XY, Ren LH, Chen J, et al. Biologics for the prevention of postoperative Crohn’s disease recurrence: a systematic review and meta-analysis. Clin Res Hepatol Gastroenterol. 2015;39(5):637–49.
Qiu Y, Mao R, Chen BL, He Y, Zeng ZR, Chen MH. Systematic review with meta-analysis of prospective studies: anti-tumour necrosis factor for prevention of postoperative Crohn’s disease recurrence. J Crohns Colitis. 2015;9(10):918–27.
Feng JS, Li JY, Chen XY, Yang Z, Li SH. Strategies for preventing endoscopic recurrence of Crohn’s disease 1 year after surgery: a network meta-analysis. Gastroenterol Res Pract. 2017;2017:7896160.
Huang H, Xu S, Huang F, Wang X, Chen Y, Xu Z. A meta-analysis of efficacy and safety of infliximab for prevention of postoperative recurrence in patients with Crohn’s disease. Biomed Res Int. 2018;2018:2615978.
Bakouny Z, Yared F, El Rassy E, Jabbour R, Hallit R, Khoury N, et al. Comparative efficacy of anti-TNF therapies for the prevention of postoperative recurrence of Crohn’s disease: a systematic review and network meta-analysis of prospective trials. J Clin Gastroenterol. 2019;53(6):409–17.
Erős A, Farkas N, Hegyi P, Szabó A, Balaskó M, Veres G, et al. Anti-TNFα agents are the best choice in preventing postoperative Crohn’s disease: a meta-analysis. Dig Liver Dis. 2019;51(8):1086–95.
Jain SR, Ow ZGW, Chin YH, Lim WH, Kong G, Tham HY, et al. Quantifying the rate of recurrence of postoperative Crohn’s disease with biological therapy. A meta-analysis. J Dig Dis. 2021;22(7):399–407.
Uchino M, Ikeuchi H, Hata K, Minagawa T, Horio Y, Kuwahara R, et al. Does anti-tumor necrosis factor alpha prevent the recurrence of Crohn’s disease? Systematic review and meta-analysis. J Gastroenterol Hepatol. 2021;36(4):864–72.
Beelen EMJ, Nieboer D, Arkenbosch JHC, Regueiro MD, Satsangi J, Ardizzone S, et al. Risk prediction and comparative efficacy of anti-TNF vs thiopurines, for preventing postoperative recurrence in Crohn’s disease: a pooled analysis of 6 trials. Clin Gastroenterol Hepatol. 2022;20(12):2741-52.e6.
Shinagawa T, Hata K, Ikeuchi H, Fukushima K, Futami K, Sugita A, et al. Rate of reoperation decreased significantly after year 2002 in patients with Crohn's disease. Clin Gastroenterol Hepatol. 2020;18(4):898–907 e5.
Nguyen VQ, Mays JL, Lang M, Wu Y, Dassopoulos T, Regueiro M, et al. Knowledge gaps in the management of postoperative Crohn’s disease: a US national survey. Dig Dis Sci. 2018;63(1):53–60.
Dragoni G, Ding N, Gecse KB, Mansfield JC, Kopylov U, Beaugerie L, et al. The prevention and management of Crohn’s disease postoperative recurrence: results from the Y-ECCO/ClinCom 2019 survey. Eur J Gastroenterol Hepatol. 2020;32(8):1062–6.
Regueiro M, El-Hachem S, Kip KE, Schraut W, Baidoo L, Watson A, et al. Postoperative infliximab is not associated with an increase in adverse events in Crohn’s disease. Dig Dis Sci. 2011;56(12):3610–5.
De Cruz P, Kamm MA, Hamilton AL, Ritchie KJ, Krejany EO, Gorelik A, et al. Crohn’s disease management after intestinal resection: a randomised trial. Lancet (London, England). 2015;385(9976):1406–17.
Ardizzone S, Maconi G, Sampietro GM, Russo A, Radice E, Colombo E, et al. Azathioprine and mesalamine for prevention of relapse after conservative surgery for Crohn’s disease. Gastroenterology. 2004;127(3):730–40.
Mowat C, Arnott I, Cahill A, Smith M, Ahmad T, Subramanian S, et al. Mercaptopurine versus placebo to prevent recurrence of Crohn’s disease after surgical resection (TOPPIC): a multicentre, double-blind, randomised controlled trial. Lancet Gastroenterol Hepatol. 2016;1(4):273–82.
Reese GE, Nanidis T, Borysiewicz C, Yamamoto T, Orchard T, Tekkis PP. The effect of smoking after surgery for Crohn's disease: a meta-analysis of observational studies. Int J Colorectal Dis. 2008;23(12):1213–21.
Simillis C, Yamamoto T, Reese GE, Umegae S, Matsumoto K, Darzi AW, et al. A meta-analysis comparing incidence of recurrence and indication for reoperation after surgery for perforating versus nonperforating Crohn’s disease. Am J Gastroenterol. 2008;103(1):196–205.
Domenech E, Lopez-Sanroman A, Nos P, Vera M, Chaparro M, Esteve M, et al. Recommendations of the Spanish Working Group on Crohn's Disease and Ulcerative Colitis (GETECCU) on the monitoring, prevention and treatment of post-operative recurrence in Crohn's disease. Gastroenterologia y hepatologia. 2017;40(7):472–83.
Candia R, Bravo-Soto GA, Monrroy H, Hernandez C, Nguyen GC. Colonoscopy-guided therapy for the prevention of post-operative recurrence of Crohn's disease. Cochrane Database Syst Rev. 2020;8(8):Cd012328.
Joustra V, van Sabben J, van der Does de Willebois E, Duijvestein M, de Boer N, Jansen J, et al. Benefit of risk-stratified prophylactic treatment on clinical outcome in postoperative Crohn's disease. J Crohn's Colitis. 2023;17(3):318–28.
Dragoni G, Castiglione F, Bezzio C, Pugliese D, Spagnuolo R, Viola A, et al. Comparison of two strategies for the management of postoperative recurrence in Crohn’s disease patients with one clinical risk factor: a multicentre IG-IBD study. United Eur Gastroenterol J. 2023;11(3):271–81.
D’Haens GR, Vermeire S, Van Assche G, Noman M, Aerden I, Van Olmen G, et al. Therapy of metronidazole with azathioprine to prevent postoperative recurrence of Crohn’s disease: a controlled randomized trial. Gastroenterology. 2008;135(4):1123–9.
Tang S, Liu W, Qi W, Yu T, Cao Q, Ge X, et al. Real-world experience with AGA guidelines in the management of Crohn’s disease following ileocolonic resection: a retrospective cohort study. Gastroenterol Res Pract. 2020;2020:8618574.
Colombel JF, Sandborn WJ, Reinisch W, Mantzaris GJ, Kornbluth A, Rachmilewitz D, et al. Infliximab, azathioprine, or combination therapy for Crohn’s disease. N Engl J Med. 2010;362(15):1383–95.
Panaccione R, Ghosh S, Middleton S, Marquez JR, Scott BB, Flint L, et al. Combination therapy with infliximab and azathioprine is superior to monotherapy with either agent in ulcerative colitis. Gastroenterology. 2014;146(2):392-400 e3.
Roblin X, Verot C, Paul S, Duru G, Williet N, Boschetti G, et al. Is the pharmacokinetic profile of a first anti-TNF predictive of the clinical outcome and pharmacokinetics of a second anti-TNF? Inflamm Bowel Dis. 2018;24(9):2078–85.
D’Haens GR, Geboes K, Peeters M, Baert F, Penninckx F, Rutgeerts P. Early lesions of recurrent Crohn’s disease caused by infusion of intestinal contents in excluded ileum. Gastroenterology. 1998;114(2):262–7.
Cohen-Mekelburg S, Gold S, Schneider Y, Dennis M, Oromendia C, Yeo H, et al. Delays in initiating post-operative prophylactic biologic therapy are common among Crohn’s disease patients. Dig Dis Sci. 2019;64(1):196–203.
Fields AC, Melnitchouk N. Medical prophylaxis of post-surgical Crohn’s disease recurrence: towards timely anti-TNF therapy. Dig Dis Sci. 2019;64(1):7–8.
Gisbert JP, Panes J. Loss of response and requirement of infliximab dose intensification in Crohn’s disease: a review. Am J Gastroenterol. 2009;104(3):760–7.
Allez M, Karmiris K, Louis E, Van Assche G, Ben-Horin S, Klein A, et al. Report of the ECCO pathogenesis workshop on anti-TNF therapy failures in inflammatory bowel diseases: definitions, frequency and pharmacological aspects. J Crohns Colitis. 2010;4(4):355–66.
Chaparro M, Guerra I, Munoz-Linares P, Gisbert JP. Systematic review: antibodies and anti-TNF-alpha levels in inflammatory bowel disease. Aliment Pharmacol Ther. 2012;35(9):971–86.
Gisbert JP, Marin AC, McNicholl AG, Chaparro M. Systematic review with meta-analysis: the efficacy of a second anti-TNF in patients with inflammatory bowel disease whose previous anti-TNF treatment has failed. Aliment Pharmacol Ther. 2015;41(7):613–23.
VandeCasteele N, Feagan BG, Wolf DC, Pop A, Yassine M, Horst SN, et al. Therapeutic drug monitoring of tumor necrosis factor antagonists in Crohn disease: a theoretical construct to apply pharmacokinetics and guidelines to clinical practice. Inflamm Bowel Dis. 2021;27(8):1346–55.
van Hoeve K, Dreesen E, Hoffman I, Van Assche G, Ferrante M, Gils A, et al. Higher infliximab trough levels are associated with better outcome in paediatric patients with inflammatory bowel disease. J Crohns Colitis. 2018;12(11):1316–25.
Boivineau L, Guillon F, Altwegg R. Serum adalimumab concentration after surgery is correlated with postoperative endoscopic recurrence in Crohn’s disease patients: one step before proactive therapeutic drug monitoring. J Crohns Colitis. 2020;14(10):1500–1.
Nones RB, Fleshner PR, Queiroz NSF, Cheifetz AS, Spinelli A, Danese S, et al. Therapeutic drug monitoring of biologics in IBD: essentials for the surgical patient. J Clin Med. 2021;10(23).
Baraúna F, Kotze PG. Correlation between trough levels of infliximab and postoperative endoscopic recurrence in Crohn’s disease patients submitted to ileocolonic resections: a systematic review. Arq Gastroenterol. 2021;58(1):107–13.
Wright EK, Kamm MA, De Cruz P, Hamilton AL, Selvaraj F, Princen F, et al. Anti-TNF therapeutic drug monitoring in postoperative Crohn’s disease. J Crohns Colitis. 2018;12(6):653–61.
Herfarth HH. Anti-tumor necrosis factor therapy to prevent Crohn’s disease recurrence after surgery. Clin Gastroenterol Hepatol. 2014;12(9):1503–6.
Doherty G, Katsanos KH, Burisch J, Allez M, Papamichael K, Stallmach A, et al. European Crohn’s and colitis organisation topical review on treatment withdrawal [’Exit Strategies’] in inflammatory bowel disease. J Crohns Colitis. 2018;12(1):17–31.
Noor NM, Sousa P, Bettenworth D, Gomollon F, Lobaton T, Bossuyt P, et al. ECCO topical review on biological treatment cycles in Crohn's disease. J Crohns Colitis (in press).
Regueiro M, Kip KE, Baidoo L, Swoger JM, Schraut W. Postoperative therapy with infliximab prevents long-term Crohn’s disease recurrence. Clin Gastroenterol Hepatol. 2014;12(9):1494-502.e1.
Ananthakrishnan AN, Hur C, Juillerat P, Korzenik JR. Strategies for the prevention of postoperative recurrence in Crohn’s disease: results of a decision analysis. Am J Gastroenterol. 2011;106(11):2009–17.
Doherty GA, Miksad RA, Cheifetz AS, Moss AC. Comparative cost-effectiveness of strategies to prevent postoperative clinical recurrence of Crohn’s disease. Inflamm Bowel Dis. 2012;18(9):1608–16.
Candia R, Naimark D, Sander B, Nguyen GC. Cost-utility analysis: thiopurines plus endoscopy-guided biological step-up therapy is the optimal management of postoperative Crohn’s disease. Inflamm Bowel Dis. 2017;23(11):1930–40.
Yamamoto T, Umegae S, Matsumoto K. Impact of infliximab therapy after early endoscopic recurrence following ileocolonic resection of Crohn’s disease: a prospective pilot study. Inflamm Bowel Dis. 2009;15(10):1460–6.
Sorrentino D, Terrosu G, Paviotti A, Geraci M, Avellini C, Zoli G, et al. Early diagnosis and treatment of postoperative endoscopic recurrence of Crohn’s disease: partial benefit by infliximab–a pilot study. Dig Dis Sci. 2012;57(5):1341–8.
Freeman JJ, Rabah R, Hirschl RB, Maspons A, Meier D, Teitelbaum DH. Anti-TNF-α treatment for post-anastomotic ulcers and inflammatory bowel disease with Crohn’s-like pathologic changes following intestinal surgery in pediatric patients. Pediatr Surg Int. 2015;31(1):77–82.
Cañete F, Mañosa M, Pérez-Martínez I, Barreiro-de Acosta M, González-Sueyro RC, Nos P, et al. Antitumor necrosis factor agents to treat endoscopic postoperative recurrence of Crohn’s disease: a nationwide study with propensity-matched score analysis. Clin Transl Gastroenterol. 2020;11(8): e00218.
Assa A, Bronsky J, Kolho KL, Zarubova K, de Meij T, Ledder O, et al. Anti-TNFα treatment after surgical resection for Crohn’s disease is effective despite previous pharmacodynamic failure. Inflamm Bowel Dis. 2017;23(5):791–7.
Ten Bokkel HS, Beelen EMJ, Ten Bokkel HT, Hoentjen F, Dijkstra G, et al. Retreatment with anti-tumor necrosis factor therapy in combination with an immunomodulator for recurrence of Crohn’s disease after ileocecal resection results in prolonged continuation as compared to anti-tumor necrosis factor monotherapy. Eur J Gastroenterol Hepatol. 2023;35(1):45–51.
Yarur AJ, Jain A, Sussman DA, Barkin JS, Quintero MA, Princen F, et al. The association of tissue anti-TNF drug levels with serological and endoscopic disease activity in inflammatory bowel disease: the ATLAS study. Gut. 2016;65(2):249–55.
Atreya R, Neumann H, Neufert C, Waldner MJ, Billmeier U, Zopf Y, et al. In vivo imaging using fluorescent antibodies to tumor necrosis factor predicts therapeutic response in Crohn’s disease. Nat Med. 2014;20(3):313–8.
Sorrentino D, Fogel S, Van den Bogaerde J. Surgery for Crohn’s disease and anti-TNF agents: the changing scenario. Expert Rev Gastroenterol Hepatol. 2013;7(8):689–700.
Sorrentino D, Paviotti A, Fiorino G. Anti-TNF’s for postoperative recurrence in Crohn’s disease: the if’s and how’s. Curr Drug Targets. 2010;11(2):219–26.
Meresse B, Rutgeerts P, Malchow H, Dubucquoi S, Dessaint JP, Cohard M, et al. Low ileal interleukin 10 concentrations are predictive of endoscopic recurrence in patients with Crohn’s disease. Gut. 2002;50(1):25–8.
Barnes EL, Lightner AL, Regueiro M. Perioperative and postoperative management of patients with Crohn’s disease and ulcerative colitis. Clin Gastroenterol Hepatol. 2020;18(6):1356–66.
Gisbert JP, Domenech E. Vedolizumab in the treatment of Crohn’s disease. Gastroenterol Hepatol. 2015;38(5):338–48.
Attauabi M, Madsen GR, Bendtsen F, Seidelin JB, Burisch J. Vedolizumab as the first line of biologic therapy for ulcerative colitis and Crohn’s disease—a systematic review with meta-analysis. Dig Liver Dis. 2022;54(9):1168–78.
Qiu B, Liang JX, Li C. Efficacy and safety of vedolizumab for inflammatory bowel diseases: a systematic review and meta-analysis of randomized controlled trials. Medicine. 2022;101(40): e30590.
Chaparro M, Garre A, Ricart E, Iborra M, Mesonero F, Vera I, et al. Short and long-term effectiveness and safety of vedolizumab in inflammatory bowel disease: results from the ENEIDA registry. Aliment Pharmacol Ther. 2018;48(8):839–51.
Lemmens B, de Buck van Overstraeten A, Arijs I, Sagaert X, Van Assche G, Vermeire S, et al. Submucosal plexitis as a predictive factor for postoperative endoscopic recurrence in patients with Crohn's disease undergoing a resection with ileocolonic anastomosis: results from a prospective single-centre study. J Crohn's Colitis. 2017;11(2):212–20.
Mañosa M, Fernández-Clotet A, Nos P, Martín-Arranz MD, Manceñido N, Carbajo A, et al. Ustekinumab and vedolizumab for the prevention of postoperative recurrence of Crohn’s disease: results from the ENEIDA registry. Dig Liver Dis. 2023;55(1):46–52.
D’Haens G, Taxonera C, Lopez-Sanroman A, Nos Mateu P, Danese S, Armuzzi A, et al. Prevention of postoperative recurrence of Crohn's disease with vedolizumab: first results of the prospective placebo-controlled randomised trial REPREVIO. J Crohn's Colitis. 2023;17(Issue S1):i19.
Brierley R. 18th congress of the European Crohn’s and colitis organisation. Lancet Gastroenterol Hepatol. 2023;8(5):404.
Macaluso FS, Cappello M, Crispino F, Grova M, Privitera AC, Piccillo G, et al. Vedolizumab may be an effective option for the treatment of postoperative recurrence of Crohn’s disease. Dig Liver Dis. 2022;54(5):629–34.
Sandborn WJ, Gasink C, Gao LL, Blank MA, Johanns J, Guzzo C, et al. Ustekinumab induction and maintenance therapy in refractory Crohn’s disease. N Engl J Med. 2012;367(16):1519–28.
Honap S, Meade S, Ibraheim H, Irving PM, Jones MP, Samaan MA. Effectiveness and safety of ustekinumab in inflammatory bowel disease: a systematic review and meta-analysis. Dig Dis Sci. 2022;67(3):1018–35.
Rubín de Célix C, Chaparro M, Gisbert JP. Real-world evidence of the effectiveness and safety of ustekinumab for the treatment of Crohn's disease: systematic review and meta-analysis of observational studies. J Clin Med. 2022;11(14):4202.
Zundler S, Fischer A, Schillinger D, Binder MT, Atreya R, Rath T, et al. The alpha4beta1 homing pathway is essential for ileal homing of Crohn’s disease effector T Cells in vivo. Inflamm Bowel Dis. 2017;23(3):379–91.
HallouchToutouh S, LázaroSáez M, Hernández MÁ. Ustekinumab for prevention of postoperative recurrence: our clinical experience. Gastroenterol Hepatol. 2021;44(4):296–7.
Buisson A, Nancey S, Manlay L, Rubin DT, Hebuterne X, Pariente B, et al. Ustekinumab is more effective than azathioprine to prevent endoscopic postoperative recurrence in Crohn’s disease. United Eur Gastroenterol J. 2021;9(5):552–60.
Macaluso FS, Grova M, Mocciaro F, Di Mitri R, Privitera AC, Distefano ME, et al. Ustekinumab is a promising option for the treatment of postoperative recurrence of Crohn's disease. J Gastroenterol Hepatol (In press).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author contributions
JP Gisbert wrote the first draft of the manuscript and critically reviewed the final version. M Chaparro complemented draft sections and critically reviewed the final version.
Conflict of interest
Dr Gisbert has served as speaker, consultant, and advisory member for or has received research funding from MSD, Abbvie, Pfizer, Kern Pharma, Biogen, Mylan, Takeda, Janssen, Roche, Sandoz, Celgene/Bristol Myers, Gilead/Galapagos, Lilly, Ferring, Faes Farma, Shire Pharmaceuticals, Dr Falk Pharma, Tillotts Pharma, Chiesi, Casen Fleet, Gebro Pharma, Otsuka Pharmaceutical, Norgine and Vifor Pharma. Dr Chaparro has served as a speaker, or has received research or education funding from MSD, Abbvie, Hospira, Pfizer, Takeda, Janssen, Ferring, Shire Pharmaceuticals, Dr Falk Pharma, Tillotts Pharma, Lilly.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors give their consent to publish this article.
Code availability
Not applicable.
Data availability
No new data are generated.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gisbert, J.P., Chaparro, M. Anti-TNF Agents and New Biological Agents (Vedolizumab and Ustekinumab) in the Prevention and Treatment of Postoperative Recurrence After Surgery in Crohn’s Disease. Drugs 83, 1179–1205 (2023). https://doi.org/10.1007/s40265-023-01916-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01916-2