Abstract
Background
Fatigue is a frequent complaint in patients with inflammatory bowel disease. Biological drugs have demonstrated beneficial effects on some extraintestinal manifestations, but the effect on fatigue is not clear.
Objective
This study investigated the effects of biological and small molecule drugs approved for inflammatory bowel disease on fatigue.
Methods
We performed a systematic review and meta-analysis of randomized, placebo-controlled trials reporting Federal Drug Agency (FDA)-approved biological and small molecule drugs for use in ulcerative colitis and Crohn’s disease in which measures of fatigue were recorded before and after treatment. Only induction studies were included. Maintenance studies were excluded. We searched Embase (Ovid), Medline (Ovid), PsycINFO (Ovid), Cinahl (EBSCOhost), Web of Science Core Collection, Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov in May 2022. Risk of bias was analyzed using the Cochrane risk-of-bias tool. Standardized mean difference was used to measure the treatment effect.
Results
A total of seven randomized controlled trials composed of 3835 patients were included in the meta-analysis. All of the studies included patients with moderately to severely active ulcerative colitis or Crohn’s disease. The studies used three different generic fatigue instruments: the Functional Assessment of Chronic Illness Therapy-Fatigue and the Short Form 36 Health Survey Vitality Subscale versions 1 and 2. Overall treatment with biological or small molecule agents showed a beneficial effect compared with placebo, with a standardized mean difference of 0.25 (95% confidence interval 0.15–0.34, p < 0.001). The effect was independent of type of drug or subtype of inflammatory bowel disease.
Discussion
The risk of bias was considered to be low for all domains except for missing outcome data. Even though the included studies were of high methodological quality, the review is limited by the small number of studies included and that the available studies were not designed to evaluate fatigue specifically.
Conclusion
Biological and small molecule drugs used in inflammatory bowel disease have a consistent, though small, beneficial effect on fatigue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Fatigue is a major extraintestinal complaint in patients with IBD. | |
Biological and small molecule drugs reduce fatigue in inflammatory bowel disease. | |
Fatigue should be assessed in future drug efficacy studies in IBD. |
1 Introduction
Inflammatory bowel disease (IBD) is made up of ulcerative colitis and Crohn’s disease, which are chronic inflammatory diseases in the gastrointestinal tract. Although the etiology is not completely understood, an interplay between genetic and environmental factors in a genetically susceptible host and a dysregulated immune response are regarded as essential elements in the pathogenesis. Many patients also experience a range of manifestations not directly related to the gastrointestinal tract, such as joint pain, erythema nodosum, pyoderma gangrenosum, episcleritis, uveitis, and fatigue. These phenomena frequently have a negative impact on quality of life and can occur independent of disease activity [1]. Treatment of extraintestinal manifestations can be challenging. However, biological agents, such as tumor necrosis factor inhibitors (anti-TNF agents) and integrin receptor antagonists have shown promising results in the treatment of several manifestations outside the gut, including cutaneous lesions and joint pain [2].
Fatigue can be defined as an “overwhelming sense of tiredness, lack of energy, and feeling of exhaustion” [3] and is one of the most frequently reported extraintestinal manifestations in IBD, affecting approximately 50% of newly diagnosed patients [4]. Fatigue is frequent in all chronic inflammatory, malignant, and neurodegenerative diseases and can, from a biological basis, be understood as a major component of the “sickness behavior response”. This response occurs in animals and humans when exposed to pathogens or conditions with bodily harm and is considered an evolutionarily conserved survival mechanism. The sickness behavior response encompasses several orchestrated processes, including fatigue, depression, social withdrawal, lack of grooming, hunger, and thirst [5]. The mechanisms underlying this response involve proinflammatory cytokines and biomolecular activation of cerebral neurons [6,7,8]. In chronic inflammatory conditions, this response is constantly active, leading to chronic fatigue, which manifests as a long-lasting, limiting, and purposeless phenomenon.
Although many patients with IBD report fatigue as their most bothersome complaint, it remains to be used as the primary endpoint in IBD-related drug trials. The reasons for this are probably diverse and include its subjective nature, the need for a commonly accepted fatigue measure, and different opinions on the significance and concept. Traditionally, the outcome measures of IBD studies have been closely related to disease activity or inflammatory measures, such as clinical, endoscopic, or biochemical/biomarker remission and response, as well as mucosal healing. However, there is a growing interest in patient-reported outcome measures (PROMs) in IBD, and quality of life was recently recommended to be included as an endpoint in future treatment studies [9]. In rheumatological diseases, fatigue has been implemented as a core outcome measure in drug trials for the last 15 years [10]. Although this has not generally been the case for drug studies in IBD, fatigue has recently been put forward among the top 10 research questions in IBD [11]. Moreover, an ongoing initiative to develop a core outcome set for trials of IBD strongly encourages sponsors to measure relevant PROMs, including fatigue [12].
No therapeutic strategy has been established for the management of fatigue in IBD. Although biological agents, as well as the emerging small molecule drugs in the form of JAK inhibitors and S1PR modulators, have shown promising antiinflammatory effects, their influence on fatigue severity is not clear.
The effect of biological treatment on quality of life has previously been reviewed in patients with IBD, in whom treatment with infliximab, adalimumab, certolizumab, and natalizumab showed significant improvement compared with placebo [13]. A recent Cochrane review evaluated the efficacy of a range of different interventions on fatigue in IBD, including adalimumab, electroacupuncture, cognitive behavioral therapy, physical activity, and ferric maltol, but no firm conclusions could be made [14].
In the present study, we aimed to investigate the effects of biological and small molecule treatment on fatigue in IBD in general and in disease subtypes, and to assess whether efficacy varies between drug classes. We wanted to look at induction studies to investigate treatment versus no treatment, and excluded maintenance studies because the patient population is usually selected on the basis of previous response to the drug in such studies.
2 Methods
We performed a systematic review and meta-analysis of randomized controlled studies comparing biological or small molecule agents with placebo in which measures of fatigue were recorded before and after treatment. The recommendations of the Preferred Items for Reporting of Systematic Reviews Meta-Analysis (PRISMA) statement were followed [15]. Ethical approval and informed consent were not required for this study, as no patient information was collected and patient treatment was not influenced. The review was not registered, and a protocol was not prepared.
2.1 Eligibility Criteria
All US Food and Drug Administration (FDA)-approved biological or small molecule interventions with an indication for ulcerative colitis and/or Crohn’s disease as of April 2022 were included in this study. These drugs included anti-TNF-α agents (i.e., adalimumab, infliximab, golimumab, and certolizumab pegol), IL-12/23 inhibitor (ustekinumab), anti-integrins (i.e., vedolizumab and natalizumab), JAK inhibitors (i.e., tofacitinib and upadacitinib), and sphingosine-1-phosphate receptor modulator (ozanimod). We included randomized, placebo-controlled trials that had publicly available outcome data for fatigue and used validated fatigue scoring scales. Only studies that compared treatment with placebo were included, and maintenance studies were excluded.
2.2 Search Strategy
A systematic literature search was performed in May 2022 in collaboration with a senior librarian (EHM). We searched the following databases: Embase (Ovid), Medline (Ovid), PsycINFO (Ovid), Cinahl (EBSCOhost), Web of Science Core Collection, Cochrane Central Register of Controlled Trials, and ClinicalTrials.gov. The search strategies consisted of search terms for IBD, including Crohn’s disease and ulcerative colitis, combined with search terms for fatigue, quality of life, and the following biological agents and small molecule agents: adalimumab or infliximab or golimumab or certolizumab pegol or ustekinumab or vedolizumab or natalizumab or tofacitinib or upadacitinib or ozanimod. Relevant controlled subject headings, such as MeSH terms, were included where applicable. We also added search strategies for identifying controlled trials to some of the searches [16,17,18]. Results were limited to the English language. No date limits were applied. The complete search strategies are described in the supplementary material (Supplementary Information 1).
2.3 Data Collection
Two authors (BMS and IMS) independently screened all records. Studies that were not relevant to the review were excluded on the basis of title and abstract. The remaining records were examined for eligibility based on the predefined inclusion criteria. Full-text papers were retrieved for all studies that appeared to meet the inclusion criteria (Fig. 1).
Information was extracted independently from all relevant publications by BMS and ID. If baseline information was not provided in the paper, we used the underlying original publication, supplementary material, or protocol to retrieve this information. The following data were recorded for each study: study design, number of participants, participant age and sex, disease duration, measure of disease activity, C-reactive protein (CRP), subtype of IBD (ulcerative colitis or Crohn’s disease), follow-up time, comparator group, fatigue instrument used, mean score on the fatigue rating scale, number of patients lost to follow-up, and method for handling missing data.
2.4 Fatigue Instruments Used in the Included Studies
Medical Outcomes Study 36-item Short-Form Health Survey (SF-36) is a generic multi-item instrument yielding eight different subscores, including vitality. The vitality subscale (SF-36 vitality) consists of four questions addressing energy and fatigue within the last 4 weeks, yielding scores between 0 and 100, with a higher score indicating less fatigue [19]. The SF-36v2 differs from the original SF-36 vitality in that the final score ranging from 0 to 100 is standardized into norm-based T-scores with a mean of 50 and standard deviation of 10 for the US general population. In addition, the SF-36v2 only addresses the prior week [20]. The Functional Assessment of Chronic Illness Therapy-Fatigue (FACIT-F) is a generic fatigue measure in which 13 items regarding fatigue are graded from 0 to 4, yielding scores between 0 and 52, with higher scores reflecting less fatigue. The FACIT-F addresses fatigue during the last 7 days [21].
2.5 Quality Assessment
A quality assessment was performed using version 2 of the Cochrane risk-of-bias tool for randomized trials [22]. This tool addresses the randomization process, including the concealment of allocation and allocation sequence, the blinding of participants and outcome measures, handling of missing data, risk of bias in measurement of the outcome, and selective reporting. We used information from the included articles and underlying articles [23,24,25,26], as well as from the protocols of two of the studies [26, 27], to perform this assessment. Risk of bias summary table is found in Supplementary Information 2.
2.6 Statistical Analysis
The identified studies used different fatigue scoring scales; therefore, standardized mean differences (SMDs) were applied as scale-free measures of the treatment effect after estimating the “raw” mean differences (MDs) with standard errors (SEs), which was achieved by various approaches according to the data available from the papers.
For most studies [28,29,30], we were able to identify the mean change in SF-36 vitality, the standard deviation (SD) of the change, and number of patients in the treatment and control groups. For these studies, the MD was estimated as the difference in the mean changes, and SE was estimated from the pooled SD of the changes [31]. However, the UNITI-1 and two studies reported by Sands [29] both contained two dosage groups, which were first combined by averaging the means and SDs of the change [32].
For the OCTAVE Induction 1 and 2 trials [33], so-called least squares (LS) mean changes (i.e., marginal mean changes in SF-36 vitality scores after adjusting for baseline SF-36 vitality scores plus other baseline variables) were reported with SEs for each group. The MD was estimated as the difference in LS mean changes. The SE of the MD was estimated conservatively as the square root of the sum of the squared individual SEs, assuming no correlation between the adjusted mean change estimates. These SEs gave Wald p-values that were consistent with the p-values reported by Panés [33].
Ghosh [34] reported observed mean changes in the FACIT-F score for four dosage groups plus placebo, accompanied only by sample sizes and indications of p-values within different thresholds from what is assumedly Wald tests within an ANCOVA including all dosage groups and adjusting for the baseline fatigue score. MDs were estimated as differences in the reported observed mean changes. Approximate SEs for MDs between three dosage groups and placebo were conservatively based on worst case p-values (e.g., for “statistically significant at 0.01 level,” we assumed p = 0.01) and using methods for Wald z-tests [35] while assuming that adjusted differences in the mean change were the same as the observed differences. These SEs ranged from 2.33 to 2.58. For the lowest dose group in comparison with placebo, for which we only know p > 0.1, we assumed an SE of 2.42, which is the average of the SEs for the other group comparisons. We combined the dosage groups by averaging the individual MDs and by estimating the SE for the combined group as the square root of the sum of the individual squared SEs and dividing by the number of SEs (i.e., conservatively assuming independence).
From the studies that reported baseline SDs for SF-36 vitality scores, one study by Dudley–Brown [30] reported SDs of approximately 20, whereas the four studies by Sands and Panés [29, 33] reported SDs of approximately 10. All of these studies were reasonably large, and the most likely explanation for the difference between them was that Sands and Panés applied stricter inclusion criterion than Dudley-Brown, in that the included participants had an inadequate response or intolerance to other therapy. Ghosh [34] used similarly strict inclusion criteria but did not report the baseline SD for FACIT-F. In this situation with likely true differences in variance, the recommendation is to standardize using common, possibly external, estimates of SD [36]. For FACIT-F, Danese et al. [37] reported baseline SDs of 11.3 and 11.7 (average 11.5) for two equally sized groups of 220 patients with moderate-to-severe Crohn’s disease in the STARDUST trial. To match the inclusion criteria of this trial, we used the baseline SDs reported in Dudley–Brown [30] for SF-36 vitality (i.e., 19.4 for n = 259 in the treatment arm and 19.3 for n = 250 in the placebo arm, with a weighted average of 19.4). In summary, to calculate SMDs and accompanying SEs, we divided by an SD of 11.5 for FACIT-F and an SD of 19.4 for SF-36 vitality, giving SMDs that are generalizable to populations with moderate-to-severe IBD.
Given the differences between the studies with regard to the disease population, intervention medications, and dosage schemes, we opted to perform a random effects meta-analysis using the DerSimonian and Laird method [38]. With this method, we assume that the observed treatment effects are a random sample from a distribution of treatment effects with a variance of τ2, the estimate of which is included in the calculation of study weights. Heterogeneity was further assessed using the I2 statistic, which estimates the percentage of between-study heterogeneity attributable to variability in the true treatment effect rather than sampling variation, and tested it using χ2 [38]. With substantial heterogeneity, various subgroup analyses were explored, though without pursuing a full meta-regression due to the small number of studies.
Forest plots of the estimated SMDs and 95% confidence intervals (CIs) were used to visualize the range of effects, with the relative size of the markers indicating the weight of each point estimate in the calculation of the combined estimate. Possible small study effects were illustrated using a funnel plot and tested with the Egger test. Supplementary analyses were performed with within-study dosage groups treated separately while sharing the placebo comparator group. An overall MD based on the studies applying SF-36 vitality as fatigue instrument were estimated. All analyses were performed using Stata v.17.0 functions metan and metafunnel.
2.7 Funding Source
This work was supported by a grant from Stavanger University Hospital. The funding source had no role in the design of the study or in the analyses or interpretation of the data.
3 Results
The literature search was completed in May 2022, and the search identified 1654 records. Of the 1427 records screened, 5 publications reported results from seven randomized controlled trials. These trials were composed of a total of 3835 patients, including 1774 with Crohn’s disease and 2061 with ulcerative colitis, who fulfilled the inclusion criteria (Fig. 1). Baseline characteristics were comparable between studies regarding age and sex. Patients with Crohn’s disease had longer disease duration compared with the patients with ulcerative colitis, and CRP levels were higher in the Crohn’s disease cohort presented by Dudley-Brown et al. [30] The disease activity scores were comparable within patient groups (Table 1). Fatigue measures were performed at baseline and the follow-up visit, which in most studies (6 of 7) was at 8 weeks. An overview of the available data used for estimating effect size and 95% CIs is given in Table 2.
All of the included studies were multicenter, double-blind, randomized, and placebo-controlled studies. Two studies included patients with Crohn’s disease [29, 30], whereas the others included patients with ulcerative colitis [28, 33, 34]. Fatigue was not defined as a primary outcome except for in the conference abstract by Ghosh [34]. The remaining studies assessed quality of life using SF-36 and SF-36v2, and the fatigue data were collected from the reported vitality subscales.
Two of the publications reported data from two separate trials: UNITI-1 and -2 and OCTAVE-1 and -2 [29, 33]. The results from these trials are presented separately in Tables 1 and 2.
3.1 Risk of Bias
All of the studies had a low risk of bias for all quality assessment domains, except for missing outcome data, and were considered to be of high methodological quality. With respect to missing outcome data, two of the studies were deemed as being at low risk of bias [29, 30], whereas the remaining studies had some concerns for risk of bias. Missing follow-up data in the included studies were handled using two different approaches, either by last observation carried forward or by complete case analysis. The lost-to-follow-up numbers were not explicitly stated in the included articles, but were retrieved from the underlying articles, supplementary material, and graphics (Table 2). Overall, the trial is judged to raise some concerns for bias with regard to missing data, but there is not high risk of bias for any domain.
3.2 Treatment Regimens
The biological and small molecule agents tested in the included articles were ustekinumab, infliximab, natalizumab, tofacitinib, and upadacitinib. Treatment regimens for ustekinumab were 130 mg or 6 mg/kg at week 0; for infliximab 5 mg/kg or 10 mg/kg at weeks 0, 2, and 6; for natalizumab 300 mg at weeks 0 and 4; for tofacitinib 10 mg twice daily; and for upadacitinib 7.5 mg, 15 mg, 30 mg, or 45 mg once daily. Relevant data for fatigue in trials of adalimumab, certolizumab pegol, golimumab, vedolizumab, or ozanimod were not available. The following drugs were administered at lower doses than currently recommended: ustekinumab 130 mg and upadacitinib 7.5 mg, 15 mg, and 30 mg.
3.3 Fatigue Scores
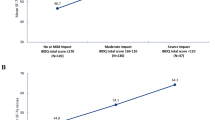
All of the included trials reported significant improvement in fatigue scores compared with placebo. Overall, treatment with biological or small molecule agents compared with placebo led to a small reduction in fatigue with a pooled SMD of 0.25 (95% CI 0.15–0.34, p < 0.001; Table 3, Fig. 2) [39]. Trial SMDs varied between 0.08 [29] and 0.53 [34]. I2 was estimated to be 78.4% (p < 0.001), indicating high heterogeneity in treatment effects [40, 41]. The between-trial variance in SMD was 0.013.
3.4 Subgroup Analysis
Treating ulcerative colitis and Crohn’s disease separately, we found SMDs of 0.18 (95% CI 0.05–0.30, p = 0.005) for Crohn’s disease and 0.30 (95% CI 0.17–0.44, p < 0.001) for ulcerative colitis. However, the test for between-group heterogeneity was not significant (p = 0.17; Table 3, Supplementary Information 3, Fig. S1). Similar subgroup analyses were performed for biological versus small molecule, broad versus narrow inclusion criteria, and SF-36 vitality versus FACIT-F instrument (Table 3 and Supplementary Information 3 Fig. S2–S4). We saw indications of higher SMDs with small molecule agents, broad inclusion (not significant), and a substantially higher effect using FACIT-F compared with SF-36 vitality (SMD 0.53 versus 0.21, p = 0.005). We did a supplementary analysis where the different dosing regimens were presented separately and not combined as in the main analysis (Supplementary Information 3, Fig. S5). For the studies that reported on more than one dose settings, we observed tendencies toward better effect with higher dosages, however, none of these differences were statistically significant. When analyzing lower dose regimens (ustekinumab 130 mg and upadacitinib ≤ 30 mg) versus currently recommended dose regimens (all other drugs and doses) no difference was revealed between the groups (p = 0.89) (Supplementary Information 3, Fig. S6). None of the studies involving different dosage groups [28, 29, 34] reported statistically significant differences between these groups. On the basis of the data presented, Feagan [28] had a statistical power of 31% for detecting a difference in changes between dosage groups of 3 points (i.e., MID of SF-36 vitality [42]) on a two-sided 5% significance level. Sands [29] had a power of 94% (UNITI-1) and 81% (UNITI-2) for detecting the same differences. Comparing two dosage groups of n = 48, as in Ghosh [34], would yield statistical power of 27–44% for differences of MID 3–4 points [43]. Apart from the Ghosh findings [34], only slight (non-clinically important) differences were seen between dosage groups.
The funnel plot showed a substantial small study effect (p = 0.005) with smaller studies reporting larger effects (Supplementary Information 3, Fig. S7) [44]. In the smallest study, three of the drug regimens used were lower than currently recommended (7.5 mg, 15 mg, and 30 mg upadacitinib) [34]. The study was the main outlier, and the only study applying FACIT-F as the fatigue instrument.
By including only the studies that used SF-36 vitality as fatigue instrument, we found a MD of 4.0 (95% CI 2.4–5.7) (Supplementary Information 3, Fig. S8).
4 Discussion
In this study, we provide an overview of the effects of biological and small molecule drugs on fatigue in patients with IBD. The meta-analysis including seven randomized controlled trials revealed a small, but consistent, reducing effect on fatigue compared to placebo. For SF-36 vitality we found a MD of 4.0, which slightly exceeds the previously published “minimally important differences” threshold of 3 [42], indicating that the difference is clinically meaningful.
When separating patients according to diagnosis (ulcerative colitis and Crohn’s disease groups), there was a similarly significant reduction in fatigue severity in both groups. A tendency toward a better effect in the ulcerative colitis group appeared, though this difference did not reach statistical significance. Moreover, when comparing the effects on fatigue of biological versus small molecule agents, no significant differences were seen. This finding in IBD overall, as well as in the ulcerative colitis and Crohn’s disease groups, is in agreement with other meta-analyses of the effect of biological drug treatment regimens on fatigue in patients with rheumatoid arthritis and psoriasis [45, 46].
The mechanisms underlying the beneficial effects of these drugs on fatigue are not fully understood but are likely due to reduced production of proinflammatory cytokines and a lessened central-nervous-system-driven sickness behavior response. Inhibition of IL-1β improves fatigue in both animals and humans and provides good evidence of how this cytokine is important [47,48,49,50,51]. However, other factors also influence fatigue. Notably, even with the most optimal treatment with biological agents in rheumatoid arthritis and IBD, fatigue persists in many patients who achieve remission [52, 53]. This indicates that other pathways are involved in the generation of fatigue, and two factors that are always associated with fatigue are pain and depression [54]. Therefore, fewer intestinal symptoms and less concern in IBD patients in remission could also be a factor that contributes to reduced fatigue.
The influence of disease activity on fatigue is a frequent topic of discussion. Some studies have reported an association between disease activity and fatigue, but studies employing generic and unidimensional fatigue instruments fail to confirm such a relationship [4, 55, 56]. Nevertheless, the consistent beneficial effect from biological and small molecule drugs on fatigue is an important aspect to consider in patients with IBD. The included studies were quite homogenous when it comes to study population, and we believe the inflammatory burden (assessed as moderate-to-severe disease activity in all study participants) is comparable across studies.
Aerobic exercise and cognitive behavioral therapy are other options for treatment of fatigue and have been reported to have beneficial effects across many diseases [57, 58]. However, this is beyond the scope of this article.
The most frequently used instrument to measure quality of life in IBD is the Inflammatory Bowel Disease Questionnaire (IBDQ). The IBDQ contains two questions regarding fatigue/energy loss, but the results from these questions are usually not reported separately; they are combined into a “systemic symptoms” score together with the assessment of sleep quality and whether patients feel “generally unwell” [59, 60]. Therefore, it is not regarded as a valid fatigue measure. Moreover, disease-specific fatigue instruments may record elements of disease activity that could lead to false associations between fatigue and disease activity.
Most pharmacological IBD studies do not employ fatigue as one of the primary outcomes, however, SF-36 is a generic measure of quality of life and has been used in many IBD studies. The SF-36 vitality subscale is a unidimensional, generic fatigue measure, and even though previous IBD studies have primarily applied SF-36 as a quality of life measure, the SF-36 vitality subscale is regarded as a valid fatigue measure. However, in most of the studies, only the combined mental component summary and physical component summary were reported, implying that even though researchers used an instrument suitable in assessing fatigue, these results were generally not retrieved and presented. In articles that used SF-36, we searched for further results at ClinicalTrials.gov but could not retrieve any additional information regarding the subscores.
The included studies differed from those in a recent Cochrane review on interventions for fatigue in IBD, as fatigue had to be explicitly stated in the aims, content, or as a primary or secondary endpoint for the study to be eligible [14]. Thus, only one biological treatment regimen, maintenance therapy with TNFα-inhibitor adalimumab, was evaluated, indicating a reduction of fatigue. In the current study, we chose to evaluate the effects of treatment versus no treatment on fatigue in induction studies, excluding reports involving maintenance therapy [37, 61,62,63].
Some of the identified reports had insufficient or incomplete data on fatigue and were excluded from this review. One of these was a crossover study in which the participants received placebo for 2 weeks before switching to infliximab. Because fatigue scores had not returned to baseline before commencing infliximab treatment, we excluded this study [64]. Another study evaluated the meaningfulness of improvements in health-related quality of life using the SF-36 questionnaire but did not present the actual fatigue data [65]. One study presented IBDQ subscores but only in graphics [66]. One study presented the same patient population as in the Ghosh abstract [34] but used a non-validated subscore of the Ulcerative Colitis Symptoms Questionnaire [67].
All studies included in this review used biological agents approved by the FDA for treatment of IBD as of April 2022. Notably, there were no studies matching our inclusion criteria reporting fatigue data for adalimumab, certolizumab pegol, golimumab, vedolizumab, or ozanimod. There was a tendency toward a better effect of small molecule drugs compared with biological drugs, though this did not reach statistical significance. Disease entity may be a confounder in this analysis, as small molecule agents approved by the FDA are currently only recommended in ulcerative colitis. We found a difference in the SMD when comparing fatigue instruments; FACIT-F demonstrated a higher effect, but only one of the studies used the FACIT-F score, which must be taken into consideration.
Some of the studies reported different dosage regimens. When doing analysis separated by dose there was no significant difference between higher versus lower doses. Defining each dosage as “recommended” or “lower dose than currently recommended,” we were able to combine the studies. However, whereas the statistical power was thus increased, the potential impact of confounding factors was also very much so. Due to the small number of studies and the lack of power for detecting differences between different dosage groups, as well as confounding factors (disease type, different fatigue instruments, number of patients), it is difficult to draw any firm conclusion regarding effect of different doses.
The strengths of this study are that we performed an extensive literature search using a systematic approach in the selection of relevant articles, and that the identified and included articles were of high methodological quality with a low risk of bias. The limitations of this review are the small number of studies included, and we were not able to make adjusted comparisons (e.g., difference between small molecule drugs and biological drugs after accounting for differences in the disease population, inclusion criteria, and fatigue instrument). The studies were not designed to evaluate fatigue specifically, though all of the studies had a change in quality of life as a prespecified secondary or tertiary outcome measure, and SF-36 vitality serves as a good, generic, unidimensional fatigue instrument. We only evaluated the effects from induction therapy, and the long-term effect of biological treatment on fatigue in IBD is unknown and should be evaluated in future studies. The asymmetry in the funnel plot implies a possible overestimation of the overall effect, as small studies with small or negative results seem underreported. On the contrary, heterogeneity between studies is also a possible explanation, though our rather small sample of studies prevented a thorough investigation of the heterogeneity. We did, however, observe a significantly larger effect for FACIT-F in the subgroup analysis of SF-36 vitality versus FACIT-F, which could indicate that FACIT-F is not directly comparable to SF-36 vitality, despite standardization.
5 Conclusion
The biological and small molecule drugs investigated in this review have a small effect in reducing fatigue in patients with ulcerative colitis and Crohn’s disease. As fatigue is of great importance to both patients and society, it should be addressed in future studies of drug effects in IBD.
References
Rogler G, Singh A, Kavanaugh A, Rubin DT. Extraintestinal manifestations of inflammatory bowel disease: current concepts, treatment, and implications for disease management. Gastroenterology. 2021;161(4):1118–32.
Greuter T, Rieder F, Kucharzik T, Peyrin-Biroulet L, Schoepfer AM, Rubin DT, et al. Emerging treatment options for extraintestinal manifestations in IBD. Gut. 2021;70(4):796–802.
Krupp LB, Pollina DA. Mechanisms and management of fatigue in progressive neurological disorders. Curr Opin Neurol. 1996;9(6):456–60.
Grimstad T, Norheim KB, Isaksen K, Leitao K, Hetta AK, Carlsen A, et al. Fatigue in newly diagnosed inflammatory bowel disease. J Crohns Colitis. 2015;9(9):725.
Hart BL. Biological basis of the behavior of sick animals. Neurosci Biobehav Rev. 1988;12(2):123–37.
Dantzer R, Heijnen CJ, Kavelaars A, Laye S, Capuron L. The neuroimmune basis of fatigue. Trends Neurosci. 2014;37(1):39–46.
Ilanges A, Shiao R, Shaked J, Luo J-D, Yu X, Friedman JM. Brainstem ADCYAP1+ neurons control multiple aspects of sickness behaviour. Nature. 2022;609(7928):761–71.
Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46–56.
Turner D, Ricciuto A, Lewis A, D’Amico F, Dhaliwal J, Griffiths AM, et al. STRIDE-II: an update on the selecting therapeutic targets in inflammatory bowel disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology. 2021;160(5):1570–83.
Kirwan JR, Minnock P, Adebajo A, Bresnihan B, Choy E, de Wit M, et al. Patient perspective: fatigue as a recommended patient centered outcome measure in rheumatoid arthritis. J Rheumatol. 2007;34(5):1174–7.
Hart AL, Lomer M, Verjee A, Kemp K, Faiz O, Daly A, et al. What are the top 10 research questions in the treatment of inflammatory bowel disease? A priority setting partnership with the James Lind Alliance. J Crohns Colitis. 2017;11(2):204–11.
Ma C, Hanzel J, Panaccione R, Sandborn WJ, D'Haens GR, Ahuja V, et al. CORE-IBD: A Multidisciplinary International Consensus Initiative to develop a core outcome set for randomized controlled trials in inflammatory bowel disease. Gastroenterology. 2022.
Vogelaar L, Spijker AV, van der Woude CJ. The impact of biologics on health-related quality of life in patients with inflammatory bowel disease. Clin Exp Gastroenterol. 2009;2:101–9.
Farrell D, Artom M, Czuber-Dochan W, Jelsness-Jørgensen LP, Norton C, Savage E. Interventions for fatigue in inflammatory bowel disease. Cochrane Database Syst Rev. 2020;4(4): CD012005.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clin Res Ed). 2021;29(372): n71.
Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. www.training.cochrane.org/handbook: Cochrane; 2021.
Lefebvre C, Glanville J, Briscoe S, Featherstone R, Littlewood A, Marshall C, et al. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. www.training.cochrane.org/handbook: Cochrane; 2022.
Glanville J, Dooley G, Wisniewski S, Foxlee R, Noel-Storr A. Development of a search filter to identify reports of controlled clinical trials within CINAHL Plus. Health Info Libr J. 2019;36(1):73–90.
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. 1993.
Maruish M, Kosinski M, Bjorner J, Gandek B, Turner-Bowker D, Ware J. User’s manual for the SF-36v2® health survey, 3rd ed. QualityMetric Inc; 2011.
Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manag. 1997;13(2):63–74.
Higgins J, Savović J, Page M, Elbers R, Sterne J. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. Cochrane handbook for systematic reviews of interventions version 63 (Updated february 2022). www.training.cochrane.org/handbook: Cochrane; 2022.
Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, Johanns J, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353(23):2462–76.
Targan SR, Feagan BG, Fedorak RN, Lashner BA, Panaccione R, Present DH, et al. Natalizumab for the treatment of active Crohn’s disease: results of the ENCORE Trial. Gastroenterology. 2007;132(5):1672–83.
Sandborn WJ, Ghosh S, Panes J, Schreiber S, D’Haens G, Tanida S, et al. Efficacy of upadacitinib in a randomized trial of patients with active ulcerative colitis. Gastroenterology. 2020;158(8):2139-49.e14.
Feagan BG, Sandborn WJ, Gasink C, Jacobstein D, Lang Y, Friedman JR, et al. Ustekinumab as induction and maintenance therapy for Crohn’s disease. N Engl J Med. 2016;375(20):1946–60.
Sandborn WJ, Su C, Sands BE, D’Haens GR, Vermeire S, Schreiber S, et al. Tofacitinib as induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2017;376(18):1723–36.
Feagan BG, Reinisch W, Rutgeerts P, Sandborn WJ, Yan S, Eisenberg D, et al. The effects of infliximab therapy on health-related quality of life in ulcerative colitis patients. Am J Gastroenterol. 2007;102(4):794–802.
Sands BE, Han C, Gasink C, Jacobstein D, Szapary P, Gao LL, et al. The effects of ustekinumab on health-related quality of life in patients with moderate to severe Crohn’s disease. J Crohns Colitis. 2018;12(8):883–95.
Dudley-Brown S, Nag A, Cullinan C, Ayers M, Hass S, Panjabi S. Health-related quality-of-life evaluation of crohn disease patients after receiving natalizumab therapy. Gastroenterol Nurs. 2009;32(5):327–39.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Wiley; 2009.
Higgins J, Li T, Deeks J. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane, 2021, Section 6.5.2.10. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. Available from https://training.cochrane.org/handbook.
Panés J, Vermeire S, Lindsay JO, Sands BE, Su C, Friedman G, et al. Tofacitinib in patients with ulcerative colitis: health-related quality of life in phase 3 randomised controlled induction and maintenance studies. J Crohns Colitis. 2018;12(2):145–56.
Ghosh S, Colombel J-F, Vermeire S, Lee S D, Lee W-J, Zhou W, et al. Improved patient-reported outcomes with upadacitinib as an induction therapy for patients with ulcerative colitis: data from u-achieve. UEG Week 2018. Vienne, Austria; 2018.
Higgins J, Li T, Deeks J. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane, 2021, Section 6.5.2.3. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. https://training.cochrane.org/handbook.
Higgins J, Li T, Deeks J. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane, 2021, Section 6.5.1.2. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. https://training.cochrane.org/handbook.
Danese S, Vermeire S, D’Haens G, Panés J, Dignass A, Magro F, et al. P301 Ustekinumab improves health-related quality of life in patients with moderate-to-severe Crohn’s disease: results up to Week 48 of the STARDUST trial. J Crohn’s Colitis. 2021;15(Supplement 1):S330–1.
Bradburn M, Deeks J, Altman D. Metan—an alternative meta-analysis command. Stata Tech Bull. 1999;8.
Sullivan GM, Feinn R. Using effect size-or why the P value is not enough. J Grad Med Educ. 2012;4(3):279–82.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clin Res Ed). 2003;327(7414):557–60.
Harris RJ, Deeks JJ, Altman DG, Bradburn MJ, Harbord RM, Sterne JAC. Metan: fixed- and random-effects meta-analysis. Stand Genom Sci. 2008;8(1):3–28.
Blum SI, Tourkodimitris S, Ruth A. Evaluation of functional health and well-being in patients receiving levomilnacipran ER for the treatment of major depressive disorder. J Affect Disord. 2015;1(170):230–6.
Cella D, Yount S, Sorensen M, Chartash E, Sengupta N, Grober J. Validation of the functional assessment of chronic illness therapy fatigue scale relative to other instrumentation in patients with rheumatoid arthritis. J Rheumatol. 2005;32(5):811–9.
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ (Clin Res Ed). 2011;22(343): d4002.
Skoie IM, Dalen I, Omdal R. Effect of biological treatment on fatigue in psoriasis: a systematic review and meta-analysis. Am J Clin Dermatol. 2019;20(4):493–502.
Almeida C, Choy EH, Hewlett S, Kirwan JR, Cramp F, Chalder T, et al. Biologic interventions for fatigue in rheumatoid arthritis. Cochrane Database Syst Rev. 2016;2016(6): CD008334.
Omdal R, Gunnarsson R. The effect of interleukin-1 blockade on fatigue in rheumatoid arthritis—a pilot study. Rheumatol Int. 2005;25(6):481–4.
Cavelti-Weder C, Furrer R, Keller C, Babians-Brunner A, Solinger AM, Gast H, et al. Inhibition of IL-1beta improves fatigue in type 2 diabetes. Diabetes Care. 2011;34(10): e158.
Norheim KB, Harboe E, Gøransson LG, Omdal R. Interleukin-1 inhibition and fatigue in primary Sjögren’s syndrome—a double blind, randomised clinical trial. PLoS ONE. 2012;7(1): e30123.
Huang Y, Smith DE, Ibáñez-Sandoval O, Sims JE, Friedman WJ. Neuron-specific effects of interleukin-1β are mediated by a novel isoform of the IL-1 receptor accessory protein. J Neurosci. 2011;31(49):18048–59.
Qian J, Zhu L, Li Q, Belevych N, Chen Q, Zhao F, et al. Interleukin-1R3 mediates interleukin-1-induced potassium current increase through fast activation of Akt kinase. Proc Natl Acad Sci USA. 2012;109(30):12189–94.
Walter MJM, Kuijper TM, Hazes JMW, Weel AE, Luime JJ. Fatigue in early, intensively treated and tight-controlled rheumatoid arthritis patients is frequent and persistent: a prospective study. Rheumatol Int. 2018;38(9):1643–50.
Villoria A, Garcia V, Dosal A, Moreno L, Montserrat A, Figuerola A, et al. Fatigue in out-patients with inflammatory bowel disease: prevalence and predictive factors. PLoS ONE. 2017;12(7): e0181435.
Omdal R, Mellgren SI, Norheim KB. Pain and fatigue in primary Sjögren’s syndrome. Rheumatology. 2019.
Bager P, Befrits R, Wikman O, Lindgren S, Moum B, Hjortswang H, et al. Fatigue in out-patients with inflammatory bowel disease is common and multifactorial. Alimentary Pharmacol Ther. 2012;35(1):133–41.
Römkens TE, van Vugt-van Pinxteren MW, Nagengast FM, van Oijen MG, de Jong DJ. High prevalence of fatigue in inflammatory bowel disease: a case control study. J Crohns Colitis. 2011;5(4):332–7.
van Erp LW, Roosenboom B, Komdeur P, Dijkstra-Heida W, Wisse J, Horjus Talabur Horje CS, et al. Improvement of fatigue and quality of life in patients with quiescent inflammatory bowel disease following a personalized exercise program. Dig Dis Sci. 2021;66(2):597–604.
Vogelaar L, van’t Spijker A, Timman R, van Tilburg AJ, Bac D, Vogelaar T, et al. Fatigue management in patients with IBD: a randomised controlled trial. Gut. 2014;63(6):911–8.
Guyatt G, Mitchell A, Irvine EJ, Singer J, Williams N, Goodacre R, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96(3):804–10.
Irvine EJ. Development and subsequent refinement of the inflammatory bowel disease questionnaire: a quality-of-life instrument for adult patients with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 1999;28(4):S23–7.
Feagan BG, Coteur G, Tan S, Keininger DL, Schreiber S. Clinically meaningful improvement in health-related quality of life in a randomized controlled trial of certolizumab pegol maintenance therapy for Crohn’s disease. Am J Gastroenterol. 2009;104(8):1976–83.
Loftus EV, Feagan BG, Colombel JF, Rubin DT, Wu EQ, Yu AP, et al. Effects of adalimumab maintenance therapy on health-related quality of life of patients with Crohn’s disease: patient-reported outcomes of the CHARM trial. Am J Gastroenterol. 2008;103(12):3132–41.
Feagan BG, Sandborn WJ, Hass S, Niecko T, White J. Health-related quality of life during natalizumab maintenance therapy for Crohn’s disease. Am J Gastroenterol. 2007;102(12):2737–46.
Minderhoud IM, Samsom M, Oldenburg B. Crohn’s disease, fatigue, and infliximab: is there a role for cytokines in the pathogenesis of fatigue? World J Gastroenterol. 2007;13(14):2089–93.
Coteur G, Feagan B, Keininger DL, Kosinski M. Evaluation of the meaningfulness of health-related quality of life improvements as assessed by the SF-36 and the EQ-5D VAS in patients with active Crohn’s disease. Aliment Pharmacol Ther. 2009;29(9):1032–41.
Rubin DT, Tudor D, Khalid JM, Patel H. P570 Improvements in subcomponents of the inflammatory bowel disease questionnaire in patients treated with vedolizumab: results from GEMINI trial data. J Crohn’s Colitis. 2018;12(supplement 1):S394–5.
Ghosh S, Aberra F, Cross R, Zhou W, Chen N, Lee W-J, et al. P296 Effect of upadacitinib on patient-reported symptoms by the new Ulcerative Colitis Symptoms Questionnaire (UC-SQ) in patients with moderate to severe ulcerative colitis: data from the Phase 2b study U-ACHIEVE. J Crohn’s Colitis. 2019;13(Supplement 1):S247–8.
Acknowledgements
The authors thank senior librarian Elisabeth Hundstad Molland at the Stavanger University Library for providing expert help with the systematic literature search.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Conflicts of interest
IMS has served as a speaker for AbbVie and Pfizer and advisory board member for Novartis, Eli-Lilly, Janssen, AbbVie, and Pfizer. TG has served as a speaker for Ferring Pharmaceuticals, Takeda, and advisory board member for Takeda, Janssen-Cilag, and Tillotts Pharma. RO has served as a speaker for Swedish Orphan Biovitrum and Novartis Norway. BMS and ID declare that they have no conflicts of interest.
Availability of data and materials
All data used to perform this meta-analysis are publicly available. There are no disclosures to report.
Funding
Open access funding provided by University of Bergen (incl Haukeland University Hospital). This article was supported by a grant from Stavanger University Hospital.
Authors contributions
BMS was responsible for data collection, performing the analysis, and writing the paper. IMS was responsible for data collection and writing the paper. ID was responsible for performing the analysis and writing the paper. TG was responsible for writing the paper. RO conceived the study and wrote the paper.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Skjellerudsveen, B.M., Skoie, I.M., Dalen, I. et al. The Effect of Biological Treatment on Fatigue in Inflammatory Bowel Disease: A Systematic Review and Meta-analysis. Drugs 83, 909–921 (2023). https://doi.org/10.1007/s40265-023-01888-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01888-3