Abstract
Background
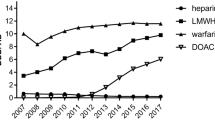
Direct oral anticoagulants (DOACs) have been increasingly utilised over warfarin. However, little is known about the relative consumption trends and costs of each DOAC at the global level.
Methods
An ecological study using pharmaceutical sales data from IQVIA-MIDAS database was used to estimate consumption and cost of individual DOACs in 65 countries from 2008 to 2019. Consumption was estimated from the volume of DOACs sold, expressed as defined-daily-dose/1000-inhabitants/day (DDDTID). Compound and absolute annual growth rates were reported to quantify consumption changes over time. Costs were estimated as manufacturer price per day-of-therapy.
Results
Global consumption of dabigatran, rivaroxaban, apixaban and edoxaban were 0.31, 1.05, 1.08 and 0.78 DDDTID, respectively, in Q2–2019, compared to 0.23, 0.54, 0.21 and 0.03 in Q2–2015, with highest consumption in Western Europe, Northern Europe and Oceania (18.2, 14.07, 13.14 DDDTID). In most countries (46/65, 70%), rivaroxaban contributed to most DOAC consumption (35%–100%), whereas dabigatran accounted for less than one-third. Edoxaban accounted for < 20% of the total in Northern America and Europe but contributed significant proportions in Japan (28.58%) and South Korea (31.37%). Longer median time-to-adoption from FDA approval for apixaban and edoxaban was observed. Costs of all DOACs were ~2–4 times higher in the USA, Puerto Rico and Thailand than in other countries.
Conclusions
Regional differences exist in consumption pattern and trends of individual DOACs over the past decade. Consumption of rivaroxaban and apixaban overtook dabigatran in most countries, whereas use of edoxaban remains limited except in East Asian countries. The USA pays higher prices for DOACs than other countries.










Similar content being viewed by others
References
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51. https://doi.org/10.1056/NEJMoa0905561.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91. https://doi.org/10.1056/NEJMoa1009638.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92. https://doi.org/10.1056/NEJMoa1107039.
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104. https://doi.org/10.1056/NEJMoa1310907.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. 2019;140(2):e125–51.
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS): The task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. Published online 2020.
Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543–603. https://doi.org/10.1093/eurheartj/ehz405.
Zhu J, Alexander GC, Nazarian S, Segal JB, Wu AW. Trends and variation in oral anticoagulant choice in patients with atrial fibrillation, 2010–2017. Pharmacotherapy. 2018;38(9):907–20. https://doi.org/10.1002/phar.2158.
Perreault S, de Denus S, White-Guay B, et al. Oral anticoagulant prescription trends, profile use, and determinants of adherence in patients with atrial fibrillation. Pharmacotherapy. 2020;40(1):40–54. https://doi.org/10.1002/phar.2350.
Weitz JI, Semchuk W, Turpie AG, et al. Trends in prescribing oral anticoagulants in Canada, 2008–2014. Clin Ther. 2015;37(11):2506-2514.e4. https://doi.org/10.1016/j.clinthera.2015.09.008.
Loo SY, Dell’Aniello S, Huiart L, Renoux C. Trends in the prescription of novel oral anticoagulants in UK primary care. Br J Clin Pharmacol. 2017;83(9):2096–106. https://doi.org/10.1111/bcp.13299.
Staerk L, Fosbøl EL, Gadsbøll K, et al. Non-vitamin k antagonist oral anticoagulation usage according to age among patients with atrial fibrillation: temporal trends 2011–2015 in Denmark. Sci Rep. 2016;6:31477. https://doi.org/10.1038/srep31477.
Hanemaaijer S, Sodihardjo F, Horikx A, et al. Trends in antithrombotic drug use and adherence to non-vitamin k oral anticoagulants in the Netherlands. Int J Clin Pharm. 2015;37(6):1128–35. https://doi.org/10.1007/s11096-015-0174-4.
Rodríguez-Bernal CL, Hurtado I, García-Sempere A, Peiró S, Sanfélix-Gimeno G. Oral anticoagulants initiation in patients with atrial fibrillation: real-world data from a population-based cohort. Front Pharmacol. 2017;8:63. https://doi.org/10.3389/fphar.2017.00063.
Baker D, Wilsmore B, Narasimhan S. Adoption of direct oral anticoagulants for stroke prevention in atrial fibrillation. Intern Med J. 2016;46(7):792–7. https://doi.org/10.1111/imj.13088.
Yu Z, Yu L, Shan C. Trends of ambulatory oral anticoagulant prescription in five major cities of china, 2012–2017. BMC Health Serv Res. 2020;20(1):209. https://doi.org/10.1186/s12913-020-5072-3.
Elewa H, Alhaddad A, Al-Rawi S, Nounou A, Mahmoud H, Singh R. Trends in oral anticoagulant use in Qatar: a 5-year experience. J Thromb Thrombolysis. 2017;43(3):411–6. https://doi.org/10.1007/s11239-017-1474-4.
IQVIA. ACTS: IQVIA quality assurance. Published online 2018. https://www.iqvia.com/landing/acts. Accessed 1 Nov 2020
Ju C, Wei L, Man KKC, Wang Z, Ma TT, Chan AYL, Brauer R, Chui CSL, Chan EW, Jani YH, Hsia Y, Wong ICK, Lau WCY. Global, regional, and national trends in opioid analgesic consumption from 2015 to 2019: a longitudinal study. Lancet Public Health. 2022;7(4):e335–46.
Brauer R, Alfageh B, Blais JE, Chan EW, Chui CSL, Hayes JF, Man KKC, Lau WCY, Yan VKC, Beykloo MY, Wang Z, Wei L, Wong ICK. Psychotropic medicine consumption in 65 countries and regions, 2008–19: a longitudinal study. Lancet Psychiatry. 2021;8(12):1071–82.
United Nations. World population prospects 2019. Published online 2019. https://population.un.org/wpp/. Accessed 1 Nov 2020.
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) results. Published online 2020. http://ghdx.healthdata.org/gbd-results-tool. Accessed 1 Nov 2020.
World Bank. World Bank Open Data. Published online 2019. https://data.worldbank.org/. Accessed 1 Nov 2020.
World Bank. World Bank Country and Lending Groups. Published online 2018. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 1 Nov 2020.
Barnes GD, Lucas E, Alexander GC, Goldberger ZD. National trends in ambulatory oral anticoagulant use. Am J Med. 2015;128(12):1300-5.e2. https://doi.org/10.1016/j.amjmed.2015.05.044.
Desai NR, Krumme AA, Schneeweiss S, et al. Patterns of initiation of oral anticoagulants in patients with atrial fibrillation-quality and cost implications. Am J Med. 2014;127(11):1075-1082.e1. https://doi.org/10.1016/j.amjmed.2014.05.013.
Lauffenburger JC, Farley JF, Gehi AK, Rhoney DH, Brookhart MA, Fang G. Factors driving anticoagulant selection in patients with atrial fibrillation in the united states. Am J Cardiol. 2015;115(8):1095–101. https://doi.org/10.1016/j.amjcard.2015.01.539.
Xu Y, Holbrook AM, Simpson CS, Dowlatshahi D, Johnson AP. Prescribing patterns of novel oral anticoagulants following regulatory approval for atrial fibrillation in Ontario, Canada: a population-based descriptive analysis. CMAJ Open. 2013;1(3):E115–9. https://doi.org/10.9778/cmajo.20130032.
Lippi G, Mattiuzzi C, Cervellin G, Favaloro EJ. Direct oral anticoagulants: analysis of worldwide use and popularity using google trends. Ann Transl Med. 2017;5(16):322–322. https://doi.org/10.21037/atm.2017.06.65.
Conen D. Epidemiology of atrial fibrillation. Eur Heart J. 2018;39(16):1323–4. https://doi.org/10.1093/eurheartj/ehy171.
Schnabel RB, Yin X, Gona P, et al. 50-year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham heart study: a cohort study. Lancet. 2015;386(9989):154–62. https://doi.org/10.1016/s0140-6736(14)61774-8.
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. Circulation. 2014;130(23):e199–267. https://doi.org/10.1161/CIR.0000000000000041.
Drug Administration USF &. Drugs@FDA: FDA-approved drugs. Published online 2020. https://www.accessdata.fda.gov/scripts/cder/daf/. Accessed 1 Nov 2020.
Wann LS, Curtis AB, Ellenbogen KA, et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (update on dabigatran). Circulation. 2011;123(10):1144–50. https://doi.org/10.1161/CIR.0b013e31820f14c0.
Wolfe Z, Khan SU, Nasir F, Raghu Subramanian C, Lash B. A systematic review and Bayesian network meta-analysis of risk of intracranial hemorrhage with direct oral anticoagulants. J Thromb Haemost. 2018;16(7):1296–306. https://doi.org/10.1111/jth.14131.
Ray WA, Chung CP, Murray KT, et al. Association of oral anticoagulants and proton pump inhibitor cotherapy with hospitalization for upper gastrointestinal tract bleeding. JAMA. 2018;320(21):2221–30. https://doi.org/10.1001/jama.2018.17242.
Laliberté F, Bookhart BK, Nelson WW, et al. Impact of once-daily versus twice-daily dosing frequency on adherence to chronic medications among patients with venous thromboembolism. Patient. 2013;6(3):213–24. https://doi.org/10.1007/s40271-013-0020-5.
Chan EW, Lau WC, Leung WK, Mok MT, He Y, Tong TS, Wong IC. Prevention of dabigatran-related gastrointestinal bleeding with gastroprotective agents: a population-based study. Gastroenterology. 2015;149(3):586–95 (e3).
Zhang Y, Méndez SJ, Scott A. Factors affecting general practitioners’ decisions to adopt new prescription drugs—cohort analyses using Australian longitudinal physician survey data. BMC Health Serv Res. 2019;19(1):94. https://doi.org/10.1186/s12913-019-3889-4.
Son K-B. The speed of adoption of new drugs and prescription volume after the amendments in reimbursement coverage: the case of non-vitamin k antagonist oral anticoagulants in South Korea. BMC Public Health. 2020;20(1):797. https://doi.org/10.1186/s12889-020-08929-6.
Emanuel EJ, Zhang C, Glickman A, Gudbranson E, DiMagno SSP, Urwin JW. Drug reimbursement regulation in 6 peer countries. JAMA Intern Med. 2020. https://doi.org/10.1001/jamainternmed.2020.4793.
Kesselheim AS, Avorn J, Sarpatwari A. The high cost of prescription drugs in the United States: origins and prospects for reform. JAMA. 2016;316(8):858–71. https://doi.org/10.1001/jama.2016.11237.
Kanavos P, Ferrario A, Vandoros S, Anderson GF. Higher US branded drug prices and spending compared to other countries may stem partly from quick uptake of new drugs. Health Aff (Millwood). 2013;32(4):753–61. https://doi.org/10.1377/hlthaff.2012.0920.
Ng SS, Nathisuwan S, Phrommintikul A, Chaiyakunapruk N. Cost-effectiveness of warfarin care bundles and novel oral anticoagulants for stroke prevention in patients with atrial fibrillation in Thailand. Thromb Res. 2020;185:63–71. https://doi.org/10.1016/j.thromres.2019.11.012.
Government of the People’s Republic of China. National basic medical insurance, work injury insurance and maternity insurance drug list (2020). Published online 2020. http://www.mohrss.gov.cn/xxgk2020/fdzdgknr/shbx_4216/gsbx/202101/t20210112_407492.html
Yan VKC, Blais JE, Li X, et al. Trends in cardiovascular medicine use in 65 middle- and high-income countries. J Am Coll Cardiol. 2020;77(7):1021–3. https://doi.org/10.1016/j.jacc.2020.12.025.
Acknowledgements
We thank Salman Rizvi and Ashwin Oberoi from IQVIA for their assistance and information regarding the use of IQVIA-MIDAS data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported through internal seed funding from the Li Ka Shing Faculty of Medicine, The University of Hong Kong.
Conflict of interest
ICKW reports personal fees and non-financial support from IQVIA, outside the submitted work. EWC has received honorarium from the Hospital Authority, research grants from Narcotics Division of the Security Bureau of HKSAR, National Health and Medical Research Council (NHMRC, Australia), National Natural Science Foundation of China (NSFC), Research Fund Secretariat of the Food and Health Bureau (HMRF, HKSAR), Research Grants Council (RGC, HKSAR), Amgen, AstraZeneca, Bayer, Bristol-Myers Squibb, Janssen, Novartis, Pfizer, RGA and Takeda outside the submitted work. All other authors declare no competing interests.
Ethics approval
This study was exempt from ethics approval by the Institutional Review Board of The University of Hong Kong and the Hong Kong West Cluster of the Hospital Authority.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability
Source data was obtained under license from IQVIA: IQVIA-MIDAS monthly sales data, 2008–2018; all rights reserved. The aggregated datasets generated and analysed during the current study will be available from the corresponding author upon request.
Code availability
Not applicable.
Authors’ contributions
EWC, ICKW, and VKCY conceptualised the study. EWC and IWCK provided resources, supervised the study, and acquired the data. VKCY conducted the formal analysis and wrote the original draft. All authors read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, V.K.C., Li, HL., Wei, L. et al. Evolving Trends in Consumption of Direct Oral Anticoagulants in 65 Countries/Regions from 2008 to 2019. Drugs 83, 315–340 (2023). https://doi.org/10.1007/s40265-023-01837-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-023-01837-0