Abstract
Around 20% of the American population have chronic pain and estimates in other Western countries report similar numbers. This represents a major challenge for global health care systems. Additional problems for the treatment of chronic and persistent pain are the comparably low efficacy of existing therapies, the failure to translate effects observed in preclinical pain models to human patients and related setbacks in clinical trials from previous attempts to develop novel analgesics. Drug repurposing offers an alternative approach to identify novel analgesics as it can bypass various steps of classical drug development. In recent years, several approved drugs were attributed analgesic properties. Here, we review available data and discuss recent findings suggesting that the approved drugs minocycline, fingolimod, pioglitazone, nilotinib, telmisartan, and others, which were originally developed for the treatment of different pathologies, can have analgesic, antihyperalgesic, or neuroprotective effects in preclinical and clinical models of inflammatory or neuropathic pain. For our analysis, we subdivide the drugs into substances that can target neuroinflammation or substances that can act on peripheral sensory neurons, and highlight the proposed mechanisms. Finally, we discuss the merits and challenges of drug repurposing for the development of novel analgesics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The development of novel analgesics is particularly difficult and has faced many setbacks in the past |
Drug repurposing is an alternative approach to classical drug development because it decreases development time and costs, and the drugs can be considered safe for clinical use. Recent preclinical and clinical findings suggest several widely used drugs could be employed as analgesics |
Pharmacological network analysis, pathway mapping, and other computational methods combined with phenotypic screening could identify additional drugs that may be repurposed as novel analgesics |
1 Introduction
Chronic and persistent pain are a massive burden for global health care systems. Around 20% of the adult US population (50 million people) have chronic pain and around 8% of US adults have high-impact chronic pain according to recent estimates [1, 2]. The existing therapies for chronic and neuropathic pain have either low analgesic efficacy, represented by a high number needed to treat, or rather severe side effects [3]. Despite a clear unmet medical need for novel effective and safe analgesics, there has not been an approval of a new first-in-class small molecule analgesic in recent years.
The development of novel analgesics faces several problems and challenges. First, there is the failure to translate effects observed in preclinical pain models to human patients. The readouts of preclinical pain models in rodents are mostly withdrawal responses to evoked stimulations. These are difficult to compare with a patient who has chronic pain for weeks or months. Accordingly, the effects of a treatment may vary profoundly. This is the reason why several promising substances, such as the enhancer of the potassium channel Kv 7/M retigabine, failed to ameliorate neuropathic pain in clinical trials [4]. Consequently, other behavioral readouts such as the grimace scale have been suggested to complement pain threshold tests and to have a broader spectrum of experimental approaches to assess potential antihyperalgesic or antinociceptive effects of a treatment substance [5].
It should also be mentioned that there are various examples of translational success using preclinical pain models. For example, the analgesic effects of the ω-conotoxin MVIIA ziconotide that blocks N-type voltage-gated calcium channels were first identified using preclinical pain models of acute, inflammatory, and neuropathic pain in rodents [6]. Ziconotide was eventually approved for the management of chronic inflammatory and neuropathic pain by the FDA in 2004.
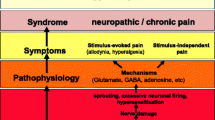
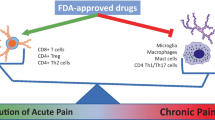
However, another challenge for the development of novel analgesics is the mechanistical differences between different pain states, as well as their complexity. For example, neuroinflammation strongly contributes to chronic and neuropathic pain, but a variety of cells and mediators are involved in this process, making it difficult to select and target a specific receptor or mediator [7, 8].
These limitations hamper the development of novel analgesics and led many pharmaceutical companies to withdraw from the pain market [9].
Drug repurposing (also called drug repositioning) is an alternative approach to identify novel analgesics. It is defined as the identification of new indications for drugs that are already in clinical use [10]. The advantage of drug repurposing is that it can bypass several steps of classical drug development. For example, safety studies can be limited to a minimum because the drugs are already in clinical use, and development time and costs can be reduced to a great extent, especially regarding preclinical development and early clinical trials [11]. The drugs can be directly tested in the clinical setting, since they are already well characterized.
For some drugs that have already been in clinical use for years or decades, there is plenty of pharmacology and pharmacovigilance data available from a large number of treated patients and adverse effects in patients are well known and documented.
A large-scale analysis of drug development pipelines between 2012 and 2017 showed that almost 170 repurposed drugs entered development stages across a range of indications. Of these, some 72% were in phase II clinical development. Of particular interest is that almost 70% of the phase I and II trials for repurposed drugs were sponsored by academia, indicating the key role this sector has in promoting drug repurposing as a solution to unmet patient needs [12]. For example, the estrogen receptor modulator raloxifene, that was originally developed for the treatment of osteoporosis in post-menopausal women, was found to be effective in reducing the risk of invasive breast cancer in a retrospective clinical analysis [13]. These observations led to an FDA approval for raloxifene for invasive breast cancer in 2007 [11]. Raloxifene is also undergoing clinical trials in Europe to evaluate its efficacy and safety in adult paucisymptomatic COVID-19 patients (EudraCT Number: 2020-003936-25).
1.1 Previous Advances in Repurposing Analgesic Therapies
In the pain field, several drugs have also been successfully repurposed. For example, the serotonin-norepinephrine reuptake inhibitor duloxetine, originally developed for the treatment of depression, is recommended as one of the first-line drugs for the treatment of neuropathic pain in a recent review and meta-analysis [3]. Another example is the tricyclic antidepressant amitriptyline, nowadays considered as first-line treatment for neuropathic pain [3, 14]. Also, topical formulations of amitriptyline alone or in combination with ketamine caused a reduction of pelvic pain in patients [15].
Likewise, several antiepileptic drugs with analgesic properties have been identified previously. Among them are carbamazepine, which is primarily used for the treatment of trigeminal neuralgia, lamotrigine, gabapentin, and pregabalin [16]. Both pregabalin and gabapentin are now established standard therapeutics for the treatment of neuropathic pain, although their efficacy seems to be lower than that of amitriptyline and duloxetine [3].
These previous advances demonstrate that drug repurposing for the development of novel analgesics can be successful.
1.2 Drug Repurposing: Focus on Spinal Neuroinflammation and Sensory Neurons
Ideally, we suggest that the following criteria concerning safety and efficacy should be met by any analgesic drug: (1) clinical evidence for analgesic effects, (2) good tolerability of the drug, (3) the analgesic dose needs to be in the therapeutic range of the drug, (4) no major drug interaction with other analgesics or substances treating obvious comorbidities, and (5) no confounding long-term effects.
However, none of the already existing analgesics can meet all these criteria. Examples are tolerance of opioids, interactions of celecoxib and tamoxifen and many more. It is therefore difficult for any repurposed drug to meet all these criteria.
We previously summarized and discussed progress in drug repurposing for the development of novel analgesics [17]. Here, we provide a brief and updated review of the available data and discuss recent findings suggesting that several approved drugs, such as minocycline, fingolimod, pioglitazone, nilotinib, telmisartan, and others, that were originally developed for the treatment of different pathologies, have analgesic, antihyperalgesic, or neuroprotective effects in preclinical models of inflammatory or neuropathic pain.
For this review, we focus on two essential mechanisms of persistent pain: (1) neuroinflammation in the spinal cord and (2) targeting peripheral sensory neurons. Although persistent pain is not a monocausal disease and involves various processes in different tissues, these two mechanisms stand out.
Neuroinflammation is an overlapping mechanism and a mechanistic hallmark of various persistent pain states [7, 8]. It is especially interesting for drug repurposing because of its mechanistic interface with other neurological diseases, such as multiple sclerosis and Parkinson’s disease, for which drugs have already been approved and are in clinical use.
Likewise, stress and damage of sensory neurons is a critical hallmark of several neuropathic pain conditions [18]. Sensory neurons also represent the initial physiological system of the body that encounters nociceptive stimuli from the environment, and their increased activity can lead to both peripheral and central sensitization. Targeting sensory neurons means targeting the beginning of the pain pathway [19], which is strategically important because it can prevent the downstream sensitization and wind-up effects that are caused by excessive neuronal activity.
2 Targeting Neuroinflammation with Approved Drugs
Neuroinflammation involves activation of microglia and astrocytes, as well as migration of immune cells to trigeminal or dorsal root ganglia and the spinal cord [7]. The activated and recruited immune cells release proinflammatory cytokines, chemokines, signaling lipids and other mediators that can increase neuronal activity in the peripheral and central nervous system [8]. This enhancement of neuronal activity can cause exacerbated sensory phenomena such as allodynia and hyperalgesia to sensory stimuli [20].
Reducing neuroinflammation and the subsequent increase of neuronal activity may thus represent a therapeutic approach to target persistent pain in patients. However, the variety of released mediators makes it difficult to target them. Among the proinflammatory mediators are cytokines such as tumor necrosis factor alpha (TNFα), and the interleukins IL-1β, IL-6, chemokines such as CCL2, CCL5 and CXCL1 [21], as well as lipids such as eicosanoids, lysophospholipids, and oxidized linoleic acid metabolites [22]. Although several substances or monoclonal antibodies such as infliximab or tocilizumab may block individual mediators and in doing so disrupt their signaling, there is still an abundance of other mediators that can compensate for individual losses. This may be the reason why, for example, the TNFα-blocking antibody infliximab, which is widely used in the clinic for the treatment of chronic inflammatory diseases [23], did not show any effect in reducing persistent pain in clinical trials [24, 25]. Likewise, the IL-6 receptor-blocking antibody tocilizumab failed to ameliorate pain in a randomized, double-blind, placebo-controlled clinical trial in 79 patients with osteoarthritis of the hand [26].
In consequence, it may be more promising to (1) reduce the activation of glial cells and/or prevent the migration of other immune cells to the nervous system, (2) reduce the synthesis and release of proinflammatory mediators, such as cytokines, chemokines, and lipids from immune cells, or (3) reduce excessive neuronal activity and synaptic glutamate release.
Several approved drugs have anti-inflammatory properties but only a few of them target neuroinflammation and can reduce neuronal activity in the spinal cord in preclinical pain models. Among them are antibiotics such as minocycline, ceftriaxone, demeclocycline, and chlortetracycline, as well as the sphingolipid signaling modulator fingolimod, the antidiabetic drug pioglitazone, and the phosphodiesterase inhibitor ibudilast (Fig. 1, Table 1).
Proposed mechanisms of approved drugs in reducing neuroinflammation. CCL2 chemokine (C–C motif) ligand 2, EphB1 ephrin type-B receptor 1, GLT-1 glutamate transporter 1, IκB inhibitor of nuclear factor kappa B, IL-1β interleukin-1β, IL-6 interleukin-6, mTOR mammalian target of rapamycin, NF-κB nuclear factor kappa B, NMDAR N-methyl-d-aspartate receptor, pERK phosphorylated extracellular-signal regulated kinase, PPARγ peroxisome proliferator-activated receptor γ, S1P1R sphingosine-1-phosphate receptor 1, TNFα tumor necrosis factor α
2.1 Targeting ROS Production and Cytokine Release in Microglia
2.1.1 Minocycline
Minocycline is a semisynthetic tetracycline that received its FDA approval in 1971. Due to its high lipophilicity, it can penetrate through the blood–brain barrier better than other tetracyclines [27]. Minocycline has previously been suggested as a therapeutic option for neurodegenerative diseases, as its neuroprotective and anti-inflammatory properties became apparent [28]. However, clinical studies of the last 20 years showed mixed results. While in some clinical trials beneficial effects of minocycline have been reported, a recent meta-analysis concluded that to date there is no conclusive evidence for a strong amelioration of clinical symptoms in neurodegenerative diseases after minocycline treatment [29].
In the context of neuropathic pain, several recent studies confirmed previous observations that minocycline may ameliorate neuroinflammation in persistent pain states. It was shown that intrathecal injection reduced mechanical allodynia in vivo and reduced the A1/A2 ratio of spinal astrocytes in a rat model of skin/muscle incision and retraction (SMIR) by downregulating CXCR7 and the PI3K/Akt system [30]. In the context of chemotherapy-induced neuropathic pain, minocycline treatment reduced vincristine-induced mechanical hypersensitivity in mice, as well as tactile allodynia and cold hyperalgesia caused by oxaliplatin when administered alone or in combination with duloxetine [31, 32]. Likewise, minocycline alone and in combination with botulinum toxin decreased the inflammatory response and oxidative stress of glial cells after spinal cord injury pain in rats by activating SIRT1 and restraining pAKT, P53, and p-NF-kB [33]. In a model of systemic lipopolysaccharide (LPS)-induced spinal cord inflammation in neonatal rats, minocycline treatment reduced LPS-induced allodynia and hyperalgesia, and in a rat model of streptozotocin-induced type 1 diabetes mellitus, minocycline administration led to a reduction in mechanical hypersensitivity [34, 35].
Apart from minocycline monotherapy, a combination with other tetracyclines may also be beneficial for ameliorating neuropathic pain. A recent study identified that demeclocycline, chlortetracycline, and minocycline bind and inhibit the tyrosine kinase ephrin type-B receptor 1 (EphB1) in the brain, spinal cord, and dorsal root ganglia (DRG). Treating mice with a combination of these three tetracyclines caused a reduction of mechanical and thermal hypersensitivity in capsaicin-, CFA- and formalin-induced pain [36]. Mechanistically, minocycline seems to reduce the production of reactive oxygen species in microglia and the release of proinflammatory and prologetic cytokines and chemokines, such as TNFα, IL-1β, and CXCL1 [37] (Fig. 1).
In recent years, several small clinical trials have contributed to the concept of using minocycline as a treatment option for persistent pain in patients. For example, minocycline reduced bilateral muscular hyperalgesia and cutaneous cold allodynia caused by repeated intramuscular injections of hypertonic saline in healthy humans [38], and minocycline reduced muscle hyperalgesia induced by intramuscular injection of nerve growth factor (NGF) in humans in a small placebo-controlled double-blind clinical trial [39]. Moreover, minocycline treatment for 12 weeks caused a reduction of paclitaxel-induced acute pain and fatigue in cancer patients in a pilot study [40]. In another randomized clinical trial, minocycline treatment for 6–7 weeks reduced chemotherapy-induced neuropathic pain and fatigue in patients with non-small lung cancer [41].
A recently published systematic review of studies in humans concluded that minocycline could potentially reduce neuropathic pain in patients [42] (Table 1). However, its analgesic effect has not yet been assessed in a large, randomized, placebo-controlled clinical trial.
2.2 Enhancing Spinal Glutamate Uptake
2.2.1 Ceftriaxone
Several lines of evidence suggest analgesic effects of the antibiotic ceftriaxone in preclinical pain models. The first observation showing that ceftriaxone causes upregulation of the glutamate transporter GLT-1 in the spinal cord, which reduces spinal glutamate concentrations and decreases transmission of painful signals to the central nervous system in the context of neuropathic pain, was published in 2010 [43] (Fig. 1).
Similar observations were reported by recent studies. For example, ceftriaxone treatment reduced mechanical hypersensitivity and thermal hyperalgesia in a GLT-1 dependent manner in a rat model of trigeminal neuropathic pain (TNP) by chronic compression of the infraorbital nerve (CCI-ION) [44]. Likewise, local or systemic, single or repeated administration of ceftriaxone caused a reduction of formalin-induced nociception (flinching behavior) in rats [45].
However, the effect of ceftriaxone in spinal nerve ligation (SNL)-induced pain is controversial. A recent study reported that ceftriaxone alone or in combination with pioglitazone reduced mechanical hypersensitivity, thermal hyperalgesia and cold allodynia after SNL in rats [46]. Conversely, another study found that ceftriaxone caused delayed onset of formalin-induced nocifensive responses and reduced thermal hyperalgesia but had no significant effect on mechanical hypersensitivity after spinal nerve ligation (SNL) in rats [47] (Table 1). In summary, the results from preclinical studies are promising and suggest analgesic efficacy of ceftriaxone in inflammatory and neuropathic pain. In human patients undergoing surgery (n = 15), treatment with intravenous ceftriaxone (2 g) 1 h before surgery caused a reduction in mechanical pain threshold for several hours after surgery [48]. These data indicate that ceftriaxone may reduce postoperative pain in patients and has the additional beneficial effect of antimicrobial prophylaxis when applied prior to surgery.
2.3 Targeting Sphingolipid Signaling in Spinal Neurons and Glial Cells
2.3.1 Fingolimod
The sphingolipid sphingosin-1-phosphate (S1P) is an important lipid mediator that exerts a wide range of pleiotropic immunological effects via its five G-protein-coupled receptors (S1PR1–5) [49]. The S1P receptors 1–3 are also expressed in peripheral sensory neurons [50]. It has previously been suggested that S1P and its precursor ceramide may be involved in peripheral sensitization and aberrant ion channel activity in sensory neurons in the context of persistent pain [51, 52]. Recently it was shown that the dysregulation of S1P signaling causes increased activation of the S1P1 receptor in spinal astrocytes during neuropathic pain evoked by the cytostatic bortezomib or by nerve injury. In consequence, astrocytes release proinflammatory mediators that initiate and maintain neuroinflammation. Treating mice with the fucS1P1 receptor agonist fingolimod acting as a functional antagonist, which is approved for the treatment of multiple sclerosis, reduced astrocyte-induced neuroinflammation and neuropathic pain in vivo [53, 54]. Similar results were observed in a cancer-induced bone pain (CIBP) model in mice. As reported by the authors, fingolimod treatment reduced flinching and guarding behavior in these animals [55]. Likewise, fingolimod treatment was found to reduce mechanical hypersensitivity and cold allodynia by reducing pERK activation in the spinal cord via the S1P1 receptor in a mouse model of multiple-sclerosis-induced neuropathic pain [56].
Fingolimod itself is an example of successful drug repurposing because it was originally considered as treatment for kidney transplant rejection [57].
Based on these preclinical observations, two clinical trials have been initiated to assess the effect of fingolimod in chemotherapy-induced neuropathic pain in patients (ClinicalTrials.gov identifiers NCT03941743, NCT03943498), but have not yet reported results (Fig. 1, Table 1).
2.4 Activating PPARγ in Spinal Cord Neurons
2.4.1 Pioglitazone
The antidiabetic drug pioglitazone is a highly potent agonist of the peroxisome proliferator activating factor-γ (PPARγ) [58]. Intrathecal injection of pioglitazone was shown to reduce mechanical hypersensitivity in a bone cancer pain model in rats, possibly via activation of PPARγ and reduction of mTOR signaling in spinal cord neurons [59]. Pioglitazone may also reduce the inflammatory response of spinal astrocytes in the context of nerve-injury-induced neuropathic pain [60]. Moreover, pioglitazone also seems to have beneficial effects on peripheral sensory neurons in the context of persistent pain that are discussed in Sect. 3.3 (Figs 1 and 2; Tables 1 and 2).
Proposed mechanisms of approved drugs targeting or protecting sensory neurons. Ca2+ calcium, CGRP calcitonin gene-related peptide, CYP2J2 cytochrome-P450-epoxygenase isoform 2J2, DMF dimethyl fumarate, EphB1 ephrin type-B receptor 1, GLP-1 glucagon-like peptide-1, GLT-1 glutamate transporter 1, NMDAR N-methyl-D-aspartate receptor, OATP1B2 organic anion-transporting polypeptide 1b, OCT2 organic cation/carnitine transporter 2, ROS reactive oxygen species, Src sarcoma, SOD superoxide dismutase, TRPA1 transient receptor potential ankyrin 1 channel, TRPV1 transient receptor potential vanilloid 1 channel, TRPM8 transient receptor potential melastatin 8 channel. The dashed line for minoxidil indicates preliminary observations
2.5 Reducing Microglia Activation
2.5.1 Ibudilast
The phosphodiesterase inhibitor ibudilast is an FDA-approved drug for the treatment of amyotrophic lateral sclerosis (ALS). Mechanistically it seems to reduce the production of the proinflammatory mediators TNFα, IL-1β, IL-6, and glial fibrillary acidic protein (GFAP) [61], which are also hallmarks of neuroinflammation [8]. In recent studies, intraperitoneal injection of ibudilast was found to reduce mechanical hypersensitivity of rats after treatment with the cytostatic oxaliplatin [62]. In another study, intrathecal administration of ibudilast caused a reduction in hypersensitivity in two different rat models of nerve-injury-induced neuropathic pain. The mechanism for these effects are unclear but seem to be related to a reduced number of p-p38-positive activated spinal microglia [63] (Fig. 1, Table 1).
Ibudilast was also assessed in clinical trials in the context of opioid withdrawal. A small recent trial reported that treatment with ibudilast (50 mg twice daily) reduces opioid withdrawal symptoms and seems to increase the analgesic effects of oxycodone in human volunteers diagnosed with opioid dependence [64]. These results are promising and suggest ibudilast for the treatment of opioid use disorders. However, larger clinical trials are required for conclusive evidence about the analgesic effects of ibudilast in patients.
2.6 Targeting T-Cell–Neuron Interaction
2.6.1 Sivelestat
Peripheral nerve injury causes recruitment and infiltration of T cells to dorsal root ganglia. These T cells were shown to release leukocyte elastase, which is a serine protease that interacts with and sensitizes sensory neurons. Inhibiting leukocyte elastase with the specific inhibitor sivelestat, which is an approved drug in Southeast Asia for the treatment of acute lung injury, causes a reduction of nerve-injury-induced neuropathic pain in vivo [65]. In another study by the same group, sivelestat was also found to reduce diabetes-induced neuropathic pain and cancer pain in respective rodent models [66].
Recently, it was shown that sivelestat attenuates the expression of proinflammatory cytokines and chemokines such as TNFα, IL-1β, IL-6, and CCL2 after spinal cord injury in rats, reducing both neuroinflammation and mechanical hypersensitivity in vivo [67]. These recent results point towards an additional role of sivelestat in reducing neuroinflammation in the spinal cord, apart from its already described effect in peripheral sensory neurons, and suggest repurposing the compound for the treatment of neuropathic pain in patients (Fig. 1, Table 1).
3 Targeting Peripheral Sensory Neurons with Approved Drugs
Apart from neuroinflammation, other mechanisms that mainly involve increased activity of peripheral sensory neurons have been identified as hallmarks of neuropathic pain [18, 68]. Of course, the peripheral nervous system and the immune system are not completely different entities and there is communication between the two systems in persistent pain states [69, 70]. However, alterations in the activity of ion channels, as well as axonal degradation and mitochondrial dysfunction, have been described as key mechanisms of neuropathic pain in peripheral sensory neurons, respectively [19, 71,72,73]. In particular, neuropathic pain caused by cytostatics (chemotherapy-induced neuropathic pain) seems to develop as a result of toxic effects and severe damage of peripheral sensory neurons [74,75,76]. The absence of a barrier, such as the blood–brain barrier, to prevent external substances from entering the system makes peripheral sensory neurons more exposed to toxic substances that may enter, accumulate, and damage the cells. Several approved drugs seem to target these mechanisms.
3.1 Preventing Uptake of Cytostatics into Sensory Neurons
3.1.1 Nilotinib, Dasatinib, and Cimetidine
The two cytostatics, paclitaxel and oxaliplatin, are widely used in the clinic and are first-line therapeutics for breast and ovarian cancer (paclitaxel) and colorectal cancer (oxaliplatin). Both can cause peripheral neuropathies and neuropathic pain in patients, which is a dose- and therapy-limiting side effect that can lead to dose reduction of discontinuation of chemotherapy in affected patients [77,78,79]. Currently, there is no approved drug available to treat paclitaxel- or oxaliplatin-induced neuropathic pain in patients [80].
However, two transporters have been identified that seem to be responsible for uptake of these cytostatics into sensory neurons. For paclitaxel, the organic anion–transporter OATP1B2 seems to be responsible for the transport of paclitaxel into sensory neurons [81]. Likewise, an organic cation transporter called OCT2 seems to facilitate transport of oxaliplatin into sensory neurons [82]. In both cases, blocking these transporters with the approved drugs nilotinib (OATP1B2), dasatinib, or cimetidine (OCT2) reduces uptake of the cytostatics into sensory neurons and ameliorates hypersensitivity caused by these substances in preclinical models in vivo [81, 83] (Fig. 2, Table 2). Preventing toxic substances from being transported into sensory neurons may thus be a promising strategy to ameliorate toxic neuropathies and associated neuropathic pain.
For nilotinib, there is also evidence for analgesic effects from a human study. Nilotinib was found to increase thermal pain thresholds in human patients (n = 31) at a mean dose of 480 mg/day, possibly due to inhibition of the tyrosine kinase c-Kit [64].
However, other strategies involve the reduction of ion channel activity, axonal degeneration, and calcium dysregulation in sensory neurons. Several approved drugs have been proposed to target these mechanisms.
3.2 Reducing TRP Channel Activity
3.2.1 Topiramate, Acetazolamide, Telmisartan, and Riluzole
The transient receptor potential vanilloid 1 (TRPV1) channel is a ligand-gated ion channel, permeable mainly for calcium, that is expressed in sensory neurons. Under physiological conditions, it can be activated by heat (<43 °C), low pH (<5.2) and the vanilloid capsaicin [84]. Under pathophysiological conditions, its aviation threshold is reduced, and its excessive activity contributes to enhanced neuronal activity during inflammatory and neuropathic pain [19, 85]. Also, cold temperatures are sensed by a member of the TRP channel family. The transient receptor potential melastatin 8 (TRPM8) channel responds to cold temperatures, and the compounds menthol and icilin [86, 87]. Likewise, the TRPA1 (ankyrin) channel is expressed in a subset of sensory neurons acting as a chemosensor that is activated by pungent electrophilic substances such as mustard oil and cinnamaldehyde [88, 89].
Despite their well described role in persistent pain states, clinical development of TRP channel antagonists has not yet succeeded in providing new therapeutics for persistent pain in patients. However, several FDA-approved drugs seem to reduce TRP channel activity or their expression in sensory neurons indirectly.
A recent study showed that the cytostatic oxaliplatin reduces the intracellular pH of murine DRG neurons, causing sensitization of TRPV1 and TRPA1 channels. The two approved drugs acetazolamide and topiramate inhibit carbonic anhydrase. While this is the main function of acetazolamide, it is an off-target effect of topiramate, which was originally developed as an anticonvulsant drug that modulates the activity of voltage-gated sodium channels, GABA receptors, glutamate, and kainate receptors [90]. Blocking carbonic anhydrase with either of the two drugs leads to elevation of the pH in sensory neurons, causing restoration of the physiological activity of TRPV1 and TRPA1 and a reduction of oxaliplatin-induced cold allodynia in vivo [91].
For acetazolamide, there is some evidence from small clinical trials suggesting analgesic effects. Acetazolamide 5 mg/kg, when applied intravenously after induction of anesthesia, was found to reduce referred pain after laparoscopic surgical procedures in 18 patients [92]. Likewise, a single dose of oral acetazolamide (5 mg/kg) decreased radiated shoulder pain immediately after laparoscopy in a randomized trial involving 70 patients [93]. These data indicate that acetazolamide can reduce referred postoperative pain in patients, but they are yet to be confirmed in larger clinical trials.
The drug riluzole was approved by the FDA in 1995 for the treatment of ALS, as it blocks tetrodoxin-sensitive sodium channels [94]. In the context of neuropathic pain caused by the cytostatic oxaliplatin, riluzole reduced neurite shortening and decreased mechanical and cold hypersensitivity in rats after oxaliplatin treatment. Mechanistically, riluzole seems to reduce the expression of the TRPM8 channel and the expression of the glutamate transporter GLT-1 in sensory neurons, which balances spinal glutamate levels [95, 96].
A different mechanism was observed for the angiotensin II receptor type 1 antagonist telmisartan. Treating mice with the cytostatic drug paclitaxel causes increased expression of the cytochrome-P450-epoxygenase isoform 2J2 (CYP2J2) in sensory neurons. Telmisartan inhibits CYP2J2 [97] which reduces synthesis of the oxidized linoleic acid metabolite 9,10-EpOME (epoxy-octadecenoic acid) in sensory neurons. This prevents 9,10-EpOME-mediated sensitization of TRPV1 and subsequent release of calcitonin gene-related peptide (CGRP) and neurogenic inflammation. Treating mice with telmisartan prevents and reduces mechanical and thermal hypersensitivity after paclitaxel treatment [98] (Fig. 2, Table 2).
Direct inhibition of TRP channels seems to be an obvious strategy to reduce their pathophysiological activity in persistent pain states. However, until now TRPV1 antagonists failed in early clinical trials due to severe side effects, such as hyperthermia [99]. These results described above suggest indirect targeting of TRP channels with approved drugs as a promising alternative strategy to reduce their excessive activity in neuropathic pain states.
3.3 Reducing Oxidative and Neuronal Stress by PPARγ Activation
3.3.1 Pioglitazone
Mitochondrial dysfunction and the production of reactive oxygen species (ROS) in peripheral sensory neurons is another characteristic mechanism of neuropathic pain after nerve injury or neuronal damage [100]. As mentioned above, the antidiabetic drug pioglitazone activates the PPARγ [58]. Treatment with pioglitazone increases the expression of ROS-metabolizing enzymes in peripheral sensory neurons, such as superoxide dismutase (SOD) and catalase. This causes degradation of ROS into their innocuous metabolites. In mice that were treated with the cytostatic cisplatin, additional treatment with pioglitazone reduces mechanical and cold hypersensitivity induced by the cytostatic cisplatin in vivo [101]. Another recent study observed that intraplantar or intraperitoneal injection of pioglitazone reduced post-formalin nocifensive behavior in rats in a PPARγ-dependent manner that may involve reduction of nitric oxide (NO) synthesis [102] (Fig. 2, Table 2).
Together these preclinical studies imply that pioglitazone may have a dual effect on both reducing damage in peripheral sensory neurons and in reducing the activity of spinal cord neurons (see Sect. 2.3), thereby decreasing the transmission of nociceptive signals to the central nervous system. However, this concept has not yet been addressed by clinical studies.
3.4 Enhancing Neuroprotection
3.4.1 Alogliptin, Dimethyl Fumarate, Donepezil, Fulvestrant, and Minoxidil
Several drugs lead to a reduction of neurite shortening, axonal degradation, or demyelination caused by the cytostatics paclitaxel, oxaliplatin, or bortezomib in vitro without affecting the anti-tumor effects of the cytostatics. Treatment of rodents with these drugs caused a reduction of mechanical or thermal hypersensitivity in models of chemotherapy-induced neuropathic pain. This has been reported for the antidiabetic drug and DPP-4 inhibitor alogliptin [103], the multiple sclerosis agent dimethyl fumarate [104], the anti-dementia drug donepezil [105], the estrogen receptor antagonist and cytostatic fulvestrant [106], and the strong anti-hypertensive drug minoxidil [107]. The authors claim possible neuroprotective effects, such as the reduction of calcium dysregulation for minoxidil [107] or enhanced activity of superoxide dismutase and ROS degradation for donepezil [105], to be responsible for these effects.
Indeed, cotreatment with donepezil (5 mg/d) was found to enhance gabapentin analgesia in neuropathic pain patients in a small randomized controlled clinical trial, indicating that a combination therapy of donepezil and gabapentin may be beneficial for patients with insufficient response to gabapentin [108].
However, the precise mechanisms of action of these drugs on peripheral sensory neurons remain unknown and should be addressed to understand the effects and estimate the potency of these drugs for their potential off-label use as analgesics in patients with chemotherapy-induced neuropathic pain (Fig. 2, Table 2).
4 Concluding Remarks
As described above, several approved drugs showed promising antihyperalgesic or analgesic effects in preclinical pain models by either targeting neuroinflammation in the spinal cord or by reducing activity or stress of peripheral sensory neurons.
Analyzing the list of drugs discussed above, there is no clear pattern recognizable that, for example, drugs of a certain drug class are more likely to exhibit analgesic effects than drugs of another class. In contrast, the list includes antihypertensive drugs (telmisartan), antidiabetic drugs (pioglitazone), as well as tyrosine kinase inhibitors (dasatinib, nilotinib) that had not been associated with persistent pain before.
Instead, the analgesic effects of the drugs discussed in this manuscript were identified because of mechanistic overlap with pathophysiological pain. In most cases, off-target effects of the drugs have been identified that address crucial mechanisms in development or maintenance of persistent pain.
Today, the availability of large data sets, such as genome-wide association (GWAS) data, in combination with pathway analysis tools, molecular docking, and signature matching of drugs makes it easier to identify overlapping therapeutic effects of various diseases and simplifies the identification of drugs that could be repurposed for the treatment of other pathologies [11]. The use of novel databases, such as the connectivity map (Cmap) and the multi-institutional library of integrated network-based cellular signatures (LINCS), as well as the implementation of network analysis and machine learning approaches may additionally help to identify mechanistical connections between approved drugs and disease pathologies [109, 110]. However, better integration of public and proprietary data with resources such as Connectivity mapping tools is needed to reveal compounds exhibiting common activity profiles across multiple targets for selectivity evaluation to select the optimal compounds for progression and provide clear insights into the potential mechanisms of action.
Network pharmacology in combination with phenotypic screening is another powerful tool to identify novel analgesics because the screening hits can be directly validated on a neuronal system [111]. Using this approach, drug repurposing screens could easily be implemented and validated.
Also, the use of induced pluripotent stem cell (iPSC)-derived neurons for compound screening is a promising approach to identify novel analgesics [112]. For example, disease modeling using iPSC-derived neurons from persistent pain patients could be used to identify common pathophysiological alterations that may be responsible for the pain state of subgroups of patients. Based on these common pathophysiological patterns, a treatment option could be recommended for these populations. This technology could be eventually integrated in drug repurposing workflows.
However, despite potential merits of drug repurposing, there are also setbacks. For example, the antibiotic ceftriaxone showed neuroprotective effects in preclinical studies but failed to show efficacy in a randomized, double-blind, placebo-controlled, phase III trial for the treatment of ALS [113, 114].
This example and several other failures show that there are confounding factors and problems in drug repurposing that need to be addressed as well.
First, drug repurposing may cause pharmacological problems, because the drugs were originally designed and optimized for targeting different receptors, cells, or even organs. This may lead to lower efficacy and to increases in the required dose or to enhanced interactions with other drugs. Also, alterations of the dose regimen may be a consequence, and subsequently an increase of adverse events can occur. For example, long-term use of antibiotics such as ceftriaxone, or the tetracyclines minocycline, demeclocycline, and chlortetracycline, may reduce neuroinflammation in persistent pain states but may also enhance the risk of antimicrobial resistance and severe infections [17, 37]. However, as indicated by preliminary studies in human patients, their effective analgesic dose is in the same range as their antimicrobial dose. If possible, equal doses and treatment schedules should be used for both antimicrobial and analgesic therapy for these drugs and the treatment duration should be restricted to reduce the risk of antibiotic resistance. Since ceftriaxone was applied only once before surgery, the risk of developing antimicrobial resistance was comparably low. In this special case, ceftriaxone may serve a dual role of reducing postoperative pain and simultaneously reducing postoperative microbial infections.
Repurposing of fingolimod, for example, may also reveal additional unforeseen safety issues; when treatment was stopped in multiple sclerosis, the disease was observed to worsen, leading to a recent safety announcement from regulators.
Second, the patent situation and the weak protection of intellectual property of already approved drugs discourages many companies from further exploration and development. Many of the repurposing uses have already been described in the scientific literature, which limits the possibility of receiving patent protection for the repurposed context [109]. In many cases, patent protection for the original drugs has already expired, and generic products that are already available could simply be used off-label [115]. At present there exists a reimbursement and health technology assessment (HTA) environment that has impediments to efficient uptake of repurposed drugs. The lack of a viable path to market for repurposed generic medicines is compounded by a regulatory landscape that is not yet fully aligned to the specific needs of the drug repurposing process.
Third, many companies are hesitant to engage in collaborations, and the exchange of substances and data with the scientific community is often accompanied by restricted information exchange or publication restrictions. Likewise, companies are often unwilling to pursue repurposing programs if the repurposed indication does not fall within the core expertise or disease priorities of the respective company, which may also hamper drug repurposing programs and further clinical development [11].
Fourth, the repurposed drug addresses a different group of patients. Factors such as age, comorbidities, and specific drug combinations in this group of patients could be problematic when implementing the repurposed drug in their therapeutic regimen [110].
Fifth, as mentioned above, the problem of translating effects from preclinical pain models to human patients is not only a challenge for classical drug development but also for drug repurposing. In preclinical pain models, withdrawal reflexes to evoked stimulations are mostly used to assess mechanical or thermal pain thresholds and to investigate potential analgesic effects of a substance. But these readouts are difficult to compare with a chronic pain patient [4].
Despite these confounding factors and challenges, drug repurposing is a chance to accelerate the availability of new therapies. In the case of persistent and neuropathic pain, several drugs have shown promising effects in preclinical studies and a few of them are already being tested in clinical trials. Of course, drug repurposing cannot and should not replace the search for novel analgesics, but it can be used as a complementary strategy to relieve and ameliorate persistent pain in patients.
References
Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, et al. Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(36):1001–6.
Zelaya CE, Dahlhamer JM, Lucas JW, Connor EM. Chronic pain and high-impact chronic pain among U.S. adults, 2019. NCHS Data Brief. 2020;390:1–8.
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, et al. Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol. 2015;14(2):162–73.
Yekkirala AS, Roberson DP, Bean BP, Woolf CJ. Breaking barriers to novel analgesic drug development. Nat Rev Drug Discov. 2017;16(8):545–64.
Sadler KE, Mogil JS, Stucky CL. Innovations and advances in modelling and measuring pain in animals. Nat Rev Neurosci. 2021;23:70–85. https://doi.org/10.1038/s41583-021-00536-7.
McGivern JG. Ziconotide: a review of its pharmacology and use in the treatment of pain. Neuropsychiatr Dis Treat. 2007;3(1):69–85.
Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology. 2018;129(2):343–66. https://doi.org/10.1097/ALN.0000000000002130
Ji RR, Xu ZZ, Gao YJ. Emerging targets in neuroinflammation-driven chronic pain. Nat Rev Drug Discov. 2014;13(7):533–48.
Woolf CJ. Overcoming obstacles to developing new analgesics. Nat Med. 2010;16(11):1241–7. https://doi.org/10.1038/nm.2230
Ashburn TT, Thor KB. Drug repositioning: identifying and developing new uses for existing drugs. Nat Rev Drug Discov. 2004;3(8):673–83.
Pushpakom S, Iorio F, Eyers PA, Escott KJ, Hopper S, Wells A, et al. Drug repurposing: progress, challenges and recommendations. Nat Rev Drug Discov. 2019;18(1):41–58.
Polamreddy P, Gattu N. The drug repurposing landscape from 2012 to 2017: evolution, challenges, and possible solutions. Drug Discov Today. 2019;24(3):789–95.
Vogel VG, Costantino JP, Wickerham DL, Cronin WM, Cecchini RS, Atkins JN, et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial. JAMA. 2006;295(23):2727–41.
Rintala DH, Holmes SA, Courtade D, Fiess RN, Tastard LV, Loubser PG. Comparison of the effectiveness of amitriptyline and gabapentin on chronic neuropathic pain in persons with spinal cord injury. Arch Phys Med Rehabil. 2007;88(12):1547–60.
Poterucha TJ, Murphy SL, Rho RH, Sandroni P, Warndahl RA, Weiss WT, et al. Topical amitriptyline-ketamine for treatment of rectal, genital, and perineal pain and discomfort. Pain Physician. 2012;15(6):485–8.
Finnerup NB. Nonnarcotic methods of pain management. N Engl J Med. 2019;380(25):2440–8.
Sisignano M, Parnham MJ, Geisslinger G. Drug repurposing for the development of novel analgesics. Trends Pharmacol Sci. 2016;37(3):172–83.
von Hehn CA, Baron R, Woolf CJ. Deconstructing the neuropathic pain phenotype to reveal neural mechanisms. Neuron. 2012;73(4):638–52.
Patapoutian A, Tate S, Woolf CJ. Transient receptor potential channels: targeting pain at the source. Nat Rev Drug Discov. 2009;8(1):55–68.
Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl):S2-15.
Ellis A, Bennett DL. Neuroinflammation and the generation of neuropathic pain. Br J Anaesth. 2013;111(1):26–37.
Osthues T, Sisignano M. Oxidized lipids in persistent pain states. Front Pharmacol. 2019;10:1147.
Melsheimer R, Geldhof A, Apaolaza I, Schaible T. Remicade((R)) (infliximab): 20 years of contributions to science and medicine. Biologics. 2019;13:139–78.
Leung L, Cahill CM. TNF-alpha and neuropathic pain—a review. J Neuroinflammation. 2010;16(7):27.
Korhonen T, Karppinen J, Paimela L, Malmivaara A, Lindgren KA, Jarvinen S, et al. The treatment of disc herniation-induced sciatica with infliximab: results of a randomized, controlled, 3-month follow-up study. Spine. 2005;30(24):2724–8.
Richette P, Latourte A, Sellam J, Wendling D, Piperno M, Goupille P, et al. Efficacy of tocilizumab in patients with hand osteoarthritis: double blind, randomised, placebo-controlled, multicentre trial. Ann Rheum Dis. 2020;80:349–55. https://doi.org/10.1136/annrheumdis-2020-218547.
Yong VW, Wells J, Giuliani F, Casha S, Power C, Metz LM. The promise of minocycline in neurology. Lancet Neurol. 2004;3(12):744–51.
Kim HS, Suh YH. Minocycline and neurodegenerative diseases. Behav Brain Res. 2009;196(2):168–79.
Romero-Miguel D, Lamanna-Rama N, Casquero-Veiga M, Gomez-Rangel V, Desco M, Soto-Montenegro ML. Minocycline in neurodegenerative and psychiatric diseases: an update. Eur J Neurol. 2021;28(3):1056–81.
Li T, Liu T, Chen X, Li L, Feng M, Zhang Y, et al. Microglia induce the transformation of A1/A2 reactive astrocytes via the CXCR7/PI3K/Akt pathway in chronic post-surgical pain. J Neuroinflamm. 2020;17(1):211.
Starobova H, Mueller A, Allavena R, Lohman RJ, Sweet MJ, Vetter I. Minocycline prevents the development of mechanical allodynia in mouse models of vincristine-induced peripheral neuropathy. Front Neurosci. 2019;13:653.
Salat K, Furgala-Wojas A, Salat R. The microglial activation inhibitor minocycline, used alone and in combination with duloxetine, attenuates pain caused by oxaliplatin in mice. Molecules. 2021;26(12):3577. https://doi.org/10.3390/molecules26123577.
Yu Z, Liu J, Sun L, Wang Y, Meng H. Combination of botulinum toxin and minocycline ameliorates neuropathic pain through antioxidant stress and anti-inflammation via promoting SIRT1 pathway. Front Pharmacol. 2020;11: 602417.
Hsieh CT, Lee YJ, Dai X, Ojeda NB, Lee HJ, Tien LT, et al. Systemic lipopolysaccharide-induced pain sensitivity and spinal inflammation were reduced by minocycline in neonatal rats. Int J Mol Sci. 2018;19(10):2947. https://doi.org/10.3390/ijms19102947.
Amorim D, Puga S, Braganca R, Braga A, Pertovaara A, Almeida A, et al. Minocycline reduces mechanical allodynia and depressive-like behaviour in type-1 diabetes mellitus in the rat. Behav Brain Res. 2017;1(327):1–10.
Ahmed MS, Wang P, Nguyen NUN, Nakada Y, Menendez-Montes I, Ismail M, et al. Identification of tetracycline combinations as EphB1 tyrosine kinase inhibitors for treatment of neuropathic pain. Proc Natl Acad Sci USA. 2021;118(10):e2016265118. https://doi.org/10.1073/pnas.2016265118.
Zhou YQ, Liu DQ, Chen SP, Sun J, Wang XM, Tian YK, et al. Minocycline as a promising therapeutic strategy for chronic pain. Pharmacol Res. 2018;134:305–10.
Samour MS, Nagi SS, Shortland PJ, Mahns DA. Minocycline prevents muscular pain hypersensitivity and cutaneous allodynia produced by repeated intramuscular injections of hypertonic saline in healthy human participants. J Pain. 2017;18(8):994–1005.
Dunn JS, Nagi SS, Mahns DA. Minocycline reduces experimental muscle hyperalgesia induced by repeated nerve growth factor injections in humans: a placebo-controlled double-blind drug-crossover study. Eur J Pain. 2020;24(6):1138–50.
Pachman DR, Dockter T, Zekan PJ, Fruth B, Ruddy KJ, Ta LE, et al. A pilot study of minocycline for the prevention of paclitaxel-associated neuropathy: ACCRU study RU221408I. Support Care Cancer. 2017;25(11):3407–16.
Wang XS, Shi Q, Mendoza T, Lin S, Chang JY, Bokhari RH, et al. Minocycline reduces chemoradiation-related symptom burden in patients with non-small cell lung cancer: a phase 2 randomized trial. Int J Radiat Oncol Biol Phys. 2020;106(1):100–7.
Shin DA, Kim TU, Chang MC. Minocycline for controlling neuropathic pain: a systematic narrative review of studies in humans. J Pain Res. 2021;14:139–45.
Hu Y, Li W, Lu L, Cai J, Xian X, Zhang M, et al. An anti-nociceptive role for ceftriaxone in chronic neuropathic pain in rats. Pain. 2010;148(2):284–301.
Luo X, He T, Wang Y, Wang JL, Yan XB, Zhou HC, et al. Ceftriaxone relieves trigeminal neuropathic pain through suppression of spatiotemporal synaptic plasticity via restoration of glutamate transporter 1 in the medullary dorsal horn. Front Cell Neurosci. 2020;14:199.
Baeza-Flores GDC, Rodriguez-Palma EJ, Reyes-Perez V, Guzman-Priego CG, Torres-Lopez JE. Antinociceptive effects of ceftriaxone in formalin-induced nociception. Drug Dev Res. 2020;81(6):728–35.
Pottabathini R, Kumar A, Bhatnagar A, Garg S, Ekavali E. Ameliorative potential of pioglitazone and ceftriaxone alone and in combination in rat model of neuropathic pain: targeting PPARgamma and GLT-1 pathways. Pharmacol Rep. 2016;68(1):85–94.
Eljaja L, Bjerrum OJ, Honore PH, Abrahamsen B. Effects of the excitatory amino acid transporter subtype 2 (EAAT-2) inducer ceftriaxone on different pain modalities in rat. Scand J Pain. 2018;2(3):132–6.
Macaluso A, Bernabucci M, Trabucco A, Ciolli L, Troisi F, Baldini R, et al. Analgesic effect of a single preoperative dose of the antibiotic ceftriaxone in humans. J Pain. 2013;14(6):604–12.
Spiegel S, Milstien S. The outs and the ins of sphingosine-1-phosphate in immunity. Nat Rev Immunol. 2011;11(6):403–15.
Camprubi-Robles M, Mair N, Andratsch M, Benetti C, Beroukas D, Rukwied R, et al. Sphingosine-1-phosphate-induced nociceptor excitation and ongoing pain behavior in mice and humans is largely mediated by S1P3 receptor. J Neurosci. 2013;33(6):2582–92.
Squillace S, Spiegel S, Salvemini D. Targeting the sphingosine-1-phosphate axis for developing non-narcotic pain therapeutics. Trends Pharmacol Sci. 2020;41(11):851–67.
Cuzzocrea S, Deigner HP, Genovese T, Mazzon E, Esposito E, Crisafulli C, et al. Inhibition of ceramide biosynthesis ameliorates pathological consequences of spinal cord injury. Shock. 2009;31(6):634–44.
Stockstill K, Doyle TM, Yan X, Chen Z, Janes K, Little JW, et al. Dysregulation of sphingolipid metabolism contributes to bortezomib-induced neuropathic pain. J Exp Med. 2018;215(5):1301–13.
Chen Z, Doyle TM, Luongo L, Largent-Milnes TM, Giancotti LA, Kolar G, et al. Sphingosine-1-phosphate receptor 1 activation in astrocytes contributes to neuropathic pain. Proc Natl Acad Sci USA. 2019;116(21):10557–62. https://doi.org/10.1073/pnas.1820466116.
Grenald SA, Doyle TM, Zhang H, Slosky LM, Chen Z, Largent-Milnes TM, et al. Targeting the S1P/S1PR1 axis mitigates cancer-induced bone pain and neuroinflammation. Pain. 2017;158(9):1733–42.
Doolen S, Iannitti T, Donahue RR, Shaw BC, Grachen CM, Taylor BK. Fingolimod reduces neuropathic pain behaviors in a mouse model of multiple sclerosis by a sphingosine-1 phosphate receptor 1-dependent inhibition of central sensitization in the dorsal horn. Pain. 2018;159(2):224–38.
Budde K, Schutz M, Glander P, Peters H, Waiser J, Liefeldt L, et al. FTY720 (fingolimod) in renal transplantation. Clin Transplant. 2006;20(Suppl 17):17–24.
Bogacka I, Xie H, Bray GA, Smith SR. The effect of pioglitazone on peroxisome proliferator-activated receptor-gamma target genes related to lipid storage in vivo. Diabetes Care. 2004;27(7):1660–7.
Gu W, Sun Y, Gu W, Huang Y, Bo J, Zhou L, et al. The analgesic effects of pioglitazone in the bone cancer pain rats via regulating the PPARgamma/PTEN/mTOR signaling pathway in the spinal dorsal horn. Biomed Pharmacother. 2020;131: 110692.
Griggs RB, Donahue RR, Morgenweck J, Grace PM, Sutton A, Watkins LR, et al. Pioglitazone rapidly reduces neuropathic pain through astrocyte and nongenomic PPARgamma mechanisms. Pain. 2015;156(3):469–82.
Schwenkgrub J, Zaremba M, Joniec-Maciejak I, Cudna A, Mirowska-Guzel D, Kurkowska-Jastrzebska I. The phosphodiesterase inhibitor, ibudilast, attenuates neuroinflammation in the MPTP model of Parkinson’s disease. PLoS ONE. 2017;12(7): e0182019.
Johnston IN, Tan M, Cao J, Matsos A, Forrest DRL, Si E, et al. Ibudilast reduces oxaliplatin-induced tactile allodynia and cognitive impairments in rats. Behav Brain Res. 2017;15(334):109–18.
Fujita M, Tamano R, Yoneda S, Omachi S, Yogo E, Rokushima M, et al. Ibudilast produces anti-allodynic effects at the persistent phase of peripheral or central neuropathic pain in rats: different inhibitory mechanism on spinal microglia from minocycline and propentofylline. Eur J Pharmacol. 2018;15(833):263–74.
Metz VE, Jones JD, Manubay J, Sullivan MA, Mogali S, Segoshi A, et al. Effects of ibudilast on the subjective, reinforcing, and analgesic effects of oxycodone in recently detoxified adults with opioid dependence. Neuropsychopharmacology. 2017;42(9):1825–32.
Vicuna L, Strochlic DE, Latremoliere A, Bali KK, Simonetti M, Husainie D, et al. The serine protease inhibitor SerpinA3N attenuates neuropathic pain by inhibiting T cell-derived leukocyte elastase. Nat Med. 2015;21(5):518–23.
Bali KK, Kuner R. Therapeutic potential for leukocyte elastase in chronic pain states harboring a neuropathic component. Pain. 2017;158(11):2243–58.
Kumar H, Choi H, Jo MJ, Joshi HP, Muttigi M, Bonanomi D, et al. Neutrophil elastase inhibition effectively rescued angiopoietin-1 decrease and inhibits glial scar after spinal cord injury. Acta Neuropathol Commun. 2018;6(1):73.
Costigan M, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci. 2009;32:1–32.
Chiu IM, von Hehn CA, Woolf CJ. Neurogenic inflammation and the peripheral nervous system in host defense and immunopathology. Nat Neurosci. 2012;15(8):1063–7.
Chiu IM, Heesters BA, Ghasemlou N, Von Hehn CA, Zhao F, Tran J, et al. Bacteria activate sensory neurons that modulate pain and inflammation. Nature. 2013;501(7465):52–7. https://doi.org/10.1038/nature12479.
Markman JD, Dworkin RH. Ion channel targets and treatment efficacy in neuropathic pain. J Pain. 2006;7(1 Suppl 1):S38-47.
DiAntonio A. Axon degeneration: mechanistic insights lead to therapeutic opportunities for the prevention and treatment of peripheral neuropathy. Pain. 2019;160(Suppl 1):S17–22.
Joseph EK, Levine JD. Mitochondrial electron transport in models of neuropathic and inflammatory pain. Pain. 2006;121(1–2):105–14.
Fukuda Y, Li Y, Segal RA. A mechanistic understanding of axon degeneration in chemotherapy-induced peripheral neuropathy. Front Neurosci. 2017;11:481.
Areti A, Yerra VG, Naidu V, Kumar A. Oxidative stress and nerve damage: role in chemotherapy induced peripheral neuropathy. Redox Biol. 2014;2:289–95.
Boyette-Davis JA, Walters ET, Dougherty PM. Mechanisms involved in the development of chemotherapy-induced neuropathy. Pain Manag. 2015;5(4):285–96.
Park SB, Goldstein D, Krishnan AV, Lin CS, Friedlander ML, Cassidy J, et al. Chemotherapy-induced peripheral neurotoxicity: a critical analysis. CA Cancer J Clin. 2013;63(6):419–37.
Gewandter JS, Freeman R, Kitt RA, Cavaletti G, Gauthier LR, McDermott MP, et al. Chemotherapy-induced peripheral neuropathy clinical trials: review and recommendations. Neurology. 2017;89(8):859–69. https://doi.org/10.1212/WNL.000000000000427.
Sisignano M, Baron R, Scholich K, Geisslinger G. Mechanism-based treatment for chemotherapy-induced peripheral neuropathic pain. Nat Rev Neurol. 2014;10(12):694–707.
Loprinzi CL, Lacchetti C, Bleeker J, Cavaletti G, Chauhan C, Hertz DL, et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: ASCO guideline update. J Clin Oncol. 2020;38(28):3325–48. hhttps://doi.org/10.1200/JCO.20.01399.
Leblanc AF, Sprowl JA, Alberti P, Chiorazzi A, Arnold WD, Gibson AA, et al. OATP1B2 deficiency protects against paclitaxel-induced neurotoxicity. J Clin Invest. 2018;128(2):816–25. https://doi.org/10.1172/JCI96160.
Sprowl JA, Ciarimboli G, Lancaster CS, Giovinazzo H, Gibson AA, Du G, et al. Oxaliplatin-induced neurotoxicity is dependent on the organic cation transporter OCT2. Proc Natl Acad Sci USA. 2013;110(27):11199–204.
Huang KM, Leblanc AF, Uddin ME, Kim JY, Chen M, Eisenmann ED, et al. Neuronal uptake transporters contribute to oxaliplatin neurotoxicity in mice. J Clin Invest. 2020;130(9):4601–6.
Julius D. TRP channels and pain. Annu Rev Cell Dev Biol. 2013;29:355–84.
Basbaum AI, Bautista DM, Scherrer G, Julius D. Cellular and molecular mechanisms of pain. Cell. 2009;139(2):267–84.
Bautista DM, Siemens J, Glazer JM, Tsuruda PR, Basbaum AI, Stucky CL, et al. The menthol receptor TRPM8 is the principal detector of environmental cold. Nature. 2007;448(7150):204–8.
Dhaka A, Murray AN, Mathur J, Earley TJ, Petrus MJ, Patapoutian A. TRPM8 is required for cold sensation in mice. Neuron. 2007;54(3):371–8.
Bautista DM, Jordt SE, Nikai T, Tsuruda PR, Read AJ, Poblete J, et al. TRPA1 mediates the inflammatory actions of environmental irritants and proalgesic agents. Cell. 2006;124(6):1269–82.
Nilius B, Prenen J, Owsianik G. Irritating channels: the case of TRPA1. J Physiol. 2010;589(Pt 7):1543–9. https://doi.org/10.1113/jphysiol.2010.200717.
Shank RP, Gardocki JF, Streeter AJ, Maryanoff BE. An overview of the preclinical aspects of topiramate: pharmacology, pharmacokinetics, and mechanism of action. Epilepsia. 2000;41(S1):3–9.
Potenzieri A, Riva B, Rigolio R, Chiorazzi A, Pozzi E, Ballarini E, et al. Oxaliplatin-induced neuropathy occurs through impairment of haemoglobin proton buffering and is reversed by carbonic anhydrase inhibitors. Pain. 2020;161(2):405–15.
Woehlck HJ, Otterson M, Yun H, Connolly LA, Eastwood D, Colpaert K. Acetazolamide reduces referred postoperative pain after laparoscopic surgery with carbon dioxide insufflation. Anesthesiology. 2003;99(4):924–8.
Movassaghi R, Peirovifar A, Aghamohammadi D, Mohammadipour Anvari H, Golzari SE, Kourehpaz Z. Premedication with single dose of acetazolamide for the control of referral shoulder pain after laparoscopic cholecystectomy. Anesth Pain Med. 2015;5(6): e29366.
Bellingham MC. A review of the neural mechanisms of action and clinical efficiency of riluzole in treating amyotrophic lateral sclerosis: what have we learned in the last decade? CNS Neurosci Ther. 2011;17(1):4–31.
Yamamoto S, Ushio S, Egashira N, Kawashiri T, Mitsuyasu S, Higuchi H, et al. Excessive spinal glutamate transmission is involved in oxaliplatin-induced mechanical allodynia: a possibility for riluzole as a prophylactic drug. Sci Rep. 2017;7(1):9661.
Yamamoto S, Egashira N, Tsuda M, Masuda S. Riluzole prevents oxaliplatin-induced cold allodynia via inhibition of overexpression of transient receptor potential melastatin 8 in rats. J Pharmacol Sci. 2018;138(3):214–7.
Lee CA, Jones JP 3rd, Katayama J, Kaspera R, Jiang Y, Freiwald S, et al. Identifying a selective substrate and inhibitor pair for the evaluation of CYP2J2 activity. Drug Metab Disposit Biol Fate Chem. 2012;40(5):943–51.
Sisignano M, Angioni C, Park CK, Santos SMD, Jordan H, Kuzikov M, et al. Targeting CYP2J to reduce paclitaxel-induced peripheral neuropathic pain. Proc Natl Acad Sci USA. 2016;113(44):12544–9.
Gavva NR, Treanor JJ, Garami A, Fang L, Surapaneni S, Akrami A, et al. Pharmacological blockade of the vanilloid receptor TRPV1 elicits marked hyperthermia in humans. Pain. 2008;136(1–2):202–10.
Carrasco C, Naziroglu M, Rodriguez AB, Pariente JA. Neuropathic pain: delving into the oxidative origin and the possible implication of transient receptor potential channels. Front Physiol. 2018;14:9.
Khasabova IA, Khasabov SG, Olson JK, Uhelski ML, Kim AH, Albino-Ramirez AM, et al. Pioglitazone, a PPARgamma agonist, reduces cisplatin-evoked neuropathic pain by protecting against oxidative stress. Pain. 2019;160(3):688–701.
Mansouri MT, Naghizadeh B, Ghorbanzadeh B, Rajabi H, Pashmforoush M. Pharmacological evidence for systemic and peripheral antinociceptive activities of pioglitazone in the rat formalin test: role of PPARgamma and nitric oxide. Eur J Pharmacol. 2017;15(805):84–92.
Shigematsu N, Kawashiri T, Kobayashi D, Shimizu S, Mine K, Hiromoto S, et al. Neuroprotective effect of alogliptin on oxaliplatin-induced peripheral neuropathy in vivo and in vitro. Sci Rep. 2020;10(1):6734.
Miyagi A, Kawashiri T, Shimizu S, Shigematsu N, Kobayashi D, Shimazoe T. Dimethyl fumarate attenuates oxaliplatin-induced peripheral neuropathy without affecting the anti-tumor activity of oxaliplatin in rodents. Biol Pharm Bull. 2019;42(4):638–44.
Kawashiri T, Shimizu S, Shigematsu N, Kobayashi D, Shimazoe T. Donepezil ameliorates oxaliplatin-induced peripheral neuropathy via a neuroprotective effect. J Pharmacol Sci. 2019;140(3):291–4.
Yamamoto S, Yamashita T, Ito M, Caaveiro JMM, Egashira N, Tozaki-Saitoh H, et al. New pharmacological effect of fulvestrant to prevent oxaliplatin-induced neurodegeneration and mechanical allodynia in rats. Int J Cancer. 2019;145(8):2107–13.
Chen YF, Chen LH, Yeh YM, Wu PY, Chen YF, Chang LY, et al. Minoxidil is a potential neuroprotective drug for paclitaxel-induced peripheral neuropathy. Sci Rep. 2017;28(7):45366.
Boyle Y, Fernando D, Kurz H, Miller SR, Zucchetto M, Storey J. The effect of a combination of gabapentin and donepezil in an experimental pain model in healthy volunteers: results of a randomized controlled trial. Pain. 2014;155(12):2510–6.
Jarada TN, Rokne JG, Alhajj R. A review of computational drug repositioning: strategies, approaches, opportunities, challenges, and directions. J Cheminform. 2020;12(1):46.
Gns HS, Gr S, Murahari M, Krishnamurthy M. An update on drug repurposing: re-written saga of the drug’s fate. Biomed Pharmacother. 2019;110:700–16.
Sidders B, Karlsson A, Kitching L, Torella R, Karila P, Phelan A. Network-based drug discovery: coupling network pharmacology with phenotypic screening for neuronal excitability. J Mol Biol. 2018;430(18 Pt A):3005–15.
Jayakar S, Shim J, Jo S, Bean BP, Singec I, Woolf CJ. Developing nociceptor-selective treatments for acute and chronic pain. Sci Transl Med. 2021;13(619):eabj9837.
Cudkowicz ME, Titus S, Kearney M, Yu H, Sherman A, Schoenfeld D, et al. Safety and efficacy of ceftriaxone for amyotrophic lateral sclerosis: a multi-stage, randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2014;13(11):1083–91.
Lewerenz J, Albrecht P, Tien ML, Henke N, Karumbayaram S, Kornblum HI, et al. Induction of Nrf2 and xCT are involved in the action of the neuroprotective antibiotic ceftriaxone in vitro. J Neurochem. 2009;111(2):332–43.
Rastegar-Mojarad M, Ye Z, Kolesar JM, Hebbring SJ, Lin SM. Opportunities for drug repositioning from phenome-wide association studies. Nat Biotechnol. 2015;33(4):342–5.
Niculescu AB, Le-Niculescu H, Levey DF, Roseberry K, Soe KC, Rogers J, et al. Towards precision medicine for pain: diagnostic biomarkers and repurposed drugs. Mol Psychiatry. 2019;24(4):501–22.
Sim-Selley LJ, Wilkerson JL, Burston JJ, Hauser KF, McLane V, Welch SP, et al. Differential tolerance to FTY720-induced antinociception in acute thermal and nerve injury mouse pain models: role of sphingosine-1-phosphate receptor adaptation. J Pharmacol Exp Ther. 2018;366(3):509–18.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by Grants SFB1039 A09 and Z01 of the Deutsche Forschungsgemeinschaft (German Research Foundation) and from the Fraunhofer Foundation Project: Neuropathic Pain as well as the Fraunhofer Cluster of Excellence for Immune-Mediated Diseases (CIMD).
Ethics approval
Not applicable.
Informed consent
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Availability of data and material
Not applicable.
Author’s contributions
MS performed literature search and screening of available data and wrote the manuscript. PG and GG contributed, edited and critically reviewed the manuscript. GG supervised the project. All authors have read and approved the final version of the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Sisignano, M., Gribbon, P. & Geisslinger, G. Drug Repurposing to Target Neuroinflammation and Sensory Neuron-Dependent Pain. Drugs 82, 357–373 (2022). https://doi.org/10.1007/s40265-022-01689-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-022-01689-0