Abstract
In oncology, and especially in the treatment of non-small-cell lung cancer (NSCLC), dose optimization is often a neglected part of precision medicine. Many drugs are still being administered in “one dose fits all” regimens or based on parameters that are often only minor determinants for systemic exposure. These dosing approaches often introduce additional pharmacokinetic variability and do not add to treatment outcomes. Fortunately, pharmacological knowledge is increasing, providing valuable information regarding the potential of, for example, therapeutic drug monitoring. This article focuses on the evidence for the most promising and easily implemented optimized dosing approaches for the small-molecule inhibitors, chemotherapeutic agents, and monoclonal antibodies as treatment options currently approved for NSCLC. Despite limitations such as investigations having been conducted in oncological diseases other than NSCLC or the retrospective origin of many analyses, an alternative dosing regimen could be beneficial for treatment outcomes, prescriber convenience, or financial burden on healthcare systems. This review of the literature provides recommendations on the implementation of dose optimization and advice regarding promising strategies that deserve further research in NSCLC.
Similar content being viewed by others
References
Lyman GH. Impact of chemotherapy dose intensity on cancer patient outcomes. J Natl Compr Canc Netw. 2009;7(1):99–108. https://doi.org/10.6004/jnccn.2009.0009.
Maloney A. A new paradigm. “Learn-Learn More”; dose-exposure-response at the center of drug development and regulatory approval. Clin Pharmacol Ther. 2017;102(6):942–50. https://doi.org/10.1002/cpt.710.
Mathijssen RH, Sparreboom A, Verweij J. Determining the optimal dose in the development of anticancer agents. Nat Rev Clin Oncol. 2014;11(5):272–81. https://doi.org/10.1038/nrclinonc.2014.40.
Rybak MJ, Le J, Lodise T, Levine D, Bradley J, Liu C, et al. Executive summary: therapeutic monitoring of vancomycin for serious methicillin-resistant staphylococcus aureus infections: a revised consensus guideline and review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists. J Pediatr Infect Dis Soc. 2020;9(3):281–4. https://doi.org/10.1093/jpids/piaa057.
Hiemke C, Bergemann N, Clement HW, Conca A, Deckert J, Domschke K, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry. 2018;51(1–02): e1. https://doi.org/10.1055/s-0037-1600991.
Brunet M, van Gelder T, Åsberg A, Haufroid V, Hesselink DA, Langman L, et al. Therapeutic drug monitoring of tacrolimus-personalized therapy: second consensus report. Ther Drug Monit. 2019;41(3):261–307. https://doi.org/10.1097/ftd.0000000000000640.
van Dijkman SC, Wicha SG, Danhof M, Della Pasqua OE. Individualized dosing algorithms and therapeutic monitoring for antiepileptic drugs. Clin Pharmacol Ther. 2018;103(4):663–73. https://doi.org/10.1002/cpt.777.
Touw DJ, Neef C, Thomson AH, Vinks AA. Cost-effectiveness of therapeutic drug monitoring: a systematic review. Ther Drug Monit. 2005;27(1):10–7. https://doi.org/10.1097/00007691-200502000-00004.
The Global Cancer Observatory. Cancer fact sheet trachea, bronchus and lung; 2020. Accessed 14 Apr 2021.
Toschi L, Rossi S, Finocchiaro G, Santoro A. Non-small cell lung cancer treatment (r)evolution: ten years of advances and more to come. Ecancermedicalscience. 2017;11:787. https://doi.org/10.3332/ecancer.2017.787.
Groenland SL, Mathijssen RHJ, Beijnen JH, Huitema ADR, Steeghs N. Individualized dosing of oral targeted therapies in oncology is crucial in the era of precision medicine. Eur J Clin Pharmacol. 2019;75(9):1309–18. https://doi.org/10.1007/s00228-019-02704-2.
Maloney A. Personalized dosing = approved wide dose ranges + dose titration. Clin Pharmacol Ther. 2021;109(3):566–7. https://doi.org/10.1002/cpt.1997.
Lyauk YK, Jonker DM, Lund TM. Dose finding in the clinical development of 60 US Food and Drug Administration-approved drugs compared with learning vs. confirming recommendations. Clin Transl Sci. 2019;12(5):481–9. https://doi.org/10.1111/cts.12641.
Salgia R, Pharaon R, Mambetsariev I, Nam A, Sattler M. The improbable targeted therapy: KRAS as an emerging target in non-small cell lung cancer (NSCLC). Cell Rep Med. 2021;2(1): 100186. https://doi.org/10.1016/j.xcrm.2020.100186.
de Wit D, Guchelaar HJ, den Hartigh J, Gelderblom H, van Erp NP. Individualized dosing of tyrosine kinase inhibitors: are we there yet? Drug Discov Today. 2015;20(1):18–36. https://doi.org/10.1016/j.drudis.2014.09.007.
Verheijen RB, Yu H, Schellens JHM, Beijnen JH, Steeghs N, Huitema ADR. Practical recommendations for therapeutic drug monitoring of kinase inhibitors in oncology. Clin Pharmacol Ther. 2017;102(5):765–76. https://doi.org/10.1002/cpt.787.
Urata Y, Katakami N, Morita S, Kaji R, Yoshioka H, Seto T, et al. Randomized phase III study comparing gefitinib with erlotinib in patients with previously treated advanced lung adenocarcinoma: WJOG 5108L. J Clin Oncol. 2016;34(27):3248–57. https://doi.org/10.1200/jco.2015.63.4154.
Li D, Ambrogio L, Shimamura T, Kubo S, Takahashi M, Chirieac LR, et al. BIBW2992, an irreversible EGFR/HER2 inhibitor highly effective in preclinical lung cancer models. Oncogene. 2008;27(34):4702–11. https://doi.org/10.1038/onc.2008.109.
Park K, Tan EH, O’Byrne K, Zhang L, Boyer M, Mok T, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-Lung 7): a phase 2B, open-label, randomised controlled trial. Lancet Oncol. 2016;17(5):577–89. https://doi.org/10.1016/s1470-2045(16)30033-x.
Wu YL, Cheng Y, Zhou X, Lee KH, Nakagawa K, Niho S, et al. Dacomitinib versus gefitinib as first-line treatment for patients with EGFR-mutation-positive non-small-cell lung cancer (ARCHER 1050): a randomised, open-label, phase 3 trial. Lancet Oncol. 2017;18(11):1454–66. https://doi.org/10.1016/s1470-2045(17)30608-3.
Xin S, Zhao Y, Wang X, Huang Y, Zhang J, Guo Y, et al. The dissociation of gefitinib trough concentration and clinical outcome in NSCLC patients with EGFR sensitive mutations. Sci Rep. 2015;5:12675. https://doi.org/10.1038/srep12675.
Food and Drug Administration. Center for drug evaluation and research. Clinical pharmacology and biopharmaceutics review(s) NDA 206995 review-Gefitinib. 2014.
European Medicines Agency. Tarceva: EPAR-Scientific Discussion. 2005.
Miyamoto S, Azuma K, Ishii H, Bessho A, Hosokawa S, Fukamatsu N, et al. Low-dose erlotinib treatment in elderly or frail patients with EGFR mutation-positive non-small cell lung cancer: a multicenter phase 2 trial. JAMA Oncol. 2020;6(7): e201250. https://doi.org/10.1001/jamaoncol.2020.1250.
Lampson BL, Nishino M, Dahlberg SE, Paul D, Santos AA, Jänne PA, et al. Activity of erlotinib when dosed below the maximum tolerated dose for EGFR-mutant lung cancer: Implications for targeted therapy development. Cancer. 2016;122(22):3456–63. https://doi.org/10.1002/cncr.30270.
Lind JS, Postmus PE, Heideman DA, Thunnissen EB, Bekers O, Smit EF. Dramatic response to low-dose erlotinib of epidermal growth factor receptor mutation-positive recurrent non-small cell lung cancer after severe cutaneous toxicity. J Thorac Oncol. 2009;4(12):1585–6. https://doi.org/10.1097/JTO.0b013e3181bbb2b9.
Yeo WL, Riely GJ, Yeap BY, Lau MW, Warner JL, Bodio K, et al. Erlotinib at a dose of 25 mg daily for non-small cell lung cancers with EGFR mutations. J Thorac Oncol. 2010;5(7):1048–53. https://doi.org/10.1097/JTO.0b013e3181dd1386.
Satoh H, Inoue A, Kobayashi K, Maemondo M, Oizumi S, Isobe H, et al. Low-dose gefitinib treatment for patients with advanced non-small cell lung cancer harboring sensitive epidermal growth factor receptor mutations. J Thorac Oncol. 2011;6(8):1413–7. https://doi.org/10.1097/JTO.0b013e31821d43a8.
Kwok WC, Ho JCM, Tam TCC, Lui MMS, Ip MSM, Lam DCL. Efficacy of gefitinib at reduced dose in EGFR mutant non-small cell lung carcinoma. Anticancer Drugs. 2019;30(10):1048–51. https://doi.org/10.1097/cad.0000000000000849.
Hirano T, Yasuda H, Tani T, Hamamoto J, Oashi A, Ishioka K, et al. In vitro modeling to determine mutation specificity of EGFR tyrosine kinase inhibitors against clinically relevant EGFR mutants in non-small-cell lung cancer. Oncotarget. 2015;6(36):38789–803. https://doi.org/10.18632/oncotarget.5887.
European Medicines Agency. Tarceva: EPAR-product information. 2019.
Foo J, Chmielecki J, Pao W, Michor F. Effects of pharmacokinetic processes and varied dosing schedules on the dynamics of acquired resistance to erlotinib in EGFR-mutant lung cancer. J Thorac Oncol. 2012;7(10):1583–93. https://doi.org/10.1097/JTO.0b013e31826146ee.
Hayakawa H, Ichihara E, Ohashi K, Ninomiya T, Yasugi M, Takata S, et al. Lower gefitinib dose led to earlier resistance acquisition before emergence of T790M mutation in epidermal growth factor receptor-mutated lung cancer model. Cancer Sci. 2013;104(11):1440–6. https://doi.org/10.1111/cas.12284.
Fiala O, Hosek P, Pesek M, Finek J, Racek J, Stehlik P, et al. Serum concentration of erlotinib and its correlation with outcome and toxicity in patients with advanced-stage NSCLC. Anticancer Res. 2017;37(11):6469–76. https://doi.org/10.21873/anticanres.12102.
Yamada K, Miyamoto S, Azuma K, Ishii H, Bessho A, Fukamatsu N, et al. A multicenter phase II study of low-dose erlotinib in frail patients with EGFR mutation-positive, non-small cell lung cancer: thoracic oncology research group (TORG) trial 1425. J Clin Oncol. 2018;36:9063.
Timmers L, Boons CC, Moes-Ten Hove J, Smit EF, van de Ven PM, Aerts JG, et al. Adherence, exposure and patients’ experiences with the use of erlotinib in non-small cell lung cancer. J Cancer Res Clin Oncol. 2015;141(8):1481–91. https://doi.org/10.1007/s00432-015-1935-0.
Ding PN, Lord SJ, Gebski V, Links M, Bray V, Gralla RJ, et al. Risk of treatment-related toxicities from egfr tyrosine kinase inhibitors: a meta-analysis of clinical trials of gefitinib, erlotinib, and afatinib in advanced EGFR-mutated non-small cell lung cancer. J Thorac Oncol. 2017;12(4):633–43. https://doi.org/10.1016/j.jtho.2016.11.2236.
Greig MJ, Niessen S, Weinrich SL, Feng JL, Shi M, Johnson TO. Effects of activating mutations on EGFR cellular protein turnover and amino acid recycling determined using SILAC mass spectrometry. Int J Cell Biol. 2015;2015: 798936. https://doi.org/10.1155/2015/798936.
Engelman JA, Zejnullahu K, Gale CM, Lifshits E, Gonzales AJ, Shimamura T, et al. PF00299804, an irreversible pan-ERBB inhibitor, is effective in lung cancer models with EGFR and ERBB2 mutations that are resistant to gefitinib. Cancer Res. 2007;67(24):11924–32. https://doi.org/10.1158/0008-5472.Can-07-1885.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 201292 Review–Afatinib; 2012.
Brown K, Comisar C, Witjes H, Maringwa J, de Greef R, Vishwanathan K, et al. Population pharmacokinetics and exposure-response of osimertinib in patients with non-small cell lung cancer. Br J Clin Pharmacol. 2017;83(6):1216–26. https://doi.org/10.1111/bcp.13223.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 211288 Review–Dacomitinib. 2018.
Yates JW, Ashton S, Cross D, Mellor MJ, Powell SJ, Ballard P. Irreversible inhibition of EGFR: modeling the combined pharmacokinetic-pharmacodynamic relationship of osimertinib and its active metabolite AZ5104. Mol Cancer Ther. 2016;15(10):2378–87. https://doi.org/10.1158/1535-7163.Mct-16-0142.
Nakao K, Kobuchi S, Marutani S, Iwazaki A, Tamiya A, Isa S, et al. Population pharmacokinetics of afatinib and exposure-safety relationships in Japanese patients with EGFR mutation-positive non-small cell lung cancer. Sci Rep. 2019;9(1):18202. https://doi.org/10.1038/s41598-019-54804-9.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 208065 Review–Osimertinib. 2015.
Sonobe S, Taniguchi Y, Saijo N, Naoki Y, Tamiya A, Omachi N, et al. 1381—the efficacy of a reduced dose (40mg) of Osimertinib with T790M-positive advanced non-small-cell lung cancer (427P). Esmo Asia. 2017.
Fang W, Huang Y, Gan J, Shao YW, Zhang L. Durable Response of low-dose afatinib plus cetuximab in an adenocarcinoma patient with a novel EGFR exon 20 insertion mutation. J Thorac Oncol. 2019;14(10):e220–1. https://doi.org/10.1016/j.jtho.2019.05.023.
Nakamura A, Tanaka H, Saito R, Suzuki A, Harada T, Inoue S, et al. Phase II study of low-dose afatinib maintenance treatment among patients with EGFR-mutated non-small cell lung cancer: North Japan Lung Cancer Study Group Trial 1601 (NJLCG1601). Oncologist. 2020;25(10):e1451–6. https://doi.org/10.1634/theoncologist.2020-0545.
Yokoyama T, Yoshioka H, Fujimoto D, Demura Y, Hirano K, Kawai T, et al. A phase II study of low starting dose of afatinib as first-line treatment in patients with EGFR mutation-positive non-small-cell lung cancer (KTORG1402). Lung Cancer. 2019;135:175–80. https://doi.org/10.1016/j.lungcan.2019.03.030.
Food and Drug Administration. FDA grants accelerated approval to sotorasib for KRAS G12C mutated NSCLC. https://fda.gov. Accessed 12 July 2021.
Amgen. Press release, Amgen Provides Updated Information On LUMAKRAS™ (Sotorasib) Dose Comparison Study. https://amgen.com. Accessed 12 July 2021.
Shaw AT, Kim DW, Nakagawa K, Seto T, Crinó L, Ahn MJ, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368(25):2385–94. https://doi.org/10.1056/NEJMoa1214886.
Peters S, Camidge DR, Shaw AT, Gadgeel S, Ahn JS, Kim DW, et al. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med. 2017;377(9):829–38. https://doi.org/10.1056/NEJMoa1704795.
Soria JC, Tan DSW, Chiari R, Wu YL, Paz-Ares L, Wolf J, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet. 2017;389(10072):917–29. https://doi.org/10.1016/S0140-6736(17)30123-X.
Solomon BJ, Besse B, Bauer TM, Felip E, Soo RA, Camidge DR, et al. Lorlatinib in patients with ALK-positive non-small-cell lung cancer: results from a global phase 2 study. Lancet Oncol. 2018;19(12):1654–67. https://doi.org/10.1016/s1470-2045(18)30649-1.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 202570 Review–Crizotinib. 2011.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 208434 Review–Alectinib. 2015.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 205755 Review–Ceritinib. 2014.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 208772 Review–Brigatinib. 2016.
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review(s) NDA 210868 Review–Lorlatinib. 2018.
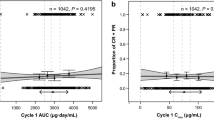
Groenland SL, Geel DR, Janssen JM, de Vries N, Rosing H, Beijnen JH, et al. Exposure-response analyses of anaplastic lymphoma kinase inhibitors crizotinib and alectinib in non-small cell lung cancer patients. Clin Pharmacol Ther. 2021;109(2):394–402. https://doi.org/10.1002/cpt.1989.
Mueller-Schoell A, Groenland SL, Scherf-Clavel O, van Dyk M, Huisinga W, Michelet R, et al. Therapeutic drug monitoring of oral targeted antineoplastic drugs. Eur J Clin Pharmacol. 2021;77(4):441–64. https://doi.org/10.1007/s00228-020-03014-8.
Gupta N, Wang X, Offman E, Rich B, Kerstein D, Hanley M, et al. Brigatinib dose rationale in anaplastic lymphoma kinase-positive non-small cell lung cancer: exposure-response analyses of pivotal ALTA Study. CPT Pharmacometr Syst Pharmacol. 2020;9(12):718–30. https://doi.org/10.1002/psp4.12569.
Yamazaki S. Translational modeling and simulation for molecularly targeted small molecule anticancer agents: case studies of multiple tyrosine kinase inhibitors, crizotinib and lorlatinib. In: Giordanetto FG, editor. Early drug development. 2018. https://doi.org/10.1002/9783527801756.ch16.
Planchard D, Smit EF, Groen HJM, Mazieres J, Besse B, Helland Å, et al. Dabrafenib plus trametinib in patients with previously untreated BRAFV600E-mutant metastatic non-small-cell lung cancer: an open-label, phase 2 trial. Lancet Oncol. 2017;18(10):1307–16. https://doi.org/10.1016/S1470-2045(17)30679-4.
Ouellet D, Kassir N, Chiu J, Mouksassi MS, Leonowens C, Cox D, et al. Population pharmacokinetics and exposure-response of trametinib, a MEK inhibitor, in patients with BRAF V600 mutation-positive melanoma. Cancer Chemother Pharmacol. 2016;77(4):807–17. https://doi.org/10.1007/s00280-016-2993-y.
Groenland SL, Janssen JM, Nijenhuis C, de Vries N, Rosing H, Wilgenhof S, et al. 567P Exposure-response analyses of dabrafenib and trametinib in melanoma patients. Ann Oncol. 2020;31:S486–7.
Corcoran RB, Settleman J, Engelman JA. Potential therapeutic strategies to overcome acquired resistance to BRAF or MEK inhibitors in BRAF mutant cancers. Oncotarget. 2011;2(4):336–46. https://doi.org/10.18632/oncotarget.262.
Ranzani M, Alifrangis C, Perna D, Dutton-Regester K, Pritchard A, Wong K, et al. BRAF/NRAS wild-type melanoma, NF1 status and sensitivity to trametinib. Pigment Cell Melanoma Res. 2015;28(1):117–9. https://doi.org/10.1111/pcmr.12316.
European Medicines Agency. Assessment report 315207, Mekinist and Tafinlar. 2017.
Corcoran RB, Atreya CE, Falchook GS, Kwak EL, Ryan DP, Bendell JC, et al. Combined BRAF and MEK inhibition with dabrafenib and trametinib in BRAF V600-mutant colorectal cancer. J Clin Oncol. 2015;33(34):4023–31. https://doi.org/10.1200/jco.2015.63.2471.
Stones CJ, Kim JE, Joseph WR, Leung E, Marshall ES, Finlay GJ, et al. Comparison of responses of human melanoma cell lines to MEK and BRAF inhibitors. Front Genet. 2013;4:66. https://doi.org/10.3389/fgene.2013.00066.
Liu L, Mayes PA, Eastman S, Shi H, Yadavilli S, Zhang T, et al. The BRAF and MEK inhibitors dabrafenib and trametinib: effects on immune function and in combination with immunomodulatory antibodies targeting PD-1, PD-L1, and CTLA-4. Clin Cancer Res. 2015;21(7):1639–51. https://doi.org/10.1158/1078-0432.Ccr-14-2339.
Scatena C, Franceschi S, Franzini M, Sanguinetti C, Romiti N, Caponi L, et al. Dabrafenib and trametinib prolong coagulation through the inhibition of tissue factor in BRAF(v600e) mutated melanoma cells in vitro. Cancer Cell Int. 2019;19:223. https://doi.org/10.1186/s12935-019-0938-3.
Negrao MV, Raymond VM, Lanman RB, Robichaux JP, He J, Nilsson MB, et al. Molecular landscape of BRAF-mutant NSCLC reveals an association between clonality and driver mutations and identifies targetable non-V600 driver mutations. J Thorac Oncol. 2020;15(10):1611–23. https://doi.org/10.1016/j.jtho.2020.05.021.
Doebele RC, Drilon A, Paz-Ares L, Siena S, Shaw AT, Farago AF, et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours: integrated analysis of three phase 1–2 trials. Lancet Oncol. 2020;21(2):271–82. https://doi.org/10.1016/s1470-2045(19)30691-6.
Food and Drug Administration. Center for Drug Evaluation and Research. Multi-disciplinary Review and Evaluation NDA 210861 and NDA 211710–larotrectinib. 2018.
Yu H, Steeghs N, Nijenhuis CM, Schellens JH, Beijnen JH, Huitema AD. Practical guidelines for therapeutic drug monitoring of anticancer tyrosine kinase inhibitors: focus on the pharmacokinetic targets. Clin Pharmacokinet. 2014;53(4):305–25. https://doi.org/10.1007/s40262-014-0137-2.
Di Maio M, Gridelli C, Gallo C, Shepherd F, Piantedosi FV, Cigolari S, et al. Chemotherapy-induced neutropenia and treatment efficacy in advanced non-small-cell lung cancer: a pooled analysis of three randomised trials. Lancet Oncol. 2005;6(9):669–77. https://doi.org/10.1016/s1470-2045(05)70255-2.
Kishida Y, Kawahara M, Teramukai S, Kubota K, Komuta K, Minato K, et al. Chemotherapy-induced neutropenia as a prognostic factor in advanced non-small-cell lung cancer: results from Japan Multinational Trial Organization LC00-03. Br J Cancer. 2009;101(9):1537–42. https://doi.org/10.1038/sj.bjc.6605348.
Centanni M, Krishnan SM, Friberg LE. Model-based dose individualization of sunitinib in gastrointestinal stromal tumors. Clin Cancer Res. 2020;26(17):4590–8. https://doi.org/10.1158/1078-0432.Ccr-20-0887.
Wallin JE, Friberg LE, Karlsson MO. Model-based neutrophil-guided dose adaptation in chemotherapy: evaluation of predicted outcome with different types and amounts of information. Basic Clin Pharmacol Toxicol. 2010;106(3):234–42. https://doi.org/10.1111/j.1742-7843.2009.00520.x.
Elferink F, van der Vijgh WJ, Klein I, Vermorken JB, Gall HE, Pinedo HM. Pharmacokinetics of carboplatin after i.v. administration. Cancer Treat Rep. 1987;71(12):1231–7.
Ivanov AI, Christodoulou J, Parkinson JA, Barnham KJ, Tucker A, Woodrow J, et al. Cisplatin binding sites on human albumin. J Biol Chem. 1998;273(24):14721–30. https://doi.org/10.1074/jbc.273.24.14721.
Schellens JH, Ma J, Planting AS, van der Burg ME, van Meerten E, de Boer-Dennert M, et al. Relationship between the exposure to cisplatin, DNA-adduct formation in leucocytes and tumour response in patients with solid tumours. Br J Cancer. 1996;73(12):1569–75. https://doi.org/10.1038/bjc.1996.296.
Campbell AB, Kalman SM, Jacobs C. Plasma platinum levels: relationship to cisplatin dose and nephrotoxicity. Cancer Treat Rep. 1983;67(2):169–72.
Reece PA, Stafford I, Russell J, Khan M, Gill PG. Creatinine clearance as a predictor of ultrafilterable platinum disposition in cancer patients treated with cisplatin: relationship between peak ultrafilterable platinum plasma levels and nephrotoxicity. J Clin Oncol. 1987;5(2):304–9. https://doi.org/10.1200/jco.1987.5.2.304.
Ibrahim ME, Chang C, Hu Y, Hogan SL, Mercke N, Gomez M, et al. Pharmacokinetic determinants of cisplatin-induced subclinical kidney injury in oncology patients. Eur J Clin Pharmacol. 2019;75(1):51–7. https://doi.org/10.1007/s00228-018-2552-z.
Mense ES, Smit AAJ, Crul M, Franssen EJF. The effect of rapid infusion of cisplatin on nephrotoxicity in patients with lung carcinoma. J Clin Pharm Ther. 2019;44(2):249–57. https://doi.org/10.1111/jcpt.12781.
Chatelut E, White-Koning ML, Mathijssen RH, Puisset F, Baker SD, Sparreboom A. Dose banding as an alternative to body surface area-based dosing of chemotherapeutic agents. Br J Cancer. 2012;107(7):1100–6. https://doi.org/10.1038/bjc.2012.357.
Schmitt A, Gladieff L, Laffont CM, Evrard A, Boyer JC, Lansiaux A, et al. Factors for hematopoietic toxicity of carboplatin: refining the targeting of carboplatin systemic exposure. J Clin Oncol. 2010;28(30):4568–74. https://doi.org/10.1200/jco.2010.29.3597.
Jodrell DI, Egorin MJ, Canetta RM, Langenberg P, Goldbloom EP, Burroughs JN, et al. Relationships between carboplatin exposure and tumor response and toxicity in patients with ovarian cancer. J Clin Oncol. 1992;10(4):520–8. https://doi.org/10.1200/jco.1992.10.4.520.
Calvert AH, Newell DR, Gumbrell LA, O’Reilly S, Burnell M, Boxall FE, et al. Carboplatin dosage: prospective evaluation of a simple formula based on renal function. J Clin Oncol. 1989;7(11):1748–56. https://doi.org/10.1200/jco.1989.7.11.1748.
Delanaye P, Ebert N, Melsom T, Gaspari F, Mariat C, Cavalier E, et al. Iohexol plasma clearance for measuring glomerular filtration rate in clinical practice and research: a review. Part 1: How to measure glomerular filtration rate with iohexol? Clin Kidney J. 2016;9(5):682–99. https://doi.org/10.1093/ckj/sfw070.
Dowling TC, Wang ES, Ferrucci L, Sorkin JD. Glomerular filtration rate equations overestimate creatinine clearance in older individuals enrolled in the Baltimore Longitudinal Study on Aging: impact on renal drug dosing. Pharmacotherapy. 2013;33(9):912–21. https://doi.org/10.1002/phar.1282.
Ekhart C, de Jonge ME, Huitema AD, Schellens JH, Rodenhuis S, Beijnen JH. Flat dosing of carboplatin is justified in adult patients with normal renal function. Clin Cancer Res. 2006;12(21):6502–8. https://doi.org/10.1158/1078-0432.Ccr-05-1076.
Millward MJ, Webster LK, Toner GC, Bishop JF, Rischin D, Stokes KH, et al. Carboplatin dosing based on measurement of renal function–experience at the Peter MacCallum Cancer Institute. Aust N Z J Med. 1996;26(3):372–9. https://doi.org/10.1111/j.1445-5994.1996.tb01925.x.
Schmitt A, Gladieff L, Lansiaux A, Bobin-Dubigeon C, Etienne-Grimaldi MC, Boisdron-Celle M, et al. A universal formula based on cystatin C to perform individual dosing of carboplatin in normal weight, underweight, and obese patients. Clin Cancer Res. 2009;15(10):3633–9. https://doi.org/10.1158/1078-0432.Ccr-09-0017.
Beunders R, van Groenendael R, Leijte GP, Kox M, Pickkers P. Proenkephalin compared to conventional methods to assess kidney function in critically ill sepsis patients. Shock. 2020;54(3):308–14. https://doi.org/10.1097/shk.0000000000001510.
Harris BDW, Phan V, Perera V, Szyc A, Galettis P, Martin JH, et al. Inability of current dosing to achieve carboplatin therapeutic targets in people with advanced non-small cell lung cancer: impact of systemic inflammation on carboplatin exposure and clinical outcomes. Clin Pharmacokinet. 2020;59(8):1013–26. https://doi.org/10.1007/s40262-020-00870-6.
Veal GJ, Errington J, Tilby MJ, Pearson ADJ, Foot ABM, McDowell H, et al. Adaptive dosing and platinum-DNA adduct formation in children receiving high-dose carboplatin for the treatment of solid tumours. Br J Cancer. 2007;96(5):725–31. https://doi.org/10.1038/sj.bjc.6603607.
Veal GJ, Errington J, Hayden J, Hobin D, Murphy D, Dommett RM, et al. Carboplatin therapeutic monitoring in preterm and full-term neonates. Eur J Cancer. 2015;51(14):2022–30. https://doi.org/10.1016/j.ejca.2015.07.011.
Picton SV, Keeble J, Holden V, Errington J, Boddy AV, Veal GJ. Therapeutic monitoring of carboplatin dosing in a premature infant with retinoblastoma. Cancer Chemother Pharmacol. 2009;63(4):749–52. https://doi.org/10.1007/s00280-008-0787-6.
Mendelsohn LG, Shih C, Chen VJ, Habeck LL, Gates SB, Shackelford KA. Enzyme inhibition, polyglutamation, and the effect of LY231514 (MTA) on purine biosynthesis. Semin Oncol. 1999;26(2 Suppl 6):42–7.
Shih C, Chen VJ, Gossett LS, Gates SB, MacKellar WC, Habeck LL, et al. LY231514, a pyrrolo[2,3-d]pyrimidine-based antifolate that inhibits multiple folate-requiring enzymes. Cancer Res. 1997;57(6):1116–23.
Stoop MP, Visser S, van Dijk E, Aerts J, Stricker BH, Luider TM. High and individually variable enzymatic activity precludes accurate determination of pemetrexed, methotrexate and their polyglutamate metabolite concentrations in plasma. J Pharm Biomed Anal. 2018;148:89–92. https://doi.org/10.1016/j.jpba.2017.09.014.
Visser S, Koolen SLW, de Bruijn P, Belderbos HNA, Cornelissen R, Mathijssen RHJ, et al. Pemetrexed exposure predicts toxicity in advanced non-small-cell lung cancer: a prospective cohort study. Eur J Cancer. 2019;121:64–73. https://doi.org/10.1016/j.ejca.2019.08.012.
Latz JE, Karlsson MO, Rusthoven JJ, Ghosh A, Johnson RD. A semimechanistic-physiologic population pharmacokinetic/pharmacodynamic model for neutropenia following pemetrexed therapy. Cancer Chemother Pharmacol. 2006;57(4):412–26. https://doi.org/10.1007/s00280-005-0077-5.
Boosman RJ, Dorlo TPC, de Rouw N, Burgers JA, Dingemans AC, van den Heuvel MM, et al. Toxicity of pemetrexed during renal impairment explained - implications for safe treatment. Int J Cancer. 2021. https://doi.org/10.1002/ijc.33721.
Dickgreber NJ, Fink TH, Latz JE, Hossain AM, Musib LC, Thomas M. Phase I and pharmacokinetic study of pemetrexed plus cisplatin in chemonaive patients with locally advanced or metastatic malignant pleural mesothelioma or non-small cell lung cancer. Clin Cancer Res. 2009;15(1):382–9. https://doi.org/10.1158/1078-0432.Ccr-08-0128.
McDonald AC, Vasey PA, Adams L, Walling J, Woodworth JR, Abrahams T, et al. A phase I and pharmacokinetic study of LY231514, the multitargeted antifolate. Clin Cancer Res. 1998;4(3):605–10.
Rinaldi DA, Burris HA, Dorr FA, Woodworth JR, Kuhn JG, Eckardt JR, et al. Initial phase I evaluation of the novel thymidylate synthase inhibitor, LY231514, using the modified continual reassessment method for dose escalation. J Clin Oncol. 1995;13(11):2842–50. https://doi.org/10.1200/jco.1995.13.11.2842.
Rinaldi DA, Kuhn JG, Burris HA, Dorr FA, Rodriguez G, Eckhardt SG, et al. A phase I evaluation of multitargeted antifolate (MTA, LY231514), administered every 21 days, utilizing the modified continual reassessment method for dose escalation. Cancer Chemother Pharmacol. 1999;44(5):372–80. https://doi.org/10.1007/s002800050992.
Joerger M, Huitema AD, Krähenbühl S, Schellens JH, Cerny T, Reni M, et al. Methotrexate area under the curve is an important outcome predictor in patients with primary CNS lymphoma: A pharmacokinetic-pharmacodynamic analysis from the IELSG no. 20 trial. Br J Cancer. 2010;102(4):673–7. https://doi.org/10.1038/sj.bjc.6605559.
Latz JE, Chaudhary A, Ghosh A, Johnson RD. Population pharmacokinetic analysis of ten phase II clinical trials of pemetrexed in cancer patients. Cancer Chemother Pharmacol. 2006;57(4):401–11. https://doi.org/10.1007/s00280-005-0036-1.
de Rouw N, Boosman RJ, Huitema ADR, Hilbrands LB, Svensson EM, Derijks HJ, et al. Rethinking the application of pemetrexed for patients with renal impairment: a pharmacokinetic analysis. Clin Pharmacokinet. 2021;60(5):649–54. https://doi.org/10.1007/s40262-020-00972-1.
Bruno R, Hille D, Riva A, Vivier N, ten Bokkel Huinnink WW, van Oosterom AT, et al. Population pharmacokinetics/pharmacodynamics of docetaxel in phase II studies in patients with cancer. J Clin Oncol. 1998;16(1):187–96. https://doi.org/10.1200/jco.1998.16.1.187.
Chen N, Li Y, Ye Y, Palmisano M, Chopra R, Zhou S. Pharmacokinetics and pharmacodynamics of nab-paclitaxel in patients with solid tumors: disposition kinetics and pharmacology distinct from solvent-based paclitaxel. J Clin Pharmacol. 2014;54(10):1097–107. https://doi.org/10.1002/jcph.304.
Smorenburg CH, Sparreboom A, Bontenbal M, Stoter G, Nooter K, Verweij J. Randomized cross-over evaluation of body-surface area-based dosing versus flat-fixed dosing of paclitaxel. J Clin Oncol. 2003;21(2):197–202. https://doi.org/10.1200/jco.2003.01.058.
Charles KA, Rivory LP, Stockler MR, Beale P, Beith J, Boyer M, et al. Predicting the toxicity of weekly docetaxel in advanced cancer. Clin Pharmacokinet. 2006;45(6):611–22. https://doi.org/10.2165/00003088-200645060-00004.
Engels FK, Loos WJ, van der Bol JM, de Bruijn P, Mathijssen RH, Verweij J, et al. Therapeutic drug monitoring for the individualization of docetaxel dosing: a randomized pharmacokinetic study. Clin Cancer Res. 2011;17(2):353–62. https://doi.org/10.1158/1078-0432.Ccr-10-1636.
Bruno R, Olivares R, Berille J, Chaikin P, Vivier N, Hammershaimb L, et al. Alpha-1-acid glycoprotein as an independent predictor for treatment effects and a prognostic factor of survival in patients with non-small cell lung cancer treated with docetaxel. Clin Cancer Res. 2003;9(3):1077–82.
Ozawa K, Minami H, Sato H. Logistic regression analysis for febrile neutropenia (FN) induced by docetaxel in Japanese cancer patients. Cancer Chemother Pharmacol. 2008;62(3):551–7. https://doi.org/10.1007/s00280-007-0648-8.
Baker SD, Li J, ten Tije AJ, Figg WD, Graveland W, Verweij J, et al. Relationship of systemic exposure to unbound docetaxel and neutropenia. Clin Pharmacol Ther. 2005;77(1):43–53. https://doi.org/10.1016/j.clpt.2004.09.005.
Pallis AG, Agelaki S, Kakolyris S, Kotsakis A, Kalykaki A, Vardakis N, et al. Chemotherapy-induced neutropenia as a prognostic factor in patients with advanced non-small cell lung cancer treated with front-line docetaxel-gemcitabine chemotherapy. Lung Cancer. 2008;62(3):356–63. https://doi.org/10.1016/j.lungcan.2008.03.030.
Lombard A, Mistry H, Aarons L, Ogungbenro K. Dose individualisation in oncology using chemotherapy-induced neutropenia: example of docetaxel in non-small cell lung cancer patients. Br J Clin Pharmacol. 2021;87(4):2053–63. https://doi.org/10.1111/bcp.14614.
Joerger M, Huitema AD, Richel DJ, Dittrich C, Pavlidis N, Briasoulis E, et al. Population pharmacokinetics and pharmacodynamics of paclitaxel and carboplatin in ovarian cancer patients: a study by the European organization for research and treatment of cancer-pharmacology and molecular mechanisms group and new drug development group. Clin Cancer Res. 2007;13(21):6410–8. https://doi.org/10.1158/1078-0432.Ccr-07-0064.
Huizing MT, Giaccone G, van Warmerdam LJ, Rosing H, Bakker PJ, Vermorken JB, et al. Pharmacokinetics of paclitaxel and carboplatin in a dose-escalating and dose-sequencing study in patients with non-small-cell lung cancer. The European Cancer Centre. J Clin Oncol. 1997;15(1):317–29. https://doi.org/10.1200/jco.1997.15.1.317.
Jiko M, Yano I, Sato E, Takahashi K, Motohashi H, Masuda S, et al. Pharmacokinetics and pharmacodynamics of paclitaxel with carboplatin or gemcitabine, and effects of CYP3A5 and MDR1 polymorphisms in patients with urogenital cancers. Int J Clin Oncol. 2007;12(4):284–90. https://doi.org/10.1007/s10147-007-0681-y.
Xin DS, Zhou L, Li CZ, Zhang SQ, Huang HQ, Qiu GD, et al. TC > 0.05 as a pharmacokinetic parameter of paclitaxel for therapeutic efficacy and toxicity in cancer patients. Recent Pat Anticancer Drug Discov. 2018;13(3):341–7. https://doi.org/10.2174/1574892813666180305170439.
Mielke S, Sparreboom A, Steinberg SM, Gelderblom H, Unger C, Behringer D, et al. Association of Paclitaxel pharmacokinetics with the development of peripheral neuropathy in patients with advanced cancer. Clin Cancer Res. 2005;11(13):4843–50. https://doi.org/10.1158/1078-0432.Ccr-05-0298.
Hertz DL, Kidwell KM, Vangipuram K, Li F, Pai MP, Burness M, et al. Paclitaxel plasma concentration after the first infusion predicts treatment-limiting peripheral neuropathy. Clin Cancer Res. 2018;24(15):3602–10. https://doi.org/10.1158/1078-0432.Ccr-18-0656.
Joerger M, von Pawel J, Kraff S, Fischer JR, Eberhardt W, Gauler TC, et al. Open-label, randomized study of individualized, pharmacokinetically (PK)-guided dosing of paclitaxel combined with carboplatin or cisplatin in patients with advanced non-small-cell lung cancer (NSCLC). Ann Oncol. 2016;27(10):1895–902. https://doi.org/10.1093/annonc/mdw290.
Zhang J, Zhou F, Qi H, Ni H, Hu Q, Zhou C, et al. Randomized study of individualized pharmacokinetically-guided dosing of paclitaxel compared with body-surface area dosing in Chinese patients with advanced non-small cell lung cancer. Br J Clin Pharmacol. 2019;85(10):2292–301. https://doi.org/10.1111/bcp.13982.
Joerger M, Kraff S, Jaehde U, Hilger RA, Courtney JB, Cline DJ, et al. Validation of a commercial assay and decision support tool for routine paclitaxel therapeutic drug monitoring (TDM). Ther Drug Monit. 2017;39(6):617–24. https://doi.org/10.1097/ftd.0000000000000446.
Socinski MA, Manikhas GM, Stroyakovsky DL, Makhson AN, Cheporov SV, Orlov SV, et al. A dose finding study of weekly and every-3-week nab-Paclitaxel followed by carboplatin as first-line therapy in patients with advanced non-small cell lung cancer. J Thorac Oncol. 2010;5(6):852–61. https://doi.org/10.1097/jto.0b013e3181d5e39e.
Mini E, Nobili S, Caciagli B, Landini I, Mazzei T. Cellular pharmacology of gemcitabine. Ann Oncol. 2006;17(Suppl 5):v7-12. https://doi.org/10.1093/annonc/mdj941.
Qiu MT, Ding XX, Hu JW, Tian HY, Yin R, Xu L. Fixed-dose rate infusion and standard rate infusion of gemcitabine in patients with advanced non-small-cell lung cancer: a meta-analysis of six trials. Cancer Chemother Pharmacol. 2012;70(6):861–73. https://doi.org/10.1007/s00280-012-1974-z.
Patil V, Noronha V, Joshi A, Chougule A, Kannan S, Bhattacharjee A, et al. Phase III non-inferiority study evaluating efficacy and safety of low dose gemcitabine compared to standard dose gemcitabine with platinum in advanced squamous lung cancer. EClinicalMedicine. 2019;9:19–25. https://doi.org/10.1016/j.eclinm.2019.03.011.
Zwitter M, Kovac V, Smrdel U, Kocijancic I, Segedin B, Vrankar M. Phase I-II trial of low-dose gemcitabine in prolonged infusion and cisplatin for advanced non-small cell lung cancer. Anticancer Drugs. 2005;16(10):1129–34. https://doi.org/10.1097/00001813-200511000-00013.
Xiong JP, Feng M, Qiu F, Xu J, Tao QS, Zhang L, et al. Phase II trial of low-dose gemcitabine in prolonged infusion and cisplatin for advanced non-small cell lung cancer. Lung Cancer. 2008;60(2):208–14. https://doi.org/10.1016/j.lungcan.2007.10.004.
Kreidieh FY, Moukadem HA, El Saghir NS. Overview, prevention and management of chemotherapy extravasation. World J Clin Oncol. 2016;7(1):87–97. https://doi.org/10.5306/wjco.v7.i1.87.
Piccirillo MC, Daniele G, Di Maio M, Bryce J, De Feo G, Del Giudice A, et al. Vinorelbine for non-small cell lung cancer. Expert Opin Drug Saf. 2010;9(3):493–510. https://doi.org/10.1517/14740331003774078.
Wong M, Balleine RL, Blair EY, McLachlan AJ, Ackland SP, Garg MB, et al. Predictors of vinorelbine pharmacokinetics and pharmacodynamics in patients with cancer. J Clin Oncol. 2006;24(16):2448–55. https://doi.org/10.1200/jco.2005.02.1295.
Schott AF, Rae JM, Griffith KA, Hayes DF, Sterns V, Baker LH. Combination vinorelbine and capecitabine for metastatic breast cancer using a non-body surface area dosing scheme. Cancer Chemother Pharmacol. 2006;58(1):129–35. https://doi.org/10.1007/s00280-005-0132-2.
Kan M, Imaoka H, Watanabe K, Sasaki M, Takahashi H, Hashimoto Y, et al. Chemotherapy-induced neutropenia as a prognostic factor in patients with pancreatic cancer treated with gemcitabine plus nab-paclitaxel: a retrospective cohort study. Cancer Chemother Pharmacol. 2020;86(2):203–10. https://doi.org/10.1007/s00280-020-04110-3.
Brahmer JR, Drake CG, Wollner I, Powderly JD, Picus J, Sharfman WH, et al. Phase I study of single-agent anti-programmed death-1 (MDX-1106) in refractory solid tumors: safety, clinical activity, pharmacodynamics, and immunologic correlates. J Clin Oncol. 2010;28(19):3167–75. https://doi.org/10.1200/jco.2009.26.7609.
Elassaiss-Schaap K, Rossenu S, Lindauer A, Kang SP, de Greef R, Sachs JR, et al. Using model-based “Learn and Confirm” to reveal the pharmacokinetics-pharmacodynamics relationship of pembrolizumab in the KEYNOTE-001 trial. CPT Pharmacometr Syst Pharmacol. 2017;6(1):21–8.
Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–54. https://doi.org/10.1056/NEJMoa1200690.
Deng R, Bumbaca D, Pastuskovas CV, Boswell CA, West D, Cowan KJ, et al. Preclinical pharmacokinetics, pharmacodynamics, tissue distribution, and tumor penetration of anti-PD-L1 monoclonal antibody, an immune checkpoint inhibitor. MAbs. 2016;8(3):593–603. https://doi.org/10.1080/19420862.2015.1136043.
Song X, Pak M, Chavez C, Liang M, Lu H, Schwickart M, et al. Pharmacokinetics and pharmacodynamics of MEDI4736, a fully human anti-programmed death ligand 1 (PD-L1) monoclonal antibody, in patients with advanced solid tumors. J Clin Oncol. 2015;33(15_suppl):e14009–e. https://doi.org/10.1200/jco.2015.33.15_suppl.e14009.
Baverel PG, Dubois VFS, Jin CY, Zheng Y, Song X, Jin X, et al. Population pharmacokinetics of durvalumab in cancer patients and association with longitudinal biomarkers of disease status. Clin Pharmacol Ther. 2018;103(4):631–42. https://doi.org/10.1002/cpt.982.
Dai HI, Vugmeyster Y, Mangal N. Characterizing exposure-response relationship for therapeutic monoclonal antibodies in immuno-oncology and beyond: challenges, perspectives, and prospects. Clin Pharmacol Ther. 2020;108(6):1156–70. https://doi.org/10.1002/cpt.1953.
Turner DC, Kondic AG, Anderson KM, Robinson AG, Garon EB, Riess JW, et al. Pembrolizumab exposure-response assessments challenged by association of cancer cachexia and catabolic clearance. Clin Cancer Res. 2018;24(23):5841–9. https://doi.org/10.1158/1078-0432.Ccr-18-0415.
Agrawal S, Feng Y, Roy A, Kollia G, Lestini B. Nivolumab dose selection: challenges, opportunities, and lessons learned for cancer immunotherapy. J Immunother Cancer. 2016;4(72):eCollection 2016. https://doi.org/10.1186/s40425-016-0177-2.
Bajaj G, Wang X, Agrawal S, Gupta M, Roy A, Feng Y. Model-based population pharmacokinetic analysis of nivolumab in patients with solid tumors. CPT Pharmacometr Syst Pharmacol. 2017;6(1):58–66. https://doi.org/10.1002/psp4.12143.
Liu C, Yu J, Li H, Liu J, Xu Y, Song P, et al. Association of time-varying clearance of nivolumab with disease dynamics and its implications on exposure response analysis. Clin Pharmacol Ther. 2017;101(5):657–66. https://doi.org/10.1002/cpt.656.
Wang R, Zheng J, Shao X, Ishii Y, Roy A, Bello A, et al. Development of a prognostic composite cytokine signature based on the correlation with nivolumab clearance: translational PK/PD analysis in patients with renal cell carcinoma. J Immunother Cancer. 2019;7(1):348. https://doi.org/10.1186/s40425-019-0819-2.
Centanni M, Moes D, Trocóniz IF, Ciccolini J, van Hasselt JGC. Clinical pharmacokinetics and pharmacodynamics of immune checkpoint inhibitors. Clin Pharmacokinet. 2019;58(7):835–57. https://doi.org/10.1007/s40262-019-00748-2.
Hendrikx J, Haanen J, Voest EE, Schellens JHM, Huitema ADR, Beijnen JH. Fixed dosing of monoclonal antibodies in oncology. Oncologist. 2017;22(10):1212–21. https://doi.org/10.1634/theoncologist.2017-0167.
Topkan E. Weight gain as a surrogate marker of longer survival in advanced non-small cell lung cancer patients. Ann Transl Med. 2016;4(19):381. https://doi.org/10.21037/atm.2016.09.33.
Del Ferraro C, Grant M, Koczywas M, Dorr-Uyemura LA. Management of anorexia-cachexia in late stage lung cancer patients. J Hosp Palliat Nurs. 2012;14(6). https://doi.org/10.1097/NJH.0b013e31825f3470.
Heinhuis KM, Barkman HJ, Beijnen JH, Hendrikx J. A cost analysis study of the implementation of fixed-dosing of monoclonal antibodies in the Netherlands Cancer Institute. Int J Clin Pharm. 2021;43(1):181–90. https://doi.org/10.1007/s11096-020-01131-z.
Yoo SH, Keam B, Kim M, Kim SH, Kim YJ, Kim TM. Low-dose nivolumab can be effective in non-small cell lung cancer: alternative option for financial toxicity. ESMO Open. 2018;3(5): e000332. https://doi.org/10.1136/esmoopen-2018-000332.
Renner A, Burotto M, Rojas C. Immune checkpoint inhibitor dosing: can we go lower without compromising clinical efficacy? J Glob Oncol. 2019;5:1–5. https://doi.org/10.1200/JGO.19.00142.
Gray JE, Villegas A, Daniel D, Vicente D, Murakami S, Hui R, et al. Three-year overall survival with durvalumab after chemoradiotherapy in stage III NSCLC-update from PACIFIC. J Thorac Oncol. 2020;15(2):288–93. https://doi.org/10.1016/j.jtho.2019.10.002.
Herbst RS, Garon EB, Kim DW, Cho BC, Perez-Gracia JL, Han JY, et al. Long-term outcomes and retreatment among patients with previously treated, programmed death-ligand 1-positive, advanced non-small-cell lung cancer in the KEYNOTE-010 Study. J Clin Oncol. 2020;38(14):1580–90. https://doi.org/10.1200/jco.19.02446.
Spigel DR, McCleod M, Hussein MN, Waterhouse DM, Einhorn L, Horn L, et al. CheckMate 153: Randomized results of continuous vs 1-year fixed-duration nivolumab in patients with advanced non-small cell lung cancer. Ann Oncol. 2017;28:Abstract 1297O.
von Pawel J, Bordoni R, Satouchi M, Fehrenbacher L, Cobo M, Han JY, et al. Long-term survival in patients with advanced non-small-cell lung cancer treated with atezolizumab versus docetaxel: results from the randomised phase III OAK study. Eur J Cancer. 2019;107:124–32. https://doi.org/10.1016/j.ejca.2018.11.020.
Feng Y, Roy A, Masson E, Chen TT, Humphrey R, Weber JS. Exposure-response relationships of the efficacy and safety of ipilimumab in patients with advanced melanoma. Clin Cancer Res. 2013;19(14):3977–86. https://doi.org/10.1158/1078-0432.Ccr-12-3243.
Sharma P, Siefker-Radtke A, de Braud F, Basso U, Calvo E, Bono P, et al. Nivolumab alone and with ipilimumab in previously treated metastatic urothelial carcinoma: CheckMate 032 nivolumab 1 mg/kg plus ipilimumab 3 mg/kg expansion cohort results. J Clin Oncol. 2019;37(19):1608–16. https://doi.org/10.1200/jco.19.00538.
Ascierto PA, Del Vecchio M, Robert C, Mackiewicz A, Chiarion-Sileni V, Arance A, et al. Ipilimumab 10 mg/kg versus ipilimumab 3 mg/kg in patients with unresectable or metastatic melanoma: a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2017;18(5):611–22. https://doi.org/10.1016/s1470-2045(17)30231-0.
Ascierto PA, Del Vecchio M, Mackiewicz A, Robert C, Chiarion-Sileni V, Arance A, et al. Overall survival at 5 years of follow-up in a phase III trial comparing ipilimumab 10 mg/kg with 3 mg/kg in patients with advanced melanoma. J Immunother Cancer. 2020;8(1). https://doi.org/10.1136/jitc-2019-000391.
Hellmann MD, Rizvi NA, Goldman JW, Gettinger SN, Borghaei H, Brahmer JR, et al. Nivolumab plus ipilimumab as first-line treatment for advanced non-small-cell lung cancer (CheckMate 012): results of an open-label, phase 1, multicohort study. Lancet Oncol. 2017;18(1):31–41. https://doi.org/10.1016/s1470-2045(16)30624-6.
European Medicines Agency. Yervoy: EPAR-Product information. 2021.
O’Brien L, Westwood P, Gao L, Heathman M. Population pharmacokinetic meta-analysis of ramucirumab in cancer patients. Br J Clin Pharmacol. 2017;83(12):2741–51. https://doi.org/10.1111/bcp.13403.
Lu JF, Bruno R, Eppler S, Novotny W, Lum B, Gaudreault J. Clinical pharmacokinetics of bevacizumab in patients with solid tumors. Cancer Chemother Pharmacol. 2008;62(5):779–86. https://doi.org/10.1007/s00280-007-0664-8.
Yang K, Wang YJ, Chen XR, Chen HN. Effectiveness and safety of bevacizumab for unresectable non-small-cell lung cancer: a meta-analysis. Clin Drug Investig. 2010;30(4):229–41. https://doi.org/10.2165/11532260-000000000-00000.
Menz BD, Stocker SL, Verougstraete N, Kocic D, Galettis P, Stove CP, et al. Barriers and opportunities for the clinical implementation of therapeutic drug monitoring in oncology. Br J Clin Pharmacol. 2021;87(2):227–36. https://doi.org/10.1111/bcp.14372.
European Medicines Agency. Xalkori: EPAR-Product information. 2020.
European Medicines Agency. Alecensa: EPAR-Product information. 2020.
European Medicines Agency. Zykadia: EPAR-Product information. 2020.
European Medicines Agency. Alunbrig: EPAR-Product information. 2020.
European Medicines Agency. Lorviqua: EPAR-Product information. 2020.
European Medicines Agency. Tafinlar: EPAR-Product information. 2020.
European Medicines Agency. Mekinist: EPAR-Product information. 2020.
European Medicines Agency. Vitrakvi: EPAR-Product information. 2020.
European Medicines Agency. Rozlytrek: EPAR-Product information. 2020.
Scheithauser W, Ramanathan RK, Moore M, Macarulla T, Goldstein D, Hammel P, et al. Dose modification and efficacy of nab-paclitaxel plus gemcitabine vs. gemcitabine for patients with metastatic pancreatic cancer: phase III MPACT trial. J Gastrointest Oncol. 2016;7(3):469–78.
Bellesoeur A, Ollier E, Allard M, Hirsch L, Boudou-Rouquette P, Arrondeau J, et al. Is there an exposure-response relationship for nivolumab in real-world NSCLC patients? Cancers (Basel). 2019;11(11):1784. https://doi.org/10.3390/cancers11111784.
Chatterjee MS, Elassaiss-Schaap J, Lindauer A, Turner DC, Sostelly A, Freshwater T, et al. Population pharmacokinetic/pharmacodynamic modeling of tumor size dynamics in pembrolizumab-treated advanced melanoma. CPT Pharmacometr Syst Pharmacol. 2017;6(1):29–39. https://doi.org/10.1002/psp4.12140.
Zielinski CC. A phase I study of MEDI4736, NNT-PD-L1 antibody in patients with advanced solid tumors. Transl Lung Cancer Res. 2014;3(6):406–7. https://doi.org/10.3978/j.issn.2218-6751.2014.08.07.
Segal NH, Hamid O, Hwu W, Massard C, Butler M, Antonia S, et al. 1058PD—a Phase I multi-arm dose-expansion study of the anti-programmed cell death-ligand-1 (Pd-L1) antibody Medi4736: preliminary data. Ann Oncol. 2014;25:iv365. https://doi.org/10.1093/annonc/mdu342.11.
Morrissey KM, Marchand M, Patel H, Zhang R, Wu B, Phyllis Chan H, et al. Alternative dosing regimens for atezolizumab: an example of model-informed drug development in the postmarketing setting. Cancer Chemother Pharmacol. 2019;84(6):1257–67. https://doi.org/10.1007/s00280-019-03954-8.
Smit EF, Garon EB, Reck M, Cappuzzo F, Bidoli P, Cohen RB, et al. Exposure-response relationship for ramucirumab from the randomized, double-blind, phase 3 REVEL trial (docetaxel versus docetaxel plus ramucirumab) in second-line treatment of metastatic non-small cell lung cancer. Cancer Chemother Pharmacol. 2018;82(1):77–86. https://doi.org/10.1007/s00280-018-3560-5.
European Medicines Agency. Cyramza: EPAR-Product information. 2020.
European Medicines Agency. Avastin: EPAR-Product information. 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflict of interest
RJ Boosman, EF Smit, ADR Huitema, and R ter Heine have no conflicts of interest that might be relevant to the contents of this manuscript. JA Burgers is a member of advisory boards for Roche and BMS and has received support from MSD for an investigator-initiated study. All of these conflicts are outside of the submitted work, and any reimbursement was paid to their institution. N Steeghs has provided consultation or attended advisory boards for AIMM Therapeutics, Boehringer Ingelheim, and Ellipses Pharma; has received research grants for the institute from AB Science, Abbvie, Actuate Therapeutics, Amgen, Array, AstraZeneca/MedImmune, Bayer, Blueprint Medicines, Boehringer Ingelheim, Bristol-Myers Squibb, Cantargia, CellCentric, Cytovation, Deciphera, Genentech/Roche, GlaxoSmithKline, Incyte, Lilly, Merck Sharp & Dohme, Merus, Molecular Partners, Novartis, Pfizer, Pierre Fabre, Roche, Sanofi, Taiho, and Takeda. All of these conflicts are outside of the submitted work, and any reimbursement was paid to their institution. AJ van der Wekken has received grants from AstraZeneca, Boehringer Ingelheim, Pfizer, Roche, and Takeda; has received payment for lectures from Pfizer, Boehringer Ingelheim, and Takeda; and is a member of the advisory boards of Boehringer Ingelheim, Takeda, and Janssen. All of these are outside of the submitted work. JH Beijnen has received payment for expert testimony for Hoyng Tokh Monegier (paid to their institution), is a part-time employee and (in)direct stockholder of Modra Pharmaceuticals and (jointly) holds a patent on oral taxane formulations clinically developed by Modra Pharmaceuticals. Modra Pharmaceuticals is a small spin-off company of the Netherlands Cancer Institute. All of these conflicts are outside of the submitted work.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material:
Not applicable.
Code availability
Not applicable.
Authors’ contributions
RJ Boosman: conceptualization, methodology, investigation, writing original draft. JA Burgers, EF Smit, N Steeghs: conceptualization, methodology, writing review and editing. AJ van der Wekken: writing review and editing. JH Beijnen: writing review and editing. ADR Huitema: conceptualization, methodology, writing review and editing, supervision. R ter Heine: conceptualization, methodology, writing review and editing, and supervision.
Rights and permissions
About this article
Cite this article
Boosman, R.J., Burgers, J.A., Smit, E.F. et al. Optimized Dosing: The Next Step in Precision Medicine in Non-Small-Cell Lung Cancer. Drugs 82, 15–32 (2022). https://doi.org/10.1007/s40265-021-01654-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-021-01654-3