Abstract
Rheumatoid arthritis (RA) is a systemic autoimmune disease characterized by inflammation and joint destruction that causes significant morbidity and mortality. However, the combined use of methotrexate (MTX), a synthetic disease-modifying anti-rheumatic drug (sDMARD) and biological DMARDs (bDMARDs) has revolutionized treatment of RA and clinical remission or low disease activity (LDA) are now realistic targets, achieved by a large proportion of RA patients. We are now in a position to evaluate if it is possible to maintain remission or LDA while at the same time reducing the burden of treatment on the patient and healthcare system. Data are emerging from large, well-conducted studies designed to answer this question, shedding light on which patient populations and treatment algorithms can survive treatment discontinuation or tapering with low risk of disease flare. For early RA, approximately half of early RA patients could discontinue TNF-targeted bDMARDs without clinical flare and functional impairment after obtaining clinical remission by bDMARDs with MTX. In contrast, for established RA, fewer patients sustained remission or LDA after the discontinuation of bDMARDs and “deep remission” at the discontinuation was a key factor to maintain the treatment holiday of bDMARDs. Thus, this article provides a brief outline on withdrawing or tapering bDMARDs once patients have achieved remission or LDA in RA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The discontinuation of biological disease-modifying anti-rheumatic drugs (bDMARDs) is possible without clinical flare and functional impairment for early rheumatoid arthritis (RA) patients with low disease activity or remission. |
For patients with established RA, “deep remission” at the time of discontinuation is required to maintain the treatment holiday from bDMARDs. |
“Treatment holiday” from bDMARDS following early intensive treatment may be beneficial for reduction of drug-induced adverse effects and costs. |
1 Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease, leading to synovial hypertrophy and adjacent bone and cartilage destruction. However, the combined use of methotrexate (MTX), a standard synthetic disease-modifying anti-rheumatic drug (sDMARD) and a biological DMARD (bDMARD) has revolutionized treatment of RA and clinical remission or low disease activity (LDA) are now realistic targets, achieved by a large proportion of RA patients. Currently, discontinuation of a bDMARD without disease flare is our next goal and desirable from the standpoint of risk reduction and cost effectiveness, especially for patients with clinical remission or LDA. Data are emerging from large, well-conducted studies designed to answer this question, shedding light on which patient populations and treatment strategies can survive treatment discontinuation or tapering with low risk of disease flare [1–5]. The goal of the present Leading article is to determine if discontinuation of a bDMARD is possible in RA patients, after obtaining LDA or clinical remission by the use of bDMARDs. The content is based on results of a systematic literature review as well as new information.
2 Systematic Literature Search Regarding Discontinuation of Biological DMARDs (bDMARDs)
First of all, a search of PubMed using a search strategy that combined terms for “rheumatoid arthritis”, “biological agent” and “discontinuation, discontinuing or cessation” was performed as below:
-
#1.
rheumatoid arthritis
-
#2.
discontinuation OR discontinuing OR stop OR stopping OR cessation OR withdrawal
-
#3.
biological dmards OR biological drugs OR anti-tnf OR tnf inhibitor OR infliximab OR remicade OR etanercept OR enbrel OR adalimumab OR humira OR tocilizumab OR actemra OR roactemra OR abatacept OR orencia OR golimumab OR simponi OR certolizumab OR cimzia OR rituximab OR rituxan
-
#4.
remission OR low disease activity
-
#5.
English[Language]
-
#6.
arthritis, juvenile rheumatoid[MeSH]
-
#7.
review[Filter]
-
#8.
#1 AND #2 AND #3 AND #4 AND #5 NOT #6 NOT #7
During screening the titles and abstracts of the citations and retrieved relevant articles, the following selection criteria were used; (a) clinical trials of bDMARDs in patients with RA, followed by discontinuation of a bDMARD due to preferable effectiveness but not to adverse events nor to insufficient efficacy, (b) patients with RA >18 years old, (c) data available on one or more of following pre-specified outcomes: proportion of remission or low disease activity after at least 12 weeks of discontinuation and/or proportion of re-administration of a bDMARDs (d) published after 1998 that the first bDMARD to be available.
By performing a PubMed search on July 5th, 2014, 86 original research articles were found. Then systematic literature review revealed that 19 articles were as candidate studies, and 67 articles were excluded. The reasons for exclusion were categorized into three groups; (1) No description of discontinuing biologics, (2) Reasons for discontinuing biologics are not specified, (3) No description of discontinuing biologics due to preferable effectiveness. We also added the abstracts search on the American College of Rheumatology (ACR) 2011, 2012, 2013, the European League against Rheumatism (EULAR) 2012, 2013, 2014, and finally identified 26 reports as the candidate studies, summarized in Table 1.
3 Stopping a bDMARD in Established RA
There is little information about characteristics of patients in which a bDMARD is successfully discontinued without functional and radiographic damage progression in patients with long-term established RA encountered during routine clinical practice.
3.1 RRR Study
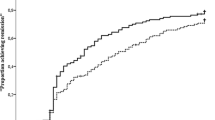
We first reported a RRR study aimed at the possibility of biologic-free remission in RA patients whose mean disease duration was 5.9 years [6]. This study included a total of 114 patients, from 26 centers, with RA who reached and maintained LDA (disease activity score 28; DAS28 <3.2) for more than 24 weeks with infliximab treatment. Among the 102 evaluable patients who completed the study, 56 and 44 maintained LDA and remission (DAS28 <2.6), respectively, after 1 year and showed no changes in radiological damage measured by yearly progression of modified total Sharp score (mTSS) and functional disturbance measured by health assessment questionnaire-disability index (HAQ-DI) score. By logistic regression and a receiver-operating characteristic curve (ROC) analysis, the cut-off point for achieving RRR at the time of patient enrollment was a DAS28 of 2.22, and a ‘deep’ remission was necessary at the time of the discontinuation. The study demonstrated that 71.4 % patients with deep remission (DAS28 ≤2.22) were able to continue LDA for 1 year, whereas only 32.6 % patients with a DAS28 score of between 2.22 and 3.2 were able to continue LDA, suggesting that established RA patients in deep remission have a possibility to achieve biologic-free remission.
3.2 HONOR Study
We also carried HONOR study to investigate the possibility of discontinuing adalimumab for 1 year without flaring measured by DAS28-ESR ≥3.2 in RA patients [7, 8]. Prior to the study, 197 RA patients with inadequate response to MTX were treated with MTX and adalimumab and 75 patients met the adalimumab-free criteria (steroid-free and sustained DAS28-ESR remission for more than 6 months). The mean disease duration and DAS28-ESR score in 75 patients was 7.5 years and 5.1 at baseline, respectively. Of the 75 patients, 52 (69 %) agreed to adalimumab discontinuation and 23 patients continued to use adalimumab for 1 year. The remission rate (83 %) and the rates of LDA (91 %) measured by DAS28-ESR in the adalimumab continuation group were significantly higher than those (48 and 62 %, respectively) in the adalimumab discontinuation group 1 year after the continuation or discontinuation decision was made. Re-administration of adalimumab to patients with flare was effective in returning LDA within 6 months in 90 % and 9 months in 100 % patients. In the analysis of predictive factors related to sustaining remission for 1 year, only DAS28-ESR had a marked correlation with sustained remission in multivariate analyses. Subsequent ROC analysis for high estimation of sustained remission indicated a cut-off value for the adalimumab-free remission of 1.98. In patients with DAS28-ESR ≤1.98 at the discontinuation, their remission rates were approximately 70 % at 1 year after the discontinuation, indicating that “deep remission” would be a key for successful discontinuation of adalimumab in established patients with RA.
3.3 ADMIRE Study
In the ADMIRE study, 33 RA patients (median disease duration 8 years) in stable DAS28 remission for more than 3 months with MTX plus adalimumab were randomized to continue adalimumab or to discontinue it for 52 weeks [9]. At 28 weeks, 15 of 16 (94 %) and 5/15 (33 %) in an adalimumab-continued group and in the discontinued group, respectively, were in DAS28-remission. In long-term extension of the BRIGHT study, 46 RA patients (mean disease duration 10.3 years) whose DAS28-CRP was less than 2.7 by MTX plus adalimumab were randomized to a continued group or discontinued group. Only 4 of 22 adalimumab-discontinued patients (18.2 %) maintained LDA through week 52 [10].
3.4 DOSERA Study
In the DOSERA study, 73 RA patients (average of disease duration 13.6 years) in stable LDA for more than 11 months with MTX plus etanercept were randomized to MTX plus etanercept 50 mg/week, 25 mg/week or placebo. The percentage of non-failures at 48 weeks was 52 % for etanercept 50 mg, 44 % for etanercept 25 mg and 13 % for placebo groups [11]. In the PRESERVE study, after patients with moderately active RA despite MTX were treated with etanercept 50 mg/week and MTX for 26 weeks, 604 patients who achieved LDA were randomized to MTX plus etanercept 50 mg/week, 25 mg/week or placebo [12]. At weeks 52 after the randomization, sustained LDA was observed in 82.6 % of patients treated with MTX plus etanercept 50 mg/week, 79.1 % of those with MTX plus etanercept 25 mg/week and 42.6 % of those with MTX alone.
3.5 ORION Study
In the ORION study, abatacept was discontinued in 34 RA patients (mean disease duration 6.4 years) with a DAS28-CRP remission on MTX plus abatacept. At 52 weeks after the withdrawal, 58.8 % failed from DAS28-CRP remission [14].
3.6 ACT-RAY Study
In the ACT-RAY study, 556 established RA patients (mean disease duration 8.2 years) who inadequately responded to MTX were randomized to either add TCZ 8 mg/kg to MTX or to switch to TCZ 8 mg/kg with oral placebo [15]. About 50 % of patients entering into year 2 discontinued tocilizumab after achieving DAS28 <2.6 at 2 consecutive visits and 86 % of these patients experienced flare before the end of year 2. In the DREAM study, 187 established RA patients who showed LDA or remission by DAS28, median disease duration was 7.8 years, preceding tocilizumab monotherapy period was 4.0 years and DAS28 was 1.5, discontinued tocilizumab [16]. Only 13.4 % of them kept LDA, but 9.1 % fulfilled drug-free remission at 52 weeks.
There results indicate that patients with established RA in sustained remission or LDA after the discontinuation of a bDMARD were controversial among studies or difficult in many studies and the proportion of patients who could successfully discontinue bDMARDs ranged from 9 to 48 % at 1 year. However, from HONOR study and RRR study, deep remission is required to sustain remission after the discontinuation of a bDMARD and DAS28-ESR cut-off point at discontinuation was 1.98 achieving remission at week 52 in the adalimumab discontinued group and 2.22 for achieving LDA at week 52 in the infliximab-free group [6–8]. In fact in HONOR study, approximately 80 % patients with deep remission (DAS28-ESR ≤1.98) were able to sustain LDA for 1 year without adalimumab, whereas, only 42 % patients with mild remission were able to do so, although there was no statistically significant difference between the two groups. Meanwhile, 60 % patients with mild remission experienced flaring within a year, suggesting that mild remission may be insufficient for the discontinuation and that adalimumab should be continued in such patients even under DAS28 remission. Thus, “treatment holiday”, successful discontinuation of a bDMARD for a certain period, is now feasible in some patients with long-standing RA encountered during routine clinical practice, but “deep remission” at the discontinuation is required to keep the treatment holiday of bDMARDs.
In our institution, among 619 patients including both early and established RA who were treated with infliximab plus MTX, 102 patients reached bDMARD-free remission (manuscript in preparation). The baseline factors affecting infliximab-free remission were disease duration and rheumatoid factor (RF), indicating that patients with early RA have more chance to discontinue bDMARDs after obtaining remission.
4 Treatment Holiday from bDMARDs in Early RA
In early RA patients several studies including TNF20, OPTIMA, HIT HARD, IDEA, PRIZE, EMPIRE and BeSt have been undertaken to investigate whether remission can be sustained after a bDMARD targeting TNF is discontinued after following disease control.
4.1 TNF20 Study
The study regarding bDMARD-free treatment in RA patients was first reported by a TNF20 study [17, 18]. Patients with early RA who had less than 12 months of symptoms were treated with a combination of infliximab and MTX. One year after stopping induction therapy, response was sustained in 70 % of patients who received infliximab and MTX. A significant reduction in magnetic resonance imaging evidence of synovitis and erosions at 1 year was also observed.
4.2 BeSt Study
The Behandelstrategieën (BeSt) study was conducted to compare 4 treatment strategies and to observe clinical outcomes in patients with early RA (disease duration less than 2 years after onset, mean disease duration 0.8 years) [19–23]. In BeSt study 508 patients with high disease activity were distributed to 4 groups and were evaluated by DAS44 every three months. If DAS44 >2.4 (intermediate or high disease activity), change or addition of medications is required, if DAS44 ≤2.4 (remission or LDA), current medication is continued, and if DAS44 ≤2.4 continued over 6 months, decrease and/or discontinue concomitant medications including infliximab. In the fourth group who started by infliximab 90 patients of 120 (75 %) achieved LDA and infliximab was withdrawn in 77 cases because they maintained LDA for 6 months. The LDA was kept in 43/77 patients (56 %) for at least 1 year. Furthermore, more than half of patients who discontinued infliximab successfully maintained LDA for more than 8 years, according to the 8-year follow-up of infliximab-free survival in patients with early RA.
4.3 IDEA Study
In the IDEA study, patients with DMARD-naïve early RA were randomized to MTX plus infliximab and MTX plus intravenous steroid therapy as remission induction [24]. In the former group, 24.5 % (14/55) had stopped infliximab due to sustained remission (DAS44 <1.6 for 6 months) and 78.6 % (11/14) of them maintained remission for half a year.
4.4 OPTIMA Study
A multinational, double-blinded, randomized controlled study was performed to determine the optimal protocol for treatment initiation with adalimumab plus MTX in patients with RA (OPTIMA) [12]. In this study, the withdrawal of adalimumab in early RA patients (with a mean RA duration of 3.9 months) was also assessed. Outcomes of withdrawal or continuation of adalimumab were assessed in patients who achieved a stable LDA target after 26 weeks of initially assigned treatment with adalimumab and MTX. Of the 466 RA patients treated with adalimumab and MTX, 207 (44 %) achieved the stable LDA measured by DAS28-CRP at weeks 22 and 26 and were re-randomized to placebo plus MTX or adalimumab plus MTX during the second study period for 52 weeks. After 52 weeks, 91 and 86 % of patients who continued adalimumab treatment maintained LDA and remission, respectively, compared with 81 and 66 % of patients who withdrew from adalimumab treatment.
4.5 HIT HARD Study
In a HIT HARD study, the withdrawal of adalimumab in patients with early RA (mean RA duration 1.7 months) was also assessed whether an early induction therapy with subsequent step down strategy leads to a long-term clinical effect in early RA patients as compared to initial and continued MTX [25]. During the first 24 weeks, 172 patients were treated with adalimumab or placebo with MTX; after week 24, both groups were treated with MTX alone for 24 weeks. During the induction phase, 47 % of patients treated with MTX and adalimumab achieved DAS28-remission; at week 48, 44 % of these patients were still in remission by 24 weeks of adalimumab-free treatment.
4.6 PRIZE Study
In the PRIZE study MTX-naïve early RA patients with moderately active disease activity were treated with etanercept and MTX and DAS28 remission was achieved by 70 % of patients [26]. These patients were randomized to a double-blinded 39-week period of reduced-dose etanercept (25 mg) plus MTX, MTX plus subcutaneous placebo, or oral placebo and subcutaneous placebo. At week 39 the sustained remission was observed in 63.5 % of patients with etanercept plus MTX, 38.5 % with MTX, those who discontinued etanercept, and 23.1 % with placebo, those who discontinued etanercept and MTX. There was no significant radiographic progression in any treatment group.
4.7 EMPIRE Study
In EMPIRE study, 110 DMARD-naïve patients with early inflammatory arthritis and the minimum of one synovitis joint were randomized to MTX plus etanercept or MTX plus placebo for 52 weeks [27]. Injections were stopped in all patients at week 52 or injections were stopped early in those with no tender or swollen joints for more than 26 weeks. In the MTX + ETN group, 41.9 and 57.7 % remained in remission and LDA according to DAS28, respectively, from week 52 to week 78.
Taken together, these recent studies indicate that 30–79 % of early RA patients could discontinue bDMARDs without clinical flare and functional impairment after reduction of disease activity to LDA or remission by bDMARDs in combination with MTX. Although there are limited studies, a treatment holiday of bDMARDs is now feasible in approximately half of patients with early RA.
5 De-Escalation of bDMARDs in RA
On the other hand, de-escalation (dose reduction/interval prolongation) of bDMARDs appears to attract attention because complete discontinuation of bDMARDs is rather difficult for the established RA patients. A group in the Netherland performed the first observational cohort study regarding de-escalation of bDMARDs in RA patients with stable LDA and reported that the down-titration of infliximab was feasible for 45 % of patients, with a mean dose reduction of 60 % after 1 year [28]. In the PRESERVE study, patients with RA achieving remission after 1-year treatment with etanercept were randomly assigned with full-dose maintenance (50 mg weekly), dose reduction (25 mg weekly) or discontinuation for 1 year [12]. However, dose reduction was associated with a non-significant risk of relapse and structural damage progression at 1 year as compared to full-dose maintenance. Recent interval prolongation STRASS study, an 18-month randomized controlled trial, was undertaken by a French group to compare the impact of a DAS28-driven step-down strategy to maintenance strategy [29]. Established RA patients, with etanercept or adalimumab for longer than 1 year, DAS28 remission for more than 6 months, stable damage on X-rays, were randomized to TNF-inhibitor injection spacing arm (n = 64) and a maintenance strategy arm (n = 73), then followed every 3 months for 18 months. The inter-injection interval was increased every 3 months up to full stop at 4th step. At 18 months, 47 (73.4 %) patients of the spacing arm tapered TNF-blockers. Mean DAS28, mean HAQ and structural damage progression were not significantly different between arms. However, relapse (ΔDAS28 > 0.6 + DAS28 > 2.6) occurred at least once more frequently in the spacing arm than in the maintenance arm (81 vs. 56 %, p = 0.0009).
However, in these studies it is not clear how to monitor the disease activity and retreat or increase the dose in case of disease worsening after dose reduction, which may rather result in equally good care as just continuing treatment. Furthermore, when considering de-escalation trials, there are quite various factors underlying to de-escalate bDMARDs. For instance, (i) baseline characteristics; early or established RA, with or without MTX and/or other DMARDs, LDA or remission, remission criteria, duration of disease control and so on, (ii) targeted medications; bDMARDs or MTX, TNF-inhibitors or non-TNF-bDMARD, dose reduction or interval prolongation, schedule of the dose reduction, criteria for de-escalation, reduction of all at once and many, (iii) disease flare after de-escalation; definition of flare, how to treat flared cases, restart all or step-up at flare and etc. Thus, there are too many factors regarding the de-escalation, very careful consideration regarding inclusion criteria, protocol, assessment, etc. would be required to perform de-escalation trials in RA patients. On the other hand, although titrating patients to the lowest dose may save medication costs, it may also lead to increased number of patient contacts and consequent costs. So far, none of the previous controlled de-escalation studies included a disease activity guided strategy or cost-effectiveness analyses. Taken together, in this manuscript we have shed light upon discontinuation of bDMARD rather than de-escalation strategy.
6 Conclusion
The combination of MTX and bDMARDs targeting TNF, IL-6 and T cells has revolutionized RA treatment, leading to clinical, functional and structural remission. Since we have obtained strong weapons to treat RA, a new strategy rather than a new target should be required for the advanced therapy of RA. For instance, how and when bDMARDs are discontinued without disease flare is an emerging theme to strategically treat RA. We are now in a position to evaluate what is possible in terms of maintaining remission or LDA while at the same time reducing the burden of treatment on the patient and healthcare system. Data emerging from large, well-conducted studies indicate that approximately half of early RA patients could discontinue bDMARDs targeting TNF without clinical flare and functional impairment after obtaining reduction of disease activity to LDA or remission by bDMARDs in combination with MTX. Saleem et al. [30] also reported that a TNF-inhibitor-free sustained remission rate was 60 % after acquiring DAS28 remission in MTX-naïve early RA patients. Within the initial treatment group, the only clinical predictor of the successful discontinuation was shorter symptom duration prior to receiving therapy (median 5.5 vs. 9.0 months, p = 0.008). No other clinical features including activity measured by power doppler were associated with the discontinuation of bDMARD.
However, fewer patients sustained remission or LDA after the discontinuation of bDMARDs for patients with established RA, compared to early RA. It is often difficult to successfully discontinue bDMARDs and the results were controversial among studies. The HONOR study and RRR study indicated that “deep remission” is required to successfully discontinue bDMARDs in established RA patients; DAS28-ESR cut-off point at discontinuation was 1.98 achieving remission at week 52 in the adalimumab withdrawal group and 2.22 for achieving LDA at week 52 in the infliximab-free group [6–8]. Thus, the mild remission is insufficient for the discontinuation and bDMARDs should be continued in such patients even under DAS28 remission.
Thus, “treatment holiday” of bDMARDs is now feasible in some patients with RA with long-standing RA, but “deep remission” at the discontinuation is a key factor to keep the treatment holiday of bDMARDs. However, such intensive treatment would have the potential of reducing drug-induced adverse effects and reducing long-terms medical costs, although the risks of worsening clinical, structural and functional outcomes should be considered with careful monitoring.
References
Pincus T, Braun J, Kavanaugh A, Smolen JS. Possible discontinuation of therapies in inflammatory rheumatic diseases—as with initiation of therapies, a shared decision between patient and rheumatologist. Clin Exp Rheumatol. 2013;31(4 Suppl 78):S1–3.
Kavanaugh A, Smolen JS. The when and how of biologic agent withdrawal in rheumatoid arthritis: learning from large randomised controlled trials. Clin Exp Rheumatol. 2013;31(4 Suppl 78):S19–21.
Tanaka Y. Next stage of RA treatment: is TNF inhibitor-free remission a possible treatment goal? Ann Rheum Dis. 2013;72(Suppl 2):ii124–7.
Tanaka Y, Hirata S. Is it possible to withdraw biologics from therapy in rheumatoid arthritis? Clin Ther. 2013;35(12):2028–35.
Tanaka Y, Hirata S, Saleem B, Emery P. Discontinuation of biologics in patients with rheumatoid arthritis. Clin Exp Rheumatol. 2013;31(4 Suppl 78):S22–7.
Tanaka Y, Takeuchi T, Mimori T, Saito K, Nawata M, Kameda H, et al. Discontinuation of infliximab after attaining low disease activity in patients with rheumatoid arthritis: RRR (remission induction by Remicade in RA) study. Ann Rheum Dis. 2010;69(7):1286–91.
Hirata S, Saito K, Kubo S, Fukuyo S, Mizuno Y, Iwata S, et al. Discontinuation of adalimumab after attaining disease activity score 28-erythrocyte sedimentation rate remission in patients with rheumatoid arthritis (HONOR study): an observational study. Arthritis Res Ther. 2013;15(5):R135.
Tanaka Y, Hirata S, Kubo S, Fukuyo S, Hanami K, Sawamukai N, et al. Discontinuation of adalimumab after achieving remission in patients with established rheumatoid arthritis: 1-year outcome of the HONOR study. Ann Rheum Dis. 2013. doi:10.1136/annrheumdis-2013-204016 [Epub ahead of print].
Chatzidionysiou K, Turesson C, Teleman A, Knight A, Lindqvst E, Larsson P, et al. A Mullicrntcr, randomized, conlrolled, open-lavel pilot study of the feasibility of discontinuation of adalimumab in rheumatoid arthritis patients in stable clinical remission. Arthritis Rheum. 2012;64(Suppl):S336.
Harigai M, Takeuchi T, Tanaka Y, Matsubara T, Yamanaka H, Miyasaka N. Discontinuation of adalimumab treatment in rheumatoid arthritis patients after achieving low disease activity. Mod Rheumatol. 2012;22(6):814–22.
Ostergaard M, Leirisalo-Repo M, Uhlig T, Jansson M, Larsson E, Brock F, et al. In rheumatoid arthritis patients with stable low disaese activity on methotrexate plus etanercept, continuation of etanercept is superior both clinically and radiographically to discontinuation: results from a randomized, 3-armed, double-blind clinical trial. Arthritis Rheum. 2013;66(Suppl):S1017.
Smolen JS, Emery P, Fleischmann R, van Vollenhoven RF, Pavelka K, Durez P, et al. Adjustment of therapy in rheumatoid arthritis on the basis of achievement of stable low disease activity with adalimumab plus methotrexate or methotrexate alone: the randomised controlled OPTIMA trial. Lancet. 2014;383(9914):321–32.
Smolen JS, Emery P, Ferraccioli GF, Samborski W, Berenbaum F, Davies OR, et al. Certolizumab pegol in rheumatoid arthritis patients with low to moderate activity: the CERTAIN double-blind, randomised, placebo-controlled trial. Ann Rheum Dis. 2014. doi:10.1136/annrheumdis-2013-204632 [Epub ahead of print].
Takeuchi T, Matsubara T, Ohta S, Mukai M, Amano K, Tohma S, Tanaka Y, Yamanaka H, Miyasaka N. Biologic-free remission of established rheumatoid arthritis after discontinuation of abatacept: a prospective, multicentre, observational study in Japan. Rheumatology (Oxford). 2014. (pii:keu338) [Epub ahead of print].
Huizinga TW, Conaghan PG, Martin-Mola E, Schett G, Amital H, Xavier RM, Troum O, Aassi M, Bernasconi C, Dougados M. Clinical and radiographic outcomes at 2 years and the effect of tocilizumab discontinuation following sustained remission in the second and third year of the ACT-RAY study. Ann Rheum Dis. 2014. doi:10.1136/annrheumdis-2014-205752 [Epub ahead of print].
Nishimoto N, Amano K, Hirabayashi Y, Horiuchi T, Ishii T, Iwahashi M, et al. Drug free REmission/low disease activity after cessation of tocilizumab (Actemra) Monotherapy (DREAM) study. Mod Rheumatol. 2014;24(1):17–25.
Quinn MA, Conaghan PG, O’Connor PJ, Karim Z, Greenstein A, Brown A, et al. Very early treatment with infliximab in addition to methotrexate in early, poor-prognosis rheumatoid arthritis reduces magnetic resonance imaging evidence of synovitis and damage, with sustained benefit after infliximab withdrawal: results from a twelve-month randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2005;52(1):27–35.
Bejarano V, Conaghan PG, Quinn MA, Saleem B, Emery P. Benefits 8 years after a remission induction regime with an infliximab and methotrexate combination in early rheumatoid arthritis. Rheumatology (Oxford, England). 2010;49(10):1971–4.
Allaart CF, Lems WF, Huizinga TW. The BeSt way of withdrawing biologic agents. Clin Exp Rheumatol. 2013;31(4 Suppl 78):S14–8.
van der Bijl AE, Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Ten Wolde S, Han KH, van Krugten MV, et al. Infliximab and methotrexate as induction therapy in patients with early rheumatoid arthritis. Arthritis Rheum. 2007;56(7):2129–34.
van der Kooij SM, Goekoop-Ruiterman YP, de Vries-Bouwstra JK, Guler-Yuksel M, Zwinderman AH, Kerstens PJ, et al. Drug-free remission, functioning and radiographic damage after 4 years of response-driven treatment in patients with recent-onset rheumatoid arthritis. Ann Rheum Dis. 2009;68(6):914–21.
Klarenbeek NB, van der Kooij SM, Guler-Yuksel M, van Groenendael JH, Han KH, Kerstens PJ, et al. Discontinuing treatment in patients with rheumatoid arthritis in sustained clinical remission: exploratory analyses from the BeSt study. Ann Rheum Dis. 2011;70(2):315–9.
van den Broek M, Klarenbeek NB, Dirven L, van Schaardenburg D, Hulsmans HM, Kerstens PJ, et al. Discontinuation of infliximab and potential predictors of persistent low disease activity in patients with early rheumatoid arthritis and disease activity score-steered therapy: subanalysis of the BeSt study. Ann Rheum Dis. 2011;70(8):1389–94.
Nam JL, Villeneuve E, Hensor EM, Conaghan PG, Keen HI, Buch MH, et al. Remission induction comparing infliximab and high-dose intravenous steroid, followed by treat-to-target: a double-blind, randomised, controlled trial in new-onset, treatment-naive, rheumatoid arthritis (the IDEA study). Ann Rheum Dis. 2014;73(1):75–85.
Detert J, Bastian H, Listing J, Weiss A, Wassenberg S, Liebhaber A, et al. Induction therapy with adalimumab plus methotrexate for 24 weeks followed by methotrexate monotherapy up to week 48 versus methotrexate therapy alone for DMARD-naive patients with early rheumatoid arthritis: HIT HARD, an investigator-initiated study. Ann Rheum Dis. 2013;72(6):844–50.
Emery P, Hammoudeh M, FitzGerald O, Combe B, Martin Mola E, Bukowski J, et al. Assessing maintanance of remissin with reduced dose etanercept plus methorrexate, methotrexate alone, or placebo in patients with eary rheumatoid arthritis who achieved remission with etanercept and methotrexate: The PRIZE study [abstract]. Ann Rheum Dis. 2013;72(Suppl 3):399.
Nam JL, Villeneuve E, Hensor EM, Wakefield RJ, Conaghan PG, Green MJ, et al. A randomised controlled trial of etanercept and methotrexate to induce remission in early inflammatory arthritis: the EMPIRE trial. Ann Rheum Dis. 2014;73(6):1027–36.
van der Maas A, Kievit W, van den Bemt BJ, van den Hoogen FH, van Riel PL, den Broeder AA. Down-titration and discontinuation of infliximab in rheumatoid arthritis patients with stable low disease activity and stable treatment: an observational cohort study. Ann Rheum Dis. 2012;71(11):1849–54.
Pham T, Morel J, Alfaiate T, Dernis E, Gaudin P, Brocq O, et al. Predictive Factors Of Relapse Or Persistent Stable Remission For Rheumatoid Arthritis (RA) Patients In Remission in a TNF Blocker-Spacing Strategy Trial (STRASS Trial). [abstract]. Arthritis Rheum. 2013;65(Suppl 10):2388. doi:10.1002/art.2013.65.issue-s10.
Saleem B, Keen H, Goeb V, Parmar R, Nizam S, Hensor EM, Churchman SM, Quinn M, Wakefield R, Conaghan PG, Ponchel F, Emery P. Patients with RA in remission on TNF blockers: when and in whom can TNF blocker therapy be stopped? Ann Rheum Dis. 2010;69:1636–42.
Nawata M, Saito K, Nakayamada S, Tanaka Y. Discontinuation of infliximab in rheumatoid arthritis patients in clinical remission. Mod Rheumatol. 2008;18(5):460–4.
Brocq O, Millasseau E, Albert C, Grisot C, Flory P, Roux CH, et al. Effect of discontinuing TNFalpha antagonist therapy in patients with remission of rheumatoid arthritis. Jt Bone Spine Revue du Rhumatisme. 2009;76(4):350–5.
Kaine J, Gladstein G, Strusberg I, Robles M, Louw I, Gujrathi S, et al. Evaluation of abatacept administered subcutaneously in adults with active rheumatoid arthritis: impact of withdrawal and reintroduction on immunogenicity, efficacy and safety (phase Iiib ALLOW study). Ann Rheum Dis. 2012;71(1):38–44.
Wevers-De Boer KVC, Heimans L, Visser K, Schouffoer A, van Oosterhout M, van Groenendaal H, et al. Drug free remission after one year of treatment in patients with early rheumatoid arthritis: Also possible for ACPA positive patients? [abstract]. Ann Rheum Dis. 2013;72(Suppl3):114.
Emery P, Burmester G, Bykerk V, Combe B, Furst DE, Barre E, et al. Induction of clinical remission followed by drug-free withdrawal with abatacept combination and monotherapy in early RA: Results from the AVERT study over 18 months [abstract]. Ann Rheum Dis. 2014;73(Suppl2).
Aguilar-Lozano L, Castillo-Ortiz JD, Vargas-Serafin C, Morales-Torres J, Sanchez-Ortiz A, Sandoval-Castro C, et al. Sustained clinical remission and rate of relapse after tocilizumab withdrawal in patients with rheumatoid arthritis. J Rheumatol. 2013;40(7):1069–73.
Competing interests
Y. Tanaka, has received consulting fees, speaking fees, and/or honoraria from Abbvie, Chugai, Astellas, Takeda, Santen, Mitsubishi-Tanabe, Pfizer, Janssen, Eisai, Daiichi-Sankyo, UCB, GlaxoSmithKline, Bristol-Myersand has received research grants from Mitsubishi-Tanabe, Chugai, MSD, Astellas, Novartis. S. Hirata declares no conflicts of interest. No funding was used to support the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Tanaka, Y., Hirata, S. Intensive Intervention Can Lead to a Treatment Holiday from Biological DMARDs in Patients with Rheumatoid Arthritis. Drugs 74, 2129–2139 (2014). https://doi.org/10.1007/s40265-014-0323-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-014-0323-4