Abstract
Treatment of multiple sclerosis (MS) is challenging: disease-modifying treatments (DMTs) must both limit unwanted immune responses associated with disease initiation and propagation (as T and B lymphocytes are critical cellular mediators in the pathophysiology of relapsing MS), and also have minimal adverse impact on normal protective immune responses. In this review, we summarize key preclinical and clinical data relating to the proposed mechanism of action of the recently approved DMT teriflunomide in MS. Teriflunomide selectively and reversibly inhibits dihydro-orotate dehydrogenase, a key mitochondrial enzyme in the de novo pyrimidine synthesis pathway, leading to a reduction in proliferation of activated T and B lymphocytes without causing cell death. Results from animal experiments modelling the immune activation implicated in MS demonstrate reductions in disease symptoms with teriflunomide treatment, accompanied by reduced central nervous system lymphocyte infiltration, reduced axonal loss, and preserved neurological functioning. In agreement with the results obtained in these model systems, phase 3 clinical trials of teriflunomide in patients with MS have consistently shown that teriflunomide provides a therapeutic benefit, and importantly, does not cause clinical immune suppression. Taken together, these data demonstrate how teriflunomide acts as a selective immune therapy for patients with MS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Multiple sclerosis (MS) is a chronic, progressive demyelinating disease of the central nervous system (CNS). MS typically emerges in young adulthood, and its incidence is highest in Northern Europe and North America, where it occurs in up to 1 in 1,000 individuals [1, 2]. In approximately 85 % of cases, MS initially manifests as a relapsing–remitting form (RRMS), which is characterized by episodes of neurological worsening followed by at least partial recovery [2].
Disease-modifying treatments (DMTs) that reduce damage to the CNS are being investigated for the treatment of patients with MS. CNS damage is assumed to result from disturbances in immune tolerance networks [3]. Multiple perivascular inflammatory foci are seen in the CNS of patients with MS, and these become sites of demyelination and axonal injury [4]. The lesions are associated with infiltrating T cells and monocytes, and occasional B cells and plasma cells: T cells may target neurons directly [5, 6]. Additionally, there is evidence for subpial cortical injury, which appears not to be in perivascular distribution [7, 8], implicating further as yet unidentified mechanism(s).
Given the dominant role of abnormal immune activation in MS pathogenesis, DMTs must limit MS-associated immune responses to be effective. On the other hand, in order not to compromise responses to pathogens, DMTs should have minimal effects on normal protective immune responses.
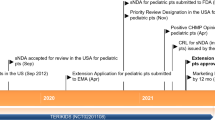
Teriflunomide, a once-daily oral immunomodulatory DMT, is approved in several regions, including the United States and the European Union, for the treatment of RRMS; further regulatory reviews are on-going in several other territories. Approvals were supported by placebo-controlled phase 3 clinical trials of teriflunomide that have demonstrated a favourable benefit/risk profile in this disease [9, 10]. In this review, we describe the hypothesized primary mechanism of action (MoA) of teriflunomide together with the preclinical evidence supporting this hypothesis in the context of MS pathogenesis. We also discuss the clinical evidence supporting preservation of protective immunity during teriflunomide treatment. Finally, we consider the place of teriflunomide in an expanding armamentarium of MS therapies.
2 MS Immunopathogenesis
MS is hypothesized to be primarily a T-helper cell-mediated autoimmune disease. Mounting evidence also supports the involvement of various other cells of the immune system. Immune cells cause demyelination and axonal/neuronal injury, and MS disease progression is considered to result partly from degenerative mechanisms as well as from ongoing (CNS-compartmentalized) inflammatory activity likely involving both T and B cells [6, 11–13].
2.1 T Cells
Various subsets of T cells exist, which are classified based on the expression of cell surface markers CD4 or CD8, and by their cytokine-secreting capacities. During a normal immune response, CD8+ T cells kill infected cells, while in MS they can mediate damage to CNS cells. CD4+ T cells, sometimes called “helper T” or “Th” cells, secrete cytokines that influence the activities of other immune cells, such as antibody-producing B cells. The roles of different immune cells in MS are illustrated in Fig. 1. According to the autoimmune hypothesis of MS pathogenesis, T cells reactive to CNS proteins (such as myelin basic protein [MBP] and myelin oligodendrocyte glycoprotein [MOG], among others [14]) must first be activated in the periphery before they gain the potential to cause damage within the CNS. Activated T cells up-regulate adhesion molecules and chemokine receptors that allow them to more efficiently cross the blood–brain barrier (BBB) [15]. Animal studies suggest that the potential to cross the BBB may depend on the specific antigen for each T cell being presented by cells of the vascular endothelium—this interaction initiates local BBB compromise and allows the T cell to enter into the CNS [16, 17]. The interleukin (IL)-17-secreting CD4+ T-cell subset (Th17 cells) has been implicated in animal models of MS and Th17 cells up-regulate the CCR6 receptor upon activation to gain entry into the CNS [18]. Recent data also indicate that neuronal activity can regulate entry of T cells into the spinal cord [19].
An overview of the roles of immune cells in multiple sclerosis pathogenesis. T cells are stimulated to proliferate when they encounter antigen-presenting cells in the lymph node. Circulating T cells and B cells can traffic from the circulation across the blood–brain barrier. In the CNS, T cells encounter CNS antigens presented by dendritic cells. Macrophages and activated T cells can attack components of the CNS directly or release cytokines to activate other cell types, including B cells, which mature into antibody-producing plasma cells. T T cell, B B cell, CNS central nervous system, BBB blood–brain barrier, APC antigen-presenting cell, DC dendritic cell [64, 81, 89, 94]
Early evidence supporting CD4+ T-cell involvement in MS came from experimental autoimmune encephalomyelitis (EAE) rodent models. EAE is induced by immunization with CNS-derived proteins or peptides, such as MBP [20, 21]. Transfer of MBP-specific CD4+ T cells from EAE animals can be sufficient to induce EAE in recipient animals, so long as the transferred cells are activated [22]. Transfer of T cells reactive to a mycobacterium derivative, which is used as an adjuvant, did not induce EAE in this experiment [22]. Further support for the involvement of CD4+ T cells in MS comes from the reported increased risk of MS associated with expression of specific major histocompatibility complex (MHC) class II alleles involved in antigen presentation to T lymphocytes [23].
Th1-type CD4+ T cells, characterized by production of interferon (IFN)γ, IL-2, and tumor necrosis factor alpha (TNFα), were initially believed to be the main drivers of MS [24, 25]. More recently, the role of Th17 cells has been recognized [26]. Interruption of Th17 differentiation using IL-23-blocking antibody in EAE mice restricts development of EAE [27], and IL-17 levels are elevated in blood and brain tissue of patients with MS [28]. Abrogation of disease activity in patients with aggressive MS following ablative chemotherapy and hematopoietic stem cell transplantation was associated with a diminished Th17 response, despite the reemergence of myelin-reactive Th1 and Th2 cells [29].
Various lines of evidence also indicate a role for CD8+ T cells in MS pathogenesis [13, 16, 30]. CD8+ T cells are able to cause EAE [31] and are present in MS lesions in patients [32], and some patients with MS have increased numbers of circulating MBP-reactive CD8+ T cells [33, 34]. Dysfunction or impaired maturation of both natural and inducible regulatory T cells (Treg), a type of CD4+ T cell, have been described in MS. Because Treg are critical for the maintenance of immune tolerance, this dysfunction or impaired maturation could possibly contribute to the disrupted tolerance found in patients with MS [35, 36].
2.2 B Cells
B-cell numbers are increased within the CNS of patients with MS [37], and B cells are considered to play an important role in MS pathogenesis through both antibody-dependent and antibody-independent functions. Antibody abnormalities within the CNS of patients include increased levels of cerebrospinal fluid (CSF) immunoglobulin (Ig) and Ig synthesis rates, as well as the presence of CSF-restricted oligoclonal bands. The target(s) of such antibodies have not been fully characterized, although several antigens have been suggested [38, 39].
B cells described within the MS brain appear to have undergone maturation within the CNS, possibly within specialized tertiary lymphoid tissue described in the pia/meninges of patients [40, 41]. Lineage analysis has shown that B cells from patients with MS can mature on either side of the BBB and traffic across it [42].
Independently of their antibody-producing capability, B cells may also affect T-cell activity in MS through cytokine production. Aberrant profiles of both pro-inflammatory (lymphotoxin, TNFα, IL-6) and anti-inflammatory (IL-10) cytokine responses have been observed in B cells from patients with MS [43]. B-cell activation in patients with MS can thus drive a pro-inflammatory T cell response, potentially resulting in new disease activity [44]. This hypothesis is supported by the observation that following B-cell depletion with the anti-CD20 monoclonal antibody rituximab, pro-inflammatory T-cell responses in patients with MS are diminished [45].
Regulatory B cells (Breg) have been shown to inhibit the progression of EAE in mice [46]. Evidence from patients also supports a role for Breg in MS, or an effect of MS on Breg. Increased numbers of Breg have been reported in patients with MS [47, 48], as have deficiencies in Breg functions, such as in IL-10 secretion [43, 44, 49].
2.3 Other Cells of the Immune System
Myeloid cells such as dendritic cells (DCs), either through their cytokine-secreting capacity or through their antigen-presenting or cell contact-mediated properties, are also likely involved in MS. In patients with MS, myeloid cells (both resident microglia and infiltrating macrophage/DCs) are abundant in CNS lesions and exhibit alterations in phenotype and function (expressing more activation markers and producing greater amounts of pro-inflammatory cytokines), supportive of a role in MS pathogenesis [50].
Roles in MS for other regulatory immune cells, including subsets of natural killer (NK) cells and resident CNS cells, such as astrocytes, have been proposed because their numbers or functions are altered in patients with MS or in response to immunomodulatory therapy. For example, NK cell cytolytic activity is reduced in patients with MS, and the DMT fingolimod is believed to influence the balance of NK cell subsets [51]. Astrocytes perform multiple roles in the evolution of changes encountered in MS depending upon the stage of development of their associated lesion [52], while microglia, also found in MS lesions, support the activity of CNS-reactive T cells [53].
3 Teriflunomide Proposed MoA: Overview of Current Hypothesis
The primary MoA of teriflunomide in MS is hypothesized to relate to its effects on the proliferation of stimulated lymphocytes. Upon activation, lymphocytes undergo division via the cell cycle, that comprises an S (‘synthesis’) phase (during which deoxyribonucleic acid [DNA] is copied), and M (‘mitosis’) phase (during which the dividing cell splits into daughter cells), separated by G (‘gap’) phases [54]. DNA synthesis in S phase requires the provision of new building blocks, including pyrimidine and purine bases. Teriflunomide blocks de novo pyrimidine synthesis by specific non-competitive, reversible inhibition of the mitochondrial enzyme dihydro-orotate dehydrogenase (DHODH) [55–57], an enzyme expressed at high levels in proliferating lymphocytes [57, 58]. Teriflunomide-mediated blockade of pyrimidine synthesis interrupts the cell cycle in S phase and exerts a cytostatic effect on proliferating T and B cells, limiting their involvement in the inflammatory processes involved in the MS pathogenesis (Fig. 2) [59].
Proposed MoA of teriflunomide. Resting lymphocytes are unaffected by teriflunomide. They self-renew without any requirement for de novo pyrimidine synthesis, as they can meet their pyrimidine requirements from the salvage pathway. Proliferation of activated lymphocytes relies on de novo pyrimidine synthesis by DHODH, so their proliferation is inhibited by teriflunomide. MoA mechanism of action, DHODH dihydro-orotate dehydrogenase, T T cell, B B cell. Homeostatic proliferation refers to self-renewal, and proliferation refers to expansion in response to stimulus
Cells that do not proliferate in response to activation, such as resting lymphocytes, can self-renew through homeostatic proliferation [60], in which pyrimidine requirements are met through the salvage pathway [61]. Thus, teriflunomide inhibition of DHODH only affects activated, rapidly proliferating lymphocytes (Fig. 2). Rapid, antigen-induced proliferative expansion is unique to lymphocytes [62]. Other proliferating cells, such as gastrointestinal mucosal cells, express lower levels of DHODH [58] and are not specifically stimulated for rapid expansion; therefore, teriflunomide is far less able to inhibit their proliferation.
Of note, teriflunomide is not a nucleotide analogue, and the Ames test shows that it is not DNA intercalating [63]. Furthermore, teriflunomide has no effect on cell viability [64], in contrast to mitoxantrone (Table 1) and the range of immunosuppressive drugs (Table 2) used in MS treatments that interact with DNA (azathioprine, cyclophosphamide) and/or induce apoptosis (azathioprine, cyclophosphamide, methotrexate, mycophenolate mofetil).
4 Supportive In Vitro Evidence
4.1 Lymphocyte Proliferation
A variety of in vitro studies have demonstrated that teriflunomide causes cell cycle arrest in early S phase without apoptosis; these include studies of a human B-cell line stimulated with CpG oligonucleotides and IL-2 [65] and of mitogen-stimulated rat lymphocytes [66]. Similarly, using cultured primary human peripheral blood mononuclear cells (PBMCs) from normal donors, Li et al. [64] demonstrated that teriflunomide inhibits proliferation of CpG-stimulated B cells and anti-CD3-stimulated T cells (both CD4+ and CD8+ T cells) in a dose-dependent manner without causing cell death (Fig. 3a–c). In each case, the inhibitory effects of teriflunomide on DHODH and de novo pyrimidine synthesis were completely abrogated by the addition of exogenous uridine [64].
In vitro, preclinical, and clinical evidence for the selective immunomodulatory MoA of teriflunomide. Teriflunomide inhibits the proliferation of a CD4+ and b CD8+ T-cell subsets, and c B cells, in vitro, in a DHODH-dependent (uridine-reversible) manner. Graphs show the degree of inhibition of proliferation in response to anti-CD3 antibody (a, b) or CpG oligonucleotide (c), measured by CFSE dye dilution and flow cytometry; data presented as mean ± standard error. d In the Dark Agouti EAE rat model of MS, teriflunomide treatment attenuates the number of T cells (identified by anti-CD3 staining and flow cytometry) in cervical spinal cord at all phases of disease; data presented as lease square mean ± standard error of the mean. e White blood cell counts in patients treated with teriflunomide 14 mg remain within the normal range and stabilize after the first 3 months of treatment. f Responses to seasonal influenza vaccine, by influenza strain, in patients treated with teriflunomide 14 mg. Dotted line shows European criteria for vaccine efficacy (70 % of patients with post-vaccination titres ≥40), error bars show 90 % confidence interval. MoA mechanism of action, EAE experimental autoimmune encephalomyelitis, DHODH dihydro-orotate dehydrogenase, CFSE carboxyfluorescein succinimidyl ester, SEM standard error of the mean. Reproduced with permission from [64] (a–c), [81] (d), [94] (f)
In B cells, decreased proliferation in the presence of teriflunomide was associated with a decrease in levels of cyclin-dependent kinase 2 (cdk2), which is required for S phase [67, 68]. These observations are consistent with reports that pyrimidine availability controls progression from early to intermediate S phase [69].
Intriguingly, the anti-proliferative effects of teriflunomide appear to be most pronounced in T cells bearing T-cell receptors (TCRs) with a high affinity for a presented peptide antigen [70]. Individual T cells each express a unique TCR, assembled by recombination at multiple TCR-encoding loci. Each TCR has a different affinity for a peptide antigen, and the mature T cell repertoire is selected on the basis of T-cell avidity for a peptide antigen [71]. Thus, this repertoire includes T cells with a range of avidities for a peptide antigen. In an in vitro setting, using CD4+ T cells specific for an ovalbumin peptide as a model, proliferation of high-avidity T cells was strongly inhibited by teriflunomide, whereas proliferation of low-avidity T cells was less affected [70]. This is of particular interest because high-avidity T cells are thought to mediate many autoimmune diseases, including MS [72]. A selective effect of teriflunomide on autoreactive high-avidity T cells would leave lower-avidity T cells available for normal responses to pathogens.
4.2 Immune Cell Function
In vitro studies have suggested that teriflunomide treatment can impede formation of the immune synapse (necessary for activation of T cells) via impaired integrin activation through a DHODH-independent mechanism [73]. Decreased protein aggregation caused by teriflunomide may further weaken the interaction between T cells and antigen-presenting cells [74].
Teriflunomide treatment significantly decreased release of IL-6, IL-8, and monocyte chemotactic protein-1 (MCP-1) from lipopolysaccharide (LPS)-stimulated human PBMCs, attributed to the monocyte compartment. These effects were not reversible by uridine and therefore unlikely to be DHODH-dependent [64]. This decrease in pro-inflammatory cytokine release is consistent with earlier reports from rodent studies of impaired Th1 differentiation and enhanced Th2 differentiation in the presence of teriflunomide [75, 76]. Li et al. also showed that teriflunomide did not impair LPS-induced maturation of monocyte-derived DCs and had no impact on the ability of LPS-matured DCs to induce allogeneic T-cell responses, suggesting that teriflunomide does not broadly impair the capacity of DCs to regulate adaptive immunity [77].
Of note, many of the earlier studies reporting DHODH-independent effects of teriflunomide used relatively high in vitro concentrations of the drug (~100 μM) when the half maximal concentration for inhibition of DHODH was in the high nanomolar range (657 nM in human splenocytes) [55]. Thus, some of the phenomena observed in these studies, such as modulation of tyrosine kinase activity (reviewed in Claussen MC, Korn T [78]), may not be pertinent to teriflunomide’s in vivo activity in patients with MS.
5 In Vivo (Preclinical) Evidence to Support Current Hypothesis of Teriflunomide MoA
5.1 Rat EAE Model
The Dark Agouti (DA) rat EAE model mimics the inflammatory features of RRMS [79] and has been used in several studies to elucidate the actions of teriflunomide. DA rats develop EAE after immunization with a syngeneic spinal cord homogenate and Freund’s adjuvant. Immunization induces a range of neurological symptoms progressing from tail paralysis, disturbed gait, and paresis to paralysis. These defects are accompanied by demyelinating inflammatory lesions in the spinal cord with infiltrating immune cells.
Administration of either prophylactic or therapeutic (post-disease onset) teriflunomide to DA EAE rats improved disease outcomes, delayed disease onset, and reduced maximal and cumulative disease scores [80]. Histopathology of teriflunomide-treated DA EAE rat spinal cord demonstrated a reduction in demyelination and axonal loss of up to 90 %, with a decrease in inflammation of up to 70 % [80]. Treatment with teriflunomide also attenuated levels of spinal cord-infiltrating T cells (Fig. 3d), NK cells, macrophages, and neutrophils [81]. It is worth noting that in patients with rheumatoid arthritis (RA) treated with leflunomide (the parent compound of teriflunomide), infiltration of macrophages and T cells into the synovial tissue was reduced, and expression patterns of lymphocyte adhesion molecules and matrix metalloproteinase were altered, suggesting an effect of teriflunomide on lymphocyte migration [82]. Teriflunomide treatment also appeared to protect against oligodendrocyte cell death in the CNS of DA EAE rats [83].
Teriflunomide treatment also improved sensory and motor functional outcomes in DA EAE rats. Studies of electrophysiological somatosensory-evoked potential showed that prophylactic teriflunomide treatment prevented both a decrease in waveform amplitude and an increase in the latency to waveform initiation in EAE animals. Therapeutic dosing had similar effects [80]. Measurement of transcranial magnetic motor-evoked potentials showed that teriflunomide prevented a delay in waveform latency and a decrease in waveform amplitude [84].
It is likely that observed reductions in maximal disease scores, decreased axonal loss, and decreased loss of nerve function in teriflunomide-treated DA EAE rats can be attributed to reduced inflammation in these animals, as a consequence of the direct effects of teriflunomide on immune cells. It remains to be determined whether local CNS effects may also contribute to the activity of teriflunomide.
Additional observations made in teriflunomide-treated DA EAE rats indicate that teriflunomide treatment at disease onset reversed immunopathological changes associated with the disease, including mitigation of reductions in spleen weight (spleen weights in teriflunomide-treated animals were only slightly lower than those observed in disease-free animals and significantly higher than those observed in untreated EAE animals), of increased levels of circulating monocytes at acute attack and relapse, and of increased ratios of CD4+/CD8+ T cells in the spleen at acute attack and remission [81].
5.2 Mouse Theiler’s Murine Encephalomyelitis Virus (TMEV) Model
Teriflunomide also showed efficacy in a mouse TMEV infection model used to simulate several pathophysiologic features of MS. In susceptible mouse strains, TMEV induces biphasic disease. A week after infection, TMEV causes polioencephalomyelitis characterized by apoptosis of gray matter neurons. During the chronic phase, approximately 1 month after infection, the virus infects glial cells and macrophages and induces inflammatory demyelination with oligodendrocyte apoptosis and axonal degeneration in the white matter of the spinal cord [85]. Progression of neurological deficits in TMEV-infected mice is mitigated by therapeutic teriflunomide treatment, as shown by a higher neurological function index in teriflunomide-treated TMEV-induced demyelinating disease mice than in vehicle-treated mice [86].
Importantly, teriflunomide treatment in this viral model of MS only resulted in a mild delay in the production of antiviral antibodies and was associated with a transient, non-significant increase in viral load in the CNS 30 days post-infection. This finding supports the concept that protective immunity is maintained in the presence of teriflunomide, and also suggests that a significant increase in viral infections would not be expected in teriflunomide-treated patients with MS [87].
6 Clinical Evidence of Immune Competence and Protective Immunity in Patients Treated with Teriflunomide
Clinical data are consistent with evidence from preclinical in vivo studies suggesting that teriflunomide treatment does not significantly disrupt protective immunity, and its anti-inflammatory activity primarily affects the pathogenic immune processes associated with disease activity.
Pooled data from placebo-controlled studies of teriflunomide, including over 2400 patients from two phase 3 studies (TEMSO [NCT00134563] [9] and TOWER [NCT00751881] [10]) and one phase 2 study (NCT01487096) [88], showed that teriflunomide treatment was associated with a mean decrease in leucocyte counts of approximately 15 % from baseline (Fig. 3e) [89]. However, mean absolute counts remained within the normal range, decreases occurred within the first 3 months of treatment, and levels did not change further with continuing treatment. In the groups treated with teriflunomide from this analysis, a low incidence of serious infections that was not significantly different from placebo was observed, and the relative risk of any infection was not increased with teriflunomide treatment. There were four serious infections considered opportunistic (opportunistic infections were broadly defined in this analysis, and generally considered to be infections that are only pathogenic in immunocompromised individuals); two in patients receiving placebo (one patient developed herpes zoster infection that resolved following treatment discontinuation, and another patient developed hepatitis C and cytomegalovirus [CMV] infection leading to permanent treatment discontinuation), and two in patients treated with teriflunomide 14 mg (one patient with a case of gastrointestinal tuberculosis who recovered following study drug discontinuation and anti-tuberculosis therapy, and a second patient who developed hepatitis with CMV who recovered after treatment discontinuation [discontinuation was protocol mandated due to increased alanine aminotransferase]) [89]. In long-term extensions of the phase 2 and TEMSO studies (up to 9 years of teriflunomide treatment) and consistent with the double-blind phases of the studies, there was no signal for increased malignancies or serious opportunistic infections [90, 91]. Taken together, these findings provide evidence that teriflunomide does not have a negative impact on protective immunity over the observed treatment period.
To investigate whether the generation of recall antigen responses was preserved under teriflunomide treatment, immune responses to the 2011–2012 seasonal influenza vaccination (including strains H1N1, H3N2, and B) were measured in patients with MS treated with IFNβ and in patients exposed to teriflunomide for at least 6 months (TERIVA, NCT014033760) [92]. Most patients had antibodies against each strain detectable at baseline, which was attributed to the 2011–2012 vaccine containing the same strains as the 2010–2011 vaccine. More than 90 % of patients achieved post-vaccination antibody titres ≥40 for H1N1 and B in all groups. For H3N2, titres ≥40 were achieved in ≥90 % of patients in the teriflunomide 7-mg and IFNβ groups, and in 77 % of the teriflunomide 14-mg group, respectively (Fig. 3f). Geometric mean titre ratios (post-/pre-vaccination) were ≥2.5 for all groups and strains, except for H1N1 in the 14-mg group (2.3), confirming vaccine efficacy as per European guidelines [92, 93]. Therefore, the mild quantitative and qualitative change in the immune response to vaccination induced with teriflunomide was not clinically significant, and the ability of patients to mount protective vaccine responses to recall antigens while receiving teriflunomide was considered to be preserved [92].
Rabies vaccination was used as a tool to assess the impact of teriflunomide on the immune responses to a neoantigen. Healthy volunteers who had never been vaccinated before with rabies vaccine received teriflunomide or placebo for 1 month prior to vaccination; a slightly lower mean antibody response in the teriflunomide group than in the placebo group was observed. However, adequate seroprotection (antibody titre >0.5 IU/mL) was achieved in all subjects [94].
In summary, data on the clinical consequences of treatment indicate that teriflunomide-while slightly reducing peripheral leucocyte counts-does not compromise clinically relevant immune competence. In keeping with this, responses to both recall and neoantigen vaccinations, though mildly reduced, remained sufficient to afford seroprotection.
7 Safety Considerations with Teriflunomide
As discussed previously, the primary action of teriflunomide is proposed to be specific to activated lymphocytes as these cells express high levels of DHODH and undergo rapid proliferative expansion [58, 62]. However, all patients with MS treated with any DMT may experience a range of side effects that are not necessarily related to the proposed primary MoA of that therapy [95]. In this regard, clinical trials of teriflunomide have demonstrated its manageable safety profile (Table 3) [96, 97].
Common side effects of treatment with teriflunomide include hair thinning, diarrhea, alanine aminotransferase elevation, nausea, and headache. The hair thinning sometimes reported in patients receiving teriflunomide is typically limited and diffuse and best described as telogen effluvium. It is distinct from the anagen effluvium complete hair loss observed in patients undergoing chemotherapy [98] and is not a sign of immune suppression. Hair thinning events mainly resolved on-treatment [96] and only led to treatment discontinuation in ≤2 % of patients [9, 10]. Teriflunomide is the active metabolite of leflunomide, approved for the treatment of RA since 1998 [99]. Elevations of serum aminotransferases in clinical trials and rare cases of liver injury in the post-marketing setting have been documented in patients treated with leflunomide [100] so as a precaution, patients receiving teriflunomide are subject to regular hepatic monitoring during the first 6 months of treatment [101, 102]. In some locations, less frequent monitoring continues throughout subsequent treatment [102].
Leflunomide is associated with embryo-lethality and teratogenicity in rats and rabbits, and therefore is contraindicated in women of childbearing potential not using reliable contraception [99]. However, two prospective studies conducted by the Organization of Teratology Information Specialists (OTIS), have found no increase in the rate of major structural defects in newborns of women with RA exposed to leflunomide [103, 104]. Additionally, in the period 2001–2013, there were more than 2.3 million patient years of leflunomide use without any signal for teratogenicity (Genzyme, data on file). Based on the occurrence of teratogenicity and embryo-lethality in the offspring of teriflunomide-treated rats and rabbits, teriflunomide is also contraindicated in pregnant women, or women of childbearing potential not using reliable contraception [101]. Preclinical teriflunomide studies showed no evidence for mutagenicity or clastogenicity [63] and consistent with the OTIS findings for leflunomide, all newborns born to mothers or fathers who received teriflunomide had no structural or functional abnormalities at birth [105]. In the event of pregnancy, patients receiving teriflunomide must undergo an accelerated elimination procedure until teriflunomide plasma concentrations fall below 0.02 mg/L, a level predicted to have minimal risk to the fetus [101].
8 Teriflunomide as Part of the Growing MS Therapeutic Armamentarium
The MoAs of therapies in development or approved for use in RRMS are summarized in Table 1. Additional therapies are sometimes used off-label in patients with MS (Table 2), though it is important to note that use of these immunosuppressant medications may be associated with serious side effects such as leukopenia or increases in the risk of malignancy.
The immunomodulation exerted by teriflunomide is seemingly selective in a manner that is particularly useful in the treatment of RRMS, a disease mainly driven by activated T and B lymphocytes. Importantly, a specific cytostatic effect on proliferating lymphocytes as a primary MoA is unique to teriflunomide. None of the agents currently in clinical trials or being marketed for MS possess a similar specificity for activated lymphocytes inherent in their MoA. Other agents rely on mechanisms such as direct cytotoxicity [106], induction of apoptosis [107], or exclusion of lymphocytes from the CNS [108–110] to reduce the numbers of lymphocytes available to contribute to MS pathogenesis.
9 Summary and Conclusions
Teriflunomide is known to reversibly inhibit DHODH, a mitochondrial enzyme specifically required for de novo pyrimidine biosynthesis in activated lymphocytes, and as such has no direct effects on DNA. In keeping with this primary MoA, teriflunomide acts to impair the proliferation of activated T and B cells, and reduces their ability to participate in a potentially damaging immune attack on the CNS.
Emerging in vitro and in vivo experimental data increasingly support the view that teriflunomide exerts a selective effect on the immune system that strikes a favorable balance between efficacy and safety. This selectivity and balance is reinforced in observations from studies in patients with MS. Phase 3 studies showed that teriflunomide can restrict the type of limited immune activation relevant to MS disease activity; trial results showed significant reductions in disability progression, relapse rates, and magnetic resonance imaging measures of disease activity [9, 111]. At the same time, vaccination studies in patients with MS or healthy subjects have shown that teriflunomide treatment does not limit the immune activation required for maintaining immune competence: the capacity to mount functional vaccine responses (to both recall antigens and neoantigens) is preserved. In addition, the comparable incidence of infections and malignancies observed with teriflunomide and placebo also indicates maintenance of functional immune competence. Teriflunomide can be considered as an immune therapy targeting pathogenic inflammatory processes involved in the MS disease process without significant compromise of the patient’s protective immune functions. Given the selectivity of its effects on the immune system, teriflunomide represents a valuable addition to the list of approved therapies available to treat patients with MS.
References
Hauser SL, Oksenberg JR. The neurobiology of multiple sclerosis: genes, inflammation, and neurodegeneration. Neuron. 2006;52:61–76.
Trapp BD, Nave KA. Multiple sclerosis: an immune or neurodegenerative disorder? Annu Rev Neurosci. 2008;31:247–69.
Sospedra M, Martin R. Immunology of multiple sclerosis. Annu Rev Immunol. 2005;23:683–747.
McFarland HF, Martin R. Multiple sclerosis: a complicated picture of autoimmunity. Nat Immunol. 2007;8:913–9.
Hafler DA. Multiple sclerosis. J Clin Invest. 2004;113:788–94.
Liblau RS, Gonzalez-Dunia D, Wiendl H, et al. Neurons as targets for T cells in the nervous system. Trends Neurosci. 2013.
Dutta R, Trapp BD. Mechanisms of neuronal dysfunction and degeneration in multiple sclerosis. Prog Neurobiol. 2011;93:1–12.
Lucchinetti CF, Popescu BF, Bunyan RF, et al. Inflammatory cortical demyelination in early multiple sclerosis. N Engl J Med. 2011;365:2188–97.
O’Connor P, Wolinsky JS, Confavreux C, et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N Engl J Med. 2011;365:1293–303.
Confavreux C, O’Connor P, Comi G, et al. Oral teriflunomide for patients with relapsing multiple sclerosis (TOWER): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol. 2014;13:247–56.
Frischer JM, Bramow S, Dal-Bianco A, et al. The relation between inflammation and neurodegeneration in multiple sclerosis brains. Brain. 2009;132:1175–89.
Christensen JR, Bornsen L, Ratzer R, et al. Systemic inflammation in progressive multiple sclerosis involves follicular T-helper, th17- and activated B-cells and correlates with progression. PLoS One. 2013;8:e57820.
Melzer N, Meuth SG, Wiendl H. CD8+ T cells and neuronal damage: direct and collateral mechanisms of cytotoxicity and impaired electrical excitability. FASEB J. 2009;23:3659–73.
Kerlero de Rosbo N, Milo R, Lees MB, et al. Reactivity to myelin antigens in multiple sclerosis. Peripheral blood lymphocytes respond predominantly to myelin oligodendrocyte glycoprotein. J Clin Invest. 1993;92:2602–8.
Ransohoff RM, Kivisakk P, Kidd G. Three or more routes for leukocyte migration into the central nervous system. Nat Rev Immunol. 2003;3:569–81.
Galea I, Bernardes-Silva M, Forse PA, et al. An antigen-specific pathway for CD8 T cells across the blood–brain barrier. J Exp Med. 2007;204:2023–30.
Archambault AS, Sim J, Gimenez MA, et al. Defining antigen-dependent stages of T cell migration from the blood to the central nervous system parenchyma. Eur J Immunol. 2005;35:1076–85.
Reboldi A, Coisne C, Baumjohann D, et al. C–C chemokine receptor 6-regulated entry of TH-17 cells into the CNS through the choroid plexus is required for the initiation of EAE. Nat Immunol. 2009;10:514–23.
Arima Y, Harada M, Kamimura D, et al. Regional neural activation defines a gateway for autoreactive T cells to cross the blood–brain barrier. Cell. 2012;148:447–57.
Hohlfeld R, Wekerle H. Autoimmune concepts of multiple sclerosis as a basis for selective immunotherapy: from pipe dreams to (therapeutic) pipelines. Proc Natl Acad Sci USA. 2004;101(Suppl 2):14599–606.
Hohlfeld R. Multiple sclerosis: human model for EAE? Eur J Immunol. 2009;39:2036–9.
Ben-Nun A, Wekerle H, Cohen IR. The rapid isolation of clonable antigen-specific T lymphocyte lines capable of mediating autoimmune encephalomyelitis. Eur J Immunol. 1981;11:195–9.
Beecham AH, Patsopoulos NA, Xifara DK, et al. Analysis of immune-related loci identifies 48 new susceptibility variants for multiple sclerosis. Nat Genet. 2013;45:1353–60.
Panitch HS, Hirsch RL, Haley AS, et al. Exacerbations of multiple sclerosis in patients treated with gamma interferon. Lancet. 1987;1:893–5.
Gutcher I, Becher B. APC-derived cytokines and T cell polarization in autoimmune inflammation. J Clin Invest. 2007;117:1119–27.
Kebir H, Kreymborg K, Ifergan I, et al. Human TH17 lymphocytes promote blood–brain barrier disruption and central nervous system inflammation. Nat Med. 2007;13:1173–5.
McKenzie BS, Kastelein RA, Cua DJ. Understanding the IL-23–IL-17 immune pathway. Trends Immunol. 2006;27:17–23.
Tzartos JS, Friese MA, Craner MJ, et al. Interleukin-17 production in central nervous system-infiltrating T cells and glial cells is associated with active disease in multiple sclerosis. Am J Pathol. 2008;172:146–55.
Darlington PJ, Touil T, Doucet JS, et al. Diminished Th17 (not Th1) responses underlie multiple sclerosis disease abrogation after hematopoietic stem cell transplantation. Ann Neurol. 2013;73:341–54.
Friese MA, Fugger L. Pathogenic CD8(+) T cells in multiple sclerosis. Ann Neurol. 2009;66:132–41.
Brisebois M, Zehntner SP, Estrada J, et al. A pathogenic role for CD8+ T cells in a spontaneous model of demyelinating disease. J Immunol. 2006;177:2403–11.
Traugott U, Reinherz EL, Raine CS. Multiple sclerosis: distribution of T cell subsets within active chronic lesions. Science. 1983;219:308–10.
Crawford MP, Yan SX, Ortega SB, et al. High prevalence of autoreactive, neuroantigen-specific CD8+ T cells in multiple sclerosis revealed by novel flow cytometric assay. Blood. 2004;103:4222–31.
Zozulya AL, Wiendl H. The role of CD8 suppressors versus destructors in autoimmune central nervous system inflammation. Hum Immunol. 2008;69:797–804.
Zozulya AL, Wiendl H. The role of regulatory T cells in multiple sclerosis. Nat Clin Pract Neurol. 2008;4:384–98.
Bjerg L, Brosbol-Ravnborg A, Torring C, et al. Altered frequency of T regulatory cells is associated with disability status in relapsing–remitting multiple sclerosis patients. J Neuroimmunol. 2012;249:76–82.
Colombo M, Dono M, Gazzola P, et al. Accumulation of clonally related B lymphocytes in the cerebrospinal fluid of multiple sclerosis patients. J Immunol. 2000;164:2782–9.
Krumbholz M, Derfuss T, Hohlfeld R, et al. B cells and antibodies in multiple sclerosis pathogenesis and therapy. Nat Rev Neurol. 2012;8:613–23.
von Budingen HC, Bar-Or A, Zamvil SS. B cells in multiple sclerosis: connecting the dots. Curr Opin Immunol. 2011;23:713–20.
Serafini B, Rosicarelli B, Magliozzi R, et al. Detection of ectopic B-cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain Pathol. 2004;14:164–74.
Lovato L, Willis SN, Rodig SJ, et al. Related B cell clones populate the meninges and parenchyma of patients with multiple sclerosis. Brain. 2011;134:534–41.
von Budingen HC, Kuo TC, Sirota M, et al. B cell exchange across the blood–brain barrier in multiple sclerosis. J Clin Invest. 2012;122:4533–43.
Duddy M, Niino M, Adatia F, et al. Distinct effector cytokine profiles of memory and naive human B cell subsets and implication in multiple sclerosis. J Immunol. 2007;178:6092–9.
Bar-Or A, Fawaz L, Fan B, et al. Abnormal B-cell cytokine responses a trigger of T-cell-mediated disease in MS? Ann Neurol. 2010;67:452–61.
Barr TA, Shen P, Brown S, et al. B cell depletion therapy ameliorates autoimmune disease through ablation of IL-6-producing B cells. J Exp Med. 2012;209:1001–10.
Ray A, Mann MK, Basu S, et al. A case for regulatory B cells in controlling the severity of autoimmune-mediated inflammation in experimental autoimmune encephalomyelitis and multiple sclerosis. J Neuroimmunol. 2011;230:1–9.
Iwata Y, Matsushita T, Horikawa M, et al. Characterization of a rare IL-10-competent B-cell subset in humans that parallels mouse regulatory B10 cells. Blood. 2011;117:530–41.
Kalampokis I, Yoshizaki A, Tedder TF. IL-10-producing regulatory B cells (B10 cells) in autoimmune disease. Arthritis Res Ther. 2013;15(Suppl 1):S1.
Correale J, Farez M, Razzitte G. Helminth infections associated with multiple sclerosis induce regulatory B cells. Ann Neurol. 2008;64:187–99.
Nuyts A, Lee W, Bashir-Dar R, et al. Dendritic cells in multiple sclerosis: key players in the immunopathogenesis, key players for new cellular immunotherapies? Mult Scler. 2013.
Chanvillard C, Jacolik RF, Infante-Duarte C, et al. The role of natural killer cells in multiple sclerosis and their therapeutic implications. Front Immunol. 2013;4:63.
Brosnan CF, Raine CS. The astrocyte in multiple sclerosis revisited. Glia. 2013;61:453–65.
Friese MA, Fugger L. T cells and microglia as drivers of multiple sclerosis pathology. Brain. 2007;130:2755–7.
Alberts B, Johnson A, Lewis J, et al. Molecular biology of the cell. 4th ed. New York: Garland Science; 2002.
Bruneau JM, Yea CM, Spinella-Jaegle S, et al. Purification of human dihydro-orotate dehydrogenase and its inhibition by A77 1726, the active metabolite of leflunomide. Biochem J. 1998;336(Pt 2):299–303.
Cherwinski HM, Cohn RG, Cheung P, et al. The immunosuppressant leflunomide inhibits lymphocyte proliferation by inhibiting pyrimidine biosynthesis. J Pharmacol Exp Ther. 1995;275:1043–9.
Ruckemann K, Fairbanks LD, Carrey EA, et al. Leflunomide inhibits pyrimidine de novo synthesis in mitogen-stimulated T-lymphocytes from healthy humans. J Biol Chem. 1998;273:21682–91.
Loffler M, Klein A, Hayek-Ouassini M, et al. Dihydroorotate dehydrogenase mRNA and protein expression analysis in normal and drug-resistant cells. Nucleosides Nucleotides Nucleic Acids. 2004;23:1281–5.
Gold R, Wolinsky JS. Pathophysiology of multiple sclerosis and the place of teriflunomide. Acta Neurol Scand. 2011;124:75–84.
Jameson SC. Maintaining the norm: T-cell homeostasis. Nat Rev Immunol. 2002;2:547–56.
Fairbanks LD, Bofill M, Ruckemann K, et al. Importance of ribonucleotide availability to proliferating T-lymphocytes from healthy humans. Disproportionate expansion of pyrimidine pools and contrasting effects of de novo synthesis inhibitors. J Biol Chem. 1995;270:29682–9.
Pearce EL. Metabolism in T cell activation and differentiation. Curr Opin Immunol. 2010;22:314–20.
Davenport L, Czich A, Turpault S. Teriflunomide: no effects on sperm DNA: ECTRIMS poster 1171. Mult Scler J. 2013;19:559–73.
Li L, Liu J, Delohery T, et al. The effects of teriflunomide on lymphocyte subpopulations in human peripheral blood mononuclear cells. J Neuroimmunol. 2013;265:82–90.
Ringshausen I, Oelsner M, Bogner C, et al. The immunomodulatory drug leflunomide inhibits cell cycle progression of B-CLL cells. Leukemia. 2008;22:635–8.
Cherwinski HM, McCarley D, Schatzman R, et al. The immunosuppressant leflunomide inhibits lymphocyte progression through cell cycle by a novel mechanism. J Pharmacol Exp Ther. 1995;272:460–8.
Siemasko KF, Chong AS, Williams JW, et al. Regulation of B cell function by the immunosuppressive agent leflunomide. Transplantation. 1996;61:635–42.
Rosenblatt J, Gu Y, Morgan DO. Human cyclin-dependent kinase 2 is activated during the S and G2 phases of the cell cycle and associates with cyclin A. Proc Natl Acad Sci USA. 1992;89:2824–8.
Quemeneur L, Gerland LM, Flacher M, et al. Differential control of cell cycle, proliferation, and survival of primary T lymphocytes by purine and pyrimidine nucleotides. J Immunol. 2003;170:4986–95.
Posevitz V, Chudyka D, Kurth F, et al. Teriflunomide suppresses antigen induced T-cell expansion in a TCR avidity dependent fashion (P1107). Mult Scler J. 2012;18(S4):509–20.
Starr TK, Jameson SC, Hogquist KA. Positive and negative selection of T cells. Annu Rev Immunol. 2003;21:139–76.
Bielekova B, Sung MH, Kadom N, et al. Expansion and functional relevance of high-avidity myelin-specific CD4+ T cells in multiple sclerosis. J Immunol. 2004;172:3893–904.
Zeyda M, Poglitsch M, Geyeregger R, et al. Disruption of the interaction of T cells with antigen-presenting cells by the active leflunomide metabolite teriflunomide: involvement of impaired integrin activation and immunologic synapse formation. Arthritis Rheum. 2005;52:2730–9.
Fuentealba RA, Marasa J, Diamond MI, et al. An aggregation sensing reporter identifies leflunomide and teriflunomide as polyglutamine aggregate inhibitors. Hum Mol Genet. 2012;21:664–80.
Korn T, Magnus T, Toyka K, et al. Modulation of effector cell functions in experimental autoimmune encephalomyelitis by leflunomide-mechanisms independent of pyrimidine depletion. J Leukoc Biol. 2004;76:950–60.
Dimitrova P, Skapenko A, Herrmann ML, et al. Restriction of de novo pyrimidine biosynthesis inhibits Th1 cell activation and promotes Th2 cell differentiation. J Immunol. 2002;169:3392–9.
Li L, Liu J, Zhang D, et al. Teriflunomide treatment of human monocyte-derived dendritic cells in vitro does not impair their maturation or ability to induce allogeneic T-cell responses|ECTRIMS 2012. Mult Scler J. 2012;18:279–508 (P950).
Claussen MC, Korn T. Immune mechanisms of new therapeutic strategies in MS: teriflunomide. Clin Immunol. 2012;142:49–56.
Lorentzen JC, Issazadeh S, Storch M, et al. Protracted, relapsing and demyelinating experimental autoimmune encephalomyelitis in DA rats immunized with syngeneic spinal cord and incomplete Freund’s adjuvant. J Neuroimmunol. 1995;63:193–205.
Merrill JE, Hanak S, Pu SF, et al. Teriflunomide reduces behavioral, electrophysiological, and histopathological deficits in the Dark Agouti rat model of experimental autoimmune encephalomyelitis. J Neurol. 2009;256:89–103.
Ringheim G, Lee L, Laws-Ricker L, et al. Teriflunomide attenuates immunopathological changes in the Dark Agouti rat model of experimental autoimmune encephalomyelitis. Front Mult Scler Neuroimmunol. 2013;4:169.
Kraan MC, Reece RJ, Barg EC, et al. Modulation of inflammation and metalloproteinase expression in synovial tissue by leflunomide and methotrexate in patients with active rheumatoid arthritis. Findings in a prospective, randomized, double-blind, parallel-design clinical trial in thirty-nine patients at two centers. Arthritis Rheum. 2000;43:1820–30.
Petty M, Lee L, Ying X. Teriflunomide treatment reduces infiltration of macrophages, T cells and B cells, and increases survival of oligodendrocytes in the spinal cord of the Dark Agouti rat model of Experimental Allergic Encephalomyelitis. AAN 2010, 10–17 April 2010, Toronto, Canada, 2010.
Iglesias-Bregna D, Hanak S, Ji Z, et al. Effects of prophylactic and therapeutic teriflunomide in transcranial magnetic stimulation-induced motor-evoked potentials in the Dark Agouti rat model of experimental autoimmune encephalomyelitis. J Pharmacol Exp Ther. 2013;347:203–11.
Tsunoda I, Fujinami RS. Neuropathogenesis of Theiler’s murine encephalomyelitis virus infection, an animal model for multiple sclerosis. J Neuroimmune Pharmacol. 2010;5:355–69.
Pachner A, Li L. Teriflunomide ameliorates disability progression in the Theiler’s virus-induced demyelinating disease model of MS [P05.196]|AAN 2013. Neurology. 2013:P05.196.
Pachner A, Li L. Effect of teriflunomide on the viral load and anti-viral antibody responses in the Theiler’s virus model of MS [P02.143]|AAN 2012. Neurology. 2012:P02.143.
O’Connor PW, Li D, Freedman MS, et al. A Phase II study of the safety and efficacy of teriflunomide in multiple sclerosis with relapses. Neurology. 2006;66:894–900.
Singer B, Comi G, Miller A, et al. Frequency of infections during treatment with teriflunomide: pooled data from three placebo-controlled teriflunomide studies|AAN 2013. Neurology. 2013.
Freedman M, Wolinsky JS, Comi G, et al. Long-term safety and efficacy of teriflunomide in patients with relapsing forms of multiple sclerosis in the TEMSO extension trial. ECTRIMS 2013 Poster 544. Mult Scler J. 2013;19:74–558.
Confavreux C, Li DK, Freedman MS, et al. Long-term follow-up of a phase 2 study of oral teriflunomide in relapsing multiple sclerosis: safety and efficacy results up to 8.5 years. Mult Scler. 2012;18:1278–89.
Bar-Or A, Freedman MS, Kremenchutzky M, et al. Teriflunomide effect on immune response to influenza vaccine in patients with multiple sclerosis. Neurology. 2013;81:552–8.
(CPMP) Cfpmp. Note for guidance on harmonisation of requirements for influenza vaccines. In: Unit HME (ed) The European Agency for the Evaluation of Medicinal Products, 1997.
Bar-Or A, Larouche R, Legrand B, et al. Immune response to neoantigen and recall antigens in healthy subjects receiving teriflunomide. ECTRIMS Poster 622. Mult Scler J. 2013;19:74–558.
Ali R, Nicholas RS, Muraro PA. Drugs in development for relapsing multiple sclerosis. Drugs. 2013;73:625–50.
Leist T, Freedman M, Kappos L, et al. Pooled safety data from three placebo-controlled teriflunomide studies: ECTRIMS 2013 Poster 633. Mult Scler J. 2013;19:74–558.
Garnock-Jones KP. Teriflunomide: a review of its use in relapsing multiple sclerosis. CNS Drugs. 2013;27:1103–23.
Trueb RM. Chemotherapy-induced alopecia. Semin Cutan Med Surg. 2009;28:11–4.
LLC s-aUS. ARAVA prescribing information. Bridgewater: Sanofi-Aventis U.S. LLC; 2012.
Strand V, Cohen S, Schiff M, et al. Treatment of active rheumatoid arthritis with leflunomide compared with placebo and methotrexate. Leflunomide Rheumatoid Arthritis Investigators Group. Arch Intern Med. 1999;159:2542–50.
Genzyme. AUBAGIO US prescribing information. Cambridge: Genzyme Corporation, a sanofi company; 2012.
Sanofi-Aventis. AUBAGIO summary of product characteristics. France: Sanofi-Aventis; 2013.
Chambers CD, Johnson DL, Robinson LK, et al. Birth outcomes in women who have taken leflunomide during pregnancy. Arthritis Rheum. 2010;62:1494–503.
Cassina M, Johnson DL, Robinson LK, et al. Pregnancy outcome in women exposed to leflunomide before or during pregnancy. Arthritis Rheum. 2012;64:2085–94.
Kieseier B, Benamor M, Truffinet P. Pregnancy outcomes from the teriflunomide clinical development programme: PACTRIMS 2013 Poster 79. In: 6th Congress of the Pan-Asian Committee for Treatment and Research in Multiple Sclerosis (PACTRIMS); 6–8 November 2013, Kyoto, Japan.
Chan A, Weilbach FX, Toyka KV, et al. Mitoxantrone induces cell death in peripheral blood leucocytes of multiple sclerosis patients. Clin Exp Immunol. 2005;139:152–8.
Tiede I, Fritz G, Strand S, et al. CD28-dependent Rac1 activation is the molecular target of azathioprine in primary human CD4+ T lymphocytes. J Clin Invest. 2003;111:1133–45.
Matloubian M, Lo CG, Cinamon G, et al. Lymphocyte egress from thymus and peripheral lymphoid organs is dependent on S1P receptor 1. Nature. 2004;427:355–60.
Bauer M, Brakebusch C, Coisne C, et al. Beta1 integrins differentially control extravasation of inflammatory cell subsets into the CNS during autoimmunity. Proc Natl Acad Sci USA. 2009;106:1920–5.
Gan Y, Liu R, Wu W, et al. Antibody to alpha4 integrin suppresses natural killer cells infiltration in central nervous system in experimental autoimmune encephalomyelitis. J Neuroimmunol. 2012;247:9–15.
Wolinsky JS, Narayana PA, Nelson F, et al. Magnetic resonance imaging outcomes from a phase III trial of teriflunomide. Mult Scler. 2013.
Genzyme. Alemtuzumab FDA highlights of prescribing information, 2007.
Ontaneda D, Cohen JA. The benefits and risks of alemtuzumab in multiple sclerosis. Expert Rev Clin Immunol. 2013;9:189–91.
Wiendl H, Kieseier B. Multiple sclerosis: reprogramming the immune repertoire with alemtuzumab in MS. Nat Rev Neurol. 2013;9:125–6.
Biogen_Idec. FDA Approved Labeling Text for Tecfidera (dimethyl fumarate). 2013.
Scannevin RH, Chollate S, Jung MY, et al. Fumarates promote cytoprotection of central nervous system cells against oxidative stress via the nuclear factor (erythroid-derived 2)-like 2 pathway. J Pharmacol Exp Ther. 2012;341:274–84.
Moharregh-Khiabani D, Blank A, Skripuletz T, et al. Effects of fumaric acids on cuprizone induced central nervous system de- and remyelination in the mouse. PLoS One. 2010;5:e11769.
Treumer F, Zhu K, Glaser R, et al. Dimethylfumarate is a potent inducer of apoptosis in human T cells. J Invest Dermatol. 2003;121:1383–8.
de Jong R, Bezemer AC, Zomerdijk TP, et al. Selective stimulation of T helper 2 cytokine responses by the anti-psoriasis agent monomethylfumarate. Eur J Immunol. 1996;26:2067–74.
Peng H, Guerau-de-Arellano M, Mehta VB, et al. Dimethyl fumarate inhibits dendritic cell maturation via nuclear factor kappaB (NF-kappaB) and extracellular signal-regulated kinase 1 and 2 (ERK1/2) and mitogen stress-activated kinase 1 (MSK1) signaling. J Biol Chem. 2012;287:28017–26.
Vandermeeren M, Janssens S, Borgers M, et al. Dimethylfumarate is an inhibitor of cytokine-induced E-selectin, VCAM-1, and ICAM-1 expression in human endothelial cells. Biochem Biophys Res Commun. 1997;234:19–23.
Schilling S, Goelz S, Linker R, et al. Fumaric acid esters are effective in chronic experimental autoimmune encephalomyelitis and suppress macrophage infiltration. Clin Exp Immunol. 2006;145:101–7.
Novartis. Gilenya (Fingolimod) summary of product characteristics updated 12/04/2013. 2013.
Mandala S, Hajdu R, Bergstrom J, et al. Alteration of lymphocyte trafficking by sphingosine-1-phosphate receptor agonists. Science. 2002;296:346–9.
Coelho RP, Payne SG, Bittman R, et al. The immunomodulator FTY720 has a direct cytoprotective effect in oligodendrocyte progenitors. J Pharmacol Exp Ther. 2007;323:626–35.
Miron VE, Ludwin SK, Darlington PJ, et al. Fingolimod (FTY720) enhances remyelination following demyelination of organotypic cerebellar slices. Am J Pathol. 2010;176:2682–94.
Kohne A, Stettner M, Jangouk P, et al. Fingolimod impedes Schwann cell-mediated myelination: implications for the treatment of immune neuropathies? Arch Neurol. 2012;69:1280–9.
Mullershausen F, Craveiro LM, Shin Y, et al. Phosphorylated FTY720 promotes astrocyte migration through sphingosine-1-phosphate receptors. J Neurochem. 2007;102:1151–61.
Xie JH, Nomura N, Koprak SL, et al. Sphingosine-1-phosphate receptor agonism impairs the efficiency of the local immune response by altering trafficking of naive and antigen-activated CD4+ T cells. J Immunol. 2003;170:3662–70.
TEVA_Pharmaceuticals. Copaxone (Galtiramer Acetate) full prescribing information, 2009.
Boster A, Bartoszek MP, O’Connell C, et al. Efficacy, safety, and cost-effectiveness of glatiramer acetate in the treatment of relapsing–remitting multiple sclerosis. Ther Adv Neurol Disord. 2011;4:319–32.
Aharoni R, Teitelbaum D, Sela M, et al. Bystander suppression of experimental autoimmune encephalomyelitis by T cell lines and clones of the Th2 type induced by copolymer 1. J Neuroimmunol. 1998;91:135–46.
Fridkis-Hareli M, Teitelbaum D, Pecht I, et al. Binding of copolymer 1 and myelin basic protein leads to clustering of class II MHC molecules on antigen-presenting cells. Int Immunol. 1997;9:925–34.
Vieira PL, Heystek HC, Wormmeester J, et al. Glatiramer acetate (copolymer-1, copaxone) promotes Th2 cell development and increased IL-10 production through modulation of dendritic cells. J Immunol. 2003;170:4483–8.
Aharoni R, Teitelbaum D, Leitner O, et al. Specific Th2 cells accumulate in the central nervous system of mice protected against experimental autoimmune encephalomyelitis by copolymer 1. Proc Natl Acad Sci USA. 2000;97:11472–7.
Teitelbaum D, Milo R, Arnon R, et al. Synthetic copolymer 1 inhibits human T-cell lines specific for myelin basic protein. Proc Natl Acad Sci USA. 1992;89:137–41.
Skihar V, Silva C, Chojnacki A, et al. Promoting oligodendrogenesis and myelin repair using the multiple sclerosis medication glatiramer acetate. Proc Natl Acad Sci USA. 2009;106:17992–7.
Novartis. Interferon beta (Extavia) summary of product characteristics updated 16/04/2013, 2013.
Bayer. Interferon beta (Betaferon) summary of product characteristics updated 05/02/2013, 2013.
Idec B. Interferon beta (Avonex) summary of product characteristics updated 07/02/2013, 2013.
Bongioanni P, Lombardo F, Moscato G, et al. T-cell interferon gamma receptor binding in interferon beta-1b-treated patients with multiple sclerosis. Arch Neurol. 1999;56:217–22.
Noronha A, Toscas A, Jensen MA. Interferon beta augments suppressor cell function in multiple sclerosis. Ann Neurol. 1990;27:207–10.
Arnason BG. Interferon beta in multiple sclerosis. Clin Immunol Immunopathol. 1996;81:1–11.
Vosoughi R, Freedman MS. Therapy of MS. Clin Neurol Neurosurg. 2010;112:365–85.
Ozenci V, Kouwenhoven M, Huang YM, et al. Multiple sclerosis is associated with an imbalance between tumour necrosis factor-alpha (TNF-alpha)- and IL-10-secreting blood cells that is corrected by interferon-beta (IFN-beta) treatment. Clin Exp Immunol. 2000;120:147–53.
Shapiro S, Galboiz Y, Lahat N, et al. The ‘immunological-synapse’ at its APC side in relapsing and secondary-progressive multiple sclerosis: modulation by interferon-beta. J Neuroimmunol. 2003;144:116–24.
Yushchenko M, Mader M, Elitok E, et al. Interferon-beta-1 b decreased matrix metalloproteinase-9 serum levels in primary progressive multiple sclerosis. J Neurol. 2003;250:1224–8.
EMD_Serono. Novotrone (mitoxantrone for injection concentrate) FDA-approved label, 2010.
Koeller J, Eble M. Mitoxantrone: a novel anthracycline derivative. Clin Pharm. 1988;7:574–81.
Burns SA, Lee Archer R, Chavis JA, et al. Mitoxantrone repression of astrocyte activation: relevance to multiple sclerosis. Brain Res. 2012;1473:236–41.
Fidler JM, DeJoy SQ, Gibbons JJ Jr. Selective immunomodulation by the antineoplastic agent mitoxantrone. I. Suppression of B lymphocyte function. J Immunol. 1986;137:727–32.
Biogen_Idec. Natalizumab (Tysabri) FDA-approved label, 2004.
Millonig A, Hegen H, Di Pauli F, et al. Natalizumab treatment reduces endothelial activity in MS patients. J Neuroimmunol. 2010;227:190–4.
Benkert TF, Dietz L, Hartmann EM, et al. Natalizumab exerts direct signaling capacity and supports a pro-inflammatory phenotype in some patients with multiple sclerosis. PLoS One. 2012;7:e52208.
Bornsen L, Christensen JR, Ratzer R, et al. Effect of natalizumab on circulating CD4+ T-cells in multiple sclerosis. PLoS One. 2012;7:e47578.
de Andres C, Teijeiro R, Alonso B, et al. Long-term decrease in VLA-4 expression and functional impairment of dendritic cells during natalizumab therapy in patients with multiple sclerosis. PLoS One. 2012;7:e34103.
Sanofi. Aubagio EMA summary of product characteristics, 2013.
Martin JF, Perry JS, Jakhete NR, et al. An IL-2 paradox: blocking CD25 on T cells induces IL-2-driven activation of CD56(bright) NK cells. J Immunol. 2010;185:1311–20.
Martin R. Anti-CD25 (daclizumab) monoclonal antibody therapy in relapsing–remitting multiple sclerosis. Clin Immunol. 2012;142:9–14.
Perry JS, Han S, Xu Q, et al. Inhibition of LTi cell development by CD25 blockade is associated with decreased intrathecal inflammation in multiple sclerosis. Sci Transl Med. 2012;4:145ra06.
Wuest SC, Edwan JH, Martin JF, et al. A role for interleukin-2 trans-presentation in dendritic cell-mediated T cell activation in humans, as revealed by daclizumab therapy. Nat Med. 2011;17:604–9.
Aharoni R, Saada R, Eilam R, et al. Oral treatment with laquinimod augments regulatory T-cells and brain-derived neurotrophic factor expression and reduces injury in the CNS of mice with experimental autoimmune encephalomyelitis. J Neuroimmunol. 2012;251:14–24.
Wegner C, Stadelmann C, Pfortner R, et al. Laquinimod interferes with migratory capacity of T cells and reduces IL-17 levels, inflammatory demyelination and acute axonal damage in mice with experimental autoimmune encephalomyelitis. J Neuroimmunol. 2010;227:133–43.
Toubi E, Nussbaum S, Staun-Ram E, et al. Laquinimod modulates B cells and their regulatory effects on T cells in multiple sclerosis. J Neuroimmunol. 2012;251:45–54.
Schulze-Topphoff U, Shetty A, Varrin-Doyer M, et al. Laquinimod, a quinoline-3-carboxamide, induces type II myeloid cells that modulate central nervous system autoimmunity. PLoS One. 2012;7:e33797.
Zou LP, Abbas N, Volkmann I, et al. Suppression of experimental autoimmune neuritis by ABR-215062 is associated with altered Th1/Th2 balance and inhibited migration of inflammatory cells into the peripheral nerve tissue. Neuropharmacology. 2002;42:731–9.
Kappos L, Li D, Calabresi PA, et al. Ocrelizumab in relapsing–remitting multiple sclerosis: a phase 2, randomised, placebo-controlled, multicentre trial. Lancet. 2011;378:1779–87.
Barun B, Bar-Or A. Treatment of multiple sclerosis with anti-CD20 antibodies. Clin Immunol. 2012;142:31–7.
Aspen_Global. Azathioprine (Imuran) summary of product characteristics, 2012.
Elion GB. The George Hitchings and Gertrude Elion Lecture. The pharmacology of azathioprine. Ann N Y Acad Sci. 1993;685:400–7.
La Mantia L, Mascoli N, Milanese C. Azathioprine. Safety profile in multiple sclerosis patients. Neurol Sci. 2007;28:299–303.
Baxter. Cyclophosphamide summary of product characteristics, 2003.
Kovarsky J. Clinical pharmacology and toxicology of cyclophosphamide: emphasis on use in rheumatic diseases. Semin Arthritis Rheum. 1983;12:359–72.
Lutsiak ME, Semnani RT, De Pascalis R, et al. Inhibition of CD4(+)25+ T regulatory cell function implicated in enhanced immune response by low-dose cyclophosphamide. Blood. 2005;105:2862–8.
Weiner HL, Cohen JA. Treatment of multiple sclerosis with cyclophosphamide: critical review of clinical and immunologic effects. Mult Scler. 2002;8:142–54.
Hospira. Methotrexate summary of product characteristics, 1987.
Bender RA, Makula DM. Effect of interaction between methotrexate and dihydrofolate reductase on DNA synthesis in L1210 cells in vitro. Br J Cancer. 1978;37:403–10.
Johnston A, Gudjonsson JE, Sigmundsdottir H, et al. The anti-inflammatory action of methotrexate is not mediated by lymphocyte apoptosis, but by the suppression of activation and adhesion molecules. Clin Immunol. 2005;114:154–63.
Spurlock CF 3rd, Aune ZT, Tossberg JT, et al. Increased sensitivity to apoptosis induced by methotrexate is mediated by JNK. Arthritis Rheum. 2011;63:2606–16.
Serraj K, Federici L, Maloisel F, et al. Pancytopenia related to low-dose methotrexate: study of five cases and review of the literature. Rev Med Interne. 2007;28:584–8.
Roche. CellCept (mycophenolate mofetil) label, FDA approved, 2009.
Allison AC, Kowalski WJ, Muller CD, et al. Mechanisms of action of mycophenolic acid. Ann N Y Acad Sci. 1993;696:63–87.
Ritter ML, Pirofski L. Mycophenolate mofetil: effects on cellular immune subsets, infectious complications, and antimicrobial activity. Transpl Infect Dis. 2009;11:290–7.
Michel L, Vukusic S, De Seze J, et al. Mycophenolate mofetil in multiple sclerosis: a multicentre retrospective study on 344 patients. J Neurol Neurosurg Psychiatry. 2014;85:279–83.
Acknowledgments
Editorial support (assistance in drafting and editing of the manuscript text, figures, and tables, as directed by authors, data checking and incorporation of comments from reviewers, and assisting with the submission process) provided by V Lawson at Fishawack Communications Ltd, funded by Genzyme, a Sanofi company. This was the only funding provided for the development of this manuscript.
Disclosures and Conflicts of Interest
ABO has participated as a speaker at meetings sponsored by, received consulting fees and/or received grant support from: Amplimmune, Bayhill Therapeutics, Berlex/Bayer, Biogen Idec, BioMS, Diogenix, Eli-Lilly, Genentech, Genzyme, GlaxoSmithKline, Guthy-Jackson/GGF, Merck/EMD Serono, Medimmune, Mitsubishi Pharma, Novartis, Ono Pharma, Receptos, Roche, Sanofi, Teva Neuroscience, Wyeth. AP has received research support, consulting fees, and support for research-related travel from Sanofi/Genzyme. FMV is an employee of Sanofi. JK is an employee of Genzyme, a Sanofi company. HW has received honoraria and consulting fees from Bayer Healthcare, Biogen Idec, Fresenius Medical Care, GlaxoSmithKline, Genzyme, Merck Serono, EMD Serono, Novartis Pharma, Sanofi-Aventis, and Teva Pharma, and grants from Bayer Healthcare, Biogen Idec, The German Ministry for Education and Research (BHBF), Deutsche Forschungsgemeinschaft (DFG), Else Kroener-Fresenius-Stiftung, Fresenius Foundation, Genzyme, Hertie Foundation, Merck Serono, Novartis, NRW Ministry of Education and Research, Interdisciplinary Center for Clinical Research (IZKF) Muenster, RE children’s foundation, Sanofi-Aventis, and Teva Pharma.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Bar-Or, A., Pachner, A., Menguy-Vacheron, F. et al. Teriflunomide and Its Mechanism of Action in Multiple Sclerosis. Drugs 74, 659–674 (2014). https://doi.org/10.1007/s40265-014-0212-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-014-0212-x