Abstract
Introduction
Adverse drug reactions (ADRs) are common among people with dementia; however, little is known about the magnitude and predictors associated with ADR-related hospitalisation among these individuals. This study aimed to determine the magnitude, types, drugs implicated and predictors of ADRs associated with hospitalisation among people with dementia.
Methods
This retrospective case-control study analysed medical records of individuals aged ≥ 65 years with dementia admitted to major public hospitals in Tasmania, Australia, from July 2010 to July 2021. Adverse drug reactions and implicated drugs were identified using administrative data and cross-checked with hospital medical records, with consensus reached among the research team.
Results
Of the 7928 people admitted to hospital at least once within the study period, 1876 (23.7%) experienced at least one ADR-related hospitalisation. Of these, 300 case patients with 311 ADRs and 300 control patients were randomly selected. The most common types of ADRs were renal (acute kidney injury; AKI) (36.0%), followed by neuropsychiatric (17.6%), cardiovascular (16.0%) and haematological (13.1%). Diuretics, renin-angiotensin system (RAS) inhibitors and anti-thrombotics constituted the main implicated drug classes. The ADR-related hospitalisation was associated with: chronic kidney disease (CKD) (OR 8.00, 95% CI 2.63–24.28, p < 0.001), Australian-born (OR 1.62, 95% CI 1.08–2.43, p = 0.019), hypertension (OR 1.48, 95% CI 1.01–2.17, p = 0.044) and the number of medicines (OR 1.06, 95% CI 1.00–1.12, p = 0.022). Potentially inappropriate medication use and anticholinergic burden did not predict ADR-related hospitalisation.
Conclusions
These predictors could help identify the individuals at the highest risk and enable targeted interventions to be designed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In total, 23.7% of hospitalised people with dementia experienced at least one ADR-related hospitalisation during the study period. |
The most common type of ADR was acute kidney injury, while diuretics and renin-angiotensin system inhibitors constituted the main drug classes associated with ADR-related hospitalisations. |
Four predictors independently associated with ADR-related hospitalisation were chronic kidney disease, Australian-born, hypertension and the number of medicines. |
1 Introduction
An adverse drug reaction (ADR) is defined by the World Health Organization (WHO) as “any response to a drug which is noxious and unintended, and which occurs at doses normally used in man for prophylaxis, diagnosis or therapy of disease, or for the modification of physiological function” [1]. Adverse drug reactions represent a significant clinical challenge, as they can lead to important adverse outcomes, including higher rates of morbidity and mortality, extended hospitalisation, and increased health care expenditures [2]. An Australian study found that ADRs were responsible for 18.9% of unplanned admissions to medical wards among elderly patients [3]. A systematic review reported that ADR-related hospitalisations had a median prevalence rate of 6.0% of all admissions [4].
The ageing population results in an exponential increase in the incidence of neurodegenerative disorders, such as dementia [5]. The global number of individuals living with dementia is expected to rise significantly from 57 million in 2019 to 153 million by 2050 [6]. The Australian Institute of Health and Welfare (AIHW) estimated that in 2022, there were around 401,300 individuals living with dementia in Australia, where dementia also ranks as the second leading cause of death [7]. Similarly, in 2023 it was estimated that there were more than 10,300 people living with all forms of dementia in Tasmania [8]. Impaired cognition, possible reduction in adherence, age, polypharmacy and increased sensitivity to drugs with anticholinergic properties make people with dementia more prone to ADRs [9]. Evidence suggests that ADRs are common among people with dementia [10], but the predictors of ADR-related hospitalisation in these individuals have not been captured. Such information is crucial to address any modifiable predictors causing hospitalisation. Developing strategies to reduce ADR-related hospitalisation is dependent on determining the nature of ADRs, drugs most frequently implicated and the clinical impact of ADRs. Multiple studies have identified several predictors of ADRs causing hospitalisation among general population [4, 11]; however, medical practitioners may lack awareness of factors predicting ADRs leading to hospitalisation among people with dementia. Hence, this research aimed to determine the magnitude, types, drugs implicated and potential predictors of ADRs associated with hospitalisation among people with dementia.
2 Methods
2.1 Study Design and Setting
This study used a retrospective case-control design, from the population of Tasmania, an Australian state with a population of 558,000 [12]. The data for the study were retrospectively collected from the four major public hospitals. This study was reported following the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) checklist for case-control studies (Supplementary Table ST1 of the Electronic Supplementary Material [ESM]).
2.2 Dataset
For this study, the Admitted Patient Care National Minimum Dataset (APC-NMDS) [13] and Digital Medical Records (DMR) were utilised to obtain patient information. The APC-NMDS is a collection of coded clinical and administrative data elements from Australian public hospitals, that includes summary information about each patient’s sociodemographic characteristics, principal diagnosis, and any additional diagnoses associated with their admission, based on the International Statistical Classification of Diseases and Related Health Problems, tenth edition, Australian Modification (ICD-10-AM) [13]. The DMR contains scanned copies of all documents related to a patient’s episode of care in a public hospital. It contains a detailed record of sociodemographic characteristics, primary and secondary diagnoses, comorbidities, medication history, and laboratory data.
2.3 Study Population and Admissions
The study population comprised people aged ≥ 65 years who had a medical admission to one of the four major Tasmanian public hospitals between July 2010 and July 2021, with a primary or secondary diagnosis of dementia, based on ICD-10-AM. The study sample consisted of two groups (i) cases: a randomly selected subset of 300 patients from the APC-NMDS who had at least one ADR-related admission during the study period, and (ii) controls: another randomly selected group of 300 patients from the APC-NMDS with no admission codes related to ADRs, i.e., the control group included patients with dementia not admitted with an ADR (patients admitted for other medical reasons) during the study period.
We used a two-step process in identifying the ADRs and implicated drugs, through the external cause codes and diagnostic codes in the APC-NMDS, followed by cross-checking and verifying the ADRs and implicated drugs using the information provided in the DMR. An ICD-10-AM external cause code between Y40 and Y59 was recorded in the APC-NMDS as a diagnosis associated with the hospitalisation. These codes align with the WHO’s ADR definition and are commonly used for ADR identification [14, 15]. The diagnostic codes (Du et al. codes) mainly refer to drug-induced symptoms or conditions without explicitly specifying the external cause of the ADR [16]. Code categories A1, A2, C and D were included, where A1: The ICD-10 code description includes the phrase ‘induced by medication/drug’, A2: The ICD-10 code description includes the phrase ‘induced by medication or other causes’, C: Adverse drug event deemed to be very likely although the ICD-10 code description does not refer to a drug, and D: Adverse drug event deemed to be likely although the ICD-10 code description does not refer to a drug. Patients coded with C and D code categories were said to have ADR-related hospitalisations when the association between the ADR and drug was stated in the DMR. The admission was not classified as ADR-related if the ADR occurred during the hospital stay. Each patient’s first ADR admission during the study period was defined as their index admission. The primary researcher (ASZ) independently reviewed all cases of suspected ADRs and cases without suspected ADRs for the presence of ADRs. If any uncertainty existed when identifying an ADR and associated drug (for the reasons outlined in Supplementary Figure SF1 of the ESM), a meeting of the research team was held to reach a consensus.
2.4 Sample Size Calculation for Identifying the Predictors of ADR-related Hospitalisations
The sample size calculation was based on the guidelines for multiple logistic regression by Peduzzi et al [17]. A rate of 0.235 (23.5%) was assumed for positive cases; our previous study investigating the trends in the incidence of ADR-related hospitalisations among people with dementia showed that 23.5% of hospitalised people experienced at least one ADR-related hospitalisation over a 10-year period [18]. An estimated 7 independent variables were included in the analysis. The minimum sample size was approximately 300 people. We doubled this number to 600 patients to ensure ample power, and any dropouts (missing or unclear information) were replaced.
2.5 Sampling Strategy
A random sampling strategy was used for recruiting the cases and controls. The patients were assigned a study ID number, and for each case, one control was randomly selected, using a web-based random number generator programme [19]. Controls were not matched with cases based on clinical characteristics such as age and sex. This decision was made for two primary reasons: first, matching variables would hinder the assessment of these variables’ impact on the outcome; second, matching has the potential to introduce bias in case-control study designs [20].
2.6 Definitions and Measures
2.6.1 Potentially Inappropriate Medication
Potentially inappropriate medications (PIMs) are drugs that carry a high risk of causing harm to patients and should be avoided in an individual due to the health risks outweighing the clinical benefits [21]. These medications may be inappropriate due to factors such as a lack of efficacy, the potential for ADRs or interactions, or the availability of safer alternatives. Given that the patients were elderly and had dementia, the use of PIMs was identified using the STOPPFrail criteria [22].
2.6.2 Drug-Drug Interactions
The Lexicomp® (Wolters Kluwer Health Inc. Riverwoods, IL, USA) database system was used to identify potential drug-drug interactions (DDIs), which are classified into five types (A, B, C, D, X) based on their level of clinical significance. Only the most severe DDIs (X) on admission were considered for this study.
2.6.3 Anticholinergic Burden
Anticholinergic drug burden is defined as the cumulative effect of drugs with anticholinergic activity that a patient is taking [23]. The Anticholinergic Cognitive Burden (ACB) Scale was utilised to ascertain the anticholinergic burden on admission in each patient [24].
2.6.4 Charlson Co-Morbidity Index
The Charlson Co-Morbidity Index (CCI) comprises 19 medical conditions that are weighted with scores ranging from 1–6, resulting in a total score range of 0–37 [25]. A pre-validated age-adjusted Microsoft Excel spreadsheet was utilised to compute the score for each patient [25].
2.6.5 Postcode
The residential postcode of the patient was used to determine the following.
a. Rurality
The Australian Bureau of Statistics Accessibility/Remoteness Index of Australia plus (ARIA+ 2016) was employed to determine the geographic location [26]. The ARIA+ classifies geographic regions into five groups: major cities, inner regional, outer regional, remote and very remote Australia. However, in Tasmania, no regions are classified as major cities based on ARIA+ 2016 [26]. Consequently, postcodes were reassigned to inner regional, outer regional, and remote/very remote Australia. The University of Sydney ARIA Lookup tool was used to generate ARIA+ classifications [27], and areas with multiple classifications were identified using the ARIA+ 2016 demonstration map [28].
b. Socio-economic status
We utilised the Socio-economic Indexes for Areas-Index of Relative Socio-economic Advantage and Disadvantage (SEIFA-IRSAD) based on the 2016 census data from the Australian Bureau of Statistics to ascertain the socio-economic status of each patient [29]. The SEIFA-IRSAD offers a concise summary of various census variables that pertain to the relative socio-economic disadvantage and/or advantage of geographical regions in Australia. These indices are assigned deciles (1 to 10) based on the patient’s residential postcode, with decile 1 representing the most socio-economically disadvantaged region and decile 10 representing the most socio-economically advantaged. We grouped these deciles into three categories: 1–3 (low socio-economic class), 4–6 (middle socio-economic class), and 7–10 (high socio-economic class) in order to achieve an approximately equal distribution of the study sample across the three groups.
2.7 Statistical Analysis
Statistical Package for Social Sciences (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, version 28.0. Armonk, NY, USA: IBM Corp.) and Microsoft Office Excel 2019 were used for data analysis. Variables were checked for normality of distribution via visual inspection of histograms. Normally distributed continuous variables were reported as mean ± standard deviation (SD), and non-normally distributed variables as median (interquartile range [IQR]). Frequency (percentage) was used to report proportions and categorical variables. A chi-square test/Student’s t-test/ANOVA/Mann-Whitney U test/Kruskal Wallis test was applied, as appropriate, to make comparisons between groups. Multiple logistic regression analysis was used to determine the predictors of ADR-related hospitalisation. A p-value < 0.05 was considered statistically significant. The collinearity was determined through collinearity diagnostics, and variables with a high variance inflation factor (VIF) (≥ 5) were excluded from the model.
3 Results
Of the 7928 people admitted to hospital at least once within the study period with a primary or secondary diagnosis of dementia, 1876 (23.7%) experienced at least one ADR-related hospitalisation. Of these 1876 people, 300 patients were randomly selected as cases, while 300 patients were randomly selected as controls from the rest of the study population. The numbers of pre-existing chronic conditions and regular medicines upon presentation, and the ACB score were significantly greater for the ADR-related admission group, as detailed in Table 1. The proportion of Australian-born individuals was significantly greater among people with ADR-related admissions, and the estimated glomerular filtration rate (eGFR) at presentation was significantly lower among people with ADR-related admissions. Nevertheless, the assessment of eGFR at the time of presentation was determined to be an unreliable measure for further analysis because the lower eGFR values observed were probably influenced by the presence of renal ADRs among individuals who had experienced ADR-related hospital admissions. Common comorbid conditions, including hypertension, diabetes, chronic kidney disease (CKD), ischaemic heart disease and cerebrovascular disease, were more prevalent in ADR-related admissions.
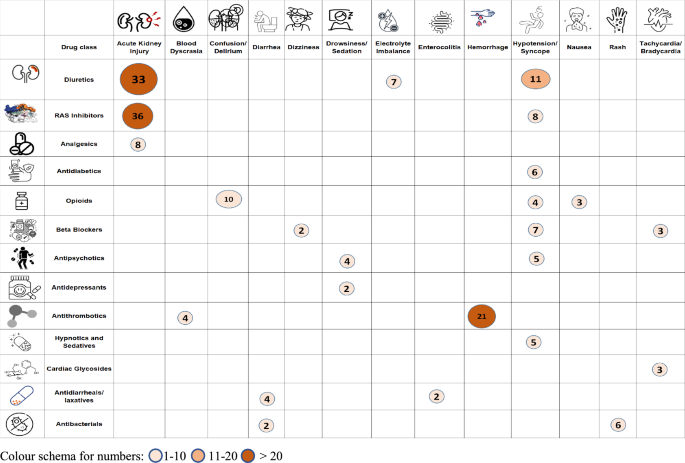
A total of 311 ADRs was identified among 300 patients with ADR-related hospitalisations. Table 2 and Fig. 1 represents the most common ADRs and the implicated drugs/drug class(es). The most common type of ADRs were renal (acute kidney injury; AKI) (36.0%), followed by neuropsychiatric (17.6%), cardiovascular (16.0%) and haematological (13.1%). A detailed description of the types of ADR causing or contributing to hospitalisations among people with dementia is given in Supplementary Table ST2 of the ESM. Of the total 2487 drugs being taken by the 300 patients with ADR-related hospitalisations, 399 drugs were implicated in the 311 ADRs. Diuretics, renin-angiotensin system (RAS) inhibitors and anti-thrombotics comprised the main drug classes implicated in ADR-related hospitalisations (Supplementary Table ST3 of the ESM).
The median number of PIMs, DDIs and anticholinergic burden score among cases and controls was 1 (IQR for cases = 1–2; IQR for controls = 0–2, respectively), 0 and 1 (IQR of 1–3 for cases and 0–2 for controls), respectively. The detailed prevalence of PIMs, DDIs and anticholinergic burden among cases and controls is given in Supplementary Tables ST4-ST7 of the ESM.
Logistic regression was used to identify the predictors of ADR-related hospitalisation (Table 3). Four predictors were identified to be independently associated with ADR-related hospitalisation: CKD (odds ratio [OR] 8.00, 95% confidence interval [CI] 2.63–24.28, p < 0.001), Australian-born (OR 1.62, 95% CI 1.08–2.43, p = 0.019), hypertension (OR 1.48, 95% CI 1.01–2.17, p = 0.044) and the number of medicines (OR 1.06, 95% CI 1.00–1.12, p = 0.022).
4 Discussion
Our study provides valuable insights into the burden of ADR-related admissions on the health system and the patients in its care. Nearly one-quarter of those admitted to hospital at least once within the study period with a primary or secondary diagnosis of dementia, experienced at least one ADR-related hospitalisation. Older people with dementia often require multiple drugs to treat cognitive difficulties, manage behavioural and neuropsychiatric symptoms, and treat various coexisting conditions [30]. Consequently, polypharmacy is common among people with dementia [31]. In addition to the physiological changes associated with aging that alter the activity and metabolism of drugs, individuals with dementia exhibit increased sensitivity to the cognitive effects of medications [32]. Additionally, these individuals are frequently excluded from clinical trials and observational studies, resulting in a significant scarcity of high-quality data. Therefore, the lack of substantial evidence impedes the capacity to establish precise guidelines for appropriate prescribing practices [33]. All of these factors collectively contribute to a substantial increase in the risk of ADRs among individuals with dementia.
Identifying the nature of ADRs, implicated drugs and predictors of ADR-related hospitalisations among people with dementia is crucial for developing strategies to reduce harm in this cohort. Our study showed that the most common ADR was AKI associated with RAS inhibitors and diuretics. Similar findings have been reported from studies conducted among the older population [34,35,36]. Most people with dementia are elderly with chronic medical conditions such as CKD, diabetes mellitus, heart failure and cancer, who regularly take medications and are at increased risk of AKI [37]. Additionally, AKI can be exacerbated by dehydration, which is a common issue among individuals with dementia, who may lose their ability to recognise thirst [38]. To address these concerns, it is essential for patients with dementia to receive regular renal function tests and primary care reviews. During these reviews, health care professionals should engage with caregivers to discuss the risk of AKI resulting from the patients’ diminished capacity for self-care, particularly in regulating fluid intake when unwell [37].
Neuropsychiatric ADRs, including confusion and delirium, were the second most common type of ADRs among people with dementia. While long-term treatment with some CNS-acting medications may be necessary for individuals with dementia, there is abundant evidence indicating that benzodiazepines, opioids, and antipsychotics may be excessively or inappropriately used in this population [39]. Opioid-induced neurotoxicity is a complex syndrome that can manifest a range of symptoms, from mild confusion and drowsiness to more severe symptoms, such as hallucinations, delirium, and seizures [40]. Older adults, especially those with pre-existing cognitive impairment, are at a greater risk of developing confusion and delirium as a result of opioid use [41].
Cardiovascular ADRs are frequently reported in the literature [11, 42]. This is due to a combination of drug and patient-related factors, including the impact of heart disease on drug pharmacokinetics, which can lead to reduced volume distribution and clearance in patients with congestive heart failure [44, 45]. Individuals with dementia may experience amplified age-related changes, further increasing the risk of cardiovascular ADRs.
Haematological complaints were the fourth most common ADRs identified. Around 20% of elderly individuals with dementia are estimated to experience atrial fibrillation (AF) [43]. People with dementia are prescribed anticoagulants or aspirin to prevent stroke in patients with AF [44]. However, individuals with advanced dementia and AF receive limited clinical benefit in terms of life prolongation from anticoagulation therapy, accompanied by an increased risk of bleeding [43]. It is crucial to regularly review the need for anti-thrombotics and deprescribe according to treatment goals.
Understanding the factors that predispose people with dementia to ADRs is crucial in developing effective preventive measures. Furthermore, enhancing prescriber education by emphasising the identification of predictors for ADRs and the significance of conducting risk-benefit assessments prior to prescribing any medication is imperative for enhancing the safety of pharmacological treatments for individuals with dementia. Our study identified the presence of CKD, being Australian-born, having hypertension and the number of medications as the predictors of ADR-related hospitalisations among people with dementia.
Patients with pre-existing renal disease exhibited a higher likelihood of hospitalisation due to ADRs than patients with normal renal function (Supplementary Table ST8 of the ESM), as observed in previous studies [11, 45]. Acute kidney injury (the most common type of ADR) was experienced by three-quarters of the individuals with ADR-associated hospitalisations who had CKD as a comorbidity (Supplementary table ST9 of the ESM). Additionally, 49% of people with comorbid CKD were prescribed at least one of the most commonly implicated drug classes (RAS inhibitors and diuretics).
In 2021 it was estimated that 15% of the Tasmanian population were individuals who were born overseas [46]. One of the predictors of ADR-related hospitalisation was being born in Australia. The most common type of ADR (AKI) and use of commonly implicated drug classes in ADRs (diuretics, RAS inhibitors and anti-thrombotics) were predominant among Australian-born individuals (Supplementary table ST10 of the ESM). The causative reasoning behind this predictor is unclear.
Hypertension is as common in people with dementia as in other populations and is as commonly treated with antihypertensive drugs [47]. Hypertension can lead to vascular changes and compromised blood flow in the brain, which can make individuals with dementia more vulnerable to the adverse effects of medications. The impaired blood supply to the brain may exacerbate the negative impact of ADRs, potentially leading to severe symptoms and hospitalisation [47]. Moreover, approximately 70% of patients with hypertension require two or more drugs to achieve their target blood pressure [48]. The use of multiple antihypertensives in elderly patients has been identified as a frequent cause of hospital admission [49].
Patients who experienced an ADR were found to be taking significantly more medications than patients without ADRs. This is consistent with findings in other studies [50, 51]. According to estimates, individuals who take two drugs face a 13% chance of encountering an ADR. However, this risk significantly escalates to 58% and 82% when an individual takes five or seven or more drugs per day, respectively [52]. People with dementia are often subject to “prescribing cascade” [53]. There might be a greater risk of error due to more complicated regimens and also a greater chance of drug-drug and drug-disease interactions among this group of people [54]. To address these concerns and minimise the risks associated with inappropriate polypharmacy in older adults living with dementia, it is crucial to integrate medication reviews and deprescribing plans into routine care [55].
Our study showed that PIM use did not predict ADR-related hospitalisation. There is controversy regarding whether the use of PIM leads to hospital admission. Adverse drug reaction-related hospitalisation among older people can be explained by idiosyncratic response or the predisposition of these patients to develop adverse drug events, whether or not drugs are classed as PIMs [56]. Similarly, we did not demonstrate DDIs to be a predictor of ADR-related hospitalisations. In contrast to other studies conducted among the general population [57, 58], our study only considered the most severe type of DDIs. The disparity in our findings compared to other studies can be attributed to various factors, including differences in the study population, methods employed for detecting DDIs and the type of DDIs included in the study. Our study showed that anticholinergic burden was not associated with ADR-related hospitalisation. A systematic review conducted among older population also showed that the use of anticholinergic medicines was not associated with hospitalisation [59]. Anticholinergic medications can cause a wide range of side effects, including cognitive impairment, dry mouth, constipation, blurred vision, and urinary retention. However, not all of these will lead to hospital admissions.
Our study has some limitations. We relied on administrative hospital coding and hospital datasets for the identification of ADR-related hospitalisations, which might result in the underestimation of ADRs. The ADR-related admissions are detected at a much lower rate using administrative datasets. It has been estimated that only 18%–35% of ADR-related admissions captured prospectively can be identified via administrative data sources, although these rates can be affected by the ICD codes used with this methodology [41, 60]. Additionally, some ADRs such as falls/fractures might not have been documented in the hospital dataset because they are not always seen as ADR related. Second, information related to some variables (such as frailty status) that might be predictors of ADR-related hospitalisation, was missing for most patients and was not incorporated in the final analysis. Third, the assessment of ADRs was not done through any formal causality assessment tool. However, the concomitant use of an administrative dataset and hospital DMR, followed by consensus between the research team, allowed for a robust evaluation of ADRs and the implicated drugs. Finally, the ACB scale utilised in this study might not capture the full extent of the anticholinergic burden because anticholinergic load is cumulative, and over-the-counter (OTC) drugs, which may not have been included in the drug list, could potentially contribute to the overall burden.
Our study is the first to identify independent predictors of ADR-related hospitalisation among people with dementia over an extensive period of time. Tasmania is an ideal location for tracking hospital admissions over time. Its relative isolation makes it reasonable to expect that almost all eligible patients’ hospital admissions would occur within the Tasmanian health system and be captured in our dataset.
5 Conclusions
The most common type of ADR was renal (AKI), followed by neuropsychiatric, cardiovascular and haematologic. Diuretics, RAS inhibitors and anti-thrombotics constituted the drug classes most potentially implicated in causing ADR-related hospitalisation in patients with dementia. Four predictors associated with ADR-related hospitalisation were CKD, being Australian-born, hypertension and the number of medicines. These factors could help identify the individuals at the highest risk and enable targeted interventions to be designed.
References
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000;356(9237):1255–9.
Wu TY, Jen MH, Bottle A, Molokhia M, Aylin P, Bell D, et al. Ten-year trends in hospital admissions for adverse drug reactions in England 1999–2009. J R Soc Med. 2010;103(6):239–50.
Parameswaran Nair N, Chalmers L, Bereznicki BJ, Curtain C, Peterson GM, Connolly M, et al. Adverse drug reaction-related hospitalizations in elderly Australians: a prospective cross-sectional study in two Tasmanian hospitals. Drug Saf. 2017;40(7):597–606.
Angamo MT, Chalmers L, Curtain CM, Bereznicki LR. Adverse drug reaction related hospitalisations in developed and developing countries: a review of prevalence and contributing factors. Drug Saf. 2016;39(9):847–57.
Prince MJ, Wimo A, Guerchet MM, Ali GC, Wu Y-T, Prina M. World Alzheimer Report 2015-The Global Impact of Dementia: An analysis of prevalence, incidence, cost and trends. 2015.
Alzheimer's Research UK. Worldwide dementia cases to triple by 2050 to over 150 million people. 2022 [cited 2023 17 March]; Available from: https://www.alzheimersresearchuk.org/worldwide-dementia-cases-to-triple-by-2050-to-over-150-million/. Accessed 17 Mar 2023.
Australian Institute of Health and Welfare. Dementia in Australia. 2023 [cited 2023 17 March]; Available from: https://www.aihw.gov.au/reports/dementia/dementia-in-aus/contents/summary. Accessed 17 Mar 2023.
Dementia Australia. Dementia in Australia; 2023. Available from: https://www.dementia.org.au/sites/default/files/2023-03/Prevalence-Data-2023-Updates.pdf. Accessed 9 Dec 2023.
Laroche ML, Perault-Pochat MC, Ingrand I, Merle L, Kreft-Jais C, Castot-Villepelet A, et al. Adverse drug reactions in patients with Alzheimer’s disease and related dementia in France: a national multicentre cross-sectional study. Pharmacoepidemiol Drug Saf. 2013;22(9):952–60.
Zaidi AS, Peterson GM, Bereznicki LR, Curtain CM, Salahudeen M. Outcomes of medication misadventure among people with cognitive impairment or dementia: a systematic review and meta-analysis. Ann Pharmacother. 2021;55(4):530–42.
Angamo MT, Curtain CM, Chalmers L, Yilma D, Bereznicki L. Predictors of adverse drug reaction-related hospitalisation in Southwest Ethiopia: a prospective cross-sectional study. PLoS ONE. 2017;12(10): e0186631.
Australian Bureau of Statistics. Snapshot of Tasmania. 2022 [cited 2023 11 March]; Available from: https://www.abs.gov.au/articles/snapshot-tas-2021. Accessed 11 Mar 2023.
Australian Institute of Health and Welfare. Admitted patient care NMDS 2022–23. 2023 [cited 2023 11 March]; Available from: https://meteor.aihw.gov.au/content/742173. Accessed 11 Mar 2023.
Veeren JC, Weiss M. Trends in emergency hospital admissions in England due to adverse drug reactions: 2008–2015. J Pharm Health Serv Res. 2017;8(1):5–11.
Walter SR, Day RO, Gallego B, Westbrook JI. The impact of serious adverse drug reactions: a population-based study of a decade of hospital admissions in New South Wales, Australia. Br J Clin Pharmacol. 2017;83(2):416–26.
Du W, Pearson SA, Buckley NA, Day C, Banks E. Diagnosis-based and external cause-based criteria to identify adverse drug reactions in hospital ICD-coded data: application to an Australia population-based study. Public Health Res Pract. 2017;27(2):e2721716.
Long JS, Long JS. Regression models for categorical and limited dependent variables. Berlin: Sage; 1997.
Zaidi AS, Peterson GM, Bereznicki LRE, Curtain CM, Salahudeen MS. Ten-year trends in adverse drug reaction-related hospitalizations among people with dementia. Ther Adv Drug Saf. 2022;13:20420986221080796.
CalculatorSoup®. Random Number Generator. 2023 [cited 2023 3 April]; Available from: https://www.calculatorsoup.com/calculators/statistics/random-number-generator.php. Accessed 3 Apr 2023.
Rose S, Laan MJ. Why match? Investigating matched case-control study designs with causal effect estimation. Int J Biostat. 2009;5(1):1.
Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly. An update Arch Intern Med. 1997;157(14):1531–6.
Lavan AH, Gallagher P, Parsons C, O’Mahony D. STOPPFrail (Screening Tool of Older Persons Prescriptions in Frail adults with limited life expectancy): consensus validation. Age Ageing. 2017;46(4):600–7.
Salahudeen MS, Duffull SB, Nishtala PS. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr. 2015;15(1):31.
Campbell NL, Maidment I, Fox C, Khan B, Boustani M. The 2012 Update to the Anticholinergic Cognitive Burden Scale. J Am Geriatr Soc. 2013;61(S1):S142–3.
Hall WH, Ramachandran R, Narayan S, Jani AB, Vijayakumar S. An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer. 2004;20(4):94.
Glover JD, Tennant SK. Remote areas statistical geography in Australia: notes on the Accessibility/Remoteness Index for Australia (ARIA+ version): Public Health Information Development Unit, the University of Adelaide; 2003.
The University of Sydney. Aria lookup tool. 2023 [cited 2023 9 March]; Available from: https://www.pocog.org.au/aria/default.aspx. Accessed 9 Mar 2023.
The University of Adelaide. ARIA+ 2016 Demonstration Map. [cited 2023 11 March]; Available from: https://services.spatial.adelaide.edu.au/giscaportal/apps/webappviewer/index.html?id=417801ba9b844792af44ea4f766a3e30. Accessed 11 Mar 2023.
Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2016. 2018 [cited 2023 8 March]; Available from: https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012016?OpenDocument. Accessed 8 Mar 2023.
Eshetie TC, Nguyen TA, Gillam MH, Kalisch Ellett LM. A narrative review of problems with medicines use in people with dementia. Expert Opin Drug Saf. 2018;17(8):825–36.
Parsons C. Polypharmacy and inappropriate medication use in patients with dementia: an underresearched problem. Ther Adv Drug Saf. 2017;8(1):31–46.
Bishara D, Harwood D. Safe prescribing of physical health medication in patients with dementia. Int J Geriatr Psychiatry. 2014;29(12):1230–41.
Rollin-Sillaire A, Breuilh L, Salleron J, Bombois S, Cassagnaud P, Deramecourt V, et al. Reasons that prevent the inclusion of Alzheimer’s disease patients in clinical trials. Br J Clin Pharmacol. 2013;75(4):1089–97.
Pedrós C, Formiga F, Corbella X, Arnau JM. Adverse drug reactions leading to urgent hospital admission in an elderly population: prevalence and main features. Eur J Clin Pharmacol. 2016;72:219–26.
Schmiedl S, Rottenkolber M, Szymanski J, Drewelow B, Siegmund W, Hippius M, et al. Preventable ADRs leading to hospitalization—results of a long-term prospective safety study with 6,427 ADR cases focusing on elderly patients. Expert Opin Drug Saf. 2018;17(2):125–37.
Jennings EL, Murphy KD, Gallagher P, O’Mahony D. In-hospital adverse drug reactions in older adults; prevalence, presentation and associated drugs—a systematic review and meta-analysis. Age Ageing. 2020;49(6):948–58.
UK Renal Registry. Guidance for mental health professionals on the management of acute kidney injury; 2016. Available from: https://www.thinkkidneys.nhs.uk/aki/wp-content/uploads/sites/2/2018/01/Guidance-for-mental-health-patients-2018.pdf. Accessed 12 May 2023.
Beales A. An innovative approach to hydration for a patient with dementia. Nurs Older People. 2017;29(4):26–9.
Meeks TW, Culberson JW, Horton MS. Medications in long-term care: when less is more. Clin Geriatr Med. 2011;27(2):171–91.
Matzo M, Dawson KA. Opioid-induced neurotoxicity. Am J Nurs. 2013;113(10):51–6.
Parameswaran Nair N, Chalmers L, Peterson GM, Bereznicki BJ, Curtain CM, Bereznicki LR. Prospective identification versus administrative coding of adverse drug reaction-related hospitalizations in the elderly: a comparative analysis. Pharmacoepidemiol Drug Saf. 2018;27(11):1281–5.
Conforti A, Costantini D, Zanetti F, Moretti U, Grezzana M, Leone R. Adverse drug reactions in older patients: an Italian observational prospective hospital study. Drug Healthc Patient Saf. 2012;4:75–80.
Ouellet GM, O’Leary JR, Leggett CG, Skinner J, Tinetti ME, Cohen AB. Benefits and harms of oral anticoagulants for atrial fibrillation in nursing home residents with advanced dementia. J Am Geriatr Soc. 2023;71(2):561–8.
Subic A, Cermakova P, Religa D, Han S, von Euler M, Kåreholt I, et al. Treatment of atrial fibrillation in patients with dementia: A cohort study from the Swedish Dementia Registry. J Alzheimers Dis. 2018;61(3):1119–28.
Caamaño F, Pedone C, Zuccalà G, Carbonin P. Socio-demographic factors related to the prevalence of adverse drug reaction at hospital admission in an elderly population. Arch Gerontol Geriatr. 2005;40(1):45–52.
tasmania Ph. Primary health tasmania, health needs assessment 2022–23 to 2024–2; 2022. Available from: https://www.primaryhealthtas.com.au/wp-content/uploads/2023/05/Health-in-Tasmania-Comprehensive-Needs-Assessment-2022-25.pdf. Accessed 17 Mar 2024.
Welsh TJ, Gladman JR, Gordon AL. The treatment of hypertension in people with dementia: a systematic review of observational studies. BMC Geriatr. 2014;14(1):19.
Guerrero-Garcia C, Rubio-Guerra AF. Combination therapy in the treatment of hypertension. Drugs Context. 2018;7: 212531.
Parameswaran Nair N, Chalmers L, Connolly M, Bereznicki BJ, Peterson GM, Curtain C, et al. Prediction of hospitalization due to adverse drug reactions in elderly community-dwelling patients (the PADR-EC score). PLoS ONE. 2016;11(10): e0165757.
Davies EC, Green CF, Taylor S, Williamson PR, Mottram DR, Pirmohamed M. Adverse drug reactions in hospital in-patients: a prospective analysis of 3695 patient-episodes. PLoS ONE. 2009;4(2): e4439.
Osanlou R, Walker L, Hughes DA, Burnside G, Pirmohamed M. Adverse drug reactions, multimorbidity and polypharmacy: a prospective analysis of 1 month of medical admissions. BMJ Open. 2022;12(7): e055551.
Zazzara MB, Palmer K, Vetrano DL, Carfi A, Onder G. Adverse drug reactions in older adults: a narrative review of the literature. Eur Geriatr Med. 2021;12(3):463–73.
Trenaman SC, Bowles SK, Kirkland S, Andrew MK. An examination of three prescribing cascades in a cohort of older adults with dementia. BMC Geriatr. 2021;21(1):297.
Pfister B, Jonsson J, Gustafsson M. Drug-related problems and medication reviews among old people with dementia. Bmc Pharmacol Toxico. 2017;18(1):52.
Sawan MJ, Moga DC, Ma MJ, Ng JC, Johnell K, Gnjidic D. The value of deprescribing in older adults with dementia: a narrative review. Expert Rev Clin Pharmacol. 2021;14(11):1367–82.
Varallo FR, Capucho HC, Planeta CdS, Mastroianni PdC. Safety assessment of potentially inappropriate medications (PIM) use in older people and the factors associated with hospital admission. J Pharm Pharm Sci. 2011;14(2):283–90.
Dechanont S, Maphanta S, Butthum B, Kongkaew C. Hospital admissions/visits associated with drug–drug interactions: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2014;23(5):489–97.
Ayalew MB, Tegegn HG, Abdela OA. Drug related hospital admissions; a systematic review of the recent literatures. Bull Emerg Trauma. 2019;7(4):339.
Cardwell K, Hughes CM, Ryan C. The association between anticholinergic medication burden and health related outcomes in the ‘oldest old’: a systematic review of the literature. Drugs Aging. 2015;32:835–48.
Hohl CM, Kuramoto L, Yu E, Rogula B, Stausberg J, Sobolev B. Evaluating adverse drug event reporting in administrative data from emergency departments: a validation study. BMC Health Serv Res. 2013;13(1):473.
Acknowledgements
ASZ gratefully acknowledges the material and financial support of the University of Tasmania in the form of a Tasmania Graduate Research Scholarship
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Approval
The study was conducted with approval from the Tasmanian Health and Medical Human Research Ethics Committee (reference number H0018582).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
The data utilised in this analysis were sourced from a third party, namely the Tasmanian Department of Health and Human Services. It is important to note that these data are not publicly accessible in Australia, and the research team has not been granted permission to make them publicly available. To access the data, necessary ethics approvals must be obtained. Upon securing these approvals, the research team will be able to request access to the data in writing by contacting: The Secretary, Department of Health, GPO Box 125, Hobart, Tasmania, 7001, Australia.
Code Availability
The code of this study is available from the corresponding author upon reasonable request.
Author Contributions
Anum Saqib Zaidi: Conceptualisation; Methodology; Formal analysis; Writing – original draft. Gregory M. Peterson: Conceptualisation; Methodology; Investigation; Supervision; Visualization; Writing—review & editing. Colin M. Curtain: Conceptualisation; Methodology; Investigation; Supervision; Writing—review & editing. Mohammed S. Salahudeen: Conceptualisation; Methodology; Investigation; Supervision; Writing—review & editing. All authors read and approved the final version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zaidi, A.S., Peterson, G.M., Curtain, C.M. et al. Predictors of Adverse Drug Reaction-Related Hospitalisations Among People with Dementia: A Retrospective Case-Control Study. Drug Saf 47, 771–781 (2024). https://doi.org/10.1007/s40264-024-01435-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-024-01435-3