Abstract
Introduction
Opioid prescribing rates are continuing to increase in Australia in line with prescribing rates seen internationally. Prescribing limits are one policy strategy to reduce short-term opioid prescribing, but there is limited evidence of their impact.
Objective
The aim of this study was to assess the impact of state and national policy interventions on changes to oxycodone 5 mg discharge prescriptions in public hospitals using electronic prescribing in Queensland, Australia by evaluating the proportion of oxycodone 5 mg discharge prescriptions written for ≤ 10 tablets across the study period.
Method
This research utilised a retrospective uncontrolled interrupted time-series design and was undertaken at 12 public hospitals using electronic prescribing from December 2018 to February 2021. The study analysed the impact of two sequential policy interventions that limited the recommended quantity of oxycodone 5 mg on discharge for all hospitalised patients. The first state-wide policy came into effect on 19 September 2019 and the second national policy came into effect on 1 June 2020.
Results
Over the 27-month period, there were 110,728 discharge prescriptions written in the 12 Queensland hospitals for oxycodone 5 mg. During the baseline period, approximately 50.7% (95% CI 49.5–51.8) of all oxycodone 5 mg prescriptions were from tablet quantities of ≤ 10 tablets. After the implementation of the state-wide policy, the proportion increased by 9% (95% CI 7.4–10.7; p = 0.001). The implementation of the national policy increased the proportion of oxycodone 5 mg prescriptions written for ≤10 tablets by 9.8% (95% CI 8.1–11.5; p < 0.001).
Conclusions
Restrictive prescribing policies at a state and national level may have resulted in decreased quantities of oxycodone 5 mg prescriptions provided on discharge from public hospitals using electronic prescribing in Queensland, Australia. Despite these positive results, continued multi-faceted policy efforts and individual tailored interventions are necessary to ensure safe and judicious opioid prescribing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The increase in opioid use is associated with parallel increases in opioid-related morbidity and mortality, including dependence and overdose. Opioids initiated in hospital, most often for acute pain management, have been identified as one key risk element over which physicians have influence. |
Restrictive prescribing policies at a state and national level resulted in decreased quantities of oxycodone 5 mg prescriptions provided on discharge from public health electronic prescribing hospitals in Queensland Australia. |
These results are informative for countries and hospitals on the meaningful impact that quantity restrictions in institutional, state, and national health care policy can have. |
1 Introduction
Opioid prescribing rates are continuing to increase in Australia in line with prescribing rates seen internationally [1,2,3]. Rates of opioid use in Australia have remained high since 2013; each year over 1.9 million adults are estimated to initiate opioids and over 3 million adults are using opioids in Australia [4]. In 2016–17, the most dispensed opioid was oxycodone with 5.7 million prescriptions dispensed to 1.3 million people [3]. The increase in opioid use is associated with parallel increases in opioid-related morbidity and mortality, including dependence and overdose [5, 6]. Morbidity and mortality from prescription opioids is a public health crisis in Australia as well as multiple other nations, and impacts nearly every level of the healthcare system [2, 3]. The ongoing opioid-overdose epidemic remains unabated with pharmaceutical opioids the most commonly identified substances in drug-induced death in Australia for over two decades [6]. The staggering increase in opioid misuse, opioid use disorder diagnoses, and overdose fatalities in the past two decades has yielded an urgent need to understand the most effective public health interventions for addressing opioid-related harms [7].
Elements of opioid prescribing associated with an increased risk of complications include excessive initial days’ supply, high doses, concurrent prescribing of opioids and sedatives, and long-term prescribing [8,9,10,11]. Hospital-initiated opioids, most often for acute pain management, have been identified as a key risk for ongoing and inappropriate use [8, 9]. Accumulating observational evidence suggests that therapeutic exposure to opioids is associated with increased likelihood of long-term use and that greater duration or intensity of initial opioid prescriptions may further elevate risk [10,11,12]. A US study [13] highlighted the high-risk characteristics of initial opioid prescribing patterns associated with long-term use and in turn higher risk of hospitalisation. They found that 5% of opioid-naïve patients became long-term users, defined as six or more opioid prescriptions in the 12 months following the initiation month [13], which is consistent with other studies’ estimates of 5–6% [14, 15]. A recent study in Australia, using group-based trajectory modelling to define persistent use, found that 2.6% of adults initiating opioids became persistent users over a 12-month period [16]. Further research suggests concerns regarding the appropriateness and number of opioid prescriptions written on discharge [8, 9].
Interventions to improve opioid prescribing behaviours remain a priority through stewardship principles, policy, and legislation [17]. Over the past decade, the Australian medicine and therapeutic regulatory agency, Therapeutic Goods Administration (TGA), implemented a number of regulatory policy reforms to reduce harm from opioid analgesics by reducing pack sizes, and improving prescribing information and Consumer Medicines Information [18]. In August 2019, the Queensland Health Medicines Advisory Committee (QHMAC) implemented a pragmatic approach to tailor opioid prescribing by restricting oxycodone 5-mg tablets to a maximum quantity of 10 tablets for discharge and outpatient use [19]. The Australian Pharmaceutical Benefits Advisory Committee (PBAC) recommends the medicines to be incorporated in the government subsidised medicines scheme (the Pharmaceutical Benefits Scheme [PBS]). In June 2020, PBAC enacted a policy reform to reduce the PBS quantity of oxycodone 5-mg tablets from 20 tablets to 10 tablets [20]. This policy initiative led to a nudge within the Queensland Health electronic prescribing software with the default quantity of 20 tablets reduced to 10 tablets for oxycodone 5 mg discharge prescriptions.
Prescribing limits are one policy strategy to reduce short-term opioid prescribing, but there is limited evidence of their impact. This study aims to evaluate the impact of two sequential state and national policy interventions on changes to oxycodone 5 mg discharge prescriptions in public health electronic prescribing hospitals in Queensland. This uncontrolled interrupted time series (ITS) analysis included data on all oxycodone 5 mg discharge prescriptions between December 2018 to February 2021 in 12 Queensland hospitals utilising electronic prescribing software.
2 Methods
2.1 Study Design
This research utilised a retrospective uncontrolled interrupted time-series design. This type of study is conducted by undertaking a series of measurements over time, which are interrupted by an intervention. In this study, there were two ‘interruption’ points. The first interruption was the implementation of the QHMAC restrictions and the second the PBS prescription restrictions. This project was reviewed by the Metro South Research Office (LNR/2020/QMS/70245).
2.2 Setting
This study was undertaken at 12 public hospitals in Queensland, Australia. Information on each site can be found in Table 1. Each site implemented electronic prescribing at various times, these differences are reflected in the ‘Data collection start’ column of Table 1.
2.3 Intervention
2.3.1 Queensland Health Medicines Advisory Committee (QHMAC)
QHMAC is a Queensland state-based committee consisting of expert practising Queensland Health doctors and pharmacists who have been appointed by the committee sponsor, the Chief Health Officer. The committee is responsible for creating, maintaining, and reviewing the state-wide List of Approved Medicines (LAM), which determines the medications that can be prescribed in Queensland Health institutions. They then provide recommendations that are reviewed and approved by the Chief Health Officer. QHMAC typically limits its actions to deciding which medicines should be on the LAM, but in August 2019 for the first time they restricted the quantity of oxycodone 5-mg tablets prescribed on discharge. The intention of this restriction was to “promote the smaller opioid pack size to encourage tailoring of opioid prescribing to the individual patient’s clinical requirements, where appropriate” [19]. The change came into effect in September 2019 when the meeting minutes were confirmed and circulated to the hospital sites. As with all QHMAC recommendations, local hospital change implementation was via training and education. There was no change to the electronic prescribing system to enforce the recommendation by QHMAC.
2.3.2 Pharmaceutical Benefits Scheme (PBS)
The PBS is a part of the Australian Government’s National Medicines Policy [21]. It provides timely, reliable, and affordable access to certain medicines for Australians by subsidising the cost of medicine for most medical conditions. In June 2020, the PBS reduced the pack sizes of oxycodone 5-mg tablets from a quantity of 20 to a quantity of 10 tablets for the short-term treatment of patients with acute severe pain. This meant that if doctors prescribed oxycodone 5 mg in larger quantities, the patient would have to pay the full price of the medication as it would not be subsidised. Since the prescribing software used by Queensland Health facilities links directly to the PBS, this policy change led to a subsequent reduction in the default oxycodone pack size from 20 tablets to 10 tablets when oxycodone prescriptions were selected. As such, the prescribers were now ‘nudged’ into prescribing the lower quantity of oxycodone.
2.4 Data Collection
Data were extracted by running reports from the electronic prescribing system across eligible hospital sites from December 2018 to February 2021 (inclusive). Extracted reports contained information on prescribed oxycodone product, directions, quantity, date of prescription, and type of prescriber. Reports were extracted into Microsoft Excel and cleaned before being analysed using SPSS (Statistical Package for Social Sciences, IBM Software Version 27).
2.5 Statistical Methods
Data were descriptively summarised using frequency and proportions. Segmented regression was applied to this ITS design allowing for level and trend changes to oxycodone 5 mg prescriptions pre- and post-interventions to be determined. Data was summarised by week, which was defined as a 7-day period with the first day of the week as Monday. Five variables were entered into an ‘enter’ multiple regression model using SPSS with proportion of prescriptions with oxycodone for ≤ 10 tablets as the dependent variable. p-Values < 0.05 were deemed statistically significant.
A post-hoc sensitivity analysis of the ITS was undertaken, with all sites who changed to electronic prescribing after December 2018 being excluded (e.g. exclusion of hospital B, F, J, K, and L).
3 Results
Over the 27-month period, there were 110,728 discharge prescriptions written in the 12 Queensland public health electronic prescribing hospitals for oxycodone 5 mg (Table 1). Of the 110,728 prescriptions, only 33 (0.03%) had a prescription repeat (or refill) written on their prescription.
Unsurprisingly, the highest proportion of oxycodone 5 mg prescriptions were written by surgical and emergency prescribers, making up 50.4% and 27.2%, respectively, of total oxycodone prescriptions during the study period (Table 2).
3.1 Proportion Changes Over Time
Of the 110,728 discharge prescriptions, 29% (32,112) were written in the baseline period, 32.2% (35,706) were written after the LAM restrictions, and 38.8% (42,910) were written after the PBS restrictions came into effect (Table 3).
3.2 Segmented Linear Regression
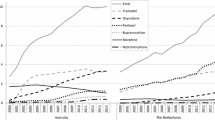
Results of the segmented linear regression for the proportion of discharge oxycodone 5 mg prescriptions written for ≤ 10 tablets across the study period are presented in Fig. 1 and Table 4. The scatterplot of standardised predicted values versus standardised residuals showed that the data met the assumptions of homogeneity of variance and linearity and the residuals were approximately normally distributed. Data were inspected visually using line plots to check for seasonality; no influence of seasonality was observed. The Durbin-Watson statistic was 1.4, just outside the accepted range of 1.5–2.5, indicating slight positive correlation.
Immediately after the QHMAC restrictions there was a 9% increase in the proportion of discharge prescriptions of oxycodone 5 mg written for ≤ 10 tablets. After the PBS restrictions there was a 9.8% increase.
3.2.1 Sensitivity and Post-Hoc Analysis
Post-hoc sensistivity analysis of the ITS was performed with the removal of all sites that changed to electronic prescribing after December 2018 (e.g. exclusion of hospitals B, F, J, K, and L). This reduced the sample size of the analysis to 62,150 prescriptions for oxycodone 5 mg. Compared with the model that included all hospitals, the sensitivity analysis demonstrated a lower baseline proportion (β0) (48.5%, 95% CI 47.2–49.8; p < 0.001), a higher baseline trend (β1) (0.5%, 95% CI 0.4–0.5; p < 0.001), a higher level of change post-QMHAC restrictions (β2) (11%, 95% CI 9.1–12.8; p < 0.001), a negative trend after QHMAC restcitions (β3) (− 0.2%, 95% CI − 0.3 to − 0.1; p < 0.001), a reduced level of change post-PBS restrictions (β4) (3.7%, 95% CI 1.8–5.5; p < 0.001), and a similar trend after PBS restrictions (β5) (− 0.2%, 95% CI − 0.3 to − 0.1; p < 0.001). After discussion with the research team, it was agreed to present the results from the data analysis that was agreed upon a prioiri.
4 Discussion
Our study found that policy reforms on prescribing limits can have an effect on excessive quantities for discharge oxycodone 5 mg prescribing. If extrapolated to a larger population, this could represent a significant decline in quantities of oxycodone 5 mg prescribed on discharge. The results suggest that policy interventions focusing on prescription quantity may be effective in influencing prescribing behaviour; however, their impact on actual patient harm and addiction are unclear.
Health care systems are implementing policy and practice interventions to mitigate the risks of long‐term opioid therapy [17, 22]. This study adds promising results that policy reform strategies can positively affect judiscious opioid prescribing on discharge. Both policy changes were successful in reducing quantities for oxycodone 5 mg prescriptions; however, further research is required to determine if local level hospital policies, statewide policies, or national interventions are most effective for reducing opioid prescriptions. Following QHMAC formularly updates to the guidelines and restrictions for oxycodone 5-mg tablets, there was a coinciding change in prescribing practices. Formularly restrictions are designed and implemented to reduce costs and use of prescription medicines and have been shown to be effective in a number of literature reviews [23]. The national PBS policy reform resulted in a similar impact on the proportion of oxycodone prescriptions for ≤10 tablets. There is evidence that electronic prescribing software influences prescribing patterns, as seen in a previous study which analysed 6390 opioid prescriptions from 448 prescribers [22]. Following the adoption of a new default quantity of 15 tablets, there was a significant increase in the proportion of opioid prescriptions for the quantity at the default level [22]. It is unclear if the PBS changes would have the same level of effectiveness in hospitals without electronic prescribing systems where discharge prescriptions are hand-written.
The QHMAC and PBS restrictions resulted in sustainable change with trends of the proportion of the reduced quantity scripts being prescribed post-intervention [19, 20]. After QHMAC changes, a steady increase in the trend of the proportion of oxycodone 5 mg prescriptions that were written for ≤ 10 tablets was observed. However, after the implementation of PBS changes, these trends plateaued and stabilised at around 90% of all discharge oxycodone 5 mg prescriptions being written for a quantity of ≤ 10. It is possible that the remaining 10% of prescriptions represent those where a larger quantity is clinically appropriate, such as for those patients in oncology or palliative care. It was interesting to note that on further analysis of the top three prescribing areas (surgical, emergency, and medical), medical prescriptions had a lower proportion of prescriptions for oxycodone written for ≤ 10 tablets. This is likely reflective of the complex nature of medical patients including those with chronic pain conditions and multiple comorbidities. Assessing the clinical appropriateness of opioids and prescription quantities was outside the scope of this research project; however, the authors acknowledge that providing opioids when they are genuinely required is an essential component to opioid stewardship.
Nearly 50% of prescriptions for opioids were distributed from surgical divisions (Table 2). This was anticipated given the widespread usage of low-dose opioids in managing post-operative pain. However, despite being low dose, studies have found that larger prescription quantities of opioids post-operatively can lead to chronic opioid use [11, 16]. Additionally, recent studies have demonstrated that patients use only 30–40% of the opioids prescribed after common surgical procedures [24]. A greater amount of initial opioid exposure (i.e., larger quantities prescribed) is associated with both greater risk of long-term use, and greater risk of overdose [25]. This overprescribing gap offers an opportunity for standardisation of prescribing quantities via policy intervention. Our results demonstrate that both policy interventions were effective in the surgical setting. This reduction in number of opioids in one of the areas with the highest rate of opioid prescribing may have led to reduced rates of dependence, misuse, and wastage.
This study aimed to investigate the impact two policy changes had on prescribing practices of oxycodone 5-mg tablets on discharge. To our knowledge, this ITS study is the first to investigate the impact of both policy-based and institutional interventions to reduce discharge oxycodone 5 mg prescribing quantities. For those countries that have not yet implemented state- or national-level policy surrounding opioid prescribing limits, the results of this study could be informative. Promising strategies such as those of QHMAC and PBS prescribing limit changes demonstrate concrete ways to reduce inappropriate quantity prescribing. Our study was able to demonstrate policy interventions that resulted in actional performance metrics and induced sustainable opioid prescribing changes.
Surveillance of opioid prescribing is critically important for understanding what changes in opioid prescribing are occurring over time, in different settings, and following interventions. While prescription changes seemed to be sustained for several months, as a next step in the research, re-evaluating to determine if changes to prescribing patterns are sustained into the future will be essential. Further research on the clinical appropriateness of those oxycodone prescriptions provided for larger quantities is required, along with any unintended consequences of providing reduced quantities of oxycodone medications.
4.1 Limitations
Our work has several limitations. Firstly, assessing clinical appropriateness of prescriptions was outside the scope of this project. While reductions in prescription quantities were observed, we are unable to say if these reductions were clinically appropriate for the patient's pain needs. We were also unable to separate between prescribing for acute or chronic pain based on the information accessed, or confirm if patients had their prescriptions filled at a pharmacy. In addition, we were unable to determine if patients recevied a re-supply of their pain medication in the community after they were discharged from hospital. Secondly, the two policy interventions coincidentally fell over the course of multiple public health hospitals implementing electronic prescribing systems in Queensland. As the reports used in this research were generated from the electronic prescribing system, we were only able to collect information from those hospitals and wards that had implemented electronic prescribing systems. This may have resulted in a skew of total number of opioids (e.g., a hospital that was utilising electronic prescribing software for longer may appear to have more oxycodone prescriptions). However, the final outcome of this research, the changes in prescribing patterns, were detected using proportions rather than raw numbers. Using proportions will have accounted for differences in raw numbers across sites. Thirdly, hospitals without electronic prescribing systems were not included in this study. It is unclear if the policy changes enacted, especially PBS changes that were accompanied by an electronic prompt, would have been as effective in the public hospitals without electronic prescribing software. Fourthly, the QHMAC phase of this project took place during the beginning of COVID-19 in Australia, which resulted in multiple large-scale lockdowns, reduced hospital activity, and reduced access to General Practitioners. It is unclear the effect these events had on opioid prescribing practices. Finally, this project used an uncontrolled ITS design rather than a controlled ITS design. A controlled design was not feasible for this project or the resources due to the nature of data collection (e.g. retrospectively downloading prescription information from electronic prescribing systems). Therefore, controls such as location-based, characteristic-based, behaviour-based, historical-cohort, outcome, and control time periods were not possible [26]. As the ITS was uncontrolled, the presence of confounding factors cannot be excluded. Additionally, the impact of hospital or ward level policy, guidelines, quality improvement projects related to oxycodone prescriptions, or shifts in hospital culture towards opioid prescribing (such as implementation of stewardship programs) are unknown to the team and may have contributed to some of the improvements seen. This may have been seen in the post-hoc sensitivity analysis, which saw a more rapid increase in the proportion of oxycodone 5-mg tablets written for <10 tablets when compared with the pooled data of all hospitals. This resulted in a smaller impact of PBS changes on the number of tablets prescribed. It is possible that hospitals in the post-hoc analysis had proactive and robust opioid stewardship cultures which resulted in these differences.
5 Conclusion
Opioid stewardship requires a multifaceted approach. The implementation of health system-wide initiatives can reduce short-term opioid prescribing. These results demonstrate that national health care policy reform with a quantity limit and subsequent electronic prescribing software integration were associated with reductions in oxycodone 5-mg tablet quantity on discharge. This study lends new emphasis to the importance of enforcement mechanisms for insitutional, state, and national policies in addressing the critical public health opioid epidemic in other institutional contexts. Continued multi-faceted policy efforts are necessary to ensure safe and judicious opioid prescribing. Interventions that only target a single aspect of the issue, such as restricting opioid supply, will not be sufficient to ameliorate the opioid epidemic. As prescribers respond to legislative and clinical pressures to reduce opioid prescriptions, further research is needed to examine downstream outcomes, including how initial treatment regimens can minimise misuse, addiction, and overdose.
Change history
04 August 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40264-022-01218-8
References
Opioid harm in Australia: and comparisons between Australia and Canada [Internet]. Canberra ACT: Australian Institute of Health and Welfare. 2018[updated 2011 Nov 26]. https://www.aihw.gov.au/reports/illicit-use-of-drugs/opioid-harm-in-australia/summary. Accessed 8 Jan 2022
Blanch B, Pearson S-A, Haber PS. An overview of the patterns of prescription opioid use, costs and related harms in Australia: prescribed opioid use in Australia. Br J Clin Pharmacol [Internet]. 2014;78(5):1159–66. https://doi.org/10.1111/bcp.12446.
Berterame S, Erthal J, Thomas J, Fellner S, Vosse B, Clare P, et al. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet [Internet]. 2016;387(10028):1644–56. https://doi.org/10.1016/S0140-6736(16)00161-6.
Lalic S, Ilomäki J, Bell JS, Korhonen MJ, Gisev N. Prevalence and incidence of prescription opoid analgesic use in Australia. Br J Clin Pharmacol [Internet]. 2019;85(1):202–15. https://doi.org/10.1111/bcp.13792.
Bohnert ASB, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA [Internet]. 2011;305(13):1315–21. https://doi.org/10.1001/jama.2011.370.
National Drug and Alcohol Research Centre. Trends in drug-induced deaths in Australia, 1997-2019 [Internet]. Sydney NSW: National Drug and Alcohol Research Centre. 2021[updated 2021 Jul 21]. https://ndarc.med.unsw.edu.au/resource-analytics/trends-drug-induced-deaths-australia-1997-2019. Accessed 9 Jan 2022.
National Drug and Alcohol Research Centre. Trends in drug-induced deaths in Australia, 1997-2019 [Internet]. Sydney NSW: National Drug and Alcohol Research Centre; 2021.[updated 2021 Jul 21;cited 2022 Jan 9] Availablefrom: https://ndarc.med.unsw.edu.au/resource-analytics/trends-drug-induced-deaths-australia-1997-2019. Australian Commission on Safety and Quality in Health Care (ACSQHC). Medication without harm—WHO Global Patient Safety Challenge. Australia’s response. Sydney NSW: ACSQHC; 2020 [updated 2020 Jan 01]. https://www.safetyandquality.gov.au/our-work/medication-safety/who-global-patient-safety-challenge-medication-without-harm. Accessed 10 Jan 2022.
Burcher KM, Suprun A, Smith A. Risk factors for opioid use disorders in adult postsurgical patients. Cureus [Internet]. 2018;10(5):e2611. https://www.cureus.com/articles/10503-risk-factors-for-opioid-use-disorders-in-adult-postsurgicalpatients.
Pouryahya P, Birkett W, McR Meyer AD, Louey S, Belhadfa M, Ferdousi S, et al. Oxycodone prescribing in the emergency department during the opioid crisis. Emerg Med Australas [Internet]. 2020;32(6):996–1000. https://doi.org/10.1111/1742-6723.13545.
Allen ML, Kim CC, Braat S, Jones K, Winter N, Hucker TR, et al. Post-discharge opioid use and handling in surgical patients: a multicentre prospective cohort study. Anaesth Intensive Care [Internet]. 2020;48(1):36–42. https://doi.org/10.1177/0310057X19895019.
Hadlandsmyth K, Lund BC, Mosher HJ. Associations between initial opioid exposure and the likelihood for long-term use. J Am Pharm Assoc [Internet]. 2019;59(1):17–22. https://doi.org/10.1016/j.japh.2018.09.005.
Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use—United States, 2006–2015. MMWR Morb Mortal Wkly Rep [Internet]. 2017;66(10):265–9. https://doi.org/10.15585/mmwr.mm6610a1.
Deyo RA, Hallvik SE, Hildebran C, Marino M, Dexter E, Irvine JM, et al. Association between initial opioid prescribing patterns and subsequent long-term use among opioid-naïve patients: a statewide retrospective cohort study. J Gen Intern Med [Internet]. 2017;32(1):21–7. https://doi.org/10.1007/s11606-016-3810-3.
Edlund MJ, Martin BC, Russo JE, DeVries A, Braden JB, Sullivan MD. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription: the role of opioid prescription. Clin J Pain [Internet]. 2014;30(7):557–64. https://doi.org/10.1097/AJP.0000000000000021.
Hooten WM, St Sauver JL, McGree ME, Jacobson DJ, Warner DO. Incidence and risk factors for progression from short-term to episodic or long-term opioid prescribing: a population-based study. Mayo Clin Proc [Internet]. 2015;90(7):850–6. https://doi.org/10.1016/j.mayocp.2015.04.012.
Lalic S, Gisev N, Bell JS, Korhonen MJ, Ilomäki J. Predictors of persistent prescription opioid analgesic use among people without cancer in Australia. Br J Clin Pharmacol [Internet]. 2018;84(6):1267–78. https://doi.org/10.1111/bcp.13556.
Pattullo C, Suckling B, Taylor S, Thomson J, Collins G, Hall L, et al. Developing and piloting an adaptable oxycodone quality improvement strategy: steps towards opioid stewardship. Aust Health Rev [Internet]. 2021;45(3):353–60. https://doi.org/10.1071/AH20262.
Australian Commission on Safety and Quality in Health Care (ACSQHC). Opioid Analgesic Stewardship in Acute Pain Clinical Care Standard [Internet]. Sydney NSW: ACSQHC. 2021. https://www.safetyandquality.gov.au/standards/clinical-care-standards/opioid-analgesic-stewardship-acute-pain-clinical-care-standard. Accessed 10 Jan 2022.
Queensland Health. Queensland Health List of Approved Medicines (Internal document). [Internet]. Brisbane QLD: Queensland Health. 2020. https://www.health.qld.gov.au/__data/assets/pdf_file/0019/442432/lam.pdf. Accessed 18 Dec 2021.
Australian Government Department of Health. Public Summary Document (PSD) December 2019 PBAC Meeting [Internet]. Canberra ACT: Australian Government Department of Health. 2019. https://www.pbs.gov.au/industry/listing/elements/pbac-meetings/psd/2019-12/files/tga-opioid-reforms-psd-december-2019.pdf. Accessed 14 Feb 2022.
Australian Government Department of Health. Pharmaceutical benefits scheme (PBS) [Internet]. Canberra ACT: Australian Government Department of Health. 2022 [updated 2022 Jan 01]. https://www.pbs.gov.au/info/about-the-pbs. Accessed 14 Feb 2022.
Zivin K, White JO, Chao S, Christensen AL, Horner L, Petersen DM, et al. Implementing electronic health record default settings to reduce opioid overprescribing: a pilot study. Pain Med [Internet]. 2019;20(1):103–12. https://doi.org/10.1093/pm/pnx304.
Park Y, Raza S, George A, Agrawal R, Ko J. The effect of formulary restrictions on patient and payer outcomes: a systematic literature review. J Manag Care Spec Pharm [Internet]. 2017;23(8):893–901. https://doi.org/10.18553/jmcp.2017.23.8.893.
Sabatino MJ, Kunkel ST, Ramkumar DB, Keeney BJ, Jevsevar DS. Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg Am [Internet]. 2018;100(3):180–8. https://doi.org/10.2106/JBJS.17.00672.
Brat GA, Agniel D, Beam A, Yorkgitis B, Bicket M, Homer M, et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. BMJ [Internet]. 2018;360: j5790. https://doi.org/10.1136/bmj.j5790.
Lopez Bernal J, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol [Internet]. 2018;47(6):2082–93. https://doi.org/10.1093/ije/dyy135.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics and data approval
This project was reviewed by the Metro South Research Office and deemed exempt from HREC review (LNR/2020/QMS/70245). Approval to use integrated electronic medical record data for an audit/quality assurance project in accordance with the Hospital and Health Boards Act 2011 (Qld) was granted by the Queensland Health Chief information Officer.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Conflicts of interest
Will Tumusiime, Caitlin Hardman and Elizabeth McCourt declare that they have no conflicts of interest.
Consent to participate
Not applicable.
Consent for publication
Approval to undertake the project was received from the quality assurance department of each organisation. As part of this process consent for external publication was obtained.
Data and/or code availability
Extracted reports contained information on oxycodone product, prescribed directions, quantity, date of prescription, and type of prescriber. Data is not available due to strict confidentiality and data information policies of Queensland Health.
Author contributions
Will Tumusiime: study design, data collection, data cleaning, writing and editing manuscript. Caitlin Hardman: study design, data cleaning, writing and editing manuscript. Elizabeth McCourt: analysis design, data cleaning, data analysis, writing and editing manuscript. All authors read and approved the final version.
Additional information
The original online version of this article was revised. In the original publication of the article, oxycodone dose was missing from the column heading of tables 1 and 2 and this has been corrected now.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tumusiime, W., Hardman, C. & McCourt, E. Impact of Policy Interventions on Oxycodone Prescribing in Queensland, Australia: An Uncontrolled Interrupted Time Series Study. Drug Saf 45, 941–949 (2022). https://doi.org/10.1007/s40264-022-01209-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-022-01209-9