Abstract
Introduction
Medication-related harm represents a significant issue for patient safety and quality of care. One strategy to avoid preventable adverse drug events is to utilize patient-specific factors such as pharmacogenomics (PGx) to individualize therapy.
Objective
We measured the number of patients enrolled in a health-system biobank with actionable PGx results who received relevant medications and assessed the incidence of adverse drug events (ADEs) that might have been prevented had the PGx results been used to inform prescribing.
Methods
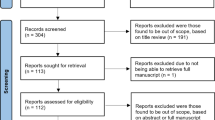
Patients with actionable PGx results in the following four genes with Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines were identified: HLA-A*31:01, HLA-B*15:02, TPMT, and VKORC1. The patients who received interacting medications (carbamazepine, oxcarbazepine, thiopurines, or warfarin) were identified, and electronic health records were reviewed to determine the incidence of potentially preventable ADEs.
Results
Of 36,424 patients with PGx results, 2327 (6.4%) were HLA-A*31:01 positive; 3543 (9.7%) were HLA-B*15:02 positive; 2893 (7.9%) were TPMT intermediate metabolizers; and 4249 (11.7%) were homozygous for the VKORC1 c.1639 G>A variant. Among patients positive for one of the HLA variants who received carbamazepine or oxcarbazepine (n = 92), four (4.3%) experienced a rash that warranted drug discontinuation. Among the TPMT intermediate metabolizers who received a thiopurine (n = 56), 11 (19.6%) experienced severe myelosuppression that warranted drug discontinuation. Among patients homozygous for the VKORC1 c.1639 G>A variant who received warfarin (n = 379), 85 (22.4%) experienced active bleeding and/or international normalized ratio (INR) > 5 that warranted drug discontinuation or dose reduction.
Conclusion
Patients with actionable PGx results from a health-system biobank who received relevant medications experienced predictable ADEs. These ADEs may have been prevented if the patients’ PGx results were available in the electronic health record with clinical decision support prior to prescribing.

Similar content being viewed by others
References
Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ. 2016;353:i2139. https://doi.org/10.1136/bmj.i2139.
Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA. 2016;316(20):2115–25. https://doi.org/10.1001/jama.2016.16201.
Aspden P, Wolcott JA, Bootman JL, Cronenwett LR. Preventing medication errors: quality chasm series. Washington, DC: The National Academic Press; 2007.
Crisamore KR, Nolin TD, Coons JC, Empey PE. Engaging and empowering stakeholders to advance pharmacogenomics. Clin Pharmacol Ther. 2019;106(2):305–8. https://doi.org/10.1002/cpt.1470.
Rogers SL, Keeling NJ, Giri J, Gonzaludo N, Jones JS, Glogowski E, et al. PARC report: a health-systems focus on reimbursement and patient access to pharmacogenomics testing. Pharmacogenomics. 2020;21(11):785–96. https://doi.org/10.2217/pgs-2019-0192.
Verbelen M, Weale ME, Lewis CM. Cost-effectiveness of pharmacogenetic-guided treatment: are we there yet? Pharmacogenomics J. 2017;17(5):395–402. https://doi.org/10.1038/tpj.2017.21.
Roden DM, McLeod HL, Relling MV, Williams MS, Mensah GA, Peterson JF, et al. Pharmacogenomics. Lancet. 2019;394(10197):521–32. https://doi.org/10.1016/S0140-6736(19)31276-0.
Volpi S, Bult CJ, Chisholm RL, Deverka PA, Ginsburg GS, Jacob HJ, et al. Research directions in the clinical implementation of pharmacogenomics: an overview of US programs and projects. Clin Pharmacol Ther. 2018;103(5):778–86. https://doi.org/10.1002/cpt.1048.
Green RC, Berg JS, Grody WW, Kalia SS, Korf BR, Martin CL, et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet Med. 2013;15(7):565–74. https://doi.org/10.1038/gim.2013.73.
Van Driest SL, Shi Y, Bowton EA, Schildcrout JS, Peterson JF, Pulley J, et al. Clinically actionable genotypes among 10,000 patients with preemptive pharmacogenomic testing. Clin Pharmacol Ther. 2014;95(4):423–31. https://doi.org/10.1038/clpt.2013.229.
O’Donnell PH, Danahey K, Ratain MJ. The outlier in all of us: why implementing pharmacogenomics could matter for everyone. Clin Pharmacol Ther. 2016;99(4):401–4. https://doi.org/10.1002/cpt.333.
Phillips EJ, Sukasem C, Whirl-Carrillo M, Muller DJ, Dunnenberger HM, Chantratita W, et al. Clinical pharmacogenetics implementation consortium guideline for HLA genotype and use of carbamazepine and oxcarbazepine: 2017 update. Clin Pharmacol Ther. 2018;103(4):574–81. https://doi.org/10.1002/cpt.1004.
Relling MV, Schwab M, Whirl-Carrillo M, Suarez-Kurtz G, Pui CH, Stein CM, et al. Clinical pharmacogenetics implementation consortium guideline for thiopurine dosing based on TPMT and NUDT15 genotypes: 2018 update. Clin Pharmacol Ther. 2019;105(5):1095–105. https://doi.org/10.1002/cpt.1304.
Johnson JA, Caudle KE, Gong L, Whirl-Carrillo M, Stein CM, Scott SA, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for pharmacogenetics-guided warfarin dosing: 2017 update. Clin Pharmacol Ther. 2017;102(3):397–404. https://doi.org/10.1002/cpt.668.
Karnes JH, Miller MA, White KD, Konvinse KC, Pavlos RK, Redwood AJ, et al. Applications of immunopharmacogenomics: predicting, preventing, and understanding immune-mediated adverse drug reactions. Annu Rev Pharmacol Toxicol. 2019;59:463–86. https://doi.org/10.1146/annurev-pharmtox-010818-021818.
Hicks JK, Dunnenberger HM, Gumpper KF, Haidar CE, Hoffman JM. Integrating pharmacogenomics into electronic health records with clinical decision support. Am J Health Syst Pharm. 2016;73(23):1967–76. https://doi.org/10.2146/ajhp160030.
Rahawi S, Naik H, Blake KV, Owusu Obeng A, Wasserman RM, Seki Y, et al. Knowledge and attitudes on pharmacogenetics among pediatricians. J Hum Genet. 2020;65(5):437–44. https://doi.org/10.1038/s10038-020-0723-0.
DeLuca J, Selig D, Poon L, Livezey J, Oliver T, Barrett J, et al. Toward personalized medicine implementation: survey of military medicine providers in the area of pharmacogenomics. Mil Med. 2020;185(3–4):336–40. https://doi.org/10.1093/milmed/usz419.
Smith DM, Namvar T, Brown RP, Springfield TB, Peshkin BN, Walsh RJ, et al. Assessment of primary care practitioners’ attitudes and interest in pharmacogenomic testing. Pharmacogenomics. 2020;21(15):1085–94. https://doi.org/10.2217/pgs-2020-0064.
Kuperman GJ, Bobb A, Payne TH, Avery AJ, Gandhi TK, Burns G, et al. Medication-related clinical decision support in computerized provider order entry systems: a review. J Am Med Inform Assoc. 2007;14(1):29–40. https://doi.org/10.1197/jamia.M2170.
Dunnenberger HM, Crews KR, Hoffman JM, Caudle KE, Broeckel U, Howard SC, et al. Preemptive clinical pharmacogenetics implementation: current programs in five US medical centers. Annu Rev Pharmacol Toxicol. 2015;55:89–106. https://doi.org/10.1146/annurev-pharmtox-010814-124835.
Aquilante CL, Kao DP, Trinkley KE, Lin CT, Crooks KR, Hearst EC, et al. Clinical implementation of pharmacogenomics via a health system-wide research biobank: the University of Colorado experience. Pharmacogenomics. 2020;21(6):375–86. https://doi.org/10.2217/pgs-2020-0007.
Relling MV, Klein TE, Gammal RS, Whirl-Carrillo M, Hoffman JM, Caudle KE. The clinical pharmacogenetics implementation consortium: 10 years later. Clin Pharmacol Ther. 2020;107(1):171–5. https://doi.org/10.1002/cpt.1651.
Dong OM, Bates J, Chanfreau-Coffinier C, Naglich M, Kelley MJ, Meyer LJ, et al. Veterans Affairs Pharmacogenomic Testing for Veterans (PHASER) clinical program. Pharmacogenomics. 2021. https://doi.org/10.2217/pgs-2020-0173.
Ramsey LB, Prows CA, Zhang K, Saldana SN, Sorter MT, Pestian JP, et al. Implementation of pharmacogenetics at cincinnati children’s hospital medical center: lessons learned over 14 years of personalizing medicine. Clin Pharmacol Ther. 2019;105(1):49–52. https://doi.org/10.1002/cpt.1165.
Marrero RJ, Cicali EJ, Arwood MJ, Eddy E, DeRemer D, Ramnaraign BH, et al. How to transition from single-gene pharmacogenetic testing to preemptive panel-based testing: a tutorial. Clin Pharmacol Ther. 2020;108(3):557–65. https://doi.org/10.1002/cpt.1912.
Arwood MJ, Chumnumwat S, Cavallari LH, Nutescu EA, Duarte JD. Implementing pharmacogenomics at your institution: establishment and overcoming implementation challenges. Clin Transl Sci. 2016;9(5):233–45. https://doi.org/10.1111/cts.12404.
Acknowledgements
We would like to acknowledge Wejdan Aljassas, Marina Amin, Youmi Son, Elaina Audi, Yihenew Ewnetu, Anthony Branco, Paige Desrosiers, Kevin Joseph, Rachel Carboni, Zeina Youssef, Adwoa Edusei, Bryanna Marie Pacheo, and Youngheon Choi for their contributions to data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
Dr. Bates consults for EarlySense, which makes patient safety monitoring systems. He receives cash compensation from CDI (Negev), Ltd, which is a not-for-profit incubator for health IT startups. He receives equity from ValeraHealth, which makes software to help patients with chronic diseases. He receives equity from Clew, which makes software to support clinical decision making in intensive care. He receives equity from MD Clone, which takes clinical data and produces deidentified versions of it. He receives equity from AESOP, which makes software to reduce medication error rates. He receives research funding from IBM Watson Health. He serves as a Visiting Professor at Stavanger University. No other authors have any conflict of interest to declare.
Ethics approval
This study has been approved by our local Institutional Review Board.
Consent to participate
N/A.
Consent to publication
All parties have consented for publication.
Availability of data and material
N/A.
Code availability
N/A.
Contributorship statement
SNS, DLS, and RSG made substantial contributions to the conception of the design of the work; SNS, RSG, MGA, MA, DR, and SH assisted in data collection, chart review, and interpretation. DLS, MGA, RSG, and MA contributed to writing and revision of the manuscript. JBK and DWB supervised the research design and contributed to the writing and revision of the manuscript. All authors give approval for the final version to be published and agree to be accountable for all aspects of the work, ensuring questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Rights and permissions
About this article
Cite this article
Shah, S.N., Gammal, R.S., Amato, M.G. et al. Clinical Utility of Pharmacogenomic Data Collected by a Health-System Biobank to Predict and Prevent Adverse Drug Events. Drug Saf 44, 601–607 (2021). https://doi.org/10.1007/s40264-021-01050-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-021-01050-6