Abstract
Introduction
Perflutren microbubble/microsphere ultrasound contrast agents have a black-box warning based on case reports of serious cardiopulmonary events. There have been several subsequent observational safety studies. Large spontaneous reporting databases may help detect/refine signals of rare adverse events that elude other data sources/study designs.
Objective
The objective of this study was to supplement existing knowledge of the reported safety of perflutren using statistical analysis of spontaneous reports.
Methods
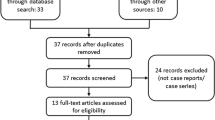
We analyzed information from the US Food and Drug Administration Adverse Event Reporting System using a disproportionality analysis. Analysis of overall reporting for perflutren was supplemented by subset (age, indication) analysis. A signal of disproportionate reporting (SDR) was defined as EB05 >2.
Results
Overall, 18/380 Preferred Terms and 1/83 Standardized Medical Queries had SDRs. Most were small (EB05 = 2–4). Back pain and flank pain were the largest SDRs followed by events compatible with signs/symptoms of hypersensitivity. The general pattern of SDRs in the subset analysis was consistent with the overall analysis. Almost all events with SDRs were literally or conceptually labeled. Except for chest pain (higher in the age <65 years subgroup) and back pain (higher in the age ≥65 years subgroup), there were no statistically significant differences between age subsets. Except for the Preferred Terms Pruritus and Urticaria and the narrow Standardized Medical Queries Ventricular tachyarrhythmia, Angioedema, Oropharyngeal allergic conditions, and Hypersensitivity (higher in the stress test subgroup), there were no statistically significant reporting differences between indication subsets. There were no SDRs associated with the major cardiovascular events of death, myocardial infarction/ischemia, angina, arrhythmias, or convulsions in any analysis.
Conclusions
Our combined signal detection/evaluation analysis did not identify SDRs of novel adverse events or major cardiovascular events associated with perflutren ultrasound contrast agents. The negative results for major cardiovascular events extend previous signal evaluation exercises supporting the relative cardiovascular safety of these agents.
Similar content being viewed by others
References
Crouse LJ, Cheirif J, Hanly DE, Kisslo JA, Labovitz AJ, Raichlen JS, Schutz RW, Shah PM, Smith MD. Opacification and border delineation improvement in patients with suboptimal endocardial border definition in routine echocardiography: results of the Phase III Albunex Multicenter Trial. J Am Coll Cardiol. 1993;22(5):1494–500.
Reilly JP, Tunick PA, Timmermans RJ, Stein B, Rosenzweig BP, Kronzon I. Contrast echocardiography clarifies uninterpretable wall motion in intensive care unit patients. J Am Coll Cardiol. 2000;35(2):485–90.
US Food and Drug Administration, revised prescribing information for Definity on August 2011. http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021064s011lbl.pdf. Accessed 3 Jun 2015.
US Food and Drug Administration, revised prescribing information for Optison on August 17, 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020899s015lbl.pdf. Accessed 3 Jun 2015.
Yu EH, Sloggett CE, Iwanochko RM, Rakowski H, Siu SC. Feasibility and accuracy of left ventricular volumes and ejection fraction determination by fundamental, tissue harmonic, and intravenous contrast imaging in difficult-to-image patients. J Am Soc Echocardiogr. 2000;13(3):216–24.
Malm S, Frigstad S, Sagberg E, Larsson H, Skjaerpe T. Accurate and reproducible measurement of left ventricular volume and ejection fraction by contrast echocardiography: a comparison with magnetic resonance imaging. J Am Coll Cardiol. 2004;44(5):1030–5.
U.S. Food and Drug Administration Alert. Micro-bubble contrast agents (marketed as Definity (Perflutren Lipid Microsphere) Injectable Suspension and Optison (Perflutren Protein-Type A Microspheres for Injection). 2007. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm152686.htm. Accessed 3 Jun 2015.
US Food and Drug Administration, FDA Advisory Committee Briefing Document, Cardiovascular and Renal Drugs Advisory Committee June 24, 2008, Safety considerations in the development of ultrasound contrast agents. http://www.fda.gov/ohrms/dockets/ac/08/briefing/2008-4369b1-01.pdf. Accessed 3 Jun 2015.
Main ML, Goldman JH, Grayburn PA. Ultrasound contrast agents: balancing safety versus efficacy. Exp Opin Drug Saf. 2009;8(1):49–56.
Smyth YM, Gabriel RS, Sabik EM, Klein AL, Grimm R, Thomas JD, Menon V. Marked decline in clinical use of ultrasound contrast agents following black box warning: observations from the clinic. Eur Heart J. 2008;29:376.
Summary Minutes of May 2, 2011 Joint Meeting of the Cardiovascular and Renal Drugs and Drug Safety and Risk Management Advisory Committees. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/CardiovascularandRenalDrugsAdvisoryCommittee/UCM255248.pdf. Accessed 3 Jun 2015.
Weiss RJ, Ahmad M, Villanueva F, Schmitz S, Bhat G, Hibberd MG, Main ML. CaRES (Contrast Echocardiography Registry for Safety Surveillance): a prospective multicenter study to evaluate the safety of the ultrasound contrast agent definity in clinical practice. J Am Soc Echocardiogr. 2012;25(7):790–5.
Wei K, Main ML, Lang RM, Klein A, Angeli S, Panetta C, Mikati I, Lee LV, Bernstein JA, Ahmad M. The effect of definity on systemic and pulmonary hemodynamics in patients. J Am Soc Echocardiogr. 2012;25(5):584–8.
Exuzides A, Main ML, Colby C, Grayburn PA, Feinstein SB, Goldman JH. A retrospective comparison of mortality in critically ill hospitalized patients undergoing echocardiography with and without ultrasound contrast. JACC Cardiovasc Imaging. 2010;3(6):578–85.
Dolan MS, Gala SS, Dodla S, Abdelmoneim SS, Xie F, Cloutier D, Bierig M, Mulvagh SL, Porter TR, Labovitz AJ. Safety and efficacy of commercially available ultrasound contrast agents for rest and stress echocardiography a multicenter experience. J Am Coll Cardiol. 2009;53(1):32–8.
Gabriel RS, Smyth YM, Menon V, Klein AL, Grimm RA, Thomas JD, Sabik EM. Safety of ultrasound contrast agents in stress echocardiography. Am J Cardiol. 2008;102(9):1269–72.
Herzog CA. Incidence of adverse events associated with use of perflutren contrast agents for echocardiography. JAMA. 2008;299(17):2023–5.
Khawaja OA, Shaikh KA, Al-Mallah MH. Meta-analysis of adverse cardiovascular events associated with echocardiographic contrast agents. Am J Cardiol. 2010;106(5):742–7.
Kusnetzky LL, Khalid A, Khumri TM, Moe TG, Jones PG, Main ML. Acute mortality in hospitalized patients undergoing echocardiography with and without an ultrasound contrast agent: results in 18,671 consecutive studies. J Am Coll Cardiol. 2008;51(17):1704–6.
Main ML, Ryan AC, Davis TE, Albano MP, Kusnetzky LL, Hibberd M. Acute mortality in hospitalized patients undergoing echocardiography with and without an ultrasound contrast agent (multicenter registry results in 4,300,966 consecutive patients). Am J Cardiol. 2008;102(12):1742–6.
Wei K, Mulvagh SL, Carson L, et al. The safety of Definity and Optison for ultrasound image enhancement: a retrospective analysis of 78,383 administered contrast doses. J Am Soc Echocardiogr. 2008;21(11):1202–6.
Aggeli C, Giannopoulos G, Roussakis G, Christoforatou E, Marinos G, Toli C, Pitsavos C, Stefanadis C. Safety of myocardial flash-contrast echocardiography in combination with dobutamine stress testing for detection of ischemia in 5250 studies. Heart. 2008;94(12):1571–7.
Platts DG, Luis SA, Roper D, Burstow D, Call T, Forshaw A, Pascoe R. The safety profile of perflutren microsphere contrast echocardiography during rest and stress imaging: results from an Australian multicentre cohort. Heart Lung Circ. 2013;22(12):996–1002.
Abdelmoneim SS, Bernier M, Scott CG, Dhoble A, Ness SA, Hagen ME, Moir S, McCully RB, Pellikka PA, Mulvagh SL. Safety of contrast agent use during stress echocardiography in patients with elevated right ventricular systolic pressure: a cohort study. Circ Cardiovasc Imaging. 2010;3(3):240–8.
Abdelmoneim SS, Bernier M, Scott CG, Dhoble A, Ness SA, Hagen ME, Moir S, McCully RB, Pellikka PA, Mulvagh SL. Safety of contrast agent use during stress echocardiography: a 4-year experience from a single-center cohort study of 26,774 patients. JACC Cardiovasc Imaging. 2009;2(9):1048–56.
Shaikh K, Chang SM, Peterson L, Rosendahl-Garcia K, Quinones MA, Nagueh SF, Kurrelmeyer K, Zoghbi WA. Safety of contrast administration for endocardial enhancement during stress echocardiography compared with noncontrast stress. Am J Cardiol. 2008;102(11):1444–50.
Anantharam B, Chahal N, Chelliah R, Ramzy I, Gani F, Senior R. Safety of contrast in stress echocardiography in stable patients and in patients with suspected acute coronary syndrome but negative 12-hour troponin. Am J Cardiol. 2009;104(1):14–8.
Hauben M, Hung EY. A quantitative analysis of the spontaneous reporting of congestive heart failure-related adverse events with systemic anti-fungal drugs. J Clin Pharmacol. 2013;53(7):762–72.
Hauben M, Hung EY. Pneumothorax as an adverse drug event: an exploratory aggregate analysis of the US FDA AERS database including a confounding by indication analysis inspired by Cornfield’s condition. Int J Med Sci. 2013;10(8):965–73.
FDA adverse event reporting system. http://www.fda.gov/drugs/guidancecomplianceregulatoryinformation/surveillance/adversedrugeffects/default.htm. Accessed 3 Jun 2015.
MedDRA® Maintenance and Support Services Organization. Introductory guide for Standardised MedDRA® Queries (SMQs) Version 17.0. 2014. http://www.meddra.org/sites/default/files/guidance/file/smq_intguide_17_0_english.pdf. Accessed 3 Jun 2015.
Brown EG. Effects of coding dictionary on signal generation: a consideration of use of MedDRA compared with WHO-ART. Drug Saf. 2002;25(6):445–52.
Hauben M, Bate A. Decision support methods for the detection of adverse events in post-marketing data. Drug Discov Today. 2009;14(7–8):343–57.
Hauben M, Aronson JK. Defining ‘signal’ and its subtypes in pharmacovigilance based on a systematic review of previous definitions. Drug Saf. 2009;32(2):99–110.
Kubota K, Koide D, Toshiki H. Comparison of data mining methodologies using Japanese spontaneous reports. Pharamcoepidemiol Drug Saf. 2004;13(6):307–94.
Maignon F, Hauben M, Hung E, VanHolle L, Dogne JM. Assessing the extent and impact of the masking effect of disproportionality analyses on two spontaneous reporting systems databases. Pharmacoepidemiol Drug Saf. 2014;23(2):195–207.
Almenoff J, Tonning JM, Gould AL, Szarfman A, Hauben M, Ouellet-Hellstrom R, Ball R, Hornbuckle K, Walsh L, Yee C, Sacks ST, Yuen N, Patadia V, Blum M, Johnston M, Gerrits C, Seifert H, Lacroix K. Perspectives on the use of data mining in pharmacovigilance. Drug Saf. 2005;28(11):981–1007.
EMEA Eudravigilance Expert Working Group (EV-EWG). Guideline on the use of statistical signal detection methods in the Eudravigilance data analysis system. 26 June 2008. London. Doc. Ref. EMEA/106464/2006 rev.1. http://www.ema.europa.eu/docs/en_GB/document_library/Regulatory_and_procedural_guideline/2009/11/WC500011434.pdf. Accessed 3 Jun 2015.
Zhao J, Karlsson I, Asker L, Boström H. Applying methods for signal detection in spontaneous reports to electronic patient records. In: Proceedings of the ACM KDD; 2013.
Bate A, Evans SJ. Quantitative signal detection using spontaneous ADR reporting. Pharmacoepidemiol Drug Saf. 2009;18(6):427–36.
Nguyen TT, Dhond MR, Sabapathy R, Bommer WJ. Contrast microbubbles improve diagnostic yield in ICU patients with poor echocardiographic windows. Chest. 2001;120(4):1287–92.
Hauben M, Aronson JK. Gold standards in pharmacovigilance: the use of definitive anecdotal reports of adverse drug reactions as pure gold and high-grade ore. Drug Saf. 2007;30(8):645–55.
Aronson JK, Hauben M. Anecdotes that provide definitive evidence. BMJ. 2006;333(7581):1267–9.
deBoissieu P, Kanagaratnam L, Abou Taam M, Roux MP, Drame M, Trenque T. Notoriety bias in a database of spontaneous reports: the example of osteonecrosis of the jaw under bisphosphonate therapy in the French national pharmacovigilance database. Pharmacoepidemiol Drug Saf. 2014;23(9):989–92.
Pariente A, Didailler M, Avillach P, Miremont-Salame G, Fourrier-Regalt A, Haramburu F, Moore N. A potential competition bias in the detection of safety signals from spontaneous reporting databases. Pharmacoepidemiol Drug Saf. 2010;19(11):1166–71.
Moore N, Hall G, Sturkenboom M, Mann R, Lagnaoui R, Begaud B. Biases affecting the proportional reporting ratio (PRR) in spontaneous reports pharmacovigilance databases: the example of sertindole. Pharmacoepidemiol Drug Saf. 2003;12(4):271–81.
Hauben M, Reich L, DeMicco J, Kim K. “Extreme duplication” in the US FDA adverse events reporting system database. Drug Saf. 2007;30(6):551–4.
Bate A, Edwards IR. Data mining in spontaneous reports. Basic Clin Pharmacol Toxicol. 2006;98(3):324–30.
Hauben M, Reich L, Gerrits CM, Younus M. Illusions of objectivity and recommendation for reporting data mining results. Eur J Clin Pharmacol. 2007;63(5):517–21.
Schenker N, Gentleman JF. On judging the significance of differences by examining the overlap between confidence intervals. Am Stat. 2001;55(3):182–6.
Chen Y, Guo JJ, Healy DP, Lin X, Patel NC. Risk of hepatotoxicity associated with the use of telithromycin: a signal detection using data mining algorithms. Ann Pharmacother. 2008;42(12):1791–6.
Hauben M, Zou C, Whalen E, Wang W, Zhang LH. A pilot study on the feasibility of using P-plots for signal detection in pharmacovigilance. Stat Biopharm Res. 2015;7(1):25–35.
Johnson K, Guo C, Gosink M, Wang V, Hauben M. Multinomial modeling and an evaluation of common data-mining algorithms for identifying signals of disproportionate reporting in pharmacovigilance databases. Bioinformatics. 2012;28(23):3123–30.
Holmes S, Morris C, Tibshirani R. Bradley Efron: a conversation with good friends. Stat Sci. 2003;18(2):268–82.
Sakaeda T, Tamon A, Kadoyama K, Okuno Y. Data mining of the public version of the FDA Adverse Event Reporting System. Int J Med Sci. 2013;10(7):796–803.
Candore G, Juhlin K, Manlik K, Thakrat B, Quarcoo N, Seabroke S, Wisniewski A, Slattery J. Comparison of statistical signal detection methods within and across spontaneous reporting system databases. Drug Saf. 2015;38(6):577–87.
Ghosh P, Dewanji A. Effect of reporting bias in the analysis of spontaneous reporting data. Pharm Stat. 2015;14(1):20–5.
Acknowledgments
Lauren Rosenberg, M.D., who assisted in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this study.
Conflict of interest
Manfred Hauben, Eric Hung, and Vincenza Snow are employees and stockholders of Pfizer, Incorporated. Manfred Hauben holds stocks in General Electric, a subsidiary of which, GE Healthcare, markets the ultrasound contrast agent OPTISON™. Manfred Hauben, Eric Hung, Vincenza Snow, Kelly C. Hanretta, and Sripal Bangalore have no other conflicts of interest that are relevant to the content of this study.
Rights and permissions
About this article
Cite this article
Hauben, M., Hung, E.Y., Hanretta, K.C. et al. Safety of Perflutren Ultrasound Contrast Agents: A Disproportionality Analysis of the US FAERS Database. Drug Saf 38, 1127–1139 (2015). https://doi.org/10.1007/s40264-015-0332-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-015-0332-6