Abstract
Background
A recent Canadian case–control study reported a 4.5-fold increased risk of retinal detachment (RD) during oral fluoroquinolone use. Of the fluoroquinolone-exposed cases, 83 % were exposed to ciprofloxacin. We sought to replicate this finding, and assess whether it applied to all fluoroquinolones.
Methods
In two large US healthcare databases, we performed three case–control analyses: one replicating the recent study; one addressing additional potential confounders; and one that increased sample size by dropping the Canadian study’s requirement for a prior ophthalmologist visit. We also performed a self-controlled case-series (SCCS) analysis in which each subject served as his or her own comparator.
Results
In the replication case–control analyses, the adjusted odds ratios (ORs) for any exposure to fluoroquinolones or ciprofloxacin were approximately 1.2 in both databases, and were statistically significant, and the ORs for current exposure were modestly above 1 in one database, modestly below 1 in the other, and not statistically significant. In the other case–control analyses, the ORs were close to 1. In a post hoc age-stratified case–control analysis, we observed an association of RD with fluoroquinolone exposure among older subjects in one of the two databases. All estimates from the SCCS analyses were below 1.2 and none was statistically significant.
Conclusion
The present study does not confirm the recent Canadian study’s finding of a strong relationship between RD and current exposure to fluoroquinolones. Instead, it found a modest association between RD and current or any exposure to fluoroquinolones in the case–control analyses, and no association in the SCCS analyses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study sought to replicate a recent Canadian case–control study that found a 4.5-fold increased risk of retinal detachment during oral fluoroquinolone use. |
In several case–control analyses, including one that mimicked the recent study, the present study found odds ratios of approximately 1.2. |
In a self-controlled case-series analysis, which, like a case-crossover analysis, uses each case as its own comparator, the present study did not detect an association between fluoroquinolone exposure and the risk of retinal detachment. |
1 Introduction
A recent nested case–control study [1] from administrative claims data for British Columbia, Canada, observed that “patients taking oral fluoroquinolones were at a higher risk of developing a retinal detachment compared with non-users, although the absolute risk for this condition was small.” The study identified current use of fluoroquinolones in 145 cases (3.3 %) and 275 controls (0.6 %) for an adjusted rate ratio of 4.50 (95 % CI 3.56–5.70). It also reported the absence of an association of retinal detachment (RD) with recent use of fluoroquinolones, past use of fluoroquinolones, any use of β-lactam antibiotics, and current use of β-lactam antibiotics, suggesting the fluoroquinolone-associated risk was specific to fluoroquinolones and short-term. Of the cases with current, recent, or past exposure to a fluoroquinolone, 82.7 % were exposed to ciprofloxacin. The publication did not stratify its adjusted rate ratio estimate by individual fluoroquinolone. A more recent study from Denmark reported that exposure to oral fluoroquinolones was not associated with an increased risk of RD [2].
Our primary objective was to replicate the Canadian study [1] described above in additional databases. Secondary objectives were to determine whether the association observed in that study was specific to ciprofloxacin or was seen with all fluoroquinolones, confirm the absence of an association between exposure to β-lactam antibiotics and RD, assess the relationship of individual fluoroquinolones to RD, and address some potential confounders that may have affected the finding of the Canadian study. We therefore replicated that study’s case–control analysis in two large US administrative claims databases, performed a second case–control analysis that adjusted for several additional potential confounders, performed a third case–control analysis that removed a restriction on cohort entry (a requirement for a prior visit to an ophthalmologist), and stratified our results by individual fluoroquinolone. We also conducted a case-only analysis to address possible confounders, such as smoking or body mass index, that vary substantially across individuals but vary relatively little over time within individual and are not usually well-captured in claims databases. Because we were uncertain whether the results of the Canadian study reflected an association with ciprofloxacin or with all fluoroquinolones, we assessed each of these two exposures separately in our case–control analyses. We repeated the analyses in two databases and used more than one analytic approach because recent work [3, 4] suggests that results of retrospective studies from healthcare databases vary by database and by analytic method. The approach we adopted allowed us to establish, within such variation, a range of plausible values for the estimates.
2 Methods
We conducted retrospective analyses in two databases: the MarketScan Commercial Claims and Encounters (CCAE) database, 1 January 2000 to 31 January 2012, representing 91 million US patients with an average of 25 months of observation; and the Optum ClinFormatics (Optum) database, 1 September 2005 to 31 March 2012, representing 34 million US patients with an average of 27 months of observation. Each database represents administrative claims for a privately insured population, and includes information on inpatient and outpatient medical services and pharmacy dispensing claims. All analyses were performed using SAS® version 9.2 (SAS Institute Inc., Cary, NC, USA). Except as noted below, all analyses were done in accordance with a protocol that was developed in advance, though this protocol was modified several times during conduct of the study, usually because of ambiguities identified as computer programs were developed to conduct the analyses. Such modifications were done before generating the results they would affect.
Calculation of the minimum detectable relative risk (the smallest relative risk for which the data are sufficiently powered at alpha = 0.05 and power = 0.80) [5] suggested each database had a sufficient sample to identify relative risks ≥1.1 for any exposure (current, recent, or past) to ciprofloxacin or levofloxacin, and relative risks ≥2.0 for moxifloxacin, gatifloxacin, gemifloxacin, ofloxacin, and norfloxacin. When the term “fluoroquinolones” or “all fluoroquinolones” is used in this report it means an oral formulation of any of these seven medications.
2.1 Case–Control Analyses
2.1.1 Eligibility and Index Date
For the replication case–control analysis, patients entered the study cohort on the day of their first ophthalmologic visit and became eligible to be cases or controls after spending at least 1 year in the cohort, ignoring breaks of up to 30 days. This year of observation allowed identification of exclusion criteria and confounders. Patients left the cohort at the first of the following: meeting any exclusion criterion; having a diagnosis of RD; having a procedure to treat RD; or reaching the end of the study period for their database. Cases were those who had an RD as defined below. The index date (the estimated date of incidence of RD) for cases was the date of the first diagnosis of RD, and for controls was the index date of the corresponding case. Up to ten controls, randomly selected from those eligible, were matched to each case on index date, age (±1 year) as of the index date, and month and year of cohort entry.
2.1.2 Outcome
As in the Canadian study [1], a patient was considered to have an RD if he/she received a diagnosis of RD and a procedure for RD, e.g., surgery consisting of a sclera buckle, a vitrectomy, retinopexy, retinal cryotherapy, silicone oil fill, air gas fluid exchange (AGFE), or pneumatic retinopexy within 14 days after the diagnosis.
2.1.3 Exposure
For each oral antibiotic of interest, exposure was classified such that the case/control index date had to be included in the intervals defined as follows:Current use: from the day after the date of dispensing through the date of dispensing plus the number of days’ supply.Recent use: from the day after the last day of current use through 7 days after the last day of current use.Past use: from the day after the last day of recent use through 365 days after dispensing.Non-use: all person time not classified as current, recent, or past use.For example, the exposure status of a subject whose index date was 10 days after a dispensing of 7 days of a fluoroquinolone would be recent use.
2.1.4 Exclusion
Patients who met any of the following criteria between cohort entry and the index date were excluded: a diagnostic or procedure code for RD between cohort entry and the day before the index date (to assure cases were incident); an index date that fell during a hospitalization or within 10 days after hospital discharge (to avoid current or recent exposures that were initiated during hospitalizations); or a diagnosis of endopthalmitis or a procedure code related to endopthalmitis—including vitreous biopsy or intravitreal injection of a therapeutic agent (to avoid including subjects with this strong risk factor for RD).
2.1.5 Confounders
Potential confounders addressed in this analysis were sex, and, in the year prior to the index date, a diagnosis of myopia, diabetes mellitus (defined by use of an anti-diabetic medication), number of ophthalmologist visits, cataract surgery, and, as a measure of general health, the number of distinct drug ingredients (active pharmaceutical substances) dispensed. Unless stated otherwise, confounders were assessed over the 365 days prior to the index date.
2.1.6 Revised Case–Control Analysis
The revised case–control analysis was the same as the replication case–control analysis, with the following exceptions: additional exclusions for a diagnosis or procedure code related to inflammatory, infectious, or traumatic retinitis between cohort entry and the index date (to avoid including patients who had these strong risk factors for RD); an index date that fell during current or recent exposure to more than one fluoroquinolone or both a fluoroquinolone and a β-lactam antibiotic (to avoid ambiguities in exposure classification); and a hospital admission between cohort entry and the index date (to avoid missing information from the hospitalization that could have affected exposure status, confounders, or exclusion criteria). Cases and controls were matched on the same characteristics as in the replication case–control analysis, and were also matched on sex (to avoid the need to adjust for sex as was done in the replication case–control study). The list of RD diagnoses for purposes of identifying the outcome (RD) was shortened to exclude International Classification of Diseases (ICD) 361.2 (serous RD), which is typically associated with inflammatory conditions or with ophthalmologic inflammation, tumor, or vascular diseases, ICD 361.22 (Harada’s disease), which is an inflammatory condition, and ICD 361.81 (traction detachment of retina), which is typically due to contraction of a scar on the surface of the retina. These were excluded because they occur by mechanisms that differ from rhegmatogenous RD, the most common type, which is due to a break or tear in the retina [6]. In all analyses, exclusion of subjects for prior RD was based on the broader list used in the replication case–control analysis. The confounders addressed in the replication case–control analysis were addressed in the revised case–control analysis, but additional potential confounders were also addressed: history of any diabetic retinopathy; history of proliferative diabetic retinopathy; recent history (in the 30 days prior to the index date) of iridotomy or iridectomy; and recent history of eye injury.
2.1.7 Sensitivity Analysis
The sensitivity analysis was identical to the revised case–control analysis except that subjects were not required to have an ophthalmologist visit before they became eligible to be cases or controls. Thus, they entered the cohort when they entered the database, and, if they didn’t meet any of the exclusion criteria, became eligible to be cases or controls a year later. We believed the ophthalmologist visit requirement excluded many subjects and could be dropped, and study power increased, without materially changing the point estimates for the association of fluoroquinolones with RD.
All case–control analysis applied multivariate conditional logistic regression, conditioned on the case–control matching, to estimate adjusted odds ratios (ORs) and associated 95 % confidence intervals.
2.2 Self-Controlled Case-Series (SCCS) Analyses (Case-Only Analyses)
The self-controlled case-series (SCCS) analyses are similar to case-crossover analyses, in which each case serves as his or her own control. Such analyses implicitly adjust for many potential confounders, e.g., body mass index and health behaviors that are not captured, or are poorly captured, in most health services databases, and thus may be the optimal perspective for assessing the relationship of fluoroquinolone exposure to RD. The SCCS analyses were performed using the cases from the sensitivity analysis, with 30 days after the start of exposure to any fluoroquinolone, ciprofloxacin, or levofloxacin as the time-at-risk and prior time as the reference period. Inclusion and exclusion criteria were similar to those in the sensitivity case–control analysis.
3 Results
3.1 Replication Case–Control Analysis
The study cohorts consisted of 6,518,408 subjects in the CCAE database and 3,233,453 in the Optum database. The numbers of cases and matched controls and their characteristics are described in Table 1. In both databases, cases were more likely than controls to be male, have had cataract surgery (almost tenfold more likely), myopia, diabetes, more ophthalmologic visits, and more medications dispensed (Table 1), and more likely to be exposed to a fluoroquinolone (Table 2). In both databases, the adjusted ORs associated with any exposure to fluoroquinolones or ciprofloxacin were approximately 1.2 and were statistically significant. In the CCAE database, the adjusted ORs for current exposure to any fluoroquinolone or ciprofloxacin were also modestly above 1, approximately 1.3, and were not statistically significant. In the Optum database the ORs for current exposure to any fluoroquinolone or ciprofloxacin were 0.9 and were not statistically significant. In both databases, the adjusted ORs associated with any exposure or current exposure to β-lactam antibiotics were above 1, not statistically significant, and consistent with those observed for fluoroquinolones (Table 2).
3.2 Revised Case–Control Analysis
The cases and controls for the revised case–control analysis came from the same cohorts as in the above analysis and are described in Table 1. Though cases and controls were matched on sex, the proportion of males among cases and controls were similar but not identical because not all cases could be matched to ten controls. In both databases, cases were more likely than controls to have had cataract surgery, myopia, eye injury, diabetic retinopathy, proliferative diabetic retinopathy, had more medications dispensed (Table 1), and were more likely to be exposed to a fluoroquinolone (Table 3). Unlike the replication case–control analysis, in this analysis and the sensitivity analysis described below, the proportion of cases with diabetes was not substantially different from the proportion of controls with diabetes. Diabetes is associated with hospital admission and examination of the steps at which potential subjects were screened out indicated a substantial number of potential subjects were excluded from the revised case–control analysis and the sensitivity analysis due to hospital admission between cohort entry and index date. In the CCAE database, the adjusted ORs for any exposure or current exposure to any fluoroquinolone or ciprofloxacin ranged from 1.1 to 1.4 and were not statistically significant. In the Optum database, the OR for any exposure to any fluoroquinolone was 1.3 and was statistically significant. The adjusted ORs for current exposure to any fluoroquinolone and for current or any exposure to ciprofloxacin were not statistically significant, were not substantially above 1, and were not substantially higher than the adjusted ORs for β-lactam antibiotics (Table 3). Except for any exposure to levofloxacin in the Optum database, the adjusted ORs for any exposure or current exposure to levofloxacin and moxifloxacin were consistent with random variation (Table 4). There were no cases with current exposure to gatifloxacin, gemifloxacin, ofloxacin, or norfloxacin, and none of the adjusted ORs for any exposure to any of these fluoroquinolones was statistically significantly different from 1 (data not shown).
3.3 Sensitivity Analysis on the Revised Case–Control Analysis
In the sensitivity analysis on the revised case–control analysis there was no requirement for an ophthalmologist visit prior to the diagnosis of RD. The study cohorts consisted of 91,343,346 subjects in the CCAE database and 34,646,669 in the Optum database. The numbers of cases and controls and their characteristics are described in Table 1, and their exposure status is described in Tables 5, 6. Based on the controls, the most frequently used fluoroquinolones were ciprofloxacin, levofloxacin, and moxifloxacin. In both databases, cases were more likely than controls to have had cataract surgery, myopia, eye injury, diabetic retinopathy, proliferative diabetic retinopathy, and more medications dispensed (Table 1), and to be exposed to a fluoroquinolone (Tables 5 and 6). In the CCAE database, the adjusted OR for any exposure to any fluoroquinolone was 1.05 (1.04 in the revised case–control analysis), current exposure to any fluoroquinolone was 1.39 (1.40 in the revised case–control analysis), any exposure to ciprofloxacin was 1.09 (1.12 in the revised case–control analysis), and current exposure to ciprofloxacin was 1.33 (1.15 in the revised case–control analysis) (see Tables 3 and 5). In the Optum database, the OR for any exposure to any fluoroquinolone was 1.12 (1.30 in the revised case–control analysis), current exposure to any fluoroquinolone was 1.19 (0.37 in the revised case–control analysis based on only two exposed cases), any exposure to ciprofloxacin was 1.15 (1.16 in the revised case–control analysis), and current exposure to ciprofloxacin was 1.68 (zero in the revised case–control analysis) (see Tables 3 and 6). As in the revised case–control analysis, the ORs for β-lactam antibiotics were close to 1.
The ORs for any exposure or current exposure to levofloxacin and for moxifloxacin were not statistically significant (Tables 5, 6), and nor were the ORs for gatifloxacin, gemifloxacin, norfloxacin, or ofloxacin, with substantially fewer exposed cases (data not shown).
3.4 SCCS Analyses
Consistent with the case–control studies, the SCCS analyses did not detect associations between RD and exposure to fluoroquinolones, ciprofloxacin, or levofloxacin in either the CCAE or Optum database. All rate ratios were between 0.65 and 1.17, and none was statistically significant, although the rate ratio associated with exposure to any fluoroquinolone in the CCAE database narrowly missed this criterion (rate ratio 1.13, 95 % CI 0.99–1.29) (Table 7).
3.5 Additional Analyses
To understand features of our replication case–control analysis that might explain the difference between our findings and those of the recent Canadian publication [1], we performed three additional analyses not included in the study protocol. First, in the replication analysis we had treated the number of distinct drug ingredients dispensed in the past year as a categorical variable, in quintiles. As a sensitivity analysis we treated it as a linear variable. Second, in the replication analysis we had excluded any RD that was a hospital discharge diagnosis or was diagnosed within the 10 days after hospitalization. As a sensitivity analysis we made no such exclusion and defined the exposure status during hospitalization as the exposure status at hospital admission. Neither of these sensitivity analyses yielded results appreciably different from those of the replication case–control analysis.
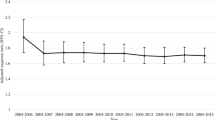
Finally, because our populations were appreciably younger than the population in the previous study (mean age 55 and 52 years for the replication and sensitivity case–control analyses from the CCAE database, respectively; 58 and 54 years for the corresponding analyses from the Optum database, vs. 61 years in the Canadian study), we stratified the estimates from the replication and sensitivity case–control analyses by age to assess whether age may have contributed to the difference in findings. The age quintiles were based on the cases and age-matched controls in the main case–control analyses. In the CCAE database, the estimates for current exposure to any fluoroquinolone and for current exposure to ciprofloxacin from the sensitivity analysis showed a clear and substantial increase in the adjusted OR with age (Table 8). None of the other age-stratified estimates from either database did so, but the numbers of fluoroquinolone-exposed cases in the estimates from the Optum database were relatively small (Tables 8, 9).
4 Discussion
We attempted to replicate, in two large US databases, the findings of a Canadian study of British Columbia administrative claims that found a substantial increased risk of RD during current use of fluoroquinolones. In both US databases and across all analyses performed, we were unable to identify a risk of similar magnitude. All our point estimates for the adjusted ORs associated with any exposure or current exposure to fluoroquinolones and to ciprofloxacin were below 1.5, and many had confidence intervals whose lower end fell below 1 and whose upper end was below 2. In contrast to the Canadian study [1], the ORs associated with fluoroquinolones were not strikingly different from those associated with β-lactam antibiotics. The SCCS analyses, which adjust for confounders that are not well captured in most health services databases, did not show a statistically significant association, suggesting the modest association found in some of the case–control analyses may have been due to confounding. Thus, in contrast to the Canadian study [1], the present study suggests no substantial increase in the incidence of RD is associated with exposure to oral fluoroquinolones. The present study also identified no significant differences in the incidence of RD among the three most widely used fluoroquinolones: ciprofloxacin, levofloxacin, and moxifloxacin. The results of the Canadian study [1] raised concerns about the safety of fluoroquinolones [7] that are not supported by the results of the current study.
Patients in the present study were younger than those in the previous study [1] and a smaller proportion had prior cataract surgery. Both studies addressed age through matching and cataract surgery by adjustment, so these differences do not appear to explain the difference in their findings. Nonetheless, the possibility remained that the difference in findings might be due to an association of RD with fluoroquinolone exposure that was entirely or mainly confined to the older subjects and therefore was observed in the previous study but missed in the present study with its younger population. We therefore stratified our estimates by quintile of age and found a clear increase in the adjusted OR for current exposure to any fluoroquinolone or to ciprofloxacin with age in the sensitivity analysis on the CCAE database, but in none of the other age-stratified analyses. This suggests the possibility of an association of RD risk with current exposure to ciprofloxacin, or to any fluoroquinolone, in the elderly. However, the evidence for this from the present study is not conclusive. This finding was in the context of examining many hypotheses and reflected a subgroup analysis from a broader analysis that did not show an association, and thus may have produced an association that cannot be replicated.
Both the Canadian study and the present study defined recent exposure as the 7 days after the end of current exposure. Comparison of the prevalence of current fluoroquinolone exposure to recent fluoroquinolone exposure among controls in the Canadian study suggested the mean duration of current exposure was approximately 21 days. A similar comparison in the replication case–control analysis in the present study suggested a mean duration of current exposure of 9–10 days. However, in the Canadian study the mean time from the start of fluoroquinolone exposure to the diagnosis of RD was 4.8 days, so the substantially shorter duration of use of fluoroquinolones in the present study does not seem likely to explain the difference in the findings of the two studies.
In addition to the usual limitations of any retrospective study, e.g., the possibility of unmeasured confounders, and questions about whether associations are causal, this study had the following specific limitations. It is unknown whether, or to what extent, the CCAE and Optum databases may overlap. To the extent that they do so, the analyses in the two databases would not be independent. To the extent that the dates of RDs or the start and end dates of exposure to the medication of interest are inaccurately recorded, their associations will also be inaccurately estimated. This may happen if RDs are diagnosed late, or the date of dispensing or using antibiotics differs from the date of the bill, or the date of end of use of antibiotics differs from the calculated date. A possible explanation for the difference in findings between the prior Canadian study and our replication is differential data capture across different health systems, as the Canadian study was based on claims processing in British Columbia, where, for example, the prevalence of recent cataract surgery was substantially higher and the median number of medications dispensed was substantially larger than in the privately insured US populations we studied. The inability to adjust for possible confounders not captured in the database (e.g., education), limited ability to adjust for diagnoses that may be under-reported (e.g. myopia), and adjustment in broad categories (e.g., diabetes present or absent) may leave appreciable confounding by these factors even in the adjusted estimates, especially in the case–control analyses. Confounding by many of these factors is better controlled in the SCCS analyses, in which each subject serves as his or her own comparator. Finally, the generalizability of the results is limited by the features of the study population that differ from the population at large and may be relevant to any observed association, e.g., the subjects in the present study were privately insured and were far more likely than the general population to be aged less than 65 years.
5 Conclusions
Though it examined two large databases using multiple analytic approaches, including one that mimicked the analysis used by the recent Canadian study, the present study does not confirm the recent Canadian study’s finding of a strong relationship between RD and current exposure to fluoroquinolones. The present study found a modest association between RD and current or recent exposure to fluoroquinolones in the case–control analyses, an association that was statistically significant in some, but not all, of the case–control analyses, and a possible relationship between RD and current fluoroquinolone exposure among the older subjects. In the SCCS analyses, the analyses that may be the least subject to confounding because they compared each subject to his or her own experience, the present study did not find an association between fluoroquinolones and RD.
References
Etminan M, Forooghian F, Brophy JM, Bird ST, Maberley D. Oral fluoroquinolones and the risk of retinal detachment. JAMA. 2012;307:1414–9.
Pasternak B, Svanstrom H, Melbye M, Hviid A. Association between oral fluoroquinolone use and retinal detachment. JAMA. 2013;310:2184–90.
Madigan D, Ryan P. What can we really learn from observational studies? The need for empirical assessment of methodology for active drug safety surveillance and comparative effectiveness research. Epidemiology. 2011;22:629–31.
Madigan D, Ryan PB, Schuemie M, Stang PE, Overhage JM, Hartzema AG, et al. Evaluating the impact of database heterogeneity on observational study results. Am J Epidemiol. 2013;178:645–51.
Armstrong B. A simple estimator of minimum detectable relative risk, sample size, or power in cohort studies. Am J Epidemiol. 1987;126:356–8.
Schwartz SG, Flynn HW Jr, Mieler WF. Update on retinal detachment surgery. Curr Opin Ophthalmol. 2013;24:255–61.
Han DP, Szabo A. Flashes, floaters, and oral fluoroquinolones. Arch Ophthalmol. Epub 2012 Sep 1:1–3.
Acknowledgments
We would like to thank Mahyar Etminan for responding to our questions about several details of his study and for reviewing our study protocol and the results of the replication analysis as we and he attempted to understand the reasons why the results of these two studies differed.
Conflict of interest
At the time of the study Daniel Fife, Vivienne Zhu, Erica Voss, and Patrick Ryan were full-time employees of Janssen Pharmaceutical Research and Development, LLC, 1125 Trenton-Harbourton Road, Titusville, NJ 08560, USA, and Grace Levy-Clarke was a full-time employee of Vistakon, 7500 Centurion Parkway #100, Jacksonville, FL 32256, USA. Both Janssen Pharmaceutical Research and Development and Vistakon are units of Johnson & Johnson, which markets levofloxacin, a fluoroquinolone. All the authors had pension rights with Johnson & Johnson, and all except Vivienne Zhu held stock. Daniel Fife, Vivienne Zhu, Erica Voss, Grace Levy-Clarke, and Patrick Ryan have no other conflicts of interest that are directly relevant to the conduct of this study. The study was performed as part of the authors’ regular work and no specific funding was received to conduct it.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Fife, D., Zhu, V., Voss, E. et al. Exposure to Oral Fluoroquinolones and the Risk of Retinal Detachment: Retrospective Analyses of Two Large Healthcare Databases. Drug Saf 37, 171–182 (2014). https://doi.org/10.1007/s40264-014-0138-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-014-0138-y