Abstract
Background
Many patients with chronic migraine do not achieve clinically meaningful improvement in their headache frequency with monotherapy. The burden associated with chronic migraine calls for a multifaceted treatment approach targeting multiple aspects of migraine pathophysiology.
Objective
The aim of this study was to evaluate the effect of concurrent anti-calcitonin gene-related peptide (CGRP) monoclonal antibody (mAb) and onabotulinumtoxinA (onabot) treatment on median monthly migraine days (MMD) in patients with chronic migraine, through a retrospective study.
Methods
The electronic medical records of Cleveland Clinic patients either concurrently (dual therapy) or consecutively (monotherapy) treated with anti-CGRP mAbs and onabot between June 2018 and November 2021 were extracted. Only adult patients (≥ 18 years of age) were included in this study. MMDs for 194 concurrently treated (86.6% female and a median [interquartile range] age of 51 [41–61] years) and 229 consecutively treated (88.2% female and median age of 47 [IQR 39–57] years) patients were examined at baseline, after first therapy of either anti-CGRP mAb or onabot, and following dual therapy for 3 consecutive months. The reduction of MMDs for each treatment group were compared. The same approach was utilized to compare consecutive monotherapy at separate times (n = 229) and dual-therapy groups.
Results
The initial treatment of the dual-therapy group reduced the median (IQR) MMDs from 30 (30–30) to 15 (12–30) [p < 0.0001]. After initiation of dual therapy, the median MMDs was further decreased from 15 (12–30) to 8 (3–22) [p < 0.0001]. A majority [132/194 (68.0%)] of the dual-therapy patients reported a ≥ 50% reduction in MMD and 90/194 (46.4%) reported a ≥ 75% reduction. For the consecutive monotherapy group, median MMDs changed from a baseline of 30 (25–30) to 15 (8–25) from onabot monotherapy and decreased from 25 (15–30) to 12 (4–25) after anti-CGRP mAb monotherapy. Almost half (113/229 [49.3%] from onabot, and 104/229 [45.4%] from anti-CGRP mAb) of these patients achieved a ≥ 50% reduction in MMDs and a minority (38/229 [16.6%] from onabot, and 45/229 [19.7%] from anti-CGRP mAb) achieved a reduction of ≥ 75%. Additionally, dual therapy showed significant improvement in MMDs compared with monotherapy of either treatment (p < 0.0001).
Conclusion
Dual therapy of anti-CGRP mAbs and onabot may be more efficacious than monotherapy, possibly due to their synergistic mechanisms of action.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The baseline migraine days per month decreased after initiation of the first therapy (anti-calcitonin gene-related peptide (CGRP) monoclonal antibodies or onabotulinumtoxinA), and led to a further decrease in migraine days with the addition of the second therapy. |
The migraine days before treatment had a median (interquartile range) of 30 (30–30) days per month, which decreased to 15 (12–30) migraine days after the first therapy and fell to 8 (3–22) migraine days after dual therapy. However, monotherapy of onabotulinumtoxinA changed from 30 (25–30) to 15 (8–25) monthly migraine days, and the migraine days per month decreased from 25 (15–30) to 12 (4–25) with anti-CGRP monoclonal antibody monotherapy. |
Combined treatment of anti-CGRP monoclonal antibodies and onabotulinumtoxinA were more beneficial than monotherapy alone when examining the total reduction in monthly migraine days. |
1 Introduction
Migraine is the second most disabling condition worldwide and affects approximately 12% of the population [1, 2]. Chronic migraine is associated with impairment in quality of life, increased medical and psychiatric comorbidities, and accounts for significant health resource utilization [1,2,3]. Many patients with chronic migraine do not achieve clinically meaningful improvement in their headache frequency and intensity with monotherapy [4]. Therefore, the immense burden associated with chronic migraine calls for a multifaceted treatment approach targeting multiple aspects of migraine pathophysiology in an effort to improve patient outcomes.
The first class of preventive medications specific to migraine pathophysiology, the anti-calcitonin gene-related peptide (CGRP) monoclonal antibodies (mAbs), gained US FDA approval in 2018 [5, 6]. Since the first anti-CGRP mAb was approved, the number has increased to four in total: erenumab, fremanezumab, galcanezumab, and eptinezumab [5,6,7,8,9,10,11]. The European Headache Federation (EHF) found sufficient evidence to recommend the four anti-CGRP mAbs for the treatment of episodic and chronic migraine. Additionally, they suggest anti-CGRP mAbs be a first-line treatment option for individuals who require preventative care [12]. CGRP is a 37 amino acid peptide that has a critical role in migraine pathophysiology [13]. CGRP receptors are present throughout regions involved in migraine pathogenesis, including the meningeal vasculature, trigeminal ganglia, and other numerous sites throughout the peripheral and central nervous system [13, 14]. CGRP is released from trigeminal axons onto meningeal blood vessels, causing vasodilation and activation of trigeminal neurons. CGRP is released in the trigeminal ganglion by C-fibers and binds to receptors on Aδ-fibers and glial cells facilitating trigeminal nociceptive transmission and triggering proposed neurogenic inflammation [13]. CGRP levels have been demonstrated to rise during migraine attacks and fall interictally as well as after abortive treatment [15,16,17]. Patients with migraine have higher levels of serum CGRP than controls, and infusion of CGRP precipitates migraine-like headaches [17, 18].
OnabotulinumtoxinA (onabot) was first demonstrated to have an effect on migraine when being used in patients for hyperfunctional lines of the face [19]. This finding led to the first open-label, non-randomized study in 2000 [20]. Onabot gained FDA approval for chronic migraine in 2010 after the PREEMPT trials showed significant reduction in headache days [21, 22]. The EHF recommends onabot as a preventative treatment option for chronic migraine [23]. Onabot acts by cleaving soluble N-ethylmaleimide-sensitive fusion attachment protein (SNAP-25), an essential protein for soluble N-ethylmaleimide-sensitive fusion attachment protein receptor (SNARE)-mediated vesicle trafficking [23,24,25,26,27]. Vesicle fusion with the inner synaptic membrane inhibited by onabot impacts migraine pathology by preventing the exocytosis of excitatory and pro-inflammatory neurotransmitters, such as CGRP, glutamate, and substance P. Additionally, this inhibits the insertion of the peripheral receptors (e.g. transient receptor potential cation channel subfamily V member 1 [TRPV1]), into the synaptic membrane, which are vital for pain signaling [27].
Onabot has been demonstrated to selectively inhibit unmyelinated C-fibers but not Aδ-meningeal nociceptors [28,29,30]. The anti-CGRP mAbs that target the CGRP peptide have been shown to prevent the activation of Aδ-fibers but not C-fibers [31]. Therefore, concurrent use of anti-CGRP mAbs with onabot may have a synergistic effect with targeting both Aδ-fibers and C-fibers. Previous studies have demonstrated that anti-CGRP mAbs and onabot may be efficacious in combination for the treatment of migraine [32,33,34,35]. We hypothesize that the possible synergistic mechanisms of onabot and anti-CGRP mAbs will result in improved treatment outcomes and reduced migraine frequency for patients with chronic migraine when compared with monotherapy.
2 Methods
All patients included in this study received a diagnosis, had appointment notes written, and had drugs prescribed by the United Council for Neurologic Subspecialties (UCNS) board-certified headache providers at the Cleveland Clinic. The patients’ self-reported MMD data were extracted from templated Epic appointment notes that were recorded by their providers. Thus, there is consistency in data reported despite a variety of different headache providers treating the patients.
2.1 Dual-Therapy Dataset
Inclusion in the dual-therapy dataset required patients be at least 18 years of age, have an official migraine diagnosis, completed a minimum of 3 consecutive months of concurrent anti-CGRP mAbs and onabot injections (between June 2018 and November 2021), and had their monthly migraine days (MMDs) recorded at baseline, after the first therapy and after dual therapy. Although the inclusion criteria include any migraine diagnosis, in order to qualify for these preventative treatments in general and receive dual therapy, the patients have likely not responded to multiple previous medications and have chronic migraine. The inclusion criteria were confirmed with a thorough chart review for each patient; 194 individuals met the study criteria and were included in the final dual-therapy group (Fig. 1). In addition to MMDs, clinical data such as the specific anti-CGRP mAbs prescribed, length of time on first therapy before dual therapy was initiated, early onabot wearing off, and migraine diagnosis (with or without aura) were extracted from the EPIC systems. Demographic data, including sex, age, and race, were gathered from EPIC for the entire sample.
Description of dataset analyzed. The first analysis was completed among the dual-therapy group. An additional analysis compared a separate consecutive monotherapy group with the dual-therapy dataset. Anti-CGRP mAb anti-calcitonin gene-related peptide monoclonal antibodies, MMDs monthly migraine days, onabot onabotulinumtoxinA
2.2 Dual-Therapy Analysis
The dual-therapy dataset consisted of 194 patients with concurrent onabot and anti-CGRP mAb therapies. Additionally, to determine if the order of therapies impacts response outcomes, the dataset was separated into patients started on onabot first before dual therapy (n = 171) and patients with anti-CGRP mAb treatment before dual therapy (n = 23). The sample size was based on the available data. No imputation was conducted for the dual-therapy group as there were no missing data for all variables extracted and evaluated. The primary analysis of these data compared the MMDs for the dual-therapy dataset among three time points: baseline, after first therapy, and after dual therapy. This same analysis was repeated separately for the onabot-first and the anti-CGRP mAb-first sub-datasets. A non-parametric test was determined most fitting for the data. A comparison of the three treatment time points was done using the Friedman test. To better understand which specific treatment time point differed from the others, the Dunn’s multiple comparison test was employed. We did not correct for multiple comparisons due to the exploratory nature of this study and therefore potential interesting findings were not missed. Additionally, the ‘reduction of MMDs’ or the difference of MMDs from baseline to the first therapy, was compared with the reduction of MMD after combined treatment with the Wilcoxon matched-pairs signed-rank test.
2.3 Consecutive Monotherapy Dataset
To further examine the impact of dual therapy, we identified a consecutive monotherapy group (individuals who received anti-CGRP mAbs and onabot separately) to serve as a comparator. The decision to use consecutive monotherapy patients as a comparison group was made to avoid individual differences in treatment response on a single treatment, and to ensure that all patients in the comparison group were good candidates for both onabot and anti-CGRP mAbs.
For the consecutive monotherapy group, the inclusion criteria were age ≥ 18 years, baseline and after treatment MMDs recorded, and treated with a minimum of three rounds of onabot and three monthly anti-CGRP mAb injections at separate times with no overlap. The exclusion criteria were concurrent treatment at any point in time and we required at least 3 months of separation after the last therapy (onabot or anti-CGRP mAb) before the next therapy was started, to limit any possible effect of the previous treatment. Each patient was confirmed to meet the inclusion criteria with a chart review; 229 patients were included in the consecutive monotherapy sample (Fig. 1).
2.4 Comparison of Consecutive Monotherapy and Dual Therapy
Similar to the dual-therapy dataset, consecutive monotherapy patients had no missing data for the variables extracted. Improvement was assessed through the reduction in MMD. The Kruskal–Wallis test compared MMD reductions among consecutive monotherapy patients while receiving onabot monotherapy, consecutive monotherapy patients while receiving anti-CGRP mAb monotherapy, and dual-therapy patients. Dunn’s multiple comparison test was used post hoc for pairwise comparisons. Lastly, to compare the reduction in MMDs between the dual-therapy group and the consecutive monotherapy group (MMD reduction following both consecutive monotherapies), a Mann–Whitney U test was used.
For all tests, a two-tailed p-value < 0.05 indicated significant differences. Unless noted otherwise, the median and interquartile ranges were used to report all study variables due to the non-parametric nature of the data. The 95% confidence intervals (CIs) were also reported. No statistical power calculation was conducted prior to the study. The Kruskal–Wallis, Dunn’s comparison, and Mann–Whitney U (two-tailed) tests were completed in GraphPad Prism version 9.4.0 (GraphPad Software, Inc., San Diego, CA, USA).
3 Results
3.1 Dual-Therapy Dataset
A retrospective review of Cleveland Clinic patients with prescriptions of both anti-CGRP mAb and onabot between June 2018 and November 2021 was completed for this study (Fig. 1). A total of 714 patients had an onabot and anti-CGRP mAb prescription within the time frame. This patient list was then separated into the dual-therapy (n = 194) and consecutive monotherapy (n = 229) datasets based on their specific inclusion criteria. Overall, 291 patients did not meet the criteria for either therapy group.
Demographic and clinical characteristics are summarized in Table 1. Among these patients, the median age was 51 (41–61) years and a majority of the patients were women (86.6%). With regard to migraine type, 164 (84.5%) patients experienced migraine without aura and 30 (15.5%) experienced migraine with aura. Regarding specific anti-CGRP treatment, 58.8% of patients were taking erenumab, 22.2% of patients were taking galcanezumab, and 19.1% of patients were taking fremanezumab. None of the patients in our dataset received eptinezumab. The majority of patients received dual therapy for > 6 months (81.4% [158/194]). The early diminishment in efficacy for onabot is a noted occurrence and a reason why dual therapy may be a beneficial approach for some patients. A total of 50.5% (98/194) of patients experienced wearing off from onabot. The wear-off occurred a median of 2 (2–4) weeks before the next cycle of injections.
3.2 Dual-Therapy Analysis
Patients were receiving their first therapy (with either onabot or anti-CGRP mAb) for a median of 1 (0.5–1.7) year prior to initiation of dual therapy (Table 1). When comparing MMDs at baseline to after first therapy with dual therapy, regardless of which therapy was used first, the first therapy reduced the median MMDs from 30 (30–30) to 15 (12–30) (Table 2). After initiation of dual therapy, the MMDs was further decreased to 8 (3–22). The reduction of MMDs was significant when comparing the first therapy and dual therapy (p < 0.0001) (Table 3, Fig. 2c). From baseline to following dual therapy, 132/194 (68.0%) patients reported a ≥ 50% reduction in MMD and 90/194 (46.4%) reported a ≥ 75% reduction (Table 2).
Monthly migraine frequency before and after therapies. a Baseline MMDs, MMDs after onabot first therapy, followed by changes in MMDs after a minimum of 3 months of dual therapy. b Baseline MMDs, MMDs after anti-CGRP mAbs-first therapy, followed by changes in MMDs after a minimum of 3 months of dual therapy. c Baseline MMDs, MMDs following first therapy (with either onabot or anti-CGRP mAbs), followed by changes in MMDs after a minimum of 3 months of dual therapy. All boxplot whiskers display the minimum to maximum values. Significance shown above. **** indicates p < 0.0001, ** indicates p < 0.01, ns indicates non-significant or p > 0.05. MMDs monthly migraine days, onabot onabotulinumtoxinA, anti-CGRP mAb anti-calcitonin gene-related peptide monoclonal antibodies
The majority of patients were receiving onabot first (88.1% [171/194]) and were receiving treatment for 1 (0.8–2.0) year prior to the initiation of concurrent anti-CGRP mAb dual therapy (Table 1). Onabot therapy-first reduced the MMDs from a median of 30 (30–30) to 19 (12–30) days (Table 2). After the addition of an anti-CGRP mAb to onabot, the median MMDs was further decreased from 19 (12–30) to 12 (3–20). The reduction was significant when comparing onabot therapy and dual therapy (p < 0.0001) (Table 3, Fig. 2a). From baseline to following dual therapy, 118/171 (69.0%) patients reported a ≥ 50% reduction in MMDs and 80/171 (46.8%) reported a ≥75% reduction (Table 2).
The 23 patients who were started on an anti-CGRP mAb first (11.9% [23/194]) were receiving treatment for an average of 0.4 (0.3–0.5) years prior to initiation of dual therapy (Table 1). Anti-CGRP mAb therapy reduced the median MMDs from 30 (20–30) to 15 (15–30) (Table 2). After the addition of onabot to the anti-CGRP mAb, the MMDs was further decreased from a median of 15 (15–30) to 7 (3–28). No significant difference was found between MMD at baseline and after anti-CGRP mAb first (p = 0.122), but this may be from the lack of power from the small sample size. However, there was a significant difference when comparing baseline MMD with dual therapy, and anti-CGRP mAb initial treatment with dual therapy (p < 0.0001 and p = 0.008, respectively) (Table 3, Fig. 2b). From baseline to following dual therapy, 14/23 (60.9%) patients reported a ≥ 50% reduction in MMD and 10/23 (43.5%) reported a ≥ 75% reduction (Table 2).
3.3 Consecutive Monotherapy Dataset
Overall, 229 patients met the criteria of consecutive monotherapy from the 714 patients with prescriptions of both onabot and anti-CGRP mAb (Fig. 1). The characteristics of the consecutive monotherapy group (n = 229) are summarized in Table 4. The median age for patients with consecutive monotherapy was 47 (39–57) years. Most of the patients in this group were female (88.2%). The dataset had 83.4% of patients diagnosed with migraine without aura. During their anti-CGRP mAb monotherapy, the specific mAbs used were erenumab for 63.8% of patients, galcanezumab for 19.2% of patients, and fremanezumab for 17% of patients.
3.4 Comparison of Consecutive Monotherapy and Dual Therapy
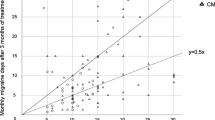
Within the consecutive monotherapy sample, onabot monotherapy decreased the MMDs from a baseline of 30 (25–30) to 15 (8–25). Anti-CGRP mAb monotherapy went from 25 (15–30) MMDs at baseline to 12 (4–25) MMDs (Table 4). A significant difference was found between the reduction of MMDs from anti-CGRP mAb monotherapy and onabot monotherapy (p = 0.04), dual therapy and anti-CGRP mAb monotherapy (p < 0.0001), and dual therapy compared with onabot monotherapy (p < 0.0001) (Table 5, Fig. 3). This difference was also seen when combining the two consecutive monotherapy groups and comparing with dual therapy using a Mann–Whitney test (p < 0.0001) (Table 5, Fig. 3b).
Reduction of MMDs for consecutive monotherapy groups (onabot and anti-CGRP mAb monotherapy) and dual therapy. a The reduction of MMDs for patients treated with onabot monotherapy, anti-CGRP mAb monotherapy, and those with concurrent onabot and anti-CGRP mAb—our dual-therapy cohort. b Monotherapy of anti-CGRP mAb or onabot compared with dual therapy of anti-CGRP mAb and onabot. All boxplot whiskers display the minimum to maximum values. Significance shown above. **** indicates p < 0.0001, * indicates p = 0.04. MMDs monthly migraine days, onabot onabotulinumtoxinA, anti-CGRP mAb anti-calcitonin gene-related peptide monoclonal antibodies
4 Discussion
Our results demonstrate that concurrent anti-CGRP and onabot therapy significantly reduces MMDs in chronic migraine patients treated at the Cleveland Clinic, when compared with monotherapy alone. These results were consistent when comparing the first therapy and dual therapy within a single group of patients who experienced both treatment conditions, as well as when comparing patients who received dual treatment with a separate group of patients who received consecutive monotherapy.
The prophylactic treatment of migraine has evolved dramatically with the addition of onabot in 2010, followed by the anti-CGRP mAbs beginning in 2018. Although concurrent use has been largely limited by insurance approval, there is surmounting evidence that their combined use leads to reduced headache frequency and disability. Our study is a retrospective chart review analyzing the concomitant use of onabot and anti-CGRP mAbs performed at one of the largest headache centers in the United States.
To date, the two largest real-world studies on combined use of anti-CGRP mAbs and onabot performed at private practice headache centers showed a reduction in monthly headache days (MHDs) [34, 35]. The study performed by Blumenfeld et al. (October 2018–November 2019 study timeline) demonstrated 25.7% (n = 218) of patients and 36.7% (n = 180) of patients experienced a ≥ 50% reduction in MHDs after approximately 3 and 6 months of dual therapy, respectively [34]. Similarly, the retrospective chart review (n = 148) performed by Mechtler et al. (June 2018–March 2020 study timeline) demonstrated that 21.2% of patients had a ≥ 50% reduction in MHD and 4.4% had a ≥ 75% reduction in MHD after 3 months of combined treatment with anti-CGRP mAbs and onabot [35]. In our study, we found that 68.0% (132/194) of patients had a ≥ 50% reduction in MMDs and 46.4% (90/194) had a ≥ 75% reduction in MMDs after a minimum of 3 months of dual therapy (Table 2). These studies may demonstrate a lower benefit of combined use of anti-CGRP mAbs and onabot, as our study focused on MMDs rather than MHDs, to better target and observe the impact on migraines specifically. Additionally, these studies looked specifically at anti-CGRP mAbs being added to onabot and did not include patients with anti-CGRP mAbs adding onabot; however, we included both routes of dual therapy. A retrospective cohort study by Nandyala et al. examining combined treatment of onabot and erenumab (n = 50) demonstrated that combined treatment presented a significantly lower number of MMDs than onabot treatment alone (11.3 ± 9.3 vs. 14.9 ± 9.4; p < 0.001) as well as a significantly lower number of MHDs than onabot treatment alone (18.2 ± 10.3 vs. 20.7 ± 9.1; p = 0.042) [36]; however, that study only looked at 1 month of combined use.
In our study, 58.8% (114/194) of the dual-therapy patients were prescribed erenumab, 22.2% (43/194) were prescribed galcanezumab, and 19.1% (37/194) were prescribed fremanezumab. In the aforementioned studies, 77.8% (200/257) of patients were prescribed erenumab, 16.3% (42/257) were prescribed galcanezumab, and 5.8% (15/257) were prescribed fremanezumab, while in the second study, 56.7% (84/148) of patients were prescribed erenumab, 0.7% were prescribed galcanezumab (1/148), and 42.6% were prescribed fremanezumab (63/148) [34, 35]. Therefore, our study has a higher percentage of patients receiving galcanezumab and fremanezumab, which bind the CGRP ligand, whereas erenumab binds to the receptor, which may reflect differences in outcomes.
Unlike the previous studies, we compared the dual-therapy dataset with a separate consecutive monotherapy group. There was a significant difference in the MMD reductions between monotherapy of onabot, anti-CGRP mAb monotherapy, and the dual-therapy groups (p < 0.0001). The MMD reduction comparison of onabot monotherapy and dual therapy proved significantly different (p < 0.0001) and anti-CGRP mAb and dual therapy were found to be significantly different (p < 0.0001). Overall, dual therapy shows improvement in MMDs compared with monotherapy of either treatment. In addition, we found a significant difference (p = 0.04) between anti-CGRP mAb monotherapy and onabot monotherapy, which may be because the onabot group is skewed towards people who took onabot for a longer time, which is more indicative of a strong positive response. Although, there is a larger median reduction of MMD from onabot monotherapy (10 [1–18] onabot vs. 7 [0–15.5]), we see a slightly higher percentage of anti-CGRP mAb monotherapy patients who experienced a ≥ 75% (16.6% onabot vs. 19.7% anti-CGRP mAb) improvement in MMD frequency. This may suggest that patients respond better to onabot generally, but those who benefit from anti-CGRP mAbs have larger margins of improvement.
Onabot is administered every 12 weeks according to the PREEMPT paradigm. However, a wear-off phenomenon has been demonstrated as early as week 8, prior to the next treatment session, resulting in increased moderate to severe migraine days, number of rescue medications used, and number of emergency room visits [37,38,39]. A retrospective chart review by Masters-Irailov and Robbins demonstrated wear-off in 62.9% (90/143) of patients receiving onabot for chronic migraine, most commonly 2–4 weeks prior to the next injection (43.3%) and after the very first injection (40.0%) [37]. Our study found 50.5% of patients experiencing wear-off at 2 (2–4) weeks prior to the next onabot injection. A retrospective chart review performed by Ozudogru et al. (n = 36) demonstrated that there is a potential benefit of anti-CGRP mAbs in delaying the wearing-off of onabot by an average of 2 weeks when used in combination, thus extending the therapeutic benefit of onabot [40].
Our study shows further evidence that concomitant use of anti-CGRP mAbs and onabot leads to improved migraine frequency. Due to the differences in administration and eptinezumab’s later FDA approval date, the anti-CGRP mAb intravenous infusion was not included in our patient population. Limitations of this study include the limited follow-up period (post-prescription follow-up appointments have predetermined timelines generally); the standard follow-up for both onabot and anti-CGRP mAbs is approximately every 3 months initially. However in practice, scheduling conflicts and availability of appointments may adjust or delay the follow-ups. In the chart review, the appointment timelines were noted and confirmed to have met the inclusion criteria. Additionally, there is variation of onabot administration among providers (ranging from 155 to 200 units within the muscle groups included in the PREEMPT protocol) that can introduce some noise into the dataset. Furthermore, the nature of a real-world retrospective chart review can be inaccurate or inconsistent. A thorough manual check of each individual patients’ charts was conducted to ensure the most accurate data were extracted, and the templated notes provided further consistency. The resulting datasets for the dual-therapy and consecutive monotherapy groups had no missing data. Of note, we also sought to evaluate whether sequence of therapy made a difference. Since anti-CGRP mAbs first gained FDA approval in 2018, the majority of patients were started on onabot first, and therefore the results in the anti-CGRP mAb-first group were likely limited by lack of power. Future randomized controlled trials should be considered to further assess their combined use.
5 Conclusions
Combination therapy of anti-CGRP mAbs and onabot is more efficacious than monotherapy in chronic migraine patients. Our study adds to the evidence that their combined use leads to a better reduction in migraine frequency and is the first to compare the treatment outcomes with a separate monotherapy patient population.
References
Burch RC, Buse DC, Lipton RB. Migraine. Neurol Clin. 2019;37(4):631–49. https://doi.org/10.1016/j.ncl.2019.06.001.
Leonardi M, Martelletti P, Burstein R, et al. The World Health Organization Intersectoral Global Action Plan on Epilepsy and Other Neurological Disorders and the headache revolution: from headache burden to a global action plan for headache disorders. J Headache Pain. 2024;25(1):4. https://doi.org/10.1186/s10194-023-01700-3.
Martelletti P, Leonardi M, Ashina M, et al. Rethinking headache as a global public health case model for reaching the SDG 3 HEALTH by 2030. J Headache Pain. 2023;24(1):140. https://doi.org/10.1186/s10194-023-01666-2.
Bigal M, Krymchantowski AV, Lipton RB. Barriers to satisfactory migraine outcomes. What have we learned, where do we stand? Headache. 2009;49(7):1028–41. https://doi.org/10.1111/j.1526-4610.2009.01410.x.
Tepper S, Ashina M, Reuter U, et al. Safety and efficacy of erenumab for preventive treatment of chronic migraine: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol. 2017;16(6):425–34. https://doi.org/10.1016/S1474-4422(17)30083-2.
Dodick DW, Ashina M, Brandes JL, et al. ARISE: a phase 3 randomized trial of erenumab for episodic migraine. Cephalalgia. 2018;38(6):1026–37. https://doi.org/10.1177/0333102418759786.
Detke HC, Goadsby PJ, Wang S, et al. Galcanezumab in chronic migraine: the randomized, double-blind, placebo-controlled REGAIN study. Neurology. 2018. https://doi.org/10.1212/WNL.0000000000006640.
Stauffer VL, Dodick DW, Zhang Q, et al. Evaluation of galcanezumab for the prevention of episodic migraine: the EVOLVE-1 randomized clinical trial. JAMA Neurol. 2018;75(9):1080. https://doi.org/10.1001/jamaneurol.2018.1212.
Silberstein SD, Dodick DW, Bigal ME, et al. Fremanezumab for the preventive treatment of chronic migraine. N Engl J Med. 2017;377(22):2113–22. https://doi.org/10.1056/NEJMoa1709038.
Ashina M, Saper J, Cady R, et al. Eptinezumab in episodic migraine: a randomized, double-blind, placebo-controlled study (PROMISE-1). Cephalalgia. 2020;40(3):241–54. https://doi.org/10.1177/0333102420905132.
Lipton RB, Goadsby PJ, Smith J, et al. Efficacy and safety of eptinezumab in patients with chronic migraine: PROMISE-2. Neurology. 2020. https://doi.org/10.1212/WNL.0000000000009169.
Sacco S, Amin FM, Ashina M, et al. European Headache Federation guideline on the use of monoclonal antibodies targeting the calcitonin gene related peptide pathway for migraine prevention—2022 update. J Headache Pain. 2022;23(1):67. https://doi.org/10.1186/s10194-022-01431-x.
Wattiez AS, Sowers LP, Russo AF. Calcitonin gene-related peptide (CGRP): role in migraine pathophysiology and therapeutic targeting. Expert Opin Ther Targets. 2020;24(2):91–100. https://doi.org/10.1080/14728222.2020.1724285.
Benarroch EE. CGRP: sensory neuropeptide with multiple neurologic implications. Neurology. 2011;77(3):281–7. https://doi.org/10.1212/WNL.0b013e31822550e2.
Edvinsson L, Fredholm BB, Hamel E, et al. Perivascular peptides relax cerebral arteries concomitant with stimulation of cyclic adenosine monophosphate accumulation or release of an endothelium-derived relaxing factor in the cat. Neurosci Lett. 1985;58(2):213–7. https://doi.org/10.1016/0304-3940(85)90166-1.
Goadsby PJ, Edvinsson L, Ekman R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol. 1990;28(2):183–7. https://doi.org/10.1002/ana.410280213.
Lassen L, Haderslev P, Jacobsen V, et al. Cgrp may play a causative role in migraine. Cephalalgia. 2002;22(1):54–61. https://doi.org/10.1046/j.1468-2982.2002.00310.x.
Ramón C, Cernuda-Morollón E, Pascual J. Calcitonin gene-related peptide in peripheral blood as a biomarker for migraine. Curr Opin Neurol. 2017;30(3):281–6. https://doi.org/10.1097/WCO.0000000000000440.
Escher CM, Paracka L, Dressler D, et al. Botulinum toxin in the management of chronic migraine: clinical evidence and experience. Ther Adv Neurol Disord. 2017;10(2):127–35. https://doi.org/10.1177/1756285616677005.
Binder WJ, Brin MF, Blitzer A, et al. Botulinum toxin type A (BOTOX) for treatment of migraine headaches: an open-label study. Otolaryngol Head Neck Surg. 2000;123(6):669–76. https://doi.org/10.1067/mhn.2000.110960.
Aurora S, Dodick D, Turkel C, et al. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia. 2010;30(7):793–803. https://doi.org/10.1177/0333102410364676.
Diener H, Dodick D, Aurora S, et al. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 2 trial. Cephalalgia. 2010;30(7):804–14. https://doi.org/10.1177/0333102410364677.
Bendtsen L, Sacco S, Ashina M, et al. Guideline on the use of onabotulinumtoxinA in chronic migraine: a consensus statement from the European Headache Federation. J Headache Pain. 2018;19(1):91. https://doi.org/10.1186/s10194-018-0921-8.
Blasi J, Chapman ER, Link E, et al. Botulinum neurotoxin A selectively cleaves the synaptic protein SNAP-25. Nature. 1993;365(6442):160–3. https://doi.org/10.1038/365160a0.
Rapp DE, Turk KW, Bales GT, et al. Botulinum toxin type A inhibits calcitonin gene-related peptide release from isolated rat bladder. J Urol. 2006;175(3):1138–42. https://doi.org/10.1016/S0022-5347(05)00322-8.
Lucioni A, Bales GT, Lotan TL, et al. Botulinum toxin type A inhibits sensory neuropeptide release in rat bladder models of acute injury and chronic inflammation. BJU Int. 2008;101(3):366–70. https://doi.org/10.1111/j.1464-410X.2007.07312.x.
Burstein R, Blumenfeld AM, Silberstein SD, et al. Mechanism of action of onabotulinumtoxinA in chronic migraine: a narrative review. Headache. 2020;60(7):1259–72. https://doi.org/10.1111/head.13849.
Durham PL, Masterson CG. Two mechanisms involved in trigeminal CGRP release: implications for migraine treatment. Headache. 2013;53(1):67–80. https://doi.org/10.1111/j.1526-4610.2012.02262.x.
Burstein R, Zhang X, Levy D, et al. Selective inhibition of meningeal nociceptors by botulinum neurotoxin type A: therapeutic implications for migraine and other pains. Cephalalgia. 2014;34(11):853–69. https://doi.org/10.1177/0333102414527648.
Zhang X, Strassman AM, Novack V, et al. Extracranial injections of botulinum neurotoxin type A inhibit intracranial meningeal nociceptors’ responses to stimulation of TRPV1 and TRPA1 channels: are we getting closer to solving this puzzle? Cephalalgia. 2016;36(9):875–86. https://doi.org/10.1177/0333102416636843.
Melo-Carrillo A, Strassman AM, Schain AJ, et al. Exploring the effects of extracranial injections of botulinum toxin type A on prolonged intracranial meningeal nociceptors responses to cortical spreading depression in female rats. Cephalalgia. 2019;39(11):1358–65. https://doi.org/10.1177/0333102419873675.
Melo-Carrillo A, Strassman AM, Nir RR, et al. Fremanezumab—a humanized monoclonal anti-CGRP antibody—inhibits thinly myelinated (Aδ) but not unmyelinated (C) meningeal nociceptors. J Neurosci. 2017;37(44):10587–96. https://doi.org/10.1523/JNEUROSCI.2211-17.2017.
Cohen F, Armand C, Lipton RB, et al. Efficacy and tolerability of calcitonin gene-related peptide-targeted monoclonal antibody medications as add-on therapy to onabotulinumtoxinA in patients with chronic migraine. Pain Med. 2021;22(8):1857–63. https://doi.org/10.1093/pm/pnab093.
Blumenfeld AM, Frishberg BM, Schim JD, et al. Real-world evidence for control of chronic migraine patients receiving CGRP monoclonal antibody therapy added to onabotulinumtoxinA: a retrospective chart review. Pain Ther. 2021;10(2):809–26. https://doi.org/10.1007/s40122-021-00264-x.
Mechtler L, Saikali N, McVige J, et al. Real-world evidence for the safety and efficacy of CGRP monoclonal antibody therapy added to onabotulinumtoxinA treatment for migraine prevention in adult patients with chronic migraine. Front Neurol. 2022;12: 788159. https://doi.org/10.3389/fneur.2021.788159.
Nandyala AS, Suri H, Dougherty CO, et al. A retrospective evaluation of the combination of erenumab and onabotulinum toxin A for the prevention of chronic migraine. Clin Neurol Neurosurg. 2022;215: 107200. https://doi.org/10.1016/j.clineuro.2022.107200.
Masters-Israilov A, Robbins MS. OnabotulinumtoxinA wear-off phenomenon in the treatment of chronic migraine. Headache. 2019;59(10):1753–61. https://doi.org/10.1111/head.13638.
Quintas S, García-Azorín D, Heredia P, et al. Wearing off response to onabotulinumtoxinA in chronic migraine: analysis in a series of 193 patients. Pain Med. 2019;20(9):1815–21. https://doi.org/10.1093/pm/pny282.
Zidan A, Roe C, Burke D, et al. OnabotulinumtoxinA wear-off in chronic migraine, observational cohort study. J Clin Neurosci. 2019;69:237–40. https://doi.org/10.1016/j.jocn.2019.07.043.
Ozudogru S, Bartell J, Yuan H, et al. The effect of adding calcitonin gene-related peptide monoclonal antibodies to onabotulinum toxin a therapy on headache burden: a retrospective observational case series. Headache J Head Face Pain 2020;60:1442–3. https://doi.org/10.1111/head.13839
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research was completed with funding from a Cleveland Clinic institutional grant.
Conflict of Interest
Amira Salim, Elise Hennessy, Claire Sonneborn, Olivia Hogue, Sudipa Biswas, MaryAnn Mays, Aarushi Suneja, Zubair Ahmed, and Ignacio F. Mata have no disclosures to declare relevant to this manuscript.
Ethics Approval
This study was approved by the Cleveland Clinic Institutional Review Board (CC IRB), and due to the use of pre-existing data, the CC IRB waived the written informed consent.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Data Availability
Due to reasons of patient data sensitivity, the data cannot be found openly available; however, the dataset will be anonymized and made available from the authors upon reasonable request from qualified investigators.
Code Availability
Not applicable.
Author Contributions
AS: Conceptualization, methodology, formal analysis, writing—original draft preparation, writing—review and editing, visualization. EH: Writing—original draft preparation, writing—review and editing, visualization. CS: Methodology, formal analysis, writing—review and editing. OH: Methodology, formal analysis, writing—review and editing. SBs: Writing—review and editing. MAM: Writing—review and editing, supervision. AS: Writing—review and editing. ZA: Conceptualization, writing—review and editing, supervision, funding acquisition. IFM: Writing—review and editing, supervision, project administration, funding acquisition.
Additional information
Elise Hennessy and Zubair Ahmed were affiliated with Cleveland Clinic at the time of this research.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Salim, A., Hennessy, E., Sonneborn, C. et al. Synergism of Anti-CGRP Monoclonal Antibodies and OnabotulinumtoxinA in the Treatment of Chronic Migraine: A Real-World Retrospective Chart Review. CNS Drugs 38, 481–491 (2024). https://doi.org/10.1007/s40263-024-01086-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-024-01086-z