Abstract
Introduction
Adequate antipsychotic treatment intensity is required before diagnosing resistant schizophrenia and initiating clozapine treatment. We aimed to investigate potential rapid drug metabolism underlying low dose-adjusted serum concentration (CD) of non-clozapine atypical antipsychotics preceding clozapine treatment.
Methods
Patients using non-clozapine, atypical antipsychotics (aripiprazole, risperidone, olanzapine, or quetiapine) within 1 year before starting clozapine were included in this study from a therapeutic drug monitoring service in Oslo, Norway, between 2005 and 2023. Patients were assigned into low CD (LCD) and normal CD (NCD) subgroups. Using a reference sample with 147,964 antipsychotic measurements, LCD was defined as CDs below the 25th percentile, while patients with NCD exhibited CDs between the 25th and 75th percentile of the respective reference measurements. Metabolic ratios, doses, and frequency of subtherapeutic levels of non-clozapine antipsychotics were compared between LCD and NCD groups.
Results
Preceding clozapine treatment, 110 out of 272 included patients (40.4%) were identified with LCD. Compared with the NCD group, LCD patients exhibited higher metabolic ratios of olanzapine (1.5-fold; p < 0.001), quetiapine (3.0-fold; p < 0.001), and risperidone (6.0-fold; p < 0.001). Metabolic ratio differences were independent of smoking and CYP2D6 genotype for olanzapine (p = 0.008) and risperidone (p = 0.016), respectively. Despite higher doses of olanzapine (1.25-fold; p = 0.054) and quetiapine (1.6-fold; p = 0.001) in LCD versus NCD patients, faster metabolism among the former was accompanied by higher frequencies of subtherapeutic levels of olanzapine (3.3-fold; p = 0.044) and quetiapine (1.8-fold; p = 0.005).
Conclusion
LCD and associated rapid metabolism of non-clozapine antipsychotics is frequent before starting clozapine treatment. For olanzapine and quetiapine, this is associated with significantly increased risk of having subtherapeutic concentrations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Rapid drug metabolism is frequent and significantly associated with risk of having subtherapeutic serum levels of olanzapine and quetiapine, possibly leading to insufficient clinical effect preceding clozapine treatment. |
The molecular mechanisms underlying the rapid drug metabolism are unclear and need to be investigated in further studies. |
Antipsychotic therapeutic drug monitoring with metabolite analyses may be valuable for clinical decision making of treatment-resistant schizophrenia and initiating clozapine treatment. |
1 Introduction
Schizophrenia usually requires long-term treatment with antipsychotic medication, however up to a third of patients with schizophrenia do not show sufficient clinical response to two trials of antipsychotic treatment and suffer from treatment-resistant schizophrenia (TRS) [1, 2]. Clozapine is the main drug indicated in treatment of TRS and is shown to have superior efficacy versus other antipsychotics in terms of clinical effect [3]. However, its use is limited to TRS due to risk of severe and potentially life-threatening side effects, such as agranulocytosis, cardiotoxicity and seizures [3, 4].
Current guidelines agree that a fundamental requirement for diagnosing TRS and initiating clozapine treatment is to rule out potential pseudo-resistance, which refers to the situation where a patient is mistakenly identified as treatment resistant when secondary confounding factors underly poor therapeutic response [1, 5]. These contributing factors can be of clinical origin, such as comorbid conditions or misdiagnosis, or they can be pharmacological issues that lead to insufficient treatment intensity, that is, low concentrations, such as inadequate dosing, poor adherence, or rapid drug metabolism [5].
Cytochrome P450 (CYP) is the key enzyme system that mediates drug metabolism of clinically important drugs, including antipsychotics [6]. CYP2D6 is the main enzyme responsible for metabolism of aripiprazole and risperidone, whereas it plays a secondary role in the metabolism of quetiapine [7] and olanzapine [8]. CYP1A2 and CYP3A4 constitute the main CYP enzymes involved in olanzapine and quetiapine metabolism, respectively [7, 8]. Increased metabolic activity of these CYP enzymes may be due to intrinsic factors (e.g., age and sex) [9, 10], environmental factors (e.g., increased CYP1A2-mediated olanzapine metabolism due to tobacco smoking) [11], drug–drug interactions [12, 13], and polymorphisms in the genes encoding CYP enzymes (e.g. CYP2D6 metabolism of aripiprazole and risperidone) [14].
Previous studies reported that substantial patient proportions have subtherapeutic serum concentrations of non-clozapine antipsychotics in patients with TRS [15, 16]. While undetectable serum levels represent a clear indication of nonadherence, low serum concentrations adjusted for prescribed dose (CD) may reflect increased clearance of the specific drug [17]. The potential role of rapid drug metabolism underlying low serum levels of non-clozapine antipsychotics before clozapine treatment is unclear. Therefore, in the current study we investigated the metabolizer status of the patients who exhibit low CD (LCD) of four commonly used non-clozapine atypical antipsychotics (aripiprazole, risperidone, olanzapine, and quetiapine) prior to initiating clozapine treatment in a real-world population with longitudinal therapeutic drug monitoring (TDM) profiles.
2 Methods
2.1 Study Population
From 3116 patients treated with clozapine, we identified patients who had a TDM history of non-clozapine, atypical antipsychotics (aripiprazole, risperidone, olanzapine, or quetiapine) preceding clozapine treatment from a TDM/pharmacogenetics service at the Center for Psychopharmacology, Diakonhjemmet Hospital, Oslo, Norway, during the period of January 2005 and February 2023. This laboratory service performs concentration analyses requested by clinicians for dose adjustments to obtain serum levels in the target concentration range, check for potential nonadherence, and determine a patient’s metabolizer status for specific drugs in psychiatric clinical settings. Longitudinal TDM profiles enable assessment of treatment stability, medications used (analyzed), change in medications (switch), and metabolic phenotypes at the patient level over time.
In TDM research, concentrations are often dose-adjusted to harmonize the data and obtain surrogate measures of drug clearance. For the study, interquartile ranges of population-based CDs were prepared for the relevant antipsychotic drugs from the measurements in the TDM registry at the study site (n = 147,964, Table S1 in the electronic supplementary material [ESM]). Patients were subgrouped based on these ranges. Those with at least one measurement with CD of non-clozapine antipsychotics below the 25th percentile of the respective drug’s population-based CDs were assigned to the LCD (cases) group, whereas patients who exhibited CDs between the 25th and 75th percentiles were assigned to the normal CD group (NCD, controls).
In the current study, adult patients with a history of detectable serum concentration of clozapine and/or its major metabolite, N-desmethylclozapine, were eligible for inclusion. Those patients with measurements of orally administered non-clozapine antipsychotics (and their major metabolites) available in the TDM database within 1 year preceding the first clozapine TDM measurement were included. The included non-clozapine antipsychotics comprised aripiprazole (metabolite: dehydroaripiprazole), olanzapine (N-desmethylolanzapine), risperidone (9-hydroxyrisperidone), and/or quetiapine (desalkylquetiapine). Exclusion criteria were (i) lack of dosing information, (ii) measurements with CDs above the 75th percentile population-based threshold (Table S1, see ESM), and (iii) for risperidone specifically, co-medication with paliperidone. Furthermore, we searched for comedication information that may influence the pharmacokinetics of the included antipsychotics [18]. These were (i) CYP inducers (carbamazepine, phenobarbital, and phenytoin), (ii) CYP2D6 inhibitors (bupropion, fluoxetine, and paroxetine; for patients treated with aripiprazole and risperidone), and (iii) valproate and CYP1A2/3A4 inhibitor fluvoxamine (for patients treated with olanzapine). There were 10 olanzapine measurements with potential drug–drug interactions (n = 1 carbamazepine, n = 9 valproate comedications) and were excluded in a secondary analysis. In addition to the typical interacting drugs (CYP inhibitors/inducers), psychiatric comedications were systematically reviewed for patients assigned to LCD or NCD groups. This was performed to assess potential differences in psychiatric drug comedication patterns between the two groups.
Information on age, sex, prescribed dosage, time between last drug intake and blood sampling for TDM (withdrawal time), comedications, and smoking habits (yes/no) were obtained from the requisition forms filled out by the physicians. The study population comprised only Norwegian inhabitants and were assumed to mainly comprise patients of Caucasian ancestry (ethnicity not confirmed due to privacy restrictions).
2.2 Determination of Drug and Metabolite Concentrations
Serum concentration of antipsychotics and their metabolites was determined using the liquid chromatography tandem mass spectrometry (LC MS/MS) method, which was validated and certified for TDM routine analyses. Due to the renewal of instrumentation during the study period, the assays had been modified and cross-validated in line with FDA guidelines on precision, accuracy, and detection limits (Table S2, see ESM).
Subtherapeutic serum level status was only applied as descriptive information and a potential measure of under-treatment when comparing LCD and NCD patient groups. To define the subtherapeutic measurements, the lower boundary of the therapeutic reference ranges recommended in the consensus guidelines were used [19, 20]. These were aripiprazole active moiety 335 nmol/L (150 µg/L, aripiprazole plus dehydroaripiprazole), olanzapine 64 nmol/L (20 µg/L), quetiapine 261 nmol/L (100 µg/L), risperidone active moiety 47 nmol/L (20 µg/L, risperidone plus 9-hydroxyrisperidone). Frequency of antipsychotic polypharmacy (at least two) preceding clozapine treatment required detectable levels of the following antipsychotics: amisulpride, aripiprazole, brexpiprazole, cariprazine, chlorprothixene, flupentixol, haloperidol, levomepromazine, lurasidone, olanzapine, paliperidone, perphenazine, quetiapine, risperidone, sertindole, ziprasidone, and zuclopenthixol.
2.3 CYP2D6 Genotyping
For patients who were using risperidone and aripiprazole before clozapine treatment, we searched the laboratory database for potential access to CYP2D6 genotypes (available for 50–53% of the patients treated with risperidone and aripiprazole, respectively). CYP2D6 genotyping of patients with schizophrenia is quite common in Norway, and offered along with TDM at the laboratory where we sourced data included in the study. The assays for CYP2D6 genotyping at the laboratory are TaqMan-based real-time polymerase chain reaction assays with the CYP2D6 pharmacogenetic panel comprising the lack-of-function variants (Nonf) CYP2D6*3 (rs35742686), CYP2D6*4 (rs3892097), CYP2D6*5 (whole gene deletion), CYP2D6*6 (rs5030655), the decreased function (Decr) variants CYP2D6*9 (rs5030656), CYP2D6*10 (rs1065852), CYP2D6*41 (rs28371725), and duplicated functional CYP2D6 alleles. Normal CYP2D6 allele (Norm, i.e., CYP2D6*1) is interpreted when none of the variant alleles included in the panel are detected.
Risperidone- and aripiprazole-treated patients with available CYP2D6 genotype information were categorized into genotype-predicted metabolic capacity/phenotype according to a previous publication [21] as poor, intermediate, intermediate plus, normal, and ultrarapid metabolizers.
2.4 Outcome Measures and Statistics
The main outcome measure of the study was the metabolic ratio differences between LCD and NCD groups who were treated with antipsychotics of interest (i.e., aripiprazole, risperidone, olanzapine, and/or quetiapine). As a secondary outcome, we investigated the frequency of subtherapeutic serum levels of these drugs among LCD and NCD patients.
Metabolic ratio was estimated by the ratio of the metabolite (nmol/L) and parent drug concentration (nmol/L). CD was calculated as a ratio of parent drug concentration (nmol/L) and total daily dose (mg/day). For statistical comparisons between LCD and NCD patients, Pearson’s chi-squared tests (sex, polypharmacy status, smoking habits, frequency of subtherapeutic levels) and Fisher’s exact tests (CYP2D6 genotype-predicted phenotypes) were conducted for categorical variables, whereas Mann–Whitney U Tests (CD, metabolic ratio, total daily dose, age, withdrawal time, time between last non-clozapine measurement and first clozapine measurement) were used for continuous variables.
All statistical analyses were conducted using R Statistical Software version 4.3.1 [22].
3 Results
In total, 272 patients who had a TDM history of non-clozapine, atypical antipsychotics (aripiprazole, risperidone, olanzapine, or quetiapine) preceding clozapine treatment were included in the study. Among the included patients, 110 (40.4%) were identified with LCD at the last TDM event within 1 year before clozapine treatment.
At the last TDM event before clozapine, 27 patients (10%) had measured two non-clozapine antipsychotics (i.e., aripiprazole, risperidone, olanzapine, and/or quetiapine); hence, 299 TDM measurements were included for statistical analyses. Demographics and treatment characteristics of the study population recorded at last TDM before clozapine treatment are presented in Table 1, while CD distribution and median values among LCD and NCD groups are illustrated in Fig. S1 and shown in Table S3 (see ESM).
We did not observe any differences in the distribution of sex or age between LCD and NCD patients (p = 0.28 and p = 0.92, respectively; Table 1). Information on smoking habits was available for 76.5% of olanzapine users with higher frequencies of smokers among LCD patients compared with NCD patients (84% vs 60%; p = 0.032). We did not observe significant differences in withdrawal time between LCD and NCD patients for the drugs of interest (available for 79% of measurements; p > 0.40; Table 1). Average time registered between last non-clozapine antipsychotic and first clozapine TDM measurements was 17.5 weeks with no significant difference between LCD and NCD groups (p = 0.49; Table 1). A comprehensive list of different psychiatric comedications used by LCD and NCD patients is included in Table S4 (see ESM). There were no apparent differences in psychiatric comedication profiles between LCD and NCD patients. Antipsychotic TDM history in the study population showed that 49% of the patients were on antipsychotic polypharmacy (at least two different non-clozapine antipsychotics) at their last TDM preceding clozapine treatment, with no statistically significant difference in proportion between LCD and NCD patients (p = 0.73; Table 1).
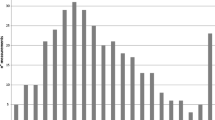
Group differences of median metabolic ratios and total daily doses between LCD and NCD patients for the various drugs are presented in Table 2. At their last TDM measurement prior to clozapine treatment, LCD patients had significantly higher metabolic ratios of olanzapine (1.5-fold; p < 0.001), quetiapine (3.0-fold; p < 0.001), and risperidone (6.0-fold; p < 0.001; Table 2 and Fig. 1) compared with NCD patients. Moreover, we still observed significantly higher median metabolic ratios of the same non-clozapine antipsychotics among LCD patients when we investigated a subpopulation of patients with withdrawal times of 10–30 hours (Table S5, see ESM) and when we excluded the measurements with potential drug–drug interactions (n = 10 olanzapine measurements; LCD: median 0.34, IQR 0.28–0.46; NCD: median 0.25, IQR 0.18–0.32; p < 0.001). There were no significant group differences in metabolic ratio between LCD and NCD patients treated with aripiprazole (p = 0.23).
Metabolic ratio comparisons between LCD and NCD groups among patients treated with different antipsychotics. The graph was plotted on a natural logarithmic scale. The p values for pairwise comparisons and number of patients are added for each subgroup. The pairwise comparisons were achieved with Mann–Whitney U tests. Metabolic ratio is the serum concentration ratios of the metabolite and its parent drug. LCD low dose-adjusted serum concentration, NCD normal dose-adjusted serum concentration
There were no significant differences in distribution of CYP2D6 genotype-predicted metabolic phenotypes between LCD and NCD groups for patients who used the CYP2D6-metabolized drugs risperidone and aripiprazole (p > 0.60; Table S6, see ESM). When we performed sub-analyses among aripiprazole and risperidone patients with CYP2D6*1/*1 genotype and stratified by smoking habits for olanzapine patients, we still observed that LCD patients had significantly higher metabolic ratios of risperidone (p = 0.016) and olanzapine (among smokers; p = 0.008) compared with NCD patients (Table 2 and Fig. 1); however, there was no difference in metabolic ratios of aripiprazole between LCD and NCD patients (p = 0.12).
Compared with NCD patients, LCD patients exhibited significantly higher total daily doses of aripiprazole (p = 0.034) and quetiapine (p = 0.001; Table 2). There was weaker evidence of higher total daily dose among LCD patients treated with olanzapine (p = 0.054), however we did not observe a significant difference among patients treated with risperidone (p = 0.55). Moreover, we observed higher proportions of subtherapeutic absolute serum concentrations among LCD patients treated with aripiprazole (30.0% vs 5.7%; p = 0.021), olanzapine (23.1% vs 7.1; p = 0.044), and quetiapine (63.6% vs 36.1%; p = 0.005) compared with the NCD patients, but not for risperidone-treated patients (42.9% vs 27.0%; p = 0.22).
Overall, LCD was significantly associated with increased (rapid) metabolism for olanzapine, quetiapine, and risperidone (n = 97), as well as increased risk of subtherapeutic serum concentrations for olanzapine and quetiapine. Among olanzapine and quetiapine LCD patients, 36 patients had subtherapeutic serum concentration at the last TDM event before starting clozapine treatment (13.2% of the total study population).
4 Discussion
In a population of 272 patients diagnosed with TRS, we observed that 40.4% of patients exhibited LCD of non-clozapine antipsychotics prior to initiating clozapine treatment. Among these LCD patients, significantly increased metabolic ratios were found for those treated with olanzapine, quetiapine, and/or risperidone. Furthermore, despite higher doses of antipsychotics prescribed, the rapid drug metabolism in the LCD group was accompanied by higher frequencies of subtherapeutic serum levels of olanzapine and quetiapine. This shows that rapid metabolism is common prior to initiating clozapine and associated with risk of undertreatment in patients using olanzapine and quetiapine. Moreover, it underscores the importance of TDM as a tool in the clinical assessments of insufficient effect of antipsychotic drugs in patients with schizophrenia.
The molecular mechanisms underlying the rapid drug metabolism in LCD patients are unclear. The main enzymes involved in metabolism of olanzapine (CYP1A2), quetiapine (CYP3A4), and risperidone (CYP2D6) differ, so a hypothesis may be that a common mechanism regulating the activities of these enzymes is changed in patients exhibiting LCD of one or more of the affected drugs. We have previously shown that enzyme activities of CYP1A2 (olanzapine) and CYP2D6 (risperidone) are regulated by nuclear factor 1B (NFIB), while the data are unclear for CYP3A4 (quetiapine) [23]. Another potential mechanism may be that oxidative stress in schizophrenia [24] has an impact on activities of drug-metabolizing enzymes in a generic manner. Regarding this, Konstandi et al. have reported interesting findings that stress can affect constitutive and induced expression levels of CYP isoforms in ways that may critically modify the pharmacokinetic profile of drug substrates [25]. However, further studies need to elucidate possible mechanism(s) behind our observations of rapid CYP metabolism in a high proportion of patients diagnosed with TRS and starting clozapine therapy.
Treatment with clozapine, evidenced by detectable serum concentrations, was in the present study used as a proxy measure for TRS diagnosis, as clozapine is only licensed for use in TRS. Results of the current study may suggest that a significant proportion of patients diagnosed with TRS do not have a ‘pharmacodynamic resistance’ underlying inadequate response during trials with non-clozapine antipsychotics, but instead are underexposed in terms of subtherapeutic concentrations. While subtherapeutic concentrations of antipsychotics may be caused by adherence issues, as indicated in previous studies [15, 16], the present study shows that occurrence of subtherapeutic concentrations before clozapine treatment is also driven by rapid drug metabolism. Thus, in the assessment of potential TRS, it is important to investigate the patient’s metabolizer phenotype to clarify whether rapid metabolism could be a possible cause of underexposure (low concentration) and insufficient clinical response of non-clozapine antipsychotics. However, this requires that TDM, including metabolite analyses, is integrated as part of the guidelines for diagnosing potential TRS.
The results of the present study provide a basis for new studies investigating molecular mechanisms underlying rapid drug metabolism of multiple drugs via different CYP enzymes and also the clinical impact of rapid metabolism on clinical outcomes of drug treatment in psychiatry. CYP enzymes are important in the metabolism of psychiatric drugs, and previous studies have demonstrated that increased CYP2D6 and CYP2C19 metabolism are associated with increased risk of treatment failure of risperidone and escitalopram, respectively, as measured by switch to another medication within the same group [26, 27]. Further, tobacco smoking is known to induce olanzapine metabolism and leads to decreased serum concentrations [8, 12, 13] and a subsequent risk of undertreatment. In the current study, we observed that an increased metabolism was present in both smoking and non-smoking patients with LCD compared with the patients in the respective NCD groups. Similarly, the difference was independent of CYP2D6 genotype for risperidone. These observations, and the fact that multiple antipsychotics were affected regardless of primary CYP enzymes involved in the respective drug’s metabolism, should be investigated further in clinical studies on patients with schizophrenia.
A study limitation is the lack of clinical data regarding disease severity, treatment response measures, and side effects. Therefore, it is not possible to ascertain the psychiatrists’ clinical assessments before deciding that patients should start clozapine treatment. Furthermore, we cannot exclude that dose increases of non-clozapine antipsychotics had been tried without success, and a lack of accompanying TDM during the 1 year preceding detection of clozapine TDM. Time between last drug intake and blood sampling for TDM (withdrawal time, information available for 79% of measurements) may influence drug serum levels at the time of measurement, however we did not observe any significant difference in withdrawal time between LCD and NCD patients. Overall, the listed limitations are unlikely to be of substantial importance for the observations of highly significant increases in metabolizer phenotypes among patients expressing LCD versus NCD before clozapine treatment. With the availability of metabolite measurements, and hence the ability to calculate metabolic ratios reflecting clearance of the respective drug, the present study enabled the investigation of pharmacokinetics separately from nonadherence as a cause underlying the LCD phenotype. This is a major strength, showing the power of using TDM data to investigate pharmacokinetic variability in uncontrolled, real-world study settings.
5 Conclusions
Our data provides evidence that LCD and associated rapid metabolism of non-clozapine antipsychotics frequently precedes clozapine treatment and, for many patients, is associated with subtherapeutic serum concentrations with possible insufficient clinical effect of non-clozapine antipsychotics. The results herein warrant replication in independent cohorts, however, they also suggest that antipsychotic TDM with metabolite analyses can be of clinical utility before initiating clozapine as a basis for decision making regarding possible TRS. Finally, new studies are necessary to identify the molecular mechanism(s) underlying the increased metabolism of non-clozapine, atypical antipsychotics.
References
Howes OD, McCutcheon R, Agid O, de Bartolomeis A, van Beveren NJM, Birnbaum ML, et al. Treatment resistant schizophrenia: Treatment Response and Resistance in Psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry. 2017;174:216–29. https://doi.org/10.1176/appi.ajp.2016.16050503.
Siskind D, Orr S, Sinha S, Yu O, Brijball B, Warren N, et al. Rates of treatment-resistant schizophrenia from first-episode cohorts: systematic review and meta-analysis. Br J Psychiatry. 2022;220:115–20. https://doi.org/10.1192/bjp.2021.61.
Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394:939–51. https://doi.org/10.1016/S0140-6736(19)31135-3.
Miller DD. Review and management of clozapine side effects. J Clin Psychiatry. 2000;61(Suppl 8):14–7.
Howes OD, Thase ME, Pillinger T. Treatment resistance in psychiatry: state of the art and new directions. Mol Psychiatry. 2022;27:58–72. https://doi.org/10.1038/s41380-021-01200-3.
Zanger UM, Schwab M. Cytochrome P450 enzymes in drug metabolism: regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacol Ther. 2013;138:103–41. https://doi.org/10.1016/j.pharmthera.2012.12.007.
Hasselstrøm J, Linnet K. In vitro studies on quetiapine metabolism using the substrate depletion approach with focus on drug-drug interactions. Drug Metabol Drug Interact. 2006;21:187–211. https://doi.org/10.1515/dmdi.2006.21.3-4.187.
Callaghan JT, Bergstrom RF, Ptak LR, Beasley CM. Olanzapine. Pharmacokinetic and pharmacodynamic profile. Clin Pharmacokinet. 1999;37:177–93. https://doi.org/10.2165/00003088-199937030-00001.
Castberg I, Westin AA, Skogvoll E, Spigset O. Effects of age and gender on the serum levels of clozapine, olanzapine, risperidone, and quetiapine. Acta Psychiatr Scand. 2017;136:455–64. https://doi.org/10.1111/acps.12794.
Solhaug V, Tveito M, Waade RB, Høiseth G, Molden E, Smith RL. Impact of age, sex and cytochrome P450 genotype on quetiapine and N-desalkylquetiapine serum concentrations: a study based on real-world data from 8118 patients. Br J Clin Pharmacol. 2023;89:3503–11. https://doi.org/10.1111/bcp.15849.
Wagner E, McMahon L, Falkai P, Hasan A, Siskind D. Impact of smoking behavior on clozapine blood levels—a systematic review and meta-analysis. Acta Psychiatr Scand. 2020;142:456–66. https://doi.org/10.1111/acps.13228.
Skogh E, Reis M, Dahl M-L, Lundmark J, Bengtsson F. Therapeutic drug monitoring data on olanzapine and its N-demethyl metabolite in the naturalistic clinical setting. Ther Drug Monit. 2002;24:518.
Tveito M, Smith RL, Høiseth G, Molden E. The effect of valproic acid on olanzapine serum concentration: a study including 2791 patients treated with olanzapine tablets or long-acting injections. J Clin Psychopharmacol. 2019;39:561–6. https://doi.org/10.1097/JCP.0000000000001126.
Jukic M, Milosavljević F, Molden E, Ingelman-Sundberg M. Pharmacogenomics in treatment of depression and psychosis: an update. Trends Pharmacol Sci. 2022;43:1055–69. https://doi.org/10.1016/j.tips.2022.09.011.
Kyllesø L, Smith RL, Karlstad Ø, Andreassen OA, Molden E. Undetectable or subtherapeutic serum levels of antipsychotic drugs preceding switch to clozapine. npj Schizophr. 2020;6:1–6. https://doi.org/10.1038/s41537-020-0107-7.
McCutcheon R, Beck K, D’Ambrosio E, Donocik J, Gobjila C, Jauhar S, et al. Antipsychotic plasma levels in the assessment of poor treatment response in schizophrenia. Acta Psychiatr Scand. 2018;137:39–46. https://doi.org/10.1111/acps.12825.
de Leon J. Personalizing dosing of risperidone, paliperidone and clozapine using therapeutic drug monitoring and pharmacogenetics. Neuropharmacology. 2020;168: 107656. https://doi.org/10.1016/j.neuropharm.2019.05.033.
Kennedy WK, Jann MW, Kutscher EC. Clinically significant drug interactions with atypical antipsychotics. CNS Drugs. 2013;27:1021–48. https://doi.org/10.1007/s40263-013-0114-6.
Hiemke C, Bergemann N, Clement HW, Conca A, Deckert J, Domschke K, et al. Consensus guidelines for therapeutic drug monitoring in neuropsychopharmacology: update 2017. Pharmacopsychiatry. 2018;51: e1. https://doi.org/10.1055/s-0037-1600991.
Schoretsanitis G, Kane JM, Correll CU, Marder SR, Citrome L, Newcomer JW, et al. Blood levels to optimize antipsychotic treatment in clinical practice: a joint consensus statement of the American Society of Clinical Psychopharmacology and the Therapeutic Drug Monitoring Task Force of the Arbeitsgemeinschaft für Neuropsychopharmakologie und Pharmakopsychiatrie. J Clin Psychiatry. 2020;81:3649. https://doi.org/10.4088/JCP.19cs13169.
Jukić MM, Smith RL, Molden E, Ingelman-Sundberg M. Evaluation of the CYP2D6 haplotype activity scores based on metabolic ratios of 4,700 patients treated with three different CYP2D6 substrates. Clin Pharmacol Ther. 2021. https://doi.org/10.1002/cpt.2246.
R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. 2021. https://www.R-project.org/. Accessed 2024 Feb 12.
Lenk HÇ, Klöditz K, Johansson I, Smith RL, Jukić MM, Molden E, et al. The polymorphic nuclear factor NFIB regulates hepatic CYP2D6 expression and influences risperidone metabolism in psychiatric patients. Clin Pharmacol Ther. 2022;111:1165–74. https://doi.org/10.1002/cpt.2571.
Murray AJ, Rogers JC, Katshu MZUH, Liddle PF, Upthegrove R. Oxidative stress and the pathophysiology and symptom profile of schizophrenia spectrum disorders. Front Psychiatry [Internet]. 2021 [cited 2024 Feb 12];12. https://doi.org/10.3389/fpsyt.2021.703452.
Konstandi M, Johnson EO, Lang MA. Stress as a potential regulatory factor in the outcome of pharmacotherapy. Front Neurosci. 2022;16: 737716. https://doi.org/10.3389/fnins.2022.737716.
Jukić MM, Smith RL, Haslemo T, Molden E, Ingelman-Sundberg M. Effect of CYP2D6 genotype on exposure and efficacy of risperidone and aripiprazole: a retrospective, cohort study. Lancet Psychiatry. 2019;6:418–26. https://doi.org/10.1016/S2215-0366(19)30088-4.
Jukić MM, Haslemo T, Molden E, Ingelman-Sundberg M. Impact of CYP2C19 genotype on escitalopram exposure and therapeutic failure: a retrospective study based on 2,087 patients. Am J Psychiatry. 2018;175:463–70. https://doi.org/10.1176/appi.ajp.2017.17050550.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by the University of Oslo (incl Oslo University Hospital). This work was supported by South-Eastern Norway Regional Health Authority (Grant No. 2020019) and the European Union's Horizon 2020 research and innovation program (REALMENT; Grant No. 964874).
Conflicts of interest
OAA is consultant to Cortechs.ai and received speaker’s honoraria from Lundbeck, Sunovion, Janssen. The other authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
The study was approved by the Regional Committee for Medical and Health Research Ethics and the Hospital Investigational Review Board.
Consent to participate
Since only historical data from already performed routine analyses was included in the study without posing any risk or burden to the patients, patient consent was not required.
Consent for publication
Not applicable.
Availability of data and material
The data that supports the findings of this study are available from the corresponding author upon reasonable request. The data is not publicly available due to privacy and ethical restrictions.
Code availability
Not applicable.
Author contributions
HÇL and RLS extracted and prepared the data material. HÇL, RLS, and EM analysed and interpreted the data. EM designed the study. HÇL drafted the initial manuscript. All authors critically reviewed, wrote, edited, and significantly contributed to the final manuscript. All authors have read and approved the final submitted manuscript and agree to be accountable for the work.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lenk, H.Ç., Smith, R.L., O’Connell, K.S. et al. Rapid Metabolism Underlying Subtherapeutic Serum Levels of Atypical Antipsychotics Preceding Clozapine Treatment: A Retrospective Analysis of Real-World Data. CNS Drugs 38, 473–480 (2024). https://doi.org/10.1007/s40263-024-01079-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-024-01079-y