Abstract
This article provides a critical appraisal of the available evidence concerning clinical exposure to orally administered cannabidiol (CBD), with special reference to factors affecting gastrointestinal absorption, presystemic elimination, and susceptibility to metabolic drug interactions. Although detailed studies have not been published, the available data suggest that the absolute bioavailability of CBD after oral dosing under fasting conditions is approximately 6%, and increases fourfold when the medication is co-administered with a high-fat meal. Based on measurements of CBD plasma exposure after oral dosing and a 6% absolute oral bioavailability estimate, the actual clearance of CBD in adults can be inferred to be in the order of 67 L/h, which is similar to the value of 74 ± 14 L/h (mean ± standard deviation) determined after intravenous injection of a 20-mg dose of deuterium-labeled CBD in five healthy subjects. Assuming that the CBD blood-to-plasma ratio is about 1, as in the case of tetrahydrocannabinol (THC), and that CBD metabolism takes place virtually entirely in the liver, it can be estimated that about 70 to 75% of an orally absorbed dose of CBD can be removed by hepatic metabolism before reaching the systemic circulation, and additionally CBD gastrointestinal absorption is incomplete. A formulation with improved biopharmaceutical properties could increase the extent of CBD absorption about fourfold (i.e., to the level achieved with the currently available formulations co-administered with a high-fat meal) and minimize the influence of food effects on CBD bioavailability. There is also potential for favoring the absorption of CBD through the enteric lymphatic system, thereby reducing the extent of presystemic hepatic elimination. Evidence that CBD can behave as a high hepatic clearance compound also has implications when predicting the magnitude of drug–drug interactions affecting CBD metabolism. These considerations have important clinical relevance, particularly with respect to the objective of minimizing pharmacokinetic variability and consequent intra- and interindividual differences in therapeutic response and susceptibility to adverse effects.
Similar content being viewed by others
References
Amin MR, Ali DW. Pharmacology of medical cannabis. Adv Exp Med Biol. 2019;1162:151–65.
Campos AC, Fogaça MV, Sonego AB, Guimarães FS. Cannabidiol, neuroprotection and neuropsychiatric disorders. Pharmacol Res. 2016;112:119–27.
Elsaid S, Kloiber S, Le Foll B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog Mol Biol Transl Sci. 2019;167:25–75.
Cassano T, Villani R, Pace L, Carbone A, Naik Bukke V, Orkisz S, et al. From Cannabis sativa to cannabidiol: promising therapeutic candidate for the treatment of neurodegenerative diseases. Front Pharmacol. 2020;11:124.
Kis B, Ifrim FC, Buda V, Avram S, Pavel IZ, Antal D, et al. Cannabidiol-from plant to human body: a promising bioactive molecule with multi-target effects in cancer. Int J Mol Sci. 2019;20(23):E5905.
Pisanti S, Malfitano AM, Ciaglia E, Lamberti A, Ranieri R, Cuomo G, et al. Cannabidiol: state of the art and new challenges for therapeutic applications. Pharmacol Ther. 2017;175:133–50.
Fitzcharles MA, Clauw DJ, Hauser W. A cautious hope for cannabidiol (CBD) in rheumatology care. Arthritis Care Res. 2020. https://doi.org/10.1002/acr.24176.
Franco V, Perucca E. Pharmacological and therapeutic properties of cannabidiol for epilepsy. Drugs. 2019;79:1435–54.
Epidiolex. Full Prescribing Information. Greenwich Biosciences Inc. 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/210365lbl.pdf. Accessed 10 Apr 2020.
Epidyolex. Summary of Product Characteristics. https://www.ema.europa.eu/en/documents/product-information/epidyolex-epar-product-information_en.pdf. Accessed 10 Apr 2020.
Geffrey AL, Pollack SF, Bruno PL, Thiele EA. Drug–drug interaction between clobazam and cannabidiol in children with refractory epilepsy. Epilepsia. 2015;56:1246–51.
Morrison G, Crockett J, Blakey G, Sommerville K. A Phase 1, open-label, pharmacokinetic trial to investigate possible drug-drug interactions between clobazam, stiripentol, or valproate and cannabidiol in healthy subjects. Clin Pharmacol Drug Dev. 2019;8:1009–31.
European Medicines Agency, Committee for Medicinal Products for Human Use (CHMP), Epidyolex Assessment Report, https://www.ema.europa.eu/en/documents/assessment-report/epidyolex-epar-public-assessment-report_en.pdf. Accessed 18 Mar 2020.
Amidon GL, Lennernas H, Shah VP, Crison JR. A theoretical basis for biopharmaceutics drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12:413–20.
Wu C-Y, Benet LZ. Predicting drug disposition via application of BCS: transport/absorption/elimination interplay and development of a biopharmaceutics drug disposition classification system. Pharm Res. 2005;22:11–23.
Chan R, Wei C-Y, Chen Y-T, Benet LZ. Use of the biopharmaceutics drug disposition classification system (BDDCS) to help predict the occurrence of idiosyncratic coetaneous adverse reaction associated with antiepileptic drug usage. AAPS J. 2016;18:757–76.
DrugBank Database: Cannabidiol. https://www.drugbank.ca/drugs/DB09061. Accessed 24 Mar 2020.
Harvey DJ, Samara E, Mechoulam R. Comparative metabolism of cannabidiol in dog, rat and man. Pharmacol Biochem Behav. 1991;40:523–32.
Samara E, Bialer M, Harvey DJ. Pharmacokinetics of urinary metabolites of cannabidiol in the dog. Biopharm Drug Dispos. 1990;11:785–95.
Gaston TE, Friedman D. Pharmacology of cannabinoids in the treatment of epilepsy. Epilepsy Behav. 2017;70(Pt B):313–8.
Zendulka O, Dovrtelova G, Noskova K, Turjap M, Sulcova A, Hanus L, et al. Cannabinoids and cytochrome P450 interactions. Curr Drug Metab. 2016;17:206–26.
Ujváry I, Hanuš L. Human metabolites of cannabidiol: a review on their formation, biological activity, and relevance in therapy. Cannabis Cannabinoid Res. 2016;1:90–101.
Miller SA, Stone NL, Yates SAS, O’Sullivan SE. A systemic review on the pharmacokinetics of cannabidiol in humans. Front Pharmacol. 2018. https://doi.org/10.3389/fphar.2018.01365.
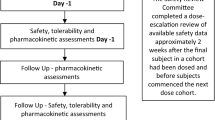
Bialer M, Johannessen SI, Koepp MJ, Levy RH, Perucca E, Tomson T, et al. Progress report on new antiepileptic drugs: a summary of the fourteen Eilat Conference on new antiepileptic drugs and devices. II. Drugs in more advanced clinical development. Epilepsia. 2018;59:1856–84.
Ohlsson A, Lindgren JE, Wahlen A, Agurell S, Hollister LE, Gillespie HK. Plasma delta-9-tetrahydrocannabinol concentrations and clinical effects after oral and intravenous administration and smoking. Clin Pharmacol Ther. 1980;28:409–16.
Grotenhermen F. Pharmacokinetics and pharmacodynamics of cannabinoids. Clin Pharmacokinet. 2003;42:327–60.
Ohlsson A, Lindgren JE, Andersson S, Agurell S, Gillespie H, Hollister LE. Single-dose kinetics of deuterium-labelled cannabidiol in man after smoking and intravenous administration. Biomed Environ Mass Spectrom. 1986;13:77–83.
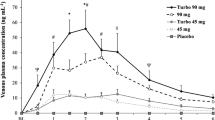
Taylor L, Gidal B, Blakey G, Tayo B, Morrison G. A phase I, randomized, double-blind, placebo-controlled, single ascending dose, multiple dose, and food effect trial of the safety, tolerability and pharmacokinetics of highly purified cannabidiol in healthy subjects. CNS Drugs. 2018;32:1053–67.
Birnbaum AK, Karanam A, Marino SE, Barkley CM, Remmel RP, Roslawski M, et al. Food effect on pharmacokinetics of cannabidiol oral capsules in adult patients with refractory epilepsy. Epilepsia. 2019;60:1586–92.
Crockett J, Critchley D, Tayo B, Berwaerts J, Morrison G. A phase 1, randomized, pharmacokinetic trial of the effect of different meal compositions, whole milk, and alcohol on cannabidiol exposure and safety in healthy subjects. Epilepsia. 2020;61:267–77.
Bialer M, Arcavi L, Sussan S, Volosov A, Yacobi D, Moros D, et al. Existing and new criteria for bioequivalent of new controlled release (CR) products of carbamazepine. Epilepsy Res. 1998;32:371–8.
Taylor L, Crockett J, Tayo B, Morrison G. A Phase 1, open-label, parallel-group, single-dose trial of the pharmacokinetics and safety of cannabidiol (CBD) in subjects with mild to severe hepatic impairment. J Clin Pharmacol. 2019;59:1110–9.
Tayo B, Taylor L, Sahebkar F, Morrison G. A Phase 1, open-label, parallel-group, single-dose trial of the pharmacokinetics, safety and tolerability of cannabidiol in subjects with mild to severe renal impairment. Clin Pharmacokinet. 2019. https://doi.org/10.1007/s40262-019-00841-6(Epub ahead of print).
Widman M, Agurell S, Ehrnebo M, Jones G. Binding of (+)- and (–)-Δ1-tetrahydrocannabinols and (–)-7-hydroxy-Δ1-tetrahydrocannabinol to blood cells and plasma proteins in man. J Pharm Pharmacol. 1974;26:914–6.
Wilkinson GR, Shand DG. Commentary: a physiological approach to hepatic drug clearance. Clin Pharmacol Ther. 1975;18:377–90.
Derendorf H, Schmidt S. Rowland and Tozer’s clinical pharmacokinetics and pharmacodynamics. 5th ed. South Holland: Wloters Kluwer; 2020. p. 78–82.
Klumpers LE, Beumer TL, van Hasselt JG, Lipplaa A, Karger LB, Kleinloog HD, et al. Novel delta(9)-tetrahydrocannabinol formulation Namisol has beneficial pharmacokinetics and promising pharmacodynamic effects. Br J Clin Pharmacol. 2012;74:42–53.
Marinol. Full Precribing information. Patheon Softgels Inc. 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018651s029lbl.pdf. Accessed 11 Apr 2020.
Zgair A, Wong JC, Lee JB, Mistry J, Sivak O, Wasan KM, et al. Dietary fats and pharmaceutical lipid excipients increase systemic exposure to orally administered cannabis and cannabis-based medicines. Am J Transl Res. 2016;8:3448–59.
Lee JB, Zgair A, Malec J, Kim TH, Kim MG, et al. Lipophilic activated ester prodrug approach for drug delivery to the intestinal lymphatic system. J Control Release. 2018;286:10–9.
Brocks DR, Davies NM. Lymphatic drug absorption via the enterocytes: pharmacokinetic simulation, modeling, and considerations for optimal dug development. J Pharm Pharm Sci. 2018;21:254s–70s.
Whalley BJ, Stott C, Gray RA. The human metabolite of cannabidiol, 7-hydroxy-cannabidiol, but not 7-carboxy-cannabidiol, is anticonvulsant in the maximal electroshock threshold test (MEST) in mouse [abstract no. 1.435]. 71st Annual Meeting of the American Epilepsy Society, Washington DS, December 1–5, 2017. https://www.aesnet.org/meetings_events/annual_meeting_abstracts/view/381222. Accessed 11 Apr 2020.
Jiang R, Yamaori S, Takeda S, Yamamoto I, Watanabe K. Identification of cytochrome P450 enzymes responsible for metabolism of cannabidiol by human liver microsomes. Life Sci. 2011;89:165–70.
Stott C, White L, Wright S, Wilbraham D, Guy G. A phase I, open-label, randomized, crossover study in three parallel groups to evaluate the effect of rifampicin, ketoconazole, and omeprazole on the pharmacokinetics of THC/CBD oromucosal spray in healthy volunteers. Springerplus. 2013;2:236.
Garnock-Jones KP. Oromucosal midazolam: a review of its use in pediatric patients with prolonged acute convulsive seizures. Paediatr Drugs. 2012;14:251–61.
Tran A, Rey E, Pons G, Rousseau M, d’Athis P, Olive G, et al. Influence of stiripentol on cytochrome P450-mediated metabolic pathways in humans: in vitro and in vivo comparison and calculation of in vivo inhibition constants. Clin Pharmacol Ther. 1997;62:490–504.
Arzimanoglou A, French J, Blume WT, Cross JH, Ernst JP, et al. Lennox–Gastaut syndrome: a consensus approach on diagnosis, assessment, management, and trial methodology. Lancet Neurol. 2009;8:82–93.
Wirrell EC. Treatment of Dravet syndrome. Can J Neurol Sci. 2016;43(Suppl 3):S13–8.
Thiele E, Bebin EM, Bhathal H, Jansen F, Kotulska-Jozwiak K, et al. Cannabidiol (CBD) treatment in patients with seizures associated with tuberous sclerosis complex: a randomized double-blind, placebo-controlled Phase 3 trial (GWPCARE6). Abstract. Annual Meeting of the American Epilepsy Society, Baltimore, Maryland, December 6–10, 2019. https://www.aesnet.org/meetings_events/annual_meeting_abstracts/view/2421288. Accessed 10 Apr 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was not supported by any funding source.
Conflict of interest
MB has received speaker’s or consultancy fees from Alkaloid, Boehringer Ingelheim, Medison, and US WorldMeds. EP has received speaker’s or consultancy fees from Amicus Therapeutics, Arvelle, Biogen, Eisai, GW Pharma, Intas Pharmaceuticals, Laboratorios Bagò, Sanofi, Sun Pharma, UCB Pharma, and Xenon Pharma.
Ethical approval
We confirm that we have read the journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Rights and permissions
About this article
Cite this article
Perucca, E., Bialer, M. Critical Aspects Affecting Cannabidiol Oral Bioavailability and Metabolic Elimination, and Related Clinical Implications. CNS Drugs 34, 795–800 (2020). https://doi.org/10.1007/s40263-020-00741-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-020-00741-5