Abstract
Background
Stimulant drugs are second only to cannabis as the most widely used class of illicit drug globally, accounting for 68 million past-year consumers. Dependence on amphetamines (AMPH) or methamphetamine (MA) is a growing global concern. Yet, there is no established pharmacotherapy for AMPH/MA dependence. A comprehensive assessment of the research literature on pharmacotherapy for AMPH/MA dependence may inform treatment guidelines and future research directions.
Methods
We systematically reviewed the peer-reviewed literature via the electronic databases PubMed, EMBASE, CINAHL and SCOPUS for randomised controlled trials reported in the English language examining a pharmacological treatment for AMPH/MA dependence or use disorder. We included all studies published to 19 June 2019. The selected studies were evaluated for design; methodology; inclusion and exclusion criteria; sample size; pharmacological and (if included) psychosocial interventions; length of follow-up and follow-up schedules; outcome variables and measures; results; overall conclusions and risk of bias. Outcome measures were any reported impact of treatment related to AMPH/MA use.
Results
Our search returned 43 studies that met our criteria, collectively enrolling 4065 participants and reporting on 23 individual pharmacotherapies, alone or in combination. Disparate outcomes and measures (n = 55 for the primary outcomes) across studies did not allow for meta-analyses. Some studies demonstrated mixed or weak positive signals (often in defined populations, e.g. men who have sex with men), with some variation in efficacy signals dependent on baseline frequency of AMPH/MA use. The most consistent positive findings have been demonstrated with stimulant agonist treatment (dexamphetamine and methylphenidate), naltrexone and topiramate. Less consistent benefits have been shown with the antidepressants bupropion and mirtazapine, the glutamatergic agent riluzole and the corticotropin releasing factor (CRF-1) antagonist pexacerfont; whilst in general, antidepressant medications (e.g. selective serotonin reuptake inhibitors [SSRIs], tricyclic antidepressants [TCAs]) have not been effective in reducing AMPH/MA use.
Conclusions
No pharmacotherapy yielded convincing results for the treatment of AMPH/MA dependence; mostly studies were underpowered and had low treatment completion rates. However, there were positive signals from several agents that warrant further investigation in larger scale studies; agonist therapies show promise. Common outcome measures should include change in use days. Future research must address the heterogeneity of AMPH/MA dependence (e.g. coexisting conditions, severity of disorder, differences between MA and AMPH dependence) and the role of psychosocial intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A comprehensive assessment of the research literature on pharmacotherapy for amphetamine/methamphetamine dependence may inform treatment guidelines and future research directions. |
We systematically reviewed 43 randomised controlled trials enrolling 4065 participants and assessing 23 pharmacotherapies for amphetamine/methamphetamine dependence. |
Outcomes and measures to assess them varied widely, making it difficult to synthesise the data; pharmacotherapies were most often assessed in defined or biased populations, and study completion rates were low. |
No pharmacotherapy demonstrated convincing results; however, some agents demonstrated promise, suggesting further, larger studies are required. |
Future research should consider the heterogeneity of amphetamine/methamphetamine dependence and the role of psychosocial intervention. |
1 Introduction
Amphetamines and other stimulant drugs are second only to cannabis as the most widely used class of (illicit) drugs globally, accounting for 68 million past-year consumers [1]. Approximately 29 million people worldwide aged 15–65 years were estimated to have consumed amphetamines in the past year to 2017 [1].
Amphetamines refer to both amphetamine (AMPH) and the structurally similar methamphetamines (MA), both of which are used extra-medically. MA is considered a more potent derivative of AMPH, with a longer duration of action and increased ability to cross the blood–brain barrier; and global shifts in the illicit stimulant market have resulted in the predominance of MA [2, 3].
Amphetamines act on the central nervous system (CNS) and acute effects include a heightened sense of alertness; increased energy; heightened curiosity; anorexia; decreased fatigue; elevated mood; dose-dependent effects on focus, attention and concentration; and elevated interest in environmental stimuli [3, 4]. Extra-medical use of AMPH and MA is usually at higher doses than those prescribed orally, and through routes of administration that result in more rapid onset (inhaled, injected intravenously, intra-nasal, per-vaginal, and per-rectal). Extra-medical consumption of amphetamines may be for enjoyment and/or for performance enhancement (such as for night-shift workers to enable longer working hours) [5].
The effects of chronic and regular high-dose AMPH/MA use are more complex than occasional use, and may involve the development of a substance use disorder—characterised by social and physiological (e.g. tolerance, withdrawal) manifestations [5]. The Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V) criteria for Stimulant Use Disorder (SUD) and Stimulant Withdrawal [6] are listed in Table 1. In the previous version of the DSM (DSM-IV) [7], the classification listed ‘dependence’ rather than ‘use disorder’; with ‘moderate to severe’ SUD being regarded as equivalent to ‘dependence’. The International Classification of Diseases (ICD) 10th Revision (ICD-10) recognises ‘stimulant dependence syndrome’ and ‘stimulant withdrawal state’ [8]. However, neither diagnostic tool differentiates between AMPH/MA and other non-cocaine stimulant SUDs; while the 11th Revision of the ICD narrows the definition to “stimulant dependence including amphetamines, methamphetamine or methcathinone” [9]. In this paper, we have reviewed articles using all of the above classifications and sometimes interchangeably and our search included both terms. Most reviewed articles had eligibility criteria that included either the DSM-IV or DSM-V diagnostic criteria, and so we have combined the terms as dependence/use disorder.
Globally, it is estimated that 7.4 million people are dependent on amphetamines, and that dependence affects 11% of people who use amphetamines [10]. Regular or dependent AMPH/MA use is associated with comorbidities including depression, anxiety, psychosis and cardiovascular disease, and is due to contextual social factors related to the consumption of AMPH/MA, sexually transmitted infections or blood borne viruses and legal issues [11, 12]. Globally, the United Nations Office of Drugs and Crime (UNODC) estimates around one in seven people with substance use disorders receives treatment [1], and that the proportion of people with stimulant use disorder in treatment is under-represented compared with opioid use disorder, for which there are effective treatments combining medication and psychosocial interventions [13].
Psychosocial therapies have been trialled for AMPH/MA dependence with varying efficacy [14, 15]. These include Cognitive Behavioural Therapy (CBT), Contingency Management (CM), Motivational Interviewing (MI) and Acceptance and Commitment Therapy (ACT). Even short periods of intervention with CBT (1–2 sessions) demonstrate a reduction in MA use in people who are dependent on MA [14]. CM has demonstrated significant reduction in stimulant use [16] alone, or in combination with CBT [16] or a community reinforcement approach [17]. However, the effects of psychosocial therapies are often not sustained following their cessation [14, 18], and are less effective for severe disorder (long duration, frequent use) [19]. There have been few controlled evaluations of residential rehabilitation approaches for people with AMPH/MA use disorders. One longitudinal, non-randomised, quasi-controlled study demonstrated that residential rehabilitation was associated with decreased MA use 3 months after treatment compared with detoxification or no treatment, but this effect was not maintained to year 3 of follow-up [20].
One priority for clinicians and researchers alike has been to establish an effective pharmacotherapy for SUD. Target pharmacotherapies have considered the mechanism of action of AMPH/MA, which affects neurotransmitters through a number of mechanisms. Consumption of MA triggers a cascading release of norepinephrine, dopamine and serotonin. The drug (to a lesser extent) acts as a dopaminergic and adrenergic reuptake inhibitor, and in higher concentrations as a monoamine oxidase inhibitor (MAOI) [1, 21]. The CNS effects produced by MA are mostly the result of influencing levels of dopamine and norepinephrine, and to a lesser extent serotonin [1, 21].
Due to the nature of drug dependence research, studies often enrol people using multiple types of stimulants or other drugs. Here we review studies reporting on pharmacotherapies for the treatment of SUD or drug dependence due to AMPH/MA. Specifically, we reviewed randomised studies of participants with MA or AMPH use disorder or dependence (recognising the shift of eligibility criteria and definitions between the DSM-IV and DSM-V) randomised to a pharmacological intervention and compared with a control group, with outcomes related to AMPH/MA use and associated symptoms (e.g. cravings or withdrawal, as these are both listed as features of dependence/use disorder). The aim of the present review is to provide clinicians with a summary of the current status of research on pharmacological treatment of AMPH/MA dependence.
2 Methods
We approached this report as a systematic review of the peer-reviewed literature, and present the methods and results in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [22].
The eligibility criteria for this review were randomised controlled trials (RCTs) enrolling participants (any age or sex) that assessed a pharmacological treatment (alone or in combination with psychosocial treatment) for the treatment of AMPH/MA dependence or use disorder. The search was limited to human trials and with text in the English language. Included were studies reporting on an outcome related to treatment efficacy as defined by AMPH/MA use, associated symptoms (e.g. cravings or withdrawal) or retention in treatment/care. We excluded human studies that were conducted in a laboratory environment, studies enrolling primarily non-AMPH/MA-dependent participants, animal studies, qualitative studies, general reviews and secondary analyses of RCTs.
A search of the electronic databases PubMed, EMBASE, CINAHL and SCOPUS was conducted. The basic search strategy for all databases was as follows: (amphetamine OR methamphetamine) AND (dependence OR disorder) AND (pharmacological treatment OR pharmacotherapy OR drug therapy). Additional studies were obtained by checking the references of selected articles. There was no start date limitation on the search—the last search date for inclusion was 19 June 2019. An example search strategy is included in Supplementary Fig. 1 (see electronic supplementary material [ESM]).
The titles and abstracts of the studies identified by the search strategy were evaluated by two reviewers (KS and LA) independently. Selected publications were read in full by the same two investigators. Divergent selection of publications was discussed among the investigators until a consensus was obtained, and if required a third reviewer (NE) resolved disputes. Data were managed in Covidence [23] up to the point of data extraction; due to the large variation in outcome measures, data extraction was completed on identical spreadsheets by the two reviewers and compared for consistency. The selected studies were evaluated for design, methodology, inclusion and exclusion criteria, sample size, pharmacological and (if included) psychosocial interventions, length of follow-up and follow-up schedules, outcome variables and measures, results and overall conclusions.
Risk of bias was assessed based on the following features: allocation of participants, blinding of participants or personnel, study sample, study completion rates, analyses of outcomes (e.g. conservative or not with respect to missing data, analysis as intention-to-treat), overstated conclusions and study funding.
This review provides a qualitative, narrative report of the data. Conducting a traditional systematic review and meta-analyses is predicated on the assumption of studies reporting on similar outcomes, using similar outcome measures, and with similar methodology. However, the data we reviewed herein was disparate in respect to the reported outcomes and measures. This prohibited meta-analysis of the literature but allowed for a comprehensive report on the current status of the research.
3 Results
3.1 Study Selection and Characteristics
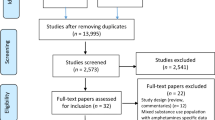
Our search returned 43 RCTs that met our criteria [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66]. A PRISMA flow diagram is presented in Fig. 1. Forty (93.0%) of these studies were double-blinded [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45, 47,48,49,50,51,52,53,54,55, 57,58,59,60,61,62,63,64,65]. In total, 39 (90.7%) were placebo controlled, while the remaining four studies (9.3%) were designed with a treatment-as-usual or alternate treatment arm as the control [36, 49, 61, 66]. The study settings are described in Table 2. The studies were published between 1995 and 2019.
The 43 studies collectively randomised 4065 participants. Of the 43 studies, 38 (88%) reported on the total number of participants who completed the study, while five studies (12%) did not [36, 39, 57, 62, 64]. Of the 38 reporting on study completion rates, the total number of participants randomised was 3733 (92% of the total) and of these, 2298 participants completed the study (61.6%).
Of the 4065 participants reported on in the reviewed studies, 2858 (70.3%) were male. Nine of the 43 studies (21%) enrolled only males [24, 29, 30, 34, 46, 52, 55, 57, 58], however not all of these were by design. One study [45] did not report the sample by those randomised, only by completers (in a non-intention-to-treat analysis) and so the total randomised figure of men versus women was not able to be determined based on randomisation (authors did not respond to a request for further data).
Thirty of the 43 studies (69.8%) included participants dependent on MA only [24,25,26,27,28,29,30, 32,33,34,35, 38,39,40,41, 44, 45, 47,48,49,50, 53,54,55, 57, 59,60,61,62, 65]; four (9.3%) were on MA/AMPH [31, 37, 51, 64]; four (9.3%) were on AMPH only [42, 43, 46, 56]; three (7.0%) were on amphetamine-type stimulants (ATS) and opioids [52, 58, 63] and two (4.7%) were on MA/cocaine [36, 66].
The 43 studies examined 23 individual pharmacotherapies, most individually and some in combination. Table 3 lists the pharmacotherapies reviewed, and the proposed mechanisms of action related to their use in studies of MA/AMPH dependence.
A summary of the reviewed studies is presented in Table 4, and an extended version is available in Supplementary Table 1 (see ESM). In addition, the data collected by both reviewers can be located in its entirety in the Supplementary Data (see ESM).
3.2 Risk of Bias Within and Across Studies
Risk of bias in individual study methods and reporting are included in Supplementary Table 1 and Supplementary Data (see ESM) as considerations across a number of domains. Across all studies, allocation of participants was by random assignment, and all but three studies [46, 56, 66] were double-blind. Study completion rates were low, with studies reporting the proportion of the sample who did not complete the protocol as 38.4% of the total randomised. Eighty-three percent of studies analysed their results by intention-to-treat, while five (12%) [33, 46, 53, 57, 61] were unclear in this regard and two (5%) [24, 45] did not. Females were underrepresented in the data, being only 29.7% of the total participants. This comprises both studies that only enrolled males (nine studies, 21%) [24, 29, 30, 34, 46, 52, 55, 57, 58] and those enrolling both males and females but with higher male enrolments. Thirty-four (79.1%) of the studies we reviewed excluded participants with depression or psychotic disorders, or those taking an antidepressant or antipsychotic medication.
Some authors overstated conclusions; for example, recommending treatment uptake despite limited sample sizes, lack of placebo and/or low completion rates. The studies were overwhelmingly government or academic funded (65.1%, n = 28) [24,25,26,27,28, 30, 32, 33, 35,36,37,38,39,40,41,42, 44, 47, 50, 51, 54, 55, 57, 58, 60, 63, 64, 66]. Ten studies (23.3%) were funded by pharmaceutical companies, or the study drug(s) were provided by a pharmaceutical company, or a mix of funding and drugs were provided by a pharmaceutical company [29, 31, 45, 46, 48, 49, 56, 59, 61, 65]. Four studies (9.3%) did not state their funding source [43, 52, 53, 62], and one study (2.3%) received no funding [34].
3.3 Outcomes and Measures
In total, 55 primary outcome measures were used (inclusive of variations) 93 times (as some studies had multiple primary outcomes). The most common primary outcome measure reported was abstinence (51 times, 55%), followed by cravings (10 times, 11%). For abstinence, urine drug screens (UDS) were used 41 times (80%) and analysed or defined in 16 different ways. The most common method for analysing UDS was weekly proportion of AMPH/MA-free UDS, or overall proportion of AMPH/MA-free UDS. There were 75 distinct secondary outcomes inclusive of variations and often analysed differently to the primary outcomes of the same domain. These were used 158 times. The most common secondary outcome measure reported was craving (25 times), predominantly reported using the visual analogue scale (VAS) (16 times, 64% of the cravings measures). The frequency with which each measure was used is noted in Table 5.
Adherence as an outcome was measured by participant self-report; pill count (i.e. total pills taken divided by total prescribed multiplied by 100 to provide a percentage of adherence); medication electronic monitoring systems (MEMS, e.g. an electronic monitor in bottle caps); proportion of study staff-administered doses received; or measures of metabolites/study drug in plasma. Eleven studies (25.6%) did not report adherence in methods/results. In studies reporting both self-report and another measure, there was low concordance between results. For example, in one study self-reported adherence was 93% but ad-hoc analysis of study drug/metabolite in urine results of participants randomised to the study drug group were presented in quartiles, with the top quartile achieving > 85% positive urines while the bottom quartile showed ≤ 40% positive urines [25]. Adherence reported by both self-report and MEMS caps demonstrated non-concordance in the two studies reporting both—one study reported adherence assessed by MEMS caps was 42% as compared with 74% by self-report [28], another reported 48.5% versus 74.7% [30]. No study reporting plasma metabolite/study drug reported a marker of adherence for placebo. Adherence rates ranged from 21% [51] to 100% [55] across studies. Full data for each study are available in the Supplementary Data (see ESM).
3.4 Results of Individual Studies
3.4.1 Antidepressants
One study (2%) examined amineptine [300 mg oral (po) daily (OD)], an atypical tricyclic antidepressant, in inpatient participants for AMPH withdrawal over 14 days [43]. Participants randomised to amineptine were significantly less depressed at Day 7 and had improved clinical global impression scores at Day 14 in the completer analysis (i.e. only those completing study protocol) compared with placebo. However, the sample size was small (29 analysed). In terms of feasibility, amineptine has never been approved by the US Federal Drug Administration (FDA) and has been suspended in other jurisdictions due to hepatotoxic effects and abuse liability.
Mirtazapine was examined in three studies (7%). Mirtazapine’s effects on withdrawal symptoms were reported on twice, yielding conflicting results. In a 2005 study examining mirtazapine (15–60 mg po OD) in AMPH withdrawal [46], Amphetamine Withdrawal Questionnaire (AWQ) [67] scores between baseline and Days 3 and 14 demonstrated significant differences favouring mirtazapine over placebo, but the study only enrolled 20 participants and the number analysed was unclear. In contrast, with a primary outcome of retention, a 2008 study of mirtazapine (30 mg po OD) for the treatment of MA withdrawal [31] demonstrated no difference in retention rates, or the secondary outcome of MA withdrawal symptoms. The third study [30] aimed to reduce MA use among MA-dependent sexually active men who have sex with men. The proportion of MA-positive UDS was significantly reduced in both study arms over time but was more pronounced and quicker in the mirtazapine (30 mg po OD) arm compared with the control arm. Participants randomised to the mirtazapine arm also reduced their high-risk sexual behaviours (based on a questionnaire), leading the authors to conclude that mirtazapine decreased both MA use and high-risk sexual behaviours in this population, despite fairly low adherence rates by MEMS caps and self-report (< 50%).
Bupropion was examined in six studies (14%) [26, 33, 39, 41, 60, 66]; four reported on AMPH/MA abstinence as the primary outcome, and two on reduction of AMPH/MA use. None of the six studies achieved a statistically significant difference in abstinence or reduction in use between the bupropion and placebo arm in planned primary outcome analyses.
In one study [60], a post hoc analysis found a statistically significant effect for bupropion (150 mg po twice daily [BD]) as compared with placebo when the sample was stratified by ‘baseline light-MA consumers’ (0–2 MA-positive UDS in 2-week baseline period) versus ‘baseline-heavy MA consumers’ (3–6 MA-positive UDS in 2-week baseline period). Among ‘baseline light-MA consumers’, the probability of achieving an MA-free week was significantly higher in the bupropion arm as compared with placebo (odds ratio [OR] of 2.8, p < 0.0001), but there was no statistically significant difference between bupropion and placebo in ‘baseline-heavy MA consumers’. A similar planned sub-group analysis in another study of bupropion (150 mg po BD) for the treatment of MA dependence [33] demonstrated that the sub-group of participants with ≤ 18 days’ MA use in the 30 days prior to baseline who were randomised to bupropion had an increase in weekly periods of MA abstinence as compared with placebo. In additional subgroup analysis, the male-only participants randomised to bupropion also demonstrated a higher proportion of MA-free weeks as compared to placebo [33]. Further analysis determined that two subgroups were significantly more likely to have an MA-free week: male participants with low baseline use (OR 1.39 and OR 1.34; p ≤ 0.001) who were randomised to bupropion; and non-depressed female participants with low baseline use (OR 1.27; p = 0.02) who were randomised to bupropion.
Given bupropion’s licensed indication as a smoking cessation aid, unsurprisingly in one study examining the effects of bupropion on both smoking and stimulant use, participants randomised to bupropion were more likely to reduce their smoking compared with placebo [66].
One study (2%) examined sertraline (50 mg po BD), along with CM for the treatment of MA dependence over 14 weeks [61]. The four study arms were sertraline only, sertraline and CM, placebo only, placebo and CM. There was no statistically significant main or interaction effect of either sertraline or CM for measures of MA use. In fact, those in the sertraline-only arm were significantly less likely to achieve 3-week abstinence and significantly more likely to have an MA-positive UDS throughout the study compared with other study arms.
One study examined imipramine (150 mg po OD) for the treatment of cocaine and MA dependence [36]. The primary outcome was retention in care, and the survival analysis indicated that higher doses of imipramine were associated with enhanced retention in treatment which in turn was associated with more frequent clinical contacts. There were no statistically significant differences between arms on secondary outcomes of time since last MA use, cravings or depression. Notably, 32 of the 183 participants (17.4%) were MA dependent, the rest were cocaine dependent. This study was not placebo controlled, control participants were provided with a reduced dose of imipramine (10 mg versus 150 mg daily), primarily to increase blinding efficacy and acceptability by staff and participants.
A study of atomoxetine (80 mg po OD), a selective norepinephrine (noradrenaline) reuptake inhibitor (SNRI), randomised 69 opioid and ATS-dependent participants to 16 weeks of treatment, assessing ATS use as the primary outcome [58]. The proportion of ATS-negative UDS was higher in the atomoxetine arm compared with placebo, but achieved only a small effect size, while there was no statistically significant difference in days abstinent. For secondary outcomes, the proportion of morphine-negative UDS was lower for the atomoxetine arm, while the depression scores were significantly reduced in the atomoxetine arm compared with placebo [58].
3.4.2 Atypical Antipsychotics
Aripiprazole was assessed in two studies on its own [28, 62], and once in a study that also had a second active agent arm—methylphenidate [64]. Aripiprazole (20 mg po OD) for the treatment of MA dependence was no more effective than placebo in reducing MA consumption or reduction in MA-positive UDS [28]. In another study of the treatment of MA dependence and associated psychoses, participants randomised to aripiprazole (5–10 mg po OD) demonstrated no significant difference in abstinence compared with placebo [62]. However, those randomised to the aripiprazole arm were more likely to be retained in treatment, and to demonstrate a decrease on symptom scores for psychopathology on the Positive and Negative Symptoms Scale (PANSS) [62].
A study investigating aripiprazole versus methylphenidate for AMPH dependence (primary outcome AMPH use, secondary outcomes change in use and retention) enrolled three study arms: aripiprazole 15 mg daily, methylphenidate 54 mg daily or placebo [64]. The aripiprazole study arm had significantly more AMPH-positive UDS compared with either the methylphenidate or placebo arms. The study was ceased early due to this finding at interim analysis. The analysis also demonstrated that participants randomised to the methylphenidate arm returned significantly fewer AMPH-positive UDS than placebo. In addition, two participants (4% of randomised participants) in the aripiprazole arm discontinued the study due to adverse events.
3.4.3 Anticonvulsants
Topiramate was investigated in two studies reviewed here. One study examined topiramate (200 mg po OD) in MA-dependent adults (n = 140 randomised, 77 completed study) with the primary outcome being MA abstinence at Week 12 [32]. While there was no statistically significant difference between topiramate and placebo on the primary outcome, a higher proportion of participants randomised to topiramate reduced their MA use compared with placebo.
In a separate study, topiramate (200 mg po OD) for MA dependence was examined in 62 males and analysed in 57, who were all on prescribed methadone for opiate replacement therapy [55], with the outcomes of interest being dependence severity, cravings, depression and MA use. There was a statistically significant difference between groups on the Addiction Severity Index (drug use severity and drug need domains) that favoured the topiramate arm; however, there was no statistically significant difference in cravings or depression symptoms between the study groups. Participants randomised to topiramate returned significantly fewer MA-positive UDS at Week 6, but this result was not sustained throughout the final 4 weeks of the treatment period [55].
3.4.4 Central Nervous System Stimulants
Two studies reviewed examined dexamphetamine as stimulant agonist treatment. The first study reviewed 49 participants with MA dependence and prescribed 110 mg daily sustained-release oral dexamphetamine over 16 weeks. It measured MA use by self-report and analysis of hair, severity of dependence over time and treatment retention—finding no statistically significant difference between the study groups on planned analysis. Post-hoc analysis demonstrated a reduction in MA dependence symptoms in the dexamphetamine arm compared with placebo using the Leeds Dependence Questionnaire [50]. Secondary analysis included withdrawal symptoms. The participants randomised to dexamphetamine demonstrated a greater reduction in withdrawal severity compared with placebo [50]; however, participants were outpatients and continued MA use complicates the interpretation of withdrawal scores.
Another study examined sustained-release oral dexamphetamine (30 mg po BD) for 60 MA-dependent participants [35]. The primary outcomes included safety and efficacy defined as abstinence from MA—measured by a new MA-positive UDS (measured twice weekly) and self-reported MA consumption. There was no significant difference between study groups on measures of MA consumption; however, the participants randomised to dexamphetamine reported significantly reduced MA withdrawal severity and cravings compared with placebo [35], although these were secondary outcome measures and again in the context of continued MA use by outpatient participants.
Three studies examined sustained/extended-release oral methylphenidate in addition to the study reporting methylphenidate versus aripiprazole discussed earlier. All three were in the outpatient setting and used the same dose (54 mg po OD).
The first randomised 79 MA/AMPH-dependent participants for 22 weeks to methylphenidate or placebo, with abstinence (measured by twice-weekly UDS, and defined as the weekly percentage of AMPH/MA-positive results) as the primary outcome [51]. Twenty-seven participants (34%) completed the study. In intention-to-treat analysis there were no differences in abstinence or study retention rates (defined by number of doses collected), although the methylphenidate arm achieved higher study retention from Week 6. The sample was heterogeneous, as participants were enrolled in both Finland, where all participants took intravenous AMPH, and New Zealand, where all participants smoked MA, but the results were analysed in aggregate. There was no concomitant psychosocial therapy.
Another study enrolled 110 MA-dependent participants in the USA with active study drug for 10 weeks followed by 4 weeks of blinded placebo treatment to encourage follow-up [48]. Participants received weekly CBT and CM. There was no difference between study groups in self-reported MA use in planned analysis of the final 30 days of treatment; however, a secondary analysis of data from baseline to Week 10 found there were significantly fewer self-reported MA use episodes in the methylphenidate arm than placebo.
The final study enrolled 56 Iranian MA-dependent participants for 10 weeks of treatment examining craving as the primary outcome [54]. At Week 10 of the study there was a reduction in craving in the treatment arm, and the treatment arm demonstrated fewer positive UDS and reduced depressive symptoms at Week 10 compared with the placebo arm.
3.4.5 Other Central Nervous System Agents
Modafinil was examined in four studies reviewed here, in doses of 200–400 mg daily. Three were conducted in outpatient settings [25, 38, 59] and one in an inpatient withdrawal setting [47]. One pilot withdrawal study examined feasibility and withdrawal symptoms in 19 participants prescribed 7 days of modafinil (200 mg po OD Days 1–5 and 100 mg po OD Days 6–7) versus placebo. There were no differences between study arms in retention or withdrawal symptoms [47]. None of the other three studies demonstrated a difference in MA use, adherence or retention between study arms. One study analysed a subset of participants with the greatest adherence (> 85%) to study treatment compared with other study participants randomised to modafinil and observed greater abstinence from MA in the > 85% adherent participants; however, the comparison did not include the placebo group and external confounders were not identified or controlled for [25].
3.4.6 GABA Agonist/GABAergic Agents
One 16-week outpatient study of 88 MA-dependent participants examined baclofen (20 mg OD three times daily [TDS]) and gabapentin (800 mg OD TDS) for their effects on MA use [40]. Secondary outcomes included treatment retention, depression, cravings and adverse events. No differences were observed between study arms. Post-hoc analysis demonstrated higher probability of MA-negative urines was associated with medication adherence in all arms, higher in the treatment arm.
3.4.7 Opioid Agonists
Two Iranian studies reviewed examined opioid agonists, one buprenorphine [57] and one buprenorphine and methadone [24]. Both studies were in MA-dependent inpatient males with no co-occurring substance use disorder. In one 16-week study of 40 participants with concomitant psychosocial therapy (Matrix model), reduction in MA cravings and fewer MA-positive UDS were demonstrated among the buprenorphine (6 mg sublingual [SL, i.e. applied under the tongue] OD) arm as compared with the placebo arm during the treatment phase, trending back to baseline following cessation of medication [57]. The second study examined buprenorphine (8 mg SL OD) versus methadone (40 mg po OD) over 17 days, with 20 participants in each study arm. There was a reduction in MA craving compared with placebo, and no participants produced MA-positive UDS in the study period, but the setting was a controlled inpatient environment [24].
3.4.8 Opioid Antagonists
Five studies examined the opioid antagonist naltrexone, including two that used an extended-release formulation [29, 56] and one that used an implant [63]. An additional study reported on naltrexone and n-acetyl cysteine (see below).
Results of the studies are conflicting. There was no difference in MA use by UDS in the treatment arm compared with placebo in the extended-release studies [29, 56]. One study of naltrexone (a single 4-week injection) reported on 37 of 52 randomised participants and found a reduction in past 30-day MA use, but relied entirely on self-report [45], and there was a crossover in primary outcome measures given the past 30-day questionnaires were administered within 3 weeks of each other. One outpatient study of AMPH-dependent participants in Sweden reported fewer AMPH-positive UDS in the naltrexone (50 mg po OD) arm compared with placebo [42], a result shared by the study examining naltrexone implants (1000 mg subcutaneously) administered to Russian participants with AMPH dependence [63].
3.4.9 5HT3-Receptor Antagonist
A single study has investigated ondansetron for the treatment of MA dependence [44]. This four-arm trial assessed different doses of ondansetron (0.5 mg, 2 mg, 8 mg po OD) against placebo in measures of abstinence, use, severity of dependence, withdrawal, craving and retention in treatment. There was no observable difference in any outcome measure between doses or against placebo. The authors suggest that the nil result may be due to the short half-life of ondansetron (approximately 5 h) and suggest a sustained-release formulation or more aggressive dosing may give more efficacious results. At the time of this review no follow-up studies had been conducted.
3.4.10 Partial Cholinergic Nicotinic Agonists
A single, recent American study assessed varenicline (1 mg po BD) as a pharmacotherapy for MA dependence [27]. There were no differences between treatment and placebo arms for any measures of dependence; however, there was a reduction in cigarettes smoked in the treatment arm (consistent with its licensed indication as a smoking cessation medication).
3.4.11 Glutamatergic Agents
Glutamatergic agents have been assessed, as either riluzole [34], N-acetyl cysteine (NAC) [53], or a combination of NAC and naltrexone [37]. A recent trial of Iranian men found that riluzole (50 mg po OD) was associated with higher rates of retention in treatment and abstinence at Week 12, as well as overall improvements in a range of secondary outcomes [34]. Efficacy for NAC is conflicted, however. When trialled as a combination of NAC (escalating dose to 2400 mg po OD) with naltrexone (escalating dose to 200 mg po OD), there was no difference between arms in measures of craving, use or psychological scales [37]. Mousavi et al., however, found that NAC treatment (escalating dose to 1200 mg po OD) was associated with a reduction in craving. This paper did not report on secondary outcomes [53]. Both studies had low participant numbers (n = 31 and n = 32, respectively). Mousavi et al. [53] allowed weekly ‘matrix model’ psychological therapy to all participants, while Grant et al. [37] did not provide any psychosocial support, and this may explain the discrepancies in results.
3.4.12 CRF1 Antagonist
We reviewed pexacerfont in one study, a 3-week trial of 51 Iranian men within residential treatment camps where treatment is not normally provided [52]. Dosing was tapered from 300 mg po OD for the first week, to 200 mg po OD in Week 2 and 100 mg po OD in Week 3. While measures of craving reduced significantly more in the treatment arm than placebo, there was no difference in end-of-treatment abstinence between groups. Additionally, levels of temptation and depression, but not anxiety, withdrawal severity, or treatment effectiveness, improved favouring treatment.
3.4.13 Benzodiazepine Antagonist/GABA Agonist/H1 Histamine Receptor
The combination therapy of flumazenil (2 mg intravenous Days 1, 2, 3, 21, 22), gabapentin (titrated up to 1200 mg po OD) and hydroxyzine (50 mg po pre-intravenous medication and as required for sleep), marketed and trademarked as the ‘PROMETA protocol’, has been assessed twice in RCTs for MA dependence. Both trials were similar in terms of participant numbers and followed an identical medication protocol; however, results were conflicting. A 30-day trial found significantly improved craving scores, but no difference in use (missing UDS imputed as positive) [65]. However, a 40-day trial conducted the same year found no differences in any measures, including craving [49].
4 Discussion
4.1 Summary of Evidence
We reviewed 43 RCTs reporting on 4065 participants that examined 23 pharmacotherapies for SUD or drug dependence due to AMPH/MA with various outcomes pertaining to use and associated symptoms. While some drugs demonstrated results that were statistically significantly better than placebo outcomes, the studies were generally small and the samples biased and study protocol completion was low. This makes it impossible to recommend any pharmacotherapy as effective at this point in time, although there are some promising signals.
4.2 Reduction in Use
There are a few pharmacotherapy candidates for the treatment of AMPH/MA dependence/use disorder that demonstrate some weak positive signals. The most consistent positive findings have been demonstrated with stimulant agonist treatment (dexamphetamine and methylphenidate), naltrexone and topiramate. Less consistent benefits have been shown with bupropion, the glutamatergic agent, riluzole, and antidepressant mirtazapine, whilst in general, antidepressant medications (e.g. SSRIs, TCAs) have not been effective in reducing AMPH/MA use.
Substitution/replacement medication approaches (i.e. agonist therapies) have demonstrated positive outcomes for other drug classes (e.g. nicotine replacement for tobacco/cigarettes, methadone for opioids, nabiximols for cannabis). Stimulant agonist treatment with dexamphetamine demonstrated promising results in post hoc and secondary analyses in the two studies reviewed here [35, 50], but predominantly with regard to withdrawal and craving symptoms in the context of continued AMPH/MA use. Methylphenidate delivered mixed results when assessed for varying outcomes. One study demonstrating higher retention rates in methylphenidate arms compared with placebo was limited by a heterogeneous study sample [51]. Conversely, lower MA use by self-report in the methylphenidate arm compared with placebo was reported in a study (n = 110) that concurrently used CBT and CM [48]; and reductions in craving and MA-positive UDS was reported in a study enrolling 56 participants [54]. Other work in this area is ongoing. One study [68] is currently examining 12 weeks of lisdexamfetamine (a pro-drug of dexamphetamine) versus placebo in a double-blind, RCT of MA-dependent (for at least 2 years) adults with baseline use of at least 14 of the prior 28 days.
The studies we reviewed here that examined the opioid antagonist naltrexone demonstrated conflicting results, but there were signals in both daily oral [42] and long-acting formulations (i.e. subcutaneous implant) [63] that naltrexone may reduce AMPH use. Recently, a large (n = 403) USA study of extended-release naltrexone (380 mg by intramuscular injection every 3 weeks) and bupropion (450 mg po OD) versus placebo completed enrolment. The primary outcome in this study was the percentage of UDS negative for MA during the 12 weeks of treatment, and results are pending (Trivedi et al.; ClinicalTrials.gov identifier: NCT03078075).
Topiramate was assessed in two studies reviewed here [32, 55], demonstrating reduced use and addiction severity compared with placebo. Furthermore, a secondary analysis of Elkashef et al. [32] found higher responders within groups in a latent class analysis [69], suggesting further studies with different eligibility criteria are warranted.
In baseline light-MA users or in men, bupropion demonstrated a reduction in MA use [60]. Encouragingly, it also reduced concurrent tobacco use in participants [66]. There are known interaction effects of nicotine and methamphetamine and a potential role of nicotine use in maintaining their co-use [70].
One study of 86 men examining the benzothiazole riluzole demonstrated positive results [34], with participants randomised to riluzole more likely to be retained in treatment and provide MA-negative UDS than those randomised to placebo. However, the study excluded participants who smoked cigarettes > 3 days per week. Further studies in more diverse settings are required.
In men who have sex with men, the antidepressant mirtazapine reduced MA use and high-risk sexual behaviours, despite low medication adherence rates [30]. In another study published by this group since our search, 120 cisgender males and transgender females who had sex with men and had MA use disorder were randomly assigned to mirtazapine 30 mg or placebo OD for 24 weeks with a further 12 weeks’ follow-up [71]. The primary outcome was MA-positive urines and secondary outcomes were sexual risk behaviours. Results were replicated, with reductions in both MA use and, although to a lesser extent than the first study and only at week 24, high-risk sexual behaviours (unprotected anal sex, number of partners) in participants randomised to mirtazapine as compared with placebo. Adherence was still imperfect, with an average of 28.1–39.5% medication adherence between the two arms. Participants received concomitant psychosocial therapy, and the authors suggest that mirtazapine may be a useful adjunct to psychosocial therapy, but only in the examined population.
There are currently other ongoing (recruiting) pharmacotherapy studies for AMPH/MA dependence. These include a double-blind placebo-controlled study of NAC (1200 mg po BD) in outpatients over 12 weeks [72] currently recruiting in Australia. A phase I study examining the safety of ascending doses of pomaglumetad (an mGlutamate 2, 3 agonist) in 24 non-treatment-seeking participants is underway in the USA (Heinzerling et al.; ClinicalTrials.gov identifier: NCT03106571). A monoclonal antibody (IXT-m200) is being investigated in a randomised, placebo-controlled study as a single dose followed by four MA ‘challenge doses’ for its effects on the pharmacokinetics of MA and implications for its effects on drug liking (Ward et al.; ClinicalTrials.gov identifier: NCT03336866).
4.3 Treatment of Withdrawal Symptoms
It should be noted that our search strategy did not seek to identify studies that were specifically for the treatment of AMPH/MA withdrawal. However, five studies in our review focused on pharmacotherapy for MA withdrawal with withdrawal measures as the primary outcome. Three of these were included in a 2009 Cochrane Review [73] of pharmacotherapies for AMPH withdrawal: a 1997 Thai study of amineptine in AMPH withdrawal [43], a 2005 study examining mirtazapine in AMPH withdrawal [46] and a 2008 study of mirtazapine in MA withdrawal [31]. The Cochrane Review included a fourth study not reviewed here. The results of the meta-analyses undertaken in the Cochrane review demonstrated that amineptine did not reduce withdrawal symptoms or cravings compared with placebo, while the mirtazapine studies yielded mixed results, with one study demonstrating a small reduction in withdrawal symptoms on the AWQ for those randomised to mirtazapine, while the other demonstrated no difference in withdrawal symptoms on the Amphetamine Cessation Symptoms Assessment (ACSA) [73]. The authors concluded that no medication was demonstrated to be effective in reducing AMPH withdrawal symptoms [73].
Our review also identified several other studies published since the Cochrane Review reporting on withdrawal. In studies reviewed here examining withdrawal symptoms, no pharmacotherapy yielded robustly convincing results, while some had marked limitations; for example, in a recent Iranian study of riluzole (n = 74) [34], secondary outcomes included the AWQ [67]; however, it excluded any participants who smoked cigarettes more than 3 days per week, severely limiting its generalisability to stimulant consumers more broadly. Overall, the studies we reviewed signalled some potential promise in agonist therapy (dexamphetamine), CRF1 antagonist therapy (pexacerfont) and glutamatergic agents (riluzole) as potential pharmacotherapy candidates for MA withdrawal; however, further larger studies in the withdrawal context are required.
Although there are no evidence-based pharmacotherapies for AMPH/MA withdrawal [74], standard of care generally includes symptomatic medications that target symptoms of withdrawal, including short-term use of benzodiazepines (e.g. diazepam) for anxiety, agitation and sleep disturbances, and antipsychotics (e.g. olanzapine) to manage any comorbid psychotic symptoms [74]. Research is required on pharmacotherapy of stimulant withdrawal.
4.4 Treatment Setting
The majority of studies we reviewed were in the outpatient setting (n = 32, 74.4%), while a minority were conducted in inpatient settings (n = 5, 11.6%) and the rest were mixed or did not state the setting.
No study we reviewed directly compared outcomes between outpatient- and inpatient-treated participants. Importantly, we did not find any evidence that either treatment setting is superior to another for any of the outcomes we assessed. Hence, we suggest that criteria for the selection of treatment setting are based on clinical judgement and resources. For example, when managing stimulant withdrawal, the likelihood of severe complications (e.g. potential for severe psychiatric and cardiovascular complications during AMPH/MA withdrawal) may favour a period of inpatient treatment, whereas most AMPH/MA withdrawals could safely be completed in an ambulatory setting. Likewise, significant comorbidity (e.g. psychoses) may impact the ability to remain in ambulatory care during periods of treatment for AMPH/MA withdrawal or treatment. Other substance use and social environments will also feature when determining the best setting for clinical care [75].
Similarly, the choice between residential or ambulatory treatment settings for longer term rehabilitation programmes may be determined by factors such as social supports, housing, employment and legal status of the patient.
4.5 Specific Populations
Nearly a quarter of the reviewed studies had no female participants, and male sex made up over 70% of the population across all studies. In nine of the studies reviewed here (20.9%), women were excluded by design. In some cases, this was due to the setting (e.g. male-only residential treatment centres), or studies conducted in specific populations (e.g. men who have sex with men), and in others the reason is not clearly stated. Research suggests women who take stimulants are more likely to become dependent consumers than men who take stimulants [77]. While women are underrepresented in the reviewed studies as a proportion of the population overall, they may not be underrepresented as a proportion of the population who present for treatment. For example, in the US, the setting of over half of the studies reviewed here, only 36% of people estimated to have accessed treatment for illicit drug use in 2016 were female [77, 78].Women are more likely to encounter barriers to alcohol and other drug treatment than men, which may explain why they are under-represented in the studies reviewed here. This is due in large part to fear of losing access to children (e.g. due to mandatory reporting), and family responsibilities (lack of alternate options for childcare, etc.); women are also more likely to encounter economic barriers to treatment access than are men [76].
4.6 Limitations
Seventy-nine percent of the reviewed studies excluded participants with comorbid mental health diagnoses or concomitant medications prescribed for comorbid mental health diagnoses. Research suggests that transient psychotic symptoms are observed in up to 40% of MA-using populations [79] and possibly more amongst treatment seekers. Forty-two percent of individuals who had used MA in the prior 12 months also reported being diagnosed or treated for a concurrent mental illness—three times as high as the non-illicit drug-using population [80]. Among MA users, the majority report a lifetime prevalence of depression and anxiety [81]. The exclusion of relatively common comorbidities such as polydrug dependence and mental health comorbidities limits the generalisability of many of the studies. For example, the role of antipsychotic and antidepressant medications may differ in patients presenting with psychosis or depression. Similarly, dependence to other substances such as alcohol, benzodiazepines or opioids is also likely to impact upon the safety and efficacy and choice of medications. Medications such as topiramate and naltrexone may be worth further examination in patients with comorbid alcohol use, whereas the role of naltrexone will vary according to opioid status; for example, responding to stimulant use in patients enrolled in opioid agonist treatment. Other comorbidities that continue to be poorly addressed include the management of patients with stimulant dependence and comorbid attention-deficit hyperactivity disorder (ADHD). Accurate diagnoses of ADHD in the context of AMPH/MA use can be complicated [82], and there may be differential effects of medications in patients with both conditions. More research is required regarding pharmacological responses for patients with ADHD and stimulant use disorders. Another key area that has not been adequately addressed in clinical trials is the issue of comorbid sleep disturbances in patients using AMPH/MA, and the likely impact upon the role of different medications.
The studies reviewed here report on a variety of outcomes defined, measured and analysed differently across most publications. The broad selection of outcomes and measures render it difficult to meta-analyse or otherwise collectively synthesise the study results as reported. Future endeavours to standardise outcome measures across clinical trials in addiction medicine would make it easier to interpret study results collectively and better translate research results to clinical practice. Importantly, only three studies reviewed here (7%) provided information on adverse events/serious adverse events, despite the standard reporting format adopted by most publishers (CONSORT [83]) including a minimum standard of harm reporting. This limits the capacity to appropriately assess the risk versus benefit of the pharmacotherapies reviewed here. We elected to include studies in this review irrespective of safety reporting, to provide a comprehensive review of the current status of research.
Although adherence was reported in most of the studies reviewed here, the methods and definitions were discordant across studies. Adherence thresholds varied and were often arbitrary. When plasma was assessed for active study drug/metabolite, there was no measurable metabolite included in the placebo, and the control data is therefore missing. Furthermore, presence of the study drug/metabolite does not necessarily indicate adherent consumption of the study drug, and authors varied in their assessments in that regard (i.e. present or not versus present at a defined level). Studies relying on pill count or self-report lacked critical appraisal of the results. For example, in one study where no participant returned un-used study drug, 100% adherence was inferred as opposed to examining if there were other reasons (e.g. discarding drug).
Definitions of efficacy of pharmacotherapies vary extensively. While some studies define success by abstinence from AMPH/MA, others consider a reduction in use to be a measure of treatment success. Abstinence as an outcome can be determined by self-report, or by negative UDS at time points pre-determined (see Table 5). The desired goal of pharmacotherapy will likely vary depending on the patient, and must be patient-focused and clinically relevant.
Disparate criteria were also used when determining eligibility for a study; for example, the definition of ‘low-use’ (AMPH/MA) in the studies reviewed here was 5 days, 10 days and 18 days of the past 30 in various studies. This is an important limitation in synthesising data and results, and establishment of a clinically meaningful cut-off for regular and frequent use is imperative. Studies that analysed results by baseline frequency of MA/AMPH use often grouped days of use into categories defined as ‘light use’ or ‘heavy use’. However, rationale for cut-points was often missing or ill-defined. In one study, consumption of MA was classified as ‘heavy use’ among participants providing three MA-positive UDS/fortnight, while in another study, ‘heavy use’ was classified as self-reported use of 18 days of the prior 30. In a 2007 paper, Hillhouse et al. [19] found that frequency of MA use prior to treatment predicted both treatment performance and outcomes following treatment in a psychosocial intervention for MA dependence, reporting that participants with baseline use of < 15 days in the 30 days prior to intake had better outcomes. Therefore, the disparity in groupings in pharmacotherapy research across studies and drugs makes it difficult to reliably recommend a strategy for determining cut-points. Further research and debate in this area is required to determine a clinically meaningful way of grouping frequency of use.
Studies conducted in (e.g. men who have sex with men) or excluding (e.g. women) specific populations are limited in their ability to generalise to other populations. The implications of contextual influences on outcomes are unknown. For example, no study we reviewed here assessed specific populations such as indigenous peoples. Similarly, while women were often excluded by the study design, no study examined only women. It is unknown how generalisable any of the results reviewed here are outside of the context in which they were conducted, and it is unwise therefore to combine results across populations.
Finally, because of the similarities in chemical structure and behavioural, psychological and physical effects of AMPH and MA [84], we have included studies of AMPH and MA, and studies that did not distinguish between AMPH and MA. MA and AMPH may be knowingly or unknowingly consumed or co-consumed in uncertain concentrations, with variability over time and place. However, there is little data on which to assess whether there are distinct differences in use disorders due to these two substances; further assessment is required.
4.7 Future Directions
Future research should address small sample sizes and low participant retention and treatment adherence rates, leading to underpowered studies lacking meaningful results. Under-powered results can be avoided by planning recruitment for high attrition rates, collaborating on multi-centre research, potentially through clinical research networks, and a greater role for consumer and clinician engagement in the planning and establishment of trials. Medication adherence also needs to be better examined and monitored in trials, particularly when using medications with abuse liability (e.g. psychoactive medications such as stimulants).
Populations under-represented in the literature must also be addressed in future research. Harmonisation of outcomes and outcome measures to produce results that can be synthesised by meta-analyses should be a sector-wide imperative, to ensure better research synthesis. At a minimum, reduction in MA/AMPH use (e.g. days used or reduction in MA/AMPH-positive UDS) is required for assessment of efficacy. The reliance on extended periods of ‘abstinence’ as a primary endpoint does not always reflect participant treatment goals and is a somewhat insensitive marker of clinically meaningful change in substance use. However, further work is required to determine outcomes that are both clinically meaningful and meaningful to consumers.
Future research should address the need to understand the influence of co-existing conditions (e.g. ADHD, depression, comorbid substance use [e.g. tobacco, alcohol, opioids, benzodiazepines], psychosis, sleep disorders, complex trauma), increasing the likelihood of generating results that can be generalised to participants with comorbid conditions consistent with the underlying population.
Studies examining the efficacy of pharmacotherapy alone versus combined medication and psychosocial counselling are required to better understand the role each treatment modality may have. Provision of client-centred care requires future work to address the need to better understand concepts of treatment matching or stepped care. Not all patients may need or benefit from the same approach. Further, treatments may differ by dose and frequency (intensity) of use. Irrespective of the promise of pharmacotherapy, effective treatment of substance use disorders requires comprehensive biopsychosocial intervention.
5 Conclusions
While there are promising candidates, no pharmacotherapy for the treatment of AMPH/MA dependence/use disorder has provided convincing results. Studies are often limited by small sample sizes in defined populations, and with low treatment retention or completion rates. Different treatment options may be indicated for various degrees of severity of disorder. Combination therapies are yet to be explored. Optimal psychosocial interventions accompanying medication must also be considered. Further and substantial investment to determine effective pharmacotherapies is required.
References
World Drug Report 2019 (United Nations publication, Sales No. E.19.XI.9).
Stoneburg D, Shukla R, Magness M. Global methamphetamine trends: an evolving problem. Int Crim Justice Rev. 2018;28(2):136–61.
Meredith CW, Jaffe C, Ang-Lee K, Saxon AJ. Implications of chronic methamphetamine use: a literature review. Harv Rev Psychiat. 2005;13(3):141–54.
Silber BY, Croft RJ, Papafotiou K, Stough C. The acute effects of d-amphetamine and methamphetamine on attention and psychomotor performance. Psychopharmacology. 2006;187(2):154–69.
Haber P, Day C, Farrell M, editors. Addiction medicine: principles and practice. Research: IP Communications, Pty. Ltd; 2015.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-V). 5th ed. Washington: American Psychiatric Association; 2016.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-IV). 4th ed. Washington: American Psychiatric Association; 1994.
World Health Organization. ICD-10: International statistical classification of diseases and related health problems: 10th rev. 2nd ed. Geneva: World Health Organisation; 2004.
World Health Organization. ICD-11: International classification of diseases for mortality and morbidity statistics: 11th rev. Geneva: World Health Organisation; 2018.
Farrell M, Martin NK, Stockings E, Borquez A, Cepeda JA, Degenhardt L, et al. Responding to global stimulant use: challenges and opportunities. Lancet. 2019;394(10209):1652–67.
Karila L, Petit A, Cottencin O, Reynaud M. Methamphetamine dependence: consequences and complications. Presse Med. 2010;39(12):1246–53.
Chomchai C, Chomchai S. Global patterns of methamphetamine use. Curr Opin Psychiatry. 2015;28(4):269–74.
United Nations Office on Drugs and Crime. Treatment of stimulant use disorder: Current practices and promising perspectives. Vienna: United Nations Office on Drugs and Crime; 2019.
Lee NK, Rawson RA. A systematic review of cognitive and behavioural therapies for methamphetamine dependence. Drug Alcohol Rev. 2008;27(3):309–17.
Harada T, Tsutomi H, Mori R, Wilson DB. Cognitive-behavioural treatment for amphetamine-type stimulants (ATS)-use disorders. Cochrane Database Syst Rev. 2018;12:cd011315.
Shoptaw S, Reback CJ, Peck JA, Yang X, Rotheram-Fuller E, Larkins S, et al. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug Alcohol Depend. 2005;78(2):125–34.
De Crescenzo F, Ciabattini M, D’Alò GL, De Giorgi R, Del Giovane C, Cassar C, et al. Comparative efficacy and acceptability of psychosocial interventions for individuals with cocaine and amphetamine addiction: A systematic review and network meta-analysis. PLoS Med. 2018;15(12):e1002715.
Rawson RA, McCann MJ, Flammino F, Shoptaw S, Miotto K, Reiber C, et al. A comparison of contingency management and cognitive-behavioral approaches for stimulant-dependent individuals. Addiction. 2006;101(2):267–74.
Hillhouse MP, Marinelli-Casey P, Gonzales R, Ang A, Rawson RA. Predicting in-treatment performance and post-treatment outcomes in methamphetamine users. Addiction. 2007;102(Suppl 1):84–95.
McKetin R, Najman JM, Baker AL, Lubman DI, Dawe S, Ali R, et al. Evaluating the impact of community-based treatment options on methamphetamine use: findings from the methamphetamine treatment evaluation study (MATES). Addiction. 2012;107(11):1998–2008.
United Nations Office on Drugs and Crime (UNODC). Terminology and Information on Drugs. 3rd ed. New York: United Nations; 2016.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. www.covidence.org.
Ahmadi J, Razeghian Jahromi L. Comparing the effect of buprenorphine and methadone in the reduction of methamphetamine craving: a randomized clinical trial. Trials. 2017;18(1):259.
Anderson AL, Li SH, Biswas K, McSherry F, Holmes T, Iturriaga E, et al. Modafinil for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2012;120(1–3):135–41.
Anderson AL, Li SH, Markova D, Holmes TH, Chiang N, Kahn R, et al. Bupropion for the treatment of methamphetamine dependence in non-daily users: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. 2015;150:170–4.
Briones M, Shoptaw S, Cook R, Worley M, Swanson AN, Moody DE, et al. Varenicline treatment for methamphetamine dependence: a randomized, double-blind phase II clinical trial. Drug Alcohol Depend. 2018;189:30–6.
Coffin PO, Santos GM, Das M, Santos DM, Huffaker S, Matheson T, et al. Aripiprazole for the treatment of methamphetamine dependence: a randomized, double-blind, placebo-controlled trial. Addiction. 2013;108(4):751–61.
Coffin PO, Santos GM, Hern J, Vittinghoff E, Santos D, Matheson T, et al. Extended-release naltrexone for methamphetamine dependence among men who have sex with men: a randomized placebo-controlled trial. Addiction. 2018;113(2):268–78.
Colfax GN, Santos GM, Das M, Santos DM, Matheson T, Gasper J, et al. Mirtazapine to reduce methamphetamine use: a randomized controlled trial. Arch Gen Psychiatry. 2011;68(11):1168–75.
Cruickshank CC, Montebello ME, Dyer KR, Quigley A, Blaszczyk J, Tomkins S, et al. A placebo-controlled trial of mirtazapine for the management of methamphetamine withdrawal. Drug Alcohol Rev. 2008;27(3):326–33.
Elkashef A, Kahn R, Yu E, Iturriaga E, Li SH, Anderson A, et al. Topiramate for the treatment of methamphetamine addiction: a multi-center placebo-controlled trial. Addiction. 2012;107(7):1297–306.
Elkashef AM, Rawson RA, Anderson AL, Li SH, Holmes T, Smith EV, et al. Bupropion for the treatment of methamphetamine dependence. Neuropsychopharmacology. 2008;33(5):1162–70.
Farahzadi MH, Moazen-Zadeh E, Razaghi E, Zarrindast MR, Bidaki R, Akhondzadeh S. Riluzole for treatment of men with methamphetamine dependence: a randomized, double-blind, placebo-controlled clinical trial. J Psychopharmacol. 2019;33(3):305–15.
Galloway GP, Buscemi R, Coyle JR, Flower K, Siegrist JD, Fiske LA, et al. A randomized, placebo-controlled trial of sustained-release dextroamphetamine for treatment of methamphetamine addiction. Clin Pharmacol Therapeutics. 2011;89(2):276–82.
Galloway GP, Newmeyer J, Knapp T, Stalcup SA, Smith D. Imipramine for the treatment of cocaine and methamphetamine dependence. J Addict Dis. 1994;13(4):201–16.
Grant JE, Odlaug BL, Kim SW. A double-blind, placebo-controlled study of N-acetyl cysteine plus naltrexone for methamphetamine dependence. Eur Neuropsychopharmacol. 2010;20(11):823–8.
Heinzerling KG, Swanson AN, Kim S, Cederblom L, Moe A, Ling W, et al. Randomized, double-blind, placebo-controlled trial of modafinil for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2010;109(1–3):20–9.
Heinzerling KG, Gadzhyan J, van Oudheusden H, Rodriguez F, McCracken J, Shoptaw S. Pilot randomized trial of bupropion for adolescent methamphetamine abuse/dependence. J Adolesc Health. 2013;52(4):502–5.
Heinzerling KG, Shoptaw S, Peck JA, Yang X, Liu J, Roll J, et al. Randomized, placebo-controlled trial of baclofen and gabapentin for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2006;85(3):177–84.
Heinzerling KG, Swanson AN, Hall TM, Yi Y, Wu Y, Shoptaw SJ. Randomized, placebo-controlled trial of bupropion in methamphetamine-dependent participants with less than daily methamphetamine use. Addiction. 2014;109(11):1878–86.
Jayaram-Lindström N, Hammarberg A, Beck O, Franck J. Naltrexone for the treatment of amphetamine dependence: a randomized, placebo-controlled trial. Am J Psychiatry. 2008;165(11):1442–8.
Jittiwutikan J, Srisurapanont M, Jarusuraisin N. Amineptine in the treatment of amphetamine withdrawal: a placebo-controlled, randomised, double-blind study. J Med Assoc Thai. 1997;80(9):587–92.
Johnson BA, Ait-Daoud N, Elkashef AM, Smith EV, Kahn R, Vocci F, et al. A preliminary randomized, double-blind, placebo-controlled study of the safety and efficacy of ondansetron in the treatment of methamphetamine dependence. Int J Neuropsychopharmacol. 2008;11(1):1–14.
Kohno M, Dennis LE, McCready H, Schwartz DL, Hoffman WF, Korthuis PT. A preliminary randomized clinical trial of naltrexone reduces striatal resting state functional connectivity in people with methamphetamine use disorder. Drug Alcohol Depend. 2018;192:186–92.
Kongsakon R, Papadopoulos KI, Saguansiritham R. Mirtazapine in amphetamine detoxification: a placebo-controlled pilot study. Int Clin Psychopharmacol. 2005;20(5):253–6.
Lee N, Pennay A, Hester R, McKetin R, Nielsen S, Ferris J. A pilot randomised controlled trial of modafinil during acute methamphetamine withdrawal: feasibility, tolerability and clinical outcomes. Drug Alcohol Rev. 2013;32(1):88–95.
Ling W, Chang L, Hillhouse M, Ang A, Striebel J, Jenkins J, et al. Sustained-release methylphenidate in a randomized trial of treatment of methamphetamine use disorder. Addiction. 2014;109(9):1489–500.
Ling W, Shoptaw S, Hillhouse M, Bholat MA, Charuvastra C, Heinzerling K, et al. Double-blind placebo-controlled evaluation of the PROMETA protocol for methamphetamine dependence. Addiction. 2012;107(2):361–9.
Longo M, Wickes W, Smout M, Harrison S, Cahill S, White JM. Randomized controlled trial of dexamphetamine maintenance for the treatment of methamphetamine dependence. Addiction. 2010;105(1):146–54.
Miles SW, Sheridan J, Russell B, Kydd R, Wheeler A, Walters C, et al. Extended-release methylphenidate for treatment of amphetamine/methamphetamine dependence: a randomized, double-blind, placebo-controlled trial. Addiction. 2013;108(7):1279–86.
Morabbi MJ, Razaghi E, Moazen-Zadeh E, Safi-Aghdam H, Zarrindast MR, Vousoghi N, et al. Pexacerfont as a CRF1 antagonist for the treatment of withdrawal symptoms in men with heroin/methamphetamine dependence: a randomized, double-blind, placebo-controlled clinical trial. Int Clin Psychopharmacol. 2018;33(2):111–9.
Mousavi SG, Sharbafchi MR, Salehi M, Peykanpour M, Karimian Sichani N, Maracy M. The efficacy of N-acetylcysteine in the treatment of methamphetamine dependence: a double-blind controlled, crossover study. Arch Iranian Med. 2015;18(1):28–33.
Rezaei F, Emami M, Zahed S, Morabbi MJ, Farahzadi M, Akhondzadeh S. Sustained-release methylphenidate in methamphetamine dependence treatment: a double-blind and placebo-controlled trial. Daru. 2015;23:2.
Rezaei F, Ghaderi E, Mardani R, Hamidi S, Hassanzadeh K. Topiramate for the management of methamphetamine dependence: a pilot randomized, double-blind, placebo-controlled trial. Fundam Clin Pharmacol. 2016;30(3):282–9.
Runarsdottir V, Hansdottir I, Tyrfingsson T, Einarsson M, Dugosh K, Royer-Malvestuto C, et al. Extended-release injectable naltrexone (XR-NTX) with intensive psychosocial therapy for amphetamine-dependent persons seeking treatment: a placebo-controlled trial. J Addict Med. 2017;11(3):197–204.
Salehi M, Emadossadat A, Kheirabadi GR, Maracy MR, Sharbafchi MR. The effect of buprenorphine on methamphetamine cravings. J Clinical Psychopharmacol. 2015;35(6):724–7.
Schottenfeld RS, Chawarski MC, Sofuoglu M, Chooi WT, Zaharim NM, Yasmin M, et al. Atomoxetine for amphetamine-type stimulant dependence during buprenorphine treatment: a randomized controlled trial. Drug Alcohol Depend. 2018;186:130–7.
Shearer J, Darke S, Rodgers C, Slade T, van Beek I, Lewis J, et al. A double-blind, placebo-controlled trial of modafinil (200 mg/day) for methamphetamine dependence. Addiction. 2009;104(2):224–33.
Shoptaw S, Heinzerling KG, Rotheram-Fuller E, Steward T, Wang J, Swanson AN, et al. Randomized, placebo-controlled trial of bupropion for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2008;96(3):222–32.
Shoptaw S, Huber A, Peck J, Yang X, Liu J, Jeff D, et al. Randomized, placebo-controlled trial of sertraline and contingency management for the treatment of methamphetamine dependence. Drug Alcohol Depend. 2006;85(1):12–8.
Sulaiman AH, Gill JS, Said MA, Zainal NZ, Hussein HM, Guan NC. A randomized, placebo-controlled trial of aripiprazole for the treatment of methamphetamine dependence and associated psychosis. Int J Psychiatry Clin Pract. 2013;17(2):131–8.
Tiihonen J, Krupitsky E, Verbitskaya E, Blokhina E, Mamontova O, Fohr J, et al. Naltrexone implant for the treatment of polydrug dependence: a randomized controlled trial. Am J Psychiatry. 2012;169(5):531–6.
Tiihonen J, Kuoppasalmi K, Fohr J, Tuomola P, Kuikanmaki O, Vorma H, et al. A comparison of aripiprazole, methylphenidate, and placebo for amphetamine dependence. Am J Psychiatry. 2007;164(1):160–2.
Urschel HC 3rd, Hanselka LL, Baron M. A controlled trial of flumazenil and gabapentin for initial treatment of methylamphetamine dependence. J Psychopharmacol. 2011;25(2):254–62.
Winhusen TM, Brigham GS, Kropp F, Lindblad R, Gardin JG 2nd, Penn P, et al. A randomized trial of concurrent smoking-cessation and substance use disorder treatment in stimulant-dependent smokers. J Clin Psychiatry. 2014;75(4):336–43.
Srisurapanont M, Jarusuraisin N, Jittiwutikan J. Amphetamine withdrawal: I. Reliability, validity and factor structure of a measure. Aust NZ J Psychiatry. 1999;33(1):89–93.
Ezard N, Dunlop A, Hall M, Ali R, McKetin R, Bruno R, et al. LiMA: a study protocol for a randomised, double-blind, placebo controlled trial of lisdexamfetamine for the treatment of methamphetamine dependence. BMJ Open. 2018;8(7):e020723.
Ma JZ, Johnson BA, Yu E, Weiss D, McSherry F, Saadvandi J, et al. Fine-grain analysis of the treatment effect of topiramate on methamphetamine addiction with latent variable analysis. Drug Alcohol Depend. 2013;130(1–3):45–51.
Gatch MB, Flores E, Forster MJ. Nicotine and methamphetamine share discriminative stimulus effects. Drug Alcohol Depend. 2008;93(1–2):63–71.
Coffin PO, Santos GM, Hern J, Vittinghoff E, Walker JE, Matheson T, et al. Effects of mirtazapine for methamphetamine use disorder among cisgender men and transgender women who have sex with men: a placebo-controlled randomized clinical trial. JAMA Psychiatry. 2020;77(3):246–55.
McKetin R, Dean OM, Turner A, Kelly PJ, Quinn B, Lubman DI, et al. A study protocol for the N-ICE trial: a randomised double-blind placebo-controlled study of the safety and efficacy of N-acetyl-cysteine (NAC) as a pharmacotherapy for methamphetamine (“ice”) dependence. Trials. 2019;20(1):325.
Shoptaw SJ, Kao U, Heinzerling K, Ling W. Treatment for amphetamine withdrawal. Cochrane Database Syst Rev. 2009;2:Cd003021.
Wodarz N, Krampe-Scheidler A, Christ M, Fleischmann H, Looser W, Schoett K, et al. Evidence-based guidelines for the pharmacological management of acute methamphetamine-related disorders and toxicity. Pharmacopsychiatry. 2017;50(3):87–95.
Lintzeris N, Sunjic S, Demirkol A, Branezac M, Ezard N, Siefried K, et al. Management of withdrawal from alcohol and other drugs: an evidence check rapid review brokered by the Sax Institute for the NSW Ministry of Health. Sydney: The Sax Institute; 2019.
Green CA. Gender and use of substance abuse treatment services. Alcohol Res Health. 2006;29(1):55–62.
National Institute on Drug Abuse (NIDA). Substance use in women. 2020.
Center for Behavioral Health Statistics and Quality. Results from the 2016 national survey on drug use and health: detailed tables. Rockville: Substance Abuse and Mental Health Services Administration; 2017.
Glasner-Edwards S, Mooney LJ. Methamphetamine psychosis: epidemiology and management. CNS Drugs. 2014;28(12):1115–26.
Australian Institute of Health and Welfare. National drug strategy household survey 2016: detailed findings. Canberra: Australian Institute of Health and Welfare; 2017.
Darke S, Kaye S, McKetin R, Duflou J. Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev. 2008;27(3):253–62.
Clemow DB, Walker DJ. The potential for misuse and abuse of medications in ADHD: a review. Postgrad Med. 2014;126(5):64–81.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152(11):726–32.
Kirkpatrick MG, Gunderson EW, Johanson CE, Levin FR, Foltin RW, Hart CL. Comparison of intranasal methamphetamine and d-amphetamine self-administration by humans. Addiction. 2012;107(4):783–91.
Ceci A, Garattini S, Gobbi M, Mennini T. Effect of long term amineptine treatment on pre- and postsynaptic mechanisms in rat brain. Br J Pharmacol. 1986;88(1):269–75.
Ponzio F, Achilli G, Garattini S, Perego C, Sacchetti G, Algeri S. Amineptine: its effect on the dopaminergic system of rats. J Pharm Pharmacol. 1986;38(4):301–3.
APO-Mirtazapine® (mirtazapine) [package insert on the internet]. Apotex Pty Ltd 2019 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=mirtazapine&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=82050001_2.
Zyban SR® (bupropion) [package insert on the internet]. Aspen 2017 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=Zyban+SR&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=54480001_2.
APO-Sertraline® (sertraline) [package insert on the internet]. Apotex Pty Ltd 2017 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=APO-Sertraline&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=11540001_2.
APO-Atomoxetine® (atomoxetine) [package insert on the internet]. Apotex Pty Ltd 2018 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=APO-Sertraline&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=11540001_2.
Tofranil® (imipramine) [package insert on the internet]. Amdipharm Mercury 2019 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=Tofranil&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=5080001_2.
Aripiprazole GH® (aripiprazole) [package insert on the internet]. Generic Health Pty Ltd 2019 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=Aripiprazole+GH&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=92340001_2.
APO-Topiramate® (topiramate) [package insert on the internet]. Apotex Pty Ltd 2019 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=APO-Topiramate&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=84600001_2.
Aspen Dexamfetamine® (dexamfetamine) [package insert on the internet]. Aspen Pharma 2017 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/QuickSearch.aspx?ModuleName=ProductInfo&searchKeyword=Aspen+Dexamfetamine.
Artige® (methylphenidate) [package insert on the internet]. Novartis 2017 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=Artige&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=123330001_2.
APO-Modafinil® (modafinil) [package insert on the internet]. Apotex Pty Ltd 2017 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=APO-Modafinil&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=121420001_2.
APO-Baclofen® (baclofen) [package insert on the internet]. Apotex Pty Ltd 2019 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=APO-Baclofen&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=123520001_2.
Gabapentin Generichealth® (gabapentin) [package insert on the internet]. Generic Health Pty Ltd 2018 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=abapentin+Generichealth&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=124490001_2.
Cousins MS, Roberts DC, de Wit H. GABA(B) receptor agonists for the treatment of drug addiction: a review of recent findings. Drug Alcohol Depend. 2002;65(3):209–20.
Subutex® (buprenorphine) [package insert on the internet]. Indivior Pty Ltd 2018 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=Subutex&PreviousPage=~/Search/QuickSearch.aspx&SearchType=ID=58190001_2.
Aspen Methadone Syrup® (methadone) [package insert on the internet].Aspen Pharma Pty Ltd 2017 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=Aspen+Methadone+Syrup&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=30830001_2.
APO-Naltrexone® (naltrexone) [package insert on the internet]. Apotex 2017 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=APO-Naltrexone&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=46910001_2.
Chiu CT, Ma T, Ho IK. Attenuation of methamphetamine-induced behavioral sensitization in mice by systemic administration of naltrexone. Brain Res Bull. 2005;67(1–2):100–9.
APO-Ondansetron® (ondansetron) [package insert on the internet]. Arrow 2016 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=APO-Ondansetron&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=82630001_2.
Champix® (varenecline) [package insert on the internet]. Pfizer Australia Pty Ltd 2019 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=Champix&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=78600001_2.
N-Acetyl-Cysteine (acetylcysteine) [package insert on the internet]. BioMedica Neuraceuticals (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=N-Acetyl-Cysteine&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=128250001_2.
APO-Riluzole® (riluzole) [package insert on the internet]. Apotex 2013 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=APO-Riluzole&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=96100001_2.
Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. 2016;3(8):760–73.
Zorrilla EP, Logrip ML, Koob GF. Corticotropin releasing factor: a key role in the neurobiology of addiction. Front Neuroendocrinol. 2014;35(2):234–44.
Anexate® (Flumazenil) [package insert on the internet]. Pharmaco 2017 (cited 2019 June 20). Avaliable from: https://www.mimsonline.com.au/Search/AbbrPI.aspx?ModuleName=ProductInfo&searchKeyword=Anexate&PreviousPage=~/Search/QuickSearch.aspx&SearchType=&ID=21440001_2.
Acknowledgements
The authors wish to thank Duncan Graham and Kelly Siefried for reviewing the manuscript; and Lucette Cysique for earlier work related to this review.
Author information
Authors and Affiliations
Contributions
NL had the idea for this systematic review; KJS, LSA, NL, and NE designed the study; KJS and LSA performed the literature search and data analyses; KJS drafted the first manuscript; LSA, NL and NE critically revised the manuscript.
Corresponding author
Ethics declarations
Funding
This study was supported by the National Centre for Clinical Research on Emerging Drugs (NCCRED). NCCRED is funded by the Australian Government Department of Health. NCCRED paid the open access fee.
Conflicts of Interest
KJS has no conflicts to declare. LSA has no conflicts to declare. NL has received research funding from Camurus, and has served on Advisory Boards for Mundipharma, Camurus and Indivior. NE has no conflicts to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Siefried, K.J., Acheson, L.S., Lintzeris, N. et al. Pharmacological Treatment of Methamphetamine/Amphetamine Dependence: A Systematic Review. CNS Drugs 34, 337–365 (2020). https://doi.org/10.1007/s40263-020-00711-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-020-00711-x