Abstract
Background and Purpose
Combination therapy with dipyridamole and clopidogrel in stroke prevention and long-term outcomes in aspirin-intolerant patients with acute myocardial infarction (AMI) and previous stroke are unknown. This nationwide study analyzed the impact of dipyridamole and clopidogrel on secondary stroke prevention and long-term outcomes in aspirin-intolerant stroke patients after AMI.
Methods
This was a nationwide, case-control study involving 186,112 first AMI patients, 78,607 of whom had a previous history of stroke. In the final analysis, we included 4637 patients taking clopidogrel alone and 208 patients using a combination of clopidogrel and dipyridamole.
Results
The 12-year survival rate was not different between clopidogrel and clopidogrel–dipyridamole groups (log-rank p = 0.6247). Furthermore, there were no differences in event-free survival after stroke (log-rank p = 0.6842), gastrointestinal (GI) bleeding (log-rank p = 0.9539), or intracerebral hemorrhage (ICH; log-rank p = 0.6191) between the two groups. Dipyridamole did not contribute significantly to AMI survival (hazard ratio 0.98, 95% confidence interval 0.84–1.15), and did not show benefits in any of the subgroups regardless of sex, age (younger or older than 75 years), comorbidities, percutaneous coronary intervention, or medications.
Conclusion
No differences were observed in the 12-year survival rate between clopidogrel and clopidogrel–dipyridamole groups. The two groups had balanced event-free survival in recurrent stroke, ICH, GI bleeding, and myocardial infarction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In aspirin-intolerant patients with previous stroke after acute myocardial infarction (AMI), combination therapy with clopidogrel and dipyridamole had no additional survival benefit compared with clopidogrel alone. |
Combination clopidogrel–dipyridamole therapy in patients with previous stroke after AMI had no benefit on event-free survival in recurrent stroke, intracerebral hemorrhage, gastrointestinal bleeding, or myocardial infarction. |
Adding dipyridamole to clopidogrel for secondary stroke prevention after AMI is not recommended, according to this study. |
1 Introduction
Both stroke and acute coronary syndrome can lead to disability and death worldwide [1, 2]. Antiplatelet therapy reduces the risk of recurrent non-cardioembolic stroke and other thromboembolic events [1, 3, 4]. Clopidogrel is an alternative monotherapy if patients are allergic or intolerant to aspirin [5,6,7]. The Clopidogrel Versus Aspirin in Patients at Risk of Ischaemic Events (CAPRIE) trial reported an additional effect of clopidogrel versus aspirin alone in patients with symptomatic atherosclerosis, with clopidogrel showing remarkable benefit in reducing myocardial infarction (MI) in the most severe groups of patients, providing a 19% relative risk reduction [2, 8].
For secondary ischemic stroke prevention, synergistic effect between aspirin and dipyridamole for secondary prevention was shown in the second European Stroke Prevention Study (ESPS2) [9]. Combination therapy with aspirin and dipyridamole is a first-line treatment compared with aspirin or clopidogrel alone [10, 11]. Non-inferiority of clopidogrel in secondary stroke prevention when compared with extended-release dipyridamole plus aspirin was also shown in the Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial [12].
No studies have investigated the combination therapy of dipyridamole and clopidogrel in stroke prevention and the long-term outcomes in aspirin-intolerant patients with acute myocardial infarction (AMI) and previous stroke. The aim of our study was to analyze the efficacy and safety of dipyridamole and clopidogrel in secondary prevention of stroke, and to evaluate the long-term outcomes in patients with previous ischemic stroke after AMI.
2 Methods
2.1 Data Source
The National Health Insurance (NHI) program, established by the Taiwanese government, has provided universal health coverage to approximately 99% of residents in Taiwan since 1995. A computerized database [Taiwan’s National Health Insurance Research Database (NHIRD)], consisting of data collected from more than 23 million patients, includes inpatient medical records on demographic information and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic codes, and drug codes.
Data for this study, which was approved by the Human Research Committee of Kaohsiung Veterans General Hospital, were collected from the NHIRD from January 2000 to December 2012.
2.2 Definition of the Acute Myocardial Infarction (AMI) Population
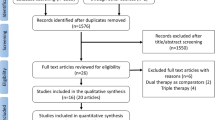
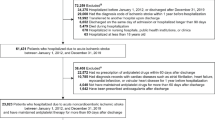
The AMI cohort, constituting 186,326 cases, was retrieved from the NHIRD in Taiwan between January 2000 and December 2012, with a primary diagnosis of AMI (ICD-9-CM code 410-410.92). We excluded patients who were under 18 years or over 120 years of age, who had previous admissions for AMI, and whose sex was undetermined, resulting in a total of 186,112 patients being included in the analysis (Fig. 1).
2.3 Study Population
Among the AMI cohort of 186,112 cases, 78,607 patients who were previously diagnosed with stroke (ICD-9-CM codes 430-438, A290-294) were analyzed. In our final analysis, we studied 4637 patients in the clopidogrel group and 208 patients in the clopidogrel–dipyridamole group (Fig. 1). Other comorbidities were also defined according to ICD-9-CM diagnostic codes, e.g. hypertension (ICD-9-CM codes 401-405), dyslipidemia (ICD-9-CM code 272), peripheral vascular disease (PVD; ICD-9-CM codes 443.9, 441, 441.9, 785.4 and V43.4, or procedure code 38.48), diabetes mellitus (DM; ICD-9-CM code 250), end-stage renal disease (ESRD; ICD-9-CM code 585), and chronic obstructive pulmonary disease (COPD; ICD-9-CM codes 491, 492 and 496). Indications of percutaneous coronary intervention (PCI) followed current guidelines [13,14,15,16].
We standardized medication status by using ‘index’ in-hospital and discharge medications. All patients were prescribed single antiplatelet therapy with clopidogrel, or dual antiplatelet therapy with clopidogrel–dipyridamole, after index discharge.
2.4 Outcome Analysis
The NHI premium is paid monthly and coverage can easily be canceled at the time of death. We defined survival based on the difference between the date of hospitalization and the end date of NHI coverage. Previous studies determined the validity of in-hospital mortality records in the NHIRD by cross-comparing them with death records from medical center electronic medical records, thus proving that the accuracy of death records in the NHIRD was high, within a maximum error of 1 month. Therefore, this database is a valid resource for population research in cardiovascular diseases [17,18,19,20].
2.5 Statistical Analysis
For data analysis, SAS software version 9.4 (SAS Institute, Inc., Cary, NC, USA) was used. All variables were calculated using descriptive statistics. Percentile values were used to express categorical data, which were analyzed using the Chi-square test, and mean and standard deviation (SD) were applied to express continuous variables, which were analyzed using a paired t test. A p value < 0.05 was considered statistically significant.
Cox proportional hazard regression analysis was used to calculate the hazard ratio (HR) and associated 95% confidence intervals (CIs) for significant variables, including PVD, ESRD, COPD, etc., while Kaplan–Meier cumulative survival curves were used to analyze outcomes between the clopidogrel and clopidogrel–dipyridamole groups based on sex, age, ST elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), DM, and PCI. Log-rank tests with a p value < 0.05 were used to determine statistical significance.
3 Results
The descriptive characteristics of 4637 patients in the clopidogrel group and 208 patients in the clopidogrel–dipyridamole group are listed in Table 1. The two groups were comparable with regard to age, sex, atrial fibrillation, comorbidities, PCI, and thrombolytic therapy (Table 1). For in-hospital and discharge medications, there was no difference between the two groups in the use of angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs), statins, β-blockers, nicorandil, atropine and dopamine. No patients in this study took warfarin or non-vitamin K antagonist oral anticoagulants. However, patients in the clopidogrel–dipyridamole group were more frequently prescribed nitrate (p = 0.0001).
Overall, the 12-year survival rate was not different between the two groups of patients after first AMI (log-rank p = 0.6247) (Fig. 2a). In the sex subgroup analysis, long-term outcomes of the clopidogrel group did not differ from the clopidogrel–dipyridamole group for both males (log-rank p = 0.7431) (Fig. 2b) and females (log-rank p = 0.6788) (Fig. 2c). In the age subgroup analysis, there was no survival difference between the two groups regardless of whether patients were older (log-rank p = 0.6833) (Fig. 2d) or younger (log-rank p = 0.5630) (Fig. 2e).
Kaplan–Meier survival curves with first AMI and previous stroke in overall, sex-specific, and age-specific subanalyses (a–e). Overall, the 12-year survival rate was not different between patients in the two groups after first AMI [log-rank p = 0.6247] (a). In the sex subgroup analysis, the long-term outcomes of the clopidogrel group did not differ from those of the clopidogrel–dipyridamole group among the male [log-rank p = 0.7431] (b) or female subgroups [log-rank p = 0.6788] (c). In the age subgroup analysis, there was no survival difference between the two groups, regardless of whether patients were older [log-rank p = 0.6833] (d) or younger [log-rank p = 0.5630] (e). AMI acute myocardial infarction
There were no statistical differences between the two therapeutic strategies in patients with (log-rank p = 0.3436) (Fig. 3a) or without diabetes (log-rank p = 0.7833) (Fig. 3b), and no superiority of either therapy was observed in subgroups of different types of MI, regardless of STEMI (log-rank p = 0.4066) (Fig. 3c) or NSTEMI (log-rank p = 0.9812) status (Fig. 3d). Similar effects between the two strategies were observed in patients who did (log-rank p = 0.8185) (Fig. 3e) or did not undergo PCI therapy (log-rank p = 0.8838) (Fig. 3f).
Kaplan–Meier survival curves after first AMI in the DM, AMI type, and PCI subgroups of patients (a–f). There were no statistical differences between the two therapeutic strategies in patients with [log-rank p = 0.3436] (a) or without [log-rank p = 0.7833] DM (b). No superiority of any therapy in subgroups of different types of myocardial infarction was observed, regardless of AMI type [log-rank p = 0.4066] (c), and log-rank p = 0.9812 (d). There were similar effects of the two strategies in patients who did [log-rank p = 0.8185] (e) or did not [log-rank p = 0.8838] undergo PCI therapy (f). AMI acute myocardial infarction, DM diabetes mellitus, PCI percutaneous coronary intervention, STEMI ST elevation myocardial infarction, NSTEMI non-ST elevation myocardial infarction
No difference in stroke-free survival (log-rank p = 0.6842) (Fig. 4b) was observed between the two groups of patients after AMI. Clopidogrel plus dipyridamole did not lead to worse intracerebral hemorrhage (ICH; log-rank p = 0.6191) (Fig. 4c) or gastrointestinal (GI) bleeding-free survival (log-rank p = 0.9539) (Fig. 4d). Moreover, the clopidogrel–dipyridamole combination did not further improve the recurrent MI-free survival rate (log-rank p = 0.8344) (Fig. 4a).
Event-free survival curves of patients with first AMI and previous stroke (a–d). There was no difference in stroke-free survival [log-rank p = 0.6842] (b) between the two groups of patients after AMI. Clopidogrel plus dipyridamole did not lead to worse intracerebral hemorrhage-free survival [log-rank p = 0.6191] (c) or gastrointestinal bleeding-free survival [log-rank p = 0.9539] (d). Furthermore, the combination with dipyridamole did not improve recurrent myocardial infarction-free survival [log-rank p = 0.8344] (a). AMI acute myocardial infarction
Cox proportional hazard regression analysis indicated HRs for mortality across different variables (Table 2). The HR for mortality was higher in older patients (HR 1.67), and in patients with DM (HR 1.20), PVD (HR 1.50), ESRD (HR 1.28), and COPD (HR 1.11). In contrast, PCI was shown to reduce the risk of mortality in patients after AMI (HR 0.57). Furthermore, the use of angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) (HR 0.70), statins (HR 0.83), and β-blockers (HR 0.86) showed a significant survival benefit. Dipyridamole did not contribute to AMI-free survival (HR 0.98).
A forest plot of HRs (Fig. 5) indicated that dipyridamole had no benefit in any subgroup regardless of sex, age (younger or older than 75 years), comorbidities (hypertension, dyslipidemia, DM, PVD, ESRD, COPD), PCI, or medications (ACEIs or ARBs, statins, β-blockers, heparin or low-molecular-weight heparin).
Forest plot of hazard ratios in patients with first AMI and previous stroke. Dipyridamole showed no benefit in any subgroup analysis regardless of sex, age (younger or older than 75 years), comorbidities (HTN, dyslipidemia, DM, PVD, ESRD, COPD), PCI, or medications (ACEIs or ARBs, statins, β-blockers, heparin, or LMWH). ACEI angiotensin-converting enzyme inhibitor, ARB angiotensin receptor blocker, COPD chronic obstructive pulmonary disease, DM diabetes mellitus, ESRD end-stage renal disease, LMWH low-molecular-weight heparin, PVD peripheral vascular disease, HTN hypertension, PCI percutaneous coronary intervention, HR hazard ratio, CI confidence interval, AMI acute myocardial infarction
4 Discussion
There was no previous study to investigate clopidogrel-dipyridamole combination therapy for secondary stroke prevention and long-term outcome in aspirin-intolerant patients with AMI and old stroke.There was no difference in long-term outcome between the clopidogrel and clopidogrel–dipyridamole groups. In addition, the two groups had comparable event-free survival in recurrent stroke, ICH, GI bleeding, and MI.
4.1 Putative Mechanism of the Combination Therapy Between Dipyridamole and Aspirin
Adenosine diphosphate (ADP) suppresses thromboxane A2 and blocks the effect of aspirin [21], while dipyridamole eliminates the above-mentioned suppression via the inhibition of ADP uptake by platelets [22]. The benefit of dipyridamole comes from its effect on the vascular wall beyond platelet inhibition [23, 24]. Previous animal studies demonstrated the synergistic antithrombotic effects of dipyridamole and aspirin in rabbits, which were also demonstrated in human trials [9, 25,26,27,28,29]. Multiple pharmacologic mechanisms and the vasodilation effect of dipyridamole contribute to the synergic effect of aspirin and dipyridamole in stroke prevention.
4.2 Clopidogrel–Dipyridamole Combination did not Improve Overall Outcomes or Prevent Secondary Stroke Recurrence After AMI
Clopidogrel is a type of ADP receptor (P2Y12) inhibitor that differs from the phosphodiesterase (PDE) inhibitor dipyridamole. Although more than 50% of Chinese people have a loss-of-function mutation of cytochrome P450 (CYP) 2C19 that renders clopidogrel less effective [30], dipyridamole did not seem to have additive effect with clopidogrel (log-rank p = 0.6247) (Fig. 2a). No synergic effect between clopidogrel and dipyridamole was noted, which could be attributed to the fact that both antiplatelet agents shared a common function of the inhibition of platelet aggregation [29].
In our national database, a higher percentage of AMI patients had previous stroke event. Previous studies validated the diagnostic accuracy of ICD codes to identify patients with stroke. Furthermore, 60% of stroke patients were found to have AMI [31], and another AMI registry with a mean age of 65 years revealed that 20% of AMI patients had previous stroke [32]. The relative incidence of stroke compared with AMI was remarkably higher and had linear growth in those older than 65 years of age [33]. In our study, 57.9% of patients in the clopidogrel group and 63.5% of patients in the clopidogrel–dipyridamole group were aged older than 75 years. The relatively older patients in our nationwide study might partly explain the higher proportion of patients with previous stroke.
Patients in the clopidogrel–dipyridamole group were prescribed with nitrate more frequently (p = 0.0001); however, there were comparable comorbidities, PCI, or other medications between the two groups. The frequent prescription of nitrate might be more symptomatic, but there was insufficient evidence to ascribe the frequency of nitrate prescription to the severity of disease. A previous study also reported that nitrate therapy after AMI does not affect prognosis [34].
4.3 Clopidogrel–Dipyridamole had No Benefit in Diabetes Mellitus and Peripheral Vascular Disease Patients
Diabetes increases the burden of stroke and PVD, and PVD is complicated by high rates of MI and stroke [35, 36]. Non-aspirin antiplatelet drugs (clopidogrel and dipyridamole) largely drive the benefits in PVD patients [36]. In patients with MI and PVD, as well as patients with concomitant DM and atherosclerotic vascular disease, clopidogrel is superior to aspirin as monotherapy [4, 8, 37,38,39].
In DM and PVD patients with a previous history of stroke after AMI, the efficacy and safety of clopidogrel–dipyridamole combination therapy are unknown, and our study revealed no additional benefits of this combination therapy.
4.4 Clopidogrel–Dipyridamole did not Increase Hemorrhage-Related Mortality
Patients who experience stroke are at high risk for recurrent stroke, MI, and vascular death [40]. The aspirin–dipyridamole combination did not increase the frequency of bleeding events [23]. Clopidogrel monotherapy is an alternate to aspirin plus dipyridamole, with a similar risk of bleeding [8, 41,42,43,44], while dipyridamole reduces the risk of recurrent stroke without excess bleeding [23].
No previous studies have evaluated the hemorrhagic complications of the clopidogrel–dipyridamole combination. Our study did not observe an increase in ICH or GI bleeding-related mortality in the combination group.
4.5 Study Limitations
There were several limitations in the present study. First, this was a non-randomized, retrospective cohort study, and the small sample size in the clopidogrel–dipyridamole group was notable, although it was acquired from a large national database. Clinical prescription and long-term follow-up of the clopidogrel–dipyridamole combination was not routine practice. This study provided important information of antiplatelet strategies for clinical practitioners. Second, the healthcare claims data did not contain objective assessments for evaluating the severity of stroke patients, such as the modified Rankin Scale, the National Institutes of Health Stroke Scale, etc. Moreover, cardiac enzyme and systolic function for evaluating severity and impact after AMI were not available. Third, indices of the risk factors were nonexistent, including body mass index, glycated hemoglobin, blood pressure, smoking history, and ankle–brachial index. However, a previous study reported that smoking duration had a linear relationship with COPD [45], thus the morbidity rate of COPD might be correlated with smoking history. In this study, there was no difference in COPD percentage between the two groups (p = 0.2395), which showed comparable proportion of patients with smoking history. Fourth, standard laboratory tests, including the assessment of renal function, liver function, and coagulation function, were not available and these factors may interfere with drug–drug interactions, bleeding risk, and medication administration. Fifth, a meta-analysis indicated that extended-release and high-dose dipyridamole are more effective than immediate-release and low-dose dipyridamole [9, 23, 26, 29]. The number of patients in the clopidogrel–dipyridamole combination group was relatively small, which limited advanced subgroup analysis. Further prospective, randomized studies are required to confirm our findings.
4.6 Strengths of this Study
This is the first study to investigate the combination therapy of dipyridamole and clopidogrel in stroke prevention and to evaluate the long-term outcomes in aspirin-intolerant patients with AMI and previous stroke. This nationwide study has a large sample size and a long-term follow-up of 12 years to analyze the outcomes of the two therapeutic strategies. The large sample size reduces the variability in sampling statistics. Our study offers information on antiplatelet strategies for physicians in clinical practice.
5 Conclusions
This nationwide study indicated that there were no differences in 12-year survival rates between clopidogrel and clopidogrel–dipyridamole groups, regardless of age, sex, type of MI, intervention or medical therapy. Event-free survival in recurrent stroke, ICH, GI bleeding, and myocardial infarction were not different between the clopidogrel and clopidogrel–dipyridamole groups.
References
Milionis H, Liontos A, Vemmos K, Spengos K. Antiplatelet treatment in stroke: new insights. Curr Pharm Des. 2016;22(29):4617–26.
Montalescot G. Value of antiplatelet therapy in preventing thrombotic events in generalized vascular disease. Clin Cardiol. 2000;23 Suppl 6:Vi-18-22.
Fang J, George MG, Hong Y, Loustalot F. Use of aspirin for prevention of recurrent atherosclerotic cardiovascular disease among adults—20 states and the district of Columbia, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(27):733–7.
Faxon DP, Nesto RW. Antiplatelet therapy in populations at high risk of atherothrombosis. J Natl Med Assoc. 2006;98(5):711–21.
Oza R, Rundell K, Garcellano M. Recurrent ischemic stroke: strategies for prevention. Am Fam Physician. 2017;96(7):436–40.
Latib A, Ielasi A, Ferri L, Chieffo A, Godino C, Carlino M, et al. Aspirin intolerance and the need for dual antiplatelet therapy after stent implantation: a proposed alternative regimen. Int J Cardiol. 2013;165(3):444–7.
Gitt AK, Zahn R. Antithrombotic treatment in patients with stable coronary artery disease. Which drugs and for how long? Herz. 2014;39(7):798–802 (in German).
CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet. 1996;348(9038):1329–39.
Diener HC, Cunha L, Forbes C, Sivenius J, Smets P, Lowenthal A. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci. 1996;143(1–2):1–13.
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–236.
Wein T, Lindsay MP, Cote R, Foley N, Berlingieri J, Bhogal S, et al. Canadian stroke best practice recommendations: secondary prevention of stroke, sixth edition practice guidelines, update 2017. Int J Stroke. 2018;13(4):420–43.
Diener HC, Sacco RL, Yusuf S, Cotton D, Ounpuu S, Lawton WA, et al. Effects of aspirin plus extended-release dipyridamole versus clopidogrel and telmisartan on disability and cognitive function after recurrent stroke in patients with ischaemic stroke in the Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial: a double-blind, active and placebo-controlled study. Lancet Neurol. 2008;7(10):875–84.
American College of Emergency Physicians, Society for Cardiovascular Angiography and Interventions, O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–140.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–77.
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2014;130(25):e344–426.
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267–315.
Cheng CL, Chien HC, Lee CH, Lin SJ, Yang YH. Validity of in-hospital mortality data among patients with acute myocardial infarction or stroke in National Health Insurance Research Database in Taiwan. Int J Cardiol. 2015;201:96–101.
Cheng CL, Lee CH, Chen PS, Li YH, Lin SJ, Yang YH. Validation of acute myocardial infarction cases in the national health insurance research database in Taiwan. J Epidemiol. 2014;24(6):500–7.
Wang MT, Lin SC, Tang PL, Hung WT, Cheng CC, Yang JS, et al. The impact of DPP-4 inhibitors on long-term survival among diabetic patients after first acute myocardial infarction. Cardiovasc Diabetol. 2017;16(1):89.
Kuo PL, Lin KC, Tang PL, Cheng CC, Huang WC, Chiang CH, et al. Contribution of hepatitis B to long-term outcome among patients with acute myocardial infarction: a nationwide study. Medicine. 2016;95(5):e2678.
Weiss HJ, Aledort LM. Impaired platelet-connective-tissue reaction in man after aspirin ingestion. Lancet. 1967;2(7514):495–7.
Weiss HJ, Aledort LM, Kochwa S. The effect of salicylates on the hemostatic properties of platelets in man. J Clin Invest. 1968;47(9):2169–80.
Li X, Zhou G, Zhou X, Zhou S. The efficacy and safety of aspirin plus dipyridamole versus aspirin in secondary prevention following TIA or stroke: a meta-analysis of randomized controlled trials. J Neurol Sci. 2013;332(1–2):92–6.
Davidai G, Cotton D, Gorelick P, Bath PM, Lipton RB, Sacco R, et al. Dipyridamole-induced headache and lower recurrence risk in secondary prevention of ischaemic stroke: a post hoc analysis. Eur J Neurol. 2014;21(10):1311–7.
Honour AJ, Hockaday TD, Mann JI. The synergistic effect of aspirin and dipyridamole upon platelet thrombi in living blood vessels. Br J Exp Pathol. 1977;58(3):268–72.
Halkes PH, van Gijn J, Kappelle LJ, Koudstaal PJ, Algra A. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet. 2006;367(9523):1665–73.
Tirschwell D. Aspirin plus dipyridamole was more effective than aspirin alone for preventing vascular events after minor cerebral ischemia. ACP J Club. 2006;145(3):57.
Leonardi-Bee J, Bath PM, Bousser MG, Davalos A, Diener HC, Guiraud-Chaumeil B, et al. Dipyridamole for preventing recurrent ischemic stroke and other vascular events: a meta-analysis of individual patient data from randomized controlled trials. Stroke. 2005;36(1):162–8.
Mansoor AH, Mujtaba MT, Silver B. Antiplatelet therapy to prevent recurrent stroke: three good options. Cleve Clin J Med. 2013;80(12):787–95.
Wang Y, Zhao X, Lin J, Li H, Johnston SC, Lin Y, et al. Association between CYP2C19 loss-of-function allele status and efficacy of clopidogrel for risk reduction among patients with minor stroke or transient ischemic attack. JAMA. 2016;316(1):70–8.
Bener A, Kamran S, Elouzi EB, Hamad A, Heller RF. Association between stroke and acute myocardial infarction and its related risk factors: hypertension and diabetes. Anadolu Kardiyol Derg. 2006;6(1):24–7.
Tian L, Yang Y, Zhu J, Liu L, Liang Y, Li J, et al. Impact of previous stroke on short-term myocardial reinfarction in patients with acute ST segment elevation myocardial infarction: an observational multicenter study. Medicine. 2016;95(6):e2742.
Gentil A, Bejot Y, Lorgis L, Durier J, Zeller M, Osseby GV, et al. Comparative epidemiology of stroke and acute myocardial infarction: the Dijon vascular project (Diva). J Neurol Neurosurg Psychiatry. 2009;80(9):1006–11.
Kojima S, Matsui K, Sakamoto T, Ishihara M, Kimura K, Miyazaki S, et al. Long-term nitrate therapy after acute myocardial infarction does not improve or aggravate prognosis. Circ J. 2007;71(3):301–7.
Paneni F, Beckman JA, Creager MA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J. 2013;34(31):2436–43.
Violi F, Basili S, Berger JS, Hiatt WR. Antiplatelet therapy in peripheral artery disease. Handb Exp Pharmacol. 2012;210:547–63.
Beckman JA, Paneni F, Cosentino F, Creager MA. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part II. Eur Heart J. 2013;34(31):2444–52.
Azarbal A, Clavijo L, Gaglia MA Jr. Antiplatelet therapy for peripheral arterial disease and critical limb ischemia: guidelines abound, but where are the data? J Cardiovasc Pharmacol Ther. 2015;20(2):144–56.
Jones L, Griffin S, Palmer S, Main C, Orton V, Sculpher M, et al. Clinical effectiveness and cost-effectiveness of clopidogrel and modified-release dipyridamole in the secondary prevention of occlusive vascular events: a systematic review and economic evaluation. Health Technol Assess. 2004;8(38):iii–iv, 1–196.
Isabel C, Calvet D, Mas JL. Stroke prevention. Presse Med. 2016;45(12 Pt 2):e457–71.
Zuurbier SM, Vermeer SE, Hilkens PH, Algra A, Roos YB. Secondary prevention with clopidogrel after TIA or stroke. Ned Tijdschr Geneeskd. 2013;157(25):A5836 (in Dutch).
Katsanos K, Spiliopoulos S, Saha P, Diamantopoulos A, Karunanithy N, Krokidis M, et al. Comparative efficacy and safety of different antiplatelet agents for prevention of major cardiovascular events and leg amputations in patients with peripheral arterial disease: a systematic review and network meta-analysis. PloS One. 2015;10(8):e0135692.
Sacco RL, Diener HC, Yusuf S, Cotton D, Ounpuu S, Lawton WA, et al. Aspirin and extended-release dipyridamole versus clopidogrel for recurrent stroke. N Engl J Med. 2008;359(12):1238–51.
Christiansen CB, Pallisgaard J, Gerds TA, Olesen JB, Jorgensen ME, Nume AK, et al. Comparison of antiplatelet regimens in secondary stroke prevention: a nationwide cohort study. BMC Neurol. 2015;15:225.
Liu Y, Pleasants RA, Croft JB, Wheaton AG, Heidari K, Malarcher AM, et al. Smoking duration, respiratory symptoms, and COPD in adults aged ≥ 45 years with a smoking history. Int J Chron Obstruct Pulmon Dis. 2015;10:1409–16.
Acknowledgements
The authors would like to thank Miss Chia-Jung Chin, Miss Tzu-Jung Chuang, Miss Hsiao Ching Kuo, and Hsiao-Chin Lin for their expert statistical assistance.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
The open access fee was paid by the authors. This study was supported by grants from the Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan (Grant Numbers VGHKS 212347-23, 106-084, 106-142, 106-D01-3, 106-160, 106-156, 106-062, 105-139, and 106-159) and the Ministry of Science and Technology (Grant Numbers Most 105-2314-B-075B-006 and Most 105-2314-B-075B-007).
Consent for Publication
All authors provided their consent for publication of this article.
Availability of Data and Materials
Data are available from the NHIRD, published by the Taiwan NHI Bureau. Due to legal restrictions imposed by the government of Taiwan in relation to the ‘Personal Information Protection Act’, data cannot be made publicly available. Requests for data access can be sent as a formal proposal to the NHIRD (http://nhird.nhri.org.tw).
Conflict of Interest
Mei-Tzu Wang, Hsin-Li Liang, Cheng Chung Hung, Pei-Ling Tang, Kun-Chang Lin, Cheng-Hung Chiang, Feng-You Kuo, Jin-Shiou Yang, Chun-Peng Liu, Guang-Yuan Mar, and Wei-Chun Huang declare that they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Ethics Approval and Consent to Participate
This study was approved by the Institutional Review Board (IRB) of the Kaohsiung Veterans General Hospital (No. VGHKS14-CT7-07). Written informed consent was not required for this study as the NHI dataset consists of de-identified secondary data for research purposes, and the IRB of Kaohsiung Veterans General Hospital issued a formal written waiver of the requirement for informed consent.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wang, MT., Liang, HL., Hung, C.C. et al. Combination Therapy with Dipyridamole and Clopidogrel for Secondary Stroke Prevention in Aspirin-Intolerant Patients After Myocardial Infarction: Results of a Nationwide Case-Control Study. CNS Drugs 33, 175–185 (2019). https://doi.org/10.1007/s40263-018-0591-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-018-0591-8