Abstract
Data from clinical trials in adults, extrapolated to predict benefits in paediatric patients, could result in fewer or smaller trials being required to obtain a new drug licence for paediatrics. This article outlines the place of such extrapolation in the development of drugs for use in paediatric epilepsies. Based on consensus expert opinion, a proposal is presented for a new paradigm for the clinical development of drugs for focal epilepsies. Phase I data should continue to be collected in adults, and phase II and III trials should simultaneously recruit adults and paediatric patients aged above 2 years. Drugs would be provisionally licensed for children subject to phase IV collection of neurodevelopmental safety data in this age group. A single programme of trials would suffice to license the drug for use as either adjunctive therapy or monotherapy. Patients, clinicians and sponsors would all benefit from this new structure through cost reduction and earlier access to novel treatments. Further work is needed to elicit the views of patients, their parents and guardians as appropriate, regulatory authorities and bodies such as the National Institute for Health and Care Excellence (UK).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Based on consensus expert opinion, we propose a new paradigm for the clinical development of drugs for focal epilepsies. |
In this new paradigm phase II and III trials should simultaneously recruit adults and paediatric patients aged above 2 years and drugs would be provisionally licensed for children subject to phase IV collection of neurodevelopmental safety data. |
Patients, clinicians and sponsors would all benefit from this new structure through cost reduction and earlier access to novel treatments. |
1 Introduction
The European Medicines Agency (EMA) defines extrapolation as “…extending information and conclusions available from studies in one or more subgroups of the patient population (source population)… to make inferences for another subgroup of the population (target population)…” [1, 2]. There are several examples of how this definition can be applied. Using the terminology of Dunne et al. [3], extrapolation can range from complete (no additional data needed in the target population) to partial (supporting data needed) to none. Extrapolation can be used to streamline drug development. Avoiding unnecessary studies in populations whose response to therapy is well understood enables sponsors to focus research on patient groups about which least is known. This paper considers how the extrapolation of adult efficacy and safety data can be used to streamline the development of drugs for use in paediatric epilepsies.
Off-label prescribing in paediatrics is prevalent in the USA [4] and EU [5]. In routine clinical practice, informal extrapolation from adult data increases the confidence of doctors and families regarding off-label prescribing in children. When developing new medicines, it is reasonable practice to extrapolate from adult data to predict the clinical benefits of a new medicine in paediatrics such that smaller trials may suffice to demonstrate efficacy in this age group. However, extrapolations only have value if robust assumptions on similarity hold when applied to the adult and paediatric populations. The US Food and Drug Administration (FDA) [6] and International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) E11 [7] guidelines outline an algorithmic approach for determining which data are needed to support paediatric licensing of a medicine depending on whether it is reasonable to assume that disease progression, drug pharmacology, and pharmacokinetic/pharmacodynamic relationships are consistent across adults and paediatric patients. An alternative framework has recently been proposed which stipulates that emerging and cumulative data in the target population should be used to confirm extrapolation assumptions [1, 2].
In the context of epilepsy research, it is not always possible to predict clinical benefits in paediatric patients using adult data due to disparities in the different types (syndromes) of epilepsy and their specific natural histories. The acceptability of extrapolation will depend on several factors, including age, seizure type and epilepsy syndrome, treatment regimen and the individual antiepileptic drug (AED). Whilst there is broad agreement that efficacy in adults with focal epilepsies can be extrapolated to paediatric patients with focal epilepsies, there is disagreement about the boundary of certainty, with different expert groups supporting extrapolation down to the ages of either 2 [8] or 4 years [9]. The FDA has recently suggested that complete extrapolation of efficacy from adult to paediatric patients aged 4 years and older with partial-onset seizures is acceptable [10]. This is a major development, and one that is consistent with our view, but the potential of extrapolation goes much further.
This paper explores these issues and provides recommendations on the role of extrapolation in drug development for epilepsy and identifies opportunities to improve current practice. It reflects work conducted within a project funded by the National Institute for Health Research (UK) on extrapolation approaches in paediatric trials.
2 Considerations
2.1 Are Paediatric Patients Just Small Adults?
In the case of common focal epilepsies, the answer to the question “are paediatric patients just small adults?” may well be yes. The aetiology of extra-temporal focal epilepsy in both adults and children is predominated by vascular lesions, trauma and, most frequently, cortical dysplasias. Dysplasias are present from birth and while the time to seizure onset may vary widely, the underlying pathology is the same, which suggests that this is likely to reflect a single pathophysiological process independent of age.
All patients aged 2 years and above with focal epilepsy would be expected to respond similarly to drug treatment in terms of seizure frequency reduction, provided that dosing led to an equivalent serum concentration–time profile. Although there are some subtle differences in semiology of focal seizures in the youngest age groups (i.e. paucity of automatisms, predominance of bilateral motor signs, etc.), these rapidly disappear with age and there is no evidence that these seizure types are differentially responsive to first-line therapies for focal epilepsy [11]. Consequently, it should be possible to extrapolate efficacy data obtained in adults with focal epilepsy to patients aged 2 years and above. It would be inappropriate, however, to extrapolate efficacy to patients below 2 years of age primarily because of greater variability in aetiology and difficulties in diagnosis.
While the natural history of epilepsies may differ between adults and paediatrics, any differences in treatment effect between adult and paediatric patients with focal epilepsies are likely to be quantitative rather than qualitative [8, 12–14]. However, this does not obviate the continued need for trials of new AEDs in paediatrics, particularly in the case of the rarer epilepsy syndromes.
2.2 Are All Paediatric Patients the Same?
For focal epilepsies, the older age groups proposed in the ICH E11 guidance (Table 1) [7] could in theory be merged to create a single group that encompasses children and adolescents aged 2–16/18 years. However, there would be less confidence regarding the younger age groups and discussions with neonatologists would be required.
There is no doubt that preterm and term infants are relatively under-investigated with minimal phase I or randomised controlled trial (RCT) data. Extrapolation of efficacy data from adults or older paediatric patients to these groups is not possible because of differences in the pathophysiology of the epilepsy as well as brain biochemistry, brain development and drug metabolism. Drug clearance is low in preterm and term newborn infants, subsequently increases rapidly until around 2 years and then declines steadily until around 12 years at which point it is considered to have reached adult levels, such that adult dosing can be considered for adolescents aged >12 years [15]; this is well-illustrated by carbamazepine [16]. However, sufficient variability exists that pharmacokinetic studies are likely to be required to support dose choices for paediatric patients aged 2–12 years even when efficacy is extrapolated.
In general, the behaviour of AEDs in patients aged 2 years and above is usually predictable. However, there is a need for more robust studies in patients under 2 years with both focal and generalised epilepsies. This is acknowledged to be challenging, especially for patients less than 1 month old in whom the study design would be critical.
2.3 If a Drug is Safe in Adults, is it Safe in Paediatrics?
There are a variety of adverse outcomes associated with AED use, including those that are acute and dose related, those that are chronic and exposure related, and those that are idiosyncratic and likely to be immune mediated. For the purposes of this article, we group them all under the term ‘safety’. Most safety issues are considered to be essentially similar in adults and paediatrics at equivalent doses. There is anecdotal evidence suggesting that some idiosyncratic reactions occur at differing frequencies in adults and children (i.e. lamotrigine-induced Stevens-Johnson syndrome), but this may simply reflect differences in drug disposition and in systemic exposure to the drugs or their reactive metabolites. Those aside, it is possible, with appropriate caution, to extrapolate most adult safety data to paediatric patients aged 2 years and above.
Important safety issues that are specific to paediatrics include effects on growth and on pubertal, motor, speech and language, and cognitive development. These paediatric safety signals cannot be reliably identified from an adult population. Effects on learning and on social and educational development are also important, and in paediatric patients with severe epilepsies it may be difficult to distinguish the influence of the epilepsy and its underlying aetiology from the effects of the medications used to treat it. Nevertheless, improvements in attention, memory, cognition and behaviour can be observed during AED withdrawal in paediatric patients with challenging epilepsy, suggesting a strong influence of drug treatment.
Seizure aggravation is another important safety issue, particularly in rare idiopathic focal epilepsies that are typically diagnosed in childhood only. Standard treatments can occasionally exacerbate seizures in these children but their low prevalence in the focal epilepsy population means that they might evade detection in controlled trials of short duration. Inclusion of EEG follow-up in the phase II and III trial protocols for paediatric participants would improve detection of these paradoxical effects.
2.4 When is it Reasonable to Use Therapies in Paediatrics that are Licensed Only for Adults?
The decision regarding when it is reasonable to use drugs in paediatrics that are licensed only for use in adults would depend on the clinical situation, with a risk–benefit trade-off determining the acceptability of off-label prescribing. When prescribing off-label in paediatrics, a drug will often be tried initially in adolescents before then being used in younger patients.
In this situation there would likely be greater confidence to enter patients in clinical trials rather than prescribe an AED off-label, particularly because of the detailed monitoring performed within a trial. There is a clear need for paediatric RCTs to be conducted earlier than at present and in parallel or in conjunction with adult trials. This would incentivise the recruitment of children into trials since accrual can be challenging when a trial treatment licensed in adults is available off-label in children. Improving enrolment will improve the quality of paediatric RCTs since inadequate accrual currently obliges many trialists to recruit from small, inexperienced centres, increasing patient heterogeneity and the risk of internal biases. Earlier paediatric RCTs would also widen participation in trials to include children with refractory epilepsy who are often excluded from new drug studies on the basis that they have already been prescribed the drug off-label after failing all other licensed medicines.
It is important to acknowledge that there may be paediatric-specific issues for any RCTs undertaken in the idiopathic focal epilepsies of childhood and particularly benign partial epilepsy with centro-temporal spikes (BECTS) and benign epilepsy of childhood with occipital paroxysms (BECOP; Panayiotopoulos syndrome). The natural history of BECTS (and probably BECOP) is such that a spontaneous remission may occur any time, including soon after its onset or diagnosis. Consequently, any apparent efficacy of a drug in RCT participants with BECTS or BECOP may be due to the drug itself or to the natural history of the syndrome. This might risk assay sensitivity in a non-inferiority trial but would be of less concern if the trial was designed to detect differences and found them.
2.5 Can we Extrapolate Efficacy Data from Adjunctive Therapy to Monotherapy?
Extensive trial data and clinical experience with existing AEDs has failed to find any instance where a drug behaves differently in terms of its spectrum of efficacy and adverse effects when administered alone or as adjunctive therapy, except in circumstances where drug interactions might be expected. Consequently, it would be reasonable to extrapolate efficacy data from adjunctive trials to inform the use of an AED as monotherapy. Mintzer et al. [17] state that the need for separate monotherapy and adjunctive therapy licenses in epilepsy is “unnecessarily restrictive” and that AEDs should be approved for specific seizure types or epilepsy syndromes only.
3 An Alternative Paradigm for Developing Medicines for Focal Epilepsies
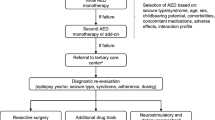
This section outlines our proposal for the future clinical development of drugs for focal epilepsies. This proposal uses a partial extrapolation of adult efficacy data, generating only supportive efficacy data in children aged 2 years and above, and a limited extrapolation of adult safety data to justify joint phase II and III studies recruiting adult and paediatric patients aged 2 years and above.
3.1 Phase I Trials
The primary purpose of phase I trials remains the identification of a safe range of doses of a new compound to be used in the subsequent clinical development programme. Such studies should continue to be undertaken in healthy male adults only in an effort to reduce variability, limit confounding influences and minimise the likelihood of unexpected adverse events.
3.2 Phase IIa and IIb Trials
The primary purpose of phase IIa and IIb trials remains determination of the effective dose range and a preliminary assessment of safety and efficacy. Trials should be randomised, placebo-controlled, adjunctive therapy studies following current guidelines for adjunctive trials but now recruiting patients with focal epilepsy aged 2 years and above, obviating the current requirement for a separate development programme in paediatrics. Using partial extrapolation of adult efficacy data, power calculations should be based on the entire study population but the final analysis should be stratified by age. Long-term extension will allow provisional assessment of safety in adults, paediatrics or both. There would not be a requirement to complete the long-term extension before progressing to phase III. Pharmacokinetic investigations will reveal the dose–concentration relationship in adults, paediatrics or both. Wherever possible, pharmacokinetic data should be analysed using population pharmacokinetic models to accommodate sparse sampling schedules. Inclusion of mandatory EEG follow-up for paediatric participants would allow detection of seizure aggravation.
3.3 Phase III Trials
The primary purpose of phase III trials remains the identification of efficacy in comparison to placebo. Traditional approaches are appropriate; i.e. randomised and placebo-controlled trials of adjunctive therapy. Efficient adaptive [18] and/or Bayesian [19] strategies to the design and analysis of trials should be considered if appropriate. Studies should again recruit patients with focal epilepsy aged 2 years and above and should be powered to detect treatment effects based on the total sample size accumulated across adults and paediatrics but should also include the potential for a stratified analysis. Minimum sample sizes in each age group might be prespecified to ensure that reliable (but not necessarily definitive) conclusions can be drawn from the paediatric data. If a significant treatment effect was demonstrated in adults but not in paediatric patients and the differences could be attributed to sample size alone, then the treatment would still be acceptable for paediatric use provided there were no qualitative differences in the effects between adults and paediatric patients.
Long-term extension will allow additional open-label assessment of safety and efficacy in adults, paediatrics or both. Further pharmacokinetic investigations and EEG follow-up may be required, particularly in paediatric patients.
3.4 Licensing of Treatments
Under this new paradigm, since all pivotal trials would be conducted in both paediatrics and adults, licensing should also apply to all age groups from 2 years upwards. Licenses should be granted for a general indication of ‘focal epilepsy’, allowing their discretionary use as either adjunctive therapy or monotherapy unless there is reason to impose a restriction. Approval for paediatric use (2–16/18 years) should be conditional on a prospective, time-limited commitment to collect safety data from paediatric patients on growth and on neurological and cognitive development. Ideally, these neurodevelopmental safety data would be collected within a randomised, placebo-controlled design, but this is likely to pose significant logistical issues. Consequently, it would be appropriate and sufficient to collate multiple audit and observational data. This is a pragmatic solution since the challenges of deducing unbiased estimates of causal effects from observational data in the presence of unmeasured confounders are well-documented [20]. Caution should also be exercised to prevent or at least monitor the use of drugs licensed for ‘focal epilepsy’ in more complex epilepsies that express multiple seizure types; the focal component may be improved but other seizure types may be simultaneously exacerbated.
The approach proposed here has been used to develop rufinamide for Lennox-Gastaut syndrome [21, 22]. However, this was a syndrome-specific development programme for a relatively rare epilepsy. The paradigm suggested here is a more general framework for common epilepsies which considers other factors such as adjunctive therapy and monotherapy. It dispenses with the need for a separate paediatric development programme and a separate monotherapy trial programme, neither of which have clear additional benefits in focal epilepsies.
3.5 Shift in Research Culture
The adoption of this proposed framework for drug development in epilepsy may require a shift in culture. A network of specialist paediatric epilepsy centres is needed to coordinate recruitment of patients into regulatory trials of AEDs, in a manner similar to the common practice in paediatric oncology. Rather than specialists making third- or fourth-line treatment decisions for paediatric patients, they should randomise those patients into trials; this would advance knowledge much more rapidly. Those anxious about undertaking combined trials in adults and paediatrics should consider the SANAD (Standard and New Antiepileptic Drugs) studies, which remain the largest ever randomised trials in epilepsy and which successfully recruited across the age spectrum from 5 years upwards [23, 24]. Fears over inclusion of paediatric patients in randomised trials should be tempered with examples of paediatric epilepsy studies that have successfully hit their recruitment targets in a timely manner [25–28] and with evidence regarding parents’ opinions on enrolment of their children into RCTs [29]. Finally, improved interaction with neonatologists would help to ensure that treatments for epileptic seizures in the very youngest age groups do not lag behind those for others.
4 Conclusions
This proposed paradigm for drug development in epilepsy has many potential benefits for epilepsy and epilepsy research; paediatric patients gain from immediate access to new treatments, trialists have access to a broader patient population, fewer trials and less restrictive licensing will incentivise sponsors, broaden their market and re-invigorate drug development for epilepsy, and research and development savings can be expected to have knock-on effects for medication costs and the allocation of healthcare resources.
It is acknowledged that there are potential dangers in a condensed AED trial programme because of the volume of data and number of patient exposures. There may also be additional complexities to conducting trials in adults and children if, for example, drug formulations or dosing rules vary across age groups, although several successful trials show these barriers are not insurmountable [28]. The next step in this process is to seek the opinion of patients, parents and guardians, regulatory authorities and sponsors on the risks, benefits and feasibility of the proposed paradigm.
This article is written within the context of growing international interest in the place of extrapolation in the development of medicines for paediatric epilepsies. Following the publication of robust evidence demonstrating that efficacy in RCTs recruiting adults with focal epilepsies can similarly predict efficacy in children [12], a US consortium from academia, industry, the FDA and the Epilepsy Foundation was formed to further explore and develop this concept. The Pediatric Epilepsy Academic Consortium for Extrapolation (PEACE) has since drafted a white paper establishing disease similarity in adults and children. Additional pharmacometric analyses are also currently underway at the FDA to further evaluate pharmacokinetic and pharmacodynamic properties of AEDs. The PEACE group has shown that ever since a 1994 National Institute of Neurological Disorders and Stroke (NINDS) workshop agreed that most children with focal epilepsies would respond to a drug that was also efficacious in adults with focal epilepsies [30], further clinical and basic science data have served to strengthen this viewpoint. After excluding children below 4 years and those with focal seizures associated with epileptic encephalopathy, such as Lennox-Gastaut syndrome, the pathophysiology of focal epilepsies is similar in children and adults. The PEACE white paper will therefore recommend that AEDs shown to be effective in adults with focal epilepsies should be considered as effective in children aged 4 years and above. This proposal will be limited to efficacy, noting that safety and pharmacokinetics may not necessarily be extrapolated.
There are subtle differences in the proposals being developed by the PEACE group in the USA and those presented here. Nonetheless, it is encouraging to note that these discussions are taking place, simultaneously and independently, on both sides of the Atlantic. Extrapolation is clearly high on the agenda of those interested in expediting the development of new medications for epilepsy.
References
European Medicines Agency. Concept paper on extrapolation of efficacy and safety in medicine development. 2012. EMA/129698/2012. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2013/04/WC500142358.pdf. Accessed 24 Nov 2014.
European Medicines Agency. Reflection paper on extrapolation of efficacy and safety in paediatric medicine development - Draft. 2016 EMA/199678/2016. http://www.ema.europa.eu/docs/en_GB/document_library/Regulatory_and_procedural_guideline/2016/04/WC500204187.pdf. Accessed 24 May 2016.
Dunne J, Rodriguez WJ, Murphy MD, et al. Extrapolation of adult data and other data in pediatric drug-development programs. Pediatrics. 2011;128:1242–9.
Bazzano AT, Mangione-Smith R, Schonlau M, et al. Off-label prescribing to children in the United States outpatient setting. Acad Pediatr. 2009;9:81–8.
Palmaro A, Bissuel R, Renaud N, et al. Off-label prescribing in pediatric outpatients. Pediatrics. 2014;135:49–58.
Food and Drug Administration. Guidance for industry: exposure-response relationships—study design, data analysis, and regulatory applications. 2003. http://www.gmp-compliance.org/guidemgr/files/EXPOSURE.PDF. Accessed 24 Nov 2014.
ICH Guidance. E11: note for guidance on clinical investigation of medicinal products in the paediatric population. 2001. (CPMP/ICH/2711/99). http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2009/09/WC500002926.pdf. Accessed 24 Nov 2014.
French JA, Kanner AM, Bautista J, et al. Efficacy and tolerability of the new antiepileptic drugs II: treatment of refractory epilepsy: report of the TTA and QSS subcommittees of the American Academy of Neurology and the American Epilepsy Society. Epilepsia. 2004;45:410–23.
European Medicines Agency. Conclusions of the paediatric epilepsy experts group meeting, held in London 1 September 2009. 2010. EMA/153272/2010. http://www.ema.europa.eu/docs/en_GB/document_library/Other/2010/05/WC500090218.pdf. Accessed 24 Nov 2014.
Pediatric News. FDA conducts analysis to assess acceptability of extrapolation of antiepileptic drug (AED) effectiveness in adults to children four years of age and older with partial onset seizures (POS). J Pediatr Pharmacol Ther 2016;21:98. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4778704/pdf/i1551-6776-21-1-98.pdf. Accessed 11 Apr 2016.
Fogarasi A, Jokeit H, Faveret E, et al. The effect of age on seizure semiology in childhood temporal lobe epilepsy. Epilepsia. 2002;43:638–43.
Pellock JM, Carman WJ, Thyagarajan V, et al. Efficacy of antiepileptic drugs in adults predicts efficacy in children—a systematic review. Neurology. 2012;79:1482–9.
Bourgeois BF, Goodkin HP. Efficacy of antiepileptic drugs in adults vs children, does one size fit all? Neurology. 2012;79:1420–1.
Rheims S, Cucherat M, Arzimanoglou A, et al. Greater response to placebo in children than in adults: a systematic review and meta-analysis in drug-resistant partial epilepsy. PLoS Med. 2008;5:1223–37.
Ginsberg G, Hattis D, Sonawane B, et al. Evaluation of child/adult pharmacokinetic differences from a database derived from the therapeutic drug literature. Toxicol Sci. 2002;66:185–200.
Battino D, Estienne M, Avanzini G. Clinical pharmacokinetics of antiepileptic drugs in paediatric patients. Part II. Phenytoin, carbamazepine, sulthiame, lamotrigine, vigabatrin, oxcarbazepine and felbamate. Clin Pharmacokinet. 1995;29:341–69.
Mintzer S, French JA, Perucca E, et al. Is a separate monotherapy indication warranted for antiepileptic drugs? Lancet Neurol. 2015;14:1229–40.
Chow SC, Chang M. Adaptive design methods in clinical trials. Boca Raton: CRC; 2011.
Berry SM, Carlin BP, Lee JJ, Muller P. Bayesian adaptive methods for clinical trials. Boca Raton: CRC; 2010.
VanderWeele TJ, Arah OA. Unmeasured confounding for general outcomes, treatments, and confounders: bias formulas for sensitivity analysis. Epidemiology. 2011;22:42–52.
Eisai Inc. Highlights of prescribing information (Banzel). 2015. https://www.banzel.com/pdfs/BanzelPI.pdf. Accessed 13 Jan 2016.
Glauser T, Kluger G, Sachedo R, et al. Efficacy and safety of rufinamide adjunctive therapy in patients with Lennox-Gastaut syndrome (LGS): a multicenter, randomized, double-blind, placebo-controlled, parallel trial [abstract no. LBS.001]. Neurology. 2005;64:1862.
Marson AG, Al-Kharusi AM, Alwaidh M. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet. 2007;369:1016–26.
Marson AG, Al-Kharusi AM, Alwaidh M, et al. The SANAD study of effectiveness of carbamazepine, gabapentin, lamotrigine, oxcarbazepine, or topiramate for treatment of partial epilepsy: an unblinded randomised controlled trial. Lancet. 2007;369:1000–15.
McIntyre J, Robertson S, Norris E, et al. Safety and efficacy of buccal midazolam versus rectal diazepam for emergency treatment of seizures in children: a randomised controlled trial. Lancet. 2005;366:205–10.
Lux AL, Edwards SW, Hancock E, et al. The United Kingdom Infantile Spasms Study comparing vigabatrin with prednisolone or tetracosactide at 14 days: a multicentre, randomised controlled trial. The Lancet. 2004;364:1773–8.
Glauser TA, Cnaan A, Shinnar S, et al. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy. N Engl J Med. 2010;362:790–9.
Novartis Pharmaceuticals. A placebo-controlled study of efficacy & safety of 2 trough-ranges of everolimus as adjunctive therapy in patients with tuberous sclerosis complex (TSC) & refractory partial-onset seizures (EXIST-3) [ClinicalTrials.gov identifier NCT01713946]. National Institutes of Health, ClinicalTrials.gov. 2000. https://clinicaltrials.gov/ct2/show/NCT01713946. Accessed 5 Mar 2015.
Shilling V, Williamson PR, Hickey H, et al. Processes in recruitment to randomized controlled trials of medicines for children (RECRUIT): a qualitative study. Health Technol Assess. 2011;15:1–116.
Sheridan PH, Jacobs MP. The development of antiepileptic drugs for children. Report from the NIH workshop, Bethesda, Maryland, February 17-18, 1994. Epilepsy Res. 1996;23:87–92.
Acknowledgments
The contents of this article are based on proposals made at an Epilepsy Expert Group meeting convened to elicit expert opinion on the acceptability of extrapolation in paediatric epilepsy research (Manchester, UK, 6 November 2014). IW, TJ, GS and LVH organised the meeting funded by the UK National Institute for Health Research (NIHR-RMOFS-2013-03-05). RA, JHC, AGM, TM, AM and PEMS attended the meeting. JMP contributed to the manuscript after the meeting.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The meeting on which the contents of this article are based was funded by the UK National Institute for Health Research (NIHR-RMOFS-2013-03-05). IW and TJ have received funding from the UK National Institute for Health Research (NIHR-RMOFS-2013-03-05 IW; NIHR-CDF-2010-03-32 TJ). IW has also received funding from the Medical Research Council (MR/M013510/1). LVH has received funding from the Medical Research Council (MR/J014079/1). The views expressed in this publication are those of the authors. The funders had no role in the design or delivery of the Expert Group meeting, or writing of the report. The corresponding author (LVH) had final responsibility for the decision to submit for publication. The Medical Research Council (grant MR/J014079/1) funded the open access fee for this manuscript.
Disclosure of Potential Conflicts of Interest
IW reports grants from National Institute for Health Research during the conduct of the study; and grants from Medical Research Council and grants from the pharmaceutical industry, outside the submitted work. TJ reports grants from National Institute for Health Research, during the conduct of the study; and grants from the Medical Research Council and the National Institute for Health Research, and other funding from the pharmaceutical industry, outside the study. GJS reports grants from National Institute for Health Research during the conduct of the study; and speaker fees from GSK, UCB Pharma and Eisai, and conference fees UCB Pharma, outside the submitted work. RA reports educational support, grants and honoraria from Desitin Pharma Ltd, Eisai, Shire, UCB Pharma and Viropharma, outside the submitted work before 2015. JHC has received (all paid to her department) a research grant from Vitaflo, honoraria for advisory boards from Nutricia, Shire, Takeda and UCB, and honoraria for speaking by Nutricia, Eisai, UCB and Shire, outside the submitted work. AGM reports grants from UCB Pharma, Eisai and GSK, and honorarium from UCB Pharma and Sanofi, outside the submitted work. TM reports travel grants from Viropharma, and personal speaking fees from Eisai, outside the submitted work. AM has received travel grants from UCB, Eisai and Cyberonics, meeting sponsorship from UCB, and honoraria from Eisai and UCB, outside the submitted work. PEMS reports grants from UCB Pharma, outside the submitted work. JMP reports grants and other funding from National Institutes of Health/National Institute of Neurological Disorders and Stroke (NIH/NINDS), Eisai, Lundbeck, Pfizer, Questcor, UCB Pharmaceuticals and Upshur Smith, grants from Centers for Disease Control and Prevention/Health Resources and Services Administration (CDC/HRSA) and Marinus Pharmaceuticals, and other funding from Acorda, Bial, Catalyst, GlaxoSmithKline, GLG, Guidepointe Global, Medscape, Neuropace, Sepracor and Sunovion, outside the submitted work. LVH reports grants from National Institute for Health Research and Medical Research Council, during the conduct of the study; and grants from the pharmaceutical industry, outside the submitted work.
Additional information
Dr. John M. Pellock sadly passed away after this article was written. The authors would like to acknowledge the important contribution Dr. Pellock made to this article and the field of epilepsy research.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Wadsworth, I., Jaki, T., Sills, G.J. et al. Clinical Drug Development in Epilepsy Revisited: A Proposal for a New Paradigm Streamlined Using Extrapolation. CNS Drugs 30, 1011–1017 (2016). https://doi.org/10.1007/s40263-016-0383-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-016-0383-y