Abstract
Background and Objectives
Trifluridine/tipiracil, registered for the treatment of patients with metastatic gastric and colorectal cancer, is a substrate and inhibitor for the organic cation transporter 2 (OCT2) and the multidrug and toxin extrusion protein 1 (MATE1), which raises the potential for drug–drug interactions with other OCT2/MATE1 modulators. Therefore, we prospectively examined the effect of an OCT2/MATE1 inhibitor (cimetidine) and substrate (metformin) on the pharmacokinetics of trifluridine.
Methods
In this three-phase crossover study, patients with metastatic colorectal or gastric cancer were sequentially treated with trifluridine/tipiracil alone (phase A), trifluridine/tipiracil concomitant with metformin (phase B) and trifluridine/tipiracil concomitant with cimetidine (phase C). The primary endpoint was the relative difference in exposure of trifluridine assessed by the area under the curve from timepoint zero to infinity. A > 30% change in exposure was considered clinically relevant. A p-value of < 0.025 was considered significant because of a Bonferroni correction.
Results
Eighteen patients were included in the analysis. Metformin did not significantly alter the exposure to trifluridine (− 12.6%; 97.5% confidence interval − 25.0, 1.8; p = 0.045). Cimetidine did alter the exposure to trifluridine significantly (+ 18.0%; 97.5% confidence interval 4.5, 33.3; p = 0.004), but this increase did not meet our threshold for clinical relevance. Metformin trough concentrations were not influenced by trifluridine/tipiracil.
Conclusions
Our result suggests that the OCT2/MATE1 modulators cimetidine and metformin can be co-administered with trifluridine/tipiracil without clinically relevant effects on drug exposure.
Clinical Trial Registration
NL8067 (registered 04-10-2019).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A potential drug–drug interaction between trifluridine/tipiracil and organic cation transporter 2 and multidrug and toxin extrusion protein 1-modulating drugs exists. |
This pharmacokinetic crossover study found no clinical relevant changes in systemic exposure to trifluridine when combined with either metformin or cimetidine. |
These data suggest that organic cation transporter 2 and multidrug and toxin extrusion protein 1 inhibitors or substrates can be safely co-administered with trifluridine/tipiracil in clinical practice. |
1 Introduction
Trifluridine/tipiracil (Lonsurf®, also known as TAS-102) is an oral antineoplastic agent consisting of a thymidine-based nucleoside analogue (trifluridine) and a thymidine phosphorylase inhibitor (tipiracil). Trifluridine/tipiracil is registered as monotherapy for patients with refractory metastatic colorectal cancer (mCRC) previously treated with fluoropyrimidine-based, oxaliplatin-based and irinotecan-based chemotherapy, and was recently shown to prolong survival further in these patients when combined with bevacizumab [1, 2]. In addition to mCRC, trifluridine/tipiracil is also registered for patients with metastatic gastric cancer previously treated with at least two lines of chemotherapy [3].
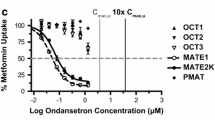
After oral administration, trifluridine is rapidly degraded by thymidine phosphorylase into the inactive metabolite 5-(trifluoromethyl)-uracil. Tipiracil prevents the degradation of trifluridine, and as such prolongs its systemic exposure [4, 5]. After metabolisation, trifluridine is primarily excreted via the urine (~ 55%) [6]. Tipiracil is excreted unchanged via urine and faeces [7]. Because the renal clearance of tipiracil (~300 mL/min) exceeds the glomerular filtration rate, a transporter-mediated excretion of tipiracil in the urine is suggested [6, 8]. In vitro studies showed that tipiracil is a substrate and inhibitor for the organic cation transporter 2 (OCT2) and the multidrug and toxin extrusion protein 1 (MATE1) [8]. OCT2 is found on the basolateral membrane of renal proximal tubular cells, facilitating the uptake of its substrates, while MATE1 is located on the brush-border membrane responsible for excretion. As tipiracil exposure is correlated with trifluridine exposure, the concomitant use of an inhibitor of OCT2 and MATE1 (e.g. cimetidine) may increase both tipiracil and trifluridine exposure. In contrast, exposure of an OCT2/MATE1 substrate (e.g. metformin) might be increased because of the inhibitory activity of tipiracil (Fig. 1). For other OCT2/MATE1 substrates, the pharmacokinetic interaction with an OCT2/MATE1 inhibitor has already been demonstrated. For example, cisplatin (an OCT2/MATE1 substrate) combined with pazopanib (an OCT1/MATE1 inhibitor) resulted in a significant in vitro increase in cisplatin exposure [9]. However, to our knowledge, there is no pharmacokinetic study available yet on a possible OCT2/MATE1 drug–drug interaction with trifluridine/tipiracil.
Schematic overview of the potential drug–drug interaction between tipiracil, metformin and cimetidine. Tipiracil is a substrate and inhibitor for the organic cation transporter 2 (OCT2) and the multidrug and toxin extrusion protein 1 (MATE1). Cimetidine inhibits the OCT2 and MATE1 transporter, whereas metformin is a substrate for the OCT2/MATE1 transporter (8). This figure was created using Biorender.com
Trifluridine/tipiracil treatment is known to induce toxicity: neutropenia was seen in 53–67% of patients in registration trials, of which 34–38% was grade 3 or higher [1, 3]. Other frequently occurring adverse events include anaemia (45–77%), nausea (37–48%) and fatigue (27–35%) [1, 3]. In a secondary analysis of the registration trial in mCRC, a relationship between exposure and the occurrence of grade ≥ 3 neutropenia and other grade ≥ 3 treatment-related adverse event was observed [8]. The potential effect on exposure by concomitant use of an OCT2/MATE1 inhibitor could therefore increase the incidence of grade ≥ 3 adverse events and lead to safety issues or premature treatment discontinuation.
Approximately one third of all patients with cancer are exposed to potentially dangerous drug–drug interactions, and this prevalence is expected to increase with age as polypharmacy is almost inevitable in elderly patients [10, 11]. Organic cation transporter 2/multidrug and toxin extrusion protein 1 inhibitors (e.g. cimetidine) and substrates (e.g. metformin) are commonly prescribed in patients with cancer. Acid-suppressive therapy with cimetidine was reported in 19% of patients with cancer aged older than 70 years [12]. Metformin is widely used for the treatment of type 2 diabetes mellitus, which is known to occur in 8–18% of patients with cancer [13].
In this study, we explored the influence of cimetidine and metformin on the exposure to trifluridine and described the tolerability of trifluridine/tipiracil in the absence and presence of metformin and cimetidine, respectively. In addition, we assessed the influence of trifluridine/tipiracil on metformin trough concentrations (Ctrough).
2 Materials and Methods
This study was a three-phase, one-way crossover clinical trial in patients using trifluridine/tipiracil, performed at the Erasmus MC Cancer Institute, Rotterdam, the Netherlands [14]. The study protocol was written in conformity with the Declaration of Helsinki and approval of the Medical Ethics Committee and the competent authorities was obtained. The study was registered at the European Clinical Trial Database (EudraCT 2019-00276-41) and the Dutch Trial Registry (NL8067).
2.1 Patients
Patients were included if they were aged 18 years or older, had a confirmed diagnosis of mCRC or metastatic gastric cancer with a registered indication for trifluridine/tipiracil, an Eastern Cooperative Oncology Group performance status ≤ 1, a body mass index between 18 and 30 kg/m2, and adequate kidney (estimated glomerular filtration rate ≥ 30 mL/min) and liver functions (serum aspartate aminotransferase and alanine aminotransferase ≤ 2.5 upper limit of normal). Patients were excluded if they could not abstain from medications or supplements that could interfere with either trifluridine/tipiracil, metformin or cimetidine (e.g. strong OCT2 or MATE1 inhibitors), had (any type of) diabetes, a known impaired drug absorption or any serious disease interfering with study treatment (e.g. HIV, hepatitis or organ transplant). All patients provided written informed consent.
2.2 Study Design
Eligible patients were already on treatment with or started treatment with trifluridine/tipiracil in a dosage of 35 mg/m2 twice a day (b.i.d.) during days 1–5 and 8–12 in 28-day treatment cycles. Upon discretion of the treating physician, reduced doses up to 20 mg/m2 b.i.d. were permitted in the case of toxicity. Phase A in this study (treatment days 1–5) consisted of trifluridine/tipiracil alone (Fig. 2). In Phase B, metformin 500 mg b.i.d. was added to trifluridine/tipiracil (days 8–12), followed by 2 additional days of metformin monotherapy (days 13 and 14). In Phase C, cimetidine 400 mg b.i.d. was combined with trifluridine/tipiracil during days 1–5 of a second treatment cycle. All patients were treated in the sequence of Phase A-B-C. Patients were provided with diaries to accurately record the timing and method of administering trifluridine/tipiracil, metformin and cimetidine during each study period. They were also required to return the used packaging of these medications to ensure proper tracking of drug usage.
2.3 Pharmacokinetics
Patients were admitted to the hospital on days 5 and 12 of the first trifluridine/tipiracil treatment cycle and on day 5 of the second treatment cycle for pharmacokinetic blood sampling. On the days of hospital admission, food intake was not permitted between 4 hours prior to and 1 hour after trifluridine/tipiracil administration. Free consumption of beverages was restricted between 1 hour before and 1 hour after trifluridine/tipiracil intake. Blood samples were collected before trifluridine/tipiracil intake and at 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 6, 8 and 12-hour timepoints after trifluridine/tipiracil intake. Two days after the second sampling day (day 14 of the first trifluridine/tipiracil cycle, to ensure a sufficient washout period of trifluridine/tipiracil), an additional blood sample was taken to determine a metformin Ctrough. Blood samples were collected in 4-mL lithium heparin blood collection tubes, processed into plasma within 30 minutes by centrifugation for 10 minutes at 2500–3000g (at 4 °C), and stored at −70 °C until the time of analysis. Trifluridine and metformin plasma concentrations were measured using a validated ultra-performance liquid chromatography-tandem mass spectrometry method. Briefly, trifluridine was extracted from 30-μL aliquots of human lithium heparinised plasma after the addition of 10 μL of internal standard working solution (10 ng/mL of triflurothymidine-13C,15N2 in acetonitrile) and 1.5 mL of ethyl acetate. After centrifugation, the organic phase was evaporated at 60 degrees under a gently stream of nitrogen. The residue was dissolved in an aliquot of 50 µL of water/formic acid (100:0.02, v/v) from which 2 µL was injected onto the high-performance liquid chromatography column. The concentrations were linear over the range of 10.0–1000 ng/mL with a lower limit of quantitation of 10.0 ng/mL. For the metformin analysis, 50 µL of human lithium heparinised plasma was mixed with 400 µL of a 2-mg/L metformin-d6 in methanol solution for protein precipitation. After vortexing and centrifugation, 50 µL of the supernatant was diluted with 800 µL of deionised water, 2 mM ammonium acetate and 0.1% formic acid from which 1 µL was injected into the ultra-performance liquid chromatography system. The concentrations were linear over a range of 0.2–80 mg/L. Pharmacokinetic parameters included exposure defined as the area under the curve from timepoint zero to infinity (AUC0–INF), maximum plasma concentration (Cmax) and the time until maximum plasma concentration (Tmax). The AUC0–INF and Cmax were dose corrected to 35 mg/m2 b.i.d. [pharmacokinetic parameter * (standard dose (35 mg/m2)/administered dose], as trifluridine was found to be dose proportional at the dose range of 40–70 mg/m2/day [15]. All pharmacokinetic parameters were calculated using Phoenix WinNonlin version 8.3 (Certara, Princeton, NJ, USA).
2.4 Toxicity
Toxicity was assessed during regular outpatient clinics, at baseline and during the pharmacokinetic sampling days, using the Common Terminology Criteria for Adverse Events (version 5.0, National Cancer Institute, Bethesda, MD, USA). All patients were given a diary during the study period and were requested to report any new or ongoing adverse events.
2.5 Statistical Analysis
The primary endpoint was the relative difference (RD) in exposure to AUC0–INF trifluridine, when used alone and in combination with metformin and cimetidine, respectively. A Bonferroni correction was applied by using an alpha of 0.025 and the calculation of 97.5% confidence intervals. A RD in the area under the curve of at least 30% was considered clinically relevant and the within-patient standard deviation was assumed to be 30% [16]. Based on the above parameters and after rounding to an even number, a total of 18 evaluable patients were required to detect a difference in RD with 80% power. Patients were evaluable if they completed all three phases (per-protocol analysis).
Analyses of the AUC0–INF, the Cmax and the minimum plasma concentration were performed on log-transformed observations, as these were assumed to follow a log-normal distribution [17]. Estimates for the mean differences in (log) area under the curve and Cmax were obtained for the two comparisons separately, and both were analysed using a paired t-test. The mean differences and CIs were then exponentiated to calculate the ratio of the geometric means, which can be interpreted as the RD in percentages. The Tmax was analysed by means of the Wilcoxon signed rank test and described with medians and interquartile ranges. The Ctrough of metformin combined with trifluridine/tipiracil was compared with the Ctrough of metformin monotherapy using a paired t-test on log-transformed data. Toxicity was described as the incidence of toxicity per study phase and was corrected for baseline toxicity. Chi-square tests were used to test for a statistical difference in toxicity between the different study phases.
3 Results
3.1 Patient Characteristics
Between October 2019 and May 2023, 23 patients were included in this study, of whom 18 were evaluable for the primary endpoint. Three patients prematurely discontinued trifluridine/tipiracil because of disease progression, one patient did not start trifluridine/tipiracil because of COVID-19 infection and one patient withdrew consent. The evaluable patients’ characteristics are presented in Table 1.
3.2 Pharmacokinetics of Trifluridine
The dose-corrected pharmacokinetics of trifluridine when taken alone, with metformin and with cimetidine are presented in Table 2. The combination with metformin did not result in a statistically significant change of exposure of trifluridine (− 12.6%; 97.5% confidence interval − 25.0, 1.8; p = 0.045). The geometric mean exposure (AUC0–INF) of trifluridine increased with 18.0% (97.5% confidence interval 4.5, 33.3; p = 0.004) when administered concomitantly with cimetidine. Figure 3 shows the trifluridine plasma concentration–time curves of the three different phases. The median Tmax ranged from 0.78 to 1.00 h. The Cmax and Tmax of trifluridine did not differ with concomitant use of metformin or cimetidine (Table 2).
Concentration–time curves of trifluridine during each study phase. Trifluridine/tipiracil alone (phase A, n = 18), compared to trifluridine/tipiracil with concomitant metformin (phase B, n = 18) and trifluridine/tipiracil with concomitant cimetidine (phase C, n = 18). The estimated parameters of patients were dose corrected to 35 mg/m2 of trifluridine/tipiracil. h hours
3.3 Pharmacokinetics of Metformin
All 18 evaluable patients had two metformin Ctrough samples available (one during trifluridine/tipiracil treatment and one during metformin monotherapy). The geometric mean Ctrough of metformin in combination with trifluridine/tipiracil was 0.24 mg/L. This did not differ significantly from the Ctrough of metformin monotherapy (0.15 mg/L, RD: − 38.2%; 95% CI − 70.7 to 30.4; p = 0.192).
3.4 Toxicity
Table 3 shows the occurrence and severity of patient-reported adverse events throughout the three study phases. The most frequently observed adverse events were anaemia (39–56%), fatigue (17–33%) and nausea (17–28%). One patient experienced grade ≥ 3 toxicity (anaemia grade 3) that resolved after transfusion and a dose reduction (70 to 55 mg/m2 per day) of trifluridine/tipiracil. No other dose reductions were performed during the study. Fatigue, nausea/vomiting and diarrhea seemed slightly more common in phase B, whereas anaemia and neutropenia were more common in phase C, compared with phase A, but these differences were not statistically significant. Constipation was reported significantly more often in phase A than in phases B or C.
4 Discussion
This is the first study to investigate the potential pharmacokinetic interaction between the OCT2/MATE1 substrate and inhibitor trifluridine/tipiracil and the OCT2/MATE1 substrate metformin and the OCT2/MATE1 inhibitor cimetidine. Metformin did not alter trifluridine exposure, whereas cimetidine resulted in a statistically significant, although not clinically relevant, 18% increase in trifluridine exposure. Moreover, trifluridine/tipiracil did not significantly alter metformin Ctrough.
In vitro studies suggested a potential effect on tipiracil exposure with concomitant OCT2/MATE1 inhibition due to delayed excretion [8]. Hence, we hypothesised that this could lead to an in vivo increase of trifluridine exposure. We observed that concomitant administration of cimetidine affected the elimination rate (increased exposure) but not the absorption and distribution kinetics (unaffected Cmax and Tmax). In the US Food and Drug Administration pharmacology assessment report, the concomitant use of OCT2 inhibitors was tested as a covariate in the population pharmacokinetic analysis (n = 239) on pharmacokinetic parameters such as the volume of distribution and clearance rate of tipiracil [15]. In this study, 10% of the patients used trifluridine/tipiracil concomitantly with a OCT2 inhibitor (most frequently famotidine or ranitidine). No clinically relevant effect was found on the pharmacokinetic parameters of tipiracil. Cimetidine is considered to be the most potent inhibitor of OCT2, compared to compounds such as famotidine [18, 19]. Therefore, based on our data, a clinically relevant interaction with other OCT2/MATE1 inhibitors and trifluridine/tipiracil is not expected.
In vitro data suggested an inhibitory effect on OCT2/MATE1 transporters by tipiracil. However, the inhibitory concentrations were higher than the human plasma Cmax at steady state [8]. Our data indeed confirm that the in vitro inhibitory effect did not result in a relevant drug–drug interaction in vivo. As metformin is considered the prototypic clinical substrate for OCT2/MATE1 according to the Food and Drug Administration, no relevant drug–drug interactions for trifluridine/tipiracil and other OCT2/MATE1 substrates are expected [20].
Data from the registration trial showed that the area under the curve of trifluridine increases with 31% in patients with mild renal impairment (creatinine clearance between 60 and 89 mL/min) and 43% in patients with moderate renal impairment (between 30 and 59 mL/min), compared with normal renal function (≥ 90 mL/min) [15]. As our study population primarily consisted of patients with a non-impaired renal function, caution is needed when extrapolating these results to patients with a renal impairment. In these patients, concomitant inhibition of OCT2/MATE1 transporters can further increase the exposure of trifluridine, thus theoretically resulting in a clinically relevant toxic concentration.
During both intervention phases (B and C), there was no outspoken increase in toxicity observed when compared to phase A. Despite toxicity being an observationally guided endpoint only due to a small sample size, this was in fact anticipated as neither cimetidine nor metformin induced a defined clinically relevant change in trifluridine/tipiracil exposure. There was a slight increase in the incidence of anaemia during phases B and C. However, this is most likely caused by a time effect, as haematological adverse events during trifluridine/tipiracil treatment are known to have a cumulative duration [21]. Moreover, a slight increase in the incidence of diarrhoea and vomiting was observed in phase B, which could also have been a direct effect of the metformin treatment.
A limitation of this study is that we did not have information on OCT2 or MATE1 genotypes of our patients. Several single nucleotide polymorphisms in both transporters have been identified in recent years that could alter the renal clearance, such as the rs316019 G>T in OCT2 or rs2289669 G>A in MATE1 [22, 23]. However, no single nucleotide polymorphisms have yet been shown to be of clinical relevance. Moreover, as a polymorphism would result in a reduced capacity of the OCT2/MATE1 transporter, it is not likely that this would have resulted in a clinically relevant effect of an OCT2/MATE1 inhibitor on the exposure of trifluridine/tipiracil. Another limitation is that patients were not randomised for the sequence of treatments (i.e. all patients were treated in the same order). Randomisation would have decreased the risks on sequence or carry-over effects [14]. Despite the fact that the washout period between the sample days was estimated to be sufficient enough to minimise a carry-over effect, a potential sequence effect cannot be ruled out. Building on the sequence effect limitation, the cumulative exposure to trifluridine/tipiracil was greatest in phase C, meaning phase C would have been at the greatest risk for cumulative exposure. If future studies are conducted, this can be minimised using a crossover study design.
5 Conclusions
Concomitant use of either metformin or cimetidine during treatment with trifluridine/tipiracil does not result in a clinically relevant change in trifluridine/tipiracil exposure in patients. These results suggest that in daily practice, combining trifluridine/tipiracil with any of these drugs can be done safely.
References
Mayer RJ, Van Cutsem E, Falcone A, Yoshino T, Garcia-Carbonero R, Mizunuma N, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med. 2015;372(20):1909–19.
Prager GW, Taieb J, Fakih M, Ciardiello F, Van Cutsem E, Elez E, et al. Trifluridine-tipiracil and bevacizumab in refractory metastatic colorectal cancer. N Engl J Med. 2023;388(18):1657–67.
Shitara K, Doi T, Dvorkin M, Mansoor W, Arkenau HT, Prokharau A, et al. Trifluridine/tipiracil versus placebo in patients with heavily pretreated metastatic gastric cancer (TAGS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19(11):1437–48.
Hong DS, Abbruzzese JL, Bogaard K, Lassere Y, Fukushima M, Mita A, et al. Phase I study to determine the safety and pharmacokinetics of oral administration of TAS-102 in patients with solid tumors. Cancer. 2006;107(6):1383–90.
Fukushima M, Suzuki N, Emura T, Yano S, Kazuno H, Tada Y, et al. Structure and activity of specific inhibitors of thymidine phosphorylase to potentiate the function of antitumor 2′-deoxyribonucleosides. Biochem Pharmacol. 2000;59(10):1227–36.
European Medicines Agency. Lonsurf summary of product characteristics. 2016. https://www.ema.europa.eu/en/documents/product-information/lonsurf-epar-product-information_en.pdf. Accessed 18 June 2024.
Lee JJ, Seraj J, Yoshida K, Mizuguchi H, Strychor S, Fiejdasz J, et al. Human mass balance study of TAS-102 using (14)C analyzed by accelerator mass spectrometry. Cancer Chemother Pharmacol. 2016;77(3):515–26.
Committee for Medicinal Products for Human Use (CHMP) European Medicines Agency. Assessment report Lonsurf 2016. https://www.ema.europa.eu/en/documents/assessment-report/lonsurf-epar-public-assessment-report_en.pdf. Accessed 18 June 2024.
Sauzay C, White-Koning M, Hennebelle I, Deluche T, Delmas C, Imbs DC, et al. Inhibition of OCT2, MATE1 and MATE2-K as a possible mechanism of drug interaction between pazopanib and cisplatin. Pharmacol Res. 2016;110:89–95.
Riechelmann RP, Del Giglio A. Drug interactions in oncology: how common are they? Ann Oncol. 2009;20(12):1907–12.
Lord S, Hall PS, Seymour MT. Concomitant medications in cancer patients: should we be more active in their management? Ann Oncol. 2010;21(2):430.
Sokol KC, Knudsen JF, Li MM. Polypharmacy in older oncology patients and the need for an interdisciplinary approach to side-effect management. J Clin Pharm Ther. 2007;32(2):169–75.
Suh S, Kim KW. Diabetes and cancer: cancer should be screened in routine diabetes assessment. Diabetes Metab J. 2019;43(6):733–43.
Lanser DAC, Van der Kleij MBA, Veerman GDM, Steeghs N, Huitema ADR, Mathijssen RHJ, et al. Design and statistics of pharmacokinetic drug-drug, herb-drug, and food-drug interaction studies in oncology patients. Biomed Pharmacother. 2023;163: 114823.
US Food and Drug Administration. Center for Drug Evaluation and Research. Lonsurf clinical pharmacology and biopharmaceutics review. 2015. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/207981Orig1s000ClinPharmR.pdf.
Schoenfeld DA. Statistical considerations for a cross-over study. http://hedwig.mgh.harvard.edu/sample_size/js/js_crossover_quant.html. Accessed 18 Jun 2024.
Committee for Medicinal Products for Human Use (CHMP) European Medicines Agency. Guideline on the investigation of bioequivalence. 2010. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-investigation-bioequivalence-rev1_en.pdf. Accessed 18 June 2024.
Koepsell H, Lips K, Volk C. Polyspecific organic cation transporters: structure, function, physiological roles, and biopharmaceutical implications. Pharm Res. 2007;24(7):1227–51.
Dumitras S, Sechaud R, Drollmann A, Pal P, Vaidyanathan S, Camenisch G, et al. Effect of cimetidine, a model drug for inhibition of the organic cation transport (OCT2/MATE1) in the kidney, on the pharmacokinetics of glycopyrronium. Int J Clin Pharmacol Ther. 2013;51(10):771–9.
US Food and Drug Administration. Drug development and drug interactions: table of substrates, inhibitors and inducers. 2023. https://www.fda.gov/drugs/drug-interactions-labeling/drug-development-and-drug-interactions-table-substrates-inhibitors-and-inducers. Accessed 18 June 2024.
Van Cutsem E, Ohtsu A, Lopez Busto N, Kanehisa A, Fougeray R, Winkler R, et al. Time to grade ≥ 3 adverse events in pts receiving trifluridine/tipiracil (TAS-102). J Clin Oncol. 2017;35(4_Suppl.):788.
Christensen MM, Pedersen RS, Stage TB, Brasch-Andersen C, Nielsen F, Damkier P, et al. A gene-gene interaction between polymorphisms in the OCT2 and MATE1 genes influences the renal clearance of metformin. Pharmacogenet Genom. 2013;23(10):526–34.
Becker ML, Visser LE, van Schaik RH, Hofman A, Uitterlinden AG, Stricker BH. Genetic variation in the multidrug and toxin extrusion 1 transporter protein influences the glucose-lowering effect of metformin in patients with diabetes: a preliminary study. Diabetes. 2009;58(3):745–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by an unrestricted grant by Servier. Servier did not have any role in designing, performing or analysing this study.
Conflict of interests
Bianca Mostert received consulting fees from Lilly, Servier, BMS, AstraZeneca and Amgen, and research funding from Sanofi, Pfizer and BMS. The other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics approval
The study protocol was written in conformity with the Declaration of Helsinki and approval of the Medical Ethics Committee of the Erasmus Medical Centre (MEC19-0560) and the competent authorities (NL70704.056.19) was obtained.
Consent to participate
All patients provided written informed consent before enrolment.
Consent for publication
Not applicable.
Availability of data and material
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Code availability
Not applicable.
Authors’ contributions
NADG, SAJB, LvD, KGAMH, YS, AvdP-P, RJvA, LP-M, IV, PdB, RWFvL, BM, FALME, EO-dH, SLWK and RHJM wrote the manuscript; SAJB, KGAMH, RWFvL, EO-dH, SLWK and RHJM designed the research; NADG, SAJB, LvD, KGAMH, YS, AvdP-P, RJvA, LP-M, BM, FALME, SLWK and RHJM performed the research; NADG and EO-dH analysed the data; IV and PdB contributed new reagents/analytical tools. All authors approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Guchelaar, N.A.D., Buck, S.A.J., van Doorn, L. et al. The OCT2/MATE1 Interaction Between Trifluridine, Metformin and Cimetidine: A Crossover Pharmacokinetic Study. Clin Pharmacokinet 63, 1037–1044 (2024). https://doi.org/10.1007/s40262-024-01390-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-024-01390-3