Abstract
Background and Objectives
Milrinone is an inotrope and vasodilator used for prophylaxis or treatment of low cardiac output syndrome after weaning from cardiopulmonary bypass (CPB). It is renally eliminated and has an acceptable therapeutic range of 100–300 μg/L, but weight-based dosing alone is associated with poor target attainment. We aimed to develop a population pharmacokinetic model for milrinone from premature neonates to adolescents, and to evaluate how age, renal function and recovery from CPB may impact dose selection.
Methods
Fifty paediatric patients (aged 4 days to 16 years) were studied after undergoing cardiac surgery supported by CPB. Data from 29 premature neonates (23–28 weeks’ postmenstrual age) treated for prophylaxis of low systemic blood flow were available for a pooled pharmacokinetic analysis. Population parameters were estimated using non-linear mixed effects modelling (NONMEM 7.5.1).
Results
There were 369 milrinone measurements available for analysis. A one-compartment model with zero-order input and first-order elimination was used to describe milrinone disposition. Population parameters were clearance 17.8 L/70 kg [95% CI 15.8–19.9] and volume 20.4 L/h/70 kg [95% CI 17.8–22.1]. Covariates included size, postmenstrual age and renal function for clearance, and size and postnatal age for volume. Milrinone clearance is reduced by 39.5% [95% CI 24.0–53.7] immediately after bypass, and recovers to baseline clearance with a half-time of 12.0 h [95% CI 9.7–15.2]. Milrinone volume was 2.07 [95% CI 1.87–2.27] times greater at birth than the population standard and decreased over the first days of life with a half-time of 0.977 days [95% CI 0.833–1.12].
Conclusion
Milrinone is predominately renally eliminated and so renal function is an important covariate describing variability in clearance. Increasing clearance over time likely reflects increasing cardiac output and renal perfusion due to milrinone and return to baseline following CPB.
Similar content being viewed by others
Renally eliminated drug pharmacokinetics are impacted by cardiopulmonary bypass (CPB), which may make dose selection challenging, especially in neonates, infants and children. |
Size, maturation, renal function and time after the end of CPB are important in determining milrinone clearance and thus an appropriate maintenance dose rate. |
We suggest a milrinone maintenance dose rate regimen of 0.375 μg/min/kg (neonates) or 0.75 μg/min/kg (infants and children) with a loading dose of 50 μg/kg for children undergoing CPB. |
1 Introduction
Milrinone is a type III phosphodiesterase inhibitor that increases cardiac contractility and myocardial relaxation rate, and decreases systemic vascular resistance. It does not raise myocardial oxygen consumption nor increase heart rate, which are favourable drug properties in patients with impaired myocardial oxygen delivery [1]. Milrinone is used in children for low cardiac output syndrome (LCOS) prophylaxis and treatment after cardiac surgery supported by cardiopulmonary bypass (CPB), and other indications such as prophylaxis of low systemic blood flow after premature birth. Mortality of patients who develop LCOS can exceed 20% [2] and so management of this low output state using pharmacological intervention may be required to reduce mortality.
An acceptable concentration range of 100–300 µg/L for LCOS prophylaxis and treatment has been suggested for milrinone [3,4,5,6,7,8]. However large variability in milrinone concentrations is seen between patients despite similar weight-based dosing strategies for loading dose and maintenance dose rate [6]. Milrinone loading doses are often infused over 10 min to 1 h to reduce the risk of hypotension. Identifying distribution volume population parameter variability above what is predicted by size is important to calculate a safe and effective loading dose. Renal function and drug clearance (CL) are expected to be reduced in patients who have developed LCOS compared with those being administered milrinone for prophylaxis and so may require lower maintenance dose rates. Vogt [4] recommended separate dosing guidelines for these two groups with larger maintenance doses in the prophylaxis group compared with the treatment group.
Cardiopulmonary bypass has been shown to cause renal dysfunction [9,10,11] and so patients administered milrinone are expected to have some degree of renal dysfunction at the initiation of therapy. Increasing cardiac output and return to homeostatic baseline means that milrinone clearance may increase over time after CPB. Differences in age, size and organ function contribute to large concentration variability seen with weight-based dosing, which is confounded by the impact of CPB. Both lack of pharmacological effect and adverse drug reactions can cause poor patient outcomes. Milrinone is predominately renally eliminated with approximately 80% excreted unchanged in the urine [12, 13], and so renal function is an important covariate to describe clearance variability. Quantifying the impact of age, size and organ function on milrinone pharmacokinetics can be used to determine an appropriate dose to reach a target concentration from premature neonates to adolescents.
2 Methods
2.1 Study Design
This was a prospective, observational study conducted at Starship Children’s Hospital, Auckland, New Zealand, from August 2011 to October 2012. Patients aged between 1 day and 18 years old undergoing cardiac surgery supported by CPB and receiving milrinone after surgery were eligible for inclusion. Written informed consent was obtained from the parents or legal guardians for all children who participated in the study. Ethical approval for this study was given by the Health and Disability Ethics Committee, reference CEN/09/04/016 with locality approval from Auckland District Health Board, reference A+4373.
2.2 Drug Administration and Blood Sampling
Milrinone (Primacor, Sanofi-Aventis, Auckland, New Zealand) was prescribed at a dose rate between 0.25 and 1.25 µg/kg/min, administered intravenously and initiated after the end of the CPB procedure (but during surgery). The maintenance dose rate was titrated empirically depending on haemodynamic and clinical response. Serial blood samples (up to 1 mL) were taken from an indwelling catheter starting in the operating room after surgery and then in the Paediatric Intensive Care Unit. Sampling occurred around clinical care and after any dose changes. The median time for the first blood sample to be taken after milrinone initiation was 5.17 h (95%ile interval 39 min to 34 h). Whole blood samples were kept on ice and then transferred to the laboratory where they were centrifuged at 3000×g for 15 min. Separated plasma samples were stored at − 80 °C until analysis.
2.3 Bioanalysis
Quantitation of total milrinone in human plasma in the Starship Hospital Clinical Study was performed using liquid chromatography coupled mass spectrometry (LC-MS). The assay was linear across the concentration range of 5–500 µg/L and the inter-day assay variability of < 15% coefficient of variation across all quality controls. The patient samples were analysed in two batches (batch 1 and batch 2) and the lower limit of quantitation for both batches was 5 µg/L.
2.4 Pooled Data
Data from another published study was available to conduct a pooled pharmacokinetic analysis [5]. The Paradisis et al. [5] study was a prospective, open-labelled, dose-escalation study conducted in 29 very premature neonates (< 28 weeks postmenstrual age [PMA]) administered milrinone for prophylaxis of low systemic blood flow following birth. Patients received an infusion of either 0.25 µg/kg/min, 0.5 µg/kg/min or 0.75 µg/kg/min for 3 h followed by 0.2 µg/kg/min. Blood samples were taken during and after the milrinone infusion and stored at − 30 °C until analysis. Quantitation of total milrinone in human serum in the Paradisis et al. [5] study used high performance liquid chromatography with ultraviolet detection (HPLC-UV), based on an assay reported by Edelson et al. [14]. The assay was linear across the concentration range of 20–1500 µg/L and the inter-day assay variability was < 10% coefficient of variation across all quality controls. The lower limit of quantitation was 20 µg/L.
2.5 Pharmacokinetics Analysis
One- two- and three-compartment models were investigated to describe milrinone distribution. Population parameters were a priori scaled for size using theory-based allometry [15, 16]. Normal fat mass (NFM) was used as a measure of size [17] (Eq. 1).
NFMi (Eq. 2) is the individual NFM calculated from total body mass (TBM) and fat free mass (FFM) predicted from neonates to adults [18]. An additional parameter, Ffat, describes both the mass and body composition effects on PK parameters. NFMstd (Eq. 3) is the standard value for NFM which may be calculated for a male with a TBM of 70 kg, an FFM of 56.1 kg, a height of 1.76 m and the drug and parameter specific value of Ffat.
Maturation of elimination process occurs over the first 2 years of life and so a maturation model was used to describe changes in CL (Eq. 4). This model was included a priori during model development.
PMA is postmenstrual age in weeks, TM50 is the maturation half-time and HILL is the exponent that describes the steepness of the maturation curve. Fmat approaches a value of 1 during infancy signalling completion of maturational processes.
Changes in body composition correlated with ageing may impact drug volume of distribution (V). An empirical exponential maturation function was investigated to describe changes in V with age, above what can be predicted by size alone (Eq. 5).
Vgrp is the group value of V after accounting for the fixed effects from covariates, Vpop is the population parameter value of V and Fsize is described in Eq. (1). The y-intercept of the function is determined by 1 + FV and describes the fractional difference in V at time = 0. TVOL is the maturation half-time when V is 50% of the mature value. Postnatal age (PNA) and PMA were explored as age descriptors to describe changes in V associated with the birth effect (PNA) or more gradual changes (PMA).
Renal function is a metric for kidney function that accounts for size, maturation and body composition. It is calculated from the ratio of estimated glomerular filtration rate (eGFR) to normal GFR (nGFR) [18] (Eq. 6).
Normal GFR is calculated using Eq. (7).
GFRstd is the standard GFR for a 70-kg TBM male, height of 176 cm, reported in Rhodin et al. [19] but updated using the models for FFR and nGFR described in O’Hanlon et al. [18]. Fsize is a factor for size using normal fat mass (Eq. 1), Fmat,PMA is a factor for maturation based on PMA and Fmat,PNA is a factor for maturation based on PNA, and describes the impact of the birth effect on maturation. Estimated GFR can be calculated under the assumption that creatinine clearance (CLcr) equals eGFR (Eq. 8).
CPR is creatinine production rate (predicted from neonates to adults in O’Hanlon et al. [18]) and Scr is serum creatinine concentration. Two Scr measurement were available in our dataset, one prior to surgery (baseline) and one at Day 1 (post-surgery). Serum creatinine measurements available post-surgery used a last-observation-carried-forward procedure for the calculation of renal function.
Milrinone increases cardiac output and so kidney function may improve, leading to increased clearance over time. An empirical exponential function was used to describe a fractional increase in clearance relative to clearance at therapy commencement (Eq. 9).
CLGRP is the group value of clearance after accounting for the fixed effects from covariates (e.g., size, age etc.), CLPOP is the population parameter value of clearance, f(size, …) includes the other clearance covariates (e.g., size, age, renal function) and TAD is time after dose (h). FCL is the fraction of clearance at the start of dose initiation and TCL is the half-time of 50% of the maximal fraction. The time-varying clearance model was incorporated in the differential equation solver block of the NM-TRAN control stream to avoid oversimplification of the model using step functions in patients with limited samples [20].
2.6 Data Analysis
Data were analysed using NONMEM (ICON Development Solutions, Maryland, USA) version 7.5.1 and Wings for NONMEM version 744 (http://wfn.sourceforge.net/). Population parameter estimates were obtained using NONMEM’s first-order conditional estimation method with the interaction option (FOCE-I). The convergence criterion (NSIG) was 3 with tolerance SIGL = 6. Model selection was based on the minimum objective function value (OFV), calculated by NONMEM from − 2log-likelihood. For two nested models, a decrease in the OFV of 3.84 was considered significant at p = 0.05, assuming one degree of freedom.
Parameter variability was described by a mixed effect approach with fixed and random effects. Fixed effect variability was based on a population standard parameter θPOP,std with a function of covariates such as size, height, sex, PMA and PNA to obtain the group parameter θgrp (Eq. 10).
θgrp is the group parameter after accounting for fixed effects due to covariates; θi is the individual parameter after accounting for random effects. Population parameter variability (PPV) was described using an exponential function of the random effect (Eq. 11), which assumes a log-normal distribution when used for simulation. The random effect, ηi, describes both between- and within-subject variability (normally distributed with mean 0 and variance ω2).
The residual unexplained variability for these models was described using a combined (additive + proportional) error model (Eq. 12).
Yi is the individual prediction of the observed value obtained from YPred i, the model prediction and the random effects εCV and εSD (proportional and additive error model components, respectively). The random effects are normally distributed with mean zero and a variance of σCV2 and σSD2.
Observations below the limit of quantitation (BLQ) were handled using the Beal [21] M3 method. The observations were modelled using maximum likelihood estimation, of which the likelihood for a BLQ observation is the likelihood that it is truly below the limit of quantitation [22]. Residual error was estimated separately for analysis of milrinone concentrations from batch 1, batch 2 (see study design) and Paradisis et al. [5].
2.7 Model Evaluation
Model evaluation was based on parameter plausibility, parameter uncertainty and visual predictive checks (VPCs). Parameter uncertainty was evaluated using non-parametric bootstrapping [23]. A total of 100 bootstrap replicates were used to describe the distribution of the parameter estimates and estimate the uncertainty of the prediction. Visual predictive checks were used to compare the 5th, 50th and 95th percentiles of the observed and predicted values from the model [24]. The 95% confidence intervals were estimated from the replicates of each of the prediction percentiles.
2.8 Simulations
Milrinone concentrations after CPB were simulated over 48 h using the final model to assess performance of dosing regimens. A total of 1000 subjects (without replacement) were sampled from the GAVamycin covariate database [25]. The sampled covariates included PMA, PNA, TBM, FFM, sex and serum creatinine. Different dosing regimens were assessed, including the dosing guidelines at Starship Children’s Hospital (0.25–0.75 μg/kg/min). The 2.5th, median and 97.5th prediction percentiles were compared to the acceptable concentration range (100–300 μg/L). The median prediction percentiles were stratified by age group (neonates, infants and children).
The following dosing regimens were assessed over 48 h with milrinone administered for 36 h.
-
1.
Milrinone 0.25 μg/kg/min.
-
2.
Milrinone 0.5 μg/kg/min.
-
3.
Milrinone 0.75 μg/kg/min.
-
4.
Milrinone 0.25 μg/kg/min for 4 h then 0.5 μg/kg/min for 32 h.
-
5.
LCOS prophylaxis indication from Vogt [4] presented in Supplementary Table S1 (see electronic supplementary material [ESM]).
-
6.
LCOS treatment indication from Vogt [4] presented in Supplementary Table S1 (see ESM).
-
7.
Milrinone 50 μg/kg loading dose over 1 h then 0.5 μg/kg/min.
-
8.
Milrinone 50 μg/kg loading dose over 1 h then 0.375 μg/kg/min (neonates) or 0.75 μg/kg/min (infants and children).
Regimens 1–3 are based on local hospital practice of milrinone 0.25–0.75 μg/kg/min.
3 Results
Fifty patients were recruited for this prospective observational study. Data from 29 patients were available for analysis from Paradisis et al. [5]. Demographic and clinical characteristics from both studies are summarised in Table 1. Primary covariate distributions of the combined dataset are shown in Supplementary Figure S1 (see ESM).
3.1 Sampling and Bioanalysis
Between one and eight blood samples were taken per patient (median five per patient). There were 369 (n = 245 from the Starship study and n = 124 from Paradisis et al. [5]) measurements available for pharmacokinetic analysis. Ten percent (n = 37) of the samples were below the limit of quantitation. No observations from Paradisis et al. [5] were below the limit of quantitation.
3.2 Pharmacokinetic Model
Milrinone was administered as an intravenous infusion between 0.25 and 1.25 µg/kg/min. Drug input was described using a zero-order input, with the amount determined from the dose rate and infusion duration. Milrinone disposition was best described by a one-compartment model with first-order elimination.
Size, maturation (PMA weeks) and renal function were included as covariates on CL. A time-varying function of CL based on time after dose initiation was also included in the model. Volume of distribution was scaled by size. This parameter also changed based on PNA (days) with neonates having a larger V than adults, after accounting for size. The Ffat parameter for both CL and V was estimated to be close to zero (~ 0.001) and so was fixed to zero in the final model. A covariance parameter between CL and V was also estimated.
3.3 Parameter Estimates
The final models for groups CL and V are shown in Eqs. (13) and (14).
The final model parameter estimates and bootstrap results are shown in Table 2. The fractional changes in CL (over time after dose initiation) and change in V (in the days after birth) predicted from the model are shown in Fig. 1.
Model predictions for time-varying clearance (CL) and postnatal age (PNA) maturation of volume. The fractional differences in parameter are in addition to those predicted from size, maturation and renal function for CL, and size for volume of distribution (V). The final parameter estimates from Table 2 were used for simulation
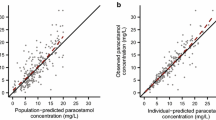
3.4 Visual Predictive Checks
The visual predictive check (VPC) for the final milrinone PK model is shown in Fig. 2. The observed percentiles are well described by the predictions with no systematic bias in the model predictions. The VPCs using PMA, TBM and RF as the independent variables are shown in Supplementary Fig. S2 (see ESM). The model describes the observed data percentiles well over the age, renal function and body mass range. The VPCs by study (Starship Hospital clinical study and Paradisis et al. [5] study) are shown in Supplementary Fig. S3 (see ESM). There is good agreement between the observed and predicted percentiles for both studies, but some systematic underprediction is observed in Paradisis et al. [5] between 15–23 h.
Visual predictive check (VPC) for the final milrinone pharmacokinetic model. The 5%, median and 95% percentiles of the distribution of the observations are in red and predictions are in black. The hollow circles in the left-side plot are the individual observations. The 95% confidence intervals for the prediction percentiles are shown by the purple shaded areas in the right-side plot. The yellow lines on the x-axis show the mid-point of data bins used in the construction of the VPC
3.5 Simulations
The covariate distributions for the sampled patients used for simulation are shown in Supplementary Fig. S4 (see ESM). The simulations using the pharmacokinetic model and dosing regimens described therein are presented in Fig. 3. The median predictions for infants and children are below the acceptable concentration range (< 100 μg/L) in A and for neonates it is above the acceptable range (> 300 μg/L) in C. The median predictions for all age groups in B and D are within the acceptable concentration range, but will be delayed in reaching an effective concentration. Using a loading dose and maintenance infusion (E–H) is associated with reaching a target concentration quickly. The median prediction for all age groups in E–H are within the acceptable concentration range, but substantial variability remains, as shown by the 97.5th prediction percentile in the simulations.
Simulation studies using the final pharmacokinetic models described in this work and dosing regimens presented in Supplementary Table S1 (see electronic supplementary material [ESM]). Concentrations from 1000 premature neonates to adolescents were simulated (covariate distributions presented in Supplementary Fig. S4 [see ESM]). The coloured lines are the median predictions for each age group, the coloured dots are the simulated time points and the outer thin black lines form the 95th prediction percentiles. The dashed lines indicate the acceptable concentration range (100–300 μg/L). The infant (blue) and child (green) lines are closely overlapping in A, B, C and G. LD loading dose, MDR maintenance dose rate
4 Discussion
We developed a population pharmacokinetic model for milrinone from very premature neonates to adolescents. Data were pooled from a clinical study conducted at Starship Children’s Hospital, Auckland, New Zealand and the Paradisis et al. [5] study. Age has been well established to describe maturation of clearance processes [15] but we also identified an age-dependent change in volume. Neonates had a higher volume (L/kg) than children and adults after accounting for allometrically scaled size, likely due to changes in body composition over the first days of life. Renal function described variability in clearance and is a useful metric for patients requiring milrinone, who usually have renal dysfunction after cardiac surgery supported by CPB [9,10,11].
Milrinone is predominately renally eliminated but a small fraction (~ 10%) is metabolised by glucuronide conjugation [26, 27]. Non-renal clearance of milrinone may increase as a partial compensatory mechanism in renal dysfunction [28]. Maturation of milrinone clearance will likely reflect both renal and non-renal elimination processes. Milrinone clearance is reported to be 17.6 L/h/70 kg in this study and 15.9 L/h/70 kg in another recent PK study [27]. These estimates are larger than the population standard GFR of 6.9 L/h/70 kg [18], which may indicate the involvement of tubular secretion in milrinone elimination.
The pooled dataset contained a large cohort of very premature neonates from Paradisis et al. [5]. Assessing renal function in 1- or 2-day old neonates remains challenging as serum creatinine concentration reflects maternal concentrations [29]. Renal function was assumed to equal 1 (normal renal function, their age, size and body composition) in the Paradisis et al. [5] dataset as all patients were <2 days old PNA. Mizuno et al. [7] and Hornik et al. [27] reported a proportional relationship between renal function and milrinone clearance. Our serum creatinine-based model for RF was a significant covariate on clearance and was also applied proportionally. Repeated measurements of serum creatinine (or another biomarker for renal function) over the full time course may explain more of the fixed effects variability in clearance due to improvement in renal function. However this is not expected to replace the need for a time-varying clearance component due to extrarenal elimination of milrinone and limitations of serum creatinine-based models for renal function [18, 30].
Paradisis et al. [5] and Giaccone et al. [31] reported population volume estimates (scaled to 70 kg TBM using theory-based allometry) of 42.2 L/70 kg and 29.9 L/70 kg (steady-state volume of distribution of 52.3 L/70 kg). These studies only contained premature neonates and indicated that neonates have a higher size-standardised volume than infants, children and adults. Foetal body composition and water distribution change considerably in utero, in the days after the birth event, and over the first months of life [32, 33]. We investigated using PNA (to describe the change in volume soon after birth) and PMA (to describe a more gradual change over months) as covariates for volume. An empirical function (Equation 5) was used to describe the maturation of volume caused by changes in body composition; a model that has been previously used for changes in paracetamol volume [34]. Our model for age-related changes in volume used PNA as a covariate for changes in body composition. At birth (0 days PNA), the estimate of volume is 42.6 L/h/70 kg and by 1 day PNA the estimate is 31.2 L/h/70 kg. After 4–5 volume maturation half-lives (TVOL), the maturation scaling factor approaches 1 and the population parameter estimate approaches 20.4 L/70 kg.
Milrinone is used in critically ill patients from very premature neonates to adults. It has a range of indications including post-cardiac surgery prophylaxis for LCOS and patent ductus arteriosus post-ligation cardiac syndrome, pulmonary hypertension of the newborn and acute decompensated heart failure. The Starship Hospital clinical study cohort had undergone cardiac surgery supported by CPB, whereas the Paradisis et al. [5] data were from very premature neonates with low systemic blood flow. Each indication may be associated with a different pathology, but all require pharmacological intervention to improve cardiac output. Milrinone has inotropic (increasing cardiac contractility), lusitropic (increasing rate of cardiac relaxation) and vasodilatory (relaxation of systemic vasculature) properties. It is usually administered at the end of the CPB procedure for LCOS prophylaxis. Patients in the Starship Hospital clinical study and patients from Paradisis et al. [5] both showed increasing clearance over time. This may be associated with milrinone’s mechanism of action of improving cardiac output, which may improve renal function, or a natural return to baseline following CPB. Time-varying clearance may be describing the underlying changes in organ function that occur with milrinone use, or simply improvement in organ function that occurs regardless of milrinone administration. Our model is unable to distinguish between these processes. They could be delineated by investigating changes in clearance of other renally eliminated drugs after cardiac surgery supported by CPB in patients not being administered milrinone. A PKPD model could explicitly explore whether milrinone’s pharmacodynamic effect (e.g., increasing cardiac output) changes it’s own clearance. This would require a drug effect measurement (e.g., cardiac output, stroke volume, blood pressure) alongside drug concentrations. The change in clearance may have clinical significance if the average concentration achieved with the dosing regimen is close to the lower bound of the acceptable concentration range. The half-time of return to ‘normal’ clearance was estimated to be ~ 12 h. After 4–5 half-times (i.e., 48 h), the change in clearance is theoretically effectively complete (analogous to reaching steady-state concentration after 4–5 half-lives with a constant rate infusion).
Simulations show that commonly used dosing regimens (Fig. 3A–C) may not be adequate to achieve a target concentration, associated with a target effect (increased cardiac output) and clinical outcome (prevention or treatment of LCOS). The milrinone 0.25 μg/kg/min infusion (Fig. 3A) shows the median prediction for infants and children is below the lower bound of the acceptable concentration range (100 μg/L), suggesting inadequate drug effect. The milrinone 0.5-μg/kg/min infusion (B) performs better than (A) and (C) (milrinone 0.75-μg/kg/min infusion), where the median prediction for neonates is ~ 400 μg/L and the 97.5th percentile for the 1000 subjects is ~ 900 μg/L. These concentrations may be associated with adverse drug effects (e.g., hypotension). This is a similar finding to using clonidine as a sedative agent in ventilated neonates, infants and children [35]. The opioid-sparing and sedative effects of clonidine were only observed in neonates (not infants and children) when all were administered the same weight-based maintenance dose rate [35]. Accounting for immaturity of clearance and subsequent longer elimination half-life in neonates means that an increased weight-based maintenance dose rate for infants and children would be required to reach the same opioid-sparing benefits [36]. Infants and children will require a higher milrinone weight-based maintenance dose rate than neonates to achieve a steady target concentration of 200 μg/L (the midpoint of the acceptable concentration range of 100–300 μg/L).
Milrinone loading doses are recommended to reach a target concentration quickly, associated with a target effect [4, 37]. Low cardiac output syndrome is associated with noteworthy morbidity and mortality and so undertreatment has serious implications. Administering an infusion without a loading dose means that it may be up to 2 h from the start of infusion before improved cardiac output, leading to LCOS development before sufficient pharmacological effect. We suggest a loading dose of 50 μg/kg be administered to reach the target concentration quickly. We simulated this loading dose be given over 1 h (the same duration as the Vogt [4] guidelines), which will reach the lower bound of the acceptable concentration range (100 μg/kg) within the first 20 min for all age groups. This is lower than the 75-μg/kg loading dose used in the double-blind randomised control trial used to establish milrinone effectiveness in paediatrics [38], and should avoid some of the excessive vasodilation. A maintenance dose rate of milrinone 0.375 μg/kg/min in neonates and milrinone 0.75 μg/kg/min in infants and children appears to be suitable to maintain a target concentration of 200 μg/L. Neonatal volume of distribution is higher in the days after birth and so the loading dose should be adjusted to account for this. Neonates 1–2 days old may require a larger weight-based loading dose to reach the same target concentration and so a dose of milrinone 75 μg/kg could be administered. By 5 days after birth, neonatal size standardised volume is the same as for infants, children and adults and so a milrinone 50-μg/kg loading dose should be sufficient.
5 Conclusion
We developed a pharmacokinetic model for milrinone pharmacokinetics from prematurity to adolescence. Maturation and changes in body composition were used to describe developmental changes in clearance and volume. Milrinone is commonly used after surgery supported by CPB, which is associated with renal dysfunction. Milrinone showed evidence of time-varying clearance which may be explained by increase in cardiac output and improved renal function, or a return to renal baseline following CPB. Simulations show substantial variability remains in milrinone pharmacokinetics when using a weight-based dosing regimen. We suggest a dosing regimen of milrinone 0.375 μg/min/kg (neonates) or milrinone 0.75 μg/min/kg (infants and children) and to include a milrinone 50-μg/kg loading dose before the infusion to reach the target concentration quickly. A full PKPD study is yet required to describe the time course of effect on cardiac output, how this might influence drug elimination, and the relationship between concentration and adverse drug reactions.
References
Grose R, Strain J, Greenberg M, LeJemtel TH. Systemic and coronary effects of intravenous milrinone and dobutamine in congestive heart failure. J Am Coll Cardiol. 1986;7(5):1107–13.
Algarni KD, Maganti M, Yau TM. Predictors of low cardiac output syndrome after isolated coronary artery bypass surgery: trends over 20 years. Ann Thorac Surg. 2011;92(5):1678–84.
Charisopoulou D, Leaver N, Banner NR. Milrinone in advanced heart failure: dose and therapeutic monitor outside intensive care unit. Angiology. 2014;65(4):343–9.
Vogt W. Evaluation and optimisation of current milrinone prescribing for the treatment and prevention of low cardiac output syndrome in paediatric patients after open heart surgery using a physiology-based pharmacokinetic drug–disease model. Clin Pharmacokinet. 2014;53(1):51–72.
Paradisis M, Jiang X, McLachlan AJ, Evans N, Kluckow M, Osborn D. Population pharmacokinetics and dosing regimen design of milrinone in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2007;92(3):F204–9.
Gist KM, Mizuno T, Goldstein SL, Vinks A. Retrospective evaluation of milrinone pharmacokinetics in children with kidney injury. Ther Drug Monit. 2015;37(6):792–6.
Mizuno T, Gist KM, Gao Z, Wempe MF, Alten J, Cooper DS, et al. Developmental pharmacokinetics and age-appropriate dosing design of milrinone in neonates and infants with acute kidney injury following cardiac surgery. Clin Pharmacokinet. 2019;58(6):793–803.
Gist KM, Korst A, Nakano SJ, Stauffer BL, Karimpour-Fard A, Zhou W, et al. Circulating cyclic adenosine monophosphate concentrations in milrinone treated paediatric patients after congenital heart surgery. Cardiol Young. 2021;31(9):1393–400.
Abu-Omar Y, Ratnatunga C. Cardiopulmonary bypass and renal injury. Perfusion. 2006;21(4):209–13.
Aydin SI, Seiden HS, Blaufox AD, Parnell VA, Choudhury T, Punnoose A, et al. Acute kidney injury after surgery for congenital heart disease. Ann Thorac Surg. 2012;94(5):1589–95.
Evans RG, Lankadeva YR, Cochrane AD, Marino B, Iguchi N, Zhu MZ, et al. Renal haemodynamics and oxygenation during and after cardiac surgery and cardiopulmonary bypass. Acta Physiol. 2018;222(3): e12995.
Gist KM, Goldstein SL, Joy MS, Vinks AA. Milrinone dosing issues in critically ill children with kidney injury: a review. J Cardiovasc Pharmacol. 2016;67(2):175–81.
Stroshane RM, Koss RF, Biddlecome CE, Luczkowec C, Edelsonx J. Oral and intravenous pharmacokinetics of milrinone in human volunteers. J Pharm Sci. 1984;73(10):1438–41.
Edelson J, Koss RF, Baker JF, Park GB. High-performance liquid chromatographic analysis of milrinone in plasma and urine: intravenous pharmacokinetics in the dog. J Chromatogr B Biomed Sci Appl. 1983;276:456–62.
Anderson BJ, Holford NH. Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol. 2008;48:303–32.
West GB, Brown JH, Enquist BJ. A general model for the origin of allometric scaling laws in biology. Science. 1997;276:122–6.
Holford NH, Anderson BJ. Allometric size: the scientific theory and extension to normal fat mass. Eur J Pharm Sci. 2017;109:S59–64.
O’Hanlon CJ, Holford N, Sumpter A, Al-Sallami HS. Consistent methods for fat free mass, creatinine clearance and glomerular filtration rate to describe renal function from neonates to adults. CPT Pharmacometr Syst Pharmacol. 2023;12(3):401–12.
Rhodin MM, Anderson BJ, Peters AM, Coulthard MG, Wilkins B, Cole M, et al. Human renal function maturation: a quantitative description using weight and postmenstrual age. Pediatr Nephrol. 2009;24(1):67.
Brochot A, Dunne A, Poggesi I, Vermeulen A, editors. Specifying models with time-dependent pharmacokinetic parameters in NONMEM. Athens: PAGE; 2011. p. 20.
Beal SL. Ways to fit a PK model with some data below the quantification limit. J Pharmacokinet Pharmacodyn. 2001;28(5):481–504.
Bergstrand M, Karlsson MO. Handling data below the limit of quantification in mixed effect models. AAPS J. 2009;11(2):371–80.
Parke J, Holford NH, Charles BG. A procedure for generating bootstrap samples for the validation of nonlinear mixed-effects population models. Comput Methods Progr Biomed. 1999;59(1):19–29.
Holford NH, editor. The visual predictive check—superiority to standard diagnostic (Rorschach) plots. PAGE. 2005;14:Abstr 738. http://www.page-meeting.org/?abstract=738. Pamploma, Spain.
Holford N, O'Hanlon CJ, Allegaert K, Anderson B, Falcão A, Simon N, et al. A physiological approach to renal clearance: from premature neonates to adults. Br J Clin Pharmacol. 2024;90(4):1066–80.
Young RA, Ward A. Milrinone. Drugs. 1988;36(2):158–92.
Hornik CP, Yogev R, Mourani PM, Watt KM, Sullivan JE, Atz AM, et al. Population pharmacokinetics of milrinone in infants, children, and adolescents. J Clin Pharmacol. 2019;59(12):1606–19.
Woolfrey S, Hegbrant J, Thysell H, Fox P, Lendrem D, Lockwood G, et al. Dose regimen adjustment for milrinone in congestive heart failure patients with moderate and severe renal failure. J Pharm Pharmacol. 1995;47(8):651–5.
Guignard J-P, Drukker A. Why do newborn infants have a high plasma creatinine? Pediatrics. 1999;103(4):e49.
Delanaye P, Cavalier E, Pottel H. Serum creatinine: not so simple! Nephron. 2017;136(4):302–8.
Giaccone A, Zuppa AF, Sood B, Cohen MS, O’Byrne ML, Moorthy G, et al. Milrinone pharmacokinetics and pharmacodynamics in neonates with persistent pulmonary hypertension of the newborn. Am J Perinatol. 2017;34(08):749–58.
Friis-Hansen B. Body water compartments in children: changes during growth and related changes in body composition: Kenneth D. Blackfan memorial lecture. Pediatrics. 1961;28(2):169–81.
Bauer K, Versmold H. Postnatal weight loss in preterm neonates < 1500 g is due to isotonic dehydration of the extracellular volume. Acta Pædiatrica. 1989;78:37–42.
Anderson BJ, van Lingen RA, Hansen TG, Lin Y-C, Holford NH. Acetaminophen developmental pharmacokinetics in premature neonates and infants: a pooled population analysis. J Am Soc Anesthesiol. 2002;96(6):1336–45.
Hünseler C, Balling G, Röhlig C, Blickheuser R, Trieschmann U, Lieser U, et al. Continuous infusion of clonidine in ventilated newborns and infants: a randomized controlled trial. Pediatr Crit Care Med. 2014;15(6):511–22.
Sheng Y, Standing JF. Pharmacokinetic reason for negative results of clonidine sedation in long-term-ventilated neonates and infants. Pediatr Crit Care Med. 2015;16(1):92–3.
Bailey JM, Hoffman TM, Wessel DL, Nelson DP, Atz AM, Chang AC, et al. A population pharmacokinetic analysis of milrinone in pediatric patients after cardiac surgery. J Pharmacokinet Pharmacodyn. 2004;31(1):43–59.
Hoffman TM, Wernovsky G, Atz AM, Kulik TJ, Nelson DP, Chang AC, et al. Efficacy and safety of milrinone in preventing low cardiac output syndrome in infants and children after corrective surgery for congenital heart disease. Circulation. 2003;107(7):996–1002.
Du Bois D, Du Bois E. A formula to estimate the approximate surface area if height and body mass be known. Arch Intern Med. 1916;17:863–71.
Pierce CB, Muñoz A, Ng DK, Warady BA, Furth SL, Schwartz GJ. Age-and sex-dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int. 2021;99(4):948–56.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This work was funded, in part, by a research grant from the Green Lane Research and Educational Fund, Auckland, New Zealand. This work used a license for NONMEM granted by ICON to the Australian Centre of Pharmacometrics. The Australian Centre for Pharmacometrics is an initiative of the Australian Government as part of the National Collaborative Research Infrastructure Strategy.
Conflict of interest
Conor J. O’Hanlon, Anita Sumpter, Brian J. Anderson, and Jacqueline A. Hannam declare that they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Data availability
The Starship Hospital Clinical Study dataset generated and analysed during the current study is available from the corresponding author on reasonable request.
Ethics approval
Ethical approval for the Starship Hospital Clinical Study was given by the Health and Disability Ethics Committee, New Zealand, reference CEN/09/04/016 with locality approval from Auckland District Health Board, New Zealand, reference A+4373.
Consent to participate
Written informed consent was obtained from the parents or legal guardians for participants in the Starship Hospital Clinical Study.
Consent for publication
Not applicable.
Code availability
The NM-TRAN control stream is available in the supplementary materials.
Author contributions
AS and BJA designed the research. CJOH, AS, BJA and JAH performed the research. CJOH, AS, BJA and JAH analysed the data. All authors contributed to critically reviewing the manuscript and gave their final approval for submission.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
O’Hanlon, C.J., Sumpter, A., Anderson, B.J. et al. Time-Varying Clearance in Milrinone Pharmacokinetics from Premature Neonates to Adolescents. Clin Pharmacokinet (2024). https://doi.org/10.1007/s40262-024-01372-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s40262-024-01372-5