Abstract
Background and Objective
High variability in tacrolimus pharmacokinetics directly after lung transplantation (LuTx) may increase the risk for acute kidney injury (AKI) and transplant rejection. The primary objective was to compare pharmacokinetic variability in patients receiving tacrolimus orally versus intravenously early after LuTx.
Methods
Pharmacokinetic and clinical data from 522 LuTx patients transplanted between 2010 and 2020 in two university hospitals were collected to compare orally administered tacrolimus to intravenous tacrolimus early post-transplantation. Tacrolimus blood concentration variability, measured as intrapatient variability (IPV%) and percentage of time within the therapeutic range (TTR%), was analyzed within the first 14 days after LuTx. Secondary outcomes were AKI, acute rejection, length of stay in the intensive care unit (ICU), and mortality in the ICU and during hospital admission.
Results
We included 224 patients in the oral and 298 in the intravenous group. The mean adjusted IPV% was 10.8% (95% confidence interval [CI] 6.9–14.6; p < 0.001) higher in the oral group (27.2%) than the intravenous group (16.4%). The mean TTR% was 7.3% (95% CI − 11.3 to − 3.4; p < 0.001) lower in the oral group (39.6%) than in the intravenous group (46.9%). The incidence of AKI was 46.0% for oral and 42.6% for intravenous administration (adjusted odds ratio [OR] 1.2; 95% CI 0.8–1.8; p = 0.451). The frequencies of clinically diagnosed acute rejection in the oral and intravenous groups were nonsignificant (24.6% vs 17.8%; OR 1.5 [95% CI 1.0–2.3; p = 0.059]). ICU and hospital mortality rate and ICU length of stay were similar.
Conclusions
Administering tacrolimus orally directly after LuTx leads to a higher variability in blood concentrations compared to intravenous administration. There was no difference in the occurrence of AKI or transplant rejection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Oral tacrolimus administration compared to continuous intravenous administration early after lung transplantation leads to a higher variability in blood concentrations with lower time within the therapeutic range. |
Oral administration of tacrolimus does not increase the frequency of acute kidney injury (AKI), although AKI stage 1 has been observed more often in the case of oral administration versus continuous intravenous administration. |
Rejection rates did not differ for oral versus continuous intravenous administration. While it may not have reached clinical significance, a difference of 28% maybe relevant for long-term graft outcomes. |
1 Introduction
Tacrolimus-based immunosuppressive regimes are considered standard of care after lung transplantation (LuTx) [1]. Nonetheless, tacrolimus is known to have a narrow therapeutic range and high interindividual pharmacokinetic (PK) variability, resulting in an increased risk of adverse effects from subtherapeutic and supratherapeutic tacrolimus blood concentrations. Cohort studies in LuTx patients found an association between higher tacrolimus PK variability and increased rejection and mortality [2,3,4], whereas another study did not [5]. Overall, unfortunately, acute rejection is not uncommon in the LuTx population. The registry of the International Society of Heart and Lung Transplantation (ISHLT), which contains data from > 60,000 LuTx recipients transplanted worldwide, reports treated acute rejection of 28% within the first year [6]. Consequently high tacrolimus trough levels are pursued post-LuTx, with the drawback of increased tacrolimus toxicity, in particular acute kidney injury (AKI) [7,8,9,10]. Especially in the early phase post-LuTx, a low variability in tacrolimus levels is of importance to lower the risk for adverse reactions when the risk for other postoperative complications is highest. Hence, close therapeutic drug monitoring (TDM) is an essential part of early post-transplantation care.
Intravenous versus oral administration of tacrolimus potentially results in more stable blood concentrations within the therapeutic range, because intravenous administration of tacrolimus bypasses the highly variable absorption step and may diminish the variation in bioavailability as an important contributing factor to high variability of tacrolimus blood levels [11].
In clinical care, consensus is lacking on the optimal route of administration in the early post-transplantation period. The oral and intravenous routes are both used to administer tacrolimus early after LuTx. Currently, there is a scarcity of substantial studies on different tacrolimus administration routes in the early post-LuTx period and their effects on intrapatient PK variability (IPV).
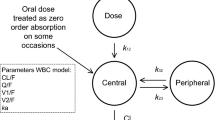
IPV is the extent of variation in tacrolimus (trough) concentrations within an individual patient over a certain period of time, often expressed as standard deviation (SD), mean absolute deviation (MAD), coefficient of variation (CV), and time within therapeutic range (TTR) [12]. Blood concentrations may differ due to changes in PK as well as changes in dose due to stringent TDM early after transplantation, making interpretation of the variability challenging. To accurately determine variability, intrapatient variability (IPV%) based on absolute concentrations could be used, as each single concentration is included in this equation [13]. Additionally, the (percentage of) time within the therapeutic range (TTR%) is of relevance. A patient may show high IPV within the therapeutic range or low IPV outside of the therapeutic range. The latter still has an increased risk for toxicity despite the low IPV.
The primary objective of this study was to compare the effect of a dosing strategy with intermittent oral versus continuous intravenous administration of tacrolimus on PK variability, measured as IPV% and TTR%, early post-LuTx. The secondary objectives were to investigate whether the dosing strategy was associated with AKI, acute rejection of the lung allograft, length of intensive care unit (ICU) stay, and mortality during ICU and hospital admission. The hypothesis was that patients receiving oral tacrolimus would have higher PK variability and consequently more adverse events such as AKI and acute rejection early post-LuTx.
2 Methods
2.1 Study Population
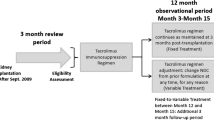
In this retrospective, multicenter, observational cohort study, patients ≥ 18 years of age who underwent LuTx in two university hospitals in the Netherlands (the University Medical Center Utrecht [UMCU] and the University Medical Center Groningen [UMCG]) between January 2010 and January 2020 were assessed for eligibility. Data from lung retransplantations were excluded. Patients were excluded if less than three tacrolimus concentrations were available within the first 14 days post-LuTx, because this is the minimum number of samples to calculate IPV% [13]. Moreover, patients with missing data regarding tacrolimus concentrations and patients whose tacrolimus concentrations were not analyzed with liquid chromatography-mass spectrometry (LC-MS/MS) were excluded (Fig. 2).
2.2 Post-transplantation Regimens
The protocol in the UMCU was to initiate oral immediate release (IR) tacrolimus in a dosage of 0.07 mg/kg twice daily on the first day after LuTx. Continuous intravenous tacrolimus in the UMCG was started 12 h after perfusion of the transplanted lung(s), at a dosage of 0.01 mg/kg/24 h. Non-polyvinylchloride lines were used to administer tacrolimus intravenously. Once the recipient experienced sufficient bowel movement with defecation, the route of administration was switched to a daily oral dose 10 times higher than the daily intravenous dose, divided into two doses per day. When patients had polyurethane nasogastric tubes in place and were receiving tube feeding, an extemporaneously compounded tacrolimus dispersion was administered in the UMCG (tacrolimus dispersion 0.5 mg/mL, Pharmacy A15 EP471). This dispersion conforms to the standard set by the European Pharmacopoeia. In the UMCU, this was done by dispersing prograft tablets (Astellas Pharma Europe BV) in a syringe with water. When patients were extubated and able to swallow, prograft tablets were used in both centers. The treatment protocols of both hospitals can be found in supplementary Table S1 (see the electronic supplementary material).
In both hospitals, a therapeutic range of 12–15 μg/L was aimed for during the first week after LuTx and 10–15 μg/L during the second week. Daily blood (trough) concentrations determined the need for dose adjustments. The additional (immunosuppressive) regimens were similar between the two centers (supplementary Table S1), consisting of basiliximab induction, mycophenolate mofetil, (methyl)prednisolone, prophylactic antibiotics, antivirals, fungicides, thromboprophylaxis, and analgesics, with a few small differences that were deemed irrelevant for the outcome of this study. Hence, the main difference was the administration route of tacrolimus initiated directly after LuTx.
2.3 Tacrolimus Concentrations
Tacrolimus blood concentrations were analyzed by means of validated TSQ Quantiva LC-MS/MS methods, equipped with a Vanquish Horizon UPLC system with binary pump, autosampler and an Accucore C18 50 × 2.1-mm column with 2.6-µm solid-core particles, in both centers [14]. All instruments were from Thermo Fisher Scientific (Waltham, MA, USA).
Peak concentrations in intermittent oral dosing were excluded since they may bias the variability. Potential peak concentrations were identified if the following two conditions were true: (1) the difference between the potential peak concentration and the preceding and following concentration was minimally 7 μg/L and (2) the two preceding and the two following concentrations showed a difference of maximally 3 μg/L. A sensitivity analysis was performed to define the optimal limits for identification. These potential peak concentrations were excluded if the timing of the sample or clinical factors (e.g., elevation of tacrolimus dose, the initiation or termination of cytochrome P450 3A [CYP3A4]- or adenosine triphosphate [ATP]-binding cassette sub-family B member 1 [ABCB1] inhibitor, diarrhea, or packed red cells therapy) could not explain the unusually high concentration.
2.4 Data Collection
Data on demographics, laboratory results, lengths of hospital admission, and mortality within the admission period were extracted from the patient data monitoring systems. For the oral group, data were extracted from Metavision (lte Medical, Tiel) and HiX© (Chipsoft BV, Amsterdam); for the intravenous group, data were extracted from Metavision and Epic (Epic System Corp., Verona, Wisconsin, USA). Information on liver enzyme, CYP enzyme, and transporter activity values were not incorporated in this study, because in an earlier cohort of heart transplantation and LuTx patients, a variability in bioavailability of 55% was observed, overwhelming all other co-variates [11]. Moreover, tacrolimus blood concentrations are the resultant of all covariates together.
2.5 Primary and Secondary Outcome Measurements
The primary outcome was variability, defined as the IPV% and the TTR%. The intrapatient variability was calculated as follows [13], in which X was the mean of all available concentrations in the first 14 days after LuTx, Xt was each individual concentration within the period mentioned, and T was the number of available tacrolimus concentrations:
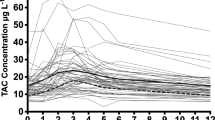
TTR% was calculated using linear interpolation to determine the time that the lower or upper limit of the therapeutic range was crossed (Fig. 1) [15]. The variability outcomes were determined with and without weighing for the number of tacrolimus samples available per patient.
One of the secondary outcomes was the occurrence of AKI, within the first week after LuTx. Daily creatinine assessment was part of the standard care protocol in both centers. AKI was defined as an increase in serum creatinine (SCr) to ≥ 1.5 times baseline within 7 days after LuTx or if SCr increased ≥ 26.5 μmol/L within 48 h, according to the Kidney Disease: Improving Global Outcomes (KDIGO) criteria [16]. AKI could be further divided into three AKI stages. AKI stage 1 was defined as a 1.5- to 1.9-times increase in SCr compared to baseline or an increase ≥ 26.5 µmol/L. AKI stage 2 was defined as a 2.0- to 2.9-times increase in SCr compared to baseline. AKI stage 3 was defined as such if SCr had increased 3.0 times compared to baseline, if the SCr had increased to ≥ 353.6 µmol/L, or if renal replacement therapy (RRT) was initiated. No information was available on urine output.
Well described risk factors for AKI following LuTx were used in the analysis whenever available and included age, sex, baseline estimated glomerular filtration rate (eGFR), primary lung disease, type of LuTx (single, double, heart-lung), post-LuTx use of extra corporeal life support (ECLS), and pre-LuTx comorbidities such as chronic kidney disease (CKD), and diabetes mellitus (DM) [7, 17, 18]. CKD was defined as a baseline eGFR < 60 mL/min/1.73m2. For DM, a pre-existent diagnosis in the patient dossier was used.
Another secondary outcome was the occurrence of acute rejection, defined as clinically diagnosed (UMCU and UMCG) rejection and treated with pulse methylprednisolone 1000 mg during 3 consecutive days. In the UMCG, routine lung biopsies are taken before hospital discharge. In the UMCU, this is not routine. Rejection data were included in the analyses when clinically diagnosed within the first 6 weeks after LuTx. Table S2 in the electronic supplementary material shows the clinical and diagnostic approaches for diagnosing acute rejection in both hospitals. Biopsy-proven acute rejection was discarded from the analyses because comparison was not possible between the two groups. Finally, length of stay in the ICU and mortality in the ICU and during hospital admission were secondary outcomes.
2.6 Statistical Analysis
Population characteristics are presented as mean ± SD, median (interquartile range [IQR]), or count (%) for normally distributed continuous variables, non-normally distributed continuous variables, and nominal variables, respectively.
The analyses were performed on an intention-to-treat basis. The independent samples t test was used to evaluate the difference in mean IPV%, TTR%, and length of stay. To investigate the difference in AKI stages, rejection, and mortality, the Chi-square test was used.
Univariate linear regression was performed in order to investigate the effect of the dosing strategy on IPV% and TTR% and univariate logistic regression to investigate the effect of the dosing strategy on AKI and rejection. Interaction terms were introduced to investigate effect modification. A variable was regarded as an effect modifier if the p value of the interaction term was < 0.05. If possible, results were stratified by significant effect modifiers. Covariates with a significant asymmetrical distribution between the groups were added to the multiple regression models. Next, the effect of statistically significant confounders was tested. If the percentage difference between the unadjusted and adjusted (Exp)B of the determinant was ≥ 10%, it was adjusted for. Identified confounders and effect modifiers were incorporated into the multiple linear or logistic regression model.
The differences in means (B), odds ratios (ORs), 95% confidence intervals (CIs), and the p values were reported. A p value < 0.05 for two-tailed tests was considered statistically significant. IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, NY, USA) was used to perform all statistical analyses.
By including only participants with the minimum numbers of tacrolimus samples needed for IPV% calculations, we ensured complete datasets for analyses. Secondary outcome analyses were based on available cases without imputing missing data. As AKI was defined as an increase in SCr within 7 days after LuTx, data on participants who died within 7 days post-LuTx were not used in these analyses. Also length of hospital stay data were incomplete and therefore not used.
3 Results
3.1 Study Population
Of 584 patients assessed for eligibility, 522 patients were included for analysis. Oral tacrolimus was used in 224 patients and intravenous tacrolimus in 298 patients. The flow of the study population is visualized in Fig. 2. Five out of 2591 tacrolimus concentrations in the oral group were identified as peak concentrations and excluded. A total of 5704 tacrolimus concentrations were available to calculate PK variability.
Table 1 describes the baseline characteristics of patients at the time of LuTx. The baseline characteristics were balanced for both groups but not for the primary cause of lung failure. The majority of patients in the oral group had lung failure caused by restrictive pulmonary disease followed by obstructive pulmonary disease. For the intravenously treated patients, obstructive pulmonary disease was the main cause and restrictive pulmonary disease thereafter (p < 0.001).
3.2 Pharmacokinetic Variability
Table 2 presents the primary comparison in PK variability parameters between the oral and intravenous groups. The weighted mean IPV% was significantly higher in the oral group (31.7% ± 10.5) compared to the intravenous group (29.2% ± 10.9) (p < 0.001). The weighted mean TTR% was 35.5% ± 15.8 for the oral group and 35.0% ± 17.6 for the intravenous group (p = 0.235). The intravenous group spent relatively more time above the therapeutic range (TAR%) (34.4% ± 22.6) than the oral group (26.0% ± 16.8) (p < 0.001), whereas the oral group spent more time beneath the therapeutic range (TBR%) (38.5% ± 19.3) than the intravenous group (30.7% ± 18.8) (p < 0.001). The average, minimum, and maximum tacrolimus concentrations were similar for both groups.
The identified effect modifiers for IPV% were sex, primary lung disease, baseline eGFR, hematocrit, ECLS, and RRT. After adjustment, the mean IPV% was 10.8% higher in the oral group (27.2%) than in the intravenous group (16.4%) (95% CI 6.9–14.6; p < 0.001). Confounders for TTR% were primary lung disease, hematocrit, and ECLS, and effect modifiers were sex, a pre-LuTx diagnosis of DM, baseline eGFR, and RRT. After adjusting for these confounders and effect modifiers, the mean TTR% was 7.3% lower in the oral group (39.6%) than in the intravenous group (46.9%) (95% CI − 11.3 to − 3.4; p < 0.001). Table S3 in the electronic supplementary material shows a complete overview of these results.
3.3 Kidney Function
The frequency of AKI within 1 week after LuTx was 46.0% in the oral group and 42.6% in the intravenous group (Table 3). The OR for AKI was 1.1 (95% CI 0.8–1.6; p = 0.484) for the oral group compared to the intravenous group (Table S4 in the electronic supplementary material). AKI stage 1 occurred in 24.6% and 15.8% in the oral and intravenous groups, respectively (OR 1.7; 95% CI 1.1–2.7; p = 0.014). AKI stage 2 occurred in 10.3% and 12.8% in the oral and intravenous groups, respectively (OR 0.8; 95% CI 0.4–1.3; p = 0.368). AKI stage 3 occurred in 11.2% and 14.1% in the oral and intravenous groups, respectively (OR 0.8; 95% CI 0.4–1.3; p = 0.308).
The risk factors for AKI that differed between the two groups were primary lung disease and ECLS. All other risk factors (i.e., age, sex, baseline eGFR, pre-LuTx DM and CKD, and type of LuTx) did not differ. Hematocrit and ECLS were identified as confounders for all AKI outcomes except AKI stage 1. The mean lowest hematocrit value in the first 14 days after LuTx was higher in the oral group (0.28 L/L) than in the intravenous group (0.23 L/L) (p < 0.001). Furthermore, ECLS post-LuTx was used in 35.3% of cases in the oral group and in 20.1% of cases in the intravenous group (p < 0.001) (Table 3).
The adjusted odds ratio (aOR) for AKI was 1.2 (95% CI 0.8–1.8; p = 0.451) for the oral group compared to the intravenous group. AKI stage 1 did not have any confounders or effect modifiers. Hence, the OR was definitive. The aOR for AKI stage 2 was 1.0 (95% CI 0.5–1.8; p = 0.936) for the oral group compared to the intravenous group. After adjusting for the confounders hematocrit and ECLS and the effect modifier baseline eGFR, the aOR for AKI stage 3 was 6.9 (95% CI 0.6–78.5; p = 0.119) for the oral group compared to the intravenous group.
Moreover, when we stratified for a higher or lower IPV% with a threshold of 30.3% (mean weighted IPV%), in the oral group the higher IPV% related to a higher risk of AKI (52.7% vs 39.3%; p = 0.044). In the intravenous group, the occurrence of AKI was lower in the group with higher IPV% (29.4% vs 51.4%; p < 0.001).
3.4 Rejection
The frequency of clinically diagnosed acute rejection within 6 weeks after LuTx was 24.6% in the oral group and 17.8% in the intravenous group (Table 3). The OR for acute rejection was 1.5 (95% CI 1.0–2.3; p = 0.060) for the oral group compared to the intravenous group. Sex was identified as an effect modifier. The aOR for rejection was 2.6 (95% CI 1.4–4.9; p = 0.003) for the male oral group compared to the male intravenous group (Table S5 in the electronic supplementary material). The aOR was 0.9 (95% CI 0.5–1.7; p = 0.803) for the female oral group compared to the female intravenous group. To gain more insight into the correlation between the TBR% and occurrence of rejection, the weighted median TBR% of 33.6% was used to stratify the whole cohort. Within the whole cohort, the OR for rejection was 1.2 (95% CI 0.8–1.7; p = 0.404) for patients with a TBR% ≥ 33.6% compared to patients with TBR% < 33.6%. When stratified by mean weighted IPV% (30.3%), in the oral group, the rejection rate was higher in patients with high IPV% (34.8% vs 14.3%; p < 0.001), and in the intravenous group, the rejection rate was comparable (29.4% vs 34.6%; p = 0.346). In the intravenous group, an additional 44 patients (14.8%) received treatment for biopsy-proven rejection within the first 6 weeks after LuTx. Although these patients did not exhibit clinically suspected acute rejection, their pathological findings indicated rejection. Consequently, all 44 patients received pulse methylprednisolone treatment. This last aspect remains unexplored for the oral group, in which routine lung biopsies were not performed.
3.5 ICU Length of Stay and Mortality
The median length of stay in the ICU did not differ significantly between the oral and the intravenous group; 7 days (4–17) and 6 days (3–18), respectively (p = 0.614). Mortality during admission to the ICU was similar for both groups: 17 patients (7.6%) in the oral group and 16 (5.4%) in the intravenous group (p = 0.828). During hospital admission, 20 patients (8.9%) in the oral group and 25 patients (8.4%) in the intravenous group died (p = 0.302).
4 Discussion
Administering IR tacrolimus orally directly after LuTx leads to a higher variability in tacrolimus concentrations in comparison to continuous intravenous administration. The oral group had a significantly higher IPV% and lower TTR% than the intravenous group in the first 14 days after LuTx. In general, the occurrence of AKI did not differ between oral and intravenous administration. The occurrence of AKI stage 1 was significantly higher after oral administration of tacrolimus. Keeping the total number of clinically diagnosed cases of acute rejection in mind, the frequency of clinically diagnosed acute rejection in the oral compared to the intravenous group appeared to be 28% higher, without statistical significance. ICU and hospital mortality rate and ICU length of stay were similar for both groups.
To our knowledge, this is the largest study in LuTx providing insightful information on the relationship between the administration route of tacrolimus in the early post-LuTx period and the variability in whole blood tacrolimus concentrations. The higher variability in the oral group may be primarily caused by highly variable bioavailability, which is mainly bypassed by the intravenous administration route. It has been shown that the bioavailability of tacrolimus is the most important factor for fluctuations in whole blood concentrations in orally treated patients and bioavailability may even vary up to 55% shortly after LuTx [11].
Variability in tacrolimus blood concentrations can be substantial among lung transplant recipients, even when adjusting for factors such as age, body weight, and concomitant medications [19]. The genetic polymorphisms of CYP3A enzymes mainly responsible for tacrolimus’ metabolism, particularly CYP3A5*3 and CYP3A4*22, and the transporter ABCB1 variants have been implicated as major contributors to the interindividual variability in tacrolimus PK [19, 20]. Moreover, drug–drug interactions involving CYP3A inducers or inhibitors can significantly alter tacrolimus metabolism, leading to subtherapeutic or toxic blood concentrations, respectively [21]. In addition to interindividual variability, tacrolimus blood concentrations may also vary within the same individual over time, especially shortly after transplantation. Factors such as inflammation, severe bleeding, shock, and organ dysfunction with gut dysmotility and liver dysfunction can influence the IPV% in tacrolimus PK directly after transplantation. Specifically, gut dysmotility is a common complication in the direct postoperative phase with a possible influence on the bioavailability of oral tacrolimus [11].
The time that tacrolimus concentrations were within the therapeutic range was shown to be longer with continuous intravenous administration compared to intermittent oral administration. After oral administration of tacrolimus, the TTR% was about 35% when therapeutic ranges of 12–15 μg/L and 10–15 μg/L were applied in the first and second week after LuTx, respectively. Ensor et al., observed a median TTR% of 21% for a therapeutic range of 12–15 μg/L in the first 6 months and 10–12 μg/L up until 1 year after LuTx [3]. In another study in lung transplant recipients, receiving oral tacrolimus in the direct post-LuTx period, a TTR% of 47% was observed, using a therapeutic range of 10–15 μg/L [5]. These are low numbers for a drug for which frequent TDM is conducted. In a recently published cohort study including 67 LuTx recipients receiving tacrolimus continuously intravenously within the first 14 days after LuTx applying a therapeutic range of 10–15 µg/L, the median percentage of tacrolimus TTR% was 35.7% [22]. These findings align closely to our TTR% of 34.6% in the intravenous group, in which a therapeutic range of 12–15 µg/L in the first week and 10–15 µg/L in the second week after LuTx was applied. These studies show the challenges in maintaining whole blood tacrolimus concentrations within the therapeutic range for oral and intravenous administration. Nevertheless, intravenous administration seems to be superior to oral administration.
It is further noticeable that there is no indisputable therapeutic range for tacrolimus after LuTx [23]. In the second consensus report on therapeutic monitoring of tacrolimus, it is stated that the therapeutic range of 15–20 µg/L early after LuTx must be revised [23], because it has been shown that a trough concentration above 15 µg/L has an increased risk of AKI in these patients [9]. Additionally, a subtherapeutic concentration may lead to higher rejection rates in LuTx patients [2]. Since dose adjustments may lead to overcompensation, resulting in more severe toxic or subtherapeutic concentrations, a concentration just beneath or above the therapeutic range is generally accepted, thereby negatively influencing TTR. Moreover, with continuous intravenous dosing, the therapeutic range for trough concentrations should be higher than the therapeutic range for trough concentrations in oral dosing, in order to obtain an area under the curve (AUC) exposure similar to that of intermittent dosing. Nevertheless, in our study, we did not find more adverse effects compared to oral treatment. Currently, no consensus is present regarding the optimal therapeutic range shortly after LuTx. Ultimately, it is of utmost importance to define specific therapeutic ranges for the postoperative LuTx tacrolimus whole blood concentrations for oral and intravenous administration to guide transplant doctors and improve tacrolimus treatment.
A standardized approach to diagnose acute rejection early after LuTx is lacking in both clinical care and in research. In a study conducted by Katada et al., there was no observed correlation between clinically diagnosed acute rejection within 2 weeks after LuTx and tacrolimus TTR [4]. However, they did report TTR to be a predictor for acute rejection after 4 weeks, albeit in a small sample of four patients. Kao et al., correlated routine biopsy-proven acute rejections with tacrolimus TTR [5]. In 157 recipients who underwent routine bronchoscopies, acute rejection was diagnosed in 20.9% and 25.7% of the biopsies, taken at 1 and 2 months post-LuTx, respectively, while no difference was found between TTR for patients with (46%) and without (47%) acute rejection. In the current study, the frequency of clinically diagnosed acute rejection within 6 weeks after LuTx tended to be 28% higher in the oral group than in the intravenous group. While this outcome did not meet the threshold for statistical significance, it may still be of relevance. Acute rejection in LuTx is associated with an unfavorable long-term graft outcome [24, 25]. Consequently, our findings may hold clinical significance. Nevertheless, more research is needed to explore this further, preferably with biopsy-proven rejection data.
There was no difference in the overall rate of AKI stage 1–3. This study only showed an effect of the tacrolimus route of administration on AKI stage 1. This could be due to the higher variability of the tacrolimus blood concentrations in the oral group. However, AKI is multifactorial and not all risk factors have been included in analyses. Moreover, no information was available about pre-LuTx pulmonary hemodynamics/right ventricular function, post-LuTx inflammation status, shock, duration of ischemia of the lung allograft, or the use of concomitant nephrotoxic medication, and were therefore not studied. When comparing our results to a large meta-analysis including > 40,000 LuTx recipients, the AKI incidence (stage 1–3), according to the KDIGO criteria, was lower for both groups in our study (42.6% for the intravenous group and 46.0% for the oral group vs 53%) [7]. In another large multinational study, including 1.800 ICU patients, the AKI incidence (stage 1–3) was 57%, with a severe AKI (stage 2 or 3) incidence of 39% and an incidence of 13.5% for AKI with need for RRT. [26] As seen in this study by Hoste et al., higher stages of AKI are associated with higher mortality rates in ICU patients, the OR for mortality and stage 1 AKI being 2.19 (95% CI 1.44–3.35) compared to no AKI, and could therefore be a clinically significant disadvantage for oral tacrolimus treatment. If we stratified by higher and lower IPV%, patients in the intravenous group with a lower IPV% had a higher AKI rate than patients with higher IPV%. This is a striking result, but could be explained by a higher TAR% in this intravenous group, while AKI is predominantly influenced by AUC.
Identified confounders for AKI were the need for ECLS in the first 14 days post-LuTx and the lowest hematocrit in the first 14 days post-LuTx. Low hematocrit increases the unbound tacrolimus plasma concentration [27,28,29]. Hematocrit in the oral group was higher than in the intravenous group, which could have had an effect on toxicity, such as nephrotoxicity. Additionally, the group without ECLS had a larger proportion of patients with obstructive airway disease as the reason for LuTx. Obstructive airway disease has been found to be predictive for a worse renal outcome [28]. All these factors could explain the higher AKI incidence in this subgroup.
The use of two large cohorts added to the strength of this study. In addition, the LuTx protocols were similar and tacrolimus concentrations were determined with the same analysis method: LC-MS/MS. The latter is in contrast to Gallagher et al., Kao et al., and Katada et al., who used immunoassay to analyze tacrolimus levels, which is known to have cross-reactivity with tacrolimus metabolites [2, 4, 5]. This potentially leads to a higher variability and makes interpretation more difficult. Whereas we compared PK variability between two administration routes, previously mentioned studies have focused on the effects of variability, often defined as the coefficient of variance or SD with only one administration route [2, 5]. These approaches ignore the outliers and may soften the observed effect.
Despite the abovementioned strengths, there are limitations in view of the retrospective nature of this study.
Due to challenges in data collection, information on tacrolimus doses and drug–drug interactions with tacrolimus could not be incorporated into the multiple linear regression model. Consequently, we were not able to determine the length of intravenous administration nor exclude peak concentrations once the switch to oral administration was made. As a result, it was not possible to correct the calculation of IPV% for dose adjustments. Doses are often altered in the early post-transplantation period, and this may in part explain the observed IPV%. Regardless, the switch to oral administration is only made after clinical stabilization, a period in which the gastro-intestinal blood supply and uptake of tacrolimus have stabilized. The contribution of drug–drug interactions to the results is expected to be small because the protocols for administration of co-medication were comparable for both hospitals. It would be desirable to confirm the results from this study in a randomized controlled trial with a direct comparison of oral and intravenous administration.
Further, even though we attempted to exclude tacrolimus peak concentrations, we cannot be certain that we excluded all misclassified ‘supratherapeutic trough’ concentrations, which could have led to a variability higher than the variability in reality. This was only relevant for the oral group and once patients in the intravenous group had switched to oral administration.
Finally, we correlated TTR% within the first 14 days to acute rejection within the first 6 weeks post-LuTx, and did not have information on whether patients had adequate tacrolimus concentrations within the desired therapeutic range from week 2 to 6 after LuTx. This would have been useful additional information.
For future perspectives, the individual tacrolimus concentrations should be corrected for the preceding dose before calculating IPV%. Furthermore, it may be interesting to look at the long-term kidney and graft outcomes.
5 Conclusion
The variability in tacrolimus concentrations, measured as IPV%, was higher when tacrolimus was administered orally in the first 14 days after LuTx in comparison to continuous intravenous infusion. Also, the time within the therapeutic range was higher when tacrolimus was administered as continuous intravenous infusion. There was no significant difference in overall renal outcome and clinically diagnosed acute rejection.
References
Chambers DC, Perch M, Zuckermann A, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: thirty-eighth adult lung transplantation report—2021; focus on recipient characteristics. J Heart Lung Transplant. 2021;40(10):1060–72. https://doi.org/10.1016/j.healun.2021.07.021.
Gallagher HM, Sarwar G, Tse T, et al. Erratic tacrolimus exposure, assessed using the standard deviation of trough blood levels, predicts chronic lung allograft dysfunction and survival. J Heart Lung Transplant. 2015;34(11):1442–8. https://doi.org/10.1016/j.healun.2015.05.028.
Ensor CR, Iasella CJ, Harrigan KM, et al. Increasing tacrolimus time-in-therapeutic range is associated with superior one-year outcomes in lung transplant recipients. Am J Transplant. 2018;18(6):1527–33. https://doi.org/10.1111/ajt.14723.
Katada Y, Nakagawa S, Itohara K, et al. Association between time in therapeutic range of tacrolimus blood concentration and acute rejection within the first three months after lung transplantation. J Pharm Health Care Sci. 2022. https://doi.org/10.1186/s40780-022-00256-9.
Kao CC, Segraves J, Parulekar AD. Tacrolimus monitoring parameters are not associated with acute cellular rejection following lung transplantation. Eur J Clin Pharmacol. 2021;77(1):63–9. https://doi.org/10.1007/s00228-020-02976-z.
Chambers DC, Yusen RD, Cherikh WS, et al. The Registry of the International Society for Heart and Lung Transplantation: thirty-fourth adult lung and heart-lung transplantation report—2017; focus theme: allograft ischemic time. J Heart Lung Transplant. 2017;36(10):1047–59. https://doi.org/10.1016/j.healun.2017.07.016.
Lertjitbanjong P, Thongprayoon C, Cheungpasitporn W, et al. Acute kidney injury after lung transplantation: a systematic review and meta-analysis. J Clin Med. 2019;8(10):1–19. https://doi.org/10.3390/jcm8101713.
Braithwaite HE, Darley DR, Brett J, Day RO, Carland JE. Identifying the association between tacrolimus exposure and toxicity in heart and lung transplant recipients: a systematic review. Transpl Rev. 2021;35(2): 100610. https://doi.org/10.1016/j.trre.2021.100610.
Sikma MA, Hunault CC, van de Graaf EA, et al. High tacrolimus blood concentrations early after lung transplantation and the risk of kidney injury. Eur J Clin Pharmacol. 2017;73(5):573–80. https://doi.org/10.1007/s00228-017-2204-8.
Miano TA, Flesch JD, Feng R, et al. Early tacrolimus concentrations after lung transplant are predicted by combined clinical and genetic factors and associated with acute kidney injury. Clin Pharmacol Ther. 2020;107(2):462–70. https://doi.org/10.1002/cpt.1629.
Sikma MA, Hunault CC, Van Maarseveen EM, et al. High variability of whole-blood tacrolimus pharmacokinetics early after thoracic organ transplantation. Eur J Drug Metab Pharmacokinet. 2020;45(1):123–34. https://doi.org/10.1007/s13318-019-00591-7.
Schumacher L, Leino AD, Park JM. Tacrolimus intrapatient variability in solid organ transplantation: A multiorgan perspective. Pharmacotherapy. 2021;41(1):103–18. https://doi.org/10.1002/phar.2480.
Shuker N, Shuker L, van Rosmalen J, et al. A high intrapatient variability in tacrolimus exposure is associated with poor long-term outcome of kidney transplantation. Transpl Int. 2016;29(11):1158–67. https://doi.org/10.1111/tri.12798.
Koster RA, Dijkers ECF, Uges DRA. Robust, high-throughput LC-MS/MS method for therapeutic drug monitoring of cyclosporine, tacrolimus, everolimus, and sirolimus in whole blood. 2009;31(1):116-125. http://journals.lww.com/drug-monitoring.
Rosendaal FR, Cannegieter SC, Van der Meer FJM, Briet E. A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost. 1993;69(3):236–9. https://doi.org/10.1055/s-0038-1651587.
Kellum JA, Lameire N, Aspelin P, et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl (2011). 2012;2(1):1–138. https://doi.org/10.1038/kisup.2012.1.
Banga A, Mohanka M, Mullins J, et al. Characteristics and outcomes among patients with need for early dialysis after lung transplantation surgery. Clin Transplant. 2017. https://doi.org/10.1111/ctr.13106.
Puttarajappa CM, Bernardo JF, Kellum JA. Renal complications following lung transplantation and heart transplantation. Crit Care Clin. 2019;35(1):61–73. https://doi.org/10.1016/j.ccc.2018.08.009.
Coste G, Lemaitre F. The role of intra-patient variability of tacrolimus drug concentrations in solid organ transplantation: a focus on liver, heart, lung and pancreas. Pharmaceutics. 2022. https://doi.org/10.3390/pharmaceutics14020379.
Brunet M, Pastor-Anglada M. Insights into the pharmacogenetics of tacrolimus pharmacokinetics and pharmacodynamics. Pharmaceutics. 2022;14(9):1–17. https://doi.org/10.3390/pharmaceutics14091755.
Christians U, Jacobsen W, Benet LZ, Lampen A. Mechanisms of clinically relevant drug interactions associated with tacrolimus. Clin Pharmacokinet. 2002;41(11):813–51. https://doi.org/10.2165/00003088-200241110-00003.
Sohn YM, Ko RE, Park HJ, et al. Clinical pharmacokinetic study of tacrolimus in continuous intravenous administration for lung transplantation. J Thorac Dis. 2023;15(6):3431–6. https://doi.org/10.21037/jtd-22-1760.
Brunet M, Van Gelder T, Åsberg A, et al. Therapeutic drug monitoring of tacrolimus-personalized therapy: second consensus report. Ther Drug Monit. 2019;41(3):261–307. https://doi.org/10.1097/FTD.0000000000000640.
Hopkins PM, Aboyoun CL, Chhajed PN, et al. Association of minimal rejection in lung transplant recipients with obliterative bronchiolitis. Am J Respir Crit Care Med. 2004;170(9):1022–6. https://doi.org/10.1164/rccm.200302-165OC.
Hachem RR, Khalifah AP, Chakinala MM, et al. The significance of a single episode of minimal acute rejection after lung transplantation. Transplantation. 2005;80(10):1406–13. https://doi.org/10.1097/01.tp.0000181161.60638.fa.
Hoste EAJ, Bagshaw SM, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411–23. https://doi.org/10.1007/s00134-015-3934-7.
Sikma MA, Hunault CC, Huitema ADR, De Lange DW, Van Maarseveen EM. Clinical pharmacokinetics and impact of hematocrit on monitoring and dosing of tacrolimus early after heart and lung transplantation. Clin Pharmacokinet. 2020;59(4):403–8. https://doi.org/10.1007/s40262-019-00846-1.
Størset E, Holford N, Midtvedt K, Bremer S, Bergan S, et al. Importance of hematocrit for a tacrolimus target concentration strategy. Eur J Clin Pharmacol. 2014;70(1):65–77. https://doi.org/10.1007/s00228-013-1584-7.
Hebert MF, Zheng S, Hays K, Shen DD, Davis CL, et al. Interpreting tacrolimus concentrations during pregnancy and postpartum. Transplantation. 2013;95(7):908–15. https://doi.org/10.1097/TP.0b013e318278d367.
Lund LH, Edwards LB, Dipchand AI, et al. The Registry of the International Society for Heart and Lung Transplantation: thirty-third adult heart transplantation report—2016; focus theme: primary diagnostic indications for transplant. J Heart Lung Transplant. 2016;35(10):1158–69. https://doi.org/10.1016/j.healun.2016.08.017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for conducting this study.
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
The study was performed in accordance with the guidelines for Strengthening the Reporting of Observational Studies in Epidemiology (STROBE), and conducted according the guidelines in the Declaration of Helsinki and the Declaration on Organ Trafficking and Transplant Tourism. The medical ethical review committee of the University of Utrecht waived the ethical approval (number 22-510) in view of the retrospective nature of the study and use of only routinely documented patients data.
Authors’ Contributions
All authors contributed to the study conception and design. Study preparation, data collection, and analyses were performed by JvD and HG. The first draft of the manuscript was written by JvD, HG, EU, and MAS. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Consent to participate
Not applicable.
Consent for Publicaiton
Not appliable
Code Avaialbility
Avaialble upon reasonable request
Availability of Data and Material
Avaialble upon reasonable request
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
van Dommelen, J.E.M., Grootjans, H., Uijtendaal, E.V. et al. Tacrolimus Variability and Clinical Outcomes in the Early Post-lung Transplantation Period: Oral Versus Continuous Intravenous Administration. Clin Pharmacokinet 63, 683–693 (2024). https://doi.org/10.1007/s40262-024-01368-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-024-01368-1