Abstract
Background and Objective
During the COVID-19 pandemic, trials on convalescent plasma (ConvP) were performed without preceding dose-finding studies. This study aimed to assess potential protective dosing regimens by constructing a population pharmacokinetic (popPK) model describing anti-SARS-CoV-2 antibody titers following the administration of ConvP or hyperimmune globulins (COVIg).
Methods
Immunocompromised patients, testing negative for anti-SARS-CoV-2 spike antibodies despite vaccination, received a range of anti-SARS-CoV-2 antibodies in the form of COVIg or ConvP infusion. The popPK analysis was performed using NONMEM v7.4. Monte Carlo simulations were performed to assess potential COVIg and ConvP dosing regimens for prevention of COVID-19.
Results
Forty-four patients were enrolled, and data from 42 were used for constructing the popPK model. A two-compartment elimination model with mixed residual error best described the Nab-titers after administration. Inter-individual variation was associated to CL (44.3%), V1 (27.3%), and V2 (29.2%). Lean body weight and type of treatment (ConvP/COVIg) were associated with V1 and V2, respectively. Median elimination half-life was 20 days (interquartile range: 17–25 days). Simulations demonstrated that even monthly infusions of 600 mL of the ConvP or COVIg used in this trial would not achieve potentially protective serum antibody titers for > 90% of the time. However, as a result of hybrid immunity and/or repeated vaccination, plasma donors with extremely high antibody titers are now readily available, and a > 90% target attainment should be possible.
Conclusion
The results of this study may inform future intervention studies on the prophylactic and therapeutic use of antiviral antibodies in the form of ConvP or COVIg.
Clinical trial registration number
NL9379 (The Netherlands Trial Register).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this study, the population pharmacokinetic model of convalescent plasma and hyperimmune globulins containing anti-SARS-CoV-2 antibodies is established for the first time. This way we were able to show that very high-titer agents are needed to achieve an optimal dosing regimen for these products. The population PK model can be applied for designing trials during future pandemics if application of polyclonal antibody therapy is considered as prevention against or treatment of viral infections. |
1 Introduction
Since the start of the pandemic, COVID-19 has taken millions of lives [1]. Effective vaccines can now prevent severe COVID-19 disease, hospitalization and mortality [2,3,4]. Unfortunately, a heterogeneous group of patients (e.g., those with solid organ transplant, hematological malignancies, or with anti-CD20 therapy) still have a poor or completely absent humoral immune response after primary vaccination as well as boosters [5]. They continue to be at risk for a prolonged and/or severe COVID-19 disease [6].
By mid-2021, several monoclonal virus neutralizing antibodies (mAbs) had become available as a treatment in parts of the world and can also be used as pre- or post-exposure prophylaxis [7, 8]. Monoclonal virus neutralizing antibodies target one specific epitope in the spike protein. Unfortunately, subsequent SARS-CoV-2 variants accumulated mutations in these epitopes, which resulted in loss of activity against these variants [9, 10].
In contrast to mAbs, polyclonal antibodies (pAbs) may be less susceptible to changes in the spike protein [11, 12]. Both convalescent plasma (ConvP) and hyperimmune globulins (COVIg) are forms of pAbs. Convalescent plasma is plasma from donors who have recovered from or were vaccinated against SARS-CoV-2 [13]. Hyperimmune globulin is an intravenous immunoglobulin product produced from pooled plasma from more than 1000 donors and included ConvP donations [14]. The main advantage of ConvP is that it can be collected very early on in a pandemic, but its antiviral activity varies between each donor. In contrast, it takes several months to produce a first batch of COVIg, but it is more polyclonal than ConvP, and ABO blood group matching is not required. Hyperimmune globulins may exhibit batch-to-batch variability; however, it is still more consistent and comparable across different batches than between individual ConvP donations.
An unprecedented number of trials on the efficacy of ConvP and a few on COVIg as a treatment for COVID-19 were completed during the first 24 months into the pandemic [15, 16]. The results of these trials have been contradictory. As with mAbs, most evidence in favor of ConvP has been generated in patients very early after symptom onset and in the context of immunodeficiency [17, 18]. More importantly, several animal studies and a recent meta-analysis on outpatient ConvP therapy showed that a high enough anti-SARS-CoV-2 spike antibody titer is essential to observe a therapeutic benefit [16, 17, 19]. Monoclonal virus neutralizing antibodies as well as pAbs may also be used to prevent SARS-CoV-2-virus infections in immunocompromised patients who lack an endogenous antibody response after vaccination. However, dosing regimens of ConvP or COVIg that result in a potentially protective neutralizing antibody (Nab) titer for a minimum duration of for example, 28 days, are unknown because proper dose-finding studies with ConvP and COVIg remain unavailable.
This study aimed to establish a population pharmacokinetic (PK) model that is able to predict anti-SARS-CoV-2 antibodies titers after infusion of ConvP or COVIg and can be applied to assess potential protective dosing regimens.
2 Methods
2.1 Study Design
A single-center, open label, Phase I/II prospective non-randomized trial (Trial NL9379) was conducted at the Erasmus Medical Center (Rotterdam, the Netherlands). The protocol was approved by the Dutch competent authority (CCMO) and the institutional review board (METC) at Erasmus MC. Written informed consent was obtained from all patients.
Based on the availability of ConvP and later of COVIg, the inclusion of a total of 104 patients was planned across groups of different doses and products. In supplementary material S1, Figure S1, the study design is presented in detail. Treatment allocation (ConvP/COVIg) was open-label. Eight study arms were created with different volumes and concentrations. We decided to first recruit patients in the COVIg arms since no ABO compatibility is required. The batches with high neutralizing antibody (Nab) titers were tested first because this minimized the risk of underdosing. Also, when a rapid clearance of Nab in patients receiving the high-titer COVIg would be observed, testing with the low Nab-titer batches would no longer be required. Patients in the ConvP group were allocated to a predefined volume and Nab-titer based on ABO compatibility. Patients included in the COVIg arm could participate a second time in a ConvP arm of the study at the time they had become SARS-CoV-2 spike antibody negative.
2.2 Study Products
Convalescent plasma was provided by the Dutch blood bank (Sanquin Blood Supply). Donors met the standard plasma donor criteria, had a history of symptomatic COVID-19, and had recovered for at least 14 days. Hyperimmune globulin was manufactured by Prothya Biosolutions and provided by the Dutch Ministry of Health, Welfare and Sport. These particular batches were derived from pooled plasma from at least 1000 donors, including ConvP donations. Both products were produced while the ancestral variant (Wuhan-1) type was dominant in the Netherlands and, therefore, the Nab-titer against this strain was measured. The Nab-titer was measured by using a virus neutralization test, methods of this test are described in the supplementary material (S2). Antibody treatment was administered intravenously. Since ConvP was collected before anti-SARS-CoV-2 vaccines had become available, plasma with very high Nab-titers was rare and the majority of the ConvP from these non-vaccinated donors had a Nab-titer ranging between 270 and 500 IU mL−1. In this study, ConvP with a Nab-titer of 500 and 910 IUmL−1 was used and is referred to as intermediate-titer and high-titer ConvP, respectively. By pooling regular plasma with ConvP, Prothya was able to produce two batches of COVIg with an increased Nab-titer of 270 and 910 IU mL−1. These products will be referred to as low-titer and high-titer COVIg, respectively. The Nab-titer, given in IUmL−1, is a unit of antibody neutralization of the ancestral SARS-COV-2 variant, as described by Nguyen et al. It facilitates the comparison of Nab-titers between a broad range of in-house virus neutralization tests [20].
Because IgG titers correlated well with neutralization assays of the ancestral virus, the LIAISON® SARS-CoV-2 TrimericS IgG assay (DiaSorin) was used for measuring anti-SARS-CoV-2 IgG antibodies [21]. This strategy avoided potential capacity issues in the laboratory since virus neutralization tests are much more labor intensive. In addition, the turn-over time of virus neutralization tests is much longer. The LIAISON® SARS-CoV-2 Trimerics IgG assay comprised a chemiluminescence immunoassay (CLIA) determining the anti-trimeric spike protein-specific IgG antibodies. The assays manual and the performance characteristics can be found in supplementary material S3 Results of the CLIA are reported in binding antibody units/mL (BAUmL−1), which is the preferred unit for binding capacity by the WHO [21,22,23]. Throughout this manuscript, we will report results from this test as the CLIA antibody test (CAT) titer in BAUmL−1. Chemiluminescence immunoassay was also performed on 11 of the 13 administered ConvP units from which median binding capacities were 3230 BAU mL−1 and 3070 BAU mL−1 for the intermediate and high Nab-titer, respectively. Chemiluminescence immunoassay was performed ten times on the high Nab-titer COVIg batch (910 IU mL−1), from which a median of 3985 BAU mL−1 was obtained. For a rough estimate of the Nab-titer in IU mL−1, the result of the LIAISON® SARS-CoV-2 TrimericS IgG assay can be divided by 4, more details can be found in supplementary material S4.
2.3 Patient Selection
Patients were aged at least 18 years and had no anti-SARS-CoV-2 antibodies at baseline. First, patients who had received B-cell-depleting therapy were included but after the start of the vaccination campaign, all patients lacking anti-SARS-CoV-2 antibodies at least two weeks after full vaccination (two mRNA vaccines, two adenovirus vector vaccines [ChAdOx1-S], or one adenovirus vector vaccine [Ad26.COV2.S]) could participate in the study as well. Patients were screened with a point-of-care antibody test (Roche SARS-CoV-2 Rapid Antibody Test®). Negative test results were verified by the DiaSorin CLIA test and were deemed negative if CAT titers were < 33.8 BAU mL−1 according to the manufacturer’s instructions [21]. Patients had no symptoms of SARS-CoV-2 infection and tested negative with a qPCR test at the time of screening for the study.
2.4 Clinical and Biochemical Monitoring
SARS-CoV-2 spike antibody measurement was performed using CLIA at baseline and, subsequently, after 24 and 48 hours and after 1, 2, 4, 6, 8, 12, 18, and 24 weeks or until the CAT titer had become negative (< 33.8 BAU mL−1) again. Blood sampling was also halted if the patient received another anti-SARS-CoV-2 vaccination during follow-up or had a breakthrough infection.
2.5 Primary Endpoints
2.5.1 Population Pharmacokinetic Analysis
To perform a population PK analysis, the measured CAT titers versus time curves from ConvP and COVIg were described using non-linear mixed-effect modeling with NONMEM v7.4 (ICON Development Solutions, Ellicott City, MD, USA), which was guided using PsN v4.9.0. Pirana v2.9.9 was used for model management and R v4.2.1 (R Core Team, 2020) with Xpose v4.5.3 were used for graphical model diagnostics [24,25,26]. For obtaining the model parameters, first-order conditional estimation (FOCE) was applied with epsilon-eta interaction.
2.5.2 Model Development
Model development commenced with evaluating the most parsimonious compartment model to describe the CAT titer versus time data with initial parameter values obtained from the literature [27, 28]. For constructing the statistical model, the residual unexplained variability (RUV) was evaluated using an additional, proportional, or mixed (additive and proportional) error model. Moreover, inter-individual variability (IIV) was evaluated for each parameter separately using a log-normal distribution. Inter-occasion variability (IOV) was not estimated, as only data from one dosing event were collected. Model building was conducted using a stepwise approach, as the addition of parameters to the model was evaluated one by one.
2.5.3 Covariate Analysis
In the covariate analysis, the patient and treatment characteristics were used to explain the obtained IIV for the model PK parameters. Selection of the covariate relationships was based on biological and clinical plausibility. For evaluating the dichotomous covariate relationships, the following model was applied:
in which θTV,i is the typical value for the individual patient i, θpop is the population PK parameter value, θcov the parameter describing the covariate effect and COV is the covariate value being 1 if present and 0 otherwise. For the continuous covariate relationships, the following relationships (linear, power, and exponential) were applied:
in which COVmed is the median for the covariate value. Before applying a covariate model, the plausibility of that relationship was first evaluated using graphical exploration. The covariate model was constructed using a standard forward inclusion (p = 0.05, df = 1) and backward elimination (p = 0.01, df = 1) procedure. For a list of the evaluated covariate relationships, see Supplementary material S5.
2.5.4 Model Evaluation
The ability of the model to predict the CAT titer measurements was described using an objective function value (OFV). As the OFV is χ2 distributed, the difference between the OFVs (dOFV) from two hierarchical models was used for model selection and dOFV values of 3.84 and 6.64 indicated a significant difference of p < 0.05 and p < 0.01 for one degree of freedom, respectively.
Model evaluation and selection were also based on graphical exploration using goodness-of-fit (GOF) plots, and prediction-corrected visual predictive checks (pcVPCs). Furthermore, the robustness of the parameter estimation from the final model was evaluated by non-parametric bootstrap analysis with 2000 replications.
2.5.5 Dosing Regimen Simulation
To explore which dosing regimen would result in predefined CAT titer targets, Monte Carlo simulations of different dosing regimens were conducted using the final model. The cut-offs were based on prior research by different research groups. Feng et al showed that a titer of 264 BAU mL−1 was associated with 80% vaccine efficacy whereas Goldblatt et al and Dimeglio et al reported 150 BAU mL−1 as sufficient for offering protection [29,30,31]. Based on this, we examined simulations for a cut-off of 100, 150, 250 and 300 BAU mL−1. For the covariate relationships of the final model, values were taken randomly from the study cohort. Dosing regimens were rounded to the nearest practical volume.
2.5.6 Secondary Endpoints
To evaluate the protective effect of ConvP and COVIg, patients were instructed to undergo PCR testing when they would become symptomatic in order to detect potential breakthrough SARS-CoV-2 infections. If possible, the viral strain was sequenced for patients admitted to the hospital. For investigating the safety of ConvP and COVIg, serious adverse events (SAEs) were assessed.
3 Results
3.1 Patient Population and Follow-Up
Patients were screened for eligibility between April 2021 and April 2022. The study was terminated prematurely due to the emergence of the Omicron variant (B.1.1.529), which became the dominant variant in early 2022 in the Netherlands [32]. Indeed, as the ConvP and COVIg available for the study had a much lower Nab-titer against this B1.1.529 variant, we did not expect any further potential benefit from study participation for the individual patient.
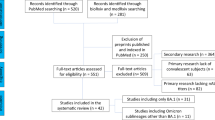
In total, 60 patients were screened and 44 were enrolled in the study (Fig. 1). Patients were allocated to the intermediate and high Nab-titer groups first. One patient in the COVIg group was excluded from further analysis since the confirmatory anti-SARS-CoV-2 antibody test turned out positive at baseline before dose administration. In addition, one patient from the ConvP group was excluded since this patient accidently received plasma without SARS-CoV-2 neutralizing antibodies. Demographics and baseline characteristics were similar for both treatment groups (Table 1 and supplementary material S6).
CONSORT flow diagram: patient enrollment and allocation of treatment. For each of the eight treatment cohorts (P1 to P4 and C1 to C4), the neutralizing antibody titers and the administered volume are depicted. N depicts the number of patients assigned to the corresponding treatment cohort. CLIA chemiluminescent immuno-assay, ConvP convalescent plasma, COVIg hyperimmune globulins containing anti-SARS-CoV-2 antibodies
In total, 86% of the patients (36/42) could be followed until CAT titers had become negative again. Antibody measurement was halted in three patients because of a breakthrough infection, and in one patient due to an antibody response after an additional booster vaccination during follow-up. In one patient, antibodies remained present after 24 weeks. However, the concentration of antibodies on this last study visit was nearly negative (35.8 BAU mL−1).
3.2 Population PK Analysis
In total, 326 data points from 42 patients were used for construction of the population PK model. Ten (3.1%) data points were missing due to patients not showing up for blood sampling. The CAT titers obtained after dose administration were most adequately described using a two-compartment model with a mixed residual error model and IIV associated with CL, V1, and V2 (Table 2). The latter model was subsequently used for the covariate analysis. In the covariate analysis, lean body weight allowed to explain 6.5% of the estimated IIV for V1 using a power relationship most adequately. Moreover, a dichotomous covariate relationship distinguishing between the administration of ConvP or COVIg allowed explaining 15.3% of the IIV estimated for V2. Using the latter covariate relationship, the value for V2 was increased by a factor of 1.99 when ConvP was administered. This reduced the population PK parameter value of the base model estimated for V2 from 2700 mL to 1640 mL.
In the group receiving high Nab-titer COVIg, CAT titers were measurable for a median duration of 41 (27–56) and 56 (52–84) days after 150 mL or 300 mL, respectively. Antibodies remained detectable for a longer time in patients who received ConvP than those who received COVIg, independent of the administered volume and Nab-titer (Table 2). However, the median elimination half-life of ConvP and COVIg was comparable with 18.6 days and 20.3 days, respectively (supplementary material S7). As expected, the peak CAT titer was highest in the group that received 600 mL ConvP with a Nab-titer of 500 IU mL−1. Duration of seropositivity for anti-SARS-CoV-2 antibodies and peak antibody concentration are presented in Table 2.
3.3 Model Evaluation
In Fig. 2, the GOF plots for the final model are shown in which the adequacy of the model predictions is demonstrated. Both the individual and population predictions of the CAT titers were symmetrically distributed around the line of identity (y = x), showing that accurate predictions of the CAT titers from ConvP and COVIg were obtained using the final model. Moreover, the prediction-corrected visual predictive check (pcVPC) (Fig. 3a) showed the accuracy of the final model as all quantiles from the measured CAT titers (solid lines) were within their respective prediction intervals (shaded areas). However, when presented on the logarithmic scale the latest measured CAT titers were slightly above the simulated CAT titers (Fig. 3b). The latter was due to the lowest amount of measured CAT titers being present for that time period. The pcVPC is also presented stratified for the study drug (ConvP or COVIg) in supplementary material S8 (Fig. S2; linear scale) and S9 (Fig. S3; logarithmic scale).
Goodness-of-fit plot from the final model. A Population predicted versus measured anti-SARS-CoV-2 antibody titers. B Individual predicted versus measured anti-SARS-CoV-2 antibody titers. C Conditional weighted residuals (CWRES) versus population predicted anti-SARS-CoV-2 antibody titers. D CWRES versus time after dose administration. Anti-SARS-CoV-2 antibody titers were measured using the LIAISON® SARS-CoV-2 TrimericS IgG assay and reported as binding antibody units per milliliter (BAU mL−1). In a, b, the blue line depicts the locally weighted smoothing (LOESS) line, whereas in Figures 2c and 2d the red lines are the linear regression line
Prediction-corrected Visual Predictive Check from the final model. A pcVPC with the measured and simulated anti-SARS-CoV-2 antibody titers on a linear scale. B pcVPC with the observed and simulated anti-SARS-CoV-2 antibody titers on a logarithmic scale. Anti-SARS-CoV-2 antibody titers were measured using the LIAISON® SARS-CoV-2 TrimericS IgG assay and reported as binding antibody units per milliliter (BAU mL−1). Black dots represent the measured anti-SARS-CoV-2 antibody titers for all patients. Solid grey line represents the median and the dashed grey lines represent the 2.5th and 97.5th quantiles for the measured anti-SARS-CoV-2 antibody titers. Red and blue-shaded areas show the 95% confidence intervals for the simulated anti-SARS-CoV-2 antibody titers of the individual patients, as obtained by 2000 Monte Carlo simulations using the final model
The bootstrap analysis showed that the model parameters were adequately estimated, as all median parameter estimates from the bootstrap were similar to that of the final model (Table 3).
3.4 Dosing Regimens Simulations
Figure 4 depicts the Monte Carlo simulations evaluating the optimal dosing regimen of ConvP and COVIg. When dosing with 600 mL of ConvP every 56 days (8 weeks), none of the simulated plasma CAT titers achieved the 90% probability target attainment (PTA) for the 300 BAU mL−1 threshold. However, reducing the dosing interval to 28 days and using ConvP with a CAT titer of at least 12,000 BAU mL−1 led to a 90% or higher PTA. For the lowest target of 100 BAU mL−1, the 90% PTA could be achieved with longer dosing intervals as long as ConvP or COVIg with an extremely high CAT titer can be used (e.g., dosing every 8 weeks with 32,000 BAU mL−1 or more).
Probability of target attainment of simulated dosing regimens for ConvP and COVIg. For obtaining prediction for the anti-SARS-CoV-2 antibody titers, Monte Carlo simulations (n = 2000) were applied using the final model. Each row of figures depicts the probability of the target attainment (PTA, %) for different target titers in BAU mL−1 in the serum of the recipient, as displayed in the facet header. The dashed line depicts 90% PTA, which was considered as the cut-off for having a protective effect. The volume of ConvP was set at 600 mL and for COVIg of 300 mL
3.5 Secondary Endpoint
Because recruitment was discontinued after 44 inclusions, the analysis of the secondary endpoints of breakthrough infections and (serious) adverse events was limited by the small sample size. They are available as supplementary material S10.
4 Discussion
In this study, a population PK model predicting the SARS-CoV-2 IgG antibody titers after ConvP and COVIg administration was constructed. The adequacy of the model predictions was demonstrated using GOF plots and a pcVPC. Furthermore, a bootstrap analysis showed the robustness of the parameter estimates from the final model. Lean body weight was associated with V1. Concerning the covariate relationship (drug product) associated with V2, its value increased approximately two times with administration of ConvP as compared with COVIg. Finally, Monte Carlo simulations showed that monthly dosing of ConvP with very high-titer ConvP (12,000 BAU mL−1) could attain the 90% PTA for the 300 BAU mL−1 target. To our knowledge, this is the first population PK model predicting Nab-titer after the administration of ConvP or COVIg.
In general, the elimination half-life of intravenous immunoglobulins ranges from 7 to 21 days. However, less is known about the elimination half-life of IgG subgroups targeting a specific antigen such as the spike protein of SARS-CoV-2 [27, 33]. Before this trial, only a few studies had been performed evaluating the PK and pharmacodynamic (PD) characteristics of these pAbs. In a hamster model very high-titer COVIg (pseudovirus virus neutralization 50% titer: 1/1240) had a median elimination half-life of 124 hours [34]. In children, Gordon et al investigated the PK of high-titer ConvP (Nab-titer of 1/320 anti-spike IgG, Euro-Immun) and found an elimination half-life for anti-SARS-CoV-2 IgG of 15 days whereas the median elimination half-life of pAbs in our population ranged between 18.6 and 20.6 days [28].
A two-compartment model described the measured CAT titers most adequately. In contrast to our model, Gordon et al did not find body weight associated with clearance of the antibodies [28]. During the first elimination phase, a rapid decline in CAT titers was observed in the first days after dose administration. During the distribution phase, IgG leaves the blood vasculature into lymph and extracellular compartments and slowly diffuses back into the blood circulation [27]. However, due to distinct antibody compositions, ConvP and COVIg exhibit different polyclonalities, leading to varying PK characteristics. Notably, the volume of distribution from the second compartment (V2) was the only PK parameter showing a significant difference between both products. This suggests that antibodies in ConvP have a greater tendency to distribute beyond the vasculature into other body fluids as compared with COVIg. While further investigation is warranted to determine the physiological and pharmacological plausibility of this covariate relationship, differences in processing methods, antibody composition, purity, and molecular structure likely contribute to the observed difference in the volume of distribution. Importantly, this difference did not yield significant changes in terminal elimination half-life (see supplementary material S7).
The rapid decline in CAT titers may pose a problem for attaining higher amounts of anti-SARS-CoV-2 antibodies for a long period and, thus, compromising the use in a prophylactic setting [35]. Adjustment of the Fc-receptor in antibodies is a strategy performed in mAbs and can prolong the elimination half-life of these antibodies [33]. Unfortunately, this is not possible in donor-based pAbs. Aside from this rapid decline, dose dilution in the systemic circulation is another factor that brings the need for very high-titer therapy [35]. In this study, the peak antibody titer measured 1 hour after administration in the blood of participants was 11 times lower than the titer in the ConvP or COVIg unit but with a broad IQR of 5–20 times. This was also observed by Shoham et al. [36]. Although elimination half-life of pAbs is long, both the rapid decline in titer and dose dilution are factors that should be taken into account during the practical application of pAb-based prophylaxis in high-risk patients.
In this study, patients who were likely to or had been proven to lack an endogenous anti-SARS-CoV-2 antibody production as a result of B-cell depleting or B- and T-cell suppressive therapies were recruited. In this way, the efficacy of ConvP and COVIg in this patient group could be investigated. However, as the study had to be discontinued prematurely and only three patients had a breakthrough infection during follow-up, no definite conclusions about the titers needed for protection could be drawn. Furthermore, all 3 breakthrough infections occurred at a time when non-ancestral variants were circulating to which the study products had reduced activity.
Since the start of the pandemic, many clinical studies on the efficacy of ConvP and to a lesser extent also COVIg as a treatment for SARS-CoV-2 infected patients have been performed. The results of these studies were mostly disappointing because in hospitalized non-immunocompromised patients no clear beneficial effect was observed [16, 37,38,39,40]. However, most of these trials were performed with plasma from convalescent and non-vaccinated donors. Therefore, donors with extremely high Nab-titers were rare. More recently, a meta-analysis including three RCTs showed that the use of convalescent plasma in immunocompromised patients was associated with a mortality benefit [18]. We previously summarized the available evidence on optimal dosing of ConvP and concluded that patients were underdosed in almost all of these trials [19]. Furthermore, it has become clear that antibody-based therapy works best when given in the first days after symptom onset. Indeed, in a recent meta-analysis of the 5 double-blind randomized trials on ConvP performed in outpatients with < 8 days of symptoms, a significant reduction in hospital admission was only observed when the intervention was given in the first 5 days of symptoms and when plasma with the highest antibody titers was used [17].
To explore the clinical application of the prophylactic use of ConvP and COVIg, a PTA was estimated with a Monte Carlo simulation using 4 antibody titer targets ranging from 100 to 300 BAU mL−1. This range was based on antibody titers that correlate with protection as described by Feng et al and Dimeglio et al ranging from 150 to 264 BAU mL−1 [29,30,31]. However, protection against infection does not come only from humoral immunity, which may implicate that in patients with a B- and T-cell deficiency higher titers may be required. Also, subsequent variants of concern are often much more resilient to vaccine-induced antibodies and higher titers are necessary to offer protection [41]. Dimeglio et al showed that achieving titers over 20,000 BAU mL−1 are necessary to achieve at least 80% of protection against Omicron infections [42]. In the current simulation, a PTA of 300 BAU mL−1 was achieved by administering ConvP or COVIg with at least 12,000 BAU mL−1 every 4 weeks.
This study has its limitations. First, we repeatedly measured antibody concentrations in serum; however, we did not directly measure these antibodies in the respiratory tract (e.g., by performing a nasal wash). In addition, the distribution ratio between antibodies in serum and the bronchoalveolar fluid is unknown. Still, the clinical benefit observed with early administration of high titer plasma suggests that antibodies reach the site of infection [17]. In SARS-CoV-2 uninfected patients, the final model can be used to predict antibody titers over time after an infusion of ConvP or COVIg. However, in patients infected with COVID-19, exogenous antibodies probably have a shorter half-life due to the direct antibody-antigen binding [34]. Also, with every new variant that occurs, the correlation of a SARS-CoV-2 spike antibody titer (in BAU mL−1) with in vitro neutralization of this new variant should be evaluated again. This means that for new variants, much higher targets (e.g., 10,000 rather than 300 BAU mL−1) may be necessary to result in any relevant protection. Fortunately, many plasma donors now have acquired immunity from a combination of infection, vaccination, and booster vaccination. Therefore, donors with extremely high Nab-titers are readily identifiable. Unfortunately, due to the rapidly evolving variant landscape of SARS-CoV-2 and the vaccination uptake, the study was discontinued prematurely and only three breakthrough infections were detected. Therefore, a protective titer could not be estimated. A fixed volume of anti-SARS-CoV-2 antibodies per study arm was chosen instead of a fixed dose per kg bodyweight because the latter would result in spillage of scarcely available ConvP and COVIg as they were provided at fixed volumes.
In conclusion, this is the first dose-finding study in which a population PK model describing anti-SARS-CoV-2 antibody titers after ConvP and COVIg administration was constructed. Lean body weight and the type of pAbs allowed to explain a part of the IIV for V1 and V2, respectively. This population PK model may be a valuable tool for designing trials during future viral pandemics at the time when application of ConvP or COVIg is considered as a prophylactic or therapeutic intervention.
References
Mathieu E. RH, Rodés-Guirao L, Appel C, Giattino C, Hasell J, Macdonald B, Dattani S, Beltekian D, Ortiz-Ospina E, Roser M. Coronavirus (COVID-19) deaths: our world in data; 2022 [updated 30/11/2022. https://ourworldindata.org/covid-deaths.
Moreira ED Jr, Kitchin N, Xu X, et al. Safety and efficacy of a third dose of BNT162b2 Covid-19 vaccine. N Engl J Med. 2022;386:1910–21. https://doi.org/10.1056/NEJMoa2200674.
Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–15. https://doi.org/10.1056/NEJMoa2034577.
Tenforde MW, Self WH, Adams K, et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA. 2021;326:2043–54. https://doi.org/10.1001/jama.2021.19499.
Boyarsky BJ, Werbel WA, Avery RK, et al. Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients. JAMA. 2021;325:2204–6. https://doi.org/10.1001/jama.2021.7489.
Belsky JA, Tullius BP, Lamb MG, et al. COVID-19 in immunocompromised patients: a systematic review of cancer, hematopoietic cell and solid organ transplant patients. J Infect. 2021;82:329–38. https://doi.org/10.1016/j.jinf.2021.01.022.
Levin MJ, Ustianowski A, De Wit S, et al. Intramuscular AZD7442 (tixagevimab-cilgavimab) for prevention of Covid-19. N Engl J Med. 2022;386:2188–200. https://doi.org/10.1056/NEJMoa2116620.
Herman GA, O’Brien MP, Forleo-Neto E, et al. Efficacy and safety of a single dose of casirivimab and imdevimab for the prevention of COVID-19 over an 8-month period: a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2022;22:1444–54. https://doi.org/10.1016/S1473-3099(22)00416-9.
Yamasoba D, Kosugi Y, Kimura I, et al. Sensitivity of novel SARS-CoV-2 Omicron subvariants, BA.2.11, BA.2.12.1, BA.4 and BA.5 to therapeutic monoclonal antibodies. bioRxiv. 2022. https://doi.org/10.1101/2022.05.03.490409.
VanBlargan LA, Errico JM, Halfmann PJ, et al. An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nat Med. 2022;28: 490-5. https://doi.org/10.1038/s41591-021-01678-y.
Focosi D, Tuccori M, Franchini M. The road towards polyclonal anti-SARS-CoV-2 immunoglobulins (hyperimmune serum) for passive immunization in COVID-19. Life (Basel). 2021. https://doi.org/10.3390/life11020144.
Alape-Giron A, Moreira-Soto A, Arguedas M, et al. Heterologous hyperimmune polyclonal antibodies against SARS-CoV-2: a broad coverage, affordable, and scalable potential immunotherapy for COVID-19. Front Med (Lausanne). 2021;8: 743325. https://doi.org/10.3389/fmed.2021.743325.
Sanquin. WP4: improving plasma potency assessment 2020 https://www.support-e.eu/work-packages/wp-4/.
Huygens S, Hofsink Q, Nijhof IS, et al. Hyperimmune globulin for severely immunocompromised patients hospitalized with coronavirus disease 2019: a randomized, controlled trial. J Infect Dis. 2023;227:206–10. https://doi.org/10.1093/infdis/jiac334.
Piechotta V, Iannizzi C, Chai KL, et al. Convalescent plasma or hyperimmune immunoglobulin for people with COVID-19: a living systematic review. Cochrane Database Syst Rev. 2021;5:CD013600. https://doi.org/10.1002/14651858.CD013600.pub4.
Jorda A, Kussmann M, Kolenchery N, et al. Convalescent plasma treatment in patients with Covid-19: a systematic review and meta-analysis. Front Immunol. 2022;13: 817829. https://doi.org/10.3389/fimmu.2022.817829.
Levine AC, Fukuta Y, Huaman MA, et al. Coronavirus disease 2019 convalescent plasma outpatient therapy to prevent outpatient hospitalization: a meta-analysis of individual participant data from 5 randomized trials. Clin Infect Dis. 2023;76:2077–86. https://doi.org/10.1093/cid/ciad088.
Senefeld JW, Franchini M, Mengoli C, et al. COVID-19 convalescent plasma for the treatment of immunocompromised patients: a systematic review and meta-analysis. JAMA Netw Open. 2023;6: e2250647. https://doi.org/10.1001/jamanetworkopen.2022.50647.
Rijnders BJA, Huygens S, Mitja O. Evidence-based dosing of convalescent plasma for COVID-19 in future trials. Clin Microbiol Infect. 2022;28:667–71. https://doi.org/10.1016/j.cmi.2022.01.026.
Nguyen D, Simmonds P, Steenhuis M, et al. SARS-CoV-2 neutralising antibody testing in Europe: towards harmonisation of neutralising antibody titres for better use of convalescent plasma and comparability of trial data. Euro Surveill. 2021;26:2100568. https://doi.org/10.2807/1560-7917.ES.2021.26.27.2100568.
DiaSorin. Liaison SARS-CoV-2 TrimericS IgG assay: A quantitative assay for immune status monitoring with an accurate correlation of neutralizing IgG antibodies. Saluggia, Italy; 2021.
Infantino M, Pieri M, Nuccetelli M, et al. The WHO International Standard for COVID-19 serological tests: towards harmonization of anti-spike assays. Int Immunopharmacol. 2021;100: 108095. https://doi.org/10.1016/j.intimp.2021.108095.
Kristiansen PA, Page M, Bernasconi V, et al. WHO International Standard for anti-SARS-CoV-2 immunoglobulin. Lancet. 2021;397:1347–8. https://doi.org/10.1016/S0140-6736(21)00527-4.
Bauer RJ. NONMEM Tutorial Part I: description of commands and options, with simple examples of population analysis. CPT Pharmacometr Syst Pharmacol. 2019;8:525–37. https://doi.org/10.1002/psp4.12404.
Keizer RJ, Karlsson MO, Hooker A. Modeling and simulation workbench for NONMEM: tutorial on Pirana, PsN, and Xpose. CPT Pharmacometr Syst Pharmacol. 2013;2: e50. https://doi.org/10.1038/psp.2013.24.
Lindbom L, Pihlgren P, Jonsson EN. PsN-Toolkit–a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed. 2005;79:241–57. https://doi.org/10.1016/j.cmpb.2005.04.005.
Barahona Afonso AF, Joao CM. The production processes and biological effects of intravenous immunoglobulin. Biomolecules. 2016;6:15. https://doi.org/10.3390/biom6010015.
Gordon O, Brosnan MK, Yoon S, et al. Pharmacokinetics of high-titer anti-SARS-CoV-2 human convalescent plasma in high-risk children. JCI Insight. 2022. https://doi.org/10.1172/jci.insight.151518.
Feng S, Phillips DJ, White T, et al. Correlates of protection against symptomatic and asymptomatic SARS-CoV-2 infection. Nat Med. 2021;27:2032–40. https://doi.org/10.1038/s41591-021-01540-1.
Dimeglio C, Herin F, Martin-Blondel G, et al. Antibody titers and protection against a SARS-CoV-2 infection. J Infect. 2022;84:248–88. https://doi.org/10.1016/j.jinf.2021.09.013.
Goldblatt D, Alter G, Crotty S, et al. Correlates of protection against SARS-CoV-2 infection and COVID-19 disease. Immunol Rev. 2022;310:6–26. https://doi.org/10.1111/imr.13091.
Variants of the coronavirus SARS-CoV-2: National Institute for Public Health and the Environment; 2022 [updated 07/22/2022. https://www.rivm.nl/en/coronavirus-covid-19/virus/variants.
Kang TH, Jung ST. Boosting therapeutic potency of antibodies by taming Fc domain functions. Exp Mol Med. 2019;51:1–9. https://doi.org/10.1038/s12276-019-0345-9.
Stauft CB, Tegenge M, Khurana S, et al. Pharmacokinetics and efficacy of human hyperimmune intravenous immunoglobulin treatment of severe acute respiratory syndrome coronavirus 2 infection in adult syrian hamsters. Clin Infect Dis. 2022;75:e459–65. https://doi.org/10.1093/cid/ciab854.
Marconato M, Abela IA, Hauser A, et al. Antibodies from convalescent plasma promote SARS-CoV-2 clearance in individuals with and without endogenous antibody response. J Clin Invest. 2022. https://doi.org/10.1172/JCI158190.
Shoham S, Bloch EM, Casadevall A, et al. Transfusing convalescent plasma as post-exposure prophylaxis against severe acute respiratory syndrome coronavirus 2 (Sars-Cov-2) infection: a double-blinded, phase 2 randomized, controlled trial. Clin Infect Dis. 2023;76:e477–86. https://doi.org/10.1093/cid/ciac372.
Group IS. Hyperimmune immunoglobulin for hospitalised patients with COVID-19 (ITAC): a double-blind, placebo-controlled, phase 3, randomised trial. Lancet. 2022;399:530–40. https://doi.org/10.1016/S0140-6736(22)00101-5.
Libster R, Perez Marc G, Wappner D, et al. Early high-titer plasma therapy to prevent severe covid-19 in older adults. N Engl J Med. 2021;384:610–8. https://doi.org/10.1056/NEJMoa2033700.
RECOVERY Collaborative Group. Convalescent plasma in patients admitted to hospital with COVID-19 (RECOVERY): a randomised controlled, open-label, platform trial. Lancet. 2021;397:2049–59. https://doi.org/10.1016/S0140-6736(21)00897-7.
Sullivan DJ, Gebo KA, Shoham S, et al. Early outpatient treatment for covid-19 with convalescent plasma. N Engl J Med. 2022;386:1700–11. https://doi.org/10.1056/NEJMoa2119657.
Cromer D, Steain M, Reynaldi A, et al. Neutralising antibody titres as predictors of protection against SARS-CoV-2 variants and the impact of boosting: a meta-analysis. Lancet Microbe. 2022;3:e52–61. https://doi.org/10.1016/S2666-5247(21)00267-6.
Dimeglio C, Migueres M, Bouzid N, et al. Antibody titers and protection against omicron (BA.1 and BA.2) SARS-CoV-2 infection. Vaccines (Basel). 2022. https://doi.org/10.3390/vaccines10091548.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Contributions
Bart Rijnders, Birgit Koch, Sammy Huygens, and Tim Preijers designed the study. Research was performed by Sammy Huygens and supervised by Bart Rijnders. Sammy Huygens and Tim Preijers analyzed the data and Tim Preijers performed the population PK analysis. The manuscript was written by Sammy Huygens and Tim Preijers, the manuscript was reviewed by Bart Rijnders, Birgit Koch, Francis Swaneveld, Ilona Kleine Budde, and Corine GeurtsvanKessel. Bart Rijnders did the overall supervision of the project.
Funding
This trial was funded by ZonMw under grant number 10430062010002.
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Erasmus Medical Center, Rotterdam (March 15th 2021/MEC-2021-0163). The trial was registered in the Netherlands Trial Register under number NL9379.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Data availability statement
The dataset is available using the online repository DANS-EASY and can be accessed upon reasonable request to the authors. Metadata is shared through CEDAR and can be accessed using the following link: https://covid19initiatives.health-ri.nl/p/Project/27866022694505955.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Huygens, S., Preijers, T., Swaneveld, F.H. et al. Dosing of Convalescent Plasma and Hyperimmune Anti-SARS-CoV-2 Immunoglobulins: A Phase I/II Dose-Finding Study. Clin Pharmacokinet 63, 497–509 (2024). https://doi.org/10.1007/s40262-024-01351-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-024-01351-w